Abstract
Autophagy is an important cellular protein control process, which plays a key role in the regulation of cell homeostasis and pathogenesis of many human diseases including neurodegenerative diseases. Reduced autophagic activity and abnormal protein aggregation are common features of neurodegenerative diseases, including Alzheimer’s disease, Parkinson’s disease, amyotrophic lateral sclerosis, and Huntington’s disease. Therefore, pharmacological regulation of overall autophagy may be helpful for effective treatment of neurodegenerative diseases. In the present study, we find Dynasore, a potent inhibitor of dynamin, can repress the lysosomal localization of mTOR and block the activity of mTORC1, which in turn enhances the nuclear translocation of the master regulators of autophagy including TFE3 and TFEB. We find that autophagic flux is upregulated in Dynasore-treated cells. Moreover, treatment of Dynasore significantly promotes the clearance of protein aggregates formed by mutant huntingtin protein containing expanded polyglutamine (polyQ), but not damaged mitochondria. In contrast, treatment with Dynasore has no effect on the clearance of polyQ aggregates of mutant huntingtin in ATG5-depleted cells, in which autophagy is defective. Taken together, our results indicate that Dynasore affects autophagic degradation of neurodegenerative disease-associated proteins by regulating mTORC1-TFEB signaling.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The damage of neurons and cognitive ability is a common cause of neurodegenerative diseases. The lack of effective disease-modifying therapies and rising incidence rate bring a huge burden to society. Most neurodegenerative diseases share the common features that the patients’ brains contain disease-related protein aggregates and inclusions (Kopito 2000; Ross and Poirier 2005). For example, Aβ peptides and hyper-phosphorylated tau form aggregates or plaques are often found in the brains of Alzheimer disease patients; α-Synuclein is another type of aggregate-prone protein which is often observed in the neurons of substantia nigra in Parkinson disease patients; Huntington disease is an autosomal dominant neurodegenerative disorder caused by expanded CAG repeats in the Huntingtin gene. In Huntington disease (HD), the CAG expansion in the huntingtin gene results in the aggregation of huntingtin (Htt) protein, and mutant Htt is the only disease-associated protein known to cause Huntington disease (Ross and Poirier 2005). Htt is expressed throughout the body and is crucial for the development of the brain. The N-terminal fragments of Htt protein containing polyglutamine (polyQ) tract are degraded in the cells mainly through autophagy (Wong and Cuervo 2010). The normal number of CAG repeats in huntingtin gene is less than 36 in normal people and pathogenic CAG expansion is found in the Huntington disease patients. Previous studies have shown that longer CAG repeats in the huntingtin gene result in longer polyQ expansion in Htt protein and the aggregate-prone feature of mutant Htt (Jana et al. 2001).
It has been well known that autophagy is a selective degradation pathway which is responsible for the clearance of misfolded proteins, protein aggregates, and damaged organelles (Dikic and Elazar 2018). Previous studies have revealed that mTORC1 signaling can regulate autophagic flux via the mTOR activity according to the levels of nutrient, energy, or redox. And recent studies show that TFEB and TFE3 are the master transcription factors, and they can regulate the biogenesis of lysosomes and autophagosomes when localized in the nucleus (Sardiello et al. 2009; Settembre et al. 2011). Under normal physiologic condition, the mTORC1 stays active and mainly locates on the lysosomes. Active mTORC1 phosphorylates TFEB thereby inhibiting the nuclear transportation of TFEB (Martina and Puertollano 2013); thus, autophagy is inhibited. Under nutrient-deficient conditions, including starvation, the mTORC1 is inactive, and TFEB is released from the lysosomes and thereafter transported into the nucleus; thus, autophagosomal and lysosomal biogenesis is increased. Therefore, nuclear TFEB promotes the autophagic flux and increases the clearance of protein aggregates (Laplante and Sabatini 2012; Zoncu et al. 2011).
Dynasore is a potent inhibitor of dynamin which is crucial for clathrin-dependent endocytosis (Macia et al. 2006; Preta et al. 2015). It can inhibit the activity of GTPase of dynamin1, dynamin2, and Drp1 and prevent the formation of vesicles from the membrane. In this study, we found Dynasore can increase autophagic flux through the inhibition of mTORC1 and nuclear translocation of TFEB/TFE3, the master regulators of autophagy and lysosomal biogenesis. Importantly, Dynasore treatment increases the clearance of protein aggregates of mutant Htt in cells through autophagy.
Results
Dynasore Treatment Induces Autophagy in Cells
Given that Dynasore has a strong effect on endocytosis and membrane-associated intracellular trafficking, we hypothesized that it may regulate autophagy. To examine the effect of Dynasore on autophagy, we treated HEK 293 cells with different concentrations of Dynasore and observed the morphologic change of EGFP-LC3, a commonly used marker of autophagy. When the cells were treated with Dynasore, EGFP-LC3 formed punctum structures in the cytoplasm (Fig. 1a). These puncta are LC3 II, the lipid-modified form of LC3 located on autophagosomal membranes, which can promote the expansion and fusion of autophagosome and is considered to be the reporter of autophagy. Next, we used the autophagic flux reporter, mCherry-EGFP-LC3, to test whether Dynasore could enhance the overall function of autophagy. Since EGFP is more easily quenched than mCherry in acidic lysosomes, red dots were considered to be autolysosomes that can reflect the overall function of autophagy, whereas yellow dots (red dots and green dots overlapped) were considered to be autophagosomes that did not fuse with the lysosomes. When treated with Dynasore, the number of autolysosomes was strikingly increased (Fig. 1b). Given that LC3 II level reflects the number of autophagosomes in cells, we observed that the amount of LC3 II, relative to the control, increased with the concentration of Dynasore (Fig. 1c–e). Taken together, our results suggest that treatment with Dynasore, a dynamin GTPase inhibitor, can induce functional autophagy in cells.
Dynasore treatment increases the numbers of autophagic structures in cells. a HEK 293 cells were transfected with EGFP-LC3. Twenty-four hours later, the cells were treated with DMSO, 25 μM or 50 μM Dynasore for another 6 h. Then, the cells were observed under a confocal microscope. Scale bars, 10 μm. b HEK 293 cells were transfected with mCherry-EGFP-LC3 for 24 h and then were treated with DMSO, 25 μM or 50 μM Dynasore for 6 h. The cells were observed under a confocal microscope. Scale bars, 10 μm. c HEK 293 cells were treated with different concentrations of Dynasore for indicated time. Then, the treated cells were collected and Western blot analysis was performed with indicated antibodies to detect LC3-I and LC3-II. GAPDH served as the loading control. The quantification data of relative density of LC3 in cells treated with Dynasore for 6 h (d) or 12 h (e) are indicated as the means ± S.E.M., *P < 0.05; **P < 0.01; ns, not significantly different, one-way ANOVA
Dynasore Treatment Enhances the Formation of Autolysosomes and Autophagy Flux
Based on the observation that Dynasore can induce autophagy in cells, we further explored at which stage it could induce autophagy. We performed starvation assay and Bafilomycin A1 treatment, which blocks the fusion of autophagosome and lysosome, thereby inhibiting the final step of autophagy. Nutrient deprivation (starvation) can stimulate the enhancement of autophagic flux by inhibiting mTOR signaling, which regulates autophagy at an early stage. Cells treated with Dynasore displayed strong autophagy flux similarly as the cells under the starvation condition. Interestingly and importantly, we found that Dynasore treatment could significantly enhance the formation of autolysosomes, similar to starvation treatment, which has been previously shown to increase autophagosome–lysosome fusion (Jean et al. 2015). Moreover, autophagosome–lysosome fusion was completely blocked by Bafilomycin A1 with or without Dynasore (Fig. 2a, b). LC3 II protein levels shown by Western blot were in accordance with the fluorescent observations (Fig. 2c–e). Since the fusion of autophagosomes and lysosomes reflects the overall functional autophagy, our data indicate Dynasore can enhance the autophagic flux.
The regulation of autophagy flux by Dynasore. a HEK 293 cells were transfected with mCherry-EGFP-LC3 for 24 h. Then, the cells were treated with or without 50 μM Dynasore for 6 h. Meanwhile, the cells were incubated in EBSS for 1 h or treated with 100 nM Bafilomycin A1 (which inhibits V-ATPase-dependent acidification and disrupts autophagosome–lysosome fusion) for 6 h. Then, the cells were analyzed by confocal microscope. Scale bars, 10 μm. b The quantification data of autophagosome and autolysosomes in a are indicated as the means ± S.E.M., **P < 0.01; ns, not significantly different, one-way ANOVA. c–e HEK 293 cells were processed as a except the transfection of mCherry-EGFP-LC3. Western blot was used to analyze the protein level of LC3. The quantification data of relative density of LC3 are indicated as the means ± S.E.M., *P < 0.05; ns, not significantly different, one-way ANOVA
Dynasore Treatment Does Not Induce Mitochondrial Damage and Mitophagy
Mitophagy is an essential pathway involved in the selective autophagic clearance of mitochondria. Given that Dynasore can enhance the autophagic flux in cells, we investigated whether it could regulate the removal of damaged mitochondria from cells by mitophagy (Pickrell and Youle 2015). We used a mitophagy probe mt-Keima to reflect autophagic degradation of mitochondria. Keima is a pH-dependent fluorescent protein which emits different-colored signals in neutral or acidic pHs. Under neutral pH, Keima emits the signals at an excitation wavelength of 440 nm. Under acidic pH, Keima emits the signals at an excitation wavelength of 586 nm. Thus, the 561-nm-excited mitochondria-targeting Keima (mt-Keima) signals reflect the quantity of mitochondria in autolysosomes (which indicates functional mitophagy) (Sun et al. 2017). Our results showed that almost no mitophagy was induced in cells without Parkin expression, although mitochondria were damaged by Antimycin A and Oligomycin (A/O) treatments (Fig. 3a). These results are in accordance with other findings (Narendra et al. 2008). When transfected with GFP-tagged Parkin and treated with A/O, the signal of mt-Keima at 561 nm dramatically increased, indicating enhanced mitophagy. Dynasore treatment had no effect on either Parkin translocation or mitophagy in cells (Fig. 3b). Our results suggest Dynasore treatment does not increase mitophagy in cells.
Dynasore treatment has no effect on mitophagy. a HEK 293 cells were transfected with mt-Keima alone. b HEK 293 cells were transfected with mt-Keima and GFP-Parkin. For Dynasore treatment, the cells were treated with Dynasore (50 μM) for 6 h. For A/O treatment, the cells were incubated with Oligomycin and Antimycin A1 (A/O, 1 μg/ml, respectively) for 6 h. Live cells were visualized using confocal microscopy. Scale bars, 10 μm
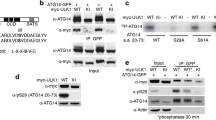
Dynasore Treatment Enhances Autophagy Through the Inhibition of mTORC1 Activity and Nuclear Translocation of TFEB
mTOR plays an important role in the regulation of lysosomal biogenesis through regulating transcription factor EB (TFEB) translocation (Martina et al. 2012; Roczniak-Ferguson et al. 2012). To elucidate the mechanism of autophagic enhancement by Dynasore treatment, we performed immunofluorescence assays to check the cellular localization of mTOR protein. We found that mTOR co-localized with lysosome marker CD63 when treated with DMSO (control), which indicated mTORC1 was activated. However, mTOR was found to be diffusely distributed in the cytoplasm when the cells were treated with Dynasore (Fig. 4a). Phosphorylated p70S6K is considered to be the hallmark of activation of mTORC1. To further check the activation of mTORC1, we evaluated the phosphorylation of p70S6K at threonine 389. The level of phosphorylated p70S6K at threonine 389 decreased as the concentration of Dynasore increased, suggesting that Dynasore could inhibit mTORC1 activity in a dose-dependent manner (Fig. 4b–e). Moreover, we found that TFEB and TFE3 (another Mit/TFE family member) translocated from the cytoplasm to the nucleus in Dynasore-treated cells (Fig. 4f–h).
Dynasore treatment induces autophagy via inhibition of mTORC1 activity. a HEK 293 cells were transfected with GFP-CD63 (lysosome marker). After 24 h, the cells were treated with 50 μM Dynasore or DMSO for 6 h. Then, the cells were subjected to immunoblot assay using antibody against mTOR (red). DAPI was used for nuclear staining. Then, cells were fixed and visualized by confocal microscopy. b–e HEK 293 cells were treated with DMSO, 25 μM or 100 μM Dynasore. After 6 h or 12 h, cell lysates were subjected to immunoblot using indicated antibodies. f–h HEK 293 cells were transfected with EGFP-TFEB and EGFP-TFE3. After 24 h, cells were treated with 50 μM of Dynasore for 6 h. Signal was analyzed by fluorescence microscopy. The data from three independent experiments are presented as means ± S.E.M.; ns, not significantly different; **P < 0.01; ns, not significantly different, one-way ANOVA. Scale bars, 10 μm
Dynasore Treatment Can Increase the Clearance of Cellular Huntingtin Aggregates
Based on the above results, we considered whether Dynasore plays any role in neurodegenerative disease pathogenesis. As known, expanded polyglutamine presenting in the huntingtin protein leads to aggregation of the protein and causes Huntington disease. The aggregates of pathogenic polyglutamine proteins are harmful to the cells. It is reported that insufficient autophagic clearance related to expanded polyglutamine proteins aggregates in neurodegenerative diseases. To evaluate the effect of Dynasore on the protein aggregates associated with neurodegenerative diseases, we transfected cells with N-terminal huntingtin exon 1 fragment with 16 or 60 polyQ repeats (htt16Q or htt60Q). Our findings showed that htt16Q did not form aggregates with or without Dynasore (Fig. 5c). On contrast, Dynasore could increase the clearance of protein aggregation formed by htt60Q (Fig. 5a, b). Consistent with the increasing clearance of htt60Q, Dynasore was also found to accelerate the clearance of htt150Q which with longer polyQ repeats (Fig. 5d). Moreover, knockout of the autophagy gene ATG5 completely blocked the effect of Dynasore on the clearance of htt60Q protein aggregates (Fig. 5e). These results indicated that Dynasore could increase the autophagic clearance of aggregated polyQ proteins.
Dynasore treatment increases the clearance of pathogenic huntingtin aggregates. a HEK 293 cells were transfected with Nhtt-60Q-EGFP. After 24 h, cells were incubated with DMSO, 25 μM, 50 μM, or 100 μM Dynasore for 6 h. Live cells were visualized by fluorescence microscopy. Scale bars, 20 μm. Quantification data of percentage of cells with protein aggregates were depicted in b. c HEK 293 cells were transfected with Nhtt-16Q-EGFP. After 24 h, cells were treated with DMSO or Dynasore (50 μM) for 6 h. Live cells were visualized by fluorescence microscope. d HEK 293 cells were transfected with Nhtt-150Q-EGFP. After 24 h, cells were treated with DMSO or Dynasore (50 μM) for 6 h. Live cells were visualized with a fluorescence microscope. Quantification data of percentage of cells with protein aggregate were shown in d. e ATG5 KO MEF cells were transfected with Nhtt-60Q-EGFP. After 24 h, cells were treated with 50 μM Dynasore for 6 h. Then, the aggregation of Nhtt-60Q-EGFP was analyzed using a fluorescent microscope. The data from three independent experiments are presented as means ± S.E.M.; ns, not significantly different; *P < 0.05; **P < 0.01; ns, not significantly different, one-way ANOVA
Discussion
It has been well known that mTORC1-TFEB signaling functions in various human diseases including neurodegenerative disorders. Previous studies showed that the enhancement of TFEB nuclear translocation and activity results in beneficial effects in cellular and transgenic animal models of neurodegenerative disorders (Martini-Stoica et al. 2018; Tsunemi et al. 2012), indicating that mTORC1-TFEB signaling-mediated autophagy can protect cells against misfolded protein-induced cytotoxicity. In the current study, we provide new insight into the potential therapy of neurodegenerative disorders such as HD. Our results suggest that Dynasore, which was previously recognized as an inhibitor of endocytosis (Macia et al. 2006; Preta et al. 2015), is a novel autophagy inducer that can increase overall autophagy flux by promoting TFEB/TFE3 nuclear translocation.
We find that Dynasore treatment specifically facilitates the intracellular turnover of mutant Nhtt (Fig. 5), but not damage mitochondria (Fig. 3), indicating that Dynasore enhances basal autophagy in cells, which in turn promotes the degradation of autophagic substrate proteins, including many misfolded and aggregated proteins. Interestingly and importantly, our data show that Dynasore treatment strikingly increases the fusion between autophagosomes and the lysosomes (Fig. 2), indicating that it could be more efficient and valuable than the traditional mTOR inhibitors such as rapamycin and Torin1, which target autophagy–lysosome pathway at the early step. Since autophagosomal accumulation in cells may reflect impaired autophagic degradation, which is broadly observed in neurodegenerative disease models and has been shown in the previous studies (Dikic and Elazar 2018; Wong and Cuervo 2010), strategies to enhance the autophagic degradation by generating more autolysosomes have been an attractive issue in the field. More specifically, the treatment of neurodegenerative disease would be a benefit from pharmacological regulation which can enhance autophagosomes–lysosomes fusion. Base on this, the present research not only helps to understand the mechanism underlying endocytic and autophagic regulations but also offers a new clue to develop therapeutic approaches for HD and other neurodegenerative diseases. Future direction will be the test of Dynasore on the clearance of protein aggregates in neuronal cells and/or animal models of neurodegenerative disease.
Material and Methods
Reagent and Antibodies
Dynasore was obtained from MedChemExpress. Bafilomycin A1 (Bafi A1) was purchased from Selleckchem. 4′6-diamidino-2-phenylindole (DAPI) and Antimycin A were purchased from Sigma. Oligomycin was purchased from Calbiochem. The following primary antibodies were used in the assay: anti-GAPDH antibody (Proteintech), anti-LC3 antibody (Novus Biologicals), anti-phospho-p70S6K antibody (Cell Signaling Technology), anti-p70S6K antibody (Epitomics), and anti-mTOR antibody (Cell Signaling Technology). The following secondary antibodies were used in the assay: horseradish peroxidase–conjugated sheep and anti-mouse and anti-rabbit antibodies (Jackson ImmunoResearch Laboratories). The proteins were visualized with an ECL detection kit (Thermo Scientific). Alexa Fluor 594–conjugated Affinipure Goat anti-rabbit IgG (Proteintech) was used as fluorescent secondary antibody.
Cell Culture and Transfection
Human embryonic kidney 293 (HEK 293) cells and ATG5 KO MEF cells were cultured in Dulbecco’s modified eagle’s medium (DMEM) (Gibco) containing 10% fetal bovine serum FBS (Gibco) with penicillin (100 U/ml) and streptomycin (100 μg/ml). Cells were cultured at 37 °C in a humidified atmosphere containing 5% CO2. Cells were starved with Earle’s balanced salt solution (Gibco) for 1 h. The cells were transfected with Lipofectamine 2000 reagent (Invitrogen) at 30% confluence in DMEM without serum according to the reagent manufacturer’s instructions.
Plasmid Constructs
The GFP-CD63, EGFP-LC3, pEGFP-N1-TFEB, mCherry-EGFP-LC3, Nhtt-16Q-EGFP, Nhtt-60Q-EGFP, Nhtt-150Q-EGFP, and EGFP-Parkin plasmids were as described previously (Tao et al. 2015; Wang et al. 2012; Xia et al. 2016; Ying et al. 2011, 2009). pcDNA3.1-mt-Keima plasmid was generated by inserting full-length mKeima into the pcDNA3.1 vector at KpnI/EcoRI sites. The pEGFP-N1-TFE3 was generously provided by Shawn Ferguson (Addgene #38120). All constructs were confirmed via sequencing.
Western Blot
Cells were lysed in a cell lysis buffer containing 50 mM Tris-HCl (pH 7.6) with protease inhibitor cocktail (Roche), 150 mM NaCl, 0.5% sodium deoxycholate, and 1% Nonidet P-40. Proteins were separated by 15% SDS-PAGE (polyacrylamide gel electrophoresis) and transferred onto a PVDF membrane (polyvinylidene difluoride membrane; Millipore). Immunoblot was performed using standard methods as previously reported (Lv et al. 2017; Yang et al. 2018).
Immunofluorescence
HEK 293 cells were washed with PBS (pH 7.4) (Gibco) and fixed with 4% paraformaldehyde for 10 min at room temperature. Then the cells were permeabilized with 0.1% Triton X-100 and pre-blocked with 0.2% fetal bovine serum for 5 min. Cells were incubated with the primary antibodies for 6 h, then with the fluorescent secondary antibodies for 2 h, followed by staining with DAPI (Sigma) for 5 min. The stained cells were visualized using a Nikon (Wu et al. 2012) or a Zeiss LSM710 confocal microscope (Fang et al. 2017; Ren et al. 2016).
Statistical Analysis
Data are shown as mean ± SD of three different independent results. Comparison was assessed by one-way analysis of variance (ANOVA). A difference was considered significant when the P value was less than 0.05.
References
Dikic I, Elazar Z (2018) Mechanism and medical implications of mammalian autophagy. Nat Rev Mol Cell Biol 19:349–364. https://doi.org/10.1038/s41580-018-0003-4
Fang LM, Li B, Guan JJ, Xu HD, Shen GH, Gao QG, Qin ZH (2017) Transcription factor EB is involved in autophagy-mediated chemoresistance to doxorubicin in human cancer cells. Acta Pharmacol Sin 38:1305–1316. https://doi.org/10.1038/aps.2017.25
Jana NR, Zemskov EA, Wang G, Nukina N (2001) Altered proteasomal function due to the expression of polyglutamine-expanded truncated N-terminal huntingtin induces apoptosis by caspase activation through mitochondrial cytochrome c release. Hum Mol Genet 10:1049–1059
Jean S, Cox S, Nassari S, Kiger AA (2015) Starvation-induced MTMR13 and RAB21 activity regulates VAMP8 to promote autophagosome-lysosome fusion. EMBO Rep 16:297–311. https://doi.org/10.15252/embr.201439464
Kopito RR (2000) Aggresomes, inclusion bodies and protein aggregation. Trends Cell Biol 10:524–530
Laplante M, Sabatini DM (2012) mTOR signaling in growth control and disease. Cell 149:274–293. https://doi.org/10.1016/j.cell.2012.03.017
Lv G, Sun D, Zhang J, Xie X, Wu X, Fang W, Tian J, Yan C, Wang H, Fu F (2017) Lx2-32c, a novel semi-synthetic taxane, exerts antitumor activity against prostate cancer cells in vitro and in vivo. Acta Pharm Sin B 7:52–58. https://doi.org/10.1016/j.apsb.2016.06.005
Macia E, Ehrlich M, Massol R, Boucrot E, Brunner C, Kirchhausen T (2006) Dynasore, a cell-permeable inhibitor of dynamin. Dev Cell 10:839–850. https://doi.org/10.1016/j.devcel.2006.04.002
Martina JA, Puertollano R (2013) Rag GTPases mediate amino acid-dependent recruitment of TFEB and MITF to lysosomes. J Cell Biol 200:475–491. https://doi.org/10.1083/jcb.201209135
Martina JA, Chen Y, Gucek M, Puertollano R (2012) MTORC1 functions as a transcriptional regulator of autophagy by preventing nuclear transport of TFEB. Autophagy 8:903–914. https://doi.org/10.4161/auto.19653
Martini-Stoica H, Cole AL, Swartzlander DB, Chen F, Wan YW, Bajaj L, Bader DA, Lee VMY, Trojanowski JQ, Liu Z, Sardiello M, Zheng H (2018) TFEB enhances astroglial uptake of extracellular tau species and reduces tau spreading. J Exp Med 215:2355–2377. https://doi.org/10.1084/jem.20172158
Narendra D, Tanaka A, Suen DF, Youle RJ (2008) Parkin is recruited selectively to impaired mitochondria and promotes their autophagy. J Cell Biol 183:795–803. https://doi.org/10.1083/jcb.200809125
Pickrell AM, Youle RJ (2015) The roles of PINK1, parkin, and mitochondrial fidelity in Parkinson’s disease. Neuron 85:257–273. https://doi.org/10.1016/j.neuron.2014.12.007
Preta G, Cronin JG, Sheldon IM (2015) Dynasore - not just a dynamin inhibitor. Cell Commun Signal 13(24):24. https://doi.org/10.1186/s12964-015-0102-1
Ren ZX, Zhao YF, Cao T, Zhen XC (2016) Dihydromyricetin protects neurons in an MPTP-induced model of Parkinson's disease by suppressing glycogen synthase kinase-3 beta activity. Acta Pharmacol Sin 37:1315–1324. https://doi.org/10.1038/aps.2016.42
Roczniak-Ferguson A, Petit CS, Froehlich F, Qian S, Ky J, Angarola B, Walther TC, Ferguson SM (2012) The transcription factor TFEB links mTORC1 signaling to transcriptional control of lysosome homeostasis. Sci Signal 5:ra42. https://doi.org/10.1126/scisignal.2002790
Ross CA, Poirier MA (2005) Opinion: what is the role of protein aggregation in neurodegeneration? Nat Rev Mol Cell Biol 6:891–898
Sardiello M, Palmieri M, di Ronza A, Medina DL, Valenza M, Gennarino VA, di Malta C, Donaudy F, Embrione V, Polishchuk RS, Banfi S, Parenti G, Cattaneo E, Ballabio A (2009) A gene network regulating lysosomal biogenesis and function. Science 325:473–477. https://doi.org/10.1126/science.1174447
Settembre C, di Malta C, Polito VA, Arencibia MG, Vetrini F, Erdin S, Erdin SU, Huynh T, Medina D, Colella P, Sardiello M, Rubinsztein DC, Ballabio A (2011) TFEB links autophagy to lysosomal biogenesis. Science 332:1429–1433. https://doi.org/10.1126/science.1204592
Sun N, Malide D, Liu J, Rovira II, Combs CA, Finkel T (2017) A fluorescence-based imaging method to measure in vitro and in vivo mitophagy using mt-Keima. Nat Protoc 12:1576–1587. https://doi.org/10.1038/nprot.2017.060
Tao Z, Wang H, Xia Q, Li K, Li K, Jiang X, Xu G, Wang G, Ying Z (2015) Nucleolar stress and impaired stress granule formation contribute to C9orf72 RAN translation-induced cytotoxicity. Hum Mol Genet 24:2426–2441. https://doi.org/10.1093/hmg/ddv005
Tsunemi T, Ashe TD, Morrison BE, Soriano KR, Au J, Roque RAV, Lazarowski ER, Damian VA, Masliah E, la Spada AR (2012) PGC-1alpha rescues Huntington’s disease proteotoxicity by preventing oxidative stress and promoting TFEB function. Sci Transl Med 4:142ra197. https://doi.org/10.1126/scitranslmed.3003799
Wang H, Ying Z, Wang G (2012) Ataxin-3 regulates aggresome formation of copper-zinc superoxide dismutase (SOD1) by editing K63-linked polyubiquitin chains. J Biol Chem 287:28576–28585. https://doi.org/10.1074/jbc.M111.299990
Wong E, Cuervo AM (2010) Autophagy gone awry in neurodegenerative diseases. Nat Neurosci 13:805–811. https://doi.org/10.1038/nn.2575
Wu JC, Qi L, Wang Y, Kegel KB, Yoder J, Difiglia M, Qin ZH, Lin F (2012) The regulation of N-terminal huntingtin (Htt552) accumulation by Beclin1. Acta Pharmacol Sin 33:743–751. https://doi.org/10.1038/aps.2012.14
Xia Q, Wang H, Hao Z, Fu C, Hu Q, Gao F, Ren H, Chen D, Han J, Ying Z, Wang G (2016) TDP-43 loss of function increases TFEB activity and blocks autophagosome-lysosome fusion. EMBO J 35:121–142. https://doi.org/10.15252/embj.201591998
Yang Y, Guan D, Lei L, Lu J, Liu JQ, Yang G, Yan C, Zhai R, Tian J, Bi Y, Fu F, Wang H (2018) H6, a novel hederagenin derivative, reverses multidrug resistance in vitro and in vivo. Toxicol Appl Pharmacol 341:98–105. https://doi.org/10.1016/j.taap.2018.01.015
Ying Z, Wang H, Fan H, Zhu X, Zhou J, Fei E, Wang G (2009) Gp78, an ER associated E3, promotes SOD1 and ataxin-3 degradation. Hum Mol Genet 18:4268–4281
Ying Z, Wang H, Fan H, Wang G (2011) The endoplasmic reticulum (ER)-associated degradation system regulates aggregation and degradation of mutant neuroserpin. J Biol Chem 286:20835–20844. https://doi.org/10.1074/jbc.M110.200808
Zoncu R, Efeyan A, Sabatini DM (2011) mTOR: from growth signal integration to cancer, diabetes and ageing. Nat Rev Mol Cell Biol 12:21–35. https://doi.org/10.1038/nrm3025
Funding
This work was supported by the National Key Plan for Scientific Research and Development of China (Nos. 2017YFC0909100), the National Natural Sciences Foundation of China (Nos. 31571053 and 31771117), a Project Funded by Jiangsu Key Laboratory of Neuropsychiatric Diseases (BM2013003), and a Project Funded by the Priority Academic Program Development of the Jiangsu Higher Education Institutes (PAPD).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, Y., Xu, S., Wang, N. et al. Dynasore Suppresses mTORC1 Activity and Induces Autophagy to Regulate the Clearance of Protein Aggregates in Neurodegenerative Diseases. Neurotox Res 36, 108–116 (2019). https://doi.org/10.1007/s12640-019-00027-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12640-019-00027-9