Abstract
Background
The aim of this study was to establish different degrees of mechanical dyssynchrony according to validated cut-off (CO) values of myocardial perfusion gated SPECT phase analysis parameters (SD, standard deviation; B, bandwidth; S, skewness; K, kurtosis).
Methods
Using Emory Cardiac Toolbox™, we prospectively analyzed 408 patients (mean age 64.1 years, 26.7% female), divided into a control group of 150 normal subjects and a validation group of 258 patients (left bundle branch block: 17.8%, right bundle branch block: 8.9%. atrial fibrillation: 16.3%, coronary revascularization: 30%, dilated cardiomyopathy: 7.4%. valvulopathies: 2.7%, ischemic test: 45.3%) with ischemic and non-ischemic cardiac diseases, by means of phase analysis.
Results
Agreement of CO values (SD > 18.4°; B > 51°; S ≤ 3.2; K ≤ 9.3) used to discriminate between normal subjects and patients was strong (c-statistic 0.9; 95% CI 0.98-0.99). Four degrees of dyssynchrony were found according to the number of abnormal phase parameters. All patients with mechanical and electrical criteria for cardiac resynchronization therapy (CCRT) (n: 82) had Grade 2 to 4 (two to four abnormal phase parameters). Agreement of CO values (SD > 40.2°; B > 132°; S ≤ 2.3; K ≤ 4.6) used to discriminate between patients with and without CCRT was strong (c-statistic 0.8; 95% CI 0.79-0.87) but 12% of patients with CCRT did not have any of these abnormal phase parameters.
Conclusions
The discriminatory capacity of gated SPECT phase analysis parameters between normal subjects and patients, and between patients with and without CCRT, is very good, making it possible to define different degrees of mechanical dyssynchrony.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The use of gated single-photon emission computed tomography (SPECT) myocardial perfusion imaging (MPI) phase analysis for quantifying left ventricular (LV) mechanical dyssynchrony has been well described in the literature. Different studies evaluated mechanical dyssynchrony and myocardial perfusion using phase analysis of gated SPECT imaging in patients with left ventricular dysfunction,1–6 and also the prevalence and predictors of mechanical dyssynchrony in patients with left ventricular dysfunction undergoing gated SPECT myocardial perfusion imaging.7 On the other hand, phase analysis of gated myocardial perfusion SPECT was compared to tissue Doppler imaging for the assessment of left ventricular dyssynchrony8,9 and used for the characterization of ventricular contraction in patients with left bundle branch block,10 in patients after acute ST elevation myocardial infarction,11 in patients with implantable cardiac defibrillators12; the mechanical dyssynchrony in other situations was analyzed.13–16 Furthermore, the repeatability and reproducibility of phase analysis of gated single-photon emission computed tomography myocardial perfusion imaging were evaluated to quantify cardiac dyssynchrony.17 The mechanical dyssynchrony analysis can predict response to CRT18 and can have long-term prognostic value,19 even in patients with end-stage renal disease and normal LVEF.20
We had already defined21 the different cut-off (CO) values for standard deviation (SD), bandwidth (B), skewness (S), and kurtosis (K) obtained from myocardial perfusion gated SPECT in normal subjects, in patients with only conduction cardiac diseases, in patients with only mechanical cardiac diseases, in patients with conduction cardiac diseases plus mechanical cardiac diseases, and in patients with criteria for cardiac resynchronization therapy. Our objective was to validate these CO values of phase analysis parameters in order to define different degrees of cardiac mechanical dyssynchrony.
Materials and methods
Study population
A prospective study was conducted at the Nuclear Cardiology Unit of a tertiary university hospital center. Patients referred for stress-rest myocardial perfusion SPECT with 99mTc compounds for standard clinical indication were screened for inclusion. In the validation group, 45.3% had myocardial ischemia, and any of the patients of the reference group presents myocardial ischemia.
We prospectively analyzed 258 patients with ischemic and non-ischemic cardiac diseases (validation group, mean age 67.5 years, 13.2% female, LVEF <50%) by means of phase analysis, using SyncTool™ (Emory Cardiac Toolbox™), in order to establish different degrees of mechanical dyssynchrony. The normal CO values for SD, B, S, and K used to discriminate between normal results and dyssynchrony were obtained previously in a control group of 150 normal subjects (mean age 60.7 years, 50% female). We compared the validation group (n = 258) with this control group (n = 150) of normal subjects, defined in a previous publication21: this group included subjects with no history of coronary artery disease, normal resting electrocardiogram (sinus rhythm, normal QRS, and repolarization), normal rest and exercise gated SPECT, maximum predicted heart rate ≥85% achieved during a symptom-limited treadmill exercise (Bruce protocol), and gated SPECT ejection fraction >50%. At the time of diagnosis, 82 patients satisfied clinical, mechanical, and electrical criteria of cardiac resynchronization therapy (CCRT) (LVEF ≤35% in NYHA Class III–IV and QRS > 120 ms).22 At the time of stress-rest myocardial perfusion gated SPECT, after optimizing medical treatment, any of these patients achieved >5 METs. The clinical characteristics of the control group and the validation group are shown in Table 1.
CO values used for validation21 were as follows:
-
(A)
standard deviation (SD) > 18.4º, bandwidth (B) > 51º, skewness (S) ≤ 3.2, and kurtosis (K) ≤ 9.3 to differentiate between the control group and the validation group in the study population;
-
(B)
standard deviation (SD) > 13.1º, bandwidth (B) > 51º, skewness (S) ≤ 4.1, and kurtosis (K) ≤ 10.4 to differentiate between women in the control group and female patients in the validation group;
-
(C)
standard deviation (SD) > 18.4º, bandwidth (B) > 55º, skewness (S) ≤ 3.1, and kurtosis (K) ≤ 9.3 to differentiate between men in the control group and male patients in the validation group;
-
(D)
standard deviation (SD) > 40.2º, bandwidth (B) > 132º, skewness (S) ≤ 2.3, and kurtosis (K) ≤ 4.6 to differentiate between patients with and without CCRT.
The study had Institutional Review Board (PR(AG)168.2010) approval, and full written informed consent was obtained from all participants. All authors had full access to the data and take responsibility for the manuscript as written. The research protocol complied with the Declaration of Helsinki.
Myocardial perfusion gated SPECT and phase analysis
All 408 patients underwent a stress-rest gated SPECT 1-day protocol with 99mTc-tetrofosmin. The first dose (30-60 seconds before ending the stress test) was 296 MBq (8 mCi), and the second (at rest) was 888 MBq (24 mCi), with an interval of over 45 minutes in between. The protocols employed for gated SPECT and phase analysis were the same as in the earlier study.21 LV ejection fraction and diastolic and systolic volumes were calculated at rest automatically using the Emory Cardiac Toolbox™ program. Phase analysis parameters of only rest gated SPECT were calculated using SyncTool™ (Emory Cardiac Toolbox™).
Statistical analysis
All continuous data were expressed as mean ± (standard deviation), and all non-continuous variables were expressed as percentages. Continuous variables were compared using the Student’s t test for unpaired samples. Differences between proportions were compared using the χ 2 test. Fisher’s exact test was used when 5 patients were expected in any subgroup.
We analyzed the Kappa index and the global agreement between the control group and the validation group according to the cut-off value for phase parameters in the population under study, the female group, the male group, and the group of patients with CCRT. For global agreement, we used the Wilson’s test, with a 95% CI. The kappa-statistic measure of agreement was scaled to be 0 when the amount of agreement was what would be expected to be observed by chance and 1 when there was perfect agreement. For intermediate values, Landis and Koch23 suggest the following interpretations: below 0.0, poor; 0.00 to 0.2, slight; 0.21 to 0.40, fair; 0.41 to 0.6, moderate; 0.61 to 0.8, substantial; and 0.81 to 1.00, almost perfect.
Subsequently, by means of multiple logistic regression analysis (METHOD = ENTER, probability for entry and removal 0.05 and 0.10, respectively, adjusted for age and hypertension), we evaluated the C-statistic for every model (including phase parameters categorized according to their CO value, a predictor of dyssynchrony). Models are typically considered reasonable when the C-statistic is higher than 0.7 and strong when C exceeds 0.8.24,25 Collinearity diagnostic statistics were analyzed looking at tolerance and variance inflation factor. We considered collinearity to occur when tolerance was less than 0.1, or the variance inflation factor was greater than 10. We detected no collinearity effect in the analysis. The model fit was evaluated with the Hosmer and Lemeshow’s goodness-of-fit test. Bootstrap analysis for multiple comparisons (control group vs. validation group, female group, male group, and patients with criteria for cardiac resynchronization therapy) was based on 1000 bootstrap samples, and the mean difference was significant at the .05 level.
According to the sum of different phase parameters, we analyzed the degrees of dyssynchrony in relation to SD, BD, S, and K. For this analysis, we used analysis of variance (ANOVA) with Bonferroni correction. We defined 4 groups of phase dyssynchrony according to the number of abnormal phase parameters: group 1 (patients with one abnormal parameter), group 2 (patients with two abnormal parameters), group 3 (patients with three abnormal parameters), and group 4 (patients with four abnormal parameters).
All tests were two sided; a value of P < .05 was considered as indicative of statistical significance. Data were analyzed by SPSS for Windows, version 15 (SPSS Inc., Chicago), and STATA 13.1.
Results
Table 2 shows the characteristics of phase parameters for the control group and the validation group, and for patients with and without criteria for CRT. There were significant differences between groups, with the exception of peak phase parameter.
Analysis of agreement
Agreement for the cut-off values obtained previously (SD > 18.4º, B > 51º, S ≤ 3.2, K ≤ 9.3) to discriminate between normal subjects and patients ranged from substantial to almost perfect (see Appendix in the online-only Data Supplement, Table 3). The most important parameters were SD > 18.4º and B > 51º, with perfect agreement. In the multiple logistic regression analysis (variables in the model: SD > 18.4º, B > 51º, S ≤ 3.2, K ≤ 9.3) adjusted for age, hypertension, and diabetes mellitus (Hosmer and Lemeshow’s test: χ 2: 0,664; P = 0.999; Nagelkerke R 2: 0.94), the c-statistic was strong (Figure 1).
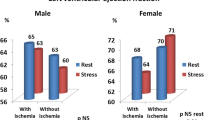
In the group of women (n = 109), agreement ranged from moderate to almost perfect (see Appendix in the online-only Data Supplement, Table 3). The most important parameters were B > 51º and K ≤ 10.4, with perfect agreement. In the multiple logistic regression analysis (variables in the model: SD > 13.1º, B > 51º, S ≤ 4.1, K ≤ 10.4) adjusted for age, hypertension, and diabetes mellitus (Hosmer and Lemeshow’s test: χ 2: 2,128; P = 0.977; Nagelkerke R 2: 0.92), the c-statistic was strong (Figure 2A).
In the group of men (n = 299), agreement ranged from moderate to almost perfect (see Appendix in the online-only Data Supplement, Table 3). The most important parameters were SD > 18.4º and B > 55º, with perfect agreement. In the multiple logistic regression analysis (variables in the model: SD > 18.4º, B > 55º, S ≤ 3.1, K ≤ 9.3) adjusted for age, hypertension, and diabetes mellitus (Hosmer and Lemeshow’s test: χ 2: 10,538; P = 0.229; Nagelkerke R 2: 0.93), the c-statistic was strong (Figure 2B).
The increased number of abnormal phase parameters is an indicator of increased dyssynchrony. An increased number of abnormal phase parameters increases the values of SD and B and also decreases the values of S and K (Figure 3). According to the number of abnormal phase parameters, we defined a normal group (n: 119, all four phase parameters are normal) and four degrees of dyssynchrony: Grade 1 (n = 14, one abnormal phase parameter); Grade 2 (n = 60, two abnormal phase parameters); Grade 3 (n = 30, three abnormal phase parameters; and Grade 4 (n = 185, four abnormal phase parameters). In Grade 1, there were 5 patients with SD > 18.4º, 5 patients with B > 51º, and 4 patients with S ≤ 3.2. In Grade 2, there were 54 patients with SD > 18.4º, 54 patients with B > 51º, 6 patients with S ≤ 3.2, and 6 patients with K ≤ 9.3. In Grade 3, there were 27 patients with SD > 18.4º, 30 patients with B > 51º, 30 patients with S ≤ 3.2, and 3 patients with K ≤ 9.3. In Grade 4, all patients had SD > 18.4º, B > 51º, S ≤ 3.2, and K ≤ 9.3. We then defined these different degrees of dyssynchrony according to different values of SD, BD, S, and K (Table 3). We found a significant linear trend between the degree of dyssynchrony and left ventricular ejection fraction (Figure 4A) on the one hand, and the degree of dyssynchrony and QRS duration (Figure 4B) on the other. Ninety percent (74/82) of patients with CCRT had Grade 3 to 4 dyssynchrony in the analysis phase (gray area in Figures 3 and 4).
In patients with (n = 82) and without (n = 326) CCRT, the agreement ranged from fair to moderate (see Appendix in the online-only Data Supplement, Table 3). The most important parameters were SD > 40.2º and B > 132º, with moderate agreement. In the multiple logistic regression analysis (variables in the model: SD > 40.2º, B > 132º, S ≤ 2.3, K ≤ 4.6) adjusted for age, hypertension, and diabetes mellitus (Hosmer and Lemeshow’s test: χ 2: 5,982; P = 0.649; Nagelkerke R 2: 0.5), the c-statistic was strong (Figure 5). We determined that 36.8% (68/185) of the patients with four phase abnormal parameters had CCRT. Ten of the 82 patients (12%) with CCRT did not have abnormal phase parameters (Figure 6).
Discussion
Mean values of phase analysis variables obtained by gated SPECT using SyncTool™ (Emory Cardiac Toolbox™) in some control groups to compare different left ventricular dyssynchrony abnormalities have been published,5,9,10,14,18 but ROC analysis was not systematically applied, and the mean values of S and K were considered in only two articles.5,9 In the present study, we validated the CO value of gated SPECT phase analysis parameters in normal subjects and patients with different electrical and mechanical cardiopathies published previously in a pilot study,21 and we defined four degrees of dyssynchrony according to the number of abnormal phase parameters. This new concept of classifying cardiac dyssynchrony in different groups includes all phase parameters that may be altered without downplaying any of them. In this clinical practice setting, we have demonstrated that although the bandwidth and standard deviation are normal, there may be dyssynchrony by skewness and kurtosis. While the bandwidth and standard deviation are the most important parameters, the analysis should not exclude skewness and kurtosis. In this way, dyssynchrony is assessed by four parameters in a more correct way. At present, we are awaiting the results regarding the prognostic value in cardiology according to these grades of dyssynchrony.
We observed that the capacity of CO values in the study population (SD > 18.4º, B > 51º, S ≤ 3.2, K ≤ 9.3) to discriminate between normal subjects and patients was strong. The most important parameters were SD and B, with perfect agreement. In women (SD > 13.1º, B > 51º, S ≤ 4.1, K ≤ 10.4) and men (SD > 18.4º, B > 55º, S ≤ 3.1, K ≤ 9.3), this discriminatory ability was also strong. The most important parameters in women were B and K, with perfect agreement; in men, the most important parameters were SD and B, with perfect agreement.
As the degree of myocardial disturbance (electrical and structural) increased, mechanical synchronicity worsened. Trimble et al.5 observed that SD, B, S, and K were significantly different for patients with LV dysfunction, left bundle branch block, right ventricular branch block, and ventricular paced rhythms compared with normal control subjects, but until now only mean values of normal patients were determined for use in comparisons. Atchley et al.14 found that patients with mild to moderate LV dysfunction (EF 35-50%) had more dyssynchrony than normal controls (EF > 55%) (SD 37.7º vs 8.8º, P < .001 and B 113.5º vs 28.7º, P < .001), but less dyssynchrony than patients with severe LV dysfunction (EF < 35%) (SD 37.7º vs 52.0º, P < .001 and B 113.5º vs 158.2º, P < .001). In patients with mild to moderate LV dysfunction, there were only weak correlations between QRS duration and dyssynchrony, and approximately one third of these patients had significant LV dyssynchrony. Samad et al.19 found a 52% prevalence of significant mechanical dyssynchrony, defined as phase SD > 43º, in patients with EF < 35%.
However, until now no graduation of dyssynchrony according to the number of abnormal phase parameters had been reported. In our series, four degrees of dyssynchrony were identified, based on the number of abnormal phase parameters. These degrees were defined according to the number of altered phase parameters (one, two, three, or four: SD > 18.4º, B > 51º, S ≤ 3.2, K ≤ 9.3), and there was a significant linear trend between the degree of dyssynchrony and SD, B, K, S, left ventricular ejection fraction, and QRS duration.
Since using phase analysis from gated SPECT myocardial perfusion imaging to evaluate left ventricular mechanical dyssynchrony can assist clinicians in the selection of patients for cardiac resynchronization therapy, we also compared the four degrees of left ventricular mechanical dyssynchrony measured by myocardial perfusion gated SPECT with CCRT (left ventricular ejection fraction ≤35% and QRS duration >120 ms). Ninety-two percent of patients with CCRT had three or four abnormal parameters in the phase analysis. In our series, the ability of CO values to discriminate between patients with CCRT (SD > 40.2º, B > 132º, S ≤ 2.3, K ≤ 4.6) and without CCRT was strong, but 12% of patients with CCRT did not have any abnormal phase parameters. This information is important since it could correspond to patients who are non-responders to resynchronization therapy. Unfortunately, 1 out of 3 patients receiving cardiac resynchronization therapy does not benefit from it.22 Left ventricular mechanical dyssynchrony in gated SPECT phase analysis could aid in the selection of cardiac resynchronization therapy candidates. Consequently, the study of mechanical dyssynchrony by means of phase analysis should undoubtedly be included in heart failure guidelines.
Phase analysis of myocardial perfusion gated SPECT is a method that can automatically quantify left ventricular mechanical dyssynchrony with high reproducibility,10,26 and some publications have observed that left ventricular mechanical dyssynchrony may serve as a predictive factor of response to both CRT3,27,28 and cardiac outcome.17,27,28 Pazhenkottil et al.17 found that LV dyssynchrony assessed by phase analysis of gated SPECT is a strong predictor of major adverse cardiac events (cardiac death and hospitalization for any cardiac cause, including worsening of heart failure, non-fatal myocardial infarction, unstable angina, and coronary revascularization) independent of other known predictors such as perfusion defects or decreased LV ejection fraction. Zafrir et al.27 observed that the independent predictors of cardiac mortality were NYHA class (for each increment in class) and SD (for each 10º increment). Hess et al.28 found in patients with coronary artery disease that mechanical LV dyssynchrony measured by gated SPECT has a stronger relationship with outcomes than electrical dyssynchrony measured by QRS duration. Among patients with LVEF > 35%, mechanical and electrical dyssynchrony together provided prognostic value above that afforded by LVEF. In the future, it will be important to verify, preferably in multicenter studies, the importance of the four degrees of dyssynchrony described in our series in order to stratify risk in patients with LV dysfunction.
Limitations
Because our study is derived from only one center, data extrapolation to the general population is open to question. The number of patients with CCRT is limited, and there is currently no follow-up on response to treatment in accordance with the phase analysis graduation described in our study. It will be important to test our results in future studies.
Conclusions
In this study, we observed that the discriminatory capacity of gated SPECT phase analysis parameters among normal subjects and patients is very good, making it possible to define different degrees of mechanical dyssynchrony.
New knowledge gained
CO values of gated SPECT phase analysis parameters among subjects and patients have been validated, and four degrees of left ventricular mechanical dyssynchrony have been described in accordance with the number of abnormal phase parameters.
Abbreviations
- B :
-
Bandwidth
- CO:
-
Cut-off
- CCRT:
-
Criteria for cardiac resynchronization therapy
- EF:
-
Ejection fraction
- K :
-
Kurtosis
- LV:
-
Left ventricle
- ROC:
-
Receiver operating characteristic
- S :
-
Skewness
- SD:
-
Standard deviation
References
Trimble MA, Borges-Neto S, Honeycutt EF, Shaw LK, Pagnanelli R, Chen J, et al. Evaluation of mechanical dyssynchrony and myocardial perfusion using phase analysis of gated SPECT imaging in patients with left ventricular dysfunction. J Nucl Cardiol. 2000;15:663–70.
Chen J, Garcia EV, Folks RD, Cooke CD, Faber TL, Tauxe EL, et al. Onset of left ventricular mechanical contraction as determined by phase analysis of ECG-gated myocardial perfusion SPECT imaging: Development of a diagnostic tool for assessment of cardiac mechanical dyssynchrony. J Nucl Cardiol. 2005;12:687–95.
Trimble MA, Borges-Neto S, Smallheiser S, Chen J, Honeycutt EF, Shaw LK, et al. Evaluation of left ventricular mechanical dyssynchrony as determined by phase analysis of ECG-gated SPECT myocardial perfusion imaging in patients with left ventricular dysfunction and conduction disturbances. J Nucl Cardiol. 2007;14:298–307.
Trimble MA, Borges-Neto S, Honeycutt EF, Smallheiser S, Chen J, Shaw LK, et al. Evaluation of mechanical dyssynchrony and myocardial perfusion using phase analysis of gated SPECT imaging in patients with left ventricular dysfunction. J Nucl Cardiol. 2008;15:663–70.
Boogers MM, Chen J, Bax JJ. Myocardial perfusion single photon emission computed tomography for the assessment of mechanical dyssynchrony. Curr Opin Cardiol. 2008;23:431–9.
Atchley AE, Trimble MA, Samad Z, Shaw LK, Pagnanelli R, Chen J, et al. Use of phase analysis of gated SPECT perfusion imaging to quantify dyssynchrony in patients with mild-to-moderate left ventricular dysfunction. J Nucl Cardiol. 2009;16:888–94.
Samad Z, Atchley AE, Trimble MA, Sun JL, Shaw LK, Pagnanelli R, et al. Prevalence and predictors of mechanical dyssynchrony as defined by phase analysis in patients with left ventricular dysfunction undergoing gated SPECT myocardial perfusion imaging. J Nucl Cardiol. 2011;18:24–30.
Henneman MM, Chen J, Ypenburg C, Dibbets P, Bleeker GB, Boersma E, et al. Phase analysis of gated myocardial perfusion single-photon emission computed tomography compared with tissue Doppler imaging for the assessment of left ventricular dyssynchrony. J Am Coll Cardiol. 2007;49:1708–14.
Marsan NA, Henneman MM, Chen J, Ypenburg C, Dibbets P, Ghio S, et al. Left ventricular dyssynchrony assessed by two threedimensional imaging modalities: Phase analysis of gated myocardial perfusion SPECT and tri-plane tissue Doppler imaging. Eur J Nucl Med Mol Imaging. 2008;35:166–73.
Van Kriekinge SD, Nishina H, Ohba M, Berman DS, Germano G. Automatic global and regional phase analysis from gated myocardial perfusion SPECT imaging: application to the characterization of ventricular contraction in patients with left bundle branch block. J Nucl Med. 2008;49:1790–7.
Murrow J, Esteves F, Galt J, Chen J, Garcia E, Lin J, et al. Characterization of mechanical dyssynchrony measured by gated single photon emission computed tomography phase analysis after acute ST-elevation myocardial infarction. J Nucl Cardiol. 2011;18:912–9.
Aljaroudi WA, Hage FG, Hermann D, Doppalapudi H, Venkataraman R, Heo J, et al. Relation of left-ventricular dyssynchrony by phase analysis of gated SPECT images and cardiovascular events in patients with implantable cardiac defibrillators. J Nucl Cardiol. 2010;17:398–404.
Chen J, Henneman MM, Trimble MA, Bax JJ, Borges-Neto S, Iskandrian AE, et al. Assessment of left ventricular mechanical dyssynchrony by phase analysis of ECG-gated SPECT myocardial perfusion imaging. J Nucl Cardiol. 2008;15:127–36.
Chen J, Faber TL, Cooke CD, Garcia EV. Temporal resolution of multiharmonic phase analysis of ECG-gated myocardial perfusion SPECT studies. J Nucl Cardiol. 2008;15:383–91.
Li D, Zhou Y, Feng J, Yuan D, Cao K, Garcia EV, et al. Impact of image reconstruction on phase analysis of ECG-gated myocardial perfusion SPECT studies. Nucl Med Commun. 2009;30:700–5.
Chen CC, Huang WS, Hung GU, Chen WC, Kao CH, Chen J. Left-ventricular dyssynchrony evaluated by Tl-201 gated SPECT myocardial perfusion imaging: A comparison with Tc-99m sestamibi. Nucl Med Commun. 2013;34:229–32.
Trimble MA, Velazquez EJ, Adams GL, Honeycutt EF, Pagnanelli RA, Barnhart HX, Chen J, et al. Repeatability and reproducibility of phase analysis of gated single-photon emission computed tomography myocardial perfusion imaging used to quantify cardiac dyssynchrony. Nucl Med Commun. 2008;29:374–81.
Henneman MM, Chen J, Dibbets-Schneider P, Stokkel MP, Bleeker GB, Ypenburg C, et al. Can LV dyssynchrony as assessed with phase analysis on gated myocardial perfusion SPECT predict response to CRT? J Nucl Med. 2007;48:1104–11.
Pazhenkottil AP, Buechel RR, Husmann L, Nkoulou RN, Wolfrum M, Ghadri JR, et al. Long-term prognostic value of left ventricular dyssynchrony assessment by phase analysis from myocardial perfusion imaging. Heart. 2011;97:33–7.
Chen J, Kalogeropoulos AP, Verdes L, Butler J, Garcia EV. Left-ventricular systolic and diastolic dyssynchrony as assessed by multi-harmonic phase analysis of gated SPECT myocardial perfusion imaging in patients with end-stage renal disease and normal LVEF. J Nucl Cardiol. 2011;18:299–308.
Romero-Farina G, Aguadé-Bruix S, Candell-Riera J, Pizzi MN, García-Dorado D. Cut-off values of myocardial perfusion gated-SPECT phase analysis parameters of normal subjects, and conduction and mechanical cardiac diseases. J Nucl Cardiol. 2015;22:1247–58.
Dickstein K, Vardas PE, Auricchio A, Daubert JC, Linde C, McMurray J, ESC Committee for Practice Guidelines (CPG), et al. Focused Update of ESC Guidelines on device therapy in heart failure: an update of the 2008 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure and the 2007 ESC guidelines for cardiac and resynchronization therapy. Eur Heart J. 2010;2010(31):2677–87.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33:159–74.
Hosmer DW, Lemeshow S. Applied logistic regression. New York, NY: Wiley; 1989.
Hosmer DW, Lemeshow S. Applied logistic regression. 2nd ed. New York, NY: Wiley; 2000.
Lin X, Xu H, Zhao X, Folks RD, Garcia EV, Soman P, et al. Repeatability of left ventricular dyssynchrony and function parameters in serial gated myocardial perfusion SPECT studies. J Nucl Cardiol. 2010;17:811–6.
Zafrir N, Nevzorov R, Bental T, Strasberg B, Gutstein A, Mats I, et al. Prognostic value of left ventricular dyssynchrony by myocardial perfusion-gated SPECT in patients with normal and abnormal left ventricular functions. J Nucl Cardiol. 2014;21:532–40.
Hess PL, Shaw LK, Fudim M, Iskandrian AE, Borges-Neto S. The prognostic value of mechanical left ventricular dyssynchrony defined by phase analysis from gated single-photon emission computed tomography myocardial perfusion imaging among patients with coronary heart disease. J Nucl Cardiol 2016 Jan 25 [Epub ahead of print]
Disclosure
The authors declare that they have no financial conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
See related editorial, doi: 10.1007/s12350-016-0717-7.
The authors of this article have provided a PowerPoint file, available for download at SpringerLink, which summarizes the contents of the paper and is free for re-use at meetings and presentations. Search for the article DOI on SpringerLink.com.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Aguadé-Bruix, S., Romero-Farina, G., Candell-Riera, J. et al. Mechanical dyssynchrony according to validated cut-off values using gated SPECT myocardial perfusion imaging. J. Nucl. Cardiol. 25, 999–1008 (2018). https://doi.org/10.1007/s12350-016-0684-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-016-0684-z