Abstract
Background
Left ventricular dyssynchrony is an adverse consequence of ST-elevation myocardial infarction (STEMI) and bears an unfavorable prognosis. Mechanical dyssynchrony as measured by phase analysis from gated single photon emission computed tomography (GSPECT) correlates well with other imaging methods of assessing dyssynchrony but has not been studied in STEMI. We hypothesized that systolic dyssynchrony as measured by GSPECT would correlate with adverse remodeling after STEMI.
Methods
In 28 subjects suffering STEMI, GSPECT with technetium-99m sestamibi was performed immediately after presentation (day 5) and remotely (6 months). Parameters of left ventricular dyssynchrony (QRS width, histogram bandwidth (HBW) and phase standard deviation (PSD)) were measured from GSPECT using the Emory Cardiac Toolbox. Left ventricular volumes, ejection fraction (LVEF) and infarct size were also assessed.
Results
After successful primary percutaneous coronary intervention to the infarct-related artery, subjects had an LVEF of 46.4% ± 11% and a resting perfusion defect of 27.4% ± 16% at baseline. Baseline QRS width was normal (91.5 ± 17.5 ms). Subjects with STEMI had dyssynchrony compared with a cohort of 22 normal subjects (age 57.2 ± 10.6 years, <5% perfusion defect) by both HBW (100.3° ± 70.7° vs 26.5° ± 5.3°, P < .0001) and PSD (35.3° ± 16.9° vs 7.9° ± 2.1°, P < .0001). Baseline HBW correlated with resting perfusion defect size (r = 0.67, P < .001), end-systolic volume (r = 0.72, P < .001), end-diastolic volume (r = 0.63, P = .001), and inversely with LVEF (r = −0.74, P < .001). HBW and PSD improved over the follow-up period (−24.1 ± 35.9 degrees, P = .003 and −8.7° ± 14.6°, P = .006, respectively), and improvement in HBW correlated with reduction in LV end-systolic volumes (r = 0.43, P = .034). Baseline HBW and PSD, however, did not independently predict LVEF at 6 months follow-up.
Conclusions
After STEMI, subjects exhibit mechanical dyssynchrony as measured by GSPECT phase analysis without evidence of electrical dyssynchrony. Improvement in mechanical dyssynchrony correlates with beneficial ventricular remodeling. The full predictive value of this measure in post-infarct patients warrants further study.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Left ventricular dyssynchrony is an adverse consequence of ST-elevation myocardial infarction (STEMI) and bears an unfavorable prognosis.1 Along with other measures of negative remodeling, subjects suffering acute myocardial infarction demonstrate ventricular dyssynchrony by echocardiography (via tissue Doppler imaging (TDI)), even in the absence of electrical dyssynchrony.2 In addition, the severity of dyssynchrony by echocardiography at the time of the initial infarct predicts the degree of long-term adverse remodeling.3 Importantly, dyssynchrony correlates with clinical outcomes including heart failure and death.1
Echocardiography as a measure of regional ventricular dysfunction has yet to provide a robust metric by which responses to resynchronization therapy can be predicted, suggesting that other diagnostic modalities may play a role.4,5 Gated myocardial perfusion imaging may contribute to the assessment of ventricular function in this setting. Measurement of regional contraction by SPECT imaging can be performed via phase analysis of ECG-gated count data, wherein the time-interval over which regions of the ventricle contract (measured by histogram bandwidth (HBW) and phase standard deviation (PSD)) reflects systolic dyssynchrony.6 This assessment has been evaluated in normal subjects, in subjects with conduction delays, and in subjects with left ventricular dysfunction.6-9 Dyssynchrony measures of HBW and PSD correlate well with measures of dyssynchrony by tissue TDI in subjects with left ventricular (LV) dysfunction.8,10 Importantly, this technique is highly reproducible and provides ample temporal resolution.11,12 While phase analysis has been studied in predicting response to cardiac resynchronization therapy with promising results, its value in measuring adverse ventricular remodeling in post-infarct patients is not well described.13
Methods
Study Design
This is an observational study of systolic dyssynchrony measures by SPECT in subjects surviving acute STEMI. Subjects were recruited and enrolled as part of a randomized clinical trial assessing the efficacy of cell therapy in acute myocardial infarction.14
Study Population and Protocol
Eligible subjects were patients between the ages of 18-75 years identified as having suffered acute STEMI within 3 days of hospital admission who had been treated with successful reperfusion by intracoronary stent placement (TIMI 2 or 3 flow, <20% residual stenosis). For inclusion, subjects demonstrated left ventricular dysfunction (defined by left ventricular ejection fraction (LVEF) >25% but ≤50%) and regional wall motion abnormality in the distribution of the infarct-related artery (IRA)—defined by transthoracic echocardiography performed 4-6 days after stent placement. Subjects were excluded if they were poor candidates for percutaneous intervention or SPECT imaging. Clinical exclusion criteria included unstable coronary heart disease, heart failure, cardiogenic shock, malignant arrhythmias, or severe valvular disease. Patients with significant co-morbid conditions or inability to adhere to standard post-myocardial infarction medical therapies were deemed ineligible. Based on these criteria, suitable subjects were enrolled after written informed consent according to the local institutional review boards of participating clinical centers. Study subjects were compared to 22 patients enrolled separately as part of a normal file cohort (age 57.2 ± 10.6 years with a perfusion defect of <5%).
SPECT Imaging
At baseline and again at 6 months follow-up, a rest/adenosine stress protocol was employed, with 6 minute of adenosine infusion. Gated SPECT imaging was performed with technetium-99m sestamibi (10 mCi [370 MBq] rest dose, 30 mCi [1,110 MBq] stress dose) using a 90° angled dual-head camera system equipped with low-energy, high-resolution collimators. Either 64 or 72 projections were obtained (depending on the camera used) in a 180° circular orbit from the right anterior oblique to left posterior oblique position. Acquisition time was 14 minute for the rest stage and 12 minute for the stress stage. Gated acquisition was performed with 8 frames per cardiac cycle. Data were reconstructed by filtered backprojection and rendered into short-axis projections. Data underwent phase analysis via the Emory Cardiac Toolbox by radiologists blinded to clinical data. A phase distribution was obtained from the gated SPECT study to represent regional onset of mechanical ventricular contraction and displayed in a polar map. Quantitative indices of HBW (including 95% of elements of the phase distribution) and PSD (the SD of the phase distribution) were analyzed.
Phase Analysis of Onset of Mechanical Contraction
This analysis of count data obtained by SPECT renders a temporal map of mechanical contraction projected on the Emory Cardiac Toolbox polar map (Figure 1).6 Ninety normal subjects (<5% likelihood of coronary artery disease) were analyzed to generate a normal database using dual phase Tl-201/Tc-99m sestamibi rest/exercise stress protocol. From 8-bin LV short-axis data sets, 3D count distribution were extracted and submitted to Fourier analysis. A first-harmonic fast Fourier transform was applied, and the calculated phase array of regional onset of myocardial contraction in 3D was rendered with 0° assigned to the peak of the R and 360° assigned to one R-R interval. The temporal resolution was tested with phantom studies at clinically relevant count densities (10 counts/pixel), demonstrating that the Fourier transform afforded high temporal resolution (approximating 1/64 of cardiac cycle).12
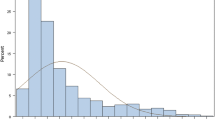
Processing steps of phase analysis. The gated SPECT MPI raw data were reconstructed and reoriented using the standard protocol to generate a gated SPECT MPI short-axis image. Regional maximal count detection was performed on the gated SPECT MPI short-axis image in 3D for each temporal frame to generate wall-thickening curves for over 600 LV regions. The wall-thickening curve for each region was approximated by the 1-harmonic function to calculate a phase angle that represented the regional onset of mechanical contraction (OMC). Once the OMC phase angles of all regions were obtained, an OMC phase distribution was generated and displayed as a polar map and a histogram. The standard deviation of the OMC phase distribution (phase standard deviation) and the histogram bandwidth (including 95% of the phase angles over the entire LV) indicated the degree of global LV dyssynchrony
Statistical Analysis
Paired t tests were used to compare measures of dyssynchrony at baseline and follow-up. Un-paired t tests were used to compare measures of dyssynchrony between cohorts. Kolmogorov-Smirnov test was performed to check the normality of the variables, and transformations were applied when needed. Relationships between measures of dyssynchrony and measures of ventricular dysfunction were assessed by Pearson’s correlation coefficients. Multivariable regression was performed by considering all the baseline dyssynchrony measures and stepwise strategy was used for variable selection. Correlations between measures of dyssynchrony and measures of ventricular dysfunction at baseline and follow-up were compared using Steiger’s Z test to account for within subject dependence. Results are expressed as mean ± SD. Statistical significance was taken at the 5% level (P < .05).
Results
Among 31 patients enrolled in the clinical trial, baseline myocardial perfusion data was not available for two patients. In one patient a gated study could not be performed. Remaining patients (n = 28) completed the initial SPECT imaging within 3 days post-infarct. Follow-up studies were performed in 25 patients approximately 6 months from index presentation. Three patients underwent repeat catheterization with repeat percutaneous coronary intervention for in-stent restenosis before the 6 month follow-up visit. One patient received an implantable cardioverter defibrillator (ICD) during the follow-up period, but was not ventricularly paced during the follow-up SPECT scan. Patients completed successful vasodilator stress without complication. Subjects exhibited a mean resting perfusion defect of 27.4% ± 16% at baseline (Table 1). Mean LVEF was relatively preserved at 46.4% ± 11%. The mean baseline QRS duration was normal (91.5 ± 17.5 ms), including one subject with a left bundle branch block. Baseline stress total severity score (STSS) was 705.0 ± 489.2 and rest total severity score (RTSS) was 549.6 ± 551.4. Among patients in the acute myocardial infarction cohort, cell therapy or standard medical therapy did not influence measures of remodeling or dyssynchrony. Compared with healthy controls (n = 22), study subjects had larger ventricular volumes and mildly reduced systolic function (Table 1).
Subjects with STEMI had prolonged regional onset of mechanical contraction compared with a cohort of 22 normal subjects (age 57.2 ± 10.6 years, <5% perfusion defect) by both HBW (100.3 ± 70.7 vs 26.5 ± 5.3 degrees, P < .0001) and PSD (35.3 ± 16.9 vs 7.9 ± 2.1 degrees, P < .0001) (Figure 2). Baseline dyssynchrony measured by HBW correlated with resting perfusion defect size (r = 0.67, P < .001), end-systolic volume (r = 0.72, P < .0001), end-diastolic volume (r = 0.63, P < .001) (Figure 3). There was an inverse correlation between baseline dyssynchrony by HBW and LVEF (r = −0.74, P < .0001). The residual ischemia after revascularization (measured by the difference between STSS and RTSS at baseline) did not correlate with remodeling or dyssynchrony measures.
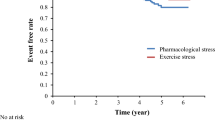
Over the follow-up period of 6 months, we observed improvements in mean LVEF (2.1% ± 14.2%, P = .01) and mean infarct size (−5.5% ± 11.1%, P = .02). Likewise, both measures of dyssynchrony by phase analysis improved (−24.1° ± 35.9°, P = .003 for HBW and −8.7° ± 14.6°, P = .006 for PSD) (Figure 4). Moreover, improvement in HBW correlated with reduction in LV end-systolic volumes (r = 0.43, P = .034)—a measure of favorable ventricular remodeling (Figure 5).
Multivariate analysis evaluated whether improvement in LVEF over the study period or 6-month LVEF was predicted by baseline LVEF, baseline perfusion defect, or baseline measurements of dyssynchrony (PSD or HBW) (Table 2). LVEF at 6 months was significantly predicted by baseline LVEF, but not independently by baseline dyssynchrony measures.
Finally, we evaluated whether a cutoff of PSD >43° predicted improvements in LVEF at 6 months using a dyssynchrony threshold described in the past to predict response to resynchronization (and therefore to demarcate severe dyssynchrony).13 In our cohort, 30.5% had PSD >43°, but this measure did not predict improvements in LVEF.
Discussion
Our study quantifies systolic dyssynchrony after STEMI, describes longitudinal changes in abnormal regional contraction during the convalescence period, and provides support that SPECT imaging can safely and reliably characterizes ventricular function in this setting. Study limitations include theoretical constraints to this count-based technique in the setting of large infarcts, the inability of our sample size to predict clinical events, and the unknown added contribution of this measure of dyssynchrony to existing measures of ventricular structure and function. Nonetheless, our study adds to a growing body of work examining an additional way myocardial perfusion imaging yields insights into cardiac function.
Here we show for the first time that survivors of STEMI demonstrate abnormal contractile regional patterns as quantified by phase analysis, even in the absence of electrical dyssynchrony. These findings confirm using a different modality observations noted by echocardiography.2 Characterization of regional mechanical function may help to better describe adverse ventricular remodeling in this setting, where even in the absence of electrical dyssynchrony we show evidence of abnormal regional ventricular contraction. The response failure of 30% of subjects with left ventricular systolic dysfunction undergoing resynchronization therapy with biventricular pacing bespeaks an underlying pathologic process where abnormal regional contraction is not entirely a consequence of delayed depolarization.15 The threshold of PSD >43° previously evaluated for response to cardiac resynchronization therapy in electrically dyssynchronous patients did not distinguish those subjects in our cohort who had adverse remodeling from those showing recovery of ventricular function.13 The clinical import of this measure of dyssynchrony remains unclear, with clinical studies needed to determine whether cardiac resynchronization or intensified medical therapy in response to abnormal dyssynchrony measures may lead to improved cardiac remodeling and clinical outcomes.
Our findings also contribute to the understanding of the natural history of post-infarct remodeling, where in the era of timely reperfusion strategies most patients avoid infarct expansion, cavity dilatation, and fall in global systolic function.16 In addition to these findings, by SPECT we also describe for the first time that measures of dyssynchrony by phase analysis improved in the 6 months following revascularization—an observation that may reflect general improvements in global systolic function. Our analysis shows that baseline LVEF remains the best predictor of LVEF at follow-up, and that in this study dyssynchrony variables do not demonstrate independent predictive value in characterizing adverse remodeling.
Use of phase analysis in this setting may find clinical value as part of a comprehensive, reproducible, and safe means of characterizing ventricular structure, function, and perfusion in the post-infarct setting—measurements with important value in prognosis.17 In addition to global contractility, chamber dimension, and infarct size, gated SPECT MPI also allows for assessment of abnormal regional contraction patterns that when taken together may ultimately predict future LV dysfunction. Here we describe for the first time a cohort of post-infarct patients characterized in serial measurements by this technique. Assessing regional uncoordinated contraction with imaging is subject to variability and technical limitations. In the PROSPECT study, variability in echo measures of dyssynchrony was high and resynchronization based on these criteria failed to outperform existing measures. MRI measurements are less variable but are technically more demanding and often not possible if an ICD or pacemaker is present.
Use of phase analysis to quantify regional ventricular systolic dysfunction is limited in some settings by its reliance on acquired counts. Since regional contractility assessment relies on changes in regional counts, contributions from scar may influence assessment of dyssynchrony. Comparisons of regional phase and function data obtained by blood pool and myocardial perfusion imaging from subjects with perfusion defects demonstrate little difference in data derived from either methodology in spite of the concern that count-poor data input from perfusion defects might influence measurements—suggesting that Fourier analysis adequately samples time-cyclic data in either method.18 Phantom studies have shown, however, that so long as >10% of regional counts are preserved, the phase analysis technique adequately reflects regional onset of mechanical contraction.19
Secondly, our small sample size is a major limitation in the statistical analysis of results, including a limited ability to evaluate the predictive value of phase analysis on clinical outcomes such as heart failure or death. Measures of adverse remodeling such as end-systolic volume are intermediate endpoints that may not be fully predictive of clinical events.
Finally, the added value of phase analysis to other measures of ventricular structure and function is unknown. In our study, HBW and PSD correlated with ventricular volumes and ejection fraction and did not outperform these measures in predicting future adverse remodeling. Further work is needed to correlate dyssynchronous regions with infarct and peri-infarct locations in order to discern the contribution of these abnormal segments to global contractile function. In spite of these limitations, measure of dyssynchrony by phase analysis may add value in understanding which patients will suffer further deterioration after myocardial infarction.
References
Shin SH, Hung CL, Uno H, Hassanein AH, Verma A, Bourgoun M, et al. Mechanical dyssynchrony after myocardial infarction in patients with left ventricular dysfunction, heart failure, or both. Circulation 2010;121:1096-103.
Zhang Y, Chan AK, Yu CM, Lam WW, Yip GW, Fung WH, et al. Left ventricular systolic asynchrony after acute myocardial infarction in patients with narrow QRS complexes. Am Heart J 2005;149:497-503.
Mollema SA, Liem SS, Suffoletto MS, Bleeker GB, van der Hoeven BL, van de Veire NR, et al. Left ventricular dyssynchrony acutely after myocardial infarction predicts left ventricular remodeling. J Am Coll Cardiol 2007;50:1532-40.
Chung ES, Leon AR, Tavazzi L, Sun JP, Nihoyannopoulos P, Merlino J, et al. Results of the Predictors of Response to CRT (PROSPECT) trial. Circulation 2008;117:2608-16.
Sanderson JE. Echocardiography for cardiac resynchronization therapy selection: Fatally flawed or misjudged? J Am Coll Cardiol 2009;53:1960-4.
Chen J, Garcia EV, Folks RD, Cooke CD, Faber TL, Tauxe EL, et al. Onset of left ventricular mechanical contraction as determined by phase analysis of ECG-gated myocardial perfusion SPECT imaging: Development of a diagnostic tool for assessment of cardiac mechanical dyssynchrony. J Nucl Cardiol 2005;12:687-95.
Trimble MA, Borges-Neto S, Smallheiser S, Chen J, Honeycutt EF, Shaw LK, et al. Evaluation of left ventricular mechanical dyssynchrony as determined by phase analysis of ECG-gated SPECT myocardial perfusion imaging in patients with left ventricular dysfunction and conduction disturbances. J Nucl Cardiol 2007;14:298-307.
Henneman MM, Chen J, Ypenburg C, Dibbets P, Bleeker GB, Boersma E, et al. Phase analysis of gated myocardial perfusion single-photon emission computed tomography compared with tissue Doppler imaging for the assessment of left ventricular dyssynchrony. J Am Coll Cardiol 2007;49:1708-14.
Trimble MA, Borges-Neto S, Honeycutt EF, Shaw LK, Pagnanelli R, Chen J, et al. Evaluation of mechanical dyssynchrony and myocardial perfusion using phase analysis of gated SPECT imaging in patients with left ventricular dysfunction. J Nucl Cardiol 2008;15:663-70.
Boogers MM, Van Kriekinge SD, Henneman MM, Ypenburg C, Van Bommel RJ, Boersma E, et al. Quantitative gated SPECT-derived phase analysis on gated myocardial perfusion SPECT detects left ventricular dyssynchrony and predicts response to cardiac resynchronization therapy. J Nucl Med 2009;50:718-25.
Trimble MA, Velazquez EJ, Adams GL, Honeycutt EF, Pagnanelli RA, Barnhart HX, et al. Repeatability and reproducibility of phase analysis of gated single-photon emission computed tomography myocardial perfusion imaging used to quantify cardiac dyssynchrony. Nucl Med Commun 2008;29:374-81.
Chen J, Faber TL, Cooke CD, Garcia EV. Temporal resolution of multiharmonic phase analysis of ECG-gated myocardial perfusion SPECT studies. J Nucl Cardiol 2008;15:383-91.
Henneman MM, Chen J, Dibbets-Schneider P, Stokkel MP, Bleeker GB, Ypenburg C, et al. Can LV dyssynchrony as assessed with phase analysis on gated myocardial perfusion SPECT predict response to CRT? J Nucl Med 2007;48:1104-11.
Quyyumi AA, Waller EK, Murrow J, Esteves F, Galt J, Oshinski J, et al. CD34(+) cell infusion after ST elevation myocardial infarction is associated with improved perfusion and is dose dependent. Am Heart J 2011;161:98-105.
Kass DA. An epidemic of dyssynchrony: But what does it mean? J Am Coll Cardiol 2008;51:12-7.
Savoye C, Equine O, Tricot O, Nugue O, Segrestin B, Sautiere K, et al. Left ventricular remodeling after anterior wall acute myocardial infarction in modern clinical practice (from the REmodelage VEntriculaire [REVE] study group). Am J Cardiol 2006;98:1144-9.
Piccini JP, Starr AZ, Horton JR, Shaw LK, Lee KL, Al-Khatib SM, et al. Single-photon emission computed tomography myocardial perfusion imaging and the risk of sudden cardiac death in patients with coronary disease and left ventricular ejection fraction >35%. J Am Coll Cardiol 2010;56:206-14.
Nichols KJ, Van Tosh A, Wang Y, Chen J, Garcia EV, Palestro CJ, et al. Relationships between blood pool and myocardial perfusion-gated SPECT global and regional left ventricular function measurements. Nucl Med Commun 2009;30:292-9.
Chen J, Henneman MM, Trimble MA, Bax JJ, Borges-Neto S, Iskandrian AE, et al. Assessment of left ventricular mechanical dyssynchrony by phase analysis of ECG-gated SPECT myocardial perfusion imaging. J Nucl Cardiol 2008;15:127-36.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Murrow, J., Esteves, F., Galt, J. et al. Characterization of mechanical dyssynchrony measured by gated single photon emission computed tomography phase analysis after acute ST-elevation myocardial infarction. J. Nucl. Cardiol. 18, 912–919 (2011). https://doi.org/10.1007/s12350-011-9414-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-011-9414-8