Abstract
Objectives
The purpose of this study is to develop a right-ventricular (RV) phase analysis tool which when coupled with our left ventricular (LV) phase analysis tool can provide measurement of the interventricular mechanical dyssynchrony from gated SPECT myocardial perfusion imaging (MPI), and validate the tool by electrocardiography (ECG).
Methods
For each patient, short-axis LV and RV SPECT MPI images were input into an automatic sampling algorithm to generate the 3D maximal count circumferential profiles for both LV and RV in each cardiac frame. Subsequently, the samples of LV and RV were separately used by our phase analysis tool based on the first-harmonic Fourier approximation to calculate the contraction onset for each sample. The difference between contraction onsets of the middle LV free wall and middle LV septal wall represented the LV contraction delay; the difference between contraction onsets of the middle RV free wall and middle RV septal wall represented the RV contraction delay. The difference between the LV and RV contraction delays represented the interventricular contraction delay, which was compared with the interventricular conduction delay classified by ECG to validate the concordance of interventricular mechanical and electrical dyssynchrony. Sixty-one bundle branch block (BBB) patients with ischemic-dilated cardiomyopathy (26, 42.6%) or non-ischemic-dilated cardiomyopathy (35, 57.4%), who underwent 12-lead surface ECG and gated resting Tc-99m sestamibi SPECT, were retrospectively analyzed in this study.
Results
In the 30 patients with left bundle branch block (LBBB) by ECG, there were 27 patients whose LV contracted later than the RV according to SPECT; and in the 31 patients with right bundle branch block (RBBB) by ECG, there were 26 patients whose LV contracted earlier than the RV according to SPECT. In total, an agreement rate of 86.9% (53 of 61) was achieved between SPECT and ECG. The Kappa agreement rate was 73.8% (95% confidence interval 0.57-0.91).
Conclusion
The preliminary results showed promise for the measurement of interventricular mechanical dyssynchrony in BBB patients with dilated cardiomyopathy using our phase analysis tool.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Interventricular mechanical dyssynchrony is an important factor to select potential responders to cardiac resynchronization therapy (CRT) in patients with heart failure.1,2 Echocardiography is a frequently used clinical tool to measure interventricular mechanical dyssynchrony in the current clinical practice.1-3 However, the reproducibility of measuring mechanical dyssynchrony by echocardiography may limit its clinical applicability.4
Phase analysis from gated SPECT MPI may provide an alternative clinical tool to measure left ventricular (LV) mechanical dyssynchrony.5-7 The LV dyssynchrony parameters have been demonstrated to correlate well with those by echocardiography.8,9 RV myocardium usually has very low counts on SPECT MPI images due to its thinner myocardium compared to the LV albeit RV perfusion has been quantified.10 As a consequence, the low RV myocardial counts make it difficult to extend the phase analysis tool for LV mechanical dyssynchrony to measure RV mechanical dyssynchrony. Nevertheless, RV is visible on MPI in certain patient populations, for example, patients with dilated cardiomyopathy. Accordingly, it may be feasible to develop RV phase analysis tool to compare the onset of contraction between the LV and RV in order to measure interventricular mechanical dyssynchrony in those patients.
The purpose of this study was to develop a RV phase analysis tool to measure interventricular mechanical dyssynchrony from gated SPECT MPI and validate it against electrocardiograms (ECG).
Materials and Methods
Patient Data
Sixty-one BBB patients with dilated cardiomyopathy, who had undergone both 12-lead surface ECG and gated resting Tc-99m sestamibi SPECT, were enrolled in this study. All of the patients had left bundle branch block (LBBB) or right bundle branch block (RBBB) classified by ECG. RV myocardium was clearly visible on the MPI images for all of the patients in this study. The baseline characteristics of all patients are listed in Table 1.
Twelve-Lead Surface ECG
Twelve-lead ECG during sinus rhythm was conducted in all patients with a Mac 5000 System (GE Medical Systems, Milwaukee, WI, USA). QRS durations were measured either manually or by a computerized ECG system analysis of intervals. The areas of QRS wave were measured manually from ECG recordings. A small compartment on the ECG recording paper was defined as 1 × 1 mm. The whole areas of QRS wave were summed on all 12 leads.
SPECT Image Processing
The gated SPECT scan was performed around 60 minutes post injection of 20-30 mCi of Tc-99m sestamibi. SPECT planar images were acquired on a dual-headed camera (Philips Medical Systems, Milpitas, CA, USA) using a standard resting protocol. The imaging parameters were 20% energy window around 140 keV, 180° orbit, 32 steps with 25 seconds per step, 8-bin gating, and 64 projections per gate. The total acquisition time was 14 minutes for each patient.
Image reconstruction and reorientation were completed with Emory Reconstruction Toolbox (ERToolbox; Atlanta, GA). SPECT images were reconstructed by ordered subset expectation maximization (OSEM) with 3 iterations and 10 subsets, and then filtered by a Butterworth low-pass filter with a cutoff frequency of 0.3 cycles/mm and an order of 10. The pixel size of reconstructed images was 6.4 × 6.4 × 6.4 mm3.
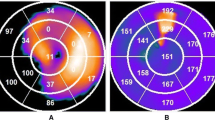
The LV and RV short-axis images were submitted to interactive interfaces to manually identify LV and RV parameters as illustrated in Figure 1A, B, which included the apex, base, and the myocardial center and radius of LV and RV, respectively. These parameters were input into an automatic sampling algorithm, which searched in 3D for the maximal count circumferential profiles for LV and RV separately. The phase analysis tool based on the first-harmonic Fourier approximation5 was used to calculate the onset of contraction for each sample. The phase angles of LV and RV samples were displayed on the LV and RV polar maps, which were then segmented using a 13-segmentation model used by electrophysiologists11,12 to calculate the regional mean phases in the segments, as illustrated in Figure 1C, D. The difference between the mean phases of the middle LV free wall and middle LV septal wall represented the LV contraction delay, expressed as Δ LV. The difference between the mean phases of the middle RV free wall and middle RV septal wall represented the RV contraction delay, expressed as Δ RV.
SPECT phase quantification. A An interactive tool to specify LV sampling parameters, including the apex, base, and the center and radius of the LV myocardium. B An interactive tool to specify RV sampling parameters, including the apex, base, and the center and radius of the RV myocardium. In order to enhance the visibility of RV myocardium, all the pixels with ≥40% maximum were set to the maximum brightness in RV SA. C The polar map of LV contraction delays. D The polar map of RV contraction delays. The number in each segment of 13-segment polar map is the mean phase in the region. The greater the number is, the later the segment contracts. The average difference of the two segments enclosed by each of the four ellipses is the measured contraction delay. Purple ellipse, the middle LV septal wall; yellow ellipse, the middle LV free wall; red ellipse, the middle RV free wall; blue ellipse, the middle RV septal wall. SA, short-axis; VLA, vertical long-axis; HLA, horizontal long-axis
Statistical Analysis
A dichotomous rule was applied to the phase analysis results to determine the interventricular contraction delay: if Δ LV > Δ RV, the LV contracted later than the RV; if Δ LV < Δ RV, the LV contracted earlier than the RV. The concordance between interventricular contraction delays by SPECT and interventricular conduction delays by ECG was evaluated by the kappa agreement rate calculated for all of the enrolled 61 patients.
Results
Figure 2 shows the contraction delays of LV (Δ LV) and RV (Δ RV) for all the enrolled patients. The individual below the line Δ LV = Δ RV is classified as the patient whose LV contracts later than the RV.
Table 2 compares the interventricular contraction delays measured by SPECT with the interventricular conduction delays classified by ECG. In the 30 patients with LBBB by ECG, there were 27 patients whose LV contracted later the RV according to SPECT; and in the 31 patients with RBBB by ECG, there were 26 patients whose LV contracted earlier than the RV according to SPECT. The agreement rate was similar in both LBBB and RBBB groups (90.0% and 83.9%, respectively). The overall agreement rate was 86.9% for all of the 61 patients. The overall Kappa agreement rate was 73.8% (95% confidence interval 0.57-0.91).
Figure 3 shows two patient examples using our LV and RV phase analysis tool to measure the interventricular mechanical dyssynchrony. Figure 3A shows a LBBB patient for whom Δ LV=1.12° and Δ RV = −7.70°, so the LV contracted later than the RV. Figure 3B shows a RBBB patient for whom Δ LV = −1.13° and Δ RV = 3.63°, so the RV contracted later than the LV. The interventricular contraction delays by SPECT were concordant with the interventricular conduction delays by ECG for both patients.
Two patient examples. A A patient with LBBB. The mean phases of the middle LV free wall, middle LV septal wall, middle RV free wall, and middle RV septal wall, measured by SPECT, were 93.18°, 92.06°, 84.58°, and 92.28°, respectively. The contraction delays of LV (Δ LV) and RV (Δ RV) are 1.12° and −7.70°, respectively, indicating the RV contracts earlier than the LV. B A patient with RBBB. The mean phases of the middle LV free wall, middle LV septal wall, middle RV free wall, and middle RV septal wall, were 91.20°, 92.33°, 103.80°, and 100.17°, respectively. The contraction delays of LV (Δ LV) and RV (Δ RV) are −1.13° and 3.63°, respectively, indicating RV contracts later than the LV
Discussion
This is the first report of a RV phase analysis tool which when coupled with our LV phase analysis tool5 measures the interventricular mechanical dyssynchrony from gated SPECT MPI. With this new tool, the contraction delays of LV and RV were quantified, and then the interventricular contraction delay was determined. There was a concordance of 86.9% between the interventricular contraction delays by SPECT and interventricular conduction delays by ECG in 61 BBB patients with dilated cardiomyopathy.
Clinical Value of Interventricular Mechanical Dyssynchrony
ECG is a standard tool to detect patients with interventricular electrical dyssynchrony. QRS duration classified by ECG has demonstrated its clinical value to predict CRT response. Sinus rhythm, LBBB with QRS duration ≥150 ms on ECG, LVEF ≤35%, NYHA class II, III, or ambulatory IV symptoms are the standard indications for CRT patient selection in the current guidelines.13 Patients with RBBB are less likely to benefit from CRT and can be even worse.14 In addition, it was found that there was a significant correlation between QRS duration and interventricular mechanical delay.15
However, ECG is ineffective to measure the presence and severity of electrical dyssynchrony in all ventricular segments and only significant myocardial masses can influence QRS morphology and duration.16 QRS duration is not specific enough to characterize the exact electric and mechanical activation pattern.17 LBBB can result in different and heterogeneous electric and mechanical LV contraction delay patterns, despite similar surface ECG morphology and duration.18,19 Patients with more severe interventricular mechanical dyssynchrony can benefit more from CRT, thus interventricular mechanical dyssynchrony has been used to select CRT patients in clinical studies.1,20
In the current clinical practice, echocardiography is a frequently used clinical tool to measure interventricular mechanical dyssynchrony.1-3 In the CARE-HF clinical trial,1 the interventricular mechanical delay was calculated as the time difference between the onset of forward flow in the LV and RV outflow tracts on echocardiography images. An interventricular mechanical delay of >40 ms can be pathological.
A major problem, which influences the clinical applicability of measuring mechanical dyssynchrony from echocardiography, is the relatively poor reproducibility of this technique. In the PROSEPCT trial,4 it was found that the reproducibility arising from technical and interpretative factors influenced the clinical value of guidance parameters measured from echocardiography; as a consequence, the echocardiographic technique failed to improve the CRT response beyond the current guidelines.
Our Tool to Measure Interventricular Mechanical Dyssynchrony
Phase analysis has been used to measure LV mechanical dyssynchrony from gated SPECT MPI. It was shown to have good temporal resolution,21 high repeatability and reproducibility,22 and good robustness with heart rate23 and perfusion defects.24 The LV mechanical dyssynchrony parameters have been demonstrated to correlate well with those by Tissue Doppler imaging.8,9 It is clinically important to extend the phase analysis technique to measure RV dyssynchrony and interventricular mechanical dyssynchrony.
Recently, we have developed a new tool to measure RV mechanical dyssynchrony by phase analysis on PET in patients with pulmonary hypertension.25 The results showed that there was a significant correlation between RV dyssynchrony by phase analysis from PET and that by speckle tracking from echocardiography. This study coupled the LV and RV tools to measure the interventricular mechanical dyssynchrony from gated SPECT MPI. The concordance with ECG in 61 patients suggested the LV and RV phase analysis tool from gated SPECT MPI was promising to be a clinical tool to measure the interventricular mechanical dyssynchrony.
Clinical Applicability of Our Tool to Measure Interventricular Mechanical Dyssynchrony
A major concern to use this tool in the clinical practice could be the visibility of RV. The timing of image acquisition in the current protocol of gated SPECT MPI is the maximal contrast agent uptake of LV. RV myocardium on MPI usually has low counts due to its thinner myocardium, so it may be unclear or even invisible. Nevertheless, RV is visible on MPI in certain patient populations, for example, patients with dilated cardiomyopathy or pulmonary hypertension, making it feasible to measure RV dyssynchrony by phase analysis. Moreover, this technique is readily applicable to MPI PET where new high contrast perfusion agents like flurpiridaz demonstrate excellent RV visualization.26
The other concern could be the repeatability and reproducibility of this tool since the manual operations are required to specify the LV and RV parameters. However, the previous study suggested the LV phase analysis tool, which required manual specification of LV parameters, had high repeatability and reproducibility.22 Since the RV phase analysis tool requires the similar parameters as the LV phase analysis tool, no significant difference in the repeatability and reproducibility is expected between these tools.
Study Limitations
The technical accuracy of measuring the interventricular mechanical dyssynchrony from gated SPECT MPI was tested in a relatively small sample size and in a single medical center. A larger multi-center clinical study is needed to establish the clinical usefulness of this technique.
New Knowledge Gained
This is the first report of a RV phase analysis tool which when coupled with our LV phase analysis tool5 measures the interventricular mechanical dyssynchrony from gated SPECT MPI. In BBB patients with dilated cardiomyopathy, the interventricular contraction delays measured by SPECT were highly concordant with interventricular conduction delays measured by ECG.
Conclusion
The preliminary results showed the promise for the measurement of interventricular mechanical dyssynchrony using our LV and RV phase analysis of gated SPECT MPI in BBB patients with dilated cardiomyopathy.
Abbreviations
- RV:
-
Right ventricle/ventricular
- LV:
-
Left ventricle/ventricular
- SPECT:
-
Single-photon emission computed tomography
- MPI:
-
Myocardial perfusion imaging/images
- ECG:
-
Electrocardiography
- CRT:
-
Cardiac resynchronization therapy
- LBBB:
-
Left bundle branch block
- RBBB:
-
Right bundle branch block
- OSEM:
-
Ordered subset expectation maximization
References
Richardson M, Freemantle N, Calvert MJ, Cleland JG, Tavazzi L. Predictors and treatment response with cardiac resynchronization therapy in patients with heart failure characterized by dyssynchrony: A pre-defined analysis from the CARE-HF trial. Eur Heart J 2007;28:1827-34.
Wiesbauer F, Baytaroglu C, Azar D, Blessberger H, Goliasch G, Graf S, et al. Echo Doppler parameters predict response to cardiac resynchronization therapy. Eur J Clin Invest 2009;39:1-10.
Galderisi M, Cattaneo F, Mondillo S. Doppler echocardiography and myocardial dyssynchrony: A practical update of old and new ultrasound technologies. Cardiovasc Ultrasound 2007;5:28.
Chung ES, Leon AR, Tavazzi L, Sun JP, Nihoyannopoulos P, Merlino J, et al. Results of the predictors of response to CRT (PROSEPCT) trial. Circulation 2008;117(20):2608-16.
Chen J, Garcia EV, Folks RD, Cooke CD, Faber TL, Tauxe EL, et al. Onset of left ventricular mechanical contraction as determined by phase analysis of ECG-gated myocardial perfusion SPECT imaging: Development of a diagnostic tool for assessment of cardiac mechanical dyssynchrony. J Nucl Cardiol 2005;12:687-95.
Boogers MJ, Chen J, van Bommel RJ, Borleffs CJ, Dibbets-Schneider P, van der Heil B, et al. Optimal left ventricular lead position assessed with phase analysis on gated myocardial perfusion SPECT. Eur J Nucl Med Mol Imaging 2011;38:230-8.
Friehling M, Chen J, Saba S, Bazaz R, Schwartzman D, Adelstein EC, et al. A prospective pilot study to evaluate the relationship between acute change in left ventricular synchrony after cardiac resynchronization therapy and patient outcome using a single-injection gated SPECT protocol. Circ Cardiovasc Imaging 2011;4:532-9.
Henneman MM, Chen J, Ypenburg C, Dibbets P, Bleeker GB, Boersma E, et al. Phase analysis of gated myocardial perfusion SPECT compared to tissue Doppler imaging for the assessment of left ventricular dyssynchrony. J Am Coll Cardiol 2007;49:1708-14.
Marsan NA, Henneman MM, Chen J, Ypenburg C, Dibbets P, Ghio S, et al. Left ventricular dyssynchrony assessed by two 3-dimensional imaging modalities: Phase analysis of gated myocardial perfusion SPECT and tri-plane tissue Doppler imaging. Eur J Nucl Med Mol Imaging 2008;35:166-73.
DePuey EG, Jones ME, Garcia EV. Evaluation of right ventricular regional perfusion with technetium-99m-sestamibi SPECT. J Nucl Med 1991;32(6):1199-205.
Becker M, Hoffmann R, Schmitz F, Hundemer A, Juhl H, Schauerte P, et al. Relation of optimal lead positioning as defined by three-dimensional echocardiography to long-term benefit of cardiac resynchronization. Am J Cardiol 2007;100(11):1671-6.
Chau J, Zhou W, Ho JK, Patel NA, Mackensen GB, Mahajan A. Acute right ventricular pressure overload compromises left ventricular function by altering septal strain and rotation. J Appl Physiol 2013;115(2):186-93.
ACCF/AHA/HRS. ACCF/AHA/HRS focused update incorporated into the ACCF/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. Circulation 2008;2013(127):e283-352.
Tompkins C, Kutyifa V, McNitt S, Polonsky B, Klein HU, Moss AJ, et al. Effect on cardiac function of cardiac resynchronization therapy in patients with right bundle branch block (from the Multicenter Automatic Defibrillator Implantation Trial With Cardiac Resynchronization Therapy [MADIT-CRT] trial). Am J Cardiol 2013;112:525-9.
Haghjoo M, Bagherzadeh A, Fazelifar AF. Prevalence of mechanical dyssynchrony in heart failure patients with different QRS durations. Pacing Clin Electrophysiol 2007;30:616-22.
Hawkins NM, Petrie MC, MacDonald MR, Hogg KJ, McMurray JJ. Selecting patients for cardiac resynchronization therapy: Electrical or mechanical dyssynchrony? Eur Heart J 2006;27:1270-81.
Delgado V, Bax JJ. Assessment of systolic dyssynchrony for cardiac resynchronization therapy is clinically useful. Circulation 2011;123:640-55.
Jia P, Ramanathan C, Ghanem RN, Ryu K, Varma N, Rudy Y. Electrocardiographic imaging of cardiac resynchronization therapy in heart failure: Observation of variable electrophysiologic responses. Heart Rhythm 2006;3:296-310.
Vatasescu R, Berruezo A, Mont L, Tamborero D, Sitges M, Silva E, et al. Midterm, “super-response” to cardiac resynchronization therapy by biventricular pacing with fusion: Insights from electro-anatomical mapping. Europace 2009;11:1675-82.
Cleland JG, Daubert JC, Erdmann E. The effect of cardiac resynchronization on morbidity and mortality in heart failure. N Engl J Med 2005;352:1539-49.
Chen J, Faber TL, Cooke CD, Garcia EV. Temporal resolution of multi-harmonic phase analysis of ECG-gated myocardial perfusion SPECT studies. J Nucl Cardiol 2008;15:383-91.
Trimble MA, Velazquez EJ, Adams GL, Honeycutt EF, Pagnanelli RA, Barnhart HX, et al. Repeatability and reproducibility of phase analysis of gated SPECT myocardial perfusion imaging used to quantify cardiac dyssynchrony. Nucl Med Commun 2008;29:374-81.
AlJaroudi W, Iqbal F, Heo J, Iskandrian AE. Relation between heart rate and left ventricular mechanical dyssynchrony in patients with end-stage renal disease. Am J Cardiol 2011;107:1235-40.
Cheung A, Zhou Y, Faber TL, Garcia EV, Zhu L, Chen J. The performance of phase analysis of gated SPECT myocardial perfusion imaging in the presence of perfusion defects: A simulation study. J Nucl Cardiol 2012;19:500-6.
Wang L, Zhou W, Liang Y, Yang Y, Garcia EV, Chen J, et al. Right ventricular dyssynchrony in pulmonary hypertension: Phase analysis using FDG-PET imaging. J Nucl Cardiol 2015. doi:10.1007/s12350-015-0341-y.
Berman DS, Germano G, Slomka PJ. Improvement in PET myocardial perfusion image quality and quantification with flurpiridaz F 18. J Nucl Cardiol 2012;19:S38-45.
Acknowledgments
This research was partly supported by a grant from the American Heart Association (15POST22690035, PI: Weihua Zhou, Ph.D.) and a New Faculty startup grant from the University of Southern Mississippi (Project No.: DE01791). Drs. Chen and Garcia receive royalties from the sales of Emory Cardiac Toolbox.
Disclosure
The terms of this arrangement have been reviewed and approved by Emory University in accordance with its conflict-of-interest practice.
Author information
Authors and Affiliations
Corresponding author
Additional information
See related editorial, doi:10.1007/s12350-016-0550-z
Rights and permissions
About this article
Cite this article
Zhou, W., Jiang, Z., Chen, J. et al. Development and validation of a phase analysis tool to measure interventricular mechanical dyssynchrony from gated SPECT MPI. J. Nucl. Cardiol. 24, 1680–1686 (2017). https://doi.org/10.1007/s12350-016-0503-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-016-0503-6