Abstract
Background
Primary microvascular angina (PMA) is a common clinical condition associated to negative impact on quality of life (QOL) and reduced physical capacity. This study aimed at evaluating the effects of aerobic physical training (APT) on myocardial perfusion, physical capacity, and QOL in patients with PMA.
Methods
We investigated 12 patients (53.8 ± 9.7 years old; 7 women) with PMA, characterized by angina, angiographycally normal coronary arteries, and reversible perfusion defects (RPDs) detected on 99mTc-sestamibi-SPECT myocardial perfusion scintigraphy (MPS). At baseline and after 4 month of APT, the patients underwent MPS, cardiopulmonary test, and QOL questionnaire. Stress-rest MPS images were visually analyzed by attributing semi-quantitative scores (0 = normal; 4 = absent uptake), using a 17-segment left ventricular model. Summed stress, rest, and difference scores (SDS) were calculated.
Results
In comparison to the baseline, in the post-training we observed a significant increase in peak-VO2 (19.4 ± 4.8 and 22.1 ± 6.2 mL·kg−1·minute−1, respectively, P = .01), reduction of SDS (10.1 ± 8.8 and 2.8 ± 4.9, P = .008), and improvement in QOL scores.
Conclusions
Physical training in patients with PMA is associated with reduction of myocardial perfusion abnormalities, increasing of physical capacity, and improvement in QOL. The findings of this hypothesis-generating study suggest that APT can be a valid therapeutic option for patients with PMA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary microvascular dysfunction (CMD) due to functional or structural derangement has been recognized as the fundamental disorder causing myocardial ischemia in the presence of normal subepicardial coronary arteries in several clinical settings such as dilated and hypertrophic cardiomyopathies, hypertension, and diabetes mellitus.1-3
CMD may also be the cause of angina in the absence of any perceptible cardiac or systemic disease, a clinical setting known as primary microvascular angina (PMA)4 In clinical practice, PMA is identified in patients with typical effort-induced chest pain exhibiting evidence of myocardial ischemia in noninvasive tests such as stress ECG or myocardial perfusion imaging, associated with failure to demonstrate fixed or dynamic obstruction in epicardial coronary arteries during angiography.5 PMA is a prevalent condition, being reported in up to 30% of patients with chest pain referred to coronary angiography.6
The clinical relevance of PMA is related not only to its high prevalence and an increased risk of future cardiovascular events,6,7 but also its association with a significant decline in quality of life (QOL).8 Several reports have shown that patients with microvascular angina present recurrent symptoms and frequently seek the emergency room, with repeated hospitalizations and coronary angiographies.9
The therapeutic options already tested for PMA include beta blockers, calcium antagonistsm and other coronary vasodilators such as nitrates,10,11 antidepressant drugs, and ACE-inhibitors. However, the majority of patients show poor initial response to treatment and frequent symptomatic recurrence.2-4,12
We hypothesize that aerobic physical training (APT) could ameliorate the myocardial perfusion disturbance and angina symptoms in patients with PMA. This therapeutic effect could theoretically be mediated by improvement in coronary microvascular function and endothelial function, an effect likely related to the physical training.13 However, no previous study tested the effect of APT over the myocardial perfusion disturbance in the clinical context of PMA.
Thus, the objective of this pilot study, designed to provide data to power a subsequent larger randomized study, was to investigate the effects of APT on myocardial perfusion abnormalities, detected by myocardial perfusion single-photon emission computed tomography (SPECT) imaging, and the impact on the QOL of patients with PMA.
Methods
Patient Series
A prospective study was conducted in 15 patients with precordial anginal pain associated with the presence of two or more myocardial segments with reversible perfusion defects (RPDs) identified by SPECT MPS with 99mTc-sestamibi and angiographically normal subepicardial coronary arteries. For this study, normal coronary arteries were defined as absence of obstruction of any degree as evaluated by selective invasive coronary angiography. Coronary artery spasm was not ruled out by using any specific provocative test, however, the clinical presentation of effort angina present in all patients and the absence of ST elevation during pain, make this diagnosis very unlikely.
Exclusion criteria were: patients with other clinical conditions potentially associated with precordial pain or coronary disturbances such as chronic obstructive pulmonary disease, inflammatory or other connective tissue diseases, dilated or hypertrophic cardiomyopathy, cardiac valve disease, obstructive lesions of the coronary artery vessels of any degree, and Chagas disease.
Three additional patients were excluded from the study because of a low compliance rate to the training sessions.
The demographic and clinical characteristics of the investigated patient sample (n = 12) are summarized in Table 1.
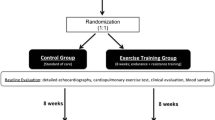
General Study Design
After inclusion in the study, the patients were submitted to baseline evaluation including a cardiopulmonary test (CPT) and a QOL questionnaire (SF-36). The results of MPS performed during the screening exams were considered to be part of the baseline evaluation of the patients included in the study. Patients were submitted to supervised aerobic physical training for a period of 4 months. In all patients, the medicines and doses were maintained the same, as registered in the baseline condition, during all the training period. In the post-training evaluation, the patients were again submitted to MPS, CPT, and QOL assessment.
Myocardial Perfusion Scintigraphy
Beta blockers and other anti-ischemic drugs were discontinued for a period of 48 hours before the exam. Images at rest were acquired 1 hour after the injection of 10 mCi 99Tc-sestamibi. After 3-4 hours, 25mCi 99Tc-sestamibi was injected during peak effort on the treadmill, using the Bruce protocol, with acquisition of effort images 1 hour after the injection. The estimated radiation exposure was 11 mSv for each stress-rest MPS study. In the study conducted at baseline, the effort test was interrupted due to cardiorespiratory exhaustion. In the evaluation after physical training, the peak effort radiotracer injection was performed, and the effort interrupted, when the patient reached the same heart rate that was obtained at the initial pre-training test. This was established in order to achieve a similar peak myocardial oxygen uptake in the two conditions.
The images were acquired with a double-detector gamma camera (DST-SMV America, Twinsburg, OH, USA) with the patient in the supine position, using a 180° circumferential orbit from the anterior right oblique projection to the posterior left oblique projection, with 32 projections, 30 seconds/projection, and a 20% energy window centered on 140 keV.
The SPECT-reconstruction (Sopha Medical Vision—General Electric) software was used for calculation of tomographic slices on the classical orthogonal axis. The perfusion images were evaluated by visual semi-quantitative analysis by two experienced observers that were blinded regarding the clinical data and phase of the study (baseline vs post-training). The discordances in the analysis were solved by consensus. These two blinded-observers were not involved in the conduction of the study or in the clinical manipulation of the patients or their data. A left ventricular segmentation model of 17-segment was used. During the images analysis, those cases suggesting the presence of attenuation artifacts, specially breast attenuation, were excluded from the study population. The segmental myocardial uptake in each stress and rest image was scored as follows: 0 = normal; 1 = mild reduction; 2 = moderate reduction; 3 = severe reduction; 4 = absence of uptake. Segments with higher scores of perfusion defect in the stress images than in the rest images were considered to present RPD. The number of segments with RPD was recorded for each patient. The average severity of the stress perfusion defects was also calculated.
Summed scores were calculated for rest images (SRS), stress images (SSS), and summed difference score between SSS and SRS (SDS). The last score estimates the combined global severity/extent of the RPDs. The percent amount of myocardium involved in the perfusion defects was estimated by calculating the ratio of the obtained summed perfusion score by its highest possible value (a maximum score of 4 in 17 segments = 68).
Cardiopulmonary Test
A continuous dynamic physical effort protocol on a treadmill was used until exhaustion. Ventilatory variables were measured using an ergospirometric system of gas analysis (Ultima CPX—Medical Graphics Corporation, St. Paul, Minnesota, UAS). The following variables were compared between the baseline and post-training period: oxygen uptake at peak effort (peak-VO2) and respiratory exchange ratio, peak heart rate, and peak systolic arterial pressure. The peak-VO2 was used to assess objectively the degree of cardiorespiratory fitness of the patients at baseline, as well as the increased physical capacity promoted by the aerobic physical training program.
Quality of Life Assessment
The QOL was evaluated by the use of SF36 QOL questionnaire at baseline and after training.
Aerobic Physical Training
After baseline evaluation, the patients were submitted to supervised aerobic physical training during 4 months, three times a week in sessions lasting 1 hour each. Training intensity was moderate, based on peak-VO2 reached in baseline CPT, with a training heart rate between 60% and 85% of VO2 peak.
The supervised physical training sessions of the program of cardiovascular rehabilitation included the following sequence of events: 5 minutes of global stretching exercises, 5 minutes of walking on the treadmill at heart rate values lower than prescribed for training, and 30 minutes of physical conditioning (60%-85% VO2 peak). Next, a 5-minute phase of cooling down was performed, followed by 10 minutes of resisted exercises and a final 5-minute phase of relaxation.
The compliance with the training protocol was carefully recorded and the patients exhibiting low compliance (<90%) were excluded from the study (n = 3).
Statistical Analysis
The continuous variables are reported as mean ± SD and the nominal variables as absolute frequency (n) and percentage (%). Statistical analysis was performed using the GraphPad InStat software version 3.05. The Kolmogorov-Smirnov normality test was applied to determine whether the variables studied presented normal distribution. The Student paired t test was used to assay the variables. The level of significance was set at 5% (P < .05) and the confidence intervals (CI) were established at 95% in all analyses.
Ethical Aspects
The study was approved by the Research Ethics Committee of our institution (protocol no. 2842/2008 Comitê em Ética e Pesquisa do HCRP-FMRP-USP). All patients participated in the study as volunteers and gave written informed consent.
Results
Cardiopulmonary Test
Table 2 shows that, among the variables obtained from CPT, the peak-VO2 showed a statistically significant increase after the period of physical training (22.1 ± 6.2 mL·kg−1·minute−1) as compared to the baseline values (19.4 ± 4.8 mL·kg−1·minute−1), P = .01 (CI −4.7 to −0.7).
Myocardial Perfusion Scintigraphy
Table 3 summarizes the results obtained with MPS. No significant differences in the hemodynamic variables were observed between the baseline and post-training evaluations. In particular, the peak heart rate vs arterial pressure product was 24,760 ± 5,069 bpm mm Hg in the baseline evaluation and reached 24,238 ± 6,680 bpm mm Hg in the post-training evaluation, with no significant difference between evaluations (P = .62, CI −1,788.6 to 2,834).
In the baseline condition although there was a wide variation among individual patients regarding the severity/extension of myocardial ischemia, all patients had at least 2 segments with reversibility (range 2-16 segments), with a mean of 7.7 ± 4.5 segments/patient. The score of the stress perfusion defects ranged from 1 to 3, but most of them were of mild severity. During the analysis, we excluded the influence of scaling and attenuation artifacts as the cause of defects encompassing a very large extent of myocardium. Although the majority of the defects were mild, we also had individuals with more severe abnormalities, as shown in the illustrative example of Figure 1. The average severity of stress perfusion score was 1.3 ± 0.4, ranging from 1.0 to 1.92.
Regarding the topography of the reversible defects and its correlation with the territory of coronary artery irrigation, 3 patients (25%) presented reversible defects in the territory depending on the left anterior descending coronary, 3 (25%) in the territory depending on the right coronary and/or circumflex coronary, and 6 (50%) showed distribution of defects in multivessel territory.
After the period of aerobic physical training, 10 of the 12 trained patients (83%) showed some degree of reduction of the number of segments with RPD, while 8 (67%) patients presented complete resolution of the RPDs.
In the baseline pre-training condition, the total number of segments with reversibility was 92, with a mean of 7.7 ± 4.5 segments per patient. After the period of physical training, there was a significant reduction of the total number of segments with perfusion reversibility to 28, with a mean per patient of 2.3 ± 4.1 segments, P = .002 (CI 2.4-8.3).
For SRS values, there was no significant difference between the pre-training exam (0.7 ± 1.1) and the post-training exam (0.3 ± 0.5), P = .31 (CI −0.3 to 1.2). However, a significant difference in SSS was observed between the baseline evaluation (10.8 ± 8.7) and the post-training evaluation (3.1 ± 5), P = .004 (CI 2.9-12.4).
The SDS showed a significant reduction in the post-training condition (2.8 ± 4.9) in comparison with the initial condition (10.1 ± 8.8), P = .008 and CI 2.2-12.2 (Figure 1).
The percent amount of left ventricular myocardium showing reversibility in the baseline was 14.8% ± 13.0%, value significantly larger than the amount observed in the post-training (4.2% ± 7.2%) (P = .008), CI 3.3-18.02.
Figure 2 is an illustrative example of MPS images of one patient investigated.
Illustrative example of a 44-year-old female patient. (A) Images of representative tomographic sections of the baseline MPS during stress and rest showing severe reversible perfusion defects (white arrows), involving a large extent in multiarterial territory on the anterior, lateral, and inferior walls of the LV. The semi-quantitative visual analysis showed an SDS of 25 points. The effort ECG showed no ischemic ST-T changes, despite the presence of limiting precordial chest pain at the peak effort. (B) At the evaluation after physical training, there was no reversible perfusion defects (SDS = 0), through the disappearance of perfusion abnormalities during stress. The patient presented no ECG changes or chest pain in this evaluation
Quality of Life Questionnaire: SF36
Table 4 summarizes the results obtained by applying the SF-36 questionnaire. Of the eight domains analyzed by the SF-36, only the General Health Status showed an improvement in the post-training evaluation (68.7% ± 28.4%) compared to baseline (54.3% ± 21.1%) P = .13 (CI −34.1 to 5.2), that was not statistically significant.
Discussion
The main results of the present investigation show that 4 months of aerobic physical training performed by patients with PMA was associated with a significant reduction in myocardial perfusion abnormalities and a relevant improvement in the QOL. To the best of our knowledge, this study is the first to suggest a therapeutic effect of physical training over myocardial perfusion disturbance in patients with primary microvascular coronary dysfunction.
In this investigation, the presence of CMD was confirmed by the detection of RPDs using MPS in patients exhibiting epicardial coronaries free of obstructive lesion of any magnitude at invasive coronary angiography.14-19 The use of this inclusion criterion was based on previous studies showing that RPDs correlate with the presence of a reduced coronary flow reserve in patients with CMD.20,21 Legrand et al demonstrated that 4 of 18 patients (22.2%) with precordial pain and normal coronaries showed RPDs in MPS and that they also had a reduced coronary flow reserve, suggesting that the presence of RPDs in patients with chest pain and normal coronaries is a strong indicator of reduced coronary blood flow caused by dysfunction of the coronary microvasculature.21
On this basis, we may consider that, in the present study, the extent/severity of RPDs reflected the severity of microvascular myocardial ischemia. Actually, the adoption of the presence of RPDs as an inclusion criterion for all patients guaranteed the constitution of a more homogeneous sample of patients with CMD regarding the demonstration of abnormal myocardial perfusion associated to the chest pain.
In the present series of patients, the amount of left ventricular myocardium exhibiting RPDs per patient was about 15%. Other studies reporting the use of MPS in patients with microvascular angina showed a similar extent of LV ischemic involvement.22,23 In a study of 20 patients with syndrome X, Vermeltfoort et al22 detected 39 (12%) segments with RPDs out of a total of 335 segments studied by MPS. Cavusoglu et al observed that 18 of 31 patients (58%) submitted to MPS presented RPDs in multiarterial segments, involving 17% of the LV surface.23
Regarding the topographic distribution of RPDs, we documented a high percentage (50%) of patients exhibiting RPDs in multivessel coronary territories. These data corroborate results of previous studies demonstrating that the perfusion defects of patients with CMD are very frequently distributed in multiple vascular territories, with a typically diffuse pattern.4,12
The results of the present investigation suggested a beneficial impact of aerobic physical training on the extent and severity of microvascular ischemia. It is important to emphasize that the reduction in the extent and severity of RPDs was attained by the normalization of perfusion during stress, not by the conversion of reversible defects into fixed perfusion defects, what would indicate an aggravation of the myocardial perfusion conditions. In fact, most patients (83%) exhibited a reduction of RPDs after physical training, with complete resolution in 8 of 12 patients (66%). These results were also confirmed by the semi-quantitative analysis based on visual scores.
No previous study evaluating the effect of physical training on the abnormalities of myocardial perfusion in patients with CMD has been reported in the literature. Few previous studies have already documented beneficial effects of physical training in patients with microvascular angina regarding improvement of functional capacity and QOL.24,25 However, in those reports the changes in myocardial perfusion were not investigated. Thus, the results of the present pilot study showing that the symptom improvement after the aerobic training occurs in association with the reduction of the myocardial perfusion disturbance suggests a therapeutic benefit of physical training in this common clinical condition.
The mechanisms possibly involved in the improvement of myocardial perfusion following the physical training may include: (1) Improved vasodilator response of the endothelium-dependent coronary microcirculation. (2) A favorable change over an impaired autonomic control of the coronary microcirculation, so that a better sympathovagal balance could lead to a reduction of the degree of activation of the sympathetic innervation and a consequent reduction of the arteriolar constrictor response during the sympathetic stimulus provoked by physical stress. (3) Reduction of the degree of spasticity of the coronary microcirculation due to intrinsic changes in the vascular smooth muscle.
Several previous investigations on patients with atherosclerotic coronary artery disease suggest that physical training can improve myocardial perfusion due to adaptations in the coronary vascular bed and/or by recruitment of collateral vessels, indirectly agreeing with the findings of the present study.26-30
The physical capacity in the baseline condition, measured by peak-VO2 (19.4 ± 4.8 mL·kg−1·minute−1) was reduced in our patients in a degree quite comparable to the results reported by Dominguez-Rodriguez et al31 (20.5 ± 5.2 mL·kg−1·minute−1) at the evaluation of 31 patients with CMD.
Additionally, our results were consistent in showing a significant increase of physical capacity with training as documented by the 14% increase in peak-VO2 from the initial to the final test (from 19.4 ± 4.8 to 22.1 ± 6.2 mL·kg−1·minute−1; P = .01, CI −4.7 to −0.7). This increase in physical capacity is similar to the results obtained by other investigators in the same clinical context. Eriksson et al24 observed a statistically significant 15% increase in peak-VO2 during CPT (from 1.26 ± 0.14 to 1.45 ± 0.16 L·minute−1, P = .018) after an 8-week period of physical training in patients with CMD.
Results obtained with the application of the SF-36 questionnaire indicated that our patient sample had significant impairment of QOL in the baseline condition, preceding the physical training program. Of the eight domains evaluated, six showed scores below 50% and two did not exceed 55%. Other studies have also reported a similar degree of impairment of the QOL in patients with microvascular angina.6,8,12,25
In agreement with findings of previous studies, after the period of physical training we observed a marked increase in the scores for all domains of the SF-36. In particular, the domain related to pain showed a significant increase of 78% (P = .007 and CI −49.9 to −10) after the period of training, from 38% in the baseline condition to 68% after training. It is plausible to assume that at least part of the improvement in this domain was due to a reduction of the angina frequency since this was the main complaint of all patients.
Study Limitations
One major limitation of our study is the relatively small sample size. Even though a large number of patients presenting chest pain and normal coronary arteries were initially screened, only 30% of the initial population also had RPDs on the myocardial perfusion study. From our initial screening for the study, we also had to exclude patients with serologic evidence of Chagas disease,32 a condition that is commonly associated with microvascular dysfunction. Additionally, a considerable proportion of subjects (50%) dropped out from the study during the physical training phase due to non-adherence to attend the training session on a 3-time weekly base.
The lack of a similar control group, not undergoing physical training, is also a methodological limitation. In fact, a larger randomized controlled trial is warranted to fully assess the therapeutic impact of aerobic physical training in patients with microvascular angina.
New Knowledge Gained
The initial evidence raised by the results of this small pilot investigation suggests a therapeutic benefit of physical training in patients with primary microvascular angina, characterized by RPDs on MPS and angiographically normal coronary arteries. A larger randomized study testing this hypothesis is warranted.
Conclusions
In conclusion, the results of this pilot study show that a 4-month physical training program applied to patients with primary microvascular angina is associated with reduction of extent/severity of reversible perfusional abnormalities that was accompanied by significant improvement of functional capacity and of QOL, including improved pain scores.
References
Camici PG, Crea F. Coronary microvascular dysfunction. N Engl J Med 2007;356:830-40.
Cannon RO III. Microvascular angina and the continuing dilemma of chest pain with normal coronary angiograms. J Am Coll Cardiol 2009;54:877-85.
Beltrame JF, Crea F, Camici P. Advances in coronary microvascular dysfunction. Heart Lung Circ 2009;18:19-27.
Lanza GA, Crea F. Primary coronary microvascular dysfunction: Clinical presentation, pathophysiology, and management. Circulation 2010;121:2317-25.
Cannon RO III, Epstein SE. “Microvascular angina” as a cause of chest pain with angiographically normal coronary arteries. Am J Cardiol 1988;61:1338-43.
Gulati M, Cooper-DeHoff RM, McClure C, Johnson BD, Shaw LJ, Handberg EM, et al. Adverse cardiovascular outcomes in women with nonobstructive coronary artery disease: A report from the Women’s Ischemia Syndrome Evaluation Study and the St James Women Take Heart Project. Arch Intern Med 2009;169:843-50.
Jespersen L, Hvelplund A, Abildstrom SZ, Pedersen F, Galatius S, Madsen JK, et al. Stable angina pectoris with no obstructive coronary artery disease is associated with increased risks of major adverse cardiovascular events. Eur Heart J 2012;33:734-44.
Atienza F, Velasco JA, Brown S, Ridocci F, Kaski JC. Assessment of quality of life in patients with chest pain and normal coronary arteriogram (syndrome X) using a specific questionnaire. Clin Cardiol 1999;22:283-90.
Shaw LJ, Merz CNB, Pepine CJ, Reis SE, Bittner V, Kip KE, et al. The economic burden of angina in women with suspected ischemic heart disease: Results from the national institutes of health—National Heart, Lung, and Blood Institute—sponsored Women’s Ischemia Syndrome Evaluation. Circulation 2006;114:894-904.
Phan A, Shufelt C, Merz NB. Persistent chest pain and no obstructive coronary artery disease. J Am Med Assoc 2009;301:1468-74.
Kaski JC, Garcia LFV. Therapeutic option for the management of patients with cardiac syndrome X. Eur Heart J 2001;22:283-93.
Crea F, Lanza GA. Angina pectoris and normal coronary arteries: Cardiac syndrome X. Heart 2004;90:457-63.
Hambrecht R, Wolf AM, Giellen S, Linke A, Hofer J, Erbs S, et al. Effect of exercise on coronary endothelial function in patients with coronary artery disease. N Engl J Med 2000;342:454-60.
Buchthal SD, den Hollander JA, Merz CN, Rogers WJ, Pepine CJ, Reichek N, et al. Abnormal myocardial phosphorus-31 nuclear magnetic resonance spectroscopy in women with chest pain but normal coronary angiograms. N Engl J Med 2000;342:829-35.
Bairey Merz CN, Pepine CJ. Syndrome X and microvascular coronary dysfunction. Circulation 2011;124:1477-80.
Panting JR, Gatehouse PD, Yang GZ, et al. Abnormal subendocardial perfusion in cardiac syndrome X detected by cardiovascular magnetic resonance imaging. N Engl J Med 2002;346:1948-53.
Pennell DJ. Cardiovascular magnetic resonance: Twenty-first century solutions in cardiology. Clin Med 2003;3:273-8.
Saghari M, Assadi M, Eftekhari M, Yaghoubi M, Fard-Esfahani A, Malekzadeh JM, et al. Frequency and severity of myocardial perfusion abnormalities using Tc-99m MIBI SPECT in cardiac syndrome X. BMC Nucl Med 2006;6:1.
Kaski JC, Rosano GM, Collins P, Nihoyannopoulos P, Maseri A, Poole-Wilson PA. Cardiac syndrome X: Clinical characteristics and left ventricular function. Long-term follow-up study. J Am Coll Cardiol 1995;25:807-14.
Lanza GA, Buffon A, Sestito A, Natale L, Sgueglia GA, Galiuto L, et al. Relation between stress-induced myocardial perfusion defects on cardiovascular magnetic resonance and coronary microvascular dysfunction in patients with cardiac syndrome X. J Am Coll Cardiol 2008;51:466-72.
Legrand V, Hodgson JM, Bates ER, Aueron FM, Mancini GB, Smith JS, et al. Abnormal coronary flow reserve and abnormal radionuclide exercise test results in patients with normal coronary angiograms. J Am Coll Cardiol 1985;6:1245-53.
Vermeltfoort IAC, Raijmakers PGHM, Bondarenko O, van Rossum AC. Correlation of myocardial perfusion on cardiac magnetic resonance versus myocardial perfusion scintigraphy in cardiac syndrome X. Open Nucl Med J 2009;1:9-14.
Cavusoglu Y, Entok E, Timuralp B, Vardareli E, Kudaiberdieva G, Birdane A, et al. Regional distribution and extent of perfusion abnormalities, and the lung to heart uptake ratios during exercise thallium-201 SPECT imaging in patients with cardiac syndrome X. Can J Cardiol 2005;21:57-62.
Eriksson BE, Tyni-Lenne R, Svedenhag J, Hallin R, Jensen-Urstad K, Jensen-Urstad M, et al. Physical training in syndrome X: Physical training counteracts deconditioning and pain in syndrome X. J Am Coll Cardiol 2000;36:1619-25.
Tyni-Lenne R, Stryjan S, Eriksson B, Berglund M, Sylven C. Beneficial therapeutic effects of physical training and relaxation therapy in women with coronary syndrome X. Physiother Res Int 2002;7:35-43.
Giallauria F, Acampa W, Ricci F, Vitelli A, Torella G, Lucci R, et al. Effects of exercise training started within 2 weeks after acute myocardial infarction on myocardial perfusion and left ventricular function: A gated SPECT imaging study. Eur J Cardiovasc Prev Rehabil 2012;19:1410-9.
Heaps CL, Parker JL. Effects of exercise training on coronary collateralization and control of collateral resistance. J Appl Physiol 2011;111:587-98.
Belardinelli R, Paolini I, Cianci G, Piva R, Georgiou D, Purcaro A. Exercise training intervention after coronary angioplasty: The ETICA trial. J Am Coll Cardiol 2001;37:1891-900.
Gielen S, Schuler G, Hambrecht R. Exercise training in coronary artery disease and coronary vasomotion. Circulation 2001;103:E1-6.
Kendziorra K, Walther C, Foerster M, Mobius-Winkler S, Conradi K, Schuler G, et al. Changes in myocardial perfusion due to physical exercise in patients with stable coronary artery disease. Eur J Nucl Med Mol Imaging 2005;32:813-9.
Dominguez-Rodriguez A, Abreu-Gonzalez P, Avanzas P, Gomez MA, Padron AL, Kaski JC. Cardiopulmonary exercise testing for the assessment of exercise capacity in patients with cardiac syndrome X. Int J Cardiol 2012;154:85-7.
Hiss FC, Lascala TF, Maciel BC, Marin-Neto JA, Simões MV. Changes in myocardial perfusion correlate with deterioration of left ventricular systolic function in chronic chagas’ cardiomyopathy. J Am Coll Cardiol Imaging 2009;2:164-72.
Acknowledgments
This study was supported by a research grant from Fundação de Apoio à Pesquisa do Estado de São Paulo (FAPESP, No. 2008/04140-3).
Disclosure
The authors declare that there is no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Carvalho, E.E.V., Santi, G.L., Crescêncio, J.C. et al. Pilot study testing the effect of physical training over the myocardial perfusion and quality of life in patients with primary microvascular angina. J. Nucl. Cardiol. 22, 130–137 (2015). https://doi.org/10.1007/s12350-014-9949-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-014-9949-6