Abstract
Depressive disorder is a chronic, recurring, and potentially life-endangering neuropsychiatric disease. According to a report by the World Health Organization, the global population suffering from depression is experiencing a significant annual increase. Despite its prevalence and considerable impact on people, little is known about its pathogenesis. One major reason is the scarcity of reliable animal models due to the absence of consensus on the pathology and etiology of depression. Furthermore, the neural circuit mechanism of depression induced by various factors is particularly complex. Considering the variability in depressive behavior patterns and neurobiological mechanisms among different animal models of depression, a comparison between the neural circuits of depression induced by various factors is essential for its treatment. In this review, we mainly summarize the most widely used behavioral animal models and neural circuits under different triggers of depression, aiming to provide a theoretical basis for depression prevention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Overview of Depressive Disorder
Depressive disorder is one of the most common neuropsychiatric disorders across the world. It affects interpersonal relationships, social life, and one’s sense of self-worth, leading to severe dysfunction [1]. The American Psychiatric Association’s Diagnostic Statistical Manual of Mental Disorders, Fifth Edition classifies depressive disorders as the following: major depressive disorder (MDD), persistent depressive disorder, disruptive mood dysregulation disorder, premenstrual dysphoric disorder, and depressive disorder due to another medical condition. MDD is also referred to as depression [2]; its development may be influenced by genetic factors, situational stress, medical conditions, adverse emotional experiences, particularly those in childhood, and individual resilience. It is characterized by persistent sadness, loss of interest or pleasure, low energy, changes in food consumption, worse appetite and sleep, and even suicidal thoughts, disrupting daily activities and psychosocial functions. In 2010, MDD was the second most significant contributor to global disability, accounting for 8.2% of the global years lived with disability (YLD) [3]. In 2016, the Global Burden of Diseases, Injuries, and Risk Factors Study revealed that depression was responsible for 34.1 million YLDs, positioning it as the fifth leading cause of YLD [4]. Recently, WHO has predicted that depression will be the leading cause of disease burden worldwide by 2030 [3].
MDD exerts a severe social and economic burden globally. The annual economic cost of MDD in the United States alone is an astonishing $70 billion in medical expenses, lost productivity, and other costs [5]. Many researchers have conducted a series of animal experiments and clinical studies on the pathogenesis and effective therapies for depression. In the past decade, there has been a rise in the total count of research papers published globally on depression almost every year, as shown in Fig. 1A. Searching the SCI-Expanded Web of Science database [2], we found a total of 59,156 articles published in the depression field from 2013 to 2023 (search strategy: (TI = (depression$) or ts = (“major depressive disorder$”)) and py = (2013–2023)). Fig. 1B displays the list of the top 10 countries in publishing papers on depression. By 2021, the disparity in the total number of publications between China and the USA has been progressively decreasing. After 2022, the number of publications published by researchers in China has surpassed that of the USA (Fig. 1C). Keywords co-occurrence analysis was conducted based on literature sourced from the Web of Science database. This analysis was performed to reflect the distribution of hot topics within the field. As shown in Fig. 1D, the hot research topics in depression are as follows: general symptoms of depression, the risks of depression, the effects of depression, animal models of depression, associated brain regions and functional connections of depression, antidepressants, and depression therapy, comorbidity of depression and other diseases, epidemiology of depression, depression management in primary care, and categories of depression. Establishing appropriate animal models is a fundamental basis for deeply studying the mechanisms and other aspects of depression.
Analysis of published papers around the world from 2013 to 2023 on depressive disorder. A The total number of papers from a search of the SCI-Expanded Web of Science database (search strategy: (TI = (depression$) or ts = (“major depressive disorder$”)) and py = (2013–2023)]. B The top 10 countries publishing on the topic of depressive disorder. C Comparison of papers in China and the USA. D Hot topics on depressive disorder research and keyword co-occurrence analysis were conducted using VOSviewer software.
Diverse Animal Models of Depressive Disorder
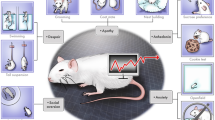
Stress is a well-known precursor to depression in individuals with genetic vulnerability [6, 7]. This established connection between stress and depression has prompted investigators to develop animal models of stress such as social defeat, unpredictable chronic stress, learned helplessness, maternal deprivation, immobilization, isolated stress, sleep deprivation, and forced swim [3, 8, 9]. Fig. 2 shows the current widely used animal model of depressive disorder. We have comprehensively compared the advantages and disadvantages of these depression models to assist researchers in selecting an appropriate animal model for depression studies (Table 1).
Animal models for the study of depressive disorder. A Chronic social defeat stress (CSDS). In this model, depression is induced over 10 days by directly exposing C57BL/6J mice to a larger and more aggressive CD-1 mouse for 5 min per day. B Chronic mild stress (CMS). In this model, the mice are exposed to a series of low-intensity stressors at unpredictable times for several weeks. C Learned helplessness (LH). The mouse is exposed to unpredictable and inescapable electric foot-shock resulting in a defect in its escape behavior and the manifestation of depressive symptoms. D Physical pain model. Transection of the sciatic nerve can result in persistent neuropathic pain, while exposure to stimuli such as a hot plate, electronic von Frey, and inflammatory agents can induce chronic nociceptive pain. These chronic pain conditions are associated with the development of depressive behaviors. E Other models. Surgical models, early-life stress, and transgenic techniques are utilized to study depression, such as 5-HTT-/- mice. Schematic figures are created with Biorender.com.
Chronic Social Defeat Stress (CSDS)
Given that social factors predominantly trigger stress-related neuropsychiatric disorders in humans [10], it's essential to study the effects of social stress using animal models. The CSDS paradigm has been widely used in rodent depression studies, as these animals exhibit some of the cardinal features of human depression like anhedonia, reduced social interaction, attenuated weight gain, increased submissive behavior, and anxiety [8, 11,12,13,14]. This paradigm repeatedly exposes animals to a stronger and more aggressive strain, such as CD-1, subjecting them to social defeat. Specifically, the defeated mice after CSDS are divided into susceptible and resilient subtypes, which model the varied human responses to stress [11]. Behavioral changes in defeated mice, such as depression, anxiety, and cognitive impairment, are observed [15].
Historically, Kudryavtseva first reported that subordinate C57BL/6J strain mice exhibited depression-like behavior after defeat in the sensory contact model [16]. Subsequently, researchers continuously standardized the CSDS model. Nestler and colleagues in 2006 reported a standard process for establishing the CSDS mouse model: male C57BL/6J mice are exposed to different CD1 aggressor mice for 10 min daily for 10 consecutive days. After defeat, the resident CD1 mice and defeated C57BL/6J mice are housed in one half of a cage separated by a perforated Plexiglas divider with holes to allow sensory contact for the remaining 24 h after each session. After the final defeat, mice are individually housed with unrestricted access to food and water [14]. In 2011, a standardized protocol was developed, considering various influential factors in the CSDS model, such as the validity of the model, experimenter experience, and differences in individual responses to stress [17].
The advantage of the CSDS model is that it simulates the mechanism of depression-like behavior at the social level and achieves higher structural validity. Unlike other stress models, social defeat represents a unique stressor in terms of the magnitude and quality of the stress response [18]. It more closely resembles human conditions compared to nonsocial stress models like repeated restraint stress [19]. Therefore, the CSDS paradigm is the most commonly used model for studying depression in rodents [20]. However, this model has two main limitations: its symptoms may overlap with those of anxiety, potentially misleading investigators; and it's applicable mostly to male rodents due to the absence of consistent and reliable aggression in female resident-intruder interactions [21].
Chronic Mild Stress (CMS) and Chronic Unpredictable Mild Stress (CUMS)
As is known, repeated presentation of the same stressor often results in adaptation and may decrease depressive and anxiety-like behaviors [22, 23], a process that can be circumvented by applying a range of stressors in an unpredictable order [1]. Besides, previous research has demonstrated that chronic, uncontrollable stress can impair the brain’s reward system [24]. Thus, the chronic stress animal model was developed to investigate neuropathology [25] and potential therapeutic targets [26, 27] of depressive disorder. The CMS paradigm uses long-term chronic low-level stimulation to continuously expose animals to a series of unpredictable mild stimuli (e.g., small temperature reductions, disruption in the dark–light cycle, changes of cage mates, or dampened bedding), as well as daily random deprivation of water or food for a period of 3 weeks to 3 months [28]. It aims to model the gradual development of a chronic depressive-like state in response to stress, as much as possible similar to the real circumstances of a patient's illness.
Historically, Katz and colleagues developed the first CMS paradigm [29], involving harsh stressors like electric shock, cold swimming, and heat stress [30, 31]. These stressors can cause an increase in plasma corticosterone levels and a reduction in sucrose preference [31, 32], indicating that chronic stress may induce anhedonia. However, this protocol has rarely been used due to serious ethical concerns and unrealistic induction conditions [30,31,32,33,34]. Then, Willner further developed the CMS paradigm [25, 35], focusing on simulating anhedonia by exposing animals to varied mild stressors, such as periods of food and water deprivation, temperature changes, and altering cage mates in an unpredictable manner [36, 37]. This approach more effectively mirrored human life stressors, with sucrose preference reduction reversible by various antidepressants (ADs), including tricyclic antidepressants, selective serotonin reuptake inhibitors, serotonin and norepinephrine reuptake inhibitors, monoamine oxidase inhibitors, and atypical ADs [38]. This protocol of CMS has since been extensively described and used [39].
The advantages of the CMS model are face validity and construct validity. This model results in enduring changes across behavioral, neurochemical, neuroimmune, and neuroendocrinological parameters, mirroring dysfunctions seen in depressed patients [25, 39, 40]. Therefore, it is considered one of the most extensively validated and realistic models of depression. However, establishing this paradigm in a new lab is challenging, and replicating data across labs is sometimes difficult, perhaps due to its time-consuming protocol, as well as mild and variable phenotypes [40]. Numerous high-frequency protocols also require extensive experimental space, which may also result in low efficiency.
Learned Helplessness (LH)
Helplessness, a core symptom of MDD, is extensively studied in both clinical and preclinical depression research. The LH paradigm, one of the earliest animal depression models [41], induces a depressive-like state through uncontrollable and unpredictable electrical foot-shock stress [42,43,44]. The classic experimental procedure is a triadic design with two control groups: the first control group experiences controllable shocks (like escaping, lever pressing, or wheel turning) [45, 46]. The second group, yoked to the first, receives the same shocks but as unpredictable and uncontrollable. The third group is an unstressed control group. This procedure allows comparison across groups, highlighting that the key factor in stress-induced deficits is the uncontrollability, not the stress itself [47].
Historically, LH was first reported in the 1960s by Richard L. Solomon, who was investigating the separability of classical Pavlovian conditioning and instrumental learning. He discovered that prolonged exposure to uncontrollable traumatic events led to unexpected behavioral changes. Overmier and Seligman later found that short, distributed exposure to uncontrollable trauma over several hours caused significant deficits in behavioral coping, associative learning, and emotional expression, a phenomenon they termed “learned helplessness” [48]. Helpless animals showed sustained changes such as weight loss, sleep pattern disruptions, altered hypothalamus-pituitary-adrenal (HPA) axis activity, and hippocampal spine synapse loss [49, 50]. These behaviors are consistent with those clinically observed in human patients.
The advantage of the LH model is that its symptoms closely resemble those of major depression, most of which are reversible by several acute antidepressant treatments (typically for 3-5 days) [51]. It has a good face, construct, and predictive validity, and the model has been instrumental in confirming various pathophysiological theories of depression [52, 53]. A major limitation, however, is the short-lived nature of depression-like symptoms after exposure to uncontrollable shocks [54]. Besides, susceptibility to LH varies among different strains: the Kyoto and Charles River Holtzmann lines are the most susceptible, and Harlan Sprague–Dawley exhibit moderate susceptibility, while Lewis, Brown Norway, Fischer F-344, and Sasco Holtzman show almost no susceptibility to the effects of inescapable shock [55].
Physical Pain Model
Physical pain, particularly neuropathic and nociceptive types, is another major contributor to depression [56, 57]. According to the literature, pain resulting from sensory nerve damage can impact depressive moods and lead to neuronal death in brain regions associated with depression, such as the insular lobe, prefrontal cortex, thalamus, hippocampus (HPC), anterior cingulate, and amygdala [58]. Furthermore, chronic pain and depression frequently co-occur [59]. The mechanisms underlying the connection between pain and depression are complex [60, 61].
Physical pain is classified into neuropathic, nociceptive, postoperative, and cancer pain, among others, organized by type of pain. Neuropathic pain specifically arises from a lesion or disease within the somatosensory system itself [62] and occurs due to injuries or chemical exposure. Neuropathic pain models involve surgical transection of specific nerves, like the sciatic nerve [63,64,65] or spinal nerves [66, 67], while preserving surrounding tissue for histologic examination. In addition, inflammation secondary to a crushing injury can also cause neuropathic pain, as reported in models like spinal nerve ligation at L5-L6 [66, 68], partial saphenous nerve ligation [69], and full or partial sciatic nerve ligation [70,71,72,73]. Nerve ligation models effectively replicate aspects of human neuropathic conditions, such as sciatica and other constrictive nerve injuries.
Nociceptive pain activates pain receptors that detect stimuli and transmit signals to the central nervous system for recognizing and reacting to injury or potential harm [74]. Nociceptive pain models are based on spinal reflexes with assessments including tail flick, paw withdrawal, paw lifting, flinching, guarding, and licking [75]. The types of nociceptive stimuli can be categorized into thermal (hot plate or radiant heat for paw/tail stimuli), mechanical (von Frey filaments and Randall-Selitto paw pressure tests for pressure application), and chemical stimulation (injecting irritants like formalin, capsaicin, or acetic acid). Inflammatory models [75, 76], such as carrageenan-induced edema in rat hind paws [77] or Complete Freund’s adjuvant for inflammation [78], are also used. These models help study the perception and sensitivity of the organism to pain stimuli, evaluate the efficacy of analgesics in nociceptive pain, and explore potential therapeutic targets for pain relief.
Postoperative nociceptive pain can lead to persistent nociplastic pain states after surgery, causing depression and increased suffering in patients. To model this, animals undergo similar surgical procedures, such as the plantar incision model [79,80,81], which involves a hind paw skin incision and can include deeper tissue manipulation by retracting, stretching, or incising the plantaris muscle in the arch of the paw. For cancer pain, the degree of pain is tied to the tumor microenvironment. Bone and pancreatic cancers are very painful, while others like lipomas and melanomas may not cause pain. In rodents, osteolytic bone cancer pain can be modeled by injecting osteolytic fibrosarcoma cells into the femur [82, 83], humerus, calcaneus [84], or tibia [85]. In addition, a transgenic mouse spontaneously expressing exocrine pancreatic tumors is used to model pancreatic cancer [86].
Other Models
In addition to the above models, in the recent decade, several modeling methods like surgical models, early-life stress models, and mutant approaches have been proposed. Bilateral olfactory bulbectomy (OBX), has been employed as a surgical model of depression, affecting endocrine, immune, and neurotransmitter systems [87]. In rodents, the olfactory system, a part of the limbic region involving the amygdala and HPC, influences behavior and emotions. Post-OBX, rodents exhibit hyperactivity, social behavior changes, increased nocturnal activity, learning and memory deficits, and altered taste-aversion [88]. These changes are thought to stem from dysfunctions or compensatory actions in the cortical → hippocampal → amygdala circuits, similar to areas affected in major depression [89]. Chronic antidepressant treatment has been shown to address many of the changes induced by OBX [88]. While OBX has a face and predictive validity, it lacks etiological and construct validity.
Numerous experimental methods have been established to induce early-life stress in rodents during crucial developmental stages [90, 91]. Maternal separation serves as a significant model for studying the pathophysiology and treatment of major depression. For instance, the administration of ADs in adult male rats undergoing maternal separation can normalize their anxiety-like behavior, endocrine stress response, and ethanol preference [92]. A recent development is the chronic early-life stress model, which has both immediate and lasting impacts on the HPA system and cognitive functions. This model involves disrupting normal interactions between a mother and her offspring, leading to impaired hippocampal learning and memory functions and decreased survival of adult neurons [93, 94].
The advancement of genetic techniques has rendered mutant models highly effective for identifying potential targets of depression. In the last few years, various mouse lines have been created to investigate depression-related genes, implicated in depression, aligned with theories on monoamines, neurotrophins, and the HPA axis [95,96,97]. For instance, mice lacking the 5-HT transporter (5-HTT-/-) display anxiolytic and antidepressant-like responses in behavioral tests like the elevated plus maze, tail suspension test, and forced swim test [98,99,100].
Although numerous animal models of depression, each with its own predictive, face, and construct validity, have significantly enhanced our understanding of the neurobiology of depression, they come with several limitations. Importantly, the exploration of specific neural circuits involved in depression represents a new frontier in advancing the treatment of this complex disorder.
Neural Circuits of Depressive Disorder
Several brain regions and circuits, notably within the interconnected limbic system, play key roles in regulating emotion, reward, and executive function. Dysfunctions in these regions are linked to depression and anti-depressant action. Classically, the ventral tegmental area (VTA) is central to reward processing, the nucleus accumbens (NAc) to hedonic and motivational deficits associated with depression, the amygdala to fear, and the HPC to cognitive impairments. The lateral habenula (LHb) is thought to influence anhedonia [101]. Here we primarily review a brain network (Fig. 3) to elucidate how specific circuits regulate depressive behavior.
Schematic of the major neural circuit connections involved in regulating depression-related behaviors. The figure shows only a subset of the many known interconnections among various brain regions. The symbols on the connecting lines signify the categories of animal models used for exploring this pathway. A Reward circuits. B Chronic pain circuits. C Memory circuits. PFC, prefrontal cortex; NAc, nucleus accumbens; LS, lateral septum; HPC, hippocampus; LHb, lateral habenula; VTA, ventral tegmental area; PVT, paraventricular thalamus; PAG, periaqueductal gray; SI, substantia innominata; AHN, anterior hypothalamic nucleus; LH, lateral hypothalamus; DRN, dorsal raphe nucleus; LPBN, lateral parabrachial nucleus; BLA, basolateral amygdala; CeA, central amygdala; Sp5C, spinal trigeminal subnucleus caudalis. Schematic figures are created with Biorender.com.
Depression and Reward
The complexity of the reward function is due to the involvement of a common circuit linking the dopaminergic midbrain, basal ganglia, and frontal cortex in many reward processes [102]. There is growing evidence of the brain’s reward circuitry playing a crucial role in the development and symptoms of depression [103]. The concept that midbrain dopamine (DA) systems influence depression-like behaviors emerged from studies using DA receptor antagonists [104]. Stress, particularly in animal models of depression, activates VTA DA neurons, enhancing dopaminergic transmission to limbic targets like the NAc. Antidepressants alter this dopaminergic activity, and experimental manipulation in the VTA → NAc dopaminergic pathway affects depression-like behaviors in rodents under acute stress. Specifically, optogenetic activation of VTA DA neurons during CSDS exacerbates depressive phenotypes [105], while optogenetic inhibition of VTA-NAc DA neurons alleviates the anhedonia induced by CSDS [106].
The ventral striatum (vSTR) is crucial in initiating reward-related behaviors and managing social stress [107, 108]. Previous research has shown that intralaminar thalamus (ILT) and PFC projections to the vSTR regulate reward behaviors [109, 110], but the specific inputs responsible for mediating chronic stress effects remain uncertain. Christoffel et al. [111] explicitly illuminated the vSTR's unique role in stress-related synaptic remodeling and behavior. This underscores how synaptic alterations in the vSTR, particularly at ILT glutamatergic inputs to vSTR medium spiny neurons, are key in stress susceptibility following CSDS. The NAc, as a region of the vSTR, is pivotal in processing rewarding stimuli. Lind et al. [112] investigated NAc shell input-specific reward behaviors, using spatially dependent optogenetic self-stimulation tasks to assess mouse responses. They confirmed distinct roles for various pathways to the NAc shell: the medial prefrontal cortex (mPFC) → NAc shell pathway in facilitating place preference, the vHPC → NAc shell pathway in consistently promoting place preference, the basolateral amygdala (BLA) → NAc shell pathway in generating modest place preference linked to time sensitivity, and the paraventricular thalamus (PVT) → NAc shell pathway in reducing but not fully negating, place preference. Besides, Vollmer et al. [113] explored the role of PVT → NAc in reward seeking. Their work revealed this pathway is crucial in suppressing sucrose self-administration through NAc parvalbumin (PV) interneurons and Ca2+-permeable AMPA receptor-rich synapses, with opioid intervention quickly changing this behavior.
The ventral HPC (vHPC) is recognized for encoding reward-predictive stimuli and influencing reward-oriented behaviors [114,115,116,117,118]. Hippocampal synapses on the NAc exhibit high plasticity, with brief, high-frequency activity inducing long-term potentiation (LTP) and sustained reward responses. Chronic stress has been shown to cause anhedonia, weaken these synaptic connections, and impair LTP, effects that can be reversed by antidepressants [115]. Chronic stress also leads to dendritic spine atrophy in hippocampal CA1 and CA3 pyramidal cells, as well as a reduction in neurogenesis [119]. Conversely, enhanced neurogenesis in the hippocampus of a transgenic mouse can reduce anxiety and depression-like behaviors [120]. In addition, cocaine exposure has been linked to strengthened HPC–NAc connections [121]. Bagot et al. [122] utilized optogenetic techniques to manipulate specific synaptic functions and discovered that glutamatergic vHPC projections to the NAc modulate the behavioral effects of CSDS.
The LHb, a brain region involved in depression, plays a key role in processing both reward and punishment [123,124,125,126]. Activation of LHb neurons has been recorded in response to nonrewarding or unpleasant events. Notably, acute stress alters LHb's response, turning reward signals into ones resembling punishment, which is linked to depression [127]. Research has highlighted that attenuating LHb hyperactivity can effectively lessen depressive symptoms. Inputs from the basal forebrain (BF), particularly the substantia innominata (SI), a BF subregion, are instrumental in relaying punishment and reward signals to the LHb [128, 129]. Previous research has shown that selective activation of glutamatergic SI neurons results in real-time conditioned place aversion, while activation of its GABAergic neurons leads to conditioned place preference (CPP) [130]. Cui et al. [131] demonstrated that chronic activation of the SI → LHb circuit induces depressive-like behaviors, whereas its inhibition alleviates stress-induced depressive-like behaviors. In addition, reward consumption can buffer depressive-like behaviors. A study on depression models discovered that glutamatergic LHb neurons that project to the VTA receive increased dopaminergic inputs, potentially causing aversion and affecting cognitive functions in major depression [124]. Clinical evidence has also shown that deep brain stimulation inactivates the habenula, leading to complete remission of treatment-resistant major depression in patients [132].
The lateral septum (LS), a forebrain structure, participates in various behavioral responses to stress and also plays a crucial role in reward processes by eliciting intrinsic rewarding properties [133, 134]. This insight originates from pioneering self-stimulation studies [135, 136]. A recent study has revealed that the CA3 → LS → VTA pathway mediates cocaine-seeking behaviors [137]. Chemogenetic inhibition of the dorsal CA3 → LS pathway has been found to reduce cocaine-seeking behavior [138]. Further research indicates that the LS, particularly its rostral part, activates lateral hypothalamic orexin neurons during cocaine CPP. This activation is essential for the expression of cocaine preference [139]. In addition, LS neurons expressing neurotensin (NTLS) and somatostatin (SstLS) are hyperactivated under stress in mice. Our group investigated NTLS neurons, uncovering that social reward functions are impaired in the CSDS depression model [140]. Our work employed a range of methods, including in vivo imaging and chemogenetics manipulations, demonstrating the necessity and sufficiency of activating the NTLS → anterior hypothalamic nucleus and NTLS → NAc circuits in altering social investigation and preference behaviors post-social trauma. An et al. [134] focused on Sstdorsal LS neurons, finding that they are responsive to various stressors, and their activity is influenced by norepinephrine of the locus coeruleus (LC). The LS consists primarily of GABAergic neurons. The GABAergic LS neurons’ projections to the dorsal periaqueductal gray (dPAG) are associated with depression-related behaviors in the chronic unpredictable stress model. Activation of the LS → dPAG circuit reduces sucrose preference in mice, whereas its suppression induces an antidepressant effect [141]. The latest research on LS has pinpointed a subset of GABAergic adenosine A2A receptor-positive LS neurons that contribute to depressive symptoms. These neurons exert their influence through direct connections to both the LHb and dorsomedial hypothalamus [142].
Depression and Chronic Pain
Chronic pain and depressive symptoms, often encountered clinically [143, 144], have been found to mutually exacerbate each other [145, 146]. Shared brain regions in these conditions include the amygdala and the dorsal raphe nucleus (DRN). Zhou et al. [147] elucidated a neural circuit for comorbid depressive symptoms in chronic pain. The 5-HT-expressing neurons in the DRN (5-HTDRN) project to somatostatin (SOM) expressing neurons in the central amygdala (CeA, referred to as the ‘nociceptive amygdala’), and the LHb is the output of the 5-HTDRN → SOMCeA circuit. As for this circuit function, they demonstrated that inhibiting the 5-HTDRN → SOMCeA → LHb pathway produces depression-like behavior, whereas its activation alleviates pain and depression-like symptoms. In addition, Zhang et al. [148] reported a neural network linking the spinal trigeminal subnucleus caudalis (Sp5C) to the lateral parabrachial nucleus (LPBN) and the VTA DA neurons, linked to depression in chronic neuropathic pain. They discovered that glutamatergic projections from the Sp5C innervate the glutamatergic neurons in the LPBN, which project to the VTA and modulate the activity of the VTA DA neurons. Upon activating the Sp5C → LPBN → VTA circuit, there is an increase in the firing activity of the VTA DA neurons. Conversely, inhibiting this elevated activity in the VTA DA neurons effectively reverses depressive behaviors, thus “uncoupling” chronic pain from comorbid depression.
The mPFC, critical in the affective processing of pain, undergoes plasticity during chronic pain progression. Several studies have demonstrated decreased activity in layer V pyramidal neurons (PNs) of the prelimbic (PL) mPFC in rodent models of chronic pain. Optogenetic activation of these neurons can alleviate symptoms of sensory and chronic pain [149, 150]. Recently, Huang et al. [151] established the significance of the BLA → mPFC → PAG → spinal cord pathway in the development of mechanical and thermal hypersensitivity following peripheral nerve injury. This pathway influences pain behaviors by reducing the noradrenergic and serotoninergic modulation of spinal signals. Subsequently, they further combined optogenetics with behavioral analysis in neuropathic pain models, focusing on the modulation of pain responses by DA projections from the VTA to the mPFC [152]. Moreover, DA was found to augment the activity of neurons projecting from the mPFC layer V PNs to the ventrolateral PAG, resulting in analgesia. At the functional level, fMRI studies in chronic pain patients have identified both hyper- and hypoactivity in the mPFC [153, 154], possibly due to different plasticity across distinct mPFC subregions and cells.
The amygdaloid complex consists of two divisions that are particularly relevant to pain: the BLA and the CeA. The BLA plays a well-established role in integrating polymodal sensory information, and by transmitting this information to the CeA, facilitates injury or pain avoidance, which are subsequently executed by brainstem centers. Apart from the CeA, the mPFC serves as another important output target of the BLA for regulating pain perception [155]. Previous seminal work from Ji et al. [156] has shown that chronic pain states result in BLA neuronal hyperactivity, causing mPFC deactivation and associated cognitive deficits. This occurs through feed-forward inhibition facilitated by PV-type GABAergic neurons in the PL cortex, activated by BLA inputs [150]. Ji and colleagues also found that metabotropic glutamate receptors 1 (mGluR1) and 5 (mGluR5) in the PFC play a significant role in regulating the inhibitory effect of BLA input. Specifically, mGluR1 receptors inhibit feedforward inhibition by dampening the excitability of PNs in the PFC, while the mGluR5 receptors increase PFC activity by enhancing endogenous cannabinoid release [157, 158]. A recent study has suggested that the CeA can bidirectionally modulate nociception [159], with neurons expressing protein kinase C-delta enhancing pain-related responses, and neurons expressing somatostatin (CeA-SOM) can drive antinociception. This dual and opposing function of the CeA arises from changes in GABAergic neuron excitability, driven by PBN excitatory inputs. The CeA also influences the interplay of chronic pain and anxiety. Zussy et al. [160] demonstrated that mGlu4 activation in the CeA not only abolishes inflammatory mechanical allodynia but also reduces anxiety and depression-like symptoms, reflecting the multifaceted role of the CeA in pain and emotion regulation.
Amygdala activity has been suggested to contribute to inflammatory processes [161]. Zheng et al. [162] reported in an LPS-induced neuroinflammation mouse model that microglial activation and pro-inflammatory cytokine production in the lateral amygdala, along with an increase in presynaptic glutamate release, leads to an excitatory/inhibitory imbalance. Mice exhibit anxiety and depression-like behavior. Interestingly, the anti-inflammatory factor IL-10 can mitigate these effects by normalizing gamma-aminobutyric acid (GABA) transmission in the amygdala, reducing anxiety-like behaviors and substance dependence [163]. Similarly, in adult male Sprague-Dawley rats, social defeat experiences enhance microglial activation and neuronal firing in the BLA, contributing to anxiety-like behaviors. Blocking microglial activation in these instances prevents such behaviors [164], suggesting a reciprocal relationship between amygdala activity and inflammation, and their joint contribution to anxiety.
The HPC is one of the brain regions involved in the regulation of pain signals, being active during the processing of pain and the modification of nociceptive stimuli. Numerous animal studies have linked elevated pro-inflammatory factors in the HPC to stress-induced anxiety and depressive-like behaviors [165]. For instance, acute stress significantly increases TNF-α production by the hippocampal microglia in mice [166]. Cytokines like IL-1β and TNF-α can suppress neurogenesis in the dentate gyrus (DG) [167], leading to neuronal apoptosis [168] and heightened anxiety-related behavior [169]. Oral administration of minocycline, a microglia inhibitor, alleviates hyperanxiety in mice [170]. In terms of neural circuits, recent research has revealed that the vCA1 → BLA and vCA1 → infralimbic cortex (IL) pathways play distinct roles in chronic inflammatory pain at different stages [171]. The vCA1 → BLA pathway appears to be associated with early-stage pain perception, whereas the vCA1 → IL pathway may be involved in pain recovery during the more complex stages.
Depression and Memory Deficit
Memory, a fundamental aspect of human and social behavior, encompasses the processes of encoding, storing, and retrieving social cues [172]. This complex function allows individuals to accurately recall past social interactions, facilitating appropriate social responses, and continuous memory updating with each new encounter. However, impairments in cognitive and memory functions can disrupt a person’s ability to regulate emotions [173, 174]. In particular, brain regions like the left dorsolateral PFC, the dorsomedial PFC, and the anterior cingulate cortex, critical for cognitive control, are also implicated in the abnormal utilization of emotion regulation strategies [175]. This includes a tendency towards the prolonged use of maladaptive strategies and challenges in the effective implementation of adaptive strategies [176]. Such memory deficits are common symptoms in patients with depression, including verbal delayed memory, visuospatial memory, verbal working and long-term memory, and working memory [177,178,179,180]. They can lead to increased suicidal tendencies, presenting serious clinical and social impacts [181, 182]. The awareness level of memory deficits is an important criterion for measuring the severity of depression [183].
A prevailing theory suggests that dopaminergic signaling plays a role in the development of memory deficits in depression. In animal models, depressive-like states are associated with alterations in dopaminergic neurotransmission, including changes in dopamine levels, tyrosine hydroxylase activity, and dopamine receptor expression [184]. Rats subjected to chronic restraint stress [185] or unpredictable CMS [186, 187] exhibit reduced dopamine levels in the PFC and HPC, which are accompanied by memory impairments. These changes can be reversed by Shen Yuan Gan and taurine [186, 187]. Temporal object memory deficits, found in the maternal separation model, can be restored by administering a D1 agonist [188]. Furthermore, patients with depression also exhibit impairments in positive memory. The release of dopamine in the HPC is essential for memory consolidation [189, 190]. Taken together, memory deficits in depressed patients may occur through the impact on HPC and dopaminergic midbrain regulation of memory consolidation [191].
The HPC is involved in managing various cognitive and mnemonic impairments induced by stress [192, 193]. It has been demonstrated that stress can inhibit hippocampal neurogenesis [194, 195]. In patients with depression, both a reduction in hippocampal neurogenesis and a decrease in hippocampal volume have been reported [196]. Various antidepressant treatments have been shown to stimulate neurogenesis in adult HPC [197]. Adult rats exposed to prenatal restraint stress exhibit a reduction in glutamate release in the vHPC, resulting in impaired social memory and depressive-like behaviors. These effects can be reversed with treatments such as agomelatine or fluoxetine [198]. In addition, dCA2 silencing impairs social memory [199]. Methods used to inactivate the dCA2 region, such as excitotoxic lesions and tetanus neurotoxin expression, result in its permanent silencing [200, 201]. This irreversible action might lead to lasting reactive changes in brain areas beyond dCA2, potentially contributing to socio-cognitive deficits. Phillips et al. [202] have confirmed that prolonged activation of mPFC-projecting vHPC neurons impairs social memory. Conversely, their sustained inhibition can rescue social memory deficits in autism spectrum disorder Rett syndrome mice, underscoring the necessity of balanced vHPC → mPFC signaling for social memory recall. Furthermore, the vHPC, receiving inputs from the medial EC, is vital for consolidating memories linked to anxiety and emotional behavior [203, 204]. Zhu et al. [204] implicated vHPC glutamatergic neurons in contextual fear memory consolidation.
The BLA is widely recognized for its critical function in handling emotions and motivation, significantly contributing to positive and negative emotion-related events [205, 206]. Importantly, the BLA is intricately connected with the HPC [207]. Emotional arousal activating the BLA impacts memory-related functions in the HPC. Studied have demonstrated that the BLA regulates LTP in the HPC DG [208], whereas BLA lesions inhibit the effect of glucocorticoid on modulating spatial memory in the dHPC [209]. Yang et al. [210] highlighted the importance of the BLA → HPC circuit in linking emotional states to spatial memory. Their finding indicated that LH attenuates the activity of the posterior BLA (pBLA) → vCA1 circuit, leading to memory deficits. In contrast, learned hopefulness strengthens this connection, thereby improving spatial memory. Stimulating this circuit effectively reverses the memory deficits induced by LH, enhancing synaptic transmission and dendritic plasticity in the CA1 region. This enhancement is facilitated by increased cAMP-response-element-binding protein (CREB) expression and a rise in intrasynaptic AMPA receptors. Pi et al. [211] employed the Barnes maze (BM) to demonstrate that anxiety status is associated with spatial memory deficits in mice with neuropsychiatric or neurodegenerative disorders, such as Alzheimer’s disease. Stimulating the glutamatergic inputs from pBLA to vCA1 reduces anxiety behaviors and spatial memory impairments, dependent on calbindin1 (Calb1) in the vCA1. Recently, another study has shown that optogenetically reactivating DG engram cells formed after a natural rewarding experience can acutely reduce depression-related behaviors. This effect is mediated by glutamatergic transmission from the amygdala’s axonal terminals to the NAc shell, essential for the real-time antidepressant effects of these reactivated DG engram cells [193].
The role of the mPFC in emotional behavior regulation is well-characterized, both negative and positive [212,213,214]. The IL PFC is essential for the extinction of memory. Chemogenetic inhibition of the IL →BLA pathway impairs the formation of extinction memory [215]. Yu et al. [216] developed a new go/go task to test the memory responses to ambiguous cues in mice. This work revealed that activation of pBLA Calb1–positive neurons is involved in the generalization of reward memory. Functionally, stimulating the IL to the pBLA projection significantly enhances the reward memory generalization and inhibits anxiety and depressive behaviors in mice subjected to unpredictable CMS stress. Studies have shown that silencing the mPFC neurons prevents the antidepressant effects of ketamine, whereas activation of CaMKII2α-expressing PNs in the mPFC can mimic these effects [217]. Hare et al. [218] demonstrated that the response to ketamine requires Drd1-expressing PNs in the mPFC, and stimulating mPFC Drd1 projections to the BLA can induce antidepressant effects. In preclinical studies of depression, working memory impairment is associated with decreased activity in Drd1-expressing PNs in the mPFC [219].
Studies indicate that mice exposed to social stress exhibit impaired memory and alterations in certain biochemical indicators. Specifically, Patki et al. used a modified resident-intruder model to induce social defeat stress, finding alterations in BDNF, ERK1/2, IL-6, glyoxalase-1, glutathione reductase-1, Ca2+/calmodulin-dependent protein kinase type-IV, and CREB levels in the HPC. These alterations lead to oxidative stress-induced anxiety, depression-like behaviors, and memory deficits [220]. Liu et al. [221] demonstrated that unpredictable CMS impairs spatial memory and decreases dendritic spine density, which can be prevented with paeoniflorin—an antidepressant-like herbal medicine. Maternal separation models impair spatial memory and reduce BDNF levels [222,223,224]. Similar results have been reported in other depression models, including restraint stress [225], chronic immobilization stress [226], LH [227], OBX [228, 229], corticosterone administration [230], LPS injections [231], and a post-stroke depression model [232].
Conclusion and Future Perspectives
In a retrospective review of previous research, we have identified the advantages and differences among various models commonly used in depression studies. In addition, we have summarized the neural circuits associated with depression. These models provide us with a platform to investigate depressive-like behaviors and physiological changes, and the study of neural circuits helps reveal the neurobiological basis of depression. However, there are still many limitations; for example, current models fail to mimic the relapsing-remitting pattern typical of depression, and there is a notable lack of models focusing on female animals. On the other hand, the development of these animal models for depression is predominantly driven by the needs and objectives of the pharmaceutical industry. Therefore, this expects researchers to undertake more profound and comprehensive research.
In the future, research will need to focus on more refined animal models and the intricacies of the nervous system and more decision-making-based models to identify other features of depression. Gaining a thorough understanding of the behaviors and behavioral characteristics exhibited by mouse depression models, along with advanced neural imaging and modulating techniques like genetically engineered sensor imaging, optogenetics, and deep brain stimulus, will help reveal subtle changes in neural circuits. Research on individual differences will also be a key focus, specifically exploring variations at the neural circuit level among different rodent individuals to better replicate the diversity observed in human depression. Collectively, the development of new strategies and advanced technologies, and the continual demand in neuroscience research for novel tools, will ultimately promote rapid and significant advancements in this field.
References
Song J, Kim YK. Animal models for the study of depressive disorder. CNS Neurosci Ther 2021, 27: 633–642.
Li Z, Ruan M, Chen J, Fang Y. Major depressive disorder: Advances in neuroscience research and translational applications. Neurosci Bull 2021, 37: 863–880.
Czéh B, Fuchs E, Wiborg O, Simon M. Animal models of major depression and their clinical implications. Prog Neuropsychopharmacol Biol Psychiatry 2016, 64: 293–310.
GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390: 1211–1259.
Disner SG, Beevers CG, Haigh EAP, Beck AT. Neural mechanisms of the cognitive model of depression. Nat Rev Neurosci 2011, 12: 467–477.
Kendler KS, Gatz M, Gardner CO, Pedersen NL. A Swedish national twin study of lifetime major depression. Am J Psychiatry 2006, 163: 109–114.
Holsboer F. The corticosteroid receptor hypothesis of depression. Neuropsychopharmacology 2000, 23: 477–501.
Krishnan V, Nestler EJ. The molecular neurobiology of depression. Nature 2008, 455: 894–902.
Wu A, Zhang J. Neuroinflammation, memory, and depression: New approaches to hippocampal neurogenesis. J Neuroinflammation 2023, 20: 283.
Schneiderman N, Ironson G, Siegel SD. Stress and health: Psychological, behavioral, and biological determinants. Annu Rev Clin Psychol 2005, 1: 607–628.
Krishnan V, Han MH, Graham DL, Berton O, Renthal W, Russo SJ. Molecular adaptations underlying susceptibility and resistance to social defeat in brain reward regions. Cell 2007, 131: 391–404.
Shimamoto A, Holly EN, Boyson CO, DeBold JF, Miczek KA. Individual differences in anhedonic and accumbal dopamine responses to chronic social stress and their link to cocaine self-administration in female rats. Psychopharmacology 2015, 232: 825–834.
Fox ME, Lobo MK. The molecular and cellular mechanisms of depression: A focus on reward circuitry. Mol Psychiatry 2019, 24: 1798–1815.
Berton O, McClung CA, Dileone RJ, Krishnan V, Renthal W, Russo SJ, et al. Essential role of BDNF in the mesolimbic dopamine pathway in social defeat stress. Science 2006, 311: 864–868.
Wang W, Liu W, Duan D, Bai H, Wang Z, Xing Y. Chronic social defeat stress mouse model: Current view on its behavioral deficits and modifications. Behav Neurosci 2021, 135: 326–335.
Kudryavtseva NN, Bakshtanovskaya IV, Koryakina LA. Social model of depression in mice of C57BL/6J strain. Pharmacol Biochem Behav 1991, 38: 315–320.
Golden SA, Covington HE 3rd, Berton O, Russo SJ. A standardized protocol for repeated social defeat stress in mice. Nat Protoc 2011, 6: 1183–1191.
Koolhaas JM, De Boer SF, De Rutter AJ, Meerlo P, Sgoifo A. Social stress in rats and mice. Acta Physiol Scand Suppl 1997, 640: 69–72.
Slattery DA, Cryan JF. The ups and Downs of modelling mood disorders in rodents. ILAR J 2014, 55: 297–309.
Bordes J, Miranda L, Reinhardt M, Narayan S, Hartmann J, Newman EL, et al. Automatically annotated motion tracking identifies a distinct social behavioral profile following chronic social defeat stress. Nat Commun 2023, 14: 4319.
Björkqvist K. Social defeat as a stressor in humans. Physiol Behav 2001, 73: 435–442.
Parihar VK, Hattiangady B, Kuruba R, Shuai B, Shetty AK. Predictable chronic mild stress improves mood, hippocampal neurogenesis and memory. Mol Psychiatry 2011, 16: 171–183.
Deng JH, Yan W, Han Y, Chen C, Meng SQ, Sun CY, et al. Predictable chronic mild stress during adolescence promotes fear memory extinction in adulthood. Sci Rep 2017, 7: 7857.
Guitart-Masip M, Walsh A, Dayan P, Olsson A. Anxiety associated with perceived uncontrollable stress enhances expectations of environmental volatility and impairs reward learning. Sci Rep 2023, 13: 18451.
Willner P. Validity, reliability and utility of the chronic mild stress model of depression: A 10-year review and evaluation. Psychopharmacology 1997, 134: 319–329.
Xu YH, Yu M, Wei H, Yao S, Chen SY, Zhu XL, et al. Fibroblast growth factor 22 is a novel modulator of depression through interleukin-1β. CNS Neurosci Ther 2017, 23: 907–916.
Zhang J, Zhou H, Yang J, Jia J, Niu L, Sun Z, et al. Low-intensity pulsed ultrasound ameliorates depression-like behaviors in a rat model of chronic unpredictable stress. CNS Neurosci Ther 2021, 27: 233–243.
Antoniuk S, Bijata M, Ponimaskin E, Wlodarczyk J. Chronic unpredictable mild stress for modeling depression in rodents: Meta-analysis of model reliability. Neurosci Biobehav Rev 2019, 99: 101–116.
Katz RJ, Hersh S. Amitriptyline and scopolamine in an animal model of depression. Neurosci Biobehav Rev 1981, 5: 265–271.
Katz RJ, Roth KA, Carroll BJ. Acute and chronic stress effects on open field activity in the rat: Implications for a model of depression. Neurosci Biobehav Rev 1981, 5: 247–251.
Katz RJ, Roth KA, Schmaltz K. Amphetamine and tranylcypromine in an animal model of depression: Pharmacological specificity of the reversal effect. Neurosci Biobehav Rev 1981, 5: 259–264.
Katz RJ. Animal model of depression: Pharmacological sensitivity of a hedonic deficit. Pharmacol Biochem Behav 1982, 16: 965–968.
Katz RJ, Baldrighi G. A further parametric study of imipramine in an animal model of depression. Pharmacol Biochem Behav 1982, 16: 969–972.
Katz RJ. Animal model of depression: Effects of electroconvulsive shock therapy. Neurosci Biobehav Rev 1981, 5: 273–277.
Willner P, Towell A, Sampson D, Sophokleous S, Muscat R. Reduction of sucrose preference by chronic unpredictable mild stress, and its restoration by a tricyclic antidepressant. Psychopharmacology 1987, 93: 358–364.
Willner P, Muscat R, Papp M. Chronic mild stress-induced anhedonia: A realistic animal model of depression. Neurosci Biobehav Rev 1992, 16: 525–534.
Monleon S, D’Aquila P, Parra A, Simon VM, Brain PF, Willner P. Attenuation of sucrose consumption in mice by chronic mild stress and its restoration by imipramine. Psychopharmacology 1995, 117: 453–457.
Mitchell PJ, Redfern PH. Animal models of depressive illness: The importance of chronic drug treatment. Curr Pharm Des 2005, 11: 171–203.
Wiborg O. Chronic mild stress for modeling anhedonia. Cell Tissue Res 2013, 354: 155–169.
Willner P. Chronic mild stress (CMS) revisited: Consistency and behavioural-neurobiological concordance in the effects of CMS. Neuropsychobiology 2005, 52: 90–110.
Seligman ME, Maier SF, Geer JH. Alleviation of learned helplessness in the dog. J Abnorm Psychol 1968, 73: 256–262.
Hitzemann R. Animal models of psychiatric disorders and their relevance to alcoholism. Alcohol Res Health 2000, 24: 149–158.
O’Neil MF, Moore NA. Animal models of depression: Are there any? Hum Psychopharmacol 2003, 18: 239–254.
Seligman ME, Maier SF. Failure to escape traumatic shock. J Exp Psychol 1967, 74: 1–9.
Chourbaji S, Zacher C, Sanchis-Segura C, Dormann C, Vollmayr B, Gass P. Learned helplessness: Validity and reliability of depressive-like states in mice. Brain Res Brain Res Protoc 2005, 16: 70–78.
Vollmayr B, Henn FA. Learned helplessness in the rat: Improvements in validity and reliability. Brain Res Brain Res Protoc 2001, 8: 1–7.
Drugan RC, Basile AS, Ha JH, Healy D, Ferland RJ. Analysis of the importance of controllable versus uncontrollable stress on subsequent behavioral and physiological functioning. Brain Res Brain Res Protoc 1997, 2: 69–74.
Yan HC, Cao X, Das M, Zhu XH, Gao TM. Behavioral animal models of depression. Neurosci Bull 2010, 26: 327–337.
Nestler EJ, Hyman SE. Animal models of neuropsychiatric disorders. Nat Neurosci 2010, 13: 1161–1169.
Cryan JF, Mombereau C, Vassout A. The tail suspension test as a model for assessing antidepressant activity: Review of pharmacological and genetic studies in mice. Neurosci Biobehav Rev 2005, 29: 571–625.
Takamori K, Yoshida S, Okuyama S. Availability of learned helplessness test as a model of depression compared to a forced swimming test in rats. Pharmacology 2001, 63: 147–153.
Pryce CR, Azzinnari D, Spinelli S, Seifritz E, Tegethoff M, Meinlschmidt G. Helplessness: A systematic translational review of theory and evidence for its relevance to understanding and treating depression. Pharmacol Ther 2011, 132: 242–267.
Vollmayr B, Gass P. Learned helplessness: Unique features and translational value of a cognitive depression model. Cell Tissue Res 2013, 354: 171–178.
Cryan JF, Markou A, Lucki I. Assessing antidepressant activity in rodents: Recent developments and future needs. Trends Pharmacol Sci 2002, 23: 238–245.
Henn FA, Vollmayr B. Stress models of depression: Forming genetically vulnerable strains. Neurosci Biobehav Rev 2005, 29: 799–804.
Li X, Hu L. The role of stress regulation on neural plasticity in pain chronification. Neural Plast 2016, 2016: 6402942.
Li XY, Wan Y, Tang SJ, Guan Y, Wei F, Ma D. Maladaptive plasticity and neuropathic pain. Neural Plast 2016, 2016: 4842159.
Meerwijk EL, Ford JM, Weiss SJ. Brain regions associated with psychological pain: Implications for a neural network and its relationship to physical pain. Brain Imaging Behav 2013, 7: 1–14.
Micov AM, Tomić MA, Todorović MB, Vuković MJ, Pecikoza UB, Jasnic NI, et al. Vortioxetine reduces pain hypersensitivity and associated depression-like behavior in mice with oxaliplatin-induced neuropathy. Prog Neuropsychopharmacol Biol Psychiatry 2020, 103: 109975.
Doan L, Manders T, Wang J. Neuroplasticity underlying the comorbidity of pain and depression. Neural Plast 2015, 2015: 504691.
Sheng J, Liu S, Wang Y, Cui R, Zhang X. The link between depression and chronic pain: Neural mechanisms in the brain. Neural Plast 2017, 2017: 9724371.
Middlemiss T, Laird BJA, Fallon MT. Mechanisms of cancer-induced bone pain. Clin Oncol (R Coll Radiol) 2011, 23: 387–392.
Ma W, Bisby MA. Partial and complete sciatic nerve injuries induce similar increases of neuropeptide Y and vasoactive intestinal peptide immunoreactivities in primary sensory neurons and their central projections. Neuroscience 1998, 86: 1217–1234.
Ma W, Bisby MA. Increase of preprotachykinin mRNA and substance P immunoreactivity in spared dorsal root ganglion neurons following partial sciatic nerve injury. Eur J Neurosci 1998, 10: 2388–2399.
Ma W, Bisby MA. Differential expression of galanin immunoreactivities in the primary sensory neurons following partial and complete sciatic nerve injuries. Neuroscience 1997, 79: 1183–1195.
Kim SH, Chung JM. An experimental model for peripheral neuropathy produced by segmental spinal nerve ligation in the rat. Pain 1992, 50: 355–363.
Tsuda M, Shigemoto-Mogami Y, Koizumi S, Mizokoshi A, Kohsaka S, Salter MW, et al. P2X4 receptors induced in spinal microglia gate tactile allodynia after nerve injury. Nature 2003, 424: 778–783.
Decosterd I, Woolf CJ. Spared nerve injury: An animal model of persistent peripheral neuropathic pain. Pain 2000, 87: 149–158.
Walczak JS, Pichette V, Leblond F, Desbiens K, Beaulieu P. Behavioral, pharmacological and molecular characterization of the saphenous nerve partial ligation: A new model of neuropathic pain. Neuroscience 2005, 132: 1093–1102.
Attal N, Jazat F, Kayser V, Guilbaud G. Further evidence for ‘pain-related’ behaviours in a model of unilateral peripheral mononeuropathy. Pain 1990, 41: 235–251.
Bennett GJ, Xie YK. A peripheral mononeuropathy in rat that produces disorders of pain sensation like those seen in man. Pain 1988, 33: 87–107.
Yi H, Kim MA, Back SK, Eun JS, Na HS. A novel rat forelimb model of neuropathic pain produced by partial injury of the Median and ulnar nerves. Eur J Pain 2011, 15: 459–466.
Shir Y, Seltzer Z. A-fibers mediate mechanical hyperesthesia and allodynia and C-fibers mediate thermal hyperalgesia in a new model of causalgiform pain disorders in rats. Neurosci Lett 1990, 115: 62–67.
Cohen SP, Mao J. Neuropathic pain: Mechanisms and their clinical implications. BMJ 2014, 348: f7656.
Kaliyaperumal S, Wilson K, Aeffner F, Dean C Jr. Animal models of peripheral pain: Biology review and application for drug discovery. Toxicol Pathol 2020, 48: 202–219.
Morado-Urbina CE, Alvarado-Vázquez PA, Montiel-Ruiz RM, Acosta-González RI, Castañeda-Corral G, Jiménez-Andrade JM. Early, middle, or late administration of zoledronate alleviates spontaneous nociceptive behavior and restores functional outcomes in a mouse model of CFA-induced arthritis. Drug Dev Res 2014, 75: 438–448.
Winter CA, Risley EA, Nuss GW. Carrageenin-induced edema in hind paw of the rat as an assay for antiiflammatory drugs. Proc Soc Exp Biol Med 1962, 111: 544–547.
Stein C, Millan MJ, Herz A. Unilateral inflammation of the hindpaw in rats as a model of prolonged noxious stimulation: Alterations in behavior and nociceptive thresholds. Pharmacol Biochem Behav 1988, 31: 445–451.
Brennan TJ. Postoperative models of nociception. ILAR J 1999, 40: 129–136.
Brennan TJ, Vandermeulen EP, Gebhart GF. Characterization of a rat model of incisional pain. Pain 1996, 64: 493–502.
Pogatzki EM, Raja SN. A mouse model of incisional pain. Anesthesiology 2003, 99: 1023–1027.
Honoré P, Schwei J, Rogers SD, Salak-Johnson JL, Finke MP, Ramnaraine ML, et al. Cellular and neurochemical remodeling of the spinal cord in bone cancer pain. Prog Brain Res 2000, 129: 389–397.
Wacnik PW, Kehl LJ, Trempe TM, Ramnaraine ML, Beitz AJ, Wilcox GL. Tumor implantation in mouse humerus evokes movement-related hyperalgesia exceeding that evoked by intramuscular carrageenan. Pain 2003, 101: 175–186.
Wacnik PW, Eikmeier LJ, Ruggles TR, Ramnaraine ML, Walcheck BK, Beitz AJ, et al. Functional interactions between tumor and peripheral nerve: Morphology, algogen identification, and behavioral characterization of a new murine model of cancer pain. J Neurosci 2001, 21: 9355–9366.
Zhang RX, Liu B, Wang L, Ren K, Qiao JT, Berman BM, et al. Spinal glial activation in a new rat model of bone cancer pain produced by prostate cancer cell inoculation of the tibia. Pain 2005, 118: 125–136.
Ornitz DM, Hammer RE, Messing A, Palmiter RD, Brinster RL. Pancreatic neoplasia induced by SV40 T-antigen expression in acinar cells of transgenic mice. Science 1987, 238: 188–193.
Hendriksen H, Korte SM, Olivier B, Oosting RS. The olfactory bulbectomy model in mice and rat: One story or two tails? Eur J Pharmacol 2015, 753: 105–113.
Song C, Leonard BE. The olfactory bulbectomised rat as a model of depression. Neurosci Biobehav Rev 2005, 29: 627–647.
Price JL, Drevets WC. Neural circuits underlying the pathophysiology of mood disorders. Trends Cogn Sci 2012, 16: 61–71.
Pryce CR, Rüedi-Bettschen D, Dettling AC, Weston A, Russig H, Ferger B, et al. Long-term effects of early-life environmental manipulations in rodents and Primates: Potential animal models in depression research. Neurosci Biobehav Rev 2005, 29: 649–674.
Lucassen PJ, Naninck EFG, van Goudoever JB, Fitzsimons C, Joels M, Korosi A. Perinatal programming of adult hippocampal structure and function; emerging roles of stress, nutrition and epigenetics. Trends Neurosci 2013, 36: 621–631.
Abelaira HM, Réus GZ, Quevedo J. Animal models as tools to study the pathophysiology of depression. Braz J Psychiatry 2013, 35: S112–S120.
Rice CJ, Sandman CA, Lenjavi MR, Baram TZ. A novel mouse model for acute and long-lasting consequences of early life stress. Endocrinology 2008, 149: 4892–4900.
Naninck EFG, Hoeijmakers L, Kakava-Georgiadou N, Meesters A, Lazic SE, Lucassen PJ, et al. Chronic early life stress alters developmental and adult neurogenesis and impairs cognitive function in mice. Hippocampus 2015, 25: 309–328.
Ridder S, Chourbaji S, Hellweg R, Urani A, Zacher C, Schmid W, et al. Mice with genetically altered glucocorticoid receptor expression show altered sensitivity for stress-induced depressive reactions. J Neurosci 2005, 25: 6243–6250.
Urani A, Chourbaji S, Gass P. Mutant mouse models of depression: Candidate genes and current mouse lines. Neurosci Biobehav Rev 2005, 29: 805–828.
Pliakas AM, Carlson RR, Neve RL, Konradi C, Nestler EJ Jr, Carlezon WA. Altered responsiveness to cocaine and increased immobility in the forced swim test associated with elevated cAMP response element-binding protein expression in nucleus accumbens. J Neurosci 2001, 21: 7397–7403.
Murphy DL, Lesch KP. Targeting the murine serotonin transporter: Insights into human neurobiology. Nat Rev Neurosci 2008, 9: 85–96.
Holmes A, Murphy DL, Crawley JN. Abnormal behavioral phenotypes of serotonin transporter knockout mice: Parallels with human anxiety and depression. Biol Psychiatry 2003, 54: 953–959.
Renoir T, Païzanis E, El Yacoubi M, Saurini F, Hanoun N, Melfort M, et al. Differential long-term effects of MDMA on the serotoninergic system and hippocampal cell proliferation in 5-HTT knock-out vs. wild-type mice. Int J Neuropsychopharmacol 2008, 11: 1149–1162.
Han S, Yang SH, Kim JY, Mo S, Yang E, Song KM, et al. Author correction: Down-regulation of cholinergic signaling in the habenula induces anhedonia-like behavior. Sci Rep 2017, 7: 17090.
Ely BA, Nguyen TNB, Tobe RH, Walker AM, Gabbay V. Multimodal investigations of reward circuitry and anhedonia in adolescent depression. Front Psychiatry 2021, 12: 678709.
Nestler EJ. Role of the brain’s reward circuitry in depression: Transcriptional mechanisms. Int Rev Neurobiol 2015, 124: 151–170.
Wise RA. Neuroleptics and operant behavior: The anhedonia hypothesis. Behav Brain Sci 1982, 5: 39–53.
Wook Koo J, Labonté B, Engmann O, Calipari ES, Juarez B, Lorsch Z, et al. Essential role of mesolimbic brain-derived neurotrophic factor in chronic social stress-induced depressive behaviors. Biol Psychiatry 2016, 80: 469–478.
Chaudhury D, Walsh JJ, Friedman AK, Juarez B, Ku SM, Koo JW, et al. Rapid regulation of depression-related behaviours by control of midbrain dopamine neurons. Nature 2013, 493: 532–536.
Russo SJ, Nestler EJ. The brain reward circuitry in mood disorders. Nat Rev Neurosci 2013, 14: 609–625.
Christoffel DJ, Golden SA, Russo SJ. Structural and synaptic plasticity in stress-related disorders. Rev Neurosci 2011, 22: 535–549.
Britt JP, Benaliouad F, McDevitt RA, Stuber GD, Wise RA, Bonci A. Synaptic and behavioral profile of multiple glutamatergic inputs to the nucleus accumbens. Neuron 2012, 76: 790–803.
Chen BT, Yau HJ, Hatch C, Kusumoto-Yoshida I, Cho SL, Hopf FW, et al. Rescuing cocaine-induced prefrontal cortex hypoactivity prevents compulsive cocaine seeking. Nature 2013, 496: 359–362.
Christoffel DJ, Golden SA, Walsh JJ, Guise KG, Heshmati M, Friedman AK, et al. Excitatory transmission at thalamo-striatal synapses mediates susceptibility to social stress. Nat Neurosci 2015, 18: 962–964.
Lind EB, Sweis BM, Asp AJ, Esguerra M, Silvis KA, David Redish A, et al. A quadruple dissociation of reward-related behaviour in mice across excitatory inputs to the nucleus accumbens shell. Commun Biol 2023, 6: 119.
Vollmer KM, Green LM, Grant RI, Winston KT, Doncheck EM, Bowen CW, et al. Author Correction: An opioid-gated thalamoaccumbal circuit for the suppression of reward seeking in mice. Nat Commun 2023, 14: 4733.
Biane JS, Ladow MA, Stefanini F, Boddu SP, Fan A, Hassan S, et al. Neural dynamics underlying associative learning in the dorsal and ventral hippocampus. Nat Neurosci 2023, 26: 798–809.
LeGates TA, Kvarta MD, Tooley JR, Francis TC, Lobo MK, Creed MC, et al. Reward behaviour is regulated by the strength of hippocampus-nucleus accumbens synapses. Nature 2018, 564: 258–262.
Park AJ, Harris AZ, Martyniuk KM, Chang CY, Abbas AI, Lowes DC, et al. Reset of hippocampal-prefrontal circuitry facilitates learning. Nature 2021, 591: 615–619.
Shpokayte M, McKissick O, Guan X, Yuan B, Rahsepar B, Fernandez FR, et al. Hippocampal cells segregate positive and negative engrams. Commun Biol 2022, 5: 1009.
Turner VS, O’Sullivan RO, Kheirbek MA. Linking external stimuli with internal drives: A role for the ventral hippocampus. Curr Opin Neurobiol 2022, 76: 102590.
McEwen BS. Stress, sex, and neural adaptation to a changing environment: Mechanisms of neuronal remodeling. Ann N Y Acad Sci 2010, 1204: E38–E59.
Hill AS, Sahay A, Hen R. Increasing adult hippocampal neurogenesis is sufficient to reduce anxiety and depression-like behaviors. Neuropsychopharmacology 2015, 40: 2368–2378.
Sjulson L, Peyrache A, Cumpelik A, Cassataro D, Buzsáki G. Cocaine place conditioning strengthens location-specific hippocampal coupling to the nucleus accumbens. Neuron 2018, 98: 926-934.e5.
Bagot RC, Parise EM, Peña CJ, Zhang HX, Maze I, Chaudhury D, et al. Ventral hippocampal afferents to the nucleus accumbens regulate susceptibility to depression. Nat Commun 2015, 6: 7062.
Matsumoto M, Hikosaka O. Lateral habenula as a source of negative reward signals in dopamine neurons. Nature 2007, 447: 1111–1115.
Li B, Piriz J, Mirrione M, Chung C, Proulx CD, Schulz D, et al. Synaptic potentiation onto habenula neurons in the learned helplessness model of depression. Nature 2011, 470: 535–539.
Li K, Zhou T, Liao L, Yang Z, Wong C, Henn F, et al. βCaMKII in lateral habenula mediates core symptoms of depression. Science 2013, 341: 1016–1020.
Yang Y, Cui Y, Sang K, Dong Y, Ni Z, Ma S, et al. Ketamine blocks bursting in the lateral habenula to rapidly relieve depression. Nature 2018, 554: 317–322.
Shabel SJ, Wang C, Monk B, Aronson S, Malinow R. Stress transforms lateral habenula reward responses into punishment signals. Proc Natl Acad Sci U S A 2019, 116: 12488–12493.
Hangya B, Ranade SP, Lorenc M, Kepecs A. Central cholinergic neurons are rapidly recruited by reinforcement feedback. Cell 2015, 162: 1155–1168.
Harrison TC, Pinto L, Brock JR, Dan Y. Calcium imaging of basal forebrain activity during innate and learned behaviors. Front Neural Circuits 2016, 10: 36.
Cui Y, Lv G, Jin S, Peng J, Yuan J, He X, et al. A central amygdala-substantia innominata neural circuitry encodes aversive reinforcement signals. Cell Rep 2017, 21: 1770–1782.
Cui Y, Huang X, Huang P, Huang L, Feng Z, Xiang X, et al. Reward ameliorates depressive-like behaviors via inhibition of the substantia innominata to the lateral habenula projection. Sci Adv 2022, 8: eabn0193.
Sartorius A, Kiening KL, Kirsch P, von Gall CC, Haberkorn U, Unterberg AW, et al. Remission of major depression under deep brain stimulation of the lateral habenula in a therapy-refractory patient. Biol Psychiatry 2010, 67: e9–e11.
Rizzi-Wise CA, Wang DV. Putting together pieces of the lateral septum: Multifaceted functions and its neural pathways. eNeuro 2021, 8: ENEURO.0315–ENEURO.0321.2021.
An M, Kim HK, Park H, Kim K, Heo G, Park HE, et al. Lateral septum somatostatin neurons are activated by diverse stressors. Exp Neurobiol 2022, 31: 376–389.
Olds J, Milner P. Positive reinforcement produced by electrical stimulation of septal area and other regions of rat brain. J Comp Physiol Psychol 1954, 47: 419–427.
Prado-Alcala R, Streather A, Wise RA. Brain stimulation reward and dopamine terminal fields. II. Septal and cortical projections. Brain Res 1984, 301: 209–219.
Luo AH, Tahsili-Fahadan P, Wise RA, Lupica CR, Aston-Jones G. Linking context with reward: A functional circuit from hippocampal CA3 to ventral tegmental area. Science 2011, 333: 353–357.
McGlinchey EM, Aston-Jones G. Dorsal hippocampus drives context-induced cocaine seeking via inputs to lateral septum. Neuropsychopharmacology 2018, 43: 987–1000.
Sartor GC, Aston-Jones GS. A septal-hypothalamic pathway drives orexin neurons, which is necessary for conditioned cocaine preference. J Neurosci 2012, 32: 4623–4631.
Li L, Durand-de Cuttoli R, Aubry AV, Burnett CJ, Cathomas F, Parise LF, et al. Social trauma engages lateral septum circuitry to occlude social reward. Nature 2023, 613: 696–703.
Wang D, Wang W, Jiang S, Ma H, Lian H, Meng F, et al. Regulation of depression-related behaviors by GABAergic neurons in the lateral septum through periaqueductal gray neuronal projections. J Psychiatr Res 2021, 137: 202–214.
Wang M, Li P, Li Z, da Silva BS, Zheng W, Xiang Z, et al. Lateral septum adenosine A2A receptors control stress-induced depressive-like behaviors via signaling to the hypothalamus and habenula. Nat Commun 1880, 2023: 14.
Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: A literature review. Arch Intern Med 2003, 163: 2433–2445.
McWilliams LA, Goodwin RD, Cox BJ. Depression and anxiety associated with three pain conditions: Results from a nationally representative sample. Pain 2004, 111: 77–83.
Arnow BA, Hunkeler EM, Blasey CM, Lee J, Constantino MJ, Fireman B, et al. Comorbid depression, chronic pain, and disability in primary care. Psychosom Med 2006, 68: 262–268.
Goyal M, Singh S, Sibinga EMS, Gould NF, Rowland-Seymour A, Sharma R, et al. Meditation programs for psychological stress and well-being: A systematic review and meta-analysis. JAMA Intern Med 2014, 174: 357–368.
Zhou W, Jin Y, Meng Q, Zhu X, Bai T, Tian Y, et al. A neural circuit for comorbid depressive symptoms in chronic pain. Nat Neurosci 2019, 22: 1649–1658.
Zhang L, Wang J, Niu C, Zhang Y, Zhu T, Huang D, et al. Activation of parabrachial nucleus - ventral tegmental area pathway underlies the comorbid depression in chronic neuropathic pain in mice. Cell Rep 2021, 37: 109936.
Dale J, Zhou H, Zhang Q, Martinez E, Hu S, Liu K, et al. Scaling up cortical control inhibits pain. Cell Rep 2018, 23: 1301–1313.
Zhang Z, Gadotti VM, Chen L, Souza IA, Stemkowski PL, Zamponi GW. Role of prelimbic GABAergic circuits in sensory and emotional aspects of neuropathic pain. Cell Rep 2015, 12: 752–759.
Huang J, Gadotti VM, Chen L, Souza IA, Huang S, Wang D, et al. A neuronal circuit for activating descending modulation of neuropathic pain. Nat Neurosci 2019, 22: 1659–1668.
Huang S, Zhang Z, Gambeta E, Xu SC, Thomas C, Godfrey N, et al. Dopamine inputs from the ventral tegmental area into the medial prefrontal cortex modulate neuropathic pain-associated behaviors in mice. Cell Rep 2020, 33: 108393.
Baliki MN, Chialvo DR, Geha PY, Levy RM, Harden RN, Parrish TB, et al. Chronic pain and the emotional brain: Specific brain activity associated with spontaneous fluctuations of intensity of chronic back pain. J Neurosci 2006, 26: 12165–12173.
Gündel H, Valet M, Sorg C, Huber D, Zimmer C, Sprenger T, et al. Altered cerebral response to noxious heat stimulation in patients with somatoform pain disorder. Pain 2008, 137: 413–421.
Kuner R, Kuner T. Cellular circuits in the brain and their modulation in acute and chronic pain. Physiol Rev 2021, 101: 213–258.
Ji G, Sun H, Fu Y, Li Z, Pais-Vieira M, Galhardo V, et al. Cognitive impairment in pain through amygdala-driven prefrontal cortical deactivation. J Neurosci 2010, 30: 5451–5464.
Sun H, Neugebauer V. mGluR1, but not mGluR5, activates feed-forward inhibition in the medial prefrontal cortex to impair decision making. J Neurophysiol 2011, 106: 960–973.
Kiritoshi T, Ji G, Neugebauer V. Rescue of impaired mGluR5-driven endocannabinoid signaling restores prefrontal cortical output to inhibit pain in arthritic rats. J Neurosci 2016, 36: 837–850.
Wilson TD, Valdivia S, Khan A, Ahn HS, Adke AP, Martinez Gonzalez S, et al. Dual and opposing functions of the central amygdala in the modulation of pain. Cell Rep 2019, 29: 332-346.e5.
Zussy C, Gómez-Santacana X, Rovira X, De Bundel D, Ferrazzo S, Bosch D, et al. Dynamic modulation of inflammatory pain-related affective and sensory symptoms by optical control of amygdala metabotropic glutamate receptor 4. Mol Psychiatry 2018, 23: 509–520.
Henke PG. The telencephalic limbic system and experimental gastric pathology: A review. Neurosci Biobehav Rev 1982, 6: 381–390.
Zheng ZH, Tu JL, Li XH, Hua Q, Liu WZ, Liu Y, et al. Neuroinflammation induces anxiety- and depressive-like behavior by modulating neuronal plasticity in the basolateral amygdala. Brain Behav Immun 2021, 91: 505–518.
Patel RR, Wolfe SA, Bajo M, Abeynaike S, Pahng A, Borgonetti V, et al. IL-10 normalizes aberrant amygdala GABA transmission and reverses anxiety-like behavior and dependence-induced escalation of alcohol intake. Prog Neurobiol 2021, 199: 101952.
Munshi S, Loh MK, Ferrara N, DeJoseph MR, Ritger A, Padival M, et al. Repeated stress induces a pro-inflammatory state, increases amygdala neuronal and microglial activation, and causes anxiety in adult male rats. Brain Behav Immun 2020, 84: 180–199.
Yue N, Huang H, Zhu X, Han Q, Wang Y, Li B, et al. Activation of P2X7 receptor and NLRP3 inflammasome assembly in hippocampal glial cells mediates chronic stress-induced depressive-like behaviors. J Neuroinflammation 2017, 14: 102.
Ohgidani M, Kato TA, Sagata N, Hayakawa K, Shimokawa N, Sato-Kasai M, et al. TNF-α from hippocampal microglia induces working memory deficits by acute stress in mice. Brain Behav Immun 2016, 55: 17–24.
Cunningham AJ, Murray CA, O’Neill LA, Lynch MA, O’Connor JJ. Interleukin-1 beta (IL-1 beta) and tumour necrosis factor (TNF) inhibit long-term potentiation in the rat dentate gyrus in vitro. Neurosci Lett 1996, 203: 17–20.
Green HF, Nolan YM. Inflammation and the developing brain: Consequences for hippocampal neurogenesis and behavior. Neurosci Biobehav Rev 2014, 40: 20–34.
Revest JM, Dupret D, Koehl M, Funk-Reiter C, Grosjean N, Piazza PV, et al. Adult hippocampal neurogenesis is involved in anxiety-related behaviors. Mol Psychiatry 2009, 14: 959–967.
Rooney S, Sah A, Unger MS, Kharitonova M, Sartori SB, Schwarzer C, et al. Neuroinflammatory alterations in trait anxiety: Modulatory effects of minocycline. Transl Psychiatry 2020, 10: 256.
Shao S, Zheng Y, Fu Z, Wang J, Zhang Y, Wang C, et al. Ventral hippocampal CA1 modulates pain behaviors in mice with peripheral inflammation. Cell Rep 2023, 42: 112017.
Kogan JH, Frankland PW, Silva AJ. Long-term memory underlying hippocampus-dependent social recognition in mice. Hippocampus 2000, 10: 47–56.
Tyng CM, Amin HU, Saad MNM, Malik AS. The influences of emotion on learning and memory. Front Psychol 2017, 8: 1454.
De Pascalis V, Moret-Tatay C. Editorial: Emotion regulation and cognitive processes. Front Hum Neurosci 2023, 17: 1250666.
Joormann J, Stanton CH. Examining emotion regulation in depression: A review and future directions. Behav Res Ther 2016, 86: 35–49.
Alexandra Kredlow M, Fenster RJ, Laurent ES, Ressler KJ, Phelps EA. Prefrontal cortex, amygdala, and threat processing: Implications for PTSD. Neuropsychopharmacology 2022, 47: 247–259.
Vythilingam M, Vermetten E, Anderson GM, Luckenbaugh D, Anderson ER, Snow J, et al. Hippocampal volume, memory, and cortisol status in major depressive disorder: Effects of treatment. Biol Psychiatry 2004, 56: 101–112.
Porter RJ, Gallagher P, Thompson JM, Young AH. Neurocognitive impairment in drug-free patients with major depressive disorder. Br J Psychiatry 2003, 182: 214–220.
Landrø NI, Stiles TC, Sletvold H. Neuropsychological function in nonpsychotic unipolar major depression. Neuropsychiatry Neuropsychol Behav Neurol 2001, 14: 233–240.
Taylor Tavares JV, Clark L, Cannon DM, Erickson K, Drevets WC, Sahakian BJ. Distinct profiles of neurocognitive function in unmedicated unipolar depression and bipolar II depression. Biol Psychiatry 2007, 62: 917–924.
Keilp JG, Gorlyn M, Russell M, Oquendo MA, Burke AK, Harkavy-Friedman J, et al. Neuropsychological function and suicidal behavior: Attention control, memory and executive dysfunction in suicide attempt. Psychol Med 2013, 43: 539–551.
Beblo T, Driessen M, Dehn L. Memory deficits in patients with major depression: Yes, they are trying hard enough! Expert Rev Neurother 2020, 20: 517–522.
Coutinho G, Drummond C, Teldeschi A, Mattos P. Awareness of memory deficits is useful to distinguish between depression and mild cognitive impairment in the elderly. Braz J Psychiatry 2016, 38: 231–234.
Sałaciak K, Koszałka A, Lustyk K, Żmudzka E, Jagielska A, Pytka K. Memory impairments in rodent depression models: A link with depression theories. Prog Neuro Psychopharmacol Biol Psychiatry 2023, 125: 110774.
Afzal A, Batool Z, Sadir S, Liaquat L, Shahzad S, Tabassum S, et al. Therapeutic potential of curcumin in reversing the depression and associated pseudodementia via modulating stress hormone, hippocampal neurotransmitters, and BDNF levels in rats. Neurochem Res 2021, 46: 3273–3285.
Sun XP, Li SD, Shi Z, Li TF, Pan RL, Chang Q, et al. Antidepressant-like effects and memory enhancement of a herbal formula in mice exposed to chronic mild stress. Neurosci Bull 2013, 29: 737–744.
Wu GF, Ren S, Tang RY, Xu C, Zhou JQ, Lin SM, et al. Antidepressant effect of taurine in chronic unpredictable mild stress-induced depressive rats. Sci Rep 2017, 7: 4989.
Lejeune S, Dourmap N, Martres MP, Giros B, Daugé V, Naudon L. The dopamine D1 receptor agonist SKF 38393 improves temporal order memory performance in maternally deprived rats. Neurobiol Learn Mem 2013, 106: 268–273.
Tsetsenis T, Broussard JI, Dani JA. Dopaminergic regulation of hippocampal plasticity, learning, and memory. Front Behav Neurosci 2022, 16: 1092420.
Duszkiewicz AJ, McNamara CG, Takeuchi T, Genzel L. Novelty and dopaminergic modulation of memory persistence: A tale of two systems. Trends Neurosci 2019, 42: 102–114.
Dillon DG. The neuroscience of positive memory deficits in depression. Front Psychol 2015, 6: 1295.
Pittenger C, Duman RS. Stress, depression, and neuroplasticity: A convergence of mechanisms. Neuropsychopharmacology 2008, 33: 88–109.
Ramirez S, Liu X, MacDonald CJ, Moffa A, Zhou J, Redondo RL, et al. Activating positive memory engrams suppresses depression-like behaviour. Nature 2015, 522: 335–339.
Mirescu C, Gould E. Stress and adult neurogenesis. Hippocampus 2006, 16: 233–238.
Snyder JS, Soumier A, Brewer M, Pickel J, Cameron HA. Adult hippocampal neurogenesis buffers stress responses and depressive behaviour. Nature 2011, 476: 458–461.
Dillon DG, Pizzagalli DA. Mechanisms of memory disruption in depression. Trends Neurosci 2018, 41: 137–149.
Malberg JE, Eisch AJ, Nestler EJ, Duman RS. Chronic antidepressant treatment increases neurogenesis in adult rat hippocampus. J Neurosci 2000, 20: 9104–9110.
Marrocco J, Reynaert ML, Gatta E, Gabriel C, Mocaër E, Di Prisco S, et al. The effects of antidepressant treatment in prenatally stressed rats support the glutamatergic hypothesis of stress-related disorders. J Neurosci 2014, 34: 2015–2024.
Meira T, Leroy F, Buss EW, Oliva A, Park J, Siegelbaum SA. A hippocampal circuit linking dorsal CA2 to ventral CA1 critical for social memory dynamics. Nat Commun 2018, 9: 4163.
Stevenson EL, Caldwell HK. Lesions to the CA2 region of the hippocampus impair social memory in mice. Eur J Neurosci 2014, 40: 3294–3301.
Hitti FL, Siegelbaum SA. The hippocampal CA2 region is essential for social memory. Nature 2014, 508: 88–92.
Phillips ML, Robinson HA, Pozzo-Miller L. Ventral hippocampal projections to the medial prefrontal cortex regulate social memory. Elife 2019, 8: e44182.
Fanselow MS, Dong HW. Are the dorsal and ventral hippocampus functionally distinct structures? Neuron 2010, 65: 7–19.
Zhu H, Pleil KE, Urban DJ, Moy SS, Kash TL, Roth BL. Chemogenetic inactivation of ventral hippocampal glutamatergic neurons disrupts consolidation of contextual fear memory. Neuropsychopharmacology 2014, 39: 1880–1892.
Tye KM, Tye LD, Cone JJ, Hekkelman EF, Janak PH, Bonci A. Methylphenidate facilitates learning-induced amygdala plasticity. Nat Neurosci 2010, 13: 475–481.
Rumpel S, LeDoux J, Zador A, Malinow R. Postsynaptic receptor trafficking underlying a form of associative learning. Science 2005, 308: 83–88.
Pikkarainen M, Rönkkö S, Savander V, Insausti R, Pitkänen A. Projections from the lateral, basal, and accessory basal nuclei of the amygdala to the hippocampal formation in rat. J Comp Neurol 1999, 403: 229–260.
Akirav I, Richter-Levin G. Mechanisms of amygdala modulation of hippocampal plasticity. J Neurosci 2002, 22: 9912–9921.
Roozendaal B, McGaugh JL. Basolateral amygdala lesions block the memory-enhancing effect of glucocorticoid administration in the dorsal hippocampus of rats. Eur J Neurosci 1997, 9: 76–83.
Yang Y, Wang ZH, Jin S, Gao D, Liu N, Chen SP, et al. Opposite monosynaptic scaling of BLP-vCA1 inputs governs hopefulness- and helplessness-modulated spatial learning and memory. Nat Commun 2016, 7: 11935.
Pi G, Gao D, Wu D, Wang Y, Lei H, Zeng W, et al. Posterior basolateral amygdala to ventral hippocampal CA1 drives approach behaviour to exert an anxiolytic effect. Nat Commun 2020, 11: 183.
Chen YH, Wu JL, Hu NY, Zhuang JP, Li WP, Zhang SR, et al. Distinct projections from the infralimbic cortex exert opposing effects in modulating anxiety and fear. J Clin Invest 2021, 131: e145692.
Pfarr S, Schaaf L, Reinert JK, Paul E, Herrmannsdörfer F, Roßmanith M, et al. Choice for drug or natural reward engages largely overlapping neuronal ensembles in the infralimbic prefrontal cortex. J Neurosci 2018, 38: 3507–3519.
Huang WC, Zucca A, Levy J, Page DT. Social behavior is modulated by valence-encoding mPFC-amygdala sub-circuitry. Cell Rep 2020, 32: 107899.
Bloodgood DW, Sugam JA, Holmes A, Kash TL. Fear extinction requires infralimbic cortex projections to the basolateral amygdala. Transl Psychiatry 2018, 8: 60.
Yu H, Chen L, Lei H, Pi G, Xiong R, Jiang T, et al. Infralimbic medial prefrontal cortex signalling to calbindin 1 positive neurons in posterior basolateral amygdala suppresses anxiety- and depression-like behaviours. Nat Commun 2022, 13: 5462.
Fuchikami M, Thomas A, Liu R, Wohleb ES, Land BB, DiLeone RJ, et al. Optogenetic stimulation of infralimbic PFC reproduces ketamine’s rapid and sustained antidepressant actions. Proc Natl Acad Sci U S A 2015, 112: 8106–8111.
Hare BD, Shinohara R, Liu RJ, Pothula S, DiLeone RJ, Duman RS. Optogenetic stimulation of medial prefrontal cortex Drd1 neurons produces rapid and long-lasting antidepressant effects. Nat Commun 2019, 10: 223.
Arnsten AFT. Stress weakens prefrontal networks: Molecular insults to higher cognition. Nat Neurosci 2015, 18: 1376–1385.
Patki G, Solanki N, Atrooz F, Allam F, Salim S. Depression, anxiety-like behavior and memory impairment are associated with increased oxidative stress and inflammation in a rat model of social stress. Brain Res 2013, 1539: 73–86.
Liu SC, Hu WY, Zhang WY, Yang L, Li Y, Xiao ZC, et al. Paeoniflorin attenuates impairment of spatial learning and hippocampal long-term potentiation in mice subjected to chronic unpredictable mild stress. Psychopharmacology 2019, 236: 2823–2834.
Daskalakis NP, De Kloet ER, Yehuda R, Malaspina D, Kranz TM. Early life stress effects on glucocorticoid-BDNF interplay in the hippocampus. Front Mol Neurosci 2015, 8: 68.
Kumar A, Singh N. Pharmacological activation of protein kinase A improves memory loss and neuropathological changes in a mouse model of dementia of Alzheimer’s type. Behav Pharmacol 2017, 28: 187–198.
Wang Q, Shao F, Wang W. Maternal separation produces alterations of forebrain brain-derived neurotrophic factor expression in differently aged rats. Front Mol Neurosci 2015, 8: 49.
Lapmanee S, Charoenphandhu J, Teerapornpuntakit J, Krishnamra N, Charoenphandhu N. Agomelatine, venlafaxine, and running exercise effectively prevent anxiety- and depression-like behaviors and memory impairment in restraint stressed rats. PLoS One 2017, 12: e0187671.
Shilpa BM, Bhagya V, Harish G, Srinivas Bharath MM, Shankaranarayana Rao BS. Environmental enrichment ameliorates chronic immobilisation stress-induced spatial learning deficits and restores the expression of BDNF, VEGF, GFAP and glucocorticoid receptors. Prog Neuropsychopharmacol Biol Psychiatry 2017, 76: 88–100.
Li S, Wang C, Wang MW, Murakami Y, Matsumoto K. Impairment of the spatial learning and memory induced by learned helplessness and chronic mild stress. Pharmacol Biochem Behav 2006, 83: 186–193.
Almeida RF, Nonose Y, Ganzella M, Loureiro SO, Rocha A, Machado DG, et al. Antidepressant-like effects of chronic guanosine in the olfactory bulbectomy mouse model. Front Psychiatry 2021, 12: 701408.
Antunes MS, Jesse CR, Ruff JR, de Oliveira Espinosa D, Gomes NS, Altvater EET, et al. Hesperidin reverses cognitive and depressive disturbances induced by olfactory bulbectomy in mice by modulating hippocampal neurotrophins and cytokine levels and acetylcholinesterase activity. Eur J Pharmacol 2016, 789: 411–420.
Capibaribe VCC, Vasconcelos Mallmann AS, Lopes IS, Oliveira ICM, de Oliveira NF, Chaves RC, et al. Thymol reverses depression-like behaviour and upregulates hippocampal BDNF levels in chronic corticosterone-induced depression model in female mice. J Pharm Pharmacol 2019, 71: 1774–1783.
Li C, Li M, Yu H, Shen X, Wang J, Sun X, et al. Neuropeptide VGF C-terminal peptide TLQP-62 alleviates lipopolysaccharide-induced memory deficits and anxiety-like and depression-like behaviors in mice: The role of BDNF/TrkB signaling. ACS Chem Neurosci 2017, 8: 2005–2018.
Zhang ZH, Wu LN, Song JG, Li WQ. Correlations between cognitive impairment and brain-derived neurotrophic factor expression in the hippocampus of post-stroke depression rats. Mol Med Rep 2012, 6: 889–893.
Acknowledgments
This review was supported by the Brain & Behavior Research Foundation (30233).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tian, X., Russo, S.J. & Li, L. Behavioral Animal Models and Neural-Circuit Framework of Depressive Disorder. Neurosci. Bull. (2024). https://doi.org/10.1007/s12264-024-01270-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12264-024-01270-7