Abstract
The majority of patients with Philadelphia chromosome-negative myeloproliferative neoplasms (MPNs) harbor JAK2, CALR, or MPL mutations. We compared clinical manifestations of different subtypes of JAK2 and CALR mutations in Japanese patients with MPNs. Within our cohort, we diagnosed 166 patients as polycythemia vera (PV), 212 patients as essential thrombocythemia (ET), 23 patients as pre-primary myelofibrosis (PMF), 65 patients as overt PMF, and 27 patients as secondary myelofibrosis following the 2016 WHO criteria. Compared to patients with JAK2V617F-mutated PV, JAK2 exon 12-mutated PV patients were younger, showed lower white blood cell (WBC) counts, lower platelet counts, higher red blood cell counts, and higher frequency of thrombotic events. Compared to JAK2-mutated ET patients, CALR-mutated ET patients were younger, showed lower WBC counts, lower hemoglobin levels, higher platelet counts, and fewer thrombotic events. CALR type 1-like mutation was the dominant subtype in CALR-mutated overt PMF patients. Compared with JAK2V617F-mutated ET patients, JAK2V617F-mutated pre-PMF patients showed higher LDH levels, lower hemoglobin levels, higher JAK2V617F allele burden, and higher frequency of splenomegaly. In conclusion, Japanese patients with MPNs grouped by different mutation subtypes exhibit characteristics similar to those of their Western counterparts. In addition, ET and pre-PMF patients show different characteristics, even when restricted to JAK2V617F-mutated patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
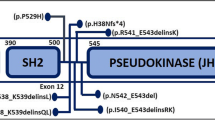
Philadelphia chromosome-negative myeloproliferative neoplasms (MPNs) are clonal hematopoietic stem cell disorders presenting with proliferation of myeloid lineage cells. Major entities of MPNs include polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF). Recurrent somatic mutations in JAK2, CALR and MPL genes have been identified in patients diagnosed with MPNs [1]. JAK2 mutations can be subclassified into the JAK2V617F mutation and JAK2 exon 12 mutations. CALR mutations can be subclassified into two major subgroups according to their predicted effect on the calreticulin C-terminal, CALR type 1-like mutations and type 2-like mutations. PV patients are known to potentially harbor JAK2V617F or JAK2 exon 12 mutations. In contrast, patients with ET and PMF can present with JAK2V617F, CALR type 1-like, CALR type 2-like, or MPL mutations. Mutation subtypes in specific entities of MPNs are known to be associated with certain clinical features in Caucasian cohorts [2,3,4.] We applied the 2016 WHO diagnostic criteria to a large cohort of Japanese patients with suspected MPNs and verified whether previous findings are the same in Japan.
Materials and methods
Study population
This study involved 2219 individuals with suspected MPNs from the Department of Hematology at Juntendo University School of Medicine and other participating institutions in Japan between April 2010 and December 2016. This study was conducted in accordance with the Declaration of Helsinki and was approved by the ethics committee of Juntendo University School of Medicine (IRB#2013020). Written informed consent was obtained prior to the use of samples and collection of clinical records.
Mutation analysis
Genomic DNA was isolated from peripheral blood using a QIAamp DNA Mini Kit (QIAGEN) or Gentra Puregene Blood Kit (QIAGEN). DNA concentration was determined using a NanoDrop LITE spectrophotometer (Thermo Scientific), and the samples were stored at − 80 °C until use. JAK2V617F allele burdens were first determined via ABC-PCR [5]. If JAK2V617F allele burdens were below 10%, we added allele-specific PCR (AS-PCR), which is more accurate for measuring low allele burdens below 10% [6]. If JAK2V617F was negative in a patient clinically suspected of PV, JAK2 exon 12 mutations were additionally analyzed by direct sequencing method or by Miniseq Sequencing System (Illumina) using primers forward; 5′-TGGAGCAATTCATACTTTCAGTG-3′, reverse; 5′-AACACAAGGTTGGCATATTTTTC-3′. MPLW515K/L mutations were assessed using an allele-specific PCR technique called dual amplification refractory mutation system PCR (DARMS-PCR) and subsequent capillary electrophoresis [7]. The CALR mutation on exon 9 was examined using our in-house fragment analysis method [8]. If the detected CALR mutation was other than CALRdel52 and CALRins5 mutations, we additionally carried out direct sequencing method to classify the CALR mutation subtype based on the definition by Pietra et al. [9] using primers forward; 5′-CTGGTCCTGGTCCTGATGTC-3′, reverse; 5′-CAGTCCAGCCCTGGAGGCAG-3′. Although JAK2, MPL, CALR mutations have been proposed to be mutually exclusive, we identified two ET patients with JAK2V617F coinciding with either MPLW515L or MPLW515K mutations, and these patients were excluded from analysis.
Diagnosis
Patients were diagnosed as PV, ET, prefibrotic PMF (pre-PMF), overt PMF, or secondary myelofibrosis (sMF) according to the 2016 WHO diagnostic criteria with available indices [10]. Clinical and laboratory parameters were obtained from the time of diagnosis. We set an erythropoietin (EPO) concentration of less than 12.5 mU/mL as subnormal serum EPO level [11].
Statistics
For comparing different patient groups, we applied the Fisher’s exact test for categorical variables and the Mann–Whitney U test for continuous variables. All statistical analysis were carried out with EZR software (Saitama Medical Center, Jichi Medical University, Saitama, Japan), which is a graphical user interface for R (The R Foundation for Statistical Computing, Vienna, Austria) [12]. p values less than 0.05 were considered significant.
Results
Diagnosis of MPNs and driver mutation frequencies
In a cohort of patients with suspected MPNs, we diagnosed 166 patients with PV, 212 patients with ET, 23 patients with pre-PMF, 65 patients with overt PMF, and 27 patients with sMF consisting of nine post-polycythemia vera myelofibrosis (post-PV MF) patients and 18 post-essential thrombocythemia myelofibrosis (post-ET MF) patients. Clinical characteristics of PV, ET, pre-PMF, overt PMF and sMF were similar compared to previous reports (Table 1) [4, 13, 14]. Of 166 PV patients, 161 (97.0%) harbored JAK2 mutations, and five (3.0%) patients were negative for JAK2, CALR and MPL mutations (triple-negative). Of 212 ET patients, 127 (59.9%) harbored JAK2 mutations, 57 (26.9%) harbored CALR mutations, 10 (4.7%) harbored MPL mutations and 18 (8.5%) patients were triple-negative. Of 23 pre-PMF patients, 18 patients (78.3%) harbored JAK2 mutations, one patient (4.3%) harbored a CALR mutation, and four patients (17.4%) were triple-negative. Of 65 overt PMF patients, 35 patients (53.8%) harbored JAK2 mutations, 18 patients (27.7%) harbored CALR mutations, one patient (1.5%) harbored an MPL mutation and 11 patients (16.9%) were triple-negative. Of 27 sMF patients, 16 patients (59.3%) harbored JAK2V617F, nine patients (33.3%) harbored CALR mutations and one patient (3.7%) harbored an MPL mutation and one patient (3.7%) was triple-negative.
JAK2V617F allele burdens in PV, ET, pre-PMF, overt PMF and sMF
Median JAK2V617F allele burdens calculated within JAK2V617F mutation-positive patients were 77.6% in PV, 30.7% in ET, 38.0% in pre-PMF, 48.2% in overt PMF, 94.5% in post-PV MF, 72.7% in post-ET MF. JAK2V617F allele burdens were significantly higher in PV compared to ET, pre-PMF, and overt PMF (p < 0.001). Pre-PMF patients showed significantly higher JAK2V617F allele burdens compared to ET patients (p = 0.036). Post-PV MF patients showed significantly higher JAK2V617F allele burdens compared to PV patients (p = 0.022). Post-ET MF patients tended to show higher allele burdens compared to ET patients (p = 0.095). Overt PMF patients tended to show higher JAK2V617F allele burdens compared to pre-PMF patients (p = 0.372) (Fig. 1).
Diversity of JAK2V617F allele burdens among MPNs. PV polycythemia vera, ET essential thrombocythemia, pre-PMF prefibrotic primary myelofibrosis, overt PMF overt fibrotic stage primary myelofibrosis, MF myelofibrosis. Median JAK2V617F allele burdens of each disease were as follows, PV 77.6% (range 8.5–100%), post-PV MF 94.5% (range 48.8–100%), ET 30.7% (range 5.2–100%), post-ET MF 72.7% (range 3.9–99.8%), pre-PMF 38.0% (range 14.9–100%), overt PMF 48.2% (range 11.2–99.3%)
Clinical characteristics of PV patients with different JAK2 mutation subtypes
Of 161 JAK2-mutated PV patients, we identified 152 patients with JAK2V617F mutations and nine patients with JAK2 exon 12 mutations. JAK2 exon 12 mutation variations of the nine patients were present in the following distributions: two c.1615_16 AA > TT, two c.1611_16 delTCACAA, one c.1615_16 AA > CT, one c.1614_16 CAA > ATT, one c.1613_16 ACAA > T, one c.1623_28 delAAATGA and one c.1627_32 delGAAGAT. Compared with JAK2V617F patients, JAK2 exon 12-mutated patients were significantly younger (exon 12: 53 years vs V617F: 64 years, p = 0.024), showed lower levels of white blood cell (WBC) counts (exon 12: 8.4 × 109/L vs V617F: 14.2 × 109/L, p = 0.028), higher red blood cell (RBC) counts (exon 12: 7.6 × 1012/L vs V617F: 7.1 × 1012/L, p = 0.019), lower mean corpuscular volume (MCV) (exon 12: 75.3 fl vs V617F: 82.6 fl, p = 0.012), lower platelet counts (exon 12: 357 × 109/L vs V617F: 565 × 109/L, p = 0.016), and higher frequency of thrombotic events (exon 12: 55.6% vs V617F: 23.4%, p = 0.046). There were no differences between the two groups concerning EPO levels, presence of splenomegaly and bone marrow fibrosis (Table 2).
Clinical characteristics of ET and PMF patients with different mutational status
Compared to JAK2-mutated ET patients (JAK2-ET), CALR-mutated ET patients (CALR-ET) were significantly younger (CALR-ET: 60 years vs JAK2-ET: 67 years, p = 0.036), showed lower WBC counts (CALR-ET: 8.0 × 109/L vs JAK2-ET: 9.8 × 109/L, p < 0.001), lower hemoglobin (Hb) levels (CALR-ET: 13.4 g/dL vs JAK2-ET: 14.3 g/dL, p < 0.001), lower hematocrit (Hct) levels (CALR-ET: 40.0% vs JAK2-ET: 43.3%, p < 0.001), higher platelet counts (CALR-ET: 1040 × 109/L vs JAK2-ET: 847 × 109/L, p < 0.001), and lower frequency of thrombotic events (CALR-ET: 5.3% vs JAK2-ET; 20.5%, p = 0.008). Compared to JAK2-ET, triple-negative ET patients also showed significantly lower WBC counts (triple-negative ET: 7.8 × 109/L vs JAK2-ET: 9.8 × 109/L, p = 0.009), lower Hb levels (triple-negative ET: 13.2 g/dL vs JAK2-ET: 14.3 g/dL, p = 0.003) and lower Hct levels (triple-negative ET: 40.1% vs JAK2-ET: 43.3%, p = 0.003), but no difference was observed concerning age, platelet counts and thrombotic events. Triple-negative ET patients showed significantly lower rate of bone marrow fibrosis (MF-1) compared to JAK2-ET and CALR-ET (triple-negative ET: 0% vs JAK2-ET: 20.5%, p = 0.044, triple-negative ET: 0% vs CALR-ET: 22.8%, p = 0.030, respectively). Compared to JAK2-ET, MPL-mutated ET patients (MPL-ET) showed significantly lower Hb levels (MPL-ET: 12.9 g/dL vs JAK2-ET: 14.3 g/dL, p = 0.016), lower Hct levels (MPL-ET: 40.0% vs JAK2-ET: 43.3%, p = 0.023) and higher platelet counts (MPL-ET: 1296 × 109/L vs JAK2-ET: 847 × 109/L, p = 0.002). No significant differences in gender ratio, lactate dehydrogenase (LDH) levels and frequency of splenomegaly were seen between different mutation groups of ET (Table 3a).
No significant differences were seen in clinical characteristics between different mutation groups within pre-PMF patients (Table S1).
Concerning overt PMF, triple-negative overt PMF patients were younger than JAK2-mutated patients (JAK2-overt PMF) (triple-negative overt PMF; 51 years vs JAK2 overt PMF; 71 years, p = 0.017). Additionally, LDH levels differed significantly between JAK2V617F-mutated, CALR-mutated, and triple-negative overt PMF patients, with CALR-mutated patients (CALR-overt PMF) showing highest LDH levels (median LDH: 610 IU/L), JAK2-overt PMF showing intermediate LDH levels (median LDH: 465 IU/L), and triple-negative overt PMF showing lowest LDH levels (median LDH: 276 IU/L) (JAK2-overt PMF vs CALR-overt PMF, p = 0.036; JAK2-overt PMF vs triple-negative overt PMF, p = 0.006; CALR-overt PMF vs triple-negative overt PMF, p = 0.007) (Table 3b).
Clinical characteristics of ET and MF (PMF + sMF) patients with different CALR mutation subtypes
Of 57 CALR-ET, 35 patients harbored CALRdel52 (type 1 mutation), 15 patients harbored CALRins5 (type 2 mutation) and seven patients harbored other CALR exon 9 mutations. Based on the definition by Pietra et al. [9], we recategorized all patients into 38 type 1-like mutations, 16 type 2-like mutations, and three other type mutations. As previously reported [8], patients with CALR type 2-like mutations tended to show higher platelet counts compared to patients with type 1-like mutations. LDH levels were significantly higher in patients with CALR type 1-like mutations (315 vs 244 IU/L, p = 0.041) (Table 4a).
In myelofibrosis (MF) patients, which included overt PMF and sMF patients, 27 CALR-mutated patients were identified and categorized into 22 (81.5%) type 1-like and five (18.5%) type 2-like mutations. In accordance with previous reports, CALR type 1-like mutations were more common in MF patients compared to ET patients (MF: 81.5% vs ET: 70.4%) [9, 15]. In particular, CALR type 1-like mutated patients constituted the vast majority of CALR-overt PMF (15/17: 88.2%) (data not shown). As previously reported, there were no significant differences in patient characteristics between CALR type 1-like and CALR type 2-like mutated MF patients (Table 4b) [9].
Discussion
We compared clinical characteristics between different driver mutation groups and different mutation subtype groups in Japanese patients with PV, ET, pre-PMF, overt PMF and sMF diagnosed by the 2016 WHO criteria. The results were for the most part in line with previous reports from Western countries [4, 9, 13, 14], but some differences were found in our cohort. Concerning PV patients, we found that JAK2 exon 12 mutated patients had higher frequency of thrombotic events compared to JAK2V617F mutated patients. Previous reports of Caucasian cohorts showed that frequency of thrombotic events were equal between the two groups [16, 17]. This is the first study comparing clinical characteristics of Japanese PV patients with JAK2V617F and JAK2 exon 12 mutations, and these conflicting results may be due to differing ethnicity. Larger studies in Asian patients are needed to verify these results. Analysis of ET patients showed that frequency of bone marrow fibrosis (MF-1) was significantly lower in triple-negative ET compared to JAK2-ET and CALR-ET. This was rather surprising, because triple-negative ET patients are reported to have shorter time to myelofibrosis when compared to CALR-ET [18]. Within CALR-mutated ET, myelofibrotic transformation is known to be higher in CALR type 1-like mutations [19, 20]. The current study found no difference between CALR type 1-like and type 2-like patients concerning presence of bone marrow fibrosis, but this may be due to the small number of patients studied. However, patients with CALR type 1-like mutation showed significantly higher LDH levels in the current study which may reflect a higher myelofibrotic transformation potential. Also concerning ET, we found no gender difference between CALR type 1-like and type 2-like mutation groups, but male gender was reported to be associated with CALR type 1 mutation in a previous study [21].
Compared to other mutation groups, CALR-overt PMF are reported to present with younger age, lower WBC counts and higher platelet counts. We found conflicting results, with triple-negative PMF patients presenting with youngest age. When compared to JAK2-overt PMF, CALR-overt PMF is reported to have lower risk of thrombotic events, but we found no difference between the two groups [3]. Additionally, we found that LDH levels significantly differed between JAK2V617F-mutated, CALR-mutated, and triple-negative PMF patients, which have not been previously reported.
JAK2V617F allele burdens are reported to differ between different MPNs, and our study verifies these findings [4, 22, 23]. JAK2V617F allele burdens cannot be directly compared between studies when methods of analysis differ, and thus analysis of a broad range of MPNs within the same study is valuable. ET and pre-PMF showed lowest JAK2V617F allele burdens whereas PV and sMF showed highest JAK2V617F allele burdens. JAK2V617F allele burdens are low in ET, but are approximately twice as high in post-ET MF, and these findings further support a previous report by Shirane et al. showing that an increase of JAK2V617F allele burdens during the disease course of ET might correlate with myelofibrotic transformation [24].
The 2016 WHO diagnostic criteria newly recognized pre-PMF as a distinct entity of the MPNs. It is important to distinguish pre-PMF from ET because the two entities present with different clinical characteristics and pre-PMF carries a worse prognosis [25], but cautious discrimination is necessary because both entities can show thrombocytosis. Compared to ET patients, pre-PMF patients are known to show higher WBC counts, lower Hb levels, higher platelet counts, higher LDH levels, higher JAK2V617F allele burdens and higher frequency of splenomegaly [14]. However, comparison of the two entities based on driver mutations is limited. We compared JAK2V617F-mutated ET patients and JAK2V617F-mutated pre-PMF patients and found that the latter showed significantly lower Hb levels (p = 0.006), lower platelet counts (p = 0.004), higher LDH levels (p = 0.043) and higher JAK2V617F allele burdens (p = 0.036). JAK2V617F-mutated pre-PMF patients also showed a tendency of higher WBC counts (p = 0.200) and higher frequency of splenomegaly (p = 0.079) (Table S2). All of these findings with the exception of platelet counts are in line with previous reports comparing entire ET and pre-PMF groups [14], and suggest that even when the comparison is done restricted to JAK2V617F-mutated patients, the result is similar and further supports that ET and pre-PMF are separate entities.
Pre-PMF and overt PMF are basically considered to be a single entity only looked upon at different time points of the disease. Half of surviving pre-PMF patients are reported to proceed to overt PMF over a time of approximately 20 years [26]. Within JAK2V617F-mutated pre-PMF, JAK2V617F allele burdens did not differ significantly between pre-PMF and overt PMF patients. However, to our surprise, JAK2V617F-mutation frequencies of pre-PMF and overt PMF differed significantly, with pre-PMF patients showing higher mutations rates of JAK2V617F (pre-PMF: 78.3% vs overt PMF: 53.8%, p = 0.049) (data not shown). A smaller percentage of JAK2V617F mutation in overt PMF may suggest that pre-PMF patients with non-mutated JAK2V617F have higher myelofibrotic potential.
We demonstrate that mutational status has a large effect on clinical characteristics of MPN patients. The findings were basically in line with previous reports, and we confirm that Japanese MPN patients grouped by different mutation subtypes show similar characteristics as that of their Western counterparts. Additionally, we show that patient characteristics differ between ET and pre-PMF patients even when restricted to JAK2V617F-mutated patients, which further supports that ET and pre-PMF are two distinct entities.
References
Imai M, Araki M, Komatsu N. Somatic mutations of calreticulin in myeloproliferative neoplasms. Int J Hematol. 2017;105(6):743–7.
Klampfl T, Gisslinger H, Harutyunyan AS, Nivarthi H, Rumi E, Milosevic JD, et al. Somatic mutations of calreticulin in myeloproliferative neoplasms. N Engl J Med. 2013;369(25):2379–90.
Rumi E, Pietra D, Pascutto C, Guglielmelli P, Martínez-Trillos A, Casetti IC, et al. Clinical effect of driver mutations of JAK2, CALR, or MPL in primary myelofibrosis. Blood. 2014;124(25):2379–90.
Rumi E, Pietra D, Ferretti V, Klampfl T, Harutyunyan AS, Milosevic JD, et al. JAK2 or CALR mutation status defines subtypes of essential thrombocythemia with substantially different clinical course and outcomes. Blood. 2014;123(10):1544–51.
Morishita S, Komatsu N, Kirito K, Koda AH, Sekiguchi Y, Tsuneda S, et al. Alternately binding probe competitive PCR as a simple, cost-effective, and accurate quantification method for JAK2V617F allele burden in myeloproliferative neoplasms. Leuk Res. 2011;35(12):1632–6.
Rapado I, Albizua E, Ayala R, Hernández JA, Garcia-Alonso L, Grande S, et al. Validity test study of JAK2 V617F and allele burden quantification in the diagnosis of myeloproliferative diseases. Ann Hematol. 2008;87(9):741–9.
Takei H, Morishita S, Araki M, Edahiro Y, Sunami Y, Hironaka Y, et al. Detection of MPLW515L/K mutations and determination of allele frequencies with a single-tube PCR assay. PLoS One. 2014;9(8):1–8.
Shirane S, Araki M, Morishita S, Edahiro Y, Takei H, Yoo Y, et al. JAK2, CALR, and MPL mutation spectrum in japanese patients with myeloproliferative neoplasms. Haematologica. 2015;100(2):e46–8.
Pietra D, Rumi E, Ferretti VV, Di Buduo CA, Milanesi C, Cavalloni C, et al. Differential clinical effects of different mutation subtypes in CALR-mutant myeloproliferative neoplasms. Leukemia. 2016;30(2):431–8.
Arber DA, Orazi A, Hasserjian R, Borowitz MJ, Le Beau MM, Bloomfield CD, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–405.
Edahiro Y, Morishita S, Takahashi K, Hironaka Y, Yahata Y, Sunami Y. JAK2 V617F mutation status and allele burden in classical Ph-negative myeloproliferative neoplasms in Japan. Int J Hematol. 2014;99:625–34.
Kanda Y. Investigation of the freely available easy-to-use software “EZR” for medical statistics. Bone Marrow Transplant. 2012;2013(48):452–8.
Tefferi A, Rumi E, Finazzi G, Gisslinger H, Vannucchi AM, Rodeghiero F, et al. Survival and prognosis among 1545 patients with contemporary polycythemia vera: an international study. Leukemia. 2013;27(9):1874–81.
Rumi E, Boveri E, Bellini M, Pietra D, Ferretti VV, Antonio ES, et al. Clinical course and outcome of essential thrombocythemia and prefibrotic myelofibrosis according to the revised WHO 2016 diagnostic criteria. Oncotarget. 2017;8(60):101735–44.
Guglielmelli P, Rotunno G, Fanelli T, Pacilli A, Brogi G, Calabresi L, et al. Validation of the differential prognostic impact of type 1/type 1-like versus type 2/type 2-like CALR mutations in myelofibrosis. Blood Cancer J. 2015;5:e360.
Scott LM, Tong W, Levine RL, Scott MA, Beer PA, Stratton MR, et al. Exon 12 mutations in polycythemia vera and idiopathic erythrocytosis. N Engl J Med. 2007;356(5):459–68.
Passamonti F, Elena C, Schnittger S, Skoda RC, Green AR, Girodon F, et al. Molecular and clinical features of the myeloproliferative neoplasm associated with JAK2 exon 12 mutations. Blood. 2011;117(10):2813–6.
Passamonti F, Mora B, Giorgino T, Guglielmelli P, Cazzola M, Maffioli M, et al. Driver mutations’ effect in secondary myelofibrosis: an international multicenter study based on 781 patients. Leukemia. 2017;31(4):970.
Cabagnols X, Defour JP, Ugo V, Ianotto JC, Mossuz P, Mondet J, et al. Differential association of calreticulin type 1 and type 2 mutations with myelofibrosis and essential thrombocythemia: relevance for disease evolution. Leukemia. 2015;29(1):249–52.
Marty C, Pecquet C, Nivarthi H, El-Khoury M, Chachoua I, Tulliez M, et al. Calreticulin mutants in mice induce an MPL-dependent thrombocytosis with frequent progression to myelofibrosis. Blood. 2016;127(10):1317–24.
Tefferi A, Wassie EA, Guglielmelli P, Gangat N, Belachew AA, Lasho TL, et al. Type 1 versus Type 2 calreticulin mutations in essential thrombocythemia: a collaborative study of 1027 patients. Am J Hematol. 2014;89(8):121–4.
Hussein K, Bock O, Theophile K, von Neuhoff N, Buhr T, Schlué J, et al. JAK2 V617F allele burden discriminates essential thrombocythemia from a subset of prefibrotic-stage primary myelofibrosis. Exp Hematol. 2009;37(10):1186–93.
Vannucchi AM, Antonioli E, Guglielmelli P, Pardanani A, Tefferi A. Clinical correlates of JAK2V617F presence or allele burden in myeloproliferative neoplasms: a critical reappraisal. Leukemia. 2008;22(7):1299–307.
Shirane S, Araki M, Morishita S, Edahiro Y, Sunami Y, Hironaka Y, et al. Consequences of the JAK2V617F allele burden for the prediction of transformation into myelofibrosis from polycythemia vera and essential thrombocythemia. Int J Hematol. 2015;101(2):148–53.
Barbui T, Thiele J, Passamonti F, Rumi E, Boveri E, Ruggeri M, et al. Survival and disease progression in essential thrombocythemia are significantly influenced by accurate morphologic diagnosis: an international study. J Clin Oncol. 2011;29(23):3179–84.
Gisslinger H, Jeryczynski G, Gisslinger B, Wölfler A, Burgstaller S, Buxhofer-Ausch V, et al. Clinical impact of bone marrow morphology for the diagnosis of essential thrombocythemia: comparison between the BCSH and the WHO criteria. Leukemia. 2016;30(5):1126–32.
Acknowledgements
We thank Masaaki Noguchi (Juntendo Urayasu Hospital), Michiaki Koike (Juntendo shizuoka Hospital) and Takao Hirano (Juntendo Nerima Hospital) for providing patient specimens and clinical data; Satoshi Tsuneda and Yuji Sekiguchi for their generous support and encouragement; Kyoko Kubo, Kazuko Kawamura, and Megumi Hasegawa for their superb secretarial assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
This study was carried out as a research program of the Project for Development of Innovative Research on Cancer Therapeutics (P-Direct), The Japan Agency for Medical Research and Development, and Ministry of Education, Culture, Sports, Science and Technology of Japan. Part of this work was supported by Japan Society for the Promotion of Science KAKENHI Grant #17H04211. The authors have no conflict of interest to declare.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12185_2018_2421_MOESM1_ESM.docx
Table S1. Clinical characteristics of JAK2V617F-mutated and triple-negative pre-PMF patients. ET: essential thrombocythemia; pre-PMF: prefibrotic primary myelofibrosis. WBC: white blood cell; Hb: hemoglobin Hct: hematocrit; LDH: lactate dehydrogenase. For continuous variables, data are shown as median values and brackets represent range. For categorical variables, right side of / represents the total number of patients studied and left side represents the number of positive patients, and brackets represent positive percentages. *There was only one CALR-mutated pre-PMF patient, and thus was removed from analysis here (DOCX 15 kb)
12185_2018_2421_MOESM2_ESM.docx
Table S2. Clinical characteristics of JAK2V617F-mutated ET and JAK2V617F-mutated pre-PMF patients. JAK2-ET: JAK2V617F-mutated essential thrombocythemia; JAK2-pre-PMF: JAK2V617F-mutated prefibrotic primary myelofibrosis. WBC: white blood cell; Hb: hemoglobin; Hct: hematocrit; LDH: lactate dehydrogenase. For continuous variables, data are shown as median values and brackets represent range. For categorical variables, right side of / represents the total number of patients studied and left side represents the number of positive patients, and brackets represent positive percentage (DOCX 15 kb)
About this article
Cite this article
Misawa, K., Yasuda, H., Araki, M. et al. Mutational subtypes of JAK2 and CALR correlate with different clinical features in Japanese patients with myeloproliferative neoplasms. Int J Hematol 107, 673–680 (2018). https://doi.org/10.1007/s12185-018-2421-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-018-2421-7