Abstract
Background
This study was designed to assess the value of a combinatorial protocol, namely, stress only myocardial perfusion SPECT (MPS), 64-slice coronary computed tomographic angiography (CTA), and SPECT/CTA 3-dimensional (3D) fusion imaging for the evaluation of coronary artery disease.
Methods
A total of 142 patients were retrospectively reviewed. All underwent stress only MPS and 64-slice CTA before invasive coronary angiography (ICA). The SPECT/CTA 3D fusion images were generated. We compared the results of the combinatorial protocol with ICA.
Results
Seventy nine (76.0%) subjects were found to have ≥50% stenoses, by ICA. The sensitivity of the combinatorial examination was 100% and its specificity 80.8%. Its positive and negative predictive values were 94.0 and 100%, respectively. The number of lesion for abnormal MPS with matching significant stenoses on CTA is 94 [43 in left anterior descending (LAD); 19 in left circumflex (LCX); 32 in right coronary artery (RCA)], the number of lesion for equivocal perfusion defect with matching stenoses on CTA is 24 (14 in LAD; 7 in LCX; 3 in RCA). The number of coronary arterial stenoses without MPS abnormality is 10, 4 stenoses were detected in left main lesion and the other stenoses were comparatively mild lesion in multi-vessel disease.
Conclusion
Stress only MPS/CTA 3D fusion imaging could provide the potential for improved diagnostic accuracy and additional information of hemodynamically relevant coronary arterial stenoses.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Numerous modalities are available for evaluating ischemic heart disease. Currently, myocardial perfusion single photon emission computed tomography (SPECT) and coronary computed tomography angiography (CTA) are among the methods most commonly used for coronary investigations. Myocardial perfusion SPECT (MPS) provides a non-invasive means of identifying patients with coronary artery disease (CAD) and determining cardiovascular prognosis. MPS findings, such as, the extent, severity, and reversibility of perfusion defects, predict future fatal and non-fatal cardiovascular events [1–3]. Furthermore, a previous study showed that MPS provides substantially more prognostic information than invasive coronary angiography (ICA) [2]. CTA is an anatomic imaging method that is used for evaluating CAD and is highly accurate at detecting coronary arterial stenoses [4–6]. In addition, CTA may provide complementary information, rather than overlapping diagnostic information, when applied with MPS [7–10].
Nowadays, many investigators are interested in ‘one-stop’ assessments. In particular, clinicians await a single diagnostic modality capable of accurately assessing myocardial perfusion and anatomical disorders. Furthermore, it is also important that standard protocols be modified to reduce the costs, time requirements, and the side effects of diagnostic tests. The SPECT/CTA 3-dimensional (3D) fusion images may prove to be important in terms of diagnostic and therapeutic decision making in different clinical scenarios [11, 12]. It is believed likely that fusion imaging will allow therapies to be more precisely tailored, reduce healthcare costs, and have better patient outcomes in the near future.
We hypothesized that combinatorial stress only MPS, 64-slice coronary CTA, and SPECT/CTA 3D fusion imaging would provide a non-invasive, reliable means of evaluating coronary artery stenoses extent, distribution, location, and composition, and thus, enable evaluation of hemodynamic relevance of coronary artery stenoses. In the present study, we compared the results of the combinatorial protocol with presence of narrowing of the coronary luminal diameter >50% in ICA.
Subjects and methods
Study population
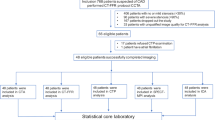
We retrospectively identified consecutive patients referred to our nuclear medicine department for evaluation of CAD by ICA within 2 months period from May 2007 to August 2008. There was no coronary event between the time of the combinatorial protocol and ICA. All patients enrolled in this study underwent both stress MPS and enhanced 64-slice CTA prior to the invasive procedure. One hundred forty-two patients with typical or atypical anginal syndrome without myocardial infarction were considered for entry into study. Exclusion criteria were severe obstructive lung disease, known intolerance to iodinated contrast agents and previous stent or coronary artery bypass graft surgery. And also, we excluded the patients with old myocardial infarction history or showed ST elevation on electrocardiography (ECG) or increased cardiac enzyme at this study which we could suspected acute myocardial infarction. Patients’ clinical characteristics were obtained by clinical history taking prior to imaging by a nuclear physician. A written informed consent was obtained from each patient in accordance with the guidelines on human investigations as established by the internal review board of Yeung-nam University, Daegu, Republic of Korea. The study protocol was approved by our institutional review board.
Stress only MPS
Stress was induced pharmacologically in each patient by an intravenous infusion of adenosine (6 min infusion at 140 μg/kg/min). Standard ECG, vital signs, and general condition were continuously monitored during the stress protocol. Three minutes after the continuous infusion of adenosine, 370 MBq of 99mTc-sestamibi was injected and flushed with saline. SPECT was performed 60 min after the stress test.
MPS images were acquired using a two headed SPECT system (Hawkeye or Infinia; GE Healthcare, Milwaukee, WI, USA) using a low-energy, high-resolution collimator, a 20% symmetric window at 140 keV, a 64 × 64 matrix, an elliptic orbit with step-and-shoot acquisition at 3° intervals over 180°, and a 30 s dwell time per stop. Acquisitions were gated at 8 frames per R-R cycle with a 50% window of acceptance. For all patients, the summed non-gated SPECT image set was reconstructed at a dedicated workstation (eNTEGRA or Xeleris; GE Medical Systems, Milwaukee, WI, USA) using an iterative reconstruction algorithm (ordered- subset expectation maximization using two iterations and 10 subsets). No scatter or attenuation correction was applied.
Coronary CTA
A 64-channel multidetector CT (DVCT; GE Healthcare, Milwaukee, WI, USA) was used using the following scanning parameters: ECG-triggered X-ray tube modulation, 64-channel detectors along the z-axis, a tube voltage of 120 kV, a tube current of 350–650 mA (depending on patient size), a scan field of view of 25 cm, a gantry rotation of 0.35 s per rotation, a matrix of 512 × 512, a slice width of 0.625 mm, and a helical pitch of 0.16.
A single oral dose of 25–50 mg metoprolol tartrate (Betaloc®; Yuhan Corporation, Seoul, Republic of Korea) was administrated 1 h before CTA if the patient’s heart rate was ≥65 beats per minute. Patients were scanned in a fasted and asymptomatic state in the supine position, and received 1.25–2.5 mg of sublingual isosorbid dinitrate (Isoket® Spray; Schwarz Pharma, Munchenstein, Switzerland) prior to scanning. After 2 localization scans, a low-dose native scan of the heart was performed for coronary calcium detection and scoring. For CTA, 80 mL of iodixanol (Visisense® 320 mg I/mL; Taejoon Pharma, Seoul, Republic of Korea) at a flow rate of 4 mL/s followed by 50 mL saline solution was injected into an antecubital vein via an 18-gauge catheter. Bolus tracking was performed with a region of interest placed into the ascending aorta.
Coronary artery calcium scoring
Coronary artery calcium (CAC) scoring was performed on the gated non-contrast images acquired prior to CTA and analyzed using GE Advantage Workstation 4.4 with Smartscore software. Electrocardiographically triggered, sequential step-and-shoot acquisition mode, with 120 kV tube voltage, 430 mA tube current, and 2.5 mm slice thickness, was performed for calcium detection and quantification by the Agatston method. Patients were considered to have minimal to no CAD burden if their CAC was <100, mild-moderate CAD burden if the CAC was 100–399, and substantial CAD burden if CAC was ≥400.
ICA
ICA was performed using a routine protocol. Images were evaluated by consensus between 2 experienced interventional cardiologists who were both unaware of clinical histories and the combinatorial examination results. A minimum of 8 projections were obtained [minimum of 5 views of the left coronary artery system and a minimum of 3 views of the right coronary artery (RCA) system].
The coronary artery tree was subdivided according to AHA guidelines, and each vessel was visually evaluated with regard to vessel border delineation on at least 2 different projections. Stenoses of ≥50% was considered a significant coronary lesion.
Images interpretation and analysis
Stress only MPS images
MPS interpretations were performed by consensus between 2 nuclear physicians who were unaware to clinical histories—on short-axis, horizontal long-axis, and vertical long-axis sections and semiquantitative polar maps of perfusion. A cine display of rotating planar projections was to assess sub-diaphragmatic activities, attenuations, and patient motion to optimize image quality. In addition, polar maps of perfusion, wall motion, and wall thickening were produced using a commercially available software package (Cedars QGS/QPS; Cedars-Sinai Medical Center, Los Angeles, CA, USA). Anterior and septal wall perfusion defects were allocated to the left anterior descending (LAD) coronary artery, lateral defects were allocated to the left circumflex (LCX) coronary artery, and inferior defects were allocated to the RCA. In watershed regions, allocations were determined based on main defect extension into the lateral, anterior, or inferior walls. And also, a summed stress score (SSS) was obtained by adding the scores of the 20 segments of the stress MPS by visual analysis with a 5-point scale (0 = normal uptake, 1 = mild hypoperfusion, 2 = moderate hypoperfusion, 3 = severe hypoperfusion and 4 = no uptake). The scoring results were classified into the following 4 groups: normal for scores <4, mildly abnormal for scores 4–8, moderately abnormal for scores 9–13, and severely abnormal for scores >13 [1, 3].
Coronary CTA
Coronary CTA images were analyzed by the same 2 observers that analyzed the stress only MPS images. All CTA images were evaluated on a 3D image analysis workstation (Advantage Workstation 4.4, GE Healthcare, Milwaukee, WI, USA). The readers were permitted to use any or all of the available postprocessing image reconstruction algorithms, including 2D axial and 3D maximal intensity projection, multiplanar reformatting, cross-sectional analysis, and volume-rendered techniques. An overall assessment of image quality was performed at the subject level. Image quality for each data set was rated by consensus using a previously published 5-point ranking scale [8]. In detail, a score of 1 indicated no motion artifacts and clear delineation of the segment; a score of 2, minor artifacts and mild blurring of the segment; a score of 3, moderate artifacts and moderate blurring without structure discontinuity; a score of 4, severe artifacts and doubling or discontinuity during the course of the segment; and a score of 5, a non-evaluable image with non-differentiable vessel structures. A significant stenosis was defined as narrowing of the coronary diameter by ≥50%. Consensus was achieved on per-patient and per-vessel basis in all cases.
SPECT/CTA 3D fusion image
Initially, the 2 nuclear physicians analyzed stress MPS and CTA images side-by-side with regard to functionally relevant coronary stenoses, and then produced SPECT/CTA 3D fusion images on a workstation (Advantage workstation 4.4, GE Healthcare) using the CardIQ Fusion software package, and identified suspect coronary lesions. (We did not make fusion image at all negative result in both stress only MPS and CTA). The SPECT/CTA 3D fusion images were analyzed with respect to coronary lesions. First, diagnostic information was obtained on new lesions missed during side by side analysis of stress only MPS and CTA. Second, anatomic relationships between perfusion defects and coronary vessels were documented. It took about 5–10 min to make fusion images.
Data analysis
The positive criteria were abnormal MPS with matching significant stenoses on CTA, equivocal perfusion defect with matching abnormal (or equivocal) stenoses on CTA and definite narrowing of the coronary diameter without MPS abnormality. Equivocal myocardial perfusion defect was defined as stress induced 2 or 3 myocardial segments with perfusion score = 1 or 1 segment with score = 2. And the ischemia was regarded as stress induced 2 or more myocardial segments with perfusion score ≥2. For patient-based analysis, true-positive was defined as the presence of ≥1 coronary artery with significant stenoses by the combinatorial examination and ICA, irrespective of location. For vessel-based analysis, a true-positive was defined as the presence of ≥1 coronary artery segment considered to have a significant stenoses by the combinatorial examination and ICA in a single arterial system. The 4 arterial systems examined were: (1) the left main artery; (2) the LAD inclusive of its diagonal branches; (3) the LCX inclusive of its obtuse marginal and left-sided posterolateral branches; and (4) the RCA inclusive of the posterior descending artery and right-sided posterolateral branches. Ramus intermediate arteries were considered as first obtuse marginal branches for per-vessel analyses.
Statistical analysis
Continuous variables were expressed as mean ± SD. Proportions were expressed as percentage.
Patient characteristics were compared using the correlation analysis and one-way ANOVA. The χ2 test was to analyze continuous and categoric variables, respectively. p values of < 0.05 were considered statistically significant. Statistical analysis was performed using PASW ver. 18.0 software (SPSS Inc, Chicago. IL, USA).
Results
Patient characteristics
The present study aimed at including 142 consecutive patients. After initial assessment 38 patients did not meet the inclusion criteria, because CTA was not feasible due to non-diagnostic CTA image (due to breathing artifact or motion artifact including arrhythmia during CTA acquisition). One hundred and four patients, of which 39.4% (n = 41) were women and 60.6% (n = 63) were men, were retrospectively recruited to participate in this study. Patients’ coronary risk factors were hypertension (n = 54), dyslipidemia (n = 44), cigarette smoking (n = 34), and diabetes mellitus (n = 32). The clinical diagnoses of the study patients were unstable angina (n = 16), effort angina (n = 70), variant angina (n = 8), and others (n = 10). The median time between stress only MPS and CTA was 0 days (range 0–1 day), and that between CTA and ICA was 10.0 ± 13.7 days. All stress only MPS and CTA studies were performed prior to ICA (Table 1). Four patients had left main vessel stenoses, except the 4 patients, among the other 100 patients were consisted with 43 patients of 1 vessel disease, 20 patients of 2 vessel disease, 12 patients of 3 vessel disease and 25 patients of no significant stenoses.
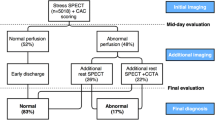
Patient-based analysis
Seventy nine (76.0%) subjects were found to have ≥50% stenoses, by ICA. Of the 79 patients with ≥50% stenoses by ICA, all patients were correctly identified as having ≥50% stenoses by the combinatorial examination. The sensitivity of the combinatorial examination was 100% and its specificity 80.8%. Its positive (PPV) and negative predictive values (NPV) were 94.0 and 100%, respectively.
Vessel-based analysis
In total, 131 (31.5%) vessels reached the 50% stenoses threshold by ICA. Among the vessels with ≥50% stenoses by ICA, 128 were correctly identified as having ≥50% stenoses by the combinatorial examination. The sensitivity of the combinatorial examination was 97.7%, its specificity 96.1%, PPV 92.1%, and NPV 98.9%.
Except the left main stenoses, the combinatorial protocol in the patients with 1 vessel (129 coronary arteries of 43 patients) had a sensitivity of 100%, specificity 97%, PPV 93%, and NPV 100% for detecting stenotic lesions. In addition, the performance of combinatorial protocol to detect stenotic lesion showed sensitivity, specificity, PPV, and NPV of 96, 95, 99, and 86%, respectively, in the patients with multiple vessel disease.
The number of lesion for abnormal MPS with matching significant stenoses on CTA is 94 (43 in LAD; 19 in LCX; 32 in RCA), the number of lesion for equivocal perfusion defect with matching stenoses on CTA is 24 (14 in LAD; 7 in LCX; 3 in RCA). The characteristics of later group was not definite perfusion defect in MPS but showed mild perfusion defect with corresponding coronary stenoses on SPECT/CTA 3D fusion image. The number of coronary arterial stenoses without MPS abnormality is 10, of which 4 stenoses were detected in left main lesion and the other stenoses were comparatively mild lesion in multi-vessel disease. Then, the cases of only perfusion defect without corresponding arterial stenoses were 26, gave consideration to attenuation artifact (Table 2).
SSS
MPS images during stress were normal (SSS < 4) in 43 (41.3%) patients. A mild abnormal MPS (4 ≤ SSS ≤ 7) was present in 42 (40.4%) patients, moderate abnormal MPS (8 ≤ SSS ≤ 12) was present in 10 (9.6%) patients and severely abnormal MPS (13 ≤ SSS) was present in 9 (8.7%) patients. Significant CAD with lesions ≥50% stenoses was observed in 28 patients (1 vessel disease in 19 patients; 2 vessel disease in 3 patients; 3 vessel disease in 4 patients; left main stenoses in 2 patients) with normal SSS.
Severely abnormal MPS was higher in patients with high Framingham risk score (r = 0.206; p = 0.036). And coronary artery calcium scores was significantly higher in patients with a severely abnormal MPS by Pearson’s correlation analysis (r = 0.202; p = 0.040). Numbers of stenotic arteries were found to be positively correlated with the presence of a severe perfusion defect by MPS resulting from one-way ANOVA test (p = 0.01).
Calcium scores
We examined baseline CAC scores. The prevalence of CAC score = 0, 1 ≤ CAC score ≤ 100, 101 ≤ CAC score ≤ 400, and 401 ≤ CAC score was 22.1% (n = 23), 22.1% (n = 23), 26.0 (n = 27), and 29.8 (n = 31), respectively. CAC scores dichotomized by ≤400 and >400 Agatston units, the specificity and PPV of combinatorial examination in the group of CAC score >400 were 91.7 and 94.1% compared to 95.1 and 90.6% in the group of CAC score ≤400 on the vessel based analysis. Difference had no statistical significance (p > 0.05).
CAC score had positive correlation with number of stenotic arteries by one-way ANOVA test (p < 0.01).
Discussion
The main finding of this study is that a combinatorial protocol, namely, stress only MPS, 64-slice coronary CTA, and SPECT/CTA 3D fusion imaging are practicable to accurate diagnoses and intuitive assurance of CAD. The SPECT/CTA 3D fusion imaging component provides complementary information on anatomic disorders and their functional relevance, and aids treatment planning of individual patients. Figure 1 shows an example of improved presentation with the SPECT/CTA 3D fusion image, MPS showed mild perfusion defect in the anterior wall and inferior wall but the SPECT/CTA 3D fusion images were read as positive for 3 vessel disease. The strong point of this study, is the near perfect alignment of coronary artery anatomy and myocardial perfusion. We closely examined arteries that supplied areas showing perfusion reduction. SPECT/CTA 3D fusion imaging enabled the extent of functionally relevant ischemic areas to be visualized and enabled the lengths and locations of stenotic coronary arteries to be determined. If a patient has more than 2 stenotic lesions, SPECT/CTA 3D fusion imaging provides the 3D relationship between ischemic lesions and indicate the culprit segment, which can provide a treatment order when multiple lesions are encountered. In case of Fig. 1, the patient has 3 vessel disease and more severe perfusion defect in anterior and inferior wall than lateral wall. It indicates therapeutic order with weighty, moreover the stenotic site and length. Accordingly, SPECT/CTA 3D fusion imaging aids therapeutic planning and may eliminate the risks posed by diagnostic ICA and reduce times to therapeutic intervention.
Example of fusion image in a 72-year-old female patient with three vessel disease. a Short axis, vertical and horizontal long axis slices of the stress myocardial perfusion image. This perfusion study was read as mild perfusion defect in the anterior wall and inferior wall. b Polar map of the same SPECT study. c Curved multiplanar reconstruction of the LCX on CT angiography showing a plaque at bifurcation. This was read as additional LCX stenoses. d Coronary calcium scoring—Agaston score: 2451. e–g Three dimensional volume rendered SPECT/CTA fusion images; the darker color area on the SPECT/CTA fusion image identified a region of myocardial ischemia during stress. These SPECT/CTA fusion images showed perfusion defect in the apex and the anterior wall corresponding to the vascular territory of the LAD; basal lateral wall corresponding to the vascular territory of the LCX; inferior wall corresponding to the vascular territory of the RCA. The fusion of anatomic (CTA) and functional (myocardial perfusion imaging) images indicated that 3 vessel disease and relatively better perfusion in the territory of LCX
Regarding CTA, to reduce radiation exposure in our study, ECG-triggered X-ray tube modulation was used in all patients. This technique allows a reduction in radiation exposure of up to 50% and can be used at all phases for coronary reconstruction in the presence of blurring or step artifact, and it can also be used in cases of arrhythmia [13]. Even though we injected only 370 MBq of 99mTc-sestamibi for MPS, we obtained satisfactory image quality. The total radiation exposure from the combinatorial protocol was lower radiation dosages than current 201Tl (148 MBq) and this protocol maintain the high diagnostic accuracy.
Recent studies that have compared 64-slice CTA and ICA have documented high sensitivity (73–100%) and specificity (90–97%) for CTA for the detection of coronary artery stenoses [4, 14, 15]. Furthermore, CTA was also found to detect subclinical atherosclerosis, which did not exhibit perfusion abnormalities by MPS [10]. The other decisive merit of CTA is its ability to detect left main arterial lesions and multiple vessel disease, which may show balanced perfusion defects on MPS [6]. In our study, all of 4 patients with left main stenosis could not be expected by MPS images alone. We anticipated the main arterial stenoses based on the CTA. However, CTA has important defects, such as, motion artifacts and the artifacts produced by heavy calcifications, which may interfere with accurate evaluations [14]. In the present study, MPS identified the existence of ischemia, therefore, its sensitivity and specificity were preserved in patients with massive calcified plaque. Totally 31 patients showed heavy calcification (>400) and except 3 patients who had left main disease, all of 48 coronary arterial stenoses in 28 patients were correctly diagnosed. The specificity was 91.7% and PPV was 94.1%.
Myocardial perfusion imaging with radioactive tracer is a well-established modality for the diagnosis and prognostic assessment of patients with known or suspected CAD, and thus, may be useful for cardiac risk stratification and as a therapeutic decision making aid [1–3, 16]. SSS is commonly used to demonstrate the extent and severity of perfusion decreases and provides a means of risk stratification [3, 17]. Recently, van Werkhoven et al. showed that increased SSS was strong significant predictor of event. So, the stress only MPS in this study is useful enough for many CAD cases [18]. In the present study, we used stress only MPS and no rest study. The majority of previous studies have found satisfactory agreement between gated stress only MPS and the standard protocol [19–21]. And also, Gibson et al. [19] demonstrated that stress only imaging in patients with low to medium probability roled safe, time- and cost- efficient imaging modality. In our study, we excluded the patients with a possibility of myocardial infarction therefore we could omit the rest MPS. However, if the patients had a possibility of myocardial infarction, the rest imaging might be needed to identify the reversibility of the perfusion defect at stress imaging.
As a result, patients with high probability of CAD were enrolled, postselect bias might contribute high sensitivity to some degree. However, the specificity and NPV were also good. So the SPECT/CTA 3D fusion protocol was useful in the patients with high probability.
In an initial comparison of CTA and MPS conducted when CTA was first introduced, it was found that a large discrepancy existed between the anatomic extent of CAD and ischemia, and that many stenoses did not cause abnormal perfusion [10, 22]. Recently, although several studies have suggested to use compensatory imaging studies in CAD, it still remains undetermined which sequences and methods should be adopted, and what benefits are obtained by performing non-invasive coronary imaging studies. Atherosclerosis by CTA did not exhibit perfusion abnormalities on MPS, which indicates that atherosclerosis frequently does not result in ischemia. Gaemperli et al. [23] demonstrated that 64-slice CTA had a high NPV in an intermediate to high-risk population. However, an abnormal CTA is a poor predictor of ischemia, and therefore, MPS is necessary to consider the optimal treatment of revascularization procedure or conservative management and risk modification [22, 24]. Accordingly, CTA and MPS provide complementary rather than repetitious information, because the techniques reflect distinct functional and anatomic pathophysiologic processes. Therefore, the present study reaffirms the complementary role of these 2 imaging studies, and supplements these with the additional benefit of fusion images. In presented study, by extension, equivocal perfusion defect was conversion to true ischemia on fusion image in 24 coronary arterial steonsis, especially in multivessel disease patients. It is different result between side by side and SPECT/CTA 3D fusion to find out hemodynamic relationship between coronary stenoses and perfusion defect, especially mild perfusion defect. On the contrary, the cases of perfusion defect without critical coronary stenoses on CTA have positive effect that could avoid unnecessary invasive procedure but might miss true lesion such as microvascular angina [25]. But in presented study, we had no patient who suffered from micorvascular angina.
Treatment strategies in patients with suspected or known CAD are determined by integrating both the extent and severity of anatomic stenoses and functional relevance [26]. In a recent study, a stepwise increase in the incidence of perfusion defects on MPS was observed to be related to the severities of stenoses on CTA [9]. These findings explain the relationship between the severity of stenoses on CTA and hemodynamic consequences as assessed by MPS [9]. Our analysis also showed that number of stenotic arteries were proportional to SSS. Severe reductions in coronary flow reserve show photon defect on MPS, while modest reductions in flow reserve, may not result in detectable defects [27]. Thus, abnormal findings on CTA do not necessarily result in abnormal MPS findings, but may more frequently represent non-obstructive atherosclerosis. Therefore, in patients with abnormal CTA findings, functional testing is required to determine the hemodynamic consequences of identified abnormalities. Myocardial perfusion studies involve assessments of how stenoses defined by CTA affects coronary supply [11, 28]. Due to variations in stenoses length, composition, and location, and to the presence or absence of collateral vessels, stenoses as determined by only MPS or only CTA is probably inadequate for therapeutic decision-making.
Several recent studies addressed the use of MPS and CTA images to investigate the incremental value of fusion image for the diagnosis of CAD. In those studies by Rispler et al. [29] and by Santana et al. [30], targeted both stress and rest MPS with CTA and older fashion of fusion software. They also showed high diagnostic accuracy and important information about functionally significant coronary lesion. But our study excluded rest MPS and used the lastest CTA with fusion software still maintained the high diagnostic accuracy and lowering radiation dose. The study by Husmann et al. [28] showed possibility of lowering radiation dose, maintaining diagnostic sensitivity and information about functionally significant coronary lesion using stress only fusion imaging with prospective electrocardiogram-trigger. Difference between the study by Husmann and this study is that our study population had more coronary stenoses (i.e., higher probability group) and showed higher specificity and PPV (96.1 vs. 84% in specificity, 92.1 vs. 30% in PPV). That was probably due to their study compared with stress and rest MPS as reference standard. Most recent report by Matsuo et al. [31] showed that cardiac SPECT/CTA fusion imaging from different manufacturers accurately diagnosed functionally relevant coronary stenoses, especially the incremental diagnostic information on SPECT/CTA fusion had significant smaller coronary artery size than that of not-improved coronary vessels. Unfortunately, we did not perform segmental analysis, could not compare the results, but the two fusion study found common results such as provide added diagnostic information on functional relevance of CAD and identification of culprit lesion.
Our study had several limitations. First, there are shortcomings regarding the use of ICA as a reference standard for functional relevant coronary stenoses. An obstacle when evaluating the diagnostic performance of comprehensive fusion imaging is the inadequacy of a relevant gold standard. Although ICA is widely accepted as the gold standard for CAD assessment it remains absolutely anatomic and lacks information on functional relevance of coronary stenoses. Conversely, the results that adding CTA to MPS improves accuracy is not amazing using the gold standard of ICA, as an anatomic test compares better to another anatomic test. Paradoxically, the information on functional status is important, however, the incremental information is lost if the gold standard is ICA. This conceptual problem is the basic dilemma using fusion imaging and thus, further long-term follow-up for cardiac events or ICA with fractional flow reserve measurements is required. Second, the study population consisted of patients with various clinical presentations, which included both suspected and known CAD, and undoubtedly, a more homogeneous cohort would have provided more uniform results. The third, the addition of CTA to MPS suggested a substantially higher radiation dose for the patient under analysis. The total radiation exposure from the combine MPS and retrospective ECG gating CTA study was estimated at 20 mSv. However, SPECT/CTA fusion imaging was associated with lower radiation dosages than current 201Tl (148 MBq) and dual-isotope thallium–99m Tc SPECT protocols. The new technique with prospective triggering CTA, new reconstructed MPS would ensure low effective radiation dose.
Conclusions
Patients referred for CAD underwent the combinatorial protocol, namely, stress only MPS, 64- slice CTA, and SPECT/CTA 3D fusion imaging, and findings were compared with ICA. Our results support that the combinatorial examination for CAD is accurate and regarding no need for the rest MPS, it can be more convenient, less time-consuming, less expensive and moreover with less radiation burden to the patients. The described combinatorial study protocol could promise the utility of a comprehensive non-invasive CAD assessment, which includes both anatomic and functional information.
References
Hachamovitch R, Berman DS, Shaw LJ, Kiat H, Cohen I, Cabico JA, et al. Incremental prognostic value of myocardial perfusion single photon emission computed tomography for the prediction of cardiac death: differential stratification for risk of cardiac death and myocardial infarction. Circulation. 1998;97:535–43.
Iskandrian AS, Chae SC, Heo J, Stanberry CD, Wasserleben V, Cave V. Independent and incremental prognostic value of exercise single-photon emission computed tomographic (SPECT) thallium imaging in coronary artery disease. J Am Coll Cardiol. 1993;22:665–70.
Hachamovitch R, Berman DS, Kiat H, Cohen I, Cabico JA, Friedman J, et al. Exercise myocardial perfusion SPECT in patients without known coronary artery disease: incremental prognostic value and use in risk stratification. Circulation. 1996;93:905–14.
Pugliese F, Mollet NR, Runza G, van Mieghem C, Meijboom WB, Malagutti P, et al. Diagnostic accuracy of non-invasive 64-slice CT coronary angiography in patients with stable angina pectoris. Eur Radiol. 2006;16:575–82.
Budoff MJ, Dowe D, Jollis JG, Gitter M, Sutherland J, Halamert E, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (assessment by coronary computed tomographic angiography of individuals undergoing invasive coronary angiography) trial. J Am Coll Cardiol. 2008;52:1724–32.
Ropers D, Baum U, Pohle K, Anders K, Ulzheimer S, Ohnesorge B, et al. Detection of coronary artery stenoses with thin-slice multi-detector row spiral computed tomography and multiplanar reconstruction. Circulation. 2003;107:664–6.
Gaemperli O, Schepis T, Koepfli P, Valenta I, Soyka J, Leschka S, et al. Accuracy of 64-slice CT angiography for the detection of functionally relevant coronary stenoses as assessed with myocardial perfusion SPECT. Eur J Nucl Med Mol Imaging. 2007;34:1162–71.
Hacker M, Jakobs T, Hack N, Nikolaou K, Becker C, von Ziegler F, et al. Sixty-four slice spiral CT angiography does not predict the functional relevance of coronary artery stenoses in patients with stable angina. Eur J Nucl Med Mol Imaging. 2007;34:4–10.
Schuijf JD, Wijns W, Jukema JW, Decramer I, Atsma DE, de Roos A, et al. A comparative regional analysis of coronary atherosclerosis and calcium score on multislice CT versus myocardial perfusion on SPECT. J Nucl Med. 2006;47:1749–55.
Schuijf JD, Wijns W, Jukema JW, Atsma DE, de Roos A, Lamb HJ, et al. Relationship between noninvasive coronary angiography with multi-slice computed tomography and myocardial perfusion imaging. J Am Coll Cardiol. 2006;48:2508–14.
Gaemperli O, Schepis T, Valenta I, Husmann L, Scheffel H, Duerst V, et al. Cardiac image fusion from stand-alone SPECT and CT: clinical experience. J Nucl Med. 2007;48:696–703.
Mahmarian JJ. Combining myocardial perfusion imaging with computed tomography for diagnosis of coronary artery disease. Curr Opin Cardiol. 2007;22:413–21.
Trabold T, Buchgeister M, Kuttner A, Heuschmid M, Kopp AF, Schroder S, et al. Estimation of radiation exposure in 16-detector row computed tomography of the heart with retrospective ECG-gating. Rofo. 2003;175:1051–5.
Raff GL, Gallagher MJ, O’Neill WW, Goldstein JA. Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol. 2005;46:552–7.
Mollet NR, Cademartiri F, van Mieghem CA, Runza G, McFadden EP, Baks T, et al. High-resolution spiral computed tomography coronary angiography in patients referred for diagnostic conventional coronary angiography. Circulation. 2005;112:2318–23.
Iskander S, Iskandrian AE. Risk assessment using single-photon emission computed tomographic technetium-99m sestamibi imaging. J Am Coll Cardiol. 1998;32:57–62.
Leslie WD, Tully SA, Yogendran MS, Ward LM, Nour KA, Metge CJ. Prognostic value of automated quantification of 99mTc-sestamibi myocardial perfusion imaging. J Nucl Med. 2005;46:204–11.
van Werkhoven JM, Schuijf JD, Gaemperli O, Jukema JW, Boersma E, Wijns W, et al. Prognostic value of multislice computed tomography and gated single-photon emission computed tomography in patients with suspected coronary artery disease. J Am Coll Cardiol. 2009;53:623–32.
Gibson PB, Demus D, Noto R, Hudson W, Johnson LL. Low event rate for stress-only perfusion imaging in patients evaluated for chest pain. J Am Coll Cardiol. 2002;39:999–1004.
Heller GV, Bateman TM, Johnson LL, Cullom SJ, Case JA, Galt JR, et al. Clinical value of attenuation correction in stress-only Tc-99m sestamibi SPECT imaging. J Nucl Cardiol. 2004;11:273–81.
Santana CA, Garcia EV, Vansant JP, Krawczynska EG, Folks RD, Cooke CD, et al. Gated stress-only 99mTc myocardial perfusion SPECT imaging accurately assesses coronary artery disease. Nucl Med Commun. 2003;24:241–9.
Hacker M, Jakobs T, Matthiesen F, Vollmar C, Nikolaou K, Becker C, et al. Comparison of spiral multidetector CT angiography and myocardial perfusion imaging in the noninvasive detection of functionally relevant coronary artery lesions: first clinical experiences. J Nucl Med. 2005;46:1294–300.
Gaemperli O, Schepis T, Valenta I, Koepfli P, Husmann L, Scheffel H, et al. Functionally relevant coronary artery disease: comparison of 64-section CT angiography with myocardial perfusion SPECT. Radiology. 2008;248:414–23.
Hachamovitch R, Hayes SW, Friedman JD, Cohen I, Berman DS. Comparison of the short-term survival benefit associated with revascularization compared with medical therapy in patients with no prior coronary artery disease undergoing stress myocardial perfusion single photon emission computed tomography. Circulation. 2003;107:2900–7.
Wilson RF, Johnson MR, Marcus ML, Aylward PE, Skorton DJ, Collins S, et al. The effect of coronary angioplasty on coronary flow reserve. Circulation. 1988;77:873–85.
Topol EJ, Nissen SE. Our preoccupation with coronary luminology: the dissociation between clinical and angiographic findings in ischemic heart disease. Circulation. 1995;92:2333–42.
Yoshinaga K, Katoh C, Noriyasu K, Iwado Y, Furuyama H, Ito Y, et al. Reduction of coronary flow reserve in areas with and without ischemia on stress perfusion imaging in patients with coronary artery disease: a study using oxygen 15-labeled water PET. J Nucl Cardiol. 2003;10:275–83.
Husmann L, Herzog BA, Gaemperli O, Tatsugami F, Burkhard N, Valenta I, et al. Diagnostic accuracy of computed tomography coronary angiography and evaluation of stress-only single-photon emission computed tomography/computed tomography hybrid imaging: comparison of prospective electrocardiogram-triggering vs retrospective gating. Eur Heart J. 2009;30:600–7.
Rispler S, Keidar Z, Ghersin E, Roguin A, Soil A, Dragu R, et al. Integrated single-photon emission computed tomography and computed tomography coronary angiography for the assessment of hemodynamically significant coronary artery lesions. J Am Coll Cardiol. 2007;49:1059–67.
Santana CA, Garcia EV, Faber TL, Sirineni GK, Esteves FP, Sanyal R, et al. Diagnostic performance of fusion of myocardial perfusion imaging (MPI) and computed tomography coronary angiography. J Nucl Cardiol. 2009;16:201–11.
Matsuo S, Nakajima K, Akhter N, Wakabayashi H, Taki J, Okuda K, et al. Clinical usefulness of novel cardiac MDCT/SPECT fusion image. Ann Nucl Med. 2009;23:579–86.
Acknowledgments
This research was supported by research grants from Yeung-nam University in 2009.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kong, EJ., Cho, IH. & Chun, KA. Clinical usefulness of combinatorial protocol with stress only myocardial perfusion SPECT, CTA and SPECT/CTA 3-dimensional fusion image. Ann Nucl Med 25, 387–395 (2011). https://doi.org/10.1007/s12149-011-0476-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12149-011-0476-0