Abstract
Background
Performing both single photon emission computerized tomography (SPECT) and coronary computed tomography angiography (CCTA) in patients suspected for coronary artery disease (CAD) leads to increased radiation exposure. We evaluated the need for additional imaging and following implications for radiation exposure of a sequential SPECT/computed tomography (CT) algorithm.
Methods and Results
5018 consecutive patients without history of CAD were referred for stress-first SPECT and coronary artery calcium (CAC) scoring. If stress SPECT was abnormal, additional rest SPECT and, if feasible, CCTA were acquired. Stress SPECT was normal in 2617 patients (52%). CCTA was not performed in 1289 of the 2401 patients referred for additional imaging (54%), mainly because of severe CAC (47%) or fast/irregular heart rate (22%). 642 patients with abnormal SPECT underwent CCTA, which excluded significant CAD in 378 patients (59%). Mean radiation dose was 4.5 ± 0.3 mSv for stress-only imaging and 13.2 ± 3.3 mSv for additional imaging (P < 0.001).
Conclusions
Half of the patients do not require additional imaging in our sequential SPECT/CT algorithm, which is accompanied with low radiation exposure. CCTA cannot be performed in half of the patients who undergo additional imaging because of (relative) contra-indications. CCTA is able to correct for false-positive SPECT findings in our algorithm.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
Although coronary computed tomography angiography (CCTA) may be an excellent tool for ruling out relevant coronary artery disease (CAD),1 it is not able to assess the hemodynamic relevance of luminal stenosis,2,3 and has limited diagnostic accuracy with higher coronary artery calcium (CAC) scores.4 Furthermore, CCTA requires specific patient characteristics such as normal renal function and low regular heart rhythm.5 Since the diagnostic and prognostic value of myocardial perfusion imaging with single photon emission computerized tomography (SPECT) has been well established, and is feasible in almost all patients, the combination of CCTA and SPECT has been suggested to result in a more definite diagnosis.6-8 However, performing both SPECT and CCTA in all patients suspected for CAD would lead to increased radiation exposure and costs, and therefore, various suggestions for a sequential SPECT/CT protocol have been made.9-12 We incorporated a sequential diagnostic algorithm starting with stress SPECT and CAC scoring, if necessary followed by additional imaging with rest SPECT and CCTA. With the current study, we evaluated the need for additional imaging and following implications for total radiation exposure of this sequential SPECT/CT imaging algorithm in patients with a low to intermediate pre-test likelihood of CAD.
Methods
Study Population
We performed a prospective observational single-center cohort study, in which consecutive patients with suspected CAD referred for non-invasive CAD detection with SPECT/computed tomography (CT) between January 2009 and June 2013 were included. Patients were referred from the cardiology outpatient clinics of our hospital, which is a large cardiovascular center with a local, regional, and supraregional catchment area. The pre-test likelihood of CAD was assigned according to the criteria of Diamond and Forrester,13 with a risk threshold of <13.4% for low risk, between 13.4% and 87.2% for intermediate risk, and >87.2% for high risk. Patients with known history of CAD were excluded, no other exclusion criteria were applied. Information regarding the presence of risk factors was collected by written questionnaires. All patients underwent a sequential 1-day 99mTc-tetrofosmin SPECT/CT protocol according to an individualized algorithm. All patients underwent initial stress SPECT combined with CAC scoring. Immediately after acquisition of stress SPECT and CAC scan, a cardiologist and nuclear physician together assessed the need for additional rest SPECT imaging and CCTA. In case of an abnormal stress perfusion, additional rest SPECT was performed, independent of CAC scoring result. The rest SPECT was combined with an additional CCTA if the heart rate allowed optimal diagnostic CT acquisition, CAC score was not too high (generally <400 and the absence of large calcified segments) and contra-indications were absent (renal insufficiency, known hypersensitivity to iodine contrast media). The final diagnosis was considered normal (i.e., no or no significant CAD) if either SPECT perfusion was normal or if CCTA excluded obstructive CAD. All procedures were performed in accordance with the Declaration of Helsinki. The study was approved by the Committee on Research Ethics of our hospital, and written informed consent was obtained from all patients.
Myocardial Perfusion Imaging
Stress testing was routinely performed with pharmacological stress using adenosine (140 μg/min/kg for 6 min) in all patients, unless there was a contra-indication for pharmacological stress. Due to logistical reasons, this is common practice in our high-volume center. Patients were instructed to refrain from caffeine-containing beverages for at least 24 hours before the test. In case of a contra-indication for adenosine, patients underwent dobutamine (starting dose of 10 μg/kg per min, increased at 3-min intervals to a maximum of 50 μg/kg per min), regadenoson (fixed-dose of 400 μg bolus injection over 15 seconds), or bicycle testing. A weight-adjusted dose of 99mTc-tetrofosmin (standard 370 MBq, 500 MBq for patients >100 kg) was administered after 3 min (adenosine), after 35 seconds (regadenoson) or when the target heart rate of > 85% of predicted maximal was reached (dobutamine, bicycle test).14 Patients scheduled for rest imaging received a dose of 99mTc-Tetrofosmin (standard 740 MBq, but 1000 MBq for patients >100 kg). Both stress and rest SPECT images were acquired 45-60 min after tracer injection. Time delay between the stress and rest studies was >3 hours.15 All patients were imaged in the supine position with arms placed above the head.
From January 2009 until April 2010, patients (n = 977) were scanned on a conventional dual-detector gamma camera (Ventri-LightSpeed VCT XT, GE Healthcare), using a low-energy, high-resolution collimator, a 20% symmetrical window at 140 keV, a 64 × 64 matrix, and an elliptical orbit with step-and-shoot acquisition at 6° intervals over a 180° arc (45° right anterior oblique to 45° left posterior oblique) with 30 steps (30 views). Acquisition time was 12 min for the stress images and 15 min for the rest images as previously described.16
From May 2010 until June 2013, patients (n = 4057) were scanned with a cadmium zinc telluride (CZT)-based SPECT/CT camera (Discovery NM/CT 570c, GE Healthcare) with 19 stationary CZT detectors simultaneously imaging 19 cardiac views. Each detector comprised 32 × 32 pixelated (2.46 × 2.46 mm) CZT elements. Acquisition time was 5 min for the stress images and 4 min for the rest images. This was derived from the recommendations of the manufacturer, published experience and our own qualitative assessment in heart phantom studies, and our initial experience in patients.17 All SPECT studies were followed by an unenhanced low-dose CT scan during a breath-hold to provide the attenuation map for attenuation correction as previously described.18
Perfusion images were unblindedly and semiquantitatively interpreted using a 17-segment model.19 Segments were scored by consensus of two experienced nuclear cardiology observers using a 5-points scoring system (0 = normal, 1 = equivocal, 2 = moderate, 3 = severe reduction of radioisotope uptake, 4 = absence of detectable tracer uptake).20 The combination of attenuation corrected and non-attenuation corrected images was reviewed and rest SPECT was acquired if there was uncertainty about normalcy of perfusion using both image sets. A stress study was interpreted as normal if the summed stress scores were ≤3.20 Additional rest SPECT was acquired if the stress images did not fulfill these criteria. Gated SPECT analysis was used as an aid to differentiate between artifacts and perfusion defects.
The perfusion images were reviewed again by a cardiologist and a nuclear physician after both stress and rest SPECT. An ischemic defect was defined as a summed difference score ≥2.20 Reversible defects not fulfilling these criteria were assessed as equivocal for ischemia. Perfusion defects which demonstrated no reversibility were defined as fixed defects. An abnormal SPECT was defined as either ischemia, equivocal for ischemia, or fixed defects. If, after reviewing both stress and rest SPECT, no reversible of fixed defects were observed, the SPECT was considered normal.
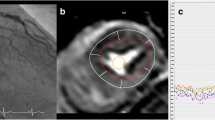
CAC Scoring and CCTA
All cardiac CT studies were performed by using the 64-section CT scanner of the integrated SPECT/CT scanner (LightSpeed VCT XT; GE Healthcare). All patients with heart rates greater than 70 beats per minute received oral beta-blocker therapy, with 50 or 100 mg of metoprolol tartrate (AstraZeneca, Zoetermeer, the Netherlands) before the CAC scan. A non-enhanced CT scan to calculate the total CAC score was acquired with ECG triggering at 75% of the R-R interval and the following scanning parameters: 40 or 48 sections and 2.5-mm section thickness; gantry rotation time, 330 ms; tube voltage, 120 kV; and a tube current ranging from 125 to 250 mA, depending on patient size. Post-processing was conducted at a dedicated workstation using Smartscore software (GE Healthcare). The CAC score was calculated using the standard Agatston criteria.21
Before acquiring CCTA images, patients with a heart rate exceeding the threshold of 65/min were administered beta-blocking medication (50-100 mg metoprolol, oral, or 5-10 mg metoprolol, intravenous). A scout view of the chest was first obtained, followed by prospectively (83%) or retrospectively (on indication) ECG-triggered CCTA according to the guidelines provided by the Society of Cardiovascular Computed Angiography.22 Coronary arteries were subdivided according to a 15-segment model as proposed by the American Heart Association.23 Each segment was evaluated on at least two planes according to Society of Cardiovascular Computed Tomography guidelines,24 and the degree of diameter stenosis was visually graded by consensus of the two readers as obstructive CAD when narrowing of the coronary lumen was 50% or greater.
Effective Radiation Dose
Radiation dose for SPECT was calculated as 99mTc-tetrofosmin activity times 7.9 mSv/GBq as suggested by the International Commission on Radiological Protection.25 Effective radiation dose for CCTA was estimated as dose-length product times a conversion coefficient for the chest k (0.017 mSv/mGy/cm).26
Follow-Up
Follow-up data were based on clinical visits, standardized telephone interviews, and by consulting the municipal population register. Events that were noted during follow-up were all-cause mortality and non-fatal myocardial infarction (MI). Non-fatal MI was defined based on the criteria of typical chest pain, elevated cardiac enzyme levels, and typical changes on the ECG as defined by Thygesen et al.27
Statistical Analysis
Continuous variables are expressed as mean ± SD or median [25th-75th percentile], and categorical variables are expressed as frequency (percentage). Differences between groups were assessed by unpaired Student t test, Mann-Whitney U test, and by Chi square test, where appropriate. We evaluated the differences in general characteristics of patients with normal or abnormal stress SPECT, of patients who underwent rest SPECT with or without additional CCTA and of patients with normal or abnormal final diagnosis. The patient’s pre-test likelihood for CAD was determined with the standard Diamond criteria with the assumption that chest pain was atypical.13 Multivariate logistic regression was performed to investigate which general characteristics were independent predictors for an abnormal stress SPECT and abnormal final diagnosis after adjusting for other significant variables in univariate analysis. A value of P < 0.05 in univariate analysis was required for entry into the multivariate analysis. Significant variables analyzed are reported with their respective odds ratio and 95% confidence intervals. In the selected group of patients who underwent both SPECT and CCTA, sensitivity, specificity, negative predictive value, and positive predictive value of SPECT were calculated with CCTA as gold standard. The normalcy rate, the rate of normal perfusion scans in patients with <5% likelihood of CAD, was reported as a surrogate for specificity to account for referral bias.28 Differences in event-free survival over time were analyzed by the Kaplan-Meier method. Time 0 was defined as the date of SPECT imaging. Annualized event rate was calculated on the basis of events per patients-year. Two-sided p-values of less than 0.05 were considered statistically significant in all tests. All statistical analysis was performed with a commercially available software package (SPSS, version 20.0 for Windows).
Results
Study Population
During a period of 4.5 years, a total of 5026 patients were included. Follow-up information was complete for 99.8% of the patients, only 8 patients were lost to follow-up. The remainder of 5018 patients are the subject of this report. The main indications for referral were atypical chest pain and dyspnoea. Pre-test likelihood was considered to be low in 9% of the patients and intermediate in 91% of the patients. The mean age was 61 ± 11 years, 57% of the patients were female, 14% were diabetic, and the mean body mass index (BMI) was 27.6 ± 4.8. Stress testing was performed with adenosine in 4816 (96.0%), with dobutamine in 114 (2.3%), with regadenoson in 34 (0.7%), and with exercise testing in 54 (1.1%) of the patients.
Sequential SPECT/CT Algorithm
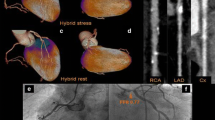
Figure 1 displays the individualized sequential SPECT/CT algorithm. All 5018 patients underwent stress SPECT. CAC score was obtained in 4897 patients (97.6%). A fast or irregular heart rate was the main reason for not acquiring CAC score. In 2617 patients (52% of the total population), the stress SPECT was normal, and these patients were discharged without additional rest SPECT or CCTA. Differences in the general characteristics between patients with normal and abnormal stress SPECT are demonstrated in Table 1. Independent predictors for abnormal stress SPECT were older age, male gender, diabetes mellitus, current smoking, left bundle branch block (LBBB), higher BMI, and higher CAC score (Fig. 2). In 2401 patients (48% of the total population), the stress SPECT was regarded abnormal, and these patients underwent additional rest SPECT and CCTA (if feasible). CCTA was not performed in 1289 patients (54%) because of high CAC scoring (n = 591, 46.7%), fast/irregular heart rate (n = 281, 21.8%), renal insufficiency (n = 89, 6.9%), small atypical perfusion defects suspected for artifact (n = 251, 19.5%), contrast allergy (n = 9, 0.7%), expected scatter from pacemaker lead (n = 6, 0.5%), anxiety/unable to hold breath (n = 11, 0.9%), or unclear reasons (n = 51, 3.9%). Table 2 demonstrates the differences in general characteristics between patients who underwent additional rest SPECT with or without CCTA.
Effective Radiation Dose
The mean radiation dose after completing the diagnostic algorithm was 8.6 ± 4.9 mSv for the entire cohort. The mean radiation dose was 4.5 ± 0.3 mSv in patients who underwent stress-only imaging and 13.2 ± 3.3 mSv in patients who underwent additional imaging (P < 0.001).
Imaging Results
All 2617 patients who were discharged after stress SPECT and CAC scoring had normal myocardial perfusion. Among 2401 patients who underwent additional rest SPECT, myocardial perfusion was considered normal in 1175 patients (49%) after reviewing both stress and rest images. Finally, SPECT was considered normal in 3790 (76%) of the total population. In the remaining 1228 patients, SPECT was considered abnormal, of which 299 patients (24%) had equivocally reversible defects, 513 (42%) had findings clearly suggestive for ischemia and 416 (34%) showed fixed perfusion defects.
The median CAC scoring for the total population was 39 [25th-75th percentile, 0-282]. 1315 of the patients (27%) demonstrated a CAC score of zero, and 995 of the patients (20%) demonstrated a CAC score >400. A total of 1112 patients underwent CCTA, of which 751 (68%) showed no obstructive CAD, 349 (31%) showed significant CAD, and 12 (1.0%) were assessed as non-evaluable due to limited image quality.
Of the 2617 patients with normal stress SPECT, the CAC score was 0 in 37%, 1-100 in 38%, 101-400 in 15%, and >400 in 11%. Of the 2401 patients who required additional imaging, the CAC score was 0 in 16%, 1-100 in 30%, 101-400 in 23%, and >400 in 31%. In the 1228 patients who had an abnormal SPECT, 13, 27, 24, and 36% had CAC scores of 0, 1-100, 101-400, and >400, respectively.
Of the total of 1112 patients who underwent CCTA, in 470 (42%), SPECT perfusion was considered normal after viewing both stress and rest SPECT. CCTA excluded obstructive CAD in 373 (80%) of these 470 patients. In the remainder of the patients who underwent CCTA (n = 642, 58%), the perfusion was considered abnormal. Of these 642 patients, in 378 patients (60%), obstructive CAD was excluded with CCTA.
In the subpopulation of patients who underwent both CCTA and SPECT, the sensitivity of SPECT was 73% and the specificity was 50% (negative predictive value 79%, positive predictive value 41%). The normalcy rate of SPECT was 87%.
With the combination of SPECT and CCTA imaging, 4168 (83%) of the patients were concluded to have normal final diagnosis after completing the diagnostic algorithm. Differences in general characteristics between patients with normal and abnormal final diagnosis are demonstrated in Table 3. Independent predictors of final abnormal diagnoses were older age, male gender, diabetes mellitus, LBBB, higher BMI, and higher CAC scoring (Fig. 3).
Significant independent predictors of final diagnosis. Age (upper quartile 69); BMI, body mass index (upper quartile: 30); LBBB, left bundle branch block; BMI, body mass index; CAC, coronary artery calcium (upper quartile: 282); normal final diagnosis, SPECT perfusion normal or CCTA without significant CAD
Follow-Up
Over a median follow-up duration of 965 days [25th-75th percentile, 600-1397], there were 205 events (166 all-cause deaths, 39 non-fatal MI). Annual event rate of patients with normal myocardial perfusion after stress-only SPECT was slightly lower compared to those with normal myocardial perfusion after additional rest imaging (1.07% vs 1.60%, P = 0.04). For patients with an abnormal SPECT but no obstructive CAD on CCTA, the annual event rate was 0.85% (9 deaths, 1 MI); for patients with normal SPECT but obstructive CAD, this was 1.64% (4 deaths, 1 MI) and for patients with both abnormal SPECT and obstructive CAD on CCTA this was 2.15% (11 deaths, 6 MIs). Survival curves of these groups are demonstrated in Fig. 4. The annual event rate was significantly higher in patients with abnormal final diagnosis compared to those with normal final diagnosis (2.55% vs. 1.19%, P < 0.001).
Discussion
This study evaluated the need for additional imaging and following implications for total radiation exposure of an individualized sequential SPECT/CT algorithm in a large, low- to intermediate-risk population suspected for CAD. After initial stress SPECT and CAC scoring, additional rest SPECT imaging could be omitted in half of the patients, which is accompanied with a low radiation exposure. In patients who required additional imaging, CCTA could not be performed in nearly half of the patients because of (relative) contra-indications. CCTA was able to correct for false-positive SPECT findings in our algorithm.
Non-invasive imaging using both functional (SPECT) and anatomical data (CT) has been suggested to be the optimal approach in the evaluation of patients with suspected CAD.6-8 Increasing concerns about both costs and radiation exposure gave rise to sequential use of these modalities. Protocols with either initial SPECT or initial CCTA have been proposed.9,10 CCTA might be appropriate as initial test in lower risk populations, due to its high negative predictive value. However, after initial CCTA, half of the patients still require SPECT imaging,10 and diagnostic quality of CCTA is reduced in a substantial number of patients due to extensive calcification, motion artifacts, or low image quality.6,8,29 SPECT is well established for the diagnostic and prognostic evaluation of patient suspected for CAD.30 When SPECT is combined with CAC scoring, information about myocardial perfusion and the extent of CAD is acquired in a single setting. Therefore, we incorporated a sequential SPECT/CT algorithm starting with stress SPECT and CAC scoring, if necessary followed by additional imaging with rest SPECT and CCTA.
In general, there may be several advantages of simultaneous CAC scoring in combination with stress-only SPECT. First, knowledge of CAC score results in more interpretative certainty for SPECT imaging with better selection of patients who require additional rest SPECT.31,32 In the absence of any CAC, the prevalence of significant CAD is low, thereby subtle stress SPECT abnormalities are likely to be disregarded, whereas these may warrant further imaging in patients with extensive coronary calcifications.18,33,34 The knowledge of CAC is likely to have contributed to our results that no additional rest SPECT was necessary in about half of the patients after stress SPECT. The patients with stress-only SPECT demonstrated an excellent prognosis during follow-up, which is in line with previous studies.35-39 Second, the CAC score assisted us to select patients suited to undergo additional CCTA, as we did not obtain additional CCTA in patients with very high CAC scores. By this means, the radiation dose from a CCTA with low expected diagnostic yield was prevented.4 Finally, information about the extent of subclinical CAD was available in patients with normal myocardial perfusion. It has been demonstrated that CAC scoring adds independent prognostic information in addition to SPECT.40,41 Therefore, a high CAC score in these patients could potentially influence treatment decisions with improved patient care through life style advise, intensification of medication use, and in case of persisting complaints an earlier invasive strategy.18
One of the most important findings in the current study was that CCTA was not performed in about half of the patients referred for additional imaging. In a small portion of the patients, this could be explained by inconsistent application of the clinical protocol leading to underuse of the CCTA in eligible patients (13% of the patients who underwent additional rest SPECT did not undergo CCTA because of atypical perfusion defect or unclear reasons). However, in the remaining 41% of the patients, CCTA indeed could not be performed. This percentage is higher than in previous observations, which demonstrated that up to 23% of the patients were unsuitable for CCTA because of calcifications or poor image quality.6,8,29 This difference is likely to be explained by both strict selection for CCTA and the different patient population which is considered for CCTA. In our study, only patients with abnormal stress SPECT were considered to undergo CCTA, and these patients probably have more (relative) contra-indications for CCTA. Of course, CCTA can be performed using less strict (relative) contra-indications, but this may be associated with more non-diagnostic scans.4,5,42 The main advantage of CCTA in our algorithm is correcting for false-positive SPECT, as previously suggested in the literature.43 This can result in a reduction of unnecessary downstream invasive coronary angiography and thereby significant cost savings.43
In patients who underwent both CCTA and SPECT imaging, specificity of SPECT was lower than expected according to current literature.44 This may be caused by patient selection. Patients who were eligible for CCTA had a lower risk of CAD, as contra-indications for CCTA (high CAC score and renal insufficiency) are well-known risk factors.45,46 The normalcy rate (as a surrogate for specificity to account for referral bias) was 87%, which is comparable with previous findings.28 Sensitivity of SPECT was also lower than expected,44 possibly due to exclusion of patients with normal stress SPECT, as these were not considered for CCTA in the current algorithm. Furthermore, CCTA is well known to overestimate the degree of coronary stenosis.47
With our sequential SPECT/CT algorithm, 83% of the patients had normal final diagnosis (i.e., no or non-significant CAD). This high rate of normal findings in our study is explained by the fact that patients with known CAD were excluded and that our algorithm was not performed in patients with a high pre-test likelihood of CAD. Furthermore, CCTA increased the percentage of patients with a normal final diagnosis in case of an abnormal SPECT. The frequency of normal SPECT findings in our study is comparable to other studies.47,48
In our study, several predictors for normal initial stress SPECT were identified. Younger age, female gender, no current smoking, and lower CAC score are indicators for low risk, with a subsequent lower prevalence of an abnormal stress SPECT, which is in line with previous studies.37,38 As a lower CAC score is associated with a higher frequency of normal SPECT, it is not surprising that patients with lower CAC scores less frequently required additional imaging.40,49,50 The absence of LBBB is an independent predictor for normal initial stress SPECT. This is likely due to anteroseptal and septal perfusion defects associated with LBBB.51,52 Patients with lower BMI more often demonstrated normal stress SPECT perfusion, likely because of the lower risk of soft tissue attenuation artifacts. These predictors for normal initial stress SPECT could be taken into account when planning patients for the SPECT/CT algorithm, optimizing capacity utilization.
The mean radiation dose for the total population after completing our diagnostic algorithm is lower compared to the radiation dose after the traditional stress-rest SPECT protocol.53 Half of the patients did not require additional imaging after stress SPECT and CAC scoring and thereby had a low mean radiation dose of 4.5 mSv. Thus, the current algorithm easily complies with the recommendations of the American Society of Nuclear Cardiology to decrease patient radiation exposure to <9 mSv in 50% of patients by 2014.54
Although our current algorithm proves feasible in daily practice, with very low event rates in patients with normal final diagnosis, alternative algorithms could be considered. A protocol starting with CAC scoring, without additional imaging in case of a CAC score of zero, could be very efficient.55 However, whether it is safe to omit further imaging in patients with a CAC score of zero remains a subject of debate, due to conflicting data with regard to the negative predictive value of CAC zero.56,57 If the CAC score is low and CCTA is feasible, additional imaging should be performed with CCTA. Otherwise, an additional functional test should be performed. Another option could be modification of our protocol, by implementing a second evaluation after rest SPECT to assess if additional CCTA is necessary. Thereby, CCTA could be prevented in patients with a normal SPECT after stress and rest imaging. Finally, a protocol starting with CCTA could be incorporated, although it is well known that half of the patients still require SPECT imaging after initial CCTA.10 Irrespective of which specific algorithm used, when implementing SPECT/CT imaging in a clinic, it is advised to opt for an individualized sequential algorithm to lower radiation dose and costs. Local expertise and logistics should be taken into consideration when choosing such an algorithm.
Although our study reflects true daily practice and included consecutive patients, we have to acknowledge several limitations. The observational design remains a major limitation of the current study, as end-points were not pre-specified, and no head-to-head comparison to other diagnostic algorithms was performed. Also, this is a single-center study in patients with suspected CAD and a low- to intermediate pre-test likelihood undergoing predominantly pharmacological stress. Therefore, extrapolation of the present results is difficult to populations with different pre-test likelihood or patients undergoing traditional exercise testing. Although CAC scoring was not included in the diagnostic algorithm to decide whether or not additional rest SPECT was performed, the SPECT observers were not blinded for the CAC score. Thus, it cannot be excluded that the need for additional rest SPECT is biased by the CAC score, as subtle stress SPECT abnormalities are possibly disregarded if the CAC score was 0. Furthermore, our current results are based on SPECT scanning predominantly performed on state-of-the art imaging equipment (CZT-based SPECT/CT camera). The result can be different if other SPECT/CT cameras are used. CCTA was not performed in about half of the patients referred for additional imaging, which was partially caused by a strict selection for the eligibility for CCTA. Possibly, results of the current algorithm would be different if patients underwent CCTA with less strict selection. Although downstream invasive coronary angiography was performed for clinical reasons in selected patients during follow-up, this was not included in the current report, as this was not part of our research question. Finally, we did not include revascularizations as an outcome for the current study, as these outcomes can be driven by imaging results.
Conclusions
Half of the patients do not require additional imaging in our sequential SPECT/CT algorithm, which is accompanied with low radiation exposure. CCTA cannot be performed in half of the patients who undergo additional imaging because of (relative) contra-indications. CCTA is able to correct for false-positive SPECT findings in our algorithm.
New Knowledge Gained
Sequential SPECT/CT imaging is feasible in clinical daily practice, without need for additional imaging after stress SPECT and CAC scoring in half of the patients. CCTA was less often performed than expected, because of (relative) contra-indications.
Abbreviations
- CAD:
-
Coronary artery disease
- CCTA:
-
Coronary computed tomography angiography
- CAC:
-
Coronary artery calcium
- SPECT:
-
Single photon emission computed tomography
- CT:
-
Computed tomography
- MI:
-
Myocardial infarction
- LBBB:
-
Left bundle branch block
- BMI:
-
Body mass index
- CZT:
-
Cadmium zinc telluride
References
Budoff MJ, Dowe D, Jollis JG, Gitter M, Sutherland J, Halamert E, et al. Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: Results from the prospective multicenter ACCURACY (assessment by coronary computed tomographic angiography of individuals undergoing invasive coronary angiography) trial. J Am Coll Cardiol 2008;52:1724-32.
Hacker M, Jakobs T, Hack N, Nikolaou K, Becker C, von Ziegler F, et al. Sixty-four slice spiral CT angiography does not predict the functional relevance of coronary artery stenoses in patients with stable angina. Eur J Nucl Med Mol Imaging 2007;34:4-10.
Gaemperli O, Schepis T, Koepfli P, Valenta I, Soyka J, Leschka S, et al. Accuracy of 64-slice CT angiography for the detection of functionally relevant coronary stenoses as assessed with myocardial perfusion SPECT. Eur J Nucl Med Mol Imaging 2007;34:1162-71.
Arbab-Zadeh A, Miller JM, Rochitte CE, Dewey M, Niinuma H, Gottlieb I, et al. Diagnostic accuracy of computed tomography coronary angiography according to pre-test probability of coronary artery disease and severity of coronary arterial calcification. The CORE-64 (coronary artery evaluation using 64-row multidetector computed tomography angiography) international multicenter study. J Am Coll Cardiol 2012;59:379-87.
Buechel RR, Husmann L, Herzog BA, Pazhenkottil AP, Nkoulou R, Ghadri JR, et al. Low-dose computed tomography coronary angiography with prospective electrocardiogram triggering: Feasibility in a large population. J Am Coll Cardiol 2011;57:332-6.
Rispler S, Keidar Z, Ghersin E, Roguin A, Soil A, Dragu R, et al. Integrated single-photon emission computed tomography and computed tomography coronary angiography for the assessment of hemodynamically significant coronary artery lesions. J Am Coll Cardiol 2007;49:1059-67.
van Werkhoven JM, Schuijf JD, Gaemperli O, Jukema JW, Boersma E, Wijns W, et al. Prognostic value of multislice computed tomography and gated single-photon emission computed tomography in patients with suspected coronary artery disease. J Am Coll Cardiol 2009;53:623-32.
Sato A, Nozato T, Hikita H, Miyazaki S, Takahashi Y, Kuwahara T, et al. Incremental value of combining 64-slice computed tomography angiography with stress nuclear myocardial perfusion imaging to improve noninvasive detection of coronary artery disease. J Nucl Cardiol 2010;17:19-26.
Slart RH, Tio RA, Zijlstra F, Dierckx RA. Diagnostic pathway of integrated SPECT/CT for coronary artery disease. Eur J Nucl Med Mol Imaging 2009;36:1829-34.
Pazhenkottil AP, Herzog BA, Husmann L, Buechel RR, Burger IA, Valenta I, et al. Non-invasive assessment of coronary artery disease with CT coronary angiography and SPECT: A novel dose-saving fast-track algorithm. Eur J Nucl Med Mol Imaging 2010;37:522-7.
von Ziegler F, Brendel M, Uebleis C, Helbig S, Greif M, Ruemmler J, et al. SPECT myocardial perfusion imaging as an adjunct to coronary calcium score for the detection of hemodynamically significant coronary artery stenosis. BMC Cardiovasc Disord 2012;12:116.
Flotats A, Knuuti J, Gutberlet M, Marcassa C, Bengel FM, Kaufmann PA, et al. Hybrid cardiac imaging: SPECT/CT and PET/CT. A joint position statement by the european association of nuclear medicine (EANM), the european society of cardiac radiology (ESCR) and the european council of nuclear cardiology (ECNC). Eur J Nucl Med Mol Imaging 2011;38:201-12.
Diamond GA, Forrester JS. Analysis of probability as an aid in the clinical diagnosis of coronary-artery disease. N Engl J Med 1979;300:1350-8.
Gowd BM, Heller GV, Parker MW. Stress-only SPECT myocardial perfusion imaging: A review. J Nucl Cardiol 2014;21:1200-12.
Henzlova MJ, Cerqueira MD, Mahmarian JJ, Yao SS. Quality Assurance Committee of the American Society of Nuclear Cardiology. Stress protocols and tracers. J Nucl Cardiol 2006;13:e80-90.
Mouden M, Timmer JR, Ottervanger JP, Reiffers S, Oostdijk AH, Knollema S, et al. Impact of a new ultrafast CZT SPECT camera for myocardial perfusion imaging: Fewer equivocal results and lower radiation dose. Eur J Nucl Med Mol Imaging 2012;39:1048-55.
Herzog BA, Buechel RR, Katz R, Brueckner M, Husmann L, Burger IA, et al. Nuclear myocardial perfusion imaging with a cadmium-zinc-telluride detector technique: Optimized protocol for scan time reduction. J Nucl Med 2010;51:46-51.
Mouden M, Ottervanger JP, Timmer JR, Reiffers S, Oostdijk AH, Knollema S, et al. Myocardial perfusion imaging in stable symptomatic patients with extensive coronary atherosclerosis. Eur J Nucl Med Mol Imaging 2014;41:136-43.
Berman DS, Abidov A, Kang X, Hayes SW, Friedman JD, Sciammarella MG, et al. Prognostic validation of a 17-segment score derived from a 20-segment score for myocardial perfusion SPECT interpretation. J Nucl Cardiol 2004;11:414-23.
Berman DS, Hachamovitch R, Kiat H, Cohen I, Cabico JA, Wang FP, et al. Incremental value of prognostic testing in patients with known or suspected ischemic heart disease: A basis for optimal utilization of exercise technetium-99 m sestamibi myocardial perfusion single-photon emission computed tomography. J Am Coll Cardiol 1995;26:639-47.
Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol 1990;15:827-32.
Abbara S, Arbab-Zadeh A, Callister TQ, Desai MY, Mamuya W, Thomson L, et al. SCCT guidelines for performance of coronary computed tomographic angiography: A report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr 2009;3:190-204.
Austen WG, Edwards JE, Frye RL, Gensini GG, Gott VL, Griffith LS, et al. A reporting system on patients evaluated for coronary artery disease. report of the Ad Hoc Committee for grading of coronary artery disease, Council on Cardiovascular Surgery, American Heart Association. Circulation 1975;51:5-40.
Raff GL, Abidov A, Achenbach S, Berman DS, Boxt LM, Budoff MJ, et al. SCCT guidelines for the interpretation and reporting of coronary computed tomographic angiography. J Cardiovasc Comput Tomogr 2009;3:122-36.
Valentin J. Radiation dose to patients from radiopharmaceuticals (addendum 2 to ICRP publication 53). Ann ICRP 1998;28:1-126.
Einstein AJ, Moser KW, Thompson RC, Cerqueira MD, Henzlova MJ. Radiation dose to patients from cardiac diagnostic imaging. Circulation 2007;116:1290-305.
Thygesen K, Alpert JS, Jaffe AS, Simoons ML, Chaitman BR, White HD, et al. Third universal definition of myocardial infarction. J Am Coll Cardiol 2012;60:1581-98.
Beller GA, Zaret BL. Contributions of nuclear cardiology to diagnosis and prognosis of patients with coronary artery disease. Circulation 2000;101:1465-78.
Schaap J, Kauling RM, Boekholdt SM, Nieman K, Meijboom WB, Post MC, et al. Incremental diagnostic accuracy of hybrid SPECT/CT coronary angiography in a population with an intermediate to high pre-test likelihood of coronary artery disease. Eur Heart J Cardiovasc Imaging 2013;14:642-9.
Underwood SR, Anagnostopoulos C, Cerqueira M, Ell PJ, Flint EJ, Harbinson M, et al. Myocardial perfusion scintigraphy: The evidence. Eur J Nucl Med Mol Imaging 2004;31:261-91.
Mouden M, Ottervanger JP, Timmer JR, Reiffers S, Oostdijk AH, Knollema S, et al. The influence of coronary calcium score on the interpretation of myocardial perfusion imaging. J Nucl Cardiol 2014;21:368-74.
Uretsky S, Cohen R, Argulian E, Balasundaram K, Supariwala A, Subero M, et al. Combining stress-only myocardial perfusion imaging with coronary calcium scanning as a new paradigm for initial patient work-up: An exploratory analysis. J Nucl Cardiol 2014;22:89-97.
Villines TC, Hulten EA, Shaw LJ, Goyal M, Dunning A, Achenbach S, et al. Prevalence and severity of coronary artery disease and adverse events among symptomatic patients with coronary artery calcification scores of zero undergoing coronary computed tomography angiography: Results from the CONFIRM (coronary CT angiography evaluation for clinical outcomes: An international multicenter) registry. J Am Coll Cardiol 2011;58:2533-40.
Ghadri JR, Pazhenkottil AP, Nkoulou RN, Goetti R, Buechel RR, Husmann L, et al. Very high coronary calcium score unmasks obstructive coronary artery disease in patients with normal SPECT MPI. Heart 2011;97:998-1003.
Chang SM, Nabi F, Xu J, Raza U, Mahmarian JJ. Normal stress-only versus standard stress/rest myocardial perfusion imaging: Similar patient mortality with reduced radiation exposure. J Am Coll Cardiol 2010;55:221-30.
Duvall WL, Wijetunga MN, Klein TM, Razzouk L, Godbold J, Croft LB, et al. The prognosis of a normal stress-only tc-99 m myocardial perfusion imaging study. J Nucl Cardiol 2010;17:370-7.
Ueyama T, Takehana K, Maeba H, Iwasaka T. Prognostic value of normal stress-only technetium-99 m myocardial perfusion imaging protocol. Comparison with standard stress-rest protocol. Circ J 2012;76:2386-91.
Edenbrandt L, Ohlsson M, Tragardh E. Prognosis of patients without perfusion defects with and without rest study in myocardial perfusion scintigraphy. EJNMMI Res 2013;3:58. 219X-3-58. eCollection 2013.
Ferreira MJ, Cunha MJ, Albuquerque A, Moreira AP, Ramos D, Costa G, et al. Prognosis of normal stress-only gated-SPECT myocardial perfusion imaging: A single center study. Int J Cardiovasc Imaging 2013;29:1639-44.
Chang SM, Nabi F, Xu J, Peterson LE, Achari A, Pratt CM, et al. The coronary artery calcium score and stress myocardial perfusion imaging provide independent and complementary prediction of cardiac risk. J Am Coll Cardiol 2009;54:1872-82.
Ramakrishna G, Miller TD, Breen JF, Araoz PA, Hodge DO, Gibbons RJ. Relationship and prognostic value of coronary artery calcification by electron beam computed tomography to stress-induced ischemia by single photon emission computed tomography. Am Heart J 2007;153:807-14.
Dewey M, Vavere AL, Arbab-Zadeh A, Miller JM, Sara L, Cox C, et al. Patient characteristics as predictors of image quality and diagnostic accuracy of MDCT compared with conventional coronary angiography for detecting coronary artery stenoses: CORE-64 multicenter international trial. AJR Am J Roentgenol 2010;194:93-102.
Patel N, Pal RS, Flores F, Budoff M. Utility of cardiac computed tomography angiography to exclude clinically significant obstructive coronary artery disease in patients after myocardial perfusion imaging. Am J Cardiol 2012;109:165-8.
Klocke FJ, Baird MG, Lorell BH, Bateman TM, Messer JV, Berman DS, et al. ACC/AHA/ASNC guidelines for the clinical use of cardiac radionuclide imaging-executive summary: A report of the american college of Cardiology/American heart association task force on practice guidelines (ACC/AHA/ASNC committee to revise the 1995 guidelines for the clinical use of cardiac radionuclide imaging). Circulation 2003;108:1404-18.
Arad Y, Spadaro LA, Goodman K, Newstein D, Guerci AD. Prediction of coronary events with electron beam computed tomography. J Am Coll Cardiol 2000;36:1253-60.
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 2004;351:1296-305.
Schuijf JD, Wijns W, Jukema JW, Atsma DE, de Roos A, Lamb HJ, et al. Relationship between noninvasive coronary angiography with multi-slice computed tomography and myocardial perfusion imaging. J Am Coll Cardiol 2006;48:2508-14.
Pazhenkottil AP, Nkoulou RN, Ghadri JR, Herzog BA, Buechel RR, Kuest SM, et al. Prognostic value of cardiac hybrid imaging integrating single-photon emission computed tomography with coronary computed tomography angiography. Eur Heart J 2011;32:1465–71.
Schepis T, Gaemperli O, Koepfli P, Namdar M, Valenta I, Scheffel H, et al. Added value of coronary artery calcium score as an adjunct to gated SPECT for the evaluation of coronary artery disease in an intermediate-risk population. J Nucl Med 2007;48:1424-30.
Berman DS, Wong ND, Gransar H, Miranda-Peats R, Dahlbeck J, Hayes SW, et al. Relationship between stress-induced myocardial ischemia and atherosclerosis measured by coronary calcium tomography. J Am Coll Cardiol 2004;44:923-30.
Hayat SA, Dwivedi G, Jacobsen A, Lim TK, Kinsey C, Senior R. Effects of left bundle-branch block on cardiac structure, function, perfusion, and perfusion reserve: Implications for myocardial contrast echocardiography versus radionuclide perfusion imaging for the detection of coronary artery disease. Circulation 2008;117:1832-41.
Tandogan I, Yetkin E, Ileri M, Ortapamuk H, Yanik A, Cehreli S, et al. Diagnosis of coronary artery disease with tl-201 SPECT in patients with left bundle branch block: Importance of alternative interpretation approaches for left anterior descending coronary lesions. Angiology 2001;52:103-8.
Depuey EG, Mahmarian JJ, Miller TD, Einstein AJ, Hansen CL, Holly TA, et al. Patient-centered imaging. J Nucl Cardiol 2012;19:185-215.
Cerqueira MD, Allman KC, Ficaro EP, Hansen CL, Nichols KJ, Thompson RC, et al. Recommendations for reducing radiation exposure in myocardial perfusion imaging. J Nucl Cardiol 2010;17:709-18.
Raman V, McWilliams ET, Holmberg SR, Miles K. Economic analysis of the use of coronary calcium scoring as an alternative to stress ECG in the non-invasive diagnosis of coronary artery disease. Eur Radiol 2012;22:579-87.
Sarwar A, Shaw LJ, Shapiro MD, Blankstein R, Hoffmann U, Cury RC, et al. Diagnostic and prognostic value of absence of coronary artery calcification. JACC Cardiovasc Imaging 2009;2:675-88.
Mouden M, Timmer JR, Reiffers S, Oostdijk AH, Knollema S, Ottervanger JP, et al. Coronary artery calcium scoring to exclude flow-limiting coronary artery disease in symptomatic stable patients at low or intermediate risk. Radiology 2013;269:77-83.
Disclosure
Dr. Engbers, Dr. Timmer, Dr. Ottervanger, Dr. Mouden, Dr. Oostdijk, Dr. Knollema, and Dr. Jager have nothing to disclose.
Author information
Authors and Affiliations
Corresponding authors
Additional information
See related editorial, doi:10.1007/s12350-015-0289-y.
Rights and permissions
About this article
Cite this article
Engbers, E.M., Timmer, J.R., Ottervanger, J.P. et al. Sequential SPECT/CT imaging for detection of coronary artery disease in a large cohort: evaluation of the need for additional imaging and radiation exposure. J. Nucl. Cardiol. 24, 212–223 (2017). https://doi.org/10.1007/s12350-015-0243-z
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-015-0243-z