Abstract
Multislice computed tomography (CT) is an emerging technique for the non-invasive detection of coronary stenoses. While the diagnostic accuracy of 4-slice scanners was limited, 16-slice CT imagers showed promising results due to increased temporal and spatial resolution. These technical advances prompted us to evaluate the diagnostic performance of 64-slice CT coronary angiography in the detection of significant stenoses (defined as ≥ 50% luminal diameter reduction) versus invasive quantitative coronary angiography (QCA). Thirty-five patients with stable angina pectoris underwent CT coronary angiography performed with a 64-slice scanner (gantry rotation time 330 ms, individual detector width 0.6 mm) prior to conventional coronary angiography. Patients with heart rates >70 beats/min received 100 mg metoprolol orally. One hundred millilitres of contrast agent with an iodine concentration of 400 mgl/ml were injected at a rate of 5 ml/s into the antecubital vein. The CT scan was triggered with the bolus tracking technique. The sensitivity, specificity and the positive and negative predictive values of 64-slice CT were 99%, 96%, 78% and 99%, respectively, on a per-segment basis. The values obtained on a per-patient basis were 100%, 90%, 96% and 100%, respectively. When referral to catheterisation is questionable, CT coronary angiography may identify subjects with normal angiograms and consistently decrease the number of unnecessary invasive procedures.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Multislice computed tomography (CT) coronary angiography is an emerging technique that allows the non-invasive detection of significant coronary stenoses. Various studies have been published exploring the diagnostic performance of CT coronary angiography using different scanner generations [1–3]. Clinical application of 4-slice CT coronary angiography was limited, due to a considerable number of non-assessable vessels (up to 39% of the included vessels) [4] as a result of a limited resolution and a relatively long breath hold of approximately 40 s. Sixteen-slice CT coronary angiography showed an improved diagnostic accuracy for the detection of significant stenoses due to an increased temporal and spatial resolution and shorter breath-hold time (approximately 20 s) [5–11]. However, these studies only evaluated coronary vessels with a luminal diameter above 1.5 mm or 2.0 mm. Most recently, a new generation of CT scanners was introduced. These scanners render 64 slices per rotation and offer a temporal resolution of 165 ms and an unprecedented spatial resolution of isotropic 0.4 mm3 [12]. These technical advances prompted us to evaluate the diagnostic performance of 64-slice CT coronary angiography to detect significant stenoses (defined as ≥50% lumen diameter reduction) in the entire coronary tree in a patient cohort with stable angina pectoris.
Materials and methods
Subjects
Thirty-five consecutive patients with stable angina pectoris (21 men; mean age±SD: 61±10 years, range: 46–80 years) underwent 64-slice CT coronary angiography within 15 days prior to coronary catheterisation. Patients exhibiting sinus heart rhythm incapable of holding their breath for 15 s and/or without contraindications to the administration of iodinated contrast agents were prospectively included. Exclusion criteria were the presence of arrhythmias, previous bypass graft surgery or percutaneous coronary intervention with stent implantation. The study protocol was approved by our institutional review board and all patients gave informed consent.
Patient preparation prior to CT
Patients with pre-scan heart rates above 70 beats/min received a single oral dose of 100 mg metoprolol 1 h prior to the CT scan.
CT scan protocol
All patients underwent CT coronary angiography using a 64-slice CT scanner (Sensation 64, Siemens, Forchheim, Germany). The scan parameters used for CT coronary angiography are detailed in Table 1. A bolus of 100 ml contrast material (iomeprol, Iomeron 400, Bracco, Milan, Italy) was injected into the antecubital vein (flow rate 5 ml/s) and the CT scan was triggered with a bolus tracking technique.
Radiation exposure associated to this scan protocol, calculated using a dedicated software package (WinDose, Institute of Medical Physics, Erlangen, Germany), was 15:20 mSv (male:female, respectively).
CT image reconstruction
A retrospective ECG-gated technique was used for image reconstruction. The images were reconstructed with data acquired during a single heartbeat. The data sets were reconstructed during the mid-to-end diastolic phase, with reconstruction windows set at −300 ms to −450 ms before the next R-wave or 60% to 70% of the R–R interval. In the case of insufficient image quality, additional reconstructions during the end-systolic phase (25% to 35% of the R–R interval) were performed. When mildly irregular heart rates were encountered, such as bundle branch blocks or premature beats, the temporal variability in the reconstruction phase were compensated for manually with ECG editing. Inaccurate detection of the R waves was corrected and temporal windows applied to premature beats were deleted, filling the next diastolic interval with one or more temporal windows to avoid data gaps. The reconstructed slice thickness was 0.75 mm, with an increment of 0.4 mm. All of the CT data sets were filtered with a medium-soft convolution kernel.
CT image analysis
The CT scans were scored by two experienced readers independently and were blinded of the results of conventional coronary angiography. Inter-observer agreement was calculated. In the cases of diverging opinions, an agreement was reached by consensus.
The maximum intensity projections were used in order to provide an anatomical overview of the coronary arteries and to identify side branches. Multi-planar reformatted images were used to visually classify lesions as significant or non-significant.
The image quality was evaluated on a per-segment basis and classified as good (absence of image-degrading artefacts related to motion, calcification or noise), adequate (presence of artefacts but images still suitable for evaluation, albeit with moderate confidence) or poor (presence of severe image-degrading artefacts, resulting in low diagnostic confidence). Reasons accounting for poor image quality were identified in calcification of the vessel wall, motion artefacts and low contrast-to-noise ratio. Calcification was rated as absent, small and isolated, dense and eccentric or bulky. Motion artefacts were defined as any blurring of the vessel contour due to movement. A low contrast-to-noise ratio was recorded in cases with scarce vessel enhancement, resulting in noisy images.
Quantitative coronary angiography (QCA)
All coronary segments visualised at catheterisation were included for comparison with CT. The segments were classified according to a modified 17-segment American Heart Association (AHA) model [13]. A single observer blinded to the CT results quantitatively evaluated the coronary lumen of all coronary segments on two projections using dedicated software (CAAS, Pie Medical, Maastricht, The Netherlands). Stenoses were scored as significant in the case of a mean lumen diameter reduction of ≥50% in two orthogonal projections.
Radiation exposure associated with diagnostic conventional angiography was 6:7 mSv (male:female, respectively).
Statistics
With QCA as the standard of reference, the diagnostic accuracy of CT coronary angiography for the detection of haemodynamically significant lesions in coronary arteries is expressed in terms of the sensitivity, specificity and the positive and negative predictive values with the corresponding 95% central confidence intervals.
The diagnostic performance was calculated on a per-segment, per-vessel (presence or absence of at least one significant lesion along each of the major coronary arteries) and per-patient (presence or absence of any lesions in each patient) basis.
Results
Prevalence of disease and patient co-morbidity
Overall, 67 significant lesions were detected by conventional coronary angiography, resulting in a prevalence of 1.9 lesions per patient.
Conventional angiography revealed no significant stenoses in 10 patients (29%). Ten (29%) patients had 1-vessel disease, 8 (23%) had 2-vessel disease and 7 (19%) had 3-vessel disease. No significant left main disease was found in any patient.
Patient co-morbidity and ongoing medication are reported in Table 2.
CT results
Oral metoprolol was administered in 77% (27/35) of the patients. As a result, the average heart rate during the scan was 58±6 beats/min versus 68±9 beats/min before the preparation.
The average scan time was 13±1 seconds (range 11–15 seconds). No significant adverse reactions to the contrast material were recorded.
After the acquisition of the angiographic part of the scan, additional reconstructions in the telesystolic phase were obtained in 31% (11/35) of the CT scans. ECG editing was necessary in 8% (3/35) of the scans.
A total of 494 coronary segments were available for comparison between coronary angiography and CT.
All except for one (66/67) significant coronary stenoses were correctly identified at CT. One false-negative result was scored in the mid-portion of a left anterior descending artery affected by calcification and motion artefacts, and accounting for a 52% stenosis at QCA.
CT image quality was judged to be good, moderate and poor in 92% (455/494), 5% (25/494), and 3% (14/494) of the included segments, respectively. The reasons for poor image quality and for incorrect CT findings are summarised in Fig. 1. The reasons for poor image quality affecting the assessability of the right coronary artery were motion artefacts (present in 7/7 segments), whereas a low contrast-to-noise ratio hampered the evaluation of posterior descending and posterolateral arteries (2/2). Bulky calcifications of the vessel wall causing a blooming effect and partial volume averaging were the major detrimental factors for the evaluation of both the left circumflex (2/2) and the left anterior descending (3/3, motion artefacts present in 1/3) arteries with their branches. However, none of the coronary segments were excluded from analysis due to limited image quality.
Image quality, artefacts and incorrect CT results. Motion artefacts account for half of the cases rated as being of poor image quality, but only for 2/20 cases of incorrect CT findings. Calcification of the vessel wall, either bulky, eccentric or isolated, is associated to 17/20 falsely positive and falsely negative CT results
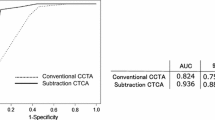
Diagnostic accuracy of 64-slice CT
The sensitivity, specificity and the positive and negative predictive values of 64-slice CT in the detection of significant coronary artery stenoses were obtained for the 494 coronary segments available for comparison. The values (confidence intervals) obtained on all segments are 99% (92–100), 96% (93–97), 78% (68–85) and 99% (99–100), respectively. On a per-patient basis, the values (confidence intervals) are 100% (87–100), 90% (59–98), 96% (81–99) and 100% (69–100), respectively.
Table 3 details the accuracy of CT in the individual coronary segments according to the AHA classification [13]. The results of all coronary segments, coronary vessels and patients are summarised in Table 4.
Inter-observer variability for the detection of significant lesions had κ-values of 0.73.
Discussion
Earlier generations of multislice CT scanners showed promise for the non-invasive detection of coronary stenoses [1–11]. However, the reported accuracy was obtained on the basis of analysable coronary segments rather than on all coronary segments. A recent study showed promising results of 64-slice CT coronary angiography in the detection of significant stenoses using a CT scanner with a rotation time of 375 ms [14]. Still, coronary branches with a diameter below the threshold of 1.5 mm were excluded from the comparative analysis. Reducing the gantry rotation time to 330 ms provided improvements in the sensitivity and specificity. Two recent papers reported sensitivity and specificity values of 86% and 95% [15] and 73% and 97% [16] in cohorts of patients referred for catheterisation. No calibre threshold was set in those studies. However, 12% of the segments [15] and 4/59 patients [16] were excluded from analysis because of poor image quality. In our population, 64-slice CT coronary angiography detected significant coronary stenoses of the entire coronary tree with a sensitivity of 99% and a specificity of 96% when compared to conventional invasive coronary angiography. Such results were obtained by including all coronary branches available for visualisation at conventional angiography and CT, regardless of the vessel diameter. In addition, none of the coronary segments available were excluded from analysis according to image quality. Thus, our results demonstrate the diagnostic accuracy of the technique to assess the entire coronary tree in the "real" clinical context.
Outcomes
All patients with significant coronary artery disease were correctly diagnosed, and only a single coronary lesion was missed at CT (sensitivity per-patient 100%, per-segment 99%). The missed lesion was found to be responsible for a 52% stenosis at QCA and was localised in the mid-tract of the left anterior descending artery. Dense eccentric calcifications and motion artefacts were scored as being responsible for poor image quality.
All but one patient with angiographically normal coronary angiograms were correctly identified at CT, which makes the technique reliable for ruling out significant coronary obstructions (specificity per-patient 90%, per-segment 96%). This brings some meaningful implications in a population where 29% (10/35) of the patients had negative angiograms, in that 9/10 unnecessary catheterisation procedures could have been avoided on the basis of CT results. This observation also counterbalances to some extent the drawback of a higher radiation dose of multislice CT compared to cardiac catheterisation, standing the periprocedural risk of, sometimes major, complications associated to the latter.
Figures 2 and 3 are examples of coronary artery stenoses detected with 64-slice CT and coronary angiography at the level of the posterolateral artery and first obtuse marginal branch, respectively.
a–d 54-year-old patient with stable angina pectoris. a 64-slice CT volume-rendered image. b 1-mm-thick curved maximum intensity projection. 0.75-mm-thick multiplanar reconstruction. d Conventional angiogram. A lesion is visible in the first marginal obtuse branch (arrowheads). Luminal narrowing determined at QCA was 64%
Specifications and scan technique shaping diagnostic accuracy
The capability to image the entire coronary tree is conceivably feasible due, in the first instance, to the technical advances of 64-slice CT scanners featuring high x-ray output, smaller individual detectors arranged in wider arrays and faster gantry rotation speed. With the above-mentioned scan parameters, an isotropic spatial resolution of 0.4 mm3 is achieved [12]. Likewise, the temporal resolution, obtained from the reconstruction of data acquired during half x-ray tube rotation, is suitable for "freezing" the beating heart.
Indeed, although motion artefacts are a major factor affecting the image quality perceived by the examiner (Fig. 1), on the other hand, only one false-negative and 1/19 false-positive CT findings were secondary to motion artefacts in our series, in patients whose heart rates were 68 beats/min and 65 beats/min, respectively. Since motion artefacts deteriorate the quality of a CT data set, the capability to find additional reconstruction windows within the cardiac cycle may allow us to minimise blurring and double-contouring, at least in a portion of the data set, thus providing complementary images suitable for evaluation. In a similar fashion, artefacts induced by mild heart rate irregularities, such as premature beats, can be compensated for with manual ECG editing. The choice of a proper reconstruction window as a key factor to a clinically reliable diagnosis of coronary lesions was also pointed out by Zhang et al. [17] and Hamoir et al. [18]. Conversely, the most common cause of incorrect CT diagnosis in our population was calcification of the vessel wall, either bulky (4/17), dense and eccentric (9/17) or isolated (4/17). Such findings are in line with the notion that the assessment of significant coronary stenoses with CT is more difficult when many calcifications are present [4]. However, it is also reported that important coronary calcification should not be used as an indication for deferring multislice CT coronary angiography [19].
In order to obtain prominent vascular enhancement, a further prerequisite has to be reproducibly fulfilled for robust coronary CT angiography: the volume, injection rate and concentration of the contrast agent must be optimised into dedicated injection protocols [20–23]. Bolus tracking is a sophisticated synchronisation technique which monitors attenuation changes in the aorta and triggers the CT scan when a threshold value is reached. Hence, the 11–15 s scan window is operated during the expected peak of coronary enhancement to image coronary arteries with optimal contrast resolution.
It is expected that bolus geometry and dynamics considerations differ slightly when applied to tiny coronary side branches. As a rule, distal vessels have a small diameter, contain less blood and, thus, suffer from poor contrast-to-noise resolution. Therefore, we used the contrast agent with the highest iodine concentration available to improve the opacification of smaller vessels and the visualisation of coronary side branches and collateral pathways [24].
The results of diagnostic accuracy reported by Mollet et al. [25], who obtained 95% sensitivity and 98% specificity in a population of stable and unstable patients examined with a 16-slice CT scanner, are not in contrast with the aforementioned considerations. Indeed, the technical parameters featured by the newer generation 16-slice scanner used in that study were gantry rotation speed of 375 ms, detector width of 0.75 mm and high x-ray output. The iodine concentration of the contrast bolus was equally chosen at 400 mgI/ml.
As a matter of fact, the interpretability of coronary images obtained with multislice CT has matched the improvement of hardware equipment and the development of the scanning technique, namely, faster gantry rotation speed, smaller individual detector width, higher x-ray output and optimised protocols for contrast agent administration and synchronisation. This created a distance between 4-slice and the first generation of 16-slice scanners on one side and the current CT scanners. Our experience suggests how 64-slice CT scanners, in association with an optimised scanning technique, provide images suitable for reliable interpretation. In association with appropriate operator training, a role for multislice CT might be shaped as a non-invasive tool capable of assisting management options in selected cardiological patients. In particular, the capability of displaying the extent and morphology of coronary atherosclerosis may help direct treatment options to either conservative therapy, percutaneous intervention or surgery [26].
Limitations of the study
Nineteen out of 494 lesions scored as being significant at coronary CT revealed to be haemodynamically insignificant at conventional angiography (false-positive findings). This could, in part, be explained with the fact that, for lesions whose CT interpretation was uncertain, the chance of overestimation of the lesion severity was deemed less undesirable than the risk of underestimation, reflecting a clinical setting where CT plays the role of a decision tool to screen patients for referral to catheterisation. In these settings, where the overestimation of the severity of lesions would refer the patient for coronary catheterisation, overlooking significant stenoses might have much more serious consequences in a symptomatic population. Besides, the positive predictive value of CT rises from 78% to 96% when the patient, not the individual lesion, is considered.
A high pre-test prevalence of disease in the population available for comparison is, somehow, inevitable, since invasive angiography is generally not performed in subjects with suspected or known coronary artery disease in the absence of symptoms. Even in asymptomatic patients with demonstrated inducible ischemia, controversy exists as whether coronary angiography should be performed, unless additional risk factors such as advanced age, diabetes mellitus or lifestyle coexist. According to the American College of Cardiologists/American Heart Association guidelines [27], coronary angiography recommendations in patients with suspected or known stable coronary artery disease are limited to patients with angina pectoris or non-specific chest pain with positive (or contraindicated) stress testing.
We did not perform quantitative CT analysis of the lesions, which is instead reported by Raff et al. [15] and Leber et al. [16]. However, although correlation is reported between quantitative diameter stenosis at multislice CT and QCA, the differences of the percentage diameter stenosis assessed by the two methods show significant variability, thus, suggesting that the quantification of lesions by means of CT cannot reliably substitute QCA at the present time.
Conclusion
Accuracy of coronary CT angiography performed with a 64-slice scanner for the assessment of disease of the entire coronary tree is superior to that of earlier-generation CT scanners.
The sensitivity in the detection of significant lesions is 99% and the specificity is 96%. The predictive value of normal CT findings is also 99%. When referral to catheterisation is questionable, CT coronary angiography may identify subjects with normal angiograms and consistently decrease the number of unnecessary invasive procedures.
References
Nieman K, Oudkerk M, Rensing BJ, van Ooijen P, Munne A, van Geuns RJ, de Feyter PJ (2001) Coronary angiography with multi-slice computed tomography. Lancet 357:599–603
Knez A, Becker CR, Leber A, Ohnesorge B, Becker A, White C, Haberl R, Reiser MF, Steinbeck G (2001) Usefulness of multislice spiral computed tomography angiography for determination of coronary artery stenoses. Am J Cardiol 88:1191–1194
Vogl TJ, Abolmaali ND, Diebold T, Engelmann K, Ay M, Dogan S, Wimmer-Greinecker G, Moritz A, Herzog C (2002) Techniques for the detection of coronary atherosclerosis: multi-detector row CT coronary angiography. Radiology 223:212–220
Kuettner A, Kopp AF, Schroeder S, Rieger T, Brunn J, Meisner C, Heuschmid M, Trabold T, Burgstahler C, Martensen J, Schoebel W, Selbmann HK, Claussen CD (2004) Diagnostic accuracy of multidetector computed tomography coronary angiography in patients with angiographically proven coronary artery disease. J Am Coll Cardiol 43:831–839
Nieman K, Cademartiri F, Lemos PA, Raaijmakers R, Pattynama PM, de Feyter PJ (2002) Reliable noninvasive coronary angiography with fast submillimeter multislice spiral computed tomography. Circulation 106:2051–2054
Heuschmid M, Kuettner A, Schroeder S, Trabold T, Feyer A, Seemann MD, Kuzo R, Claussen CD, Kopp AF (2005) ECG-gated 16-MDCT of the coronary arteries: assessment of image quality and accuracy in detecting stenoses. AJR Am J Roentgenol 184:1413–1419
Ropers D, Baum U, Pohle K, Anders K, Ulzheimer S, Ohnesorge B, Schlundt C, Bautz W, Daniel WG, Achenbach S (2003) Detection of coronary artery stenoses with thin-slice multi-detector row spiral computed tomography and multiplanar reconstruction. Circulation 107:664–666
Kuettner A, Trabold T, Schroeder S, Feyer A, Beck T, Brueckner A, Heuschmid M, Burgstahler C, Kopp AF, Claussen CD (2004) Noninvasive detection of coronary lesions using 16-detector multislice spiral computed tomography technology: initial clinical results. J Am Coll Cardiol 44:1230–1237
Martuscelli E, Romagnoli A, D’Eliseo A, Razzini C, Tomassini M, Sperandio M, Simonetti G, Romeo F (2004) Accuracy of thin-slice computed tomography in the detection of coronary stenoses. Eur Heart J 25:1043–1048
Hoffmann MH, Shi H, Schmitz BL, Schmid FT, Lieberknecht M, Schulze R, Ludwig B, Kroschel U, Jahnke N, Haerer W, Brambs HJ, Aschoff AJ (2005) Noninvasive coronary angiography with multislice computed tomography. JAMA 293:2471–2478
Mollet NR, Cademartiri F, Nieman K, Saia F, Lemos PA, McFadden EP, Pattynama PM, Serruys PW, Krestin GP, de Feyter PJ (2004) Multislice spiral computed tomography coronary angiography in patients with stable angina pectoris. J Am Coll Cardiol 43:2265–2270
Flohr T, Stierstorfer K, Raupach R, Ulzheimer S, Bruder H (2004) Performance evaluation of a 64-slice CT system with z-flying focal spot. Rofo 176:1803–1810
Austen WG, Edwards JE, Frye RL, Gensini GG, Gott VL, Griffith LS, McGoon DC, Murphy ML, Roe BB (1975) A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation 51:5–40
Leschka S, Alkadhi H, Plass A, Desbiolles L, Grunenfelder J, Marincek B, Wildermuth S (2005) Accuracy of MSCT coronary angiography with 64-slice technology: first experience. Eur Heart J 26:1482–1487
Raff GL, Gallagher MJ, O’Neill WW, Goldstein JA (2005) Diagnostic accuracy of noninvasive coronary angiography using 64-slice spiral computed tomography. J Am Coll Cardiol 46:552–557
Leber AW, Knez A, von Ziegler F, Becker A, Nikolaou K, Paul S, Wintersperger B, Reiser M, Becker CR, Steinbeck G, Boekstegers P (2005) Quantification of obstructive and nonobstructive coronary lesions by 64-slice computed tomography: a comparative study with quantitative coronary angiography and intravascular ultrasound. J Am Coll Cardiol 46:147–154
Zhang SZ, Hu XH, Zhang QW, Huang WX (2005) Evaluation of computed tomography coronary angiography in patients with a high heart rate using 16-slice spiral computed tomography with 0.37-s gantry rotation time. Eur Radiol 15:1105–1109
Hamoir XL, Flohr T, Hamoir V, Labaki L, Tricquet JY, Duhamel A, Kirsch J (2005) Coronary arteries: assessment of image quality and optimal reconstruction window in retrospective ECG-gated multislice CT at 375-ms gantry rotation time. Eur Radiol 15:296–304
Cademartiri F, Mollet NR, Lemos PA, Saia F, Runza G, Midiri M, Krestin GP, de Feyter PJ (2005) Impact of coronary calcium score on diagnostic accuracy for the detection of significant coronary stenosis with multislice computed tomography angiography. Am J Cardiol 95:1225–1227
Cademartiri F, Nieman K, van der Lugt A, Raaijmakers RH, Mollet N, Pattynama PM, de Feyter PJ, Krestin GP (2004) Intravenous contrast material administration at 16-detector row helical CT coronary angiography: test bolus versus bolus-tracking technique. Radiology 233:817–823
Bae KT, Heiken JP, Brink JA (1998) Aortic and hepatic contrast medium enhancement at CT. Part II. Effect of reduced cardiac output in a porcine model. Radiology 207:657–662
Bae KT, Heiken JP, Brink JA (1998) Aortic and hepatic contrast medium enhancement at CT. Part I. Prediction with a computer model. Radiology 207:647–655
Bae KT, Heiken JP, Brink JA (1998) Aortic and hepatic peak enhancement at CT: effect of contrast medium injection rate—pharmacokinetic analysis and experimental porcine model. Radiology 206:455–464
Cademartiri F, Mollet NR, van der Lugt A, McFadden EP, Stijnen T, de Feyter PJ, Krestin GP (2005) Intravenous contrast material administration at helical 16-detector row CT coronary angiography: effect of iodine concentration on vascular attenuation. Radiology 236:661–665
Mollet NR, Cademartiri F, Krestin GP, McFadden EP, Arampatzis CA, Serruys PW, de Feyter PJ (2005) Improved diagnostic accuracy with 16-row multi-slice computed tomography coronary angiography. J Am Coll Cardiol 45:128–132
Becker CR (2005) Coronary CT angiography in symptomatic patients. Eur Radiol 15(Suppl 2):B33–B41
Scanlon PJ, Faxon DP, Audet AM, Carabello B, Dehmer GJ, Eagle KA, Legako RD, Leon DF, Murray JA, Nissen SE, Pepine CJ, Watson RM, Ritchie JL, Gibbons RJ, Cheitlin MD, Gardner TJ, Garson A Jr, Russell RO Jr, Ryan TJ, Smith SC Jr (1999) ACC/AHA guidelines for coronary angiography: executive summary and recommendations. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Coronary Angiography) developed in collaboration with the Society for Cardiac Angiography and Interventions. Circulation 99:2345–2357
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pugliese, F., Mollet, N.R.A., Runza, G. et al. Diagnostic accuracy of non-invasive 64-slice CT coronary angiography in patients with stable angina pectoris. Eur Radiol 16, 575–582 (2006). https://doi.org/10.1007/s00330-005-0041-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-005-0041-0