Abstract
Acute-on-chronic liver failure is a distinct syndrome characterized by a rapid progression of liver disease culminating in organ failure and death. The only definitive treatment is liver transplantation. However, there is a possible element of reversibility and hepatic regeneration if the acute insult can be tided over. Exogenously administered growth factors may stimulate hepatocytes, hepatic progenitor cells and bone marrow-derived cells to supplement hepatic regeneration. The proposed review is intended to provide an in-depth analysis of the individual components of hepatic and bone marrow niches and highlight the growing role of various growth factors in liver regeneration in health and in liver failure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Most of the patients referred to a specialized hepatology center suffer from either decompensation of end-stage chronic liver disease or an acute deterioration of known or unknown underlying chronic liver disease. Chronic hepatic decompensation occurs in end-stage cirrhotic patients with progression of their underlying liver disease. The progression of primary liver disease is responsible for chronic decompensation and is irreversible in the majority of cases. Acute-on-chronic liver failure (ACLF) results because of an acute insult from a precipitating factor, and if the liver can be supported through the crisis, patient can make a clinical recovery.
ACLF was initially defined by Sen et al. as the development of recent onset (<3 months) of a first episode of liver failure in the form of ascites, jaundice, hepatic encephalopathy, hepatorenal syndrome, upper gastrointestinal bleeding in patients with diagnosed or undiagnosed chronic liver disease due to the effects of precipitating events such as complications of sepsis, ischemia or additional superimposed liver injury due to alcohol, a hepatotrophic virus or hepatotoxic drugs [1].
Subsequently, the Asian Pacific Association for the Study of the Liver consensus defined ACLF as an acute hepatic insult manifesting as jaundice (serum bilirubin ≥ 5 mg/dl) and coagulopathy (INR ≥ 1.5), complicated within 4 weeks by ascites and/or encephalopathy in a patient with previously diagnosed or undiagnosed chronic liver disease [2]. Kjaergard et al. [3] reported a mortality of 51 % mainly due to multiorgan failure. Recently, the EASL–CLIF consortium defined ACLF as an acute decompensation of cirrhosis in the form of development of ascites, hepatic encephalopathy, GI hemorrhage or bacterial infections, or a combination of these, associated with at least two organ failures with one being kidney in the form of serum creatinine > 1.5 mg/dl, leading to a high 28-day mortality of more than 15 % [4]. Wlodzimirow et al. [5] found 13 different definitions of ACLF in the literature. In a recent study, Garg et al. [6] suggested that it is the first 2 weeks that determine the outcome in patients with ACLF, i.e. before the appearance of organ failure in ACLF. The need to stress this point in ACLF is to highlight the potential for reversibility. It is imperative therefore to identify this therapeutic ‘golden window’ as treatment strategies developed during this period can change the course of the illness. New options currently being evaluated include removal of toxic metabolites using liver dialysis, immune modulation for reducing ongoing necrosis and stimulating hepatic regeneration, modulation of hepatic regeneration through growth factors and bone marrow stimulation, and hepatocyte transplantation. The present review addresses the basics of hepatic regeneration in health and disease and the potential role of growth factors.
Liver regeneration
If we look into the basis of liver injury secondary to different etiologies, vulnerable hepatocytes can undergo apoptosis via an extrinsic death receptor-mediated pathway or alternatively intracellular stress can activate the intrinsic pathway of apoptosis. Both pathways converge on mitochondria, and mitochondrial dysfunction is a prerequisite for hepatocyte apoptosis. Persistent apoptosis is a feature of chronic liver diseases, and massive apoptosis is a feature of acute liver failure. Fibrogenesis is stimulated by ongoing hepatocyte apoptosis, eventually resulting in cirrhosis of the liver in chronic liver diseases [7]. If we look into the pathophysiology of ACLF, the systemic inflammatory response, characterized by a predominantly proinflammatory cytokine profile, may cause the transition from stable cirrhosis to ACLF. Proinflammatory cytokines are believed to mediate hepatic inflammation, apoptosis and necrosis of liver cells, cholestasis and fibrosis. Elevated serum levels of several cytokines and their receptors, including TNFα, sTNF-aR1, sTNF-aR2, IL-2, IL-2R, IL-4, IL-6, IL-8, IL-10 and interferon-c, have been described in patients with ACLF. Cytokines such as TNFα and IL-6 work as a double-edged sword. On the one hand, they promote liver regeneration by inducing acute-phase proteins and hepatic proliferation and exhibiting antiapoptotic effects; on the other hand, these cytokines induce hepatic inflammation and necrosis and involve immunopathogenesis in ACLF. Many cytokines such as IL-6 and TNFα and growth factors such as TGFα, EGF and HGF are implicated in different stages of the regenerative process [8].
In normal adult liver, hepatocytes have a life span of about 200 days. After partial hepatectomy (PH), proliferation of the main epithelial compartments (hepatocytes and cholangiocytes), followed by proliferation of the mesenchymal cells [hematopoietic stem cells (HSCs) and endothelial cells] quickly restores the liver. In rodents, the liver can restore its original volume after two-thirds hepatectomy in approximately 10 days [9].
Stem cells and liver regeneration
Liver regeneration occurs by three different methods [10, 11]. Acute liver injury, for example in the PH model, results in rapid and effective regeneration with hepatocytes undergoing mitosis. When normal hepatocyte replication is impaired (by 2-acetylaminofluorene or retrorsine in animal models and by alcoholic liver disease or hepatitis C virus infection, among others, in humans), endogenous hepatic progenitor cells (HPCs) are activated and participate in the liver regeneration process.
The presence of HPC activation during chronic liver disease however is probably a feature of eventual exhaustion of hepatocyte proliferation over many years or decades [12, 13]. The clinical relevance of the HPC reaction is implied by its frequency in a wide variety of human liver diseases including acute liver failure, chronic viral hepatitis, alcoholic disease, nonalcoholic fatty liver disease, immune cholangiopathies and hereditary liver disorders [14]. Characteristically, the magnitude of HPC activation corresponds to the severity of liver fibrosis and inflammation [15]. In addition, the more aggressive a hepatocellular injury, the higher the proportion of observed HPCs that resemble intermediate hepatocytes [16].
Stem cells and niches in the liver
The liver contains different cell types with stem cell properties: hepatocytes, HPCs and hepatic stellate cells (HepSCs) [17].
HPCs are capable of differentiating toward the biliary and the hepatocytic lineages and represent the human counterpart of the oval cells (OC) in murine liver. They are heterogeneous, consisting of a spectrum of cells ranging from an immature phenotype to mature cholangiocytes and intermediate hepatocytes [18, 19].
Adult stem cells maintain their characteristics throughout their lifetime in a special microenvironment, the so-called ‘stem cell niche’ [20]. Stem cell niches are composed of microenvironmental cells that nurture stem cells and enable them to maintain tissue homeostasis [21].
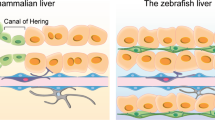
In adult livers, the stem cell niche has been shown to reside in the most proximal biliary structures, the canals of Hering [22]. Recent work has shown that stem cells can be found in the biliary tree [23] and common bile duct [24]. HepSCs possess signaling pathways required for stem cell functions such as hedgehog and β-catenin-dependent Wnt signaling [25].
We recently conducted a human study demonstrating the role of HepSCs in hepatic regeneration in ACLF. This is the first such comparative study highlighting the spectrum of HepSC activation in ACLF [26]. HepSC activation was found to be significantly more in ACLF and was observed with decreasing frequency in ACLF, acute hepatitis, cirrhosis, chronic hepatitis and normal living donor liver biopsies, respectively. There was also a significant correlation of HepSCs with HPCs, suggesting their role in liver regeneration in ACLF (Table 1; Fig. 1) [26].
The α smooth muscle actin (α SMA) immunohistochemistry to show activated HSCs. The proportion of expression was maximum in ACLF (panel a), followed by chronic viral hepatitis (panel b) and minimal expression in acute hepatitis (panel c) [25]
Molecular mechanisms of HPC activation
HPCs play a crucial role in hepatic regeneration and liver remodeling. However, the mechanisms controlling the HPC response are under intense investigation. In general, although many of the signals that control liver regeneration in the normal liver (i.e. via hepatocyte replication) are involved in HPC-mediated regeneration.
Various signaling cascades are regulating the activation of HPC by regulating the mitosis, migration and differentiation of HPC. Tumor necrosis factor super-family TNFα and TNF-like weak inducer of apoptosis (TWEAK) both play a pivotal role in HPC activation via NF-kb signaling and regulate the proliferation of HPC [27, 28].
The role of IFN-γ in liver regeneration is quite controversial. A recent study has shown that IFN-γ inhibits HPC/oval cell activation in chronic liver damage, which may inhibit liver regeneration [29]. Other data have also confirmed negative regulation of liver regeneration in the presence of IFN-γ [30]. It also induces liver inflammation and necrosis and contributes to immunopathogenesis. A variety of cytokines, including IL6, oncostatin M (OSM) and leukemia inhibitor factor (LIF), act through the gp130 signaling pathway [31]. Following homodimerization, gp130 activates the Janus kinase/signal transducer and activator of transcription and extracellular signal-regulated kinase pathways. STAT3 and its targets are upregulated during the rodent OC response and during human chronic liver disease [32, 33].
Aside from TWEAK, gp130 is the only signal demonstrated to date capable of initiating an OC response alone. Gp130 is potentially a key element in the activation and expansion of hepatic HPCs. Both LIF and OSM participate in a variety of processes including the regulation of growth and differentiation. The action of LIF is mediated via the LIF receptor (LIFR), which is composed of LIFR-β and gp130. Both LIF and LIFR are upregulated during the OC reaction in the rat [34] and human cirrhotic livers, with LIFR-β localizing to proliferating CK7+ intermediate hepatobiliary cells [35].
OSM influences extrahepatic progenitor cell activity and extracellular matrix (ECM) deposition, in addition to inducing an acute phase response. OSM has been described to promote the proliferation and differentiation of fetal hepatoblasts [36] and OCs lines [37], respectively.
There are currently a variety of established markers for HPCs. They express biliary markers (such as biliary-type CKs, oval cell marker 6, CK7 and CK19), and a subset of these cells expresses (fetal) hepatocytic markers (such as α-fetoprotein, hepPar-1 and albumin), and hematopoietic markers [such as the receptor for stem cell factor (c-kit), CD34].
Role of bone marrow: the third component
Bone marrow acts as the third tier of regenerative response. However, it is not known whether this is synergistic to the intrahepatic regenerative response or occurs once the hepatic potential has been exhausted. Bone marrow and liver share an evolutionary conserved developmental relationship. In fact, hematopoiesis is well known to occur in the fetal liver. The bone marrow acts as a reservoir for multiple stem cell populations, including HSCs, mesenchymal stem cells (MSCs), endothelial progenitor cells (EPCs) and very small embryonic-like cells (VSELs), which are mobilized at varying degrees into the peripheral circulation following injury [38, 39] where they are thought to variably contribute to tissue repair and regeneration through paracrine effects and inconsistent levels of direct differentiation [40–42].
Clinically, HSCs have been shown to mobilize from the bone marrow into the circulation following a variety of injuries, including myocardial infarction [43], stroke [44], liver injury [45] and skin burns [46], although their contribution to tissue repair and regeneration is uncertain. Petersen et al. [47] for the first time showed that HSC can contribute to liver regeneration in the adult organism in vivo. They showed OC and hepatocyte chimerism in cross-strain or cross-sex bone marrow or whole liver transplantation and proposed the possibility of bone marrow-to-hepatocyte transdifferentiation. Lagasse et al. [48] used a mouse strain (fumaryl aceto-acetate hydrolase knockout) with an inherited liver disease (corresponding to human tyrosinemia type 1) that is fatal if not treated by supportive drugs. These mice could be definitively cured by HSC transplantation, demonstrating that functioning mature hepatocytes can result from this transplant procedure. Corresponding observations were reported by Theise et al. [49] and others in the human system, in which rare male hepatocytes were demonstrated in female recipients of male bone marrow transplants and in male recipients of female whole-organ liver transplants. Closer scrutiny of the data demonstrated that cell fusion rather than transdifferentiation appears to be responsible for liver regeneration in their model [49–53].
EPCs are mobilized in response to ischemic injury [54] and contribute to neovascularization in small animal models through a combination of direct cellular differentiation and indirect production of cytokines and growth factors (VEGF, SDF-1 and IGF-1) to promote the migration of mature endothelial cells and resident progenitor cells [55, 56]. Hematopoietic EPCs secrete high levels of cytokines, including VEGF, IL-8, HGF and granulocyte-colony stimulating factor (G-CSF), and are thought to contribute to vascular repair mainly through paracrine mechanisms [57, 58], but subsets of these cells have shown the ability to directly incorporate into the endothelium [59, 60]. Nonhematopoietic EPCs exhibit low levels of cytokine production and are thought to contribute to vascular repair mainly through the direct formation of vessels [61].
MSCs are multipotent, nonhematopoietic stromal cells that can be isolated from various adult organs and tissues, including bone marrow [62]. Sachetti et al. [63] found that self-renewing osteoprogenitors in human BM, able to generate bone and stroma and organize a hematopoietic microenvironment in vivo, are CD146high (a melanoma-associated cell adhesion molecule). These CD146+ cells are located in the subendothelial layer of BM sinusoids and represent adventitial reticular cells, a subpopulation of pericytes. As pericytes are found in nearly every other organ, it has been hypothesized that all MSCs found in different tissues are also derived from the pericyte fraction in vessels. MSCs are capable of differentiating into various mesenchymal lineages in vitro, including bone, muscle, cartilage and fat [62], as well as forming cells from other germ layers, such as dermatocytes and neuron-like cells [64, 65]. Mobilized BM–MSCs home to sites of injury where they are thought to contribute to tissue repair and regeneration mainly through paracrine support of injured cells (HGF, EGF, VEGF, sFRP-4) [66, 67] and regulation of ECM remodeling [68, 69], immune response (IL-1 antagonism, IL-10) [70] and local progenitor cell proliferation and differentiation [71]. Recent studies showed the beneficial effects of bone marrow mesenchymal stem cell transplantation in liver failure caused by hepatitis B with improved survival, reduction in MELD scores and no untoward side effects [72, 73].
Under physiologic conditions, bone marrow stem cells are thought to be maintained within their niche through tightly controlled interactions of chemokines, cytokines and growth factors with cellular receptors, as well as through the presence of specific adhesion and ECM molecules [74]. Following injury, there is evidence that cytokine release by vascular endothelium and activated platelets, combined with local upregulation of growth factors, alters this homeostasis by providing a signal gradient for bone marrow stem cell mobilization and homing [75–77]. SDF-1/CXCR4, nitric oxide, Jagged/Notch interactions and monocyte chemoattractant protein-1 (MCP-1)/CCR2 interactions are the various mechanisms thought to play an important role in this. Growth factors, such as VEGF and G-CSF, may also contribute to bone marrow stem cell mobilization and recruitment following injury, as exogenous administration of G-CSF and VEGF has been shown to enhance the mobilization of specific stem cell populations and promote neovascularization and tissue regeneration within ischemic or traumatic injury models [78–80] (Fig. 2).
Immunological basis of liver injury in ACLF. There is immunological (dis)balance in the form of reduced dendritic cells (DCs), monocyte anergy, increased CD8 cytoxicity, increased TH17 and consequent proinflammatory cytokines namely IFNr, TNFa and IL-17, culminating in parenchymal dysfunction of ACLF. By addition of GCSF, there is recruitment of DCs, polymorphonuclear neutrophils (PMNLs), bone marrow-derived macrophages (BMMs) and improved monocyte function with consequent reduction in proinflammatory cytokines
Potential of growth factors in hepatic regeneration
Despite this endogenous stem cell recruitment, the inability of most adult tissue to regenerate following injury suggests that these mechanisms are easily overwhelmed. This is largely because of the complexity of liver regeneration, which is governed by a synergistic interplay between a multitude of factors, namely the number of viable hepatocytes in the injured liver, the hepatic microenvironment or the “niche” with its intrinsic HPCs and their dynamic interactions with the nonparenchymal cells (HepSCs, sinusoidal endothelial cells and Kupffer cells), the inflammatory cytokine milieu and, last but not the least, the BM with its progenitors. Therapies attempting to augment bone marrow stem cell involvement have shown the ability to mitigate injury and enhance the regenerative capacity of adult tissue in a variety of preclinical models.
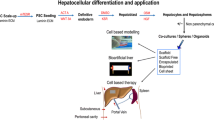
Mechanistically, these approaches can be divided into two main categories: enhancement of the endogenous stem cell response and augmentation of cell-based therapies. Enhancing a patient’s endogenous stem cell response following injury is clinically appealing because of the elimination of time and costs associated with cell harvest, ex vivo processing and transplantation. A variety of compounds have shown the ability to mobilize bone marrow-derived HSCs, MSCs, EPCs and VSELs [81, 82]. G-CSF decreases SDF-1 levels in the bone marrow [83]. Systemic administration of G-CSF has been shown to mobilize HSCs, EPCs and BM–MSCs and to improve outcomes in models of brain, liver and blood vessel injury [84–86]. Similarly, systemic administration of agents targeting the PI3K–Akt pathway, for example erythropoietin (EPO), an important mediator of cell survival and upstream modifier of eNOS, has been shown to mobilize EPCs and enhance their in vivo regenerative role [87–89]. Oh et al. [90] showed that treatment of adult bone marrow with hepatocyte growth factor could induce albumin and alpha fetoprotein expression via c-met and concluded that adult rat bone marrow contains a hepatic progenitor population. A meta-analysis of 21 trials involving 5,902 patients showed that use of recombinant human hepatocyte growth factor led to a significant reduction in overall mortality in ACLF with no serious adverse events [91]. Another intriguing protein recombinant ‘augmenter of liver regeneration’ was found to enhance hepatocyte proliferation by causing NF-κB activation, elevating polyamine levels by increasing the expression of c-Myc, ornithine decarboxylase and S-adenosylmethionine decarboxylase in the hepatocytes [92]. Even though a scarcity of data remains in the exact mechanism and contribution of each of these factors, the encouraging data that have emerged for the multifaceted action of growth factors in modulating the BM and the hepatic progenitor cell response by in vivo modulations from various trials in the recent past are a proof of concept and provide an impetus for actively exploring growth factors in the therapeutic armamentarium of patients with liver failure.
Effect on bone marrow and liver regeneration
Over the last decade, the importance of BM stem cell activation during liver disease has become apparent. CD34+- and CD133+ cells appear to be upregulated following liver resection or in diseased liver [93, 94]. BM-derived stem cells have been shown to differentiate into hepatocyte-like cells in vitro and in vivo [95].
A potential approach to improve BMC engraftment to the damaged liver could be their mobilization by using cytokine administration. G-CSF therapy has been widely studied in bone marrow transplant recipients and in the oncologic population [96]. In a study by Gaia et al. [97], BMC mobilization by G-CSF was observed in patients with severe liver cirrhosis. Spahr et al. [98] have reported that G-CSF mobilizes CD34+ cells, increases HGF and induces HPCs to proliferate within 7 days of administration in patients with alcoholic steatohepatitis.
The seminal work by Garg et al. has shown that use of G-CSF in ACLF was associated with 69 % survival compared to 29 % in the placebo group. It was the first randomized controlled trial that demonstrated a significant benefit from the use of G-CSF in the form of recruitment of CD34+ bone marrow stem cells leading to liver regeneration and affecting the outcome in the form of improved survival [99]. Another recently published double-blind randomized controlled trial by Duan et al. [100] showed that G-CSF therapy improved survival in patients associated with hepatitis B-related ACLF by increased neutrophil and more importantly CD34+ cell counts in the peripheral circulation.
EPO regulates red blood cell production by binding to its cell surface receptor, EPO-R, expressed on erythroid progenitor cells. Although EPO was originally believed to be an erythroid-specific hematopoietic cytokine, for over a decade, a substantial body of scientific evidence has accumulated to demonstrate that the biological effects of EPO are not limited to erythron [101]. In a study by Schmeding et al., rats undergoing 70–90 % hepatectomy received an intraportal venous administration of rEPO prior to resection or s/c injection for 3 days postoperatively. Regeneration capacity was studied by histology, immunohistochemistry (Ki-67, PCNA) and angiogenesis measured by VEGF and HIF. It was demonstrated that the 10-day survival rate increased significantly [102]. In a study by Greif et al., rats undergoing 70 % hepatectomy received an intraperitoneal injection of saline or rEPO (4 U/kg) 30 min prior to resection. In the EPO group, the mitotic index, Ki-67, vWF and PIPK signaling were higher on day 2 post surgery, suggestive of liver regeneration [103]. Ben Ari et al. recently investigated the effect of recombinant human EPO administration in acute liver failure induced by d-galactosamine/lipopolysaccharide in mice. They found that 90 % of mice with FHF survived for 24 h after rhEPO compared to the control group in which there was 100 % mortality. EPO caused a significant decrease in TNF-α and IL-1β (both serum and intrahepatic) associated with a decrease in NF-kB and JNK expression in mice with FHF compared to those not treated [104] (Fig. 3).
Growth factors such as GCSF and EPO act on both liver and bone marrow to recruit hematopoietic stem cells (HSCs), mesenchymal stem cells (MSCs), hepatic progenitor cells (HPCs), dendritic cells (DCs), bone marrow-derived macrophages (BMMs), endothelial progenitor cells (EPCs) and very small embryonic-like cells (VSELs) and hence augment liver regeneration
Effect on dendritic cells and liver regeneration
Dendritic cells (DCs) are a heterogeneous group of professional bone-marrow derived antigen-presenting cells required to process and present antigen to the naïve T cells for activation and expansion of antigen-specific T cells [105]. DCs are rare, ubiquitously distributed leukocytes, derived from CD34+ hematopoietic stem cells. In normal liver, they are restricted largely to the perivenular region, portal space and beneath the Glisson capsule, with a few cells scattered throughout the parenchyma.
DC dysfunction has been shown to play a major role in hepatitis B-related ACLF [106]. Restoration of the myeloid dendritic cell population improved the survival of ACLF patients receiving methylprednisolone therapy [107]. Growth factors help in recruitment of DCs in the liver. The cytokines fms-like tyrosine kinase 3 ligand (Flt3L) and GM-CSF mobilize DCs from bone marrow. GM-CSF is not only involved in the recruitment of DCs, but also in the generation of DCs from progenitor cells and monocytes. A study has shown increased liver DC numbers by Flt3L administration accelerated liver regeneration [108]. Other data have also confirmed increased number of liver DCs after PH, regulating the local immune response by inducing antiinflammatory IL-10 gene transcription and downregulation of proinflammatory gene IFN-γ, thus inducing hepatocyte proliferation and ultimately liver regeneration [109].
We have also shown lower frequencies of intrahepatic myeloid DCs and plasmacytoid DCs in nonsurvivors compared to survivors of ACLF. G-CSF enhanced the recruitment of plasmacytoid DCs, myeloid DCs and subsets of T cells including CD3, CD4 and CD8 cells and subsequently improved survival in these patients [110]. These data suggest that liver DCs may play a role in local immune regulation to support liver regeneration (Fig. 4).
Effect on macrophages and liver regeneration
The growth factors such as G-CSF and EPO modulate the synthesis of more specific cell types, mainly macrophages or monocytes. On the basis of previous studies in rat and mice models, it was observed that BM precursors differentiate into macrophages under the control of colony-stimulating factor-1 (CSF-1) via its receptor (CSF-1R). CSF-1 also regulates macrophage proliferation, viability and phenotypic fate [111].
In vitro studies by Thomas et al. showed that 7-day treatment of CSF-1 generated and accumulated macrophages in BM. Bone marrow macrophages (BMMs) possessed the characteristics of macrophage cell surface markers F4/80 and CD11b and markers of other leukocyte populations such as monocytes; T and B cells were not present in significant numbers [112].
Previous studies demonstrated that bone marrow-derived macrophages caused the recruitment of matrix metalloproteinase protein (MMP)-producing host cells into the hepatic scar [113]. MCP-1 and macrophage inflammatory protein 1α (MIP-1α) are members of the CC chemokine subfamily that bind to the CCR2 and CCR1/5 receptors of monocytes, respectively. These interactions contribute to the navigation of monocytes into target tissues during their maturation into macrophages. A recent study performed on a rat model showed that circulating monocytes have been exploited as an important progenitor cell resource for hepatocytes in vitro and are instrumental in the removal of fibrosis. In this study, CD14+ monocytes in peripheral blood stem cells contribute to hepatocyte regeneration and ECM remodeling in rat liver cirrhosis much more than CD14− cells and might offer a therapeutic alternative for patients with liver cirrhosis [114]. Monocytes produce IL-6 cytokine, which helps in liver regeneration.
The delivery of MCP-1 and MIP-1α-expressing BMMs to injured mice caused upregulation of hepatic MCP-1 and MIP-1α and the recruitment of endogenous macrophages. These macrophages produced MMP-13, whose actions include the degradation of fibrillar collagens and gelatin as well, and activation of other MMPs (such as MMP-9), hence contributing to liver regeneration. Also in recipient livers, BMMs expressed high antiinflammatory (IL-10), antifibrotic (MMP-13), proregenerative (TWEAK) and chemotactic (MCP-1, MIP-1α, MIP-2) mediators. Upon cessation of chronic liver injury, endogenous macrophages mediate hepatic scar remodeling through local MMP expression. The activities and expression of MMP increased while tissue inhibitor of metalloproteinase (TIMP)-1 expression was significantly reduced in monocyte-transplanted livers [112].
The improved liver function following BMM therapy is multifactorial. There is a less fibrotic cellular milieu, a proregenerative stimulus to LPCs, and elevated levels of cytokines such as CSF-1, VEGF and IGF-1 that are involved in reparative processes during tissue injury.
Immune dysfunction modulates hepatic regeneration in ACLF
In an important contribution, Wasmuth et al. [115] showed that in patients with ACLF or sepsis, there was a severe reduction in TNF-α production and HLA-DR expression compared to patients with compensated cirrhosis indicating a sepsis-like immune paralysis state or dysfunction in ACLF. There is indeed a state of immune disequilibrium with more systemic inflammatory response syndrome (SIRS) as shown by increased levels of proinflammatory cytokines (IL-6, TNF-α) and less compensatory antiinflammatory syndrome (CARS) with reduced HLA-DR expression on monocytes. Subsequently, Katoonizadeh et al. showed that ACLF patients are prone to infections, which lead to high short-term mortality. They showed that early markers of SIRS and ductular bilirubinostasis predicted poor outcome in ACLF [116]. In another elegant study by Mookerjee et al., they showed that although patients with alcoholic hepatitis as an acute insult to cirrhosis had peripheral neutrophilia, they were still susceptible to infections. This was because there was neutrophil dysfunction in the form of a neutrophil resting oxidative burst greater than or equal to 55 % and reduced phagocytic capacity of lower than 42 % due to persistent endotoxemia [117]. Jalan et al. [118] described the concept of PIRO (predisposition → injury → response → Organ failure). It is therefore of paramount importance to identify patients in the therapeutic golden window, probably defined as the stage between inflammatory response and prior to onset of organ failure. Therapeutic administration of G-CSF can enhance the immune function and restore the balance of SIRS and CARS (Fig. 5). As shown in the study by Garg et al. [99], patients with ACLF treated with G-CSF had reduced incidence of sepsis and consequently improved survival.
Future perspectives
ACLF is a distinct syndrome with rapid progression with high short-term mortality, however with a potential of reversibility. The concept of in vivo hepatic regeneration seems more practical and applicable. In properly selected patients, judicious use of growth factors with proper monitoring could become a potential new therapeutic option in patients with ongoing liver failure, such as ACLF. Of course, the therapy has to be used prior to onset of sepsis and organ failure so as to explore the potential of the liver and bone marrow for hepatic regeneration.
References
Sen S, William R, Jalan R. The pathophysiological basis of acute-on-chronic liver failure. Liver 2002;22(Suppl 2):5–13
Sarin SK, Kumar A, Almeida J, Chawla YC, Fan ST, Garg H, et al. Acute-on-chronic liver failure (ACLF): consensus recommendations of the Asian Pacific Association for the study of the liver (APASL). Hepatol Int 2009;3:269–282
Kjaergard LL, Liu J, Als-Nielsen B, Gluud C. Artificial and bioartificial support systems for acute and acute-on-chronic liver failure: a systematic review. JAMA 2003;289:217–222
Moreau R, Jalan R, Gines P, Pavesi M, Angeli P, Cordoba J, et al. Acute-on-chronic liver failure is a distinct syndrome that develops in patients with acute decompensation of cirrhosis. Gastroenterology 2013;144:1426–1437
Wlodzimirow KA, Eslami S, Abu-Hanna A, Nieuwoudt M, Chamuleau RA. A systematic review on prognostic indicators of acute on chronic liver failure and their predictive value for mortality. Liver Int 2013;33(1):40–52
Garg H, Kumar A, Garg V, Sharma P, Sharma BC, Sarin SK. Clinical profile and predictors of mortality in patients of acute-on-chronic liver failure. Dig Liver Dis 2012;44(2):166–171
Malhi H, Gores GJ. Cellular and molecular mechanisms of liver injury. Gastroenterology 2008;134:1641–1654
Ambrosino G, Naso A, Feltracco P, Carraro P, Basso SM, Varotto S, et al. Cytokines and liver failure: modification of TNF-a and IL–6 in patients with acute on chronic liver decompensation treated with molecular adsorbent recycling system (MARS). Acta Biomed 2003;74(Suppl 2):7–9
Roskams T. Relationships among stellate cell activation, progenitor cells and hepatic regeneration. Clin Liver Dis 2008;12:853–860
Bird TG, Lorenzini S, Forbes SJ. Activation of stem cells in hepatic diseases. Cell Tissue Res 2008;331(1):283–300
Fausto N, Campbell JS, Riehle KJ. Liver regeneration. Hepatology 2006;43:S45–S53
Falkowski O, An HJ, Ianus IA, Chiriboga L, Yee H, West AB, et al. Regeneration of hepatocyte “buds” in cirrhosis from intra-biliary stem cells. J Hepatol 2003;39:357–364
Wiemann SU, Satyanarayana A, Tsahuridu M, Tillmann HL, Zender L, Klempnauer J, et al. Hepatocyte telomere shortening and senescence are general markers of human liver cirrhosis. FASEB J 2002;16:935–942
Marshall A, Rushbrook S, Davies SE, Morris LS, Scott IS, Vowler SL, et al. Relation between hepatocyte G1 arrest, impaired hepatic regeneration, and fibrosis in chronic hepatitis C virus infection. Gastroenterology 2005;128:33–42
Libbrecht L, Desmet V, Van Damme B, Roskams T. Deep intralobular extension of human hepatic “progenitor cells” correlates with parenchymal inflammation in chronic viral hepatitis: can “progenitor cells” migrate? J Pathol 2000;192:373–378
Lowes KN, Brennan BA, Yeoh GC, Olynyk JK. Oval cell numbers in human chronic liver diseases are directly related to disease severity. Am J Pathol 1999;154:537–541
Roskams TA, Libbrecht L, Desmet VJ. Progenitor cells in diseased human liver. Semin Liver Dis 2003;23(4):385–396
Yang L, Jung Y, Omenetti A, Witek RP, Choi S, Vandongen HM, et al. Fate-mapping evidence that hepatic stellate cells are epithelial progenitors in adult mouse livers. Stem Cells 2008;26:2104–2143
Kuwahara R, Kofman AV, Landis CS, Swenson ES, Barendswaard E, et al. The hepatic stem cell niche: identification by label-retaining cell assay. Hepatology 2008;47(6):1810–1812
Sawitza I, Kordes C, Reister S. H¨aussinger D. The niche of stellate cells within rat liver. Hepatology 2009;50(5):1617–1624
Moore KA, Lemischka I. Stem cells and their niches. Science 2006;311:1880–1885
Zhang L, Theise N, Chua M, Reid LM. The stem cell niche of human livers: symmetry between development and regeneration. Hepatology 2008;48(5):1598–1607
Cardinale V, Wang Y, Carpino G, Cui GB, Gatto M, Rossi M, et al. Multipotent stem/progenitor cells in human biliary tree give rise to hepatocytes, cholangiocytes and pancreatic issues. Hepatology 2011;54(6):2159–2172
Carpino G, Cardinale V, Onori P, Franchitto A, Berloco PB, Rossi M, et al. Biliary tree stem/progenitor cells in glands of extrahepatic and intrahepatic bile ducts: an anatomical in situ study yielding evidence of maturational lineages. J Anat 2012;220(2):186–199
Spee B, Carpino G, Schotanus BA, Katoonizadeh A, Vander Borght S, Gaudio E, et al. Characterisation of the liver progenitor cell niche in liver diseases: potential involvement of Wnt and Notch signaling. Gut 2010;59:247–257
Rastogi A, Bihari C, Maiwall R, Ahuja A, Sharma MK, Kumar A, et al. Hepatic stellate cells are involved in the pathogenesis of acute-on-chronic liver failure (ACLF). Virchows Arch 2012;461(4):393–398
Knight B, Yeoh GC. TNF/LT alpha double knockout mice display abnormal inflammatory and regenerative responses to acute and chronic liver injury. Cell Tissue Res 2005;319:61–70
Jakubowski A, Ambrose C, Parr M, Lincecum JM, Wang MZ, Zheng TS, et al. TWEAK induces liver progenitor cell proliferation. J Clin Investig 2005;115:2330–2340
Weng HL, Feng DC, Radaeva S, Kong XN, Wang L, Liu Y, et al. IFN- gamma inhibits hepatic progenitor cell proliferation in HBV infected patients and in 3,5-diethoxycarbonyl-1,4- dihydrocollidine diet fed mice. J Hepatol 2013;59(4):738–745
Sun R, Gao B. Negative regulation of liver regeneration by innate immunity (natural killer cells/interferon-gamma). Gastroenterology 2004;127(5):1525–1539
Akhurst B, Matthews V, Husk K, Smyth MJ, Abraham LJ, Yeoh GC. Differential lymphotoxin-beta and interferon gamma signaling during mouse liver regeneration induced by chronic and acute injury. Hepatology 2005;41:327–335
Sanchez A, Factor VM, Schroeder IS, Nagy P, Thorgeirsson SS. Activation of NF-kappa B and STAT3 in rat oval cells during 2-acetylaminofluorene/partial hepatectomy-induced liver regeneration. Hepatology 2004;39:376–385
Subrata LS, Lowes KN, Olynyk JK, Yeoh GC, Quail EA, Abraham LJ. Hepatic expression of the tumor necrosis factor family member lymphotoxin-beta is regulated by interleukin (IL)-6 and IL-1beta: transcriptional control mechanisms in oval cells and hepatoma cell lines. Liver Int 2005;25:633–646
Omori N, Evarts RP, Omori M, Hu Z, Marsden ER, Thorgeirsson SS. Expression of leukemia inhibitory factor and its receptor during liver regeneration in the adult rat. Lab Investig 1996;75(1):15–24
Znoyko I, Sohara N, Spicer SS, Trojanowska M, Reuben A. Expression of oncostatin M and its receptors in normal and cirrhotic human liver. J Hepatol 2005;43(5):893–900
Kamiya A, Kinoshita T, Ito Y, Matsui T, Morikawa Y, Senba E, et al. Fetal liver development requires a paracrine action of oncostatin M through the gp130 signal transducer. EMBO J 1999;18(8):2127–2136
Heng BC, Yu H, Yin Y, Lim SG, Cao T. Factors influencing stem cell differentiation into the hepatic lineage in vitro. J Gastroenterol Hepatol 2005;20(7):975–987
Hamou C, Callaghan MJ, Thangarajah H, Chang E, Chang EI, et al. Mesenchymal stem cells can participate in ischemic neovascularization. Plast Reconstr Surg 2009;123(2 Suppl):45S–55S
Kucia MJ, Wysoczynski M, Wu W, Zuba-Surma EK, Ratajczak J, Ratajczak MZ. Evidence that very small embryonic-like stem cells are mobilized into peripheral blood. Stem Cells 2008;26(8):2083–2092
Tepper OM, Capla JM, Galiano RD, Ceradini DJ, Callaghan MJ, et al. Adult vasculogenesis occurs through in situ recruitment, proliferation, and tubulization of circulating bone marrow-derived cells. Blood 2005;105(3):1068–1077
Chen Y, Xiang LX, Shao JZ, Pan RL, Wang YX, Dong XJ, et al. Recruitment of endogenous bone marrow mesenchymal stem cells towards injured liver. J Cell Mol Med 2010;14(6B):1494–1508
Si Y, Tsou CL, Croft K, Charo IF. CCR2 mediates hematopoietic stem and progenitor cell trafficking to sites of inflammation in mice. J Clin Investig 2010;120(4):1192–1203
Massa M, Rosti V, Ferrario M, Campanelli R, Ramajoli I, Rosso R, et al. Increased circulating hematopoietic and endothelial progenitor cells in the early phase of acute myocardial infarction. Blood 2005;105(1):199–206
Paczkowska E, Kucia M, Koziarska D, Halasa M, Safranow K, Masuik M, et al. Clinical evidence that very small embryonic-like stem cells are mobilized into peripheral blood in patients after stroke. Stroke 2009;40(4):1237–1244
Gehling UM, Willems M, Schlagner K, Benndorf RA, Dandri M, Petersen J, et al. Mobilization of hematopoietic progenitor cells in patients with liver cirrhosis. World J Gastroenterol 2010;16(2):217–224
Drukala J, Paczkowska E, Kucia M, Mlynska E, Krajewski A, Machalinski M, et al. Stem cells, including a population of very small embryonic-like stem cells, mobilized into peripheral blood in patients after skin burn injury. Stem Cell Rev 2012;8(1):184–194
Petersen BE, Bowen WC, Patrene KD, Mars WM, Sullivan AK, Murase N, et al. Bone marrow as a potential source of hepatic oval cells. Science 1999;284:1168–1170
Lagasse E, Connors H, Al-Dhalimy M, Reitsma M, Dohse M, Osborne L, et al. Purified hematopoietic stem cells can differentiate into hepatocytes in vivo. Nat Med 2000;6:1229–1234
Theise ND, Nimmakayalu M, Gardner R, Illei PB, Morgan G, Teperman L, et al. Liver from bone marrow in humans. Hepatology 2000;32:11–16
Wang X, Willenbring H, Akkari Y, Torimaru Y, Foster M, AlDhalimy M, et al. Cell fusion is the principal source of bone marrow-derived hepatocytes. Nature 2003;422:897–901
Medvinsky A, Smith A. Stem cells: fusion brings down barriers. Nature 2003;422:823–825
Wagers AJ, Sherwood RI, Christensen JL, Weissman IL. Little evidence for developmental plasticity of adult hematopoietic stem cells. Science 2002;297:2256–2259
Theise ND, Krause DS, Sharkis S. Comment on “little evidence for developmental plasticity of adult hematopoietic stem cells”. Science 2003;299:1317
Yoon CH, Hur J, Park KW, Kim JH, Lee CS, Oh IY, et al. Synergistic neovascularization by mixed transplantation of early endothelial progenitor cells and late outgrowth endothelial cells: the role of angiogenic cytokines and matrix metalloproteinases. Circulation 2005;112(11):1618–1627
Challen GA, Boles N, Lin KK, Goodell MA. Mouse hematopoietic stem cell identification and analysis. Cytometry A 2009;75(1):14–24
Timmermans F, Van Hauwermeiren F, De Smedt M, Raedt R, Plasschaert F, De Buyzere M, et al. Endothelial outgrowth cells are not derived from CD133+ cells or CD45+ hematopoietic precursors. Arterioscler Thromb Vasc Biol 2007;27(7):1572–1579
Yoder MC, Mead LE, Prater D, Krier TR, Mroueh KN, Li F, et al. Redefining endothelial progenitor cells via clonal analysis and hematopoietic stem/progenitor cell principals. Blood 2007;109(5):1801–1809
Timmermans F, Plum J, Yoder MC, Ingram DA, Vandekerckhove B, Case J. Endothelial progenitor cells: identity defined? J Cell Mol Med 2009;13(1):87–102
Bailey AS, Willenbring H, Jiang S, Anderson DA, Schroeder DA, Wong MH, et al. Myeloid lineage progenitors give rise to vascular endothelium. Proc Natl Acad Sci USA 2006;103(35):13156–13161
Masuda H, Alev C, Akimaru H, Ito R, Shizuno T, Kobori M, et al. Methodological development of a clonogenic assay to determine endothelial progenitor cell potential. Circ Res 2011;109(1):20–37
Sandri M, Beck EB, Adams V, Geilen S, Lenk L, Hollriegel R, et al. Maximal exercise, limb ischemia, and endothelial progenitor cells. Eur J Cardiovasc Prev Rehabil 2011;18(1):55–64
Pittenger MF, Mackay AM, Beck SC, Jaiswal RK, Douglas R, Mosca JD, et al. Multilineage potential of adult human mesenchymal stem cells. Science 1999;284(5411):143–147
Sachetti B, Funari A, Michienzi S, Di Cesare S, Piersanti S, Saggio I, et al. Self-renewing osteoprogenitors in bone marrow sinusoids can organize a hematopoietic microenvironment. Cell 2007;131:324–336
Sasaki M, Abe R, Fujita Y, Ando S, Inokuma D, Shimizu H. Mesenchymal stem cells are recruited into wounded skin and contribute to wound repair by transdifferentiation into multiple skin cell type. J Immunol 2008;180(4):2581–2587
Bae KS, Park JB, Kim HS, Kim DS, Park DJ, Kang SJ. Neuron-like differentiation of bone marrow-derived mesenchymal stem cells. Yonsei Med J 2011;52(3):401–412
Nguyen BK, Maltais S, Perrault LP, Tanguay JF, Tardif JC, Stevens LM, et al. Improved function and myocardial repair of infarcted heart by intracoronary injection of mesenchymal stem cell-derived growth factors. J Cardiovasc Transl Res 2010;3(5):547–558
Katsha AM, Ohkouchi S, Xin H, Kanehira M, Sun R, Nukiwa T, et al. Paracrine factors of multipotent stromal cells ameliorate lung injury in an elastase-induced emphysema model. Mol Ther 2011;19(1):196–203
Xu X, Xu Z, Xu Y, Cui G. Selective down-regulation of extracellular matrix gene expression by bone marrow derived stem cell transplantation into infarcted myocardium. Circ J 2005;69(10):1275–1283
Xu X, Xu Z, Xu Y, Cui G. Effects of mesenchymal stem cell transplantation on extracellular matrix after myocardial infarction in rats. Coron Artery Dis 2005;16(4):245–255
Ortiz LA, Dutreil M, Fattman C, Pandey AC, Torres G, Go K, et al. Interleukin 1 receptor antagonist mediates the anti-inflammatory and antifibrotic effect of mesenchymal stem cells during lung injury. Proc Natl Acad Sci USA 2007;104(26):11002–11007
Dayan V, Yannarelli G, Billia F, Filomeno P, Wang XH, Davies JE, et al. Mesenchymal stromal cells mediate a switch to alternatively activated monocytes/macrophages after acute myocardial infarction. Basic Res Cardiol 2011;106(6):1299–1310
Peng L, Xie DY, Lin BL, Liu J, Zhu HP, Xie C, et al. Autologous bone marrow mesenchymal stem cell transplantation in liver failure caused by hepatitis B: short term and long term outcomes. Hepatology 2011;54(3):820–828
Shi M, Zhang Z, Xu R, Lin H, Fu J, Zou Z, et al. Human mesenchymal stem cell transfusion is safe and improves liver function in acute-on-chronic liver failure patients. Stem Cells Transl Med 2012;1(10):725–731
Hatzistergos KE, Quevedo H, Oskouei BN, Hu Q, Feigembaum GS, Margititch IS, et al. Bone marrow mesenchymal stem cells stimulate cardiac stem cell proliferation and differentiation. Circ Res 2010;107(7):913–922
Discher DE, Mooney DJ, Zandstra PW. Growth factors, matrices, and forces combine and control stem cells. Science 2009;324(5935):1673–1677
Youn SW, Lee SW, Lee J, Jeong HK, Suh JW, Yoon CH, et al. COMP-Ang1 stimulates HIF-1α-mediated SDF-1 overexpression and recovers ischemic injury through BM-derived progenitor cell recruitment. Blood 2011;117(16):4376–4386
Brandao D, Costa C, Canedo A, Vaz G, Pignatelli D. Endogenous vascular endothelial growth factor and angiopoietin-2 expression in critical limb ischemia. Int Angiol 2011;30(1):25–34
Massberg S, Konrad I, Schurzinger K, Lorenz M, Schneider S, Zohlnhoefer D, et al. Platelets secrete stromal cell-derived factor 1α and recruit bone marrow-derived progenitor cells to arterial thrombi in vivo. J Exp Med 2006;203(5):1221–1233
Hattori K, Dias S, Heissig B, Hackett NR, Lyden D, Tateno M, et al. Vascular endothelial growth factor and angiopoietin-1 stimulate postnatal hematopoiesis by recruitment of vasculogenic and hematopoietic stem cells. J Exp Med 2001;193(9):1005–1014
Pitchford SC, Furze RC, Jones CP, Wengner AM, Rankin SM. Differential mobilization of subsets of progenitor cells from the bone marrow. Cell Stem Cell 2009;4(1):62–72
Hopkins SP, Bulgrin JP, Sims RL, Bowman B, Donovan DL, Schmidt SP. Controlled delivery of vascular endothelial growth factor promotes neovascularization and maintains limb function in a rabbit model of ischemia. J Vasc Surg 1998;27(5):886–894
Pitchford SC, Furze RC, Jones CP, Wengner AM, Rankin SM. Differential mobilization of subsets of progenitor cells from the bone marrow. Cell Stem Cell 2009;4(1):62–72
Broxmeyer HE, Hangoc G, Cooper S, Campbell T, Ito S, Mantel C. AMD3100 and CD26 modulate mobilization, engraftment, and survival of hematopoietic stem and progenitor cells mediated by the SDF-1/CXCL12-CXCR4 axis. Ann N Y Acad Sci 2007;1106:1–19
Levesque JP, Hendy J, Takamatsu Y, Simmons PJ, Bendall LJ. Disruption of the CXCR4/CXCL12 chemotactic interaction during hematopoietic stem cell mobilization induced by GCSF or cyclophosphamide. J Clin Investig 2003;111(2):187–196
Liu F, Pan X, Chen G, Jiang D, Cong X, Fei R, et al. Hematopoietic stem cells mobilized by granulocyte colony-stimulating factor partly contribute to liver graft regeneration after partial orthotopic liver transplantation. Liver Transplant 2006;12(7):1129–1137
Takamiya M, Okigaki M, Jin D, Takai S, Nozawa Y, Adachi Y, et al. Granulocyte colony-stimulating factor-mobilized circulating c-Kit+/Flk-1+ progenitor cells regenerate endothelium and inhibit neointimal hyperplasia after vascular injury. Arterioscler Thromb Vasc Biol 2006;26(4):751–757
Li X, Xu B. HMG-CoA reductase inhibitor regulates endothelial progenitor function through the phosphatidylinositol 3′-kinase/AKT signal transduction pathway. Appl Biochem Biotechnol 2009;157(3):545–553
Urao N, Okigaki M, Yamada H, Aadachi Y, Matsuno K, Matsui A, et al. Erythropoietin-mobilized endothelial progenitors enhance reendothelialization via Akt-endothelial nitric oxide synthase activation and prevent neointimal hyperplasia. Circ Res 2006;98(11):1405–1413
Gensch C, Clever YP, Werner C, Hanhoun M, Bohm M, Laufs U. The PPAR-γ agonist pioglitazone increases neoangiogenesis and prevents apoptosis of endothelial progenitor cells. Atherosclerosis 2007;192(1):67–74
Oh SH, Miyazaki M, Kouchi H, Inoue Y, Sakaguchi M, Tsuji T, et al. Hepatocyte growth factor induces differentiation of adult rat bone marrow cells into a hepatocyte lineage in vitro. Biochem Biophys Res Commun 2000;279(2):500–504
Cui YL, Meng MB, Tang H, Zheng MH, Wang YB, Han HX, et al. Recombinant human hepatocyte growth factor for liver failure. Contemp Clin Trials 2008;29(5):696–704
Gandhi CR. Augmenter of liver regeneration. Fibrogenes Tissue Repair 2012;5:10
De Silvestro G, Vicarioto M, Donadel C, Menegazzo M, Marson P, Corsini A. Mobilization of peripheral blood hematopoietic stem cells following liver resection surgery. Hepatogastroenterology 2004;51(57):805–810
Lorenzini S, Isidori A, Catani L, Gramenzi A, Talarico S, Bonifazi F, et al. Stem cell mobilization and collection in patients with liver cirrhosis. Aliment Pharmacol Ther 2008;27(10):932–939
Vassilopoulos G, Wang PR, Russell DW. Transplanted bone marrow regenerates liver by cell fusion. Nature 2003;422:901–904
Gianni AM, Siena S, Bregni M, Tarella C, Stern AC, Pileri A, et al. Granulocyte-macrophage colony-stimulating factor to harvest circulating haemopoietic stem cells for autotransplantation. Lancet 1989;2:580–585
Gaia S, Smedile A, Omede P, Olivero A, Sanavio F, Balzola F. Feasibility and safety of G-CSF administration to induce bone marrow derived cells mobilization in patients with end stage liver disease. J Hepatol 2006;45:13–19
Spahr L, Lambert JF, Brandt LR, Chalandon Y, Frossard JL, Giostra E, et al. Granulocyte-colony stimulating factor induces proliferation of hepatic progenitors in alcoholic steatohepatitis: a randomized trial. Hepatology 2008;48(1):221–229
Garg V, Garg H, Khan A, Trehanpati N, Kumar A, Sharma BC, et al. Granulocyte-colony stimulating factor (G- CSF) therapy mobilizes CD34 cells and improves survival in patients with acute on chronic liver failure. Gastroenterology 2012;142(3):505–512
Duan XZ, Liu FF, Tong JJ, Yang HZ, Chen J, Liu XY, et al. Granulocyte colony stimulating factor therapy improves survival in patients with hepatitis B virus-associated acute-on-chronic liver failure. World J Gastroenterol 2013;19:1104–1110
Murat O. Arcasoy. Non erythroid effects of erythropoietin. Haematologica 2010;95(11):1803–1804
Schmeding M, Boas-KnoopS LippertS, Ruehl S, Somasundaram R, Dagdelen T, et al. Erythropoietin promotes hepatic regeneration after extended liver resection in rats. J Gastroenterol Hepatol 2008;23(7):1125–1131
Greif F, Ben Ari Z, Taya R, Pappo O, Kurtzwald E, Cheparko Y. Dual effect of EPO on liver protection and regeneration after subtotal hepatectomy in rats. Liver Transplant 2010;16(5):631–638
Ben Ari Z, Zilbermints V, Pappo O, Avlas O, Sharon E, Grief F, et al. Erythropoetin increases survival and attenuates fulminant hepatic failure induced by D- galactosamine/lipopolysaccharide in mice. Transplantation 2011;92(1):18–24
Bonifaz L, Bonnyay D, Mahnke K, Rivera M, Nussenzweig MC, Steinman RM. Efficient targeting of protein antigen to the dendritic cell receptor DEC-205 in the steady state leads to antigen presentation on major histocompatibility complex class I products and peripheral CD8 + T cell tolerance. J Exp Med 2002;196:1627–1638
Zhang Z, Zou ZS, Fu JL, Cai L, Jin L, Liu YJ, et al. Severe dendritic cell perturbation is actively involved in the pathogenesis of acute-on-chronic hepatitis B liver failure. J Hepatol 2008;49:396–406
Zhao J, Zhang JY, Yu HW, He YL, Zhao JJ, Li J, et al. Improved survival ratios correlate with myeloid dendritic cell restoration in acute-on-chronic liver failure patients receiving methyl prednisolone therapy. Cell Mol Immunol 2012;9(5):417–422
Sumpter TL, Abe M, Tokita D, Thomson AW. Dendritic cells, the liver and transplantation. Hepatology 2007;46:2021–2031
Castellaneta A, Di Leo A, Amoruso A, Francavilla R, Margiotta M, Barone M, et al. Functional modification of CD11c liver dendritic cells during liver regeneration after hepatectomy in mice. Hepatology 2006;43(4):807–816
Khanam A, Trehanpati N, Garg V, Kumar C, Garg H, Sarin SK. Altered Frequencies of Dendritic cells and IFN-γ secreting T cells with Granulocyte colony stimulating factor (G-CSF) therapy in acute-on-chronic liver failure. Liver Int. 2014. doi: 10.1111/liv.12415
Liu T, Wang Y, Wen C, Zhang S, Zhang C. Stem cells or macrophages: which contribute to bone marrow cell therapy for liver cirrhosis? Hepatology 2011;54(3):1103
Thomas AJ, Pope C, Wojtacha D, Robson A, Gordon Walker TT, Hartland S, et al. Macrophage therapy for murine liver fibrosis recruits host effector cells improving fibrosis, regeneration, and function. Hepatology 2011;53:2003–2015
Viebahn CS, Benseler V, Holz LE, Elsegood CL, Vo M, Bertolino P, et al. Invading macrophages play a major role in the liver progenitor cell response to chronic liver injury. J Hepatol 2010;53(3):500–507
Wang J, Zhou X, Cui L, Yan L, Liang J, Cheng X, et al. The significance of CD14+ monocytes in peripheral blood stem cells for the treatment of rat liver cirrhosis. Cytotherapy 2010;12(8):1022–1034
Wasmuth HE, Kunz D, Yagmur E, Timmer-Strangho¨ner A, Vidacek D, Siewert E, et al. Patients with acute on chronic liver failure display ‘sepsis like’ immune paralysis. J Hepatol 2005;42:195–201
Katoonizadeh A, Laleman W, Versylpe C, Wilmer A, Maleux G, Roskams T, et al. Early features of acute-on-chronic alcoholic liver failure: a prospective cohort study. Gut 2010;59:1561–1569
Mookerjee RP, Stadlbauer V, Lidder S, Wright GA, Hodges SJ, Davies NA, et al. Neutrophil dysfunction in alcoholic hepatitis superimposed on cirrhosis is reversible and predicts the outcome. Hepatology 2007;46(3):831–840
Jalan R, Gines P, Olson JC, Mookerjee RP, Moreau R, Garcia-Tsao G, et al. Acute-on-chronic liver failure review. J Hepatol 2012;57(6):1336–1348
Compliance with ethical requirements and Conflict of interest
None.
Disclosures
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kedarisetty, C.K., Anand, L., Khanam, A. et al. Growth factors enhance liver regeneration in acute-on-chronic liver failure. Hepatol Int 8 (Suppl 2), 514–525 (2014). https://doi.org/10.1007/s12072-014-9538-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-014-9538-4