Abstract
Genetic factors play a major role in the etiopathogenesis of attention-deficit/hyperactivity disorder (ADHD). In this study, we aimed to investigate the relationship between the CDH13 (rs6565113, rs11150556) and LPHN3 (rs6551665, rs6858066, rs1947274, rs2345039) gene polymorphisms and ADHD. We also sought to examine possible relationships between these polymorphisms and the clinical course and treatment response in ADHD. A total of 120 patients (79% boys), aged 6 to 18 years, newly diagnosed (medication-naïve) with ADHD according to the DSM-5 and a group of 126 controls (74% girls) were enrolled in the study. We examined the association between the aforementioned polymorphisms and ADHD. Univariate and multivariate logistic regression analysis were used to evaluate factors influencing the treatment response of ADHD. A significant difference was found between ADHD and control groups in terms of genotype distribution of the LPHN3 rs6551665 and rs1947274 polymorphisms. The results also showed that having the GG genotype of rs6551665 and CC genotype of rs1947274 of the LPHN3 gene was associated with risk for ADHD, and this relationship was more prominent in male participants. In the multivariate logistic regression model established with variables shown to have a significant relationship with treatment response, the presence of the GG genotype of the LPHN3 rs6551665 polymorphism and high severity of ADHD assessed by CGI-S were associated with poor response to treatment. This study is the first study to investigate the relationship between ADHD and these polymorphisms among Turkish adolescents. Our results imply that the LPHN3 rs6551665 and rs1947274 polymorphisms have a significant effect on ADHD in a Turkish population, and support previous observations that the presence of the GG genotype of the LPHN3 rs6551665 polymorphism may be associated with poor response to treatment in ADHD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is a neurodevelopmental disorder that usually begins in childhood. It is characterized by inattention and/or hyperactivity and impulsivity symptoms that are not appropriate for the age of the person (American Psychiatric Association 2013). In recent epidemiological studies, the prevalence of ADHD was reported to range from 5.9% to 7.1% worldwide (Willcutt 2012), whereas in Turkey this rate was 12.7% (Ercan et al. 2015). In the etiology of ADHD, the interaction of genetic and environmental factors plays an important role in the early neurodevelopmental process (Güney et al. 2014). Faraone et al. (2005) reported a high level of heritability estimated for ADHD (76%). In studies conducted on patients diagnosed with ADHD by genome-wide association studies (GWAS) used to identify many risky genes with small impact domain causing multifactorial etiology, the highest association with ADHD was found with the cadherin 13 (CDH13) gene (Lasky-Su et al. 2008; Manolio et al. 2007; Neale et al. 2010). Cadherin-13 is a member of the family of calcium-dependent cell–cell adhesion proteins and regulates neural cell growth (Patel et al. 2003). The broad distribution of cadherin-13 in the midbrain and telencephalon suggests that it may play an important role in the establishment and maintenance of neural circuits (Takeuchi et al. 2000). The functions of cadherin-13 may be associated with axonal growth, dendritic branching, synaptic development, and the maintenance of synaptic contacts (Rivero et al. 2013). In a recent GWAS, rs6565113, an intronic single-nucleotide polymorphism (SNP) in CDH13, was found to be associated with a number of symptoms in ADHD (Franke et al. 2009; Lasky-Su et al. 2008). Using a different methodology, Salatino-Oliveira et al. (2015) demonstrated that the CDH13 rs11150556 CC genotype was also related to hyperactivity and impulsivity symptoms in adolescents with ADHD.
Latrophilin 3 (LPHN3) is a brain-specific member of the LPHN subfamily of G protein-coupled receptors (GPCRs) and has been shown to be important in regulating neurotransmitter exocytosis and synaptic development (O’Sullivan et al. 2012). LPHN also mediates Gαq/11-dependent signal transduction (Langenhan 2020). UNC-13, a major presynaptic diacylglycerol receptor required for vesicle-mediated release of neurotransmitters, plays a role in LPHN-dependent regulation of exocytosis (Brose et al. 2000; Willson et al. 2004). Arcos-Burgos et al. (2004) conducted a linkage analysis in a Paisa population in Colombia and found a relationship between 4q13.2 (near LPHN3) and ADHD. The relationship between the SNPs of LPHN3 and ADHD was confirmed by detailed mapping approaches with large samples of patients with ADHD (n = 2627) and healthy controls (n = 2531) among Paisa populations and in five different populations worldwide (Arcos-Burgos et al. 2010). Jain et al. (2012) reported that some SNPs (especially rs6551665) in the LPHN3 gene interact with SNPs from the 11q region containing the DRD2 and NCAM1 genes and increase the risk of developing ADHD. In a case–control study, Hwang et al. (2015) showed that the LPHN3 rs6551665 GG genotype and the G allele may have a significant relationship with ADHD. In another case–control study in adults with ADHD and healthy individuals in Spain, SNPs of LPHN3 rs2122643, rs1868790, rs6858066, rs4860106, and rs13115125 were significantly associated with ADHD, and rs6858066 with the combined type ADHD (Ribasés et al. 2011). Another study demonstrated that LPHN3 rs6551665, rs1947274, rs6858066, and rs2345039 polymorphisms were highly related to pregnancy exposed to stress in a family-based association study (Choudhry et al. 2012). A case–control study investigating the association between the LPHN3 rs2345039 polymorphism and ADHD suggests that this polymorphism forms the basis for the development of an ADHD phenotype characterized by the persistence of ADHD symptoms in adulthood (Acosta et al. 2016).
Studies investigating response to treatment in ADHD have focused on changes in genes encoding drug-targeted molecules such as carriers and receptors. Although most of the pharmacogenetic studies based on drugs used in the treatment of ADHD have shown satisfactory results, the genetic basis of the differences in the clinical response and optimal dose of the drugs has not been elucidated in studies so far (Kieling et al. 2010). Recent studies showed that treatment response in ADHD is often associated with the alpha-2 adrenergic receptor gene (ADRA2A), catechol-O-methyltransferase gene (COMT), noradrenaline transporter gene (SLC6A2), dopamine D4 receptor gene (DRD4), dopamine transporter gene (SLC6A3), and LPHN3 (Myer et al. 2018). Arcos-Burgos et al. (2010) reported that LPHN3 rs6551665 was associated with the response efficacy of methylphenidate (MPH) in the treatment of ADHD. In that study, the G allele carriers exhibited better response to medication in the inattentive symptom domain. The LPHN3 rs6858066 polymorphism was also associated with a better response to MPH treatment among adults with ADHD (Ribasés et al. 2011). Similar results have been reported in prospective studies in children or adolescents with ADHD, where a statistically significant association was found between the LPHN3 rs1868790 polymorphism and the long-term MPH response (Gomez-Sanchez et al. 2017).
Although there are reports in the current literature regarding the relationship between the CDH13 and LPHN3 genes and ADHD and/or response to treatment of ADHD based on GWAS, to the best of our knowledge, there is no evidence regarding the relationship between these two genes among ADHD patients in Turkey. Thus, this study aimed to investigate the association between the CDH13 rs6565113 and rs11150556 and LPHN3 rs6551665, rs6858066, rs1947274, and rs2345039 polymorphisms and ADHD among Turkish children and adolescents diagnosed with ADHD in comparison with a normal control group. The study also aimed to reveal the possible relationship between these polymorphisms and the clinical course and treatment responses in ADHD.
Method
Participants
The study sample consisted of 120 (79% male) patients newly diagnosed with ADHD at the Gazi University Faculty of Medicine Child and Adolescent Psychiatry Clinics and 126 (74% male) healthy controls who applied to the Pediatric or Child and Adolescent Psychiatry Clinics. The case group consisted of children between the ages of 6 and 18 years who applied to the Gazi University Faculty of Medicine Child and Adolescent Psychiatry Clinics with ADHD symptoms (e.g., inattention, hyperactivity, impatience, impulsivity). The participants included volunteers who were diagnosed with ADHD after a clinical interview, based on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria, with both children and their family. All patients were screened for psychiatric disorders using the Schedule for Affective Disorders and Schizophrenia for School-Age Children–Present and Lifetime Version (K-SADS-PL) for the exclusion of another psychopathology and confirmed by another child and adolescent mental health specialist. Children and adolescents with a history of psychotropic drug use and neurological, metabolic, genetic, or any physical disorder (e.g., cerebral palsy, tuberous sclerosis, epilepsy, diabetes mellitus) or who were diagnosed with an additional psychiatric disorder other than ADHD according to the K-SADS-PL assessment and DSM-5 diagnostic criteria were excluded from the study. Clinical diagnoses of the patients were based on semi-structured interviews of patients and their families.
The participants in the control group included those who applied to the Gazi University Faculty of Medicine Child and Adolescent Psychiatry Clinics with various problems including adolescent, family relations, and school adaptation problems. Those who also reported other problems requiring counseling applied to the Gazi University Faculty of Medicine Pediatrics Clinics for various reasons but did not have any neurological or metabolic disease after clinical evaluation. The control group was also evaluated for the same exclusion criteria (i.e. without any psychopathology, including ADHD) by the child and adolescent psychiatrists. The control group participants consisted of children or adolescents aged 6–18 years who were socioeconomically similar to the ADHD group and met the inclusion criteria. After the aim of the study and the protocol were explained verbally, written informed consent and genetic consent forms were obtained from all participants and parents who agreed to participate in the study.
Data Tools
Sociodemographic Data Form
Demographic information was obtained from children and parents in both groups. The participants’ age, educational level (class), weight, predominance of ADHD, the medication and dose used by the participant for ADHD, and side effects found in control visits were recorded for each participant.
Schedule for Affective Disorders and Schizophrenia for School-Age Children—Present and Lifetime Version, Turkish Adaptation (K-SADS-PL-T)
The K-SADS-PL-T, which was developed by Kaufman et al. (1997), is a semi-structured interview tool used to determine past and current psychiatric psychopathologic disorders in children and adolescents (6–18 years of age). Its validity and reliability in Turkish were studied by Gökler et al. (2004).
Conners’ Teacher Rating Scale (CTRS)
The CTRS includes 28 items, and each item is rated on a four-point Likert scale ranging from 0 (never) to 3 (always). The scale is used to measure the subtypes and severity of ADHD. Each item on the scale is assessed and administered by teachers, whose assessments are based on observations of the behavioral aspects of students in the classroom. The scale was adapted and translated into Turkish by Dereboy et al. (2007), who found good internal consistency (α = 0.95).
Clinical Global Impression Scale (CGI)
The CGI evaluates the overall functionality of the patient for clinical research purposes in all psychiatric disorders at any age. There is a “severity” (CGI-S) section where the severity of psychopathology is rated from 1 to 7, and an “improvement” (CGI-I) section where the change since the beginning of treatment, which is a seven-point measure, is graded. The CGI-S rating is based mainly on the effect of symptoms on patient functionality, which is evaluated in the context of the clinician’s clinical experience. In the CGI-I subscale, the clinician is asked to rate the change in the patient’s condition in comparison to the condition at admission, with ratings that range from 1 = “very much improved” to 7 = “very much worse” (Busner and Targum 2007).
Procedure
In this study, a 5 ml sample of venous blood was obtained from all participants. Sociodemographic data were filled in with the information obtained from the participant and the parents themselves. Participants in the case group were administered the CTRS to assess clinical features such as ADHD presentation, and the CGI-S severity subscale of the CGI was scored for each participant. In the case group, the severity of ADHD was evaluated separately according to the CGI-S and CTRS baseline scores.
In the case group, ADHD treatment was arranged randomly according to the clinical opinion of the child psychiatrist. Dose titration was used to determine the most appropriate dose of MPH for maintenance treatment in patients who were planned to start MPH in the case group. During the dose titration period, MPH was administered with an increasing dose regimen until no further clinical improvement was detected or limited side effects occurred. Dose adjustment was continued weekly, and after the maintenance dose was determined, MPH was continued at this dose for 4 weeks.
To find the optimal dose of atomoxetine (ATX) for maintenance treatment in the case group, the dose of ATX was titrated to 0.5 mg/kg per day in the first week, 0.8 mg/kg per day in the second week, and 1.2 mg/kg per day in the third and fourth weeks. Those with side effects at any titration stage were kept at the same dose for 1–2 weeks. The dose was then continued for at least 4 weeks.
In the case group, treatment response was assessed at the control visits at the first, second, fourth, and eighth weeks, and at the 12th week visit at the end of the study. Drug compliance was assessed at each visit by direct questioning of the parent and children. If no improvement was observed within 1 month after the appropriate dose adjustment, drug treatment was discontinued. During the 12-week follow-up period, seven patients were unable to follow up for various reasons. At the end of this process, 82 patients received MPH and 31 patients received ATX. The mean adjusted daily doses of MPH and ATX were 0.944 ± 1.24 (0.41–11) and 1190 ± 0.074 (0.99–1.33) mg/kg/day, respectively. In similar studies, a CGI-I score of 2 or less (“much improved” or “very much improved”) and/or a 25% decrease in CTRS score compared to baseline were accepted as reference (Hazell et al. 2011; Kemner et al. 2005). In this study, we first defined a good response group as those for whom the CTRS scores at 12 weeks of the trial were more than 25% lower than the baseline scores. A secondary efficacy measure was defined as a CGI-I score at 12 weeks of 1 or 2. Finally, treatment efficacy was evaluated separately by taking into consideration either the CGI-I 12th-week score or the change in CTRS between the initial and 12th-week scores.
Genetic Analysis
DNA Isolation
Venous blood samples (approximately 5 ml) were obtained from 120 patients and 126 controls and stored in EDTA tubes at 4 °C until DNA isolation was performed. DNA isolation from the blood samples was performed according to the DNA isolation kit manufacturer’s instructions (Macherey-Nagel, Germany). Obtained genomic DNA was stored at −20 °C.
Real-Time PCR Primers and Probe Design
We designed real-time primers for the rs6565113 and rs11150556 polymorphisms in the CDH13 gene and rs6551665, rs6858066, rs1947274, and rs2345039 polymorphisms in the LPHN3 gene. Wild-type, mutant, and heterozygous genotypes were distinguished by melting curve analysis. The probes designed specifically for these polymorphisms are shown in Table 1. Genetic analyzes have been conducted in Gazi University Medical Faculty Medical Genetics Department. This research fee was supported by Gazi University Scientific Research Projects (project code no: 01/2018-17).
Statistical Analysis
Statistical analysis was performed using SPSS version 22.0 software (IBM Corp., Armonk, NY, USA). For descriptive analyses, categorical variables were reported as numbers and percentages, and continuous variables as mean ± standard deviation (SD) and median (min-max value). The chi-square test was used for comparison of categorical variables between the groups and to assess Hardy–Weinberg equilibrium (HWE). The conformity of continuous variables to normal distribution was evaluated using visual (histogram and probability graphs) and analytical methods (Kolmogorov–Smirnov/Shapiro–Wilk tests). The Mann–Whitney U test and Kruskal–Wallis test, which are based on non-normal distribution of the data, were used for comparison of data sets. Student’s t test was used for comparison of data sets which were normally distributed for the variables. Binary logistic regression was used to investigate the association between risky genotypes and ADHD and control groups. Patients’ response to the treatment was assessed using univariate and multivariate logistic regression. Variables with p < 0.05 in univariate analysis were included in the multivariate logistic regression model. The significance value was set to p < 0.05.
Results
Demographic and Clinical Characteristics of the Sample
Table 2 presents the mean, median, and standard deviation for age and frequency statistics for gender in the ADHD and control groups. There was no statistically significant difference between the ADHD and control groups in age or gender distribution (p > 0.05). Table 3 shows the clinical features of the ADHD group.
Relationship Between ADHD and SNPs of CDH13 Gene
No statistically significant difference was found between the ADHD and control groups in terms of genotype and allele frequencies of the CDH13 rs6565113 and rs11150556 polymorphisms (p > 0.05). The genotype and allele frequencies of rs6565113 and rs11150556 polymorphisms in the ADHD and control groups were also evaluated between genders, and no significant effect of gender was revealed among ADHD patients for these polymorphisms (p > 0.05).
Relationship Between ADHD and SNPs of LPHN3 Gene
When both the genotype and allele frequencies of the LPHN3 rs68588066 and rs2345039 polymorphisms were compared, no statistically significant difference was found between the ADHD and control groups (p > 0.05). The analysis also failed to show significant differences between the genotype and allele frequencies of the rs68588066 and rs2345039 polymorphisms in ADHD and control groups in terms of gender (p > 0.05).
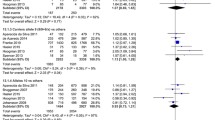
When the LPHN3 rs6551665 polymorphism was taken into consideration, a statistically significant difference was found when comparing the genotype distributions of the A/G polymorphism in the rs6551665 SNP region of the LPHN3 gene between the ADHD and control groups (p = 0.04) (Table 4). In particular, a comparison of the homozygous GG genotype with other genotypes yielded a significant difference (OR: 2.80; 95% CI: 1.12–7.03) (see Table 5). Therefore, individuals with the GG genotype had 2.80-fold greater risk of having ADHD than individuals with other genotypes. There was no significant difference in allele distributions between the ADHD and control groups (p > 0.05) (Table 4).
With regard to differences according to gender, there was no statistically significant difference in the distribution of both genotype and allele frequencies of the LPHN3 rs6551665 polymorphism in the ADHD and control groups by female gender (p > 0.05) (Table 4). There was also no statistically significant difference in the distribution of allele frequencies of the LPHN3 rs6551665 polymorphism in the ADHD and control groups by male gender (p > 0.05) (Table 4). However, in male gender, there was a statistically significant difference in the distribution of genotypes of the LPHN3 rs6551665 between ADHD and control groups (p = 0.046) (Table 4). In addition, a comparison of homozygous GG genotypes with AG and AA+AG genotypes yielded a significant difference according to male gender (OR: 3.05 95% CI: 1.09–8.52; OR: 3.19 95% CI: 1.20–8.51, respectively) (Table 5). Individuals with the GG genotype had a 3.051-fold greater risk of having ADHD when compared to individuals with the AG genotype and 3.197-fold greater risk of ADHD when compared to individuals with the AA+AG genotypes.
When the LPHN3 rs1947274 polymorphism was taken into consideration, a statistically significant difference was found between the ADHD and control groups in the genotype distributions of the A/C polymorphism in the rs1947274 SNP region of the LPHN3 gene (p = 0.02), but no significant difference was found between allele distributions (p > 0.05) (Table 4). Accordingly, a comparison of the homozygous CC genotype with other genotypes yielded a significant difference. It showed that individuals with the CC genotype had a 2.817-fold greater risk of having ADHD than individuals with the AC genotype and a 3.198-fold greater risk of having ADHD than individuals with the AA+AC genotypes. In addition, individuals with the CC genotype had a 3.61-fold greater risk of having ADHD than those with the AA genotype (OR: 2.82 95% CI: 1.10–7.25; OR: 3.2 95% GA: 1.3–7.91; OR: 3616 95% CI: 1.40–9.30, respectively) (Table 5). There was no significant difference in allele distribution between the ADHD and control groups (p > 0.05) (Table 4).
The genotype and allele frequencies of the LPHN3 rs1947274 polymorphism in the ADHD and control groups were also evaluated according to gender. In general, no significant difference was found between male and female individuals (p > 0.05) (Table 4). There was no statistically significant difference in the distribution of genotypes of the LPHN3 rs1947274 polymorphism by female gender between the ADHD and control groups (p > 0.05) (Table 4). In male individuals, however, there was a statistically significant difference in the genotype distribution of the LPHN3 rs1947274 between the ADHD and control groups (p = 0.02) (Table 4). Male individuals with the CC genotype had a 3.50-fold greater risk of having ADHD when compared to male individuals with the AC genotype and a 3.66-fold greater risk than male individuals with the AA+AC genotypes. In addition, male individuals with the CC genotype had a 3.83-fold greater risk of having ADHD than male individuals with the AA genotype (OR: 3.50 95% CI: 1.26–9.68; OR: 3.66 95% GA: 1.39–9.65; OR: 3.83 95% GA: 1.39–10.56, respectively) (Table 5). There was no significant difference in allele distributions between the ADHD and control groups by male gender (p > 0.05) (Table 4).
Relationship of LPHN3 rs6551665 and rs1947274 Polymorphisms to Clinical Features in ADHD Group
In the ADHD group, the relationship between the LPHN3 rs6551665 and rs1947274 polymorphism genotypes, ADHD predominant presentation, and CGI-S and CTRS baseline scores were examined by grouping the AA, AG, GG and AA, AC, CC genotypes, respectively. There was no statistically significant relationship between genotypes of these polymorphisms and clinical parameters except for the CGI-S scores (p > 0.05) (Table 6). When both genotype groups of LPHN3 rs6551665 and rs1947274 polymorphisms were compared according to CGI-S ADHD scores, a statistically significant difference was found between both genotype groups and ADHD CGI-S scores separately (p = 0.012) (Table 6).
Relationship of LPHN3 rs6551665 and rs1947274 Polymorphisms to Treatment Response in ADHD Group
No significant relationship was found between LPHN3 rs1947274 polymorphism genotypes and treatment response evaluated by either CTRS or CGI-I in the ADHD group (p > 0.05). There was also no significant relationship between the LPHN3 rs6551665 polymorphism genotypes and treatment response assessed by CTRS in the ADHD group (p > 0.05). There appeared to be a significant relationship between the genotypes of the LPHN3 rs6551665 polymorphism and the treatment response evaluated by CGI-I (noting that the significance value was at the borderline of the accepted value, p = 0.052). A significant correlation was found between the GG genotype, which was identified as risky genotype in ADHD, and other genotypes of LPHN3 rs6551665 polymorphism in terms of treatment responses to CGI-I (p = 0.027). The results are presented in Table 7. The factors influencing the treatment response assessed by CGI-I (age, gender, ADHD, preterm labor, prematurity, side effect, treatment choice, and disease severity) were evaluated by univariate and multivariate analyses (Table 8). Univariate variables (age and gender equalized) were evaluated in multivariate logistic regression analysis. The results showed that ADHD patients with the GG genotype were 3.4 times as likely to have a poor response to treatment as ADHD patients with the AG or AA genotype (OR: 3.41%95 GA:1.08–10.81) (Table 9). In addition, a high level of ADHD severity assessed by CGI-S before treatment was associated with poor response to treatment (OR: 2.25% 95% CI: 1.31–3.84) (Table 9).
Discussion
In this study, the genotype distribution of the CDH13 rs6565113 and rs11150556 polymorphisms and LPHN3 rs6551665, rs6858066, rs1947274, and rs2345039 polymorphisms was examined in children and adolescents diagnosed with ADHD alongside age- and sex-matched normal, healthy controls. In our sample, there was a significant difference between the ADHD and control groups in terms of genotype distribution of LPHN3 rs6551665 and rs1947274 polymorphisms. It was found that the GG genotype of rs6551665 and CC genotype of rs1947274 polymorphisms were associated with ADHD, and this association was more prominent for male gender. The possible effects of these ADHD-associated polymorphisms on the treatment response in patients with ADHD during clinical follow-up for 12 weeks were also investigated. When the factors influencing the treatment response were examined, a high severity of pretreatment ADHD assessed by CGI-S and the GG genotype of the LPHN3 rs6551665 polymorphism, which we identified as a risky genotype in ADHD, were related to poor response to treatment. The CC genotype, which we determined as a risky genotype, of the LPHN3 rs1947274 polymorphism had no effect on the treatment response in ADHD.
Most of the recent studies focusing on understanding the etiology of ADHD have examined the relationship between the human genome and the risk of developing ADHD and/or phenotypes (Faraone et al. 2014). In studies on the etiology of ADHD, extracellular matrix regulation, neuronal migration, adhesion molecules, and neurotransmission-related genes have been investigated (Franke et al. 2009; Poelmans et al. 2011). Recent results of GWAS showing SNPs in the CDH13 gene region are among the most promising findings with regard to the etiology of ADHD in these studies (Hawi et al. 2018). In our study, the distribution of the CDH13 rs6565113 and rs11150556 SNP regions in the ADHD and control groups was investigated. No significant difference was found between the ADHD and control groups or between male and female gender in the distribution of the genotype and allele frequencies of the CDH13 rs6565113 and rs11150556 polymorphisms. These results are consistent with the study of Salatino-Oliveira et al. (2015), who found no significant difference between the ADHD group and the control group according to the distribution of genotype groups of rs6565113 and rs11150556 polymorphisms. In a GWAS conducted by Lasky-Su et al. (2008), the CDH13 rs655113 polymorphism was associated with the number of symptoms in ADHD. In a study by Arias-Vásquez et al. (2011) evaluating executive functions according to verbal working memory, visual spatial working memory, and inhibition tasks in children and adolescents with ADHD, the polymorphism of CDH13 rs11150556 was associated with verbal working memory performance in children with ADHD. Unlike previous studies, the insignificant results for the CDH13 rs6565113 and rs11150556 polymorphisms reported here could be related to the small size of our sample. In future studies, our findings can be investigated using larger samples.
The relationship between LPHN3 and ADHD was first observed by fine mapping of a Paisa population in Colombia and is being investigated for the first time among a Turkish population, although replication studies have been conducted in other populations (Arcos-Burgos et al. 2010; Bruxel et al. 2015; Gomez-Sanchez et al. 2017; Huang et al. 2019; Hwang et al. 2015). In our study, the differences in the distribution of the genotypes and allele frequencies of the LPHN3 rs6858066 and rs2345039 polymorphisms between ADHD and control groups and between males and females were insignificant. Ribasés et al. (2011) found a statistically significant difference in the distribution of genotypes of the LPHN3 rs6858066 polymorphism in the combined type ADHD and control group. Similar results were reported by Acosta et al. (2016), who found a significant difference between ADHD and control groups in the distribution of allele frequencies of the LPHN3 rs2345039 polymorphism. However, Huang et al. (2019) reported no significant difference between ADHD and control groups in the distribution of the genotypes and allele frequencies of the LPHN3 rs2345039 polymorphism (Huang et al. 2019). In the literature, community-based differences have been reported in the distribution of genotypes and allele frequencies of LPHN3 rs6858066 and rs2345039 polymorphisms previously associated with ADHD. In this sense, our findings are consistent with the results of Huang et al. (2019), but differ from those of other studies. This may be explained by racial differences, as well as by methodological differences such as sample selection and number of samples. Therefore, the results may need to be supported using different samples and methodologies.
The present study showed a significant relationship between LPHN3 rs6551665 and rs1947274 polymorphisms among ADHD patients. We also found that the presence of the GG genotype of the LPHN3 rs6551665 polymorphism or the CC genotype of LPHN3 rs1947274 was a risk factor for ADHD. However, the LPHN3 rs6551665 and rs1947274 polymorphisms were not related to ADHD according to the distribution of allele frequencies between ADHD and control groups and between gender groups. Arcos-Burgos et al. (2010) showed that the G, C, and C alleles of LPHN3 rs6551665, rs1947274, and rs2345039 polymorphisms, respectively, increased the susceptibility to ADHD (Arcos-Burgos et al. 2010). Evidence from Canada supports an interaction between the LPHN3 rs6551665, rs1947274, rs6858066, and rs2345039 polymorphisms and prenatal maternal stress exposure in terms of ADHD (Choudhry et al. 2012). In a study by Hwang et al. (2015), a significant difference was found between genotype distributions of the LPHN3 rs6551665 polymorphism, and it was reported that the incidence of ADHD was 2.95 times higher in those with the GG genotype compared to the control group, and that the incidence of ADHD was 1.44 times higher in those with the G allele. While our results are consistent with previous studies showing a relationship between ADHD and LPHN3 rs6551665 and rs1947274 polymorphisms, they differ from the results of studies conducted in different populations suggesting that there is a relationship between ADHD and the G allele of the LPHN3 rs6551665 polymorphism or the C allele of the LPHN3 rs1947274 polymorphism according to their distribution in ADHD and control groups (Arcos-Burgos et al. 2010; Hwang et al. 2015). This may be due to racial differences and methodologies. Since this study is the first study showing the association between CC genotype of LPHN3 rs1947274 and ADHD, we believe that it provides insight that can serve as a basis for future studies.
In our study, when the genotypes of the LPHN3 rs6551665 and rs1947274 polymorphisms were evaluated separately in ADHD and control groups, it was found that the incidence of ADHD in boys with the GG genotype was 3.2 times that in the control group and the incidence of ADHD in boys with the CC genotype was 3.7 times that of the control group. Since there were no differences between the groups in the genotype distributions of both polymorphisms according to female gender, the probability ratio was not calculated. These results are consistent with the results of a study in which the frequency of male cases with the GG genotype of the LPHN3 rs6551665 polymorphism in an ADHD group was significantly higher than that in the control group (Hwang et al. 2015). In addition, it supports the results of previous studies showing that there may be a relationship between the LPHN3 gene and male ADHD patients (Gomez-Sanchez et al. 2016; Hwang et al. 2015). To the best of our knowledge, the present study is the first to propose that the LPHN3 rs1947274 A/C polymorphism may be related to male gender in ADHD. It is known that there are gender differences in the severity and clinical course of ADHD (Greven et al. 2018; Mowlem et al. 2019). However, our results showed differences in genetic susceptibility between male and female participants. The difference between these results in terms of gender may be related to the higher prevalence of ADHD in male individuals (Thapar et al. 2017). The imbalance between the numbers of boys and girls can be considered another limitation of the study. Having a small number of girls could make comparisons difficult in terms of obtaining significant results.
mRNA of LPHN3 has been reported to show abundant expression in the amygdala, caudate nucleus, cerebellum, and cerebral cortex in humans, and individuals carrying the LPHN3 susceptibility haplotype exhibit a significantly reduced N-acetylaspartate/creatine ratio in the left lateral and medial thalamus and the right striatum (Arcos-Burgos et al. 2010). Lange et al. (2012) showed that a decrease in the functionality of LPHN3 selectively affected the development of the dopaminergic system in zebrafish and triggered excessive motor activity and impulsivity (Lange et al. 2012). The expression of LPHN3, especially in the brain regions involved in ADHD such as the prefrontal cortex, amygdala, and mesolimbic regions (Krain and Castellanos 2006), reinforces the hypotheses regarding its functional relationship with ADHD symptoms. In our study, a significant relationship was found between the genotypes of LPHN3 rs6551665 and rs1947274 polymorphisms and the severity of pretreatment ADHD assessed by CGI-S. The only other study in which this was evaluated was conducted by Choudhry et al. (2012), who investigated the relationship between the LPHN3 rs6551665 and rs1947274 polymorphisms and ADHD severity, in which the A allele of the LPHN3 rs6551665 and rs1947274 polymorphisms was identified as a risk allele for ADHD. Excessive transport activity of the A allele for both polymorphisms was associated with more severe clinical ADHD manifestation (Choudhry et al. 2012). Our findings similarly showed a relationship between ADHD severity and LPHN3 rs6551665 and rs1947274 polymorphisms. Our results are also similar to previous studies that found no significant relationship between the LPHN3 rs6551665 and rs1947274 polymorphisms and predominant presentation of ADHD (Acosta et al. 2016; Jain et al. 2012; Ribasés et al. 2011).
LPHN3 is a member of the latrophilin subfamily of G protein-linked receptors (GPLR) in GABAergic neurotransmission, which has been shown to play an important role in regulating the exocytosis of neurotransmitters, particularly norepinephrine (Eichel and von Zastrow 2018). It has been proposed that polymorphisms that affect the structure of LPHN3 and/or transcription of the gene may affect signal transduction or vesicular trafficking (Brose et al. 2000; Willson et al. 2004). Therefore, polymorphisms in the LPHN3 gene seem to affect synaptic norepinephrine concentration. In recent studies, LPHN3 polymorphisms have been associated with treatment response in ADHD (Arcos-Burgos et al. 2010; Bruxel et al. 2015; Gomez-Sanchez et al. 2017). These studies were replicated in different populations, and inconsistent findings were reported. In a family-based association study conducted by Arcos-Burgos et al. (2010) in the Pasia community, the presence of the G allele in the LPHN3 rs6551665 polymorphism was associated with good response to MPH treatment in ADHD (Arcos-Burgos et al. 2010). A family-based association study conducted by Choudhry et al. (2012) in Canada revealed that LPHN3 rs6551665, rs1947274, and rs6858066 polymorphisms were associated with poor response to MPH treatment according to CGI-I in patients with ADHD with the AAG haplotype formed by the “A, A, G” alleles (respectively), which are known risk alleles for ADHD (Choudhry et al. 2012). In a study by Labbe et al. (2012), it was shown that the presence of the G allele of the LPHN3 rs6551665 polymorphism was associated with poor response to MPH treatment in ADHD (Labbe et al. 2012). A South Korean study investigating the relationship between the SNAP-25, SCLA6A2, and LPHN3 genes and response to OROS-MPH treatment in ADHD found that the LPHN3 rs6551665 and rs1947274 polymorphisms were not associated with treatment response (Song et al. 2014). A study in Brazil also found no association between the LPHN3 rs6551665 and rs1947274 polymorphisms and treatment response (Bruxel et al. 2015). A longitudinal study examining MPH treatment in ADHD and genetic susceptibility to ADHD pharmacogenetics over a 12-month period found no association between the LPHN3 rs6551665 polymorphism and response to MPH (Gomez-Sanchez et al. 2017). In our study, we separately evaluated the relationship between response to treatment in ADHD and various independent variables (ADHD predominance, age, sex, side effects, disease severity) thought to influence treatment response (Bonvicini et al. 2016; Gomez-Sanchez et al. 2017; Polanczyk et al. 2008). A multivariate logistic regression model yielded a significant relationship with treatment response, suggesting that the presence of the GG genotype of the LPHN3 rs6551665 polymorphism and high severity of ADHD before treatment were associated with poor response to treatment. Previous studies have similarly shown that high severity of ADHD before treatment was associated with poor treatment response (Owens et al. 2003). In this sense, our results are consistent with the results of studies showing the association between the LPHN3 rs6551665 polymorphism and treatment response in ADHD (Arcos-Burgos et al. 2010; Choudhry et al. 2012; Labbe et al. 2012). Differences between the findings obtained from our study and those from other studies may be due to the different ethnicities of the samples. Patients from different ethnic groups probably have unique risk/protective factors that affect the effectiveness of ADHD treatment. Also, because of the nature of the study, where no manipulation of variables was performed, we cannot conclude causality among the variables. In addition, methodological variables such as case selection and sample size in our study may have caused these differences. Our study reflects the major difficulties in replicating pharmacogenetic association studies in ADHD. Because the definitions of treatment response in the evaluation scales are different, it may be difficult to replicate the results. In this study, treatment responses were found to differ according to the two scales used to evaluate treatment response. When evaluating the treatment response according to the CTRS, it is important to consider the subjective opinion of the teacher. However, when CGI-I evaluation is made, the results are based on the subjective opinion of the clinician. There are many methods for evaluating treatment response reported in the literature, and there is no clear consensus on which is the most objective and reliable (Adamo et al. 2015). Moreover, this study found that evaluation of treatment response under routine clinical practice increases the likelihood of emphasizing the role of genetic factors in the real world.
Although previous studies have shown the LPHN3 rs6551665 polymorphism to be associated with treatment response in ADHD, ours is the first study to show this association among Turkish adolescents. It is also the first study examining the relationship between the treatment response in ADHD and the presence of LPHN3 rs6551665 and rs1947274 polymorphisms. Since the treatment response may vary with racial differences, our results will shed light on the pharmacogenetic studies to be conducted in a wider sample in the future.
In analyzing the strengths of our study, we believe its most powerful aspect is that it is the first research investigating the relationship between ADHD and the CDH13 and LPHN3 gene polymorphisms, which have been shown to be associated with ADHD in previous studies, in a Turkish population. In addition, exclusion of additional diseases and psychiatric disorders in the selection of the sample can be considered a strength. The constitution of the ADHD group from patients who had not received any medical treatment previously also increases the reliability of the study.
There are some limitations in this study that must be acknowledged and discussed. First, the sample size was small compared to today’s genetic research standard, which may limit the power to determine the genetic relationship. In addition, although there was no difference in treatment response between the two agents used in the ADHD group, failure to evaluate the effects of the LPHN3 gene on the treatment response separately can be considered a limitation. Genetic variants might moderate dose response, but we did not evaluate gene–dose interactions, and the maximum doses of MPH and ATX used in this study were lower than the maximum recommended doses (60 mg/day for MPH and 1.4 > mg/kg for ATX). Another limitation is the verbal evaluation of side effects known to have an effect on treatment response only through parents’ and children’s feedback.
Conclusion
This is the first study to investigate the relationship between ADHD and the CDH13 and LPHN3 gene polymorphisms in a Turkish population. Our study showed that the LPHN3 rs6551665 and rs1947274 polymorphisms had a significant relationship with ADHD, which was demonstrated in particular in the male gender. The presence of the GG genotype of the LPHN3 rs6551665 polymorphism may be related to poor response to treatment among Turkish adolescents with ADHD. The results of our study will provide insight for further studies in the pharmacogenetic domain. Moreover, the findings of our study may empower genetic counseling for early diagnosis, opening a pathway for determining suitable treatment for patients and avoiding preventable risk factors. Our results were obtained with a relatively limited sample for such a complex disease as ADHD. Therefore, multicenter and even international pharmacogenetics studies may be required in the future to support these findings.
References
Acosta MT et al (2016) ADGRL3 (LPHN3) variants are associated with a refined phenotype of ADHD in the MTA study. Mol Genet Genomic Med 4:540–547. https://doi.org/10.1002/mgg3.230
Adamo N, Seth S, Coghill D (2015) Pharmacological treatment of attention-deficit/hyperactivity disorder: assessing outcomes. Expert Rev Clin Pharmacol 8(4):383–397. https://doi.org/10.1586/17512433.2015.1050379
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders (DSM-5®). American Psychiatric Pub, Arlington. https://doi.org/10.1176/appi.books.9780890425596
Arcos-Burgos M et al (2004) Attention-deficit/hyperactivity disorder in a population isolate: linkage to loci at 4q13. 2, 5q33. 3, 11q22, and 17p11. Am J Hum Genet 75(6):998–1014. https://doi.org/10.1086/426154
Arcos-Burgos Á et al (2010) A common variant of the latrophilin 3 gene, LPHN3, confers susceptibility to ADHD and predicts effectiveness of stimulant medication. Mol Psychiatry 15(11):1053–1066. https://doi.org/10.1038/mp.2010.6
Arias-Vásquez A et al (2011) CDH13 is associated with working memory performance in attention deficit/hyperactivity disorder. Genes Brain Behav 10(8):844–851. https://doi.org/10.1111/j.1601-183X.2011.00724.x
Bonvicini C, Faraone S, Scassellati C (2016) Attention-deficit hyperactivity disorder in adults: a systematic review and meta-analysis of genetic, pharmacogenetic and biochemical studies. Mol Psychiatry 21:872–884. https://doi.org/10.1038/mp.2016.74
Brose N, Rosenmund C, Rettig J (2000) Regulation of transmitter release by Unc-13 and its homologues. Curr Opin Neurobiol 10(3):303–311. https://doi.org/10.1016/s0959-4388(00)00105-7
Bruxel EM et al (2015) LPHN3 and attention-deficit/hyperactivity disorder: a susceptibility and pharmacogenetic study. Genes Brain Behav 14:419–427. https://doi.org/10.1111/gbb.12224
Busner J, Targum SD (2007) The clinical global impressions scale: applying a research tool in clinical practice. Psychiatry (Edgmont) 4(7):28–37
Choudhry Z, Sengupta SM, Grizenko N, Fortier ME, Thakur GA, Bellingham J, Joober R (2012) LPHN3 and attention-deficit/hyperactivity disorder: interaction with maternal stress during pregnancy. J Child Psychol Psychiatry 53(8):892–902. https://doi.org/10.1111/j.1469-7610.2012.02551.x
Dereboy Ç, Şenol S, Şener Ş, Dereboy F (2007) Conners Kısa Form Öğretmen ve Ana Baba Derecelendirme Ölçeklerinin Geçerliği. Türk Psikiyatri Derg 18:48–58
Eichel K, von Zastrow M (2018) Subcellular organization of GPCR signaling. Trends Pharmacol Sci 39(2):200–208. https://doi.org/10.1016/j.tips.2017.11.009
Ercan ES, Bilaç Ö, Özaslan TU, Rohde LA (2015) Is the prevalence of ADHD in Turkish elementary school children really high? Soc Psychiatry Psychiatr Epidemiol 50(7):1145–1152. https://doi.org/10.1007/s00127-015-1071-9
Faraone SV, Perlis RH, Doyle AE, Smoller JW, Goralnick JJ, Holmgren MA, Sklar P (2005) Molecular genetics of attention-deficit/hyperactivity disorder. Biol Psychiatry 57(11):1313–1323. https://doi.org/10.1016/j.biopsych.2004.11.0243
Faraone SV, Bonvicini C, Scassellati C (2014) Biomarkers in the diagnosis of ADHD—promising directions. Curr Psychiatr Rep 16:497. https://doi.org/10.1007/s11920-014-0497-1
Franke B, Neale BM, Faraone SV (2009) Genome-wide association studies in ADHD. Hum Genet 126(1):13–50. https://doi.org/10.1007/s00439-009-0663-4
Gökler B, Ünal F, Pehlivantürk B, Kültür EÇ, Akdemir D, Taner Y (2004) Okul Çaği Çocuklari İçin Duygulanim Bozukluklari ve Şizofreni Görüşme Çizelgesi-Şimdi ve Yaşam Boyu Şekli-Türkçe uyarlamasinin geçerlik ve güvenirliği. Çocuk ve Gençlik Ruh Sağliği Dergisi 11:109–116
Gomez-Sanchez CI et al (2016) Attention deficit hyperactivity disorder: genetic association study in a cohort of Spanish children. Behav Brain Funct 12:2. https://doi.org/10.1186/s12993-015-0084-6
Gomez-Sanchez CI et al (2017) Pharmacogenetics of methylphenidate in childhood attention-deficit/hyperactivity disorder: long-term effects. Sci Rep 7:10391. https://doi.org/10.1038/s41598-017-10912-y
Greven CU, Richards JS, Buitelaar JK (2018) Sex differences in ADHD. In: Banaschewski T (ed) Oxford textbook of attention deficit hyperactivity disorder. Oxford University Press, Oxford, p 154. https://doi.org/10.1093/med/9780198739258.003.0016
Güney E, Ceylan MF, İşeri E (2014) Dikkat eksikliği hiperaktivite bozukluğunda aday gen çalışmaları. Psikiyatride Guncel Yaklasimlar-Curr Approaches Psychiatr 3:664–682. https://doi.org/10.18863/pgy.334547
Hawi Z, Tong J, Dark C, Yates H, Johnson B, Bellgrove MA (2018) The role of cadherin genes in five major psychiatric disorders: a literature update. Am J Med Genet B Neuropsychiatr Genet 177(2):168–180. https://doi.org/10.1002/ajmg.b.32592
Hazell PL, Kohn MR, Dickson R, Walton RJ, Granger RE, van Wyk GW (2011) Core ADHD symptom improvement with atomoxetine versus methylphenidate: a direct comparison meta-analysis. J Atten Disord 15(8):674–683. https://doi.org/10.1177/1087054710379737
Huang X, Zhang Q, Gu X, Hou Y, Wang M, Chen X, Wu J (2019) LPHN3 gene variations and susceptibility to ADHD in Chinese Han population: a two-stage case-control association study and gene-environment interactions. Eur Child Adolesc Psychiatry 28:861–873. https://doi.org/10.1007/s00787-018-1251-8
Hwang IW, Lim MH, Kwon HJ, Jin HJ (2015) Association of LPHN3 rs6551665 A/G polymorphism with attention deficit and hyperactivity disorder in Korean children. Gene 566(1):68–73. https://doi.org/10.1016/j.gene.2015.04.033
Jain M et al (2012) A cooperative interaction between LPHN3 and 11q doubles the risk for ADHD. Mol Psychiatry 17:741–747. https://doi.org/10.1038/mp.2011.59
Kaufman J et al (1997) Schedule for affective disorders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry 36(7):980–988. https://doi.org/10.1097/00004583-199707000-00021
Kemner JE, Starr HL, Ciccone PE, Hooper-Wood CG, Crockett RS (2005) Outcomes of OROS® methylphenidate compared with atomoxetine in children with ADHD: a multicenter, randomized prospective study. Adv Ther 22:498–512. https://doi.org/10.1007/BF02849870
Kieling C, Genro JP, Hutz MH, Rohde LA (2010) A current update on ADHD pharmacogenomics. Pharmacogenomics 11(3):407–419. https://doi.org/10.2217/pgs.10.28
Krain AL, Castellanos FX (2006) Brain development and ADHD. Clin Psychol Rev 26(4):433–444. https://doi.org/10.1016/j.cpr.2006.01.005
Labbe A, Liu A, Atherton J, Gizenko N, Fortier ME, Sengupta SM, Ridha J (2012) Refining psychiatric phenotypes for response to treatment: contribution of LPHN3 in ADHD. Am J Med Genet B Neuropsychiatr Genet 159B:776–785. https://doi.org/10.1002/ajmg.b.32083
Lange M et al (2012) The ADHD-susceptibility gene LPHN3. 1 modulates dopaminergic neuron formation and locomotor activity during zebrafish development. Mol Psychiatry 17:946–954. https://doi.org/10.1038/mp.2012.29
Langenhan T (2020) Adhesion G protein–coupled receptors—candidate metabotropic mechanosensors and novel drug targets. Basic Clin Pharmacol Toxicol 126(Suppl. 6):5–16. https://doi.org/10.1111/bcpt.13223
Lasky-Su J et al (2008) Genome-wide association scan of quantitative traits for attention deficit hyperactivity disorder identifies novel associations and confirms candidate gene associations. Am J Med Genet B Neuropsychiatr Genet 147B(8):1345–1354. https://doi.org/10.1002/ajmg.b.30867
Manolio T et al (2007) New models of collaboration in genome-wide association studies: the genetic association information network. Nat Genet 39:1045–1105. https://doi.org/10.1038/ng2127
Mowlem FD, Rosenqvist MA, Martin J, Lichtenstein P, Asherson P, Larsson H (2019) Sex differences in predicting ADHD clinical diagnosis and pharmacological treatment. Eur Child Adolesc Psychiatr 28:481–489. https://doi.org/10.1007/s00787-018-1211-3
Myer N, Boland J, Faraone S (2018) Pharmacogenetics predictors of methylphenidate efficacy in childhood ADHD. Mol Psychiatry 23(9):1929–1936. https://doi.org/10.1038/mp.2017.234
Neale BM et al (2010) Meta-analysis of genome-wide association studies of attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 49(9):884–897. https://doi.org/10.1016/j.jaac.2010.06.008
O’Sullivan ML, de Wit J, Savas JN, Comoletti D, Otto-Hitt S, Yates JR 3rd, Ghosh A (2012) FLRT proteins are endogenous latrophilin ligands and regulate excitatory synapse development. Neuron 73:903–910. https://doi.org/10.1016/j.neuron.2012.01.018
Owens EB et al (2003) Which treatment for whom for ADHD? Moderators of treatment response in the MTA. J Consult Clin Psychol 71(3):540–552. https://doi.org/10.1037/0022-006x.71.3.540
Patel SD, Chen CP, Bahna F, Honig B, Shapiro L (2003) Cadherin-mediated cell–cell adhesion: sticking together as a family. Curr Opin Struct Biol 13(6):690–698. https://doi.org/10.1016/j.sbi.2003.10.007
Poelmans G, Pauls DL, Buitelaar JK, Franke B (2011) Integrated genome-wide association study findings: identification of a neurodevelopmental network for attention deficit hyperactivity disorder. Am J Psychiatry 168(4):365–377. https://doi.org/10.1176/appi.ajp.2010.10070948
Polanczyk G et al (2008) The impact of individual and methodological factors in the variability of response to methylphenidate in ADHD pharmacogenetic studies from four different continents. Am J Med Genet B Neuropsychiatr Genet 147B(8):1419–1424. https://doi.org/10.1002/ajmg.b.30855
Ribasés Á et al (2011) Contribution of LPHN3 to the genetic susceptibility to ADHD in adulthood: a replication study. Genes Brain Behav 10(2):149–157. https://doi.org/10.1111/j.1601-183X.2010.00649.x
Rivero O, Sich S, Popp S, Schmitt A, Franke B, Lesch K-P (2013) Impact of the ADHD-susceptibility gene CDH13 on development and function of brain networks. Eur Neuropsychopharmacol 23(6):492–507. https://doi.org/10.1016/j.euroneuro.2012.06.009
Salatino-Oliveira A et al (2015) Cadherin-13 gene is associated with hyperactive/impulsive symptoms in attention/deficit hyperactivity disorder. Am J Med Genet B Neuropsychiatr Genet 168B(3):162–169. https://doi.org/10.1002/ajmg.b.32293
Song J et al (2014) Association of SNAP-25, SLC6A2, and LPHN3 with OROS methylphenidate treatment response in attention-deficit/hyperactivity disorder. Clin Neuropharmacol 37:136–141. https://doi.org/10.1097/WNF.0000000000000045
Takeuchi T, Misaki A, Liang SB, Tachibana A, Hayashi N, Sonobe H, Ohtsuki Y (2000) Expression of T-cadherin (CDH13, H-cadherin) in human brain and its characteristics as a negative growth regulator of epidermal growth factor in neuroblastoma cells. J Neurochem 74(4):1489–1497. https://doi.org/10.1046/j.1471-4159.2000.0741489.x
Thapar A, Cooper M, Rutter M (2017) Neurodevelopmental disorders. Lancet Psychiatry 4(4):339–346. https://doi.org/10.1016/S2215-0366(16)30376-5
Willcutt EG (2012) The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics 9(3):490–499. https://doi.org/10.1007/s13311-012-0135-8
Willson J et al (2004) Latrotoxin receptor signaling engages the UNC-13-dependent vesicle-priming pathway in C. elegans. Curr Biol 14(15):1374–1379. https://doi.org/10.1016/j.cub.2004.07.056
Acknowledgments
We would like to thank the Gazi University Scientific Research Projects Department and the children and their families for participating in the study on a voluntary basis.
Funding
This research was supported by Gazi University Scientific Research Projects (project code no: 01/2018-17, 2018).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. This study procedure was reviewed and approved by the Clinical Research Ethics Committee of Keçiören Training and Research Hospital in accordance with the article 2012- KAEK-15/1580 dated 10.01.2018.
Conflict of Interest
The authors declare that they have no conflict of interest. The funding sources had no role in the study design, in the interpretation of data, or in the writing of the manuscript.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Özaslan, A., Güney, E., Ergün, M.A. et al. CDH13 and LPHN3 Gene Polymorphisms in Attention-Deficit/Hyperactivity Disorder: Their Relation to Clinical Characteristics. J Mol Neurosci 71, 394–408 (2021). https://doi.org/10.1007/s12031-020-01662-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-020-01662-0