Abstract
Background
Identical bursts on electroencephalography (EEG) are considered a specific predictor of poor outcomes in cardiac arrest, but its relationship with structural brain injury severity on magnetic resonance imaging (MRI) is not known.
Methods
This was a retrospective analysis of clinical, EEG, and MRI data from adult comatose patients after cardiac arrest. Burst similarity in first 72 h from the time of return of spontaneous circulation were calculated using dynamic time-warping (DTW) for bursts of equal (i.e., 500 ms) and varying (i.e., 100–500 ms) lengths and cross-correlation for bursts of equal lengths. Structural brain injury severity was measured using whole brain mean apparent diffusion coefficient (ADC) on MRI. Pearson’s correlation coefficients were calculated between mean burst similarity across consecutive 12–24-h time blocks and mean whole brain ADC values. Good outcome was defined as Cerebral Performance Category of 1–2 (i.e., independence for activities of daily living) at the time of hospital discharge.
Results
Of 113 patients with cardiac arrest, 45 patients had burst suppression (mean cardiac arrest to MRI time 4.3 days). Three study participants with burst suppression had a good outcome. Burst similarity calculated using DTW with bursts of varying lengths was correlated with mean ADC value in the first 36 h after cardiac arrest: Pearson’s r: 0–12 h: − 0.69 (p = 0.039), 12–24 h: − 0.54 (p = 0.002), 24–36 h: − 0.41 (p = 0.049). Burst similarity measured with bursts of equal lengths was not associated with mean ADC value with cross-correlation or DTW, except for DTW at 60–72 h (− 0.96, p = 0.04).
Conclusions
Burst similarity on EEG after cardiac arrest may be associated with acute brain injury severity on MRI. This association was time dependent when measured using DTW.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Each year, approximately 475,000 Americans die of cardiac arrest [1]. Survival to hospital discharge for out-of-hospital cardiac arrest is approximately 10%, and 70% of patients admitted to the hospital die after withdrawal of life-sustaining therapies (WLST) due to severe brain injury [2, 3]. Therefore, precise and accurate brain injury diagnostic tools are essential for individualizing interventions and prognostication early on.
Current multimodal approaches to neurological prognostication integrating clinical examination, electroencephalography (EEG) monitoring, and brain imaging have limited sensitivity for early identification of patients with potential for neurological recovery and imperfect specificity to identify patients with irreversible injury [4,5,6]. EEG has emerged as a helpful tool for early stratification of recovery potential. However, the influence of sedatives on EEG signals raises concerns for clinicians when relying on these tests for decisions about WLST [7]. Burst suppression is considered one of the most specific EEG predictors of poor outcome, but current guidelines recommend the use of this EEG pattern only 24–72 h after arrest if there is no concurrent use of sedatives, which can be challenging in critically ill patients [7, 8]. Burst suppression with identical bursts is a subtype of burst suppression characterized by bursts with very high signal correlation, and it has been proposed that this pattern is nearly always associated with poor outcome independent of temperature modulation or sedative effects [9,10,11,12,13,14,15]. However, evaluation of prognostic tests in cardiac arrest can be confounded by self-fulfilling prophecies from WLST. Diffusion magnetic resonance imaging (MRI) of the brain can provide an unbiased assessment of structural brain injury after cardiac arrest as it precedes WLST in these patients [16]. Therefore, demonstrating an association between identical bursts and injury on MRI would further support the role of identical bursts in prognostication and corroborate previous studies with postmortem brain histopathology [17]. Moreover, quantifying the evolution of identical bursts from the time of cardiac arrest and defining the optimal timing and method for burst similarity evaluation needs additional investigation.
In this two-center study, our primary hypothesis was that the degree of EEG burst similarity measured during burst suppression reflects the severity of structural brain injury after cardiac arrest on MRI. To address this hypothesis, we used an objective measure of structural brain injury, that is, apparent diffusion coefficient (ADC) on MRI. In addition, we describe the application of a novel method for burst similarity evaluation (dynamic time-warping [DTW]) against a standard metric for burst similarity evaluation (cross-correlation [XCORR]).
Materials and Methods
Standard Protocol Approvals and Patient Consents
This retrospective study was approved by the Partners Healthcare Institutional Review Board, and informed consent was waived.
Cohort
This was a retrospective analysis of clinical, EEG, and MRI data from patients with cardiac arrest admitted to the Massachusetts General Hospital and Brigham and Women’s Hospital from July 2009 to February 2017. The inclusion criteria were nontraumatic cardiac arrest, age ≥ 18 years, return of spontaneous circulation (ROSC), Glasgow Coma Scale score ≤ 8 on admission, use of targeted temperature management (TTM) of 32–34 °C, and prognostication using EEG and MRI. The exclusion criteria were acute cerebral hemorrhage or acute cerebral infarction. Sedation was routinely administered to patients using propofol at 0–80 μg/kg/min and fentanyl at 0–200 μg/kg/min during TTM and continued as needed based on clinicians’ discretion. Midazolam infusion at 0–5 mg/h was used depending on side effects or contraindications to propofol. Patients were monitored with EEG as soon as possible following intensive care unit admission, and EEG monitoring was continued until after rewarming, unless study participants regained consciousness, had WLST, or died. EEG recordings in participating hospitals use 19 channels and follow the 10–20 international system. Brain MRI was performed between days 2 and 12 after cardiac arrest for all patients included in the study. Neurological outcome at hospital discharge was determined by retrospective review of the electronic health record using the Cerebral Performance Category (CPC) [8]. Good outcome was defined as a CPC score of 1–2 (i.e., independence for activities of daily living).
Quantitative EEG Analysis
EEGs were downsampled to 100 Hz, bandpass filtered from 0.5 to 50 Hz, and re-referenced to a bipolar montage. Bursts and burst suppression epochs were measured on individual EEG channels [18]. Within each EEG channel, samples were labeled as either (1) burst or (0) suppression by calculating recursive variance when a sample exceeded a variance threshold. We set the variance threshold for a timestep to be labeled as a burst to 1.75 Hz based on the optimal variance threshold for burst suppression detection in a previous study from our group [18]. The forgetting time, which controls the weight of past values in the recursive variance estimate of the current timestep, was set to 0.1047 [18].
Local burst suppression detections (per channel) were combined into a global (all channels) burst suppression detection, and a sample was labeled as a suppression if there was at least 60% agreement between channels [19]. Otherwise, the sample was labeled as a burst. Any suppression epoch shorter than 0.5 s was not labeled as suppression.
Burst Suppression Ratio and Burst Suppression Episodes
Burst suppression ratio is defined as the percentage of time steps labeled as suppression (< 5 uV amplitude) in a sliding window of 1 min using the global burst suppression labels. Burst suppression episodes were defined as epochs of time when burst suppression ratios were greater than 50% for a minimum of 10 consecutive minutes. Burst similarity analysis only included bursts contained within burst suppression episodes. If two burst suppression episodes were less than 60 s apart, the two episodes were considered as one continuous burst suppression episode. Interburst intervals were not recorded.
Burst Similarity Analysis
For each burst suppression episode, a similarity value was calculated for all available burst pairs occurring within the episode independent of its length. All burst values were individually normalized by mean and standard deviation [20]. Burst similarity analysis was performed with (1) XCORR using bursts with equal lengths, (2) DTW using bursts with equal lengths, and (3) DTW using bursts with varying lengths. To evaluate bursts with equal lengths, bursts lasting shorter than 500 ms and longer than 5 s were removed from analysis. To evaluate bursts with varying lengths, bursts lasting shorter than 100 ms and longer than 5 s were removed from analysis. For all analyses, only signal data within 500 ms from bursts’ starting times were used [9]. Allowing similarity calculation for burst shapes of varying lengths in the third implementation using DTW took advantage of the algorithm’s flexibility in comparing signals of different lengths, which is not possible using XCORR because it only allows comparison of signals with the same length. Qualitative assessment of identical bursts was not pursued. Analysis of features within each burst (e.g., entropy or spectral) was not pursued.
XCORR measures the similarity between two signals by performing a dot product between a pair of signals across various sliding positions, and it was implemented using the MATLAB xcorr (version 2017a; Mathworks, Natick, MA) function over a range of lags. The maximum value of the correlation over all time lags was stored for each pair of bursts. DTW measures the similarity between two signals after they are optimally aligned. Use of DTW allows for small amounts of local “warping” (stretching or shrinking) of the time axis to achieve optimal alignment, that is, to minimize the sum of the mean squared differences between the two signals after alignment [21]. Constraints on the largest temporal shift allowed (the “Sakoe-Chiba bound”) was set to 200 samples. Smaller DTW values indicate higher similarity (smaller difference) between the two signals after alignment. Similarity detection for DTW and XCORR was performed for all bursts within a burst suppression episode.
Time-Dependent Burst Similarity Analysis
Mean burst similarity was calculated using a sliding window for each individual burst and its 10 neighbors to the left and 10 neighbors to the right (XCORR and DTW). DTW similarity values were normalized and subtracted from 1 so that burst similarity values for DTW and XCORR were between 0 and 1 (1 indicating highest similarity).
Analysis of 50 Sequential Bursts Without Time-Dependent Analysis
To compare findings with the original XCORR method for identical bursts determination, segments of 50 sequential bursts closest to the 24-h timestamp following cardiac arrest were identified for each study participant with burst suppression episodes [9].
Brain MRI Analysis
Average whole brain ADC signal intensity was obtained using a semiautomated method, as previously described (Analyze Pro 1.0; Overland Park, KS) [22]. Briefly, the entire brain was identified as a region of interest on diffusion weighted sequences, and the resulting map was transferred to the ADC sequence. Artifact and cerebrospinal fluid were removed by masking out signal below 200 mm2/s and greater than 2000 mm2/s, respectively. Mean ADC signal intensity was then measured on the filtered region of interest map.
Correlation Between Burst Similarity and Whole Brain Mean ADC
Pearson’s correlation coefficients (r) and p values were calculated between whole brain mean ADC intensity and burst similarity for each 12–24-h time block. Not all patients had EEG data available at all epochs; therefore, the number of patients per time block varies based on EEG data availability.
Statistical Analysis
Univariate analysis of different groups was performed using Pearson χ2 for categorical variables, t-tests for continuous variables with normal distribution, and Mann–Whitney U-tests for variables without normal distribution. Statistical significance was set to an alpha level of 0.05.
Results
Of the 118 screened study participants who had both EEG monitoring and brain MRI, five patients were excluded because their EEG recordings started more than 5 days following ROSC (Supplementary Fig. 1). The mean age of the final cohort including 113 patients was 53.6 years (standard deviation 17.4), and 63.7% were men. Ventricular fibrillation or ventricular tachycardia (44.3%) was the most common initial rhythm, followed by pulseless electrical activity (29.2%), asystole (13.3%), and unknown (13.3%). Thirty (26.6%) study participants had a good neurological outcome at discharge (CPC 1–2), 11 (9.7%) had a CPC of 3, five (4.4%) had a CPC of 4, and 67 (59.3%) had a CPC of 5. The WLST rate was 89.3% for patients with CPC of 5. Burst suppression episodes were identified in 45 (39.8%) study participants; three study participants had a good neurological outcome at discharge (CPC 2), two had a CPC of 3, four a CPC of 4, and 36 CPC of 5. The WLST rate was 88.3% for patients with CPC of 5 who had burst suppression. The mean time to MRI from ROSC for patients with burst suppression was 4 days (standard deviation 1.8 days), and five patients had MRI done between days 5 and 12. The mean whole brain ADC value was 1,026 mm2/s for good outcome and 855 mm2/s for poor outcome groups. Characteristics for patients with burst suppression and the entire cohort are summarized in Table 1 and Supplementary Table 1, respectively.
Temporal Trends for Burst Suppression Ratio
The longitudinal evolution of burst suppression ratios from the time of cardiac arrest is summarized in Fig. 1 (each row represents the hourly burst suppression ratio for one study participant and rows are ranked by CPC scores). Only three study participants with burst suppression had good outcome, and the duration of burst suppression was shorter and resolved earlier than study participants with poor outcome.
Evolution of burst suppression ratio per hour from time of cardiac arrest, stratified by neurological outcome (Cerebral Performance Category score 1–5). Lighter yellow color indicates a higher percentage of time segments labeled as suppression within a 1-min sliding window. Light gray portions indicate the absence of burst suppression episodes. White spaces indicate missing signal or artifacts within the electroencephalography signal. Patients were ranked by overall mean burst suppression ratio within each Cerebral Performance Category score (Color figure online)
Burst Similarity Temporal Evolution
We summarized the temporal evolution of XCORR and DTW for bursts with equal lengths and DTW for bursts with varying lengths in Fig. 2. Evolution of burst similarity was variable between patients, with similarity trends varying from stable to up trending or down trending overtime. Mean similarity was higher for patients with poor outcome than the three patients with good outcome. Mean burst similarity between good outcome patients (n = 3) and poor outcome patients (n = 42) was 0.52 versus 0.56 for XCORR, 0.47 versus 0.54 for DTW with bursts of equal lengths, and 0.50 versus 0.59 for DTW with bursts of varying lengths.
Evolution of burst similarity for patients with burst suppression per hour since the time of cardiac arrest, stratified by neurological outcome (Cerebral Performance Category score 1–5). a Burst similarity calculated using XCORR with bursts of equal lengths. b Burst similarity calculated using DTW with bursts of equal lengths. c Burst similarity calculated using DTW with bursts of varying lengths. Values closer to 1 (yellow) indicate higher similarity between bursts. Light gray portions indicate absence of burst suppression episodes. White spaces indicate missing signal or artifacts within the electroencephalography signal. DTW, dynamic time-warping, XCORR, cross-correlation (Color figure online)
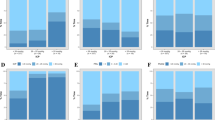
Temporal Burst Similarity Correlation with Whole Brain Mean ADC
High burst similarity was correlated with worse brain injury on MRI (i.e., lower mean ADC). We summarize mean burst similarity across 72 h and whole brain mean ADC correlation with XCORR and DTW for bursts with equal lengths and DTW for bursts with varying lengths (Fig. 3). This association was significant with bursts measured in the first 36 h using DTW with bursts of varying lengths (Pearson’s r: 0–12 h: − 0.69 [p = 0.039], 12–24 h: − 0.54 [p = 0.002], 24–36 h: − 0.41 [p = 0.049], 36–48 h: − 0.32 [p = 0.22], 48–60 h: 0.24 [p = 0.54], 60–72 h: 0.14 [p = 0.86]). The correlation between burst similarity and whole brain mean ADC values using XCORR and DTW for bursts with equal lengths was not significant except for DTW at 60–72 h; however, only four patients had burst suppression within that time window (Pearson’s r: 0–12 h: − 0.17 and − 0.43 [p = 0.67 and 0.24], 12–24 h: − 0.21 and 0.01 [p = 0.28 and 0.96], 24–36 h: − 0.20 and − 0.19 [p = 0.35 and 0.38], 36–48 h: − 0.36 and − 0.28 [p = 0.16 and 0.28], 48–60 h: 0.01 and − 0.31 [p = 0.99 and 0.45], 60–72 h: 0.21 and − 0.96 [p = 0.79 and 0.04]). The results for mean burst similarity correlation with whole brain mean ADC values across consecutive 12 h blocks are summarized in Fig. 4.
Relationship between mean ADC on brain MRI and mean burst similarity during 1–72 h since time of cardiac arrest. a Burst similarity calculated using XCORR with bursts of equal lengths. b Burst similarity calculated using DTW with bursts of equal lengths. c Burst similarity calculated using DTW with bursts of varying lengths. ADC apparent diffusion coefficient, DTW dynamic time-warping, XCORR cross-correlation
Correlations between mean ADC on brain magnetic resonance imaging and mean burst similarity across consecutive 12-h time periods since the time of cardiac arrest. a Burst similarity calculated using XCORR with bursts of equal lengths. b Burst similarity calculated using DTW with bursts of equal lengths. c Burst similarity calculated using DTW with bursts of varying lengths. The number of patients who had EEG available at each 12-h block is indicated in the x-axis. ADC apparent diffusion coefficient, DTW dynamic time-warping, EEG electroencephalography, XCORR cross-correlation
Burst Similarity Analysis for First 50 Consecutive Bursts
Two study participants in the poor outcome group were excluded because they did not have 50 consecutive bursts with lengths of at least 500 ms. Mean burst similarity values for XCORR and DTW were 0.42 and 0.74 among good outcome patients and 0.50 and 0.78 among poor outcome patients, respectively. None of the three patients with good outcomes had mean XCORR similarity greater than 0.75, which was the threshold for identical bursts determined in the original report describing identical bursts [9]. Figure 5 shows a visualization of two exemplary study participants with good or poor outcome in which all 50 bursts are overlaid.
Example burst plots and burst similarity for 50 burst epochs for good and poor outcome patients. a 50 burst shapes overlaid from good outcome patient (CPC 2). b Selected burst shapes plotted individually for good outcome patients. c Similarity calculated using cross-correlation on left and dynamic time-warping on right for good outcome patients. d Quantitative brain magnetic resonance imaging map shows bilateral thalamic hypoxic-ischemic brain injury without severe bilateral hemispheric cortical injury (mean whole brain ADC: 982 mm2/s). e 50 burst shapes overlaid from poor outcome patient (CPC 5). f Selected burst shapes plotted individually for poor outcome patient. g Similarity calculated using cross-correlation on the left and dynamic time-warping on the right for poor outcome patient. Red coloring in burst indicates the first 500 ms used for similarity analysis. h Quantitative brain magnetic resonance imaging map shows severe bilateral hemispheric cortical injury, which is worse in the posterior temporo-parietal and occipital regions (mean whole brain ADC: 778 mm2/s). ADC apparent diffusion coefficient, CPC Cerebral Performance Category, EEG electroencephalography (Color figure online)
Discussion
This study demonstrates that burst similarity measured early during burst suppression after cardiac arrest is associated with severity of structural brain injury on MRI. Burst similarity was measured through automated computational analysis of all bursts available on EEG, which was compared against whole brain quantitative analysis of diffusion weighted imaging on MRI. Importantly, this quantitative approach to validating burst similarity as an early marker of brain injury severity using MRI is not directly affected by bias from self-fulfilling prophesies related to clinical decisions about continuation of life-sustaining therapies because brain MRI is obtained prior to WLST. Potential bias from qualitative review of EEG and MRI studies is mitigated through the use of automated techniques. In addition, we propose a new method for burst similarity calculation (DTW) that is more flexible in the quantification of burst similarity by allowing nonlinear alignment of burst signals. This approach uncovered the longitudinal time-dependency of burst similarity, which had the highest association with brain injury severity within 24 h from cardiac arrest, losing its value after 36 h. These results corroborate the potential value of high burst similarity as an early marker of severe brain injury after cardiac arrest. These results emphasize the opportunity of research using automated computational analysis of EEG for early patient risk stratification and monitoring that may prevent premature WLST or unnecessary ancillary testing.
Identical bursts represent a low-dimensional state of brain activity dynamics characterized by bursts with high synchronicity caused by significant hypoxic-ischemic brain injury following cardiac arrest [9, 23]. All study participants in our cohort with average burst similarity above 0.5 using XCORR had poor outcome, corroborating several studies that have identified burst suppression with identical bursts as a marker of poor prognosis in cardiac arrest; however, WLST is an important confounder [9,10,11,12,13,14,15]. An important limitation of previous literature was that the ground truth for evaluation of predictive performance using identical bursts was neurologic functional outcome, which could have been biased by self-fulfilling prophesies, as the presence of burst suppression on EEG might lead to discontinuation of life-sustaining therapies when that information was presented to treating clinicians. The current study confirmed that the degree of burst similarity was associated with poor outcomes, but it also demonstrated that burst similarity is associated with severity of brain injury on diffusion MRI. A previous study from Barbella and colleagues [10] have also demonstrated that the presence of identical bursts was associated with severity of brain injury measured using neuron-specific enolase, underscoring the potential of burst similarity as a functional measure of neuronal damage. A study from Keijzer and colleagues [24] highlighted that EEG and MRI are complementary in prognostic assessment.
The flexibility of DTW in measuring time-series similarity enabled characterization of burst similarity despite variability in synchronicity between bursts. An advantage of the method of one-to-many matching that DTW applies is the analysis of signals of different lengths, as opposed to XCORR, which can only compare bursts with the same lengths. In addition, use of DTW in this analysis uncovered the evolution of similarity over time that was not apparent with XCORR, demonstrating that decrease in similarity was generally observed over time for patients with both good and poor outcome. This decrease in similarity was also associated with lower association with brain injury severity on MRI, suggesting that early similarity measures might be superior to late measures for prediction of brain injury burden. This observation would go against recommendations of only using EEG information about burst suppression after 24 h from the time of arrest and only when patients are completely off sedation [7]. Previous studies have shown that the important prognostic value of burst suppression within the first 24 h from arrest and despite concomitant use of sedatives and temperature control [25,26,27,28,29]. Early information from EEG is helpful in prognostication, but it must be part of a multimodal evaluation that incorporates assessment of confounders.
The limitations from this study pose further questions for future research into the predictive power of burst suppression with identical bursts in cardiac arrest. Given that only three patients with burst suppression in our cohort had good outcome, further research with larger patient cohorts would allow better comparison of outcome predictive performance of burst similarity measured with XCORR, DTW, and qualitative human morphological assessment. Evaluation of burst features (e.g., entropy, frequency) and burst discontinuity evolution may add to predictive performance and biological mechanisms underlying burst similarity [30, 31]. Our cohort had lower burst similarity than other cohorts and may not be representative. This could have been due to inclusion of patients with less severe burst suppression in our cohort, as only patients who underwent brain MRI were included, or attrition and selection bias. Use of sedatives may have affected burst signal properties and timing of burst suppression. Determination of causal effects of sedatives on burst similarity could not be determined in this retrospective analysis. Prospective studies with real-time tracking of anesthetics may help elucidate this relationship. Although only five patients underwent MRI after the fifth day after cardiac arrest, difference in MRI timing between patients limited the temporal trends analysis comparing burst similarity to MRI across consecutive time blocks. In fact, the degree of brain injury estimated from MRI data in this study may have been underestimated given potential for pseudonormalization of ADC values after 3 days from injury. Diffusion changes on MRI that are potentially reversible, such as diffusion restriction in the setting of seizure, may have confounded the measure of structural brain injury used. Regional analysis could have corroborated previous association of thalamic injury in histopathologic studies with identical bursts [17]. We only had functional recovery assessment at the time of patient discharge, and therefore evaluation of longitudinal improvement in the five study participants with CPC 3 or 4 is limited. This cohort only included patients who had both EEG and MRI performed; therefore, it is not representative of all patients with cardiac arrest undergoing multimodal prognostication in participating hospitals.
Conclusions
This study demonstrates that burst similarity is associated with the degree of brain injury severity measured with diffusion MRI after cardiac arrest and that this association is time dependent, highlighting the value of measuring early burst suppression features despite TTM and sedation use. We propose DTW as a novel metric of burst similarity with algorithmic advantages compared with the standard XCORR method; however, this approach needs further validation against XCORR and visual review in larger cohorts of patients who have sedative dosing available. Multimodal prognostication incorporating neuroimaging with quantitative EEG analysis may increase diagnostic specificity and enable early and real-time determination of burst suppression secondary to severe brain injury.
References
Meaney PA, Bobrow BJ, Mancini ME, Christenson J, de Caen AR, Bhanji F, et al. CPR Quality Summit Investigators, the American Heart Association Emergency Cardiovascular Care Committee, and the Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation. Cardiopulmonary resuscitation quality: [corrected] improving cardiac resuscitation outcomes both inside and outside the hospital: a consensus statement from the American Heart Association. Circulation. 2013;128(4):417–35.
Newman M. Latest Statistics. Sudd. Card. Arrest Found. 2022 [cited 2022 Feb 25]. Available from https://www.sca-aware.org/about-sudden-cardiac-arrest/latest-statistics
Perkins GD, Callaway CW, Haywood K, Neumar RW, Lilja G, Rowland MJ, et al. Brain injury after cardiac arrest. Lancet. 2021;398(10307):1269–78.
Greer DM, Rosenthal ES, Wu O. Neuroprognostication of hypoxic-ischaemic coma in the therapeutic hypothermia era. Nat Rev Neurol. 2014;10(4):190–203.
Sandroni C, D’Arrigo S, Cacciola S, Hoedemaekers CW, Westhall E, Kamps MJ, et al. Prediction of good neurological outcome in comatose survivors of cardiac arrest: a systematic review. Intensive Care Med. 2022;48(4):389–413.
Sandroni C, D’Arrigo S, Cacciola S, Hoedemaekers CW, Kamps MJ, Oddo M, et al. Prediction of poor neurological outcome in comatose survivors of cardiac arrest: a systematic review. Intensive Care Med. 2020;46(10):1803–51.
Panchal AR, Bartos JA, Cabañas JG, Donnino MW, Drennan IR, Hirsch KG, et al. Adult Basic and Advanced Life Support Writing Group. Part 3: Adult Basic and Advanced Life support: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020;142(162):S366–468.
Amorim E, Rittenberger JC, Zheng JJ, Westover MB, Baldwin ME, Callaway CW, et al. Post Cardiac Arrest Service. Continuous EEG monitoring enhances multimodal outcome prediction in hypoxic-ischemic brain injury. Resuscitation. 2016;109:121–6.
Hofmeijer J, Tjepkema-Cloostermans MC, van Putten MJ. Burst-suppression with identical bursts: a distinct EEG pattern with poor outcome in postanoxic coma. Clin Neurophysiol. 2014;125(5):947–54.
Barbella G, Novy J, Marques-Vidal P, Oddo M, Rossetti AO. Prognostic role of EEG identical bursts in patients after cardiac arrest: multimodal correlation. Resuscitation. 2020;148:140–4.
Sivaraju A, Gilmore EJ, Wira CR, Stevens A, Rampal N, Moeller JJ, et al. Prognostication of post-cardiac arrest coma: early clinical and electroencephalographic predictors of outcome. Intensive Care Med. 2015;41(7):1264–72.
Coppler PJ, Kusztos AE, Andreae M, Butcher BW, Doshi A, Baldwin ME, et al. University of Pittsburgh Post-Cardiac Arrest Service. Awakening from post anoxic coma with burst suppression with identical bursts. Resusc Plus. 2021;7:100151.
Peluso L, Legros B, Caroyer S, Taccone FS, Gaspard N. Falsely predictive EEG and clinical signs after post-anoxic brain injury under sevoflurane anesthesia. Clin Neurophysiol. 2021;132(5):1080–2.
Kusztos AE, Coppler PJ, Salcido DD, Callaway CW, Elmer J. Neuro-anatomical localization of EEG identical bursts in patients with and without post-anoxic myoclonus. Resuscitation. 2021;162:314–9.
Spalletti M, Carrai R, Scarpino M, Cossu C, Ammannati A, Ciapetti M, et al. Single electroencephalographic patterns as specific and time-dependent indicators of good and poor outcome after cardiac arrest. Clin Neurophysiol. 2016;127(7):2610–7.
Calabrese E, Gandhi S, Shih J, Otero M, Randazzo D, Hemphill C, et al. Parieto-occipital injury on diffusion MRI correlates with poor neurologic outcome following cardiac arrest. Am J Neuroradiol. 2023;44(3):254–60.
van Putten MJ, Jansen C, Tjepkema-Cloostermans MC, Beernink TM, Koot R, Bosch F, et al. Postmortem histopathology of electroencephalography and evoked potentials in postanoxic coma. Resuscitation. 2019;134:26–32.
Westover MB, Ching S, Shafi MM, Cash SS, Brown EN. Real-time segmentation and tracking of brain metabolic state in ICU EEG recordings of burst suppression. In: Annual international conference of the IEEE engineering in medicine and biology society. 2013;2013:7108–11
An J, Jonnalagadda D, Moura V, Purdon PL, Brown EN, Westover MB. Spatial variation in automated burst suppression detection in pharmacologically induced coma. In: Annual international conference of the IEEE engineering in medicine and biology society. 2015;2015:7430–3.
Rakthanmanon T, Campana B, Mueen A, Batista G, Westover B, Zhu Q, et al. Searching and mining trillions of time series subsequences under dynamic time warping. In: Proceedings of the 18th ACM SIGKDD international conference on knowledge discovery and data mining—KDD 12. Beijing, China: ACM Press; 2012. p. 262. [cited 2022 Feb 25], Available from http://dl.acm.org/citation.cfm?d=2339530.2339576
Sakoe H, Chiba S. Dynamic programming algorithm optimization for spoken word recognition. IEEE Trans Acoust Speech Signal Process. 1978;26(1):43–9.
Bevers MB, Scirica BM, Avery KR, Henderson GV, Lin AP, Lee JW. Combination of clinical exam, MRI and EEG to predict outcome following cardiac arrest and targeted temperature management. Neurocrit Care. 2018;29(3):396–403.
van Putten MJ, van Putten MH. Uncommon EEG burst-suppression in severe postanoxic encephalopathy. Clin Neurophysiol. 2010;121(8):1213–9.
Keijzer HM, Verhulst MM, Meijer FJ, Tonino BA, Bosch FH, Klijn CJ, et al. Prognosis after cardiac arrest: the additional value of DWI and FLAIR to EEG. Neurocrit Care. 2022;37(1):302–13.
Ruijter BJ, van Putten MJ, van den Bergh WM, Tromp SC, Hofmeijer J. Propofol does not affect the reliability of early EEG for outcome prediction of comatose patients after cardiac arrest. Clin Neurophysiol. 2019;130(8):1263–70.
Hofmeijer J, Beernink TM, Bosch FH, Beishuizen A, Tjepkema-Cloostermans MC, van Putten MJ. Early EEG contributes to multimodal outcome prediction of postanoxic coma. Neurology. 2015;85(2):137–43.
Amorim E, Zheng WL, Jing J, Ghassemi MM, Lee JW, Wu O, et al. Neurophysiology state dynamics underlying acute neurologic recovery after cardiac arrest. Neurology. 2023;101(9):e940–52.
Elmer J, Gianakas JJ, Rittenberger JC, Baldwin ME, Faro J, Plummer C, et al. Pittsburgh Post-Cardiac Arrest Service. Group-based trajectory modeling of suppression ratio after cardiac arrest. Neurocrit Care. 2016;25(3):415–23.
Elmer J, Coppler PJ, Solanki P, Westover MB, Struck AF, Baldwin ME, et al. Sensitivity of continuous electroencephalography to detect ictal activity after cardiac arrest. JAMA Netw Open. 2020;3(4): e203751.
Ruijter BJ, Hofmeijer J, Tjepkema-Cloostermans MC, van Putten MJ. The prognostic value of discontinuous EEG patterns in postanoxic coma. Clin Neurophysiol. 2018;129(8):1534–43.
Sekar K, Schiff ND, Labar D, Forgacs PB. Spectral content of electroencephalographic burst-suppression patterns may reflect neuronal recovery in comatose post-cardiac arrest patients. J Clin Neurophysiol. 2019;36(2):119–26.
Acknowledgements
The authors would like to thank the Critical Care EEG Monitoring Consortium members for constructive feedback.
Funding
This study was supported by the NIH (1K23NS119794), Weil-Society of Critical Care Medicine Research Grant, Neurocritical Care Society (NCS research training fellowship), American Heart Association (postdoctoral fellowship, 20CDA35310297, and Amos Medical Faculty Development Award), MIT-Philips Alliance (Clinician Award), Harvard College Research Program, and the Harvard College Program for Research in Science and Engineering.
Author information
Authors and Affiliations
Contributions
SS: Conceptualization, Methodology, Software, Validation, Formal Analysis, Investigation, Writing—Original Draft, Writing—Review and Editing, Visualization. TZ: Conceptualization, Methodology, Software, Formal Analysis, Investigation, Writing—Review and Editing. ADP: Methodology, Software, Formal Analysis, Investigation, Writing—Review and Editing. W-LZ: Data curation, Methodology, Software, Formal Analysis, Visualization, Supervision, Writing—Review and Editing. PK: Investigation, Data curation, Writing—Review and Editing. EP: Investigation, Data curation, Writing—Review and Editing. SS: Investigation, Writing—Review and Editing. MB: Investigation, Formal Analysis, Data Curation, Writing—Review and Editing. U-MO: Conceptualization, Methodology, Resources, Writing—Review and Editing. JWL: Investigation, Data Curation, Writing—Review and Editing. MBW: Conceptualization, Methodology, Resources, Data Curation, Writing—Review and Editing, Supervision, Project administration, Funding acquisition. EA: Conceptualization, Methodology, Software, Validation, Investigation, Data Curation, Writing—Original Draft, Writing—Review and Editing, Visualization, Supervision, Project administration, Funding acquisition. The authors approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Shawn Shivdat was supported during this research by the Harvard College Research Program and the Harvard College Program for Research in Science and Engineering. These funding agencies did not play a role in the study design, data collection, analysis, writing, or decision to submit this work. Shawn is the co-founder of Somn. Somn did not contribute funding and played no role in the study. Dr. Amorim was supported during this research by the NIH (1K23NS119794), Hellman Fellows Fund, Regents of the University of California (Resource Allocation Program), CURE Epilepsy Foundation (Taking Flight Award), Weil-Society of Critical Care Medicine Research Grant, Neurocritical Care Society (NCS research training fellowship), Zoll Foundation Grant, American Heart Association (postdoctoral fellowship and 20CDA35310297, and Amos Medical Faculty Development Award), and MIT-Philips Alliance (Clinician Award). These funding agencies did not play a role in the study design, data collection, analysis, writing, or decision to submit this work. Dr. Bevers was supported during this research by the NIH (K23NS112474) the American Academy of Neurology (Clinical Research Training Scholarship) and the David Heitman Neurovascular Research Fund. These funding agencies did not play a role in the study design, data collection, analysis, writing, or decision to submit this work. Dr. Lee was supported during this research by the Epilepsy Foundation and the NIH (R01N062092 and UH3HL145269) and UCB/Parexel. Dr. Lee served as a consultant for SK Biopharmaceuticals, performed contract work for Bioserenity and Teladoc, and is the co-founder and scientific advisor for Soterya, Inc. Soterya Inc. did not contribute funding nor played any role in the study. Dr. Westover was supported by Grants from the NIH (R01NS102190, R01NS102574, R01NS107291, RF1AG064312, RF1NS120947, R01AG073410, R01HL161253, R01NS126282, R01AG073598), and NSF (2014431). These funding agencies did not play a role in the study design, data collection, analysis, writing, or decision to submit this work. Dr. Westover is a co-founder of Beacon Biosignals, and Director for Data Science for the McCance Center for Brain Health. Beacon Biosignals did not contribute funding and played no role in the study.
Ethical Approval/Informed Consent
This article follows ethical guidelines and institutional review board approval was approved with a waiver of informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shivdat, S., Zhan, T., De Palma, A. et al. Early Burst Suppression Similarity Association with Structural Brain Injury Severity on MRI After Cardiac Arrest. Neurocrit Care (2024). https://doi.org/10.1007/s12028-024-02047-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12028-024-02047-6