Abstract
Background
Existing studies of quantitative electroencephalography (qEEG) as a prognostic tool after cardiac arrest (CA) use methods that ignore the longitudinal pattern of qEEG data, resulting in significant information loss and precluding analysis of clinically important temporal trends. We tested the utility of group-based trajectory modeling (GBTM) for qEEG classification, focusing on the specific example of suppression ratio (SR).
Methods
We included comatose CA patients hospitalized from April 2010 to October 2014, excluding CA from trauma or neurological catastrophe. We used Persyst®v12 to generate SR trends and used semi-quantitative methods to choose appropriate sampling and averaging strategies. We used GBTM to partition SR data into different trajectories and regression associate trajectories with outcome. We derived a multivariate logistic model using clinical variables without qEEG to predict survival, then added trajectories and/or non-longitudinal SR estimates, and assessed changes in model performance.
Results
Overall, 289 CA patients had ≥36 h of EEG yielding 10,404 h of data (mean age 57 years, 81 % arrested out-of-hospital, 33 % shockable rhythms, 31 % overall survival, 17 % discharged to home or acute rehabilitation). We identified 4 distinct SR trajectories associated with survival (62, 26, 12, and 0 %, P < 0.0001 across groups) and CPC (35, 10, 4, and 0 %, P < 0.0001 across groups). Adding trajectories significantly improved model performance compared to adding non-longitudinal data.
Conclusions
Longitudinal analysis of continuous qEEG data using GBTM provides more predictive information than analysis of qEEG at single time-points after CA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The majority of patients hospitalized after sudden cardiac arrest (CA) are comatose [1, 2]. Seizures or other “malignant” electroencephalographic (EEG) patterns develop commonly in these patients and are associated with worse neurological outcomes [3–8]. EEG interpretation can be qualitative (e.g., “diffuse slowing with periods of attenuation”) or quantitative (e.g., spectral power or suppression ratio (SR)). Theoretical advantages to quantitative EEG analysis (qEEG) are reduced subjectivity and inter-observer variability, and the ability to detect subtle changes that may be imperceptible to the human eye [9]. Several qEEG metrics are associated with clinical outcomes after CA, including amplitude-integrated EEG [10, 11], SR [12–14], and bispectral index [13, 14]. Multiple qEEG metrics may be combined into composite prognostic tools [15].
Previous studies of qEEG after CA have not accounted for the correlated, longitudinal nature of EEG data or dynamic evolution over time. Many report average qEEG measures within a given epoch, generally at baseline and fixed intervals thereafter. This results in significant information loss. This compression of continuous qEEG data is a specific example of a general problem for modern biomedical research: physiological variables are continuously recorded for extended durations with high time resolution, but not analyzed as such. Unfortunately, optimal analytical methods to approach intensively sampled longitudinal data in critically ill populations are not well established.
We sought to investigate longitudinal techniques for analysis of high-resolution time-series qEEG data and identify rational parameters for temporal and spatial averaging that minimize information loss. Group-based trajectory modeling (GBTM) is a specialized application of finite mixture modeling that determines trends in longitudinal data by identifying clusters of individuals with similar data evolution (trajectory) over time [16]. This approach leverages the power of repeated sampling.
We tested the utility of GBTM for qEEG analysis after CA, using the specific example of SR for methodological development. We hypothesized that GBTM could define distinct trajectories of SR that were associated with functional outcome at hospital discharge. Secondarily, we hypothesized that SR trajectory group membership would be an independent predictor of outcome and significantly improve prediction above and beyond non-longitudinal summary estimates of SR.
Methods
In this study, we aimed to (1) test whether global brain SR can be calculated from SR in individual EEG leads; (2) identify the optimal epoch length for comparing temporal trends in SR; (3) define prognostic SR trajectories that predict patient outcome; (4) test the minimum length of observation necessary to determine an SR trajectory; and (5) determine whether incremental information is gained when SR trajectories are added to a multivariable prognostic model using clinical variables to predict outcome.
Patients and Setting
The University of Pittsburgh Institutional Review Board approved this study. We performed an observational cohort study of consecutive patients hospitalized at a single academic center from April 2010 to October 2014 with ≥6 h of EEG monitoring. We maintain a registry of all patients treated by our Post-Cardiac Arrest Service including demographic and disease-specific baseline characteristics, treatments, and outcomes. Our local standard of care is to monitor all comatose survivors of CA with continuous EEG [17], and during the study period we cooled all comatose post-CA patients to 33 °C for 24 h, regardless of initial rhythm or arrest location. We excluded patients from this analysis for arrest from trauma, exsanguination, or catastrophic neurological event (arrest secondary to subarachnoid hemorrhage, stroke, or status epilepticus), and those who died or were transitioned to comfort measures only within 6 h of presentation.
EEG Acquisition and Processing
Our hospital has in-house EEG technologist coverage around-the-clock. EEG recordings generally started upon ICU arrival, an average of 6–8 h after return of spontaneous circulation (ROSC). We applied 22 gold-plated cup electrodes to the scalp in the standard 10–20 International System of Electrode Placement and recorded data using XLTech Natus® Neuroworks digital video/EEG systems (Natus Medical, Pleasanton, CA). Clinical care, including antiepileptic and sedation management, was performed by the treating clinician according to standardized protocols (Supplemental Appendix 1). We continued EEG monitoring until awakening, death, or approximately 48 h of recording without any actionable findings. It is our institutional protocol to stimulate patients sequentially using photic, auditory, and tactile stimuli at the initiation of EEG monitoring. We included data derived during this stimulation period in the present analysis.
We generated qEEG metrics using Persyst® v12 (Persyst Development Co., Prescott, AZ) using standard processing engines. For SR, the software divides each lead’s data into 10-s epochs and calculates the total duration that epoch is “suppressed” (defined as a ≥0.5 s <3μV amplitude, the default threshold values in Persyst v12). The software calculates a 60-s running average to yield each channel’s SR. We used Persyst’s standard algorithm for artifact reduction (blind source separation) and exported qEEG trends in 1-s epochs. We then combined these trends with patients’ baseline and outcomes data in a relational database using SQLServer®2014 (Microsoft, Redmond, WA).
Signal Sampling and Averaging
First, we determined whether important information was lost by averaging SR over the entire skull. Initial qEEG processing resulted second-by-second SR values for each channel in each patient. There is no theoretical limitation to the number of points that can be modeled using GBTM, but inclusion of non-informative data results in computationally intensive models that perform no better than more parsimonious models, and may perform worse if included data have a poor signal-to-noise ratio. By contrast, excessive down sampling leads to loss of information and statistical power.
Our clinical observation is that SR is highly spatially correlated across individual EEG channels and cerebral hemispheres. Thus, averaging hemispheric or whole-brain SR would result in little information loss and could improve signal-to-noise ratio by averaging out artifact from signal EEG leads. To test this, we selected a random sample of ten patients and analyzed 75,000 SR data points. We calculated the correlation coefficient between left and right hemispheres to determine whether data from a single hemisphere was representative of whole-brain SR. Next, we calculated all possible pairwise correlation coefficients between EEG channels to determine the range of correlations between leads. Finally, we used a generalized linear model with nested random effects to estimate the variance components for lead, observation, and random error (SPSS v22.0, IBM Corp, Armonk, NY). These were used to calculate the within-observation intraclass correlation coefficient (ICC) (i.e., the proportion of total variance accounted for by lead-to-lead variance).
Second, we hypothesized that clinically relevant changes in SR would occur over hours rather than seconds or minutes. Moreover, in patients with discontinuous backgrounds, large fluctuations in SR may reflect the intermittent EEG background activity rather than meaningful temporal evolution. To estimate the optimal duration for SR averaging, after developing our GBTM (see below), we repeated GBTM procedures varying epoch length (10 and 30 s; 1, 2, 5, 10, and 30 min; 1, 2, 4, and 6 h) and inspected the resultant trajectories for stability. We also compared the incremental change in Bayesian information criteria (BIC) after adjustment for the number of samples per trajectory and computational intensity between these models to identify an inflection point that balanced parsimony and information loss.
Third, we determined the minimum duration of observation necessary to accurately assign SR trajectories. GBTM requires that all trajectories be the same duration, so data from subjects with varying durations of monitoring could not be combined into a single model without censoring data at the shortest duration of observation. In our cohort, approximately one-third of subjects were monitored at least 48 h. We performed GBTM (see below) in this subgroup using 48 h of observation, then repeated GBTM procedures iteratively censoring the data at 42, 36, 30, 24, 18, and 12 h. Using the 48-h trajectories as a “gold standard,” we calculated percent misclassification for the censored data and plotted this and potential sample size against duration of observation.
Based on the results of these analyses (see Results), in our final GBTM models we used 36-h observations of median hemispheric SR evaluated in consecutive 1-h epochs.
Predictors, Covariates, and Outcomes
Our fourth step was to examine trajectory group membership from GBTM as a predictor of neurological outcome at hospital discharge in regression modeling. As non-longitudinal alternative representations of SR, we used median SR at baseline (0–1 h) and day one (24–25 h) treated as a continuous predictors. Baseline SR measurements included data obtained during patient stimulation at EEG initiation.
We abstracted demographic and basic patient information from our registry, including patient age, gender, location of arrest (out-of-hospital versus in-hospital), presenting rhythm (ventricular tachycardia or fibrillation (VT/VF) versus pulseless electrical activity (PEA) or asystole), Charlson comorbidity index (CCI), and Pittsburgh CA Category (PCAC). The PCAC is a validated clinical prediction tool that stratifies CA survivors by risk of in-hospital death or neurological deterioration based on neurological examination and cardiopulmonary dysfunction in the first 6 h after ROSC [18]. The tool stratifies survivors of CA into four categories that are strongly predictive of survival and functional outcome. PCAC I patients are by definition awake, and therefore excluded. Other standard CA covariates are collapse to cardiopulmonary resuscitation (CPR) and CPR to ROSC intervals, witnessed collapse, bystander-administered CPR resuscitation, and use of hypothermia. We have previously demonstrated arrest intervals [19], witnessed collapse, and bystander CPR [20], to be unreliable reported in our care system, and so we did not include them in our models. Temperature management during the study period was standardized across all eligible subjects (Supplemental Fig. 3), excluding this as a covariate. Finally, we collected sedative and antiepileptic medication data, which we further stratified by observation period (0–17 and 18–36 h).
Our primary outcome of interest was survival to hospital discharge, and our secondary outcome was functionally favorable survival, defined as discharge to home or acute rehabilitation.
Statistical Methods
We used descriptive statistics to summarize baseline population characteristics and outcomes. We used GBTM with a censored normal distribution, and used Bayesian and Akaike information criteria (BIC and AIC) for GBTM model selection. To test the incremental value of including SR trajectory group membership, we constructed a series of adjusted logistic regression models. First, we developed a saturated “Clinical Model” including all potential baseline predictors of outcome except for EEG data. We included baseline predictors in this model regardless of their unadjusted association with outcome since our goal was to explain the maximum amount of variability in outcome possible without EEG data, rather than determining independent predictors of outcome. We then challenged this model to assess performance improvement by sequential addition of non-longitudinal SR (baseline and day 1 medians) and trajectory group membership. Given the low incidence of favorable outcomes in certain trajectory groups, we used Firth’s penalized likelihood approach to minimize bias in coefficient estimates.
We used several complementary methods to compare performances of the Clinical Model and models incorporating SR metrics. To compare models, we calculated C-statistics for each model and compared these values and AICs between models. We also calculated the net reclassification improvement (NRI) between models using in-hospital mortality cutoffs of 15, 30, and 45 %, and 5, 50, and 95 % [21]. We used SAS v9.3 (SAS Institute, Cary NC).
Results
Cohort Composition
During the study period, 1012 CA patients were treated, and 451 (45 %) of these met both inclusion and exclusion criteria (Fig. 1). In total, 37,447 h of EEG data were obtained and analyzed (mean 83 h/patient), and 289 patients had ≥36 h of EEG data. Mean age was 58 years, 351 (78 %) arrested out-of-hospital, and 132 (34 %) had a shockable rhythm (Table 1). Survival to discharge was 30 and 16 % had functionally favorable survival.
Signal Sampling and Averaging
Calculating SR by EEG channel using a longitudinal bipolar montage resulted in approximately 2.16 × 108 data points (average 478,000 points/patient). Left and right hemisphere SRs were near-perfectly correlated (Pearson’s R = 0.98). In all possible pairwise comparisons of SR across bipolar channels, median correlation coefficient was 0.87 (IQR 0.83–0.92, all Ps for pairwise correlations <0.0001). The ICC for SR was 0.85, indicating a strong correlation between simultaneously measured SR in across leads. Since signal quality in individual leads is may be degraded by noise or artifact, falsely reducing SR, we chose to analyze average SR averaged across a single cerebral hemisphere.
Overall, 186 subjects had ≥48 h of EEG data. Using this 48-h cohort and iteratively censoring data input into GBTM, we were able to calculate the rate of trajectory group misclassification using these censored data compared to the full model. Inspecting the plot of percent misclassification and sample size versus trajectory length (Supplemental Appendix Fig. 1a), we selected 36-h trajectories for subsequent analyses and final modeling, yielding a cohort of 289 patients.
When we repeated GBTM modeling using varying epoch lengths, we found good stability of trajectories across models (Supplemental Appendix Fig. 2). Models using more than 25,000 data points (10-min epochs or shorter) failed to converge. Comparing adjusted BICs and computational intensity across these models supported the use of either 40- or 60-min epochs (Supplemental Appendix Fig. 1b). Consequently, we chose to use 60-min epochs for subsequent analyses and final modeling.
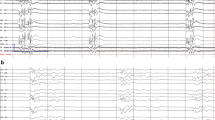
Trajectory Modeling
Using these sampling strategies and GBTM, a 4-Group trajectory model best fit the data (Fig. 2). Both survival and favorable neurological outcomes decreased by approximately 50 % across increasing trajectory groups, then fell to near 0 for trajectory Group 4 (Table 2).
Comparison of Prognostic Models
The best performing prognostic model included clinical predictors, baseline SR and trajectory group membership (Table 3). Adding baseline SR and trajectory group membership individually or in combination to the base clinical model improved discriminatory power (Supplemental Table 1). Adding baseline SR and trajectory group membership individually and in combination also resulted in significantly improved NRI (P < 0.0001 for all three comparisons).
Discussion
We present results from a large cohort study of EEG after cardiac arrest, and the first to use longitudinal methods to analyze these data. We set forth a methodological framework to analyze these intensively sampled, time-series data. Using GBTM to describe the evolution of SR over time, we identified four strongly prognostic trajectories that describe these data. Incorporating these trajectories into prognostic modeling significantly improves the discriminatory power of these models to predict outcome compared to models that use only clinical and non-longitudinal EEG data.
Our results are consistent with, and expand upon, work recently published by Oh et al., who report the association of time-to-normalization of single-channel amplitude-integrated EEG (aEEG) after CA with outcome [22]. Consistent with Oh’s results, we find that qEEG in the first 36 h after CA identifies a subpopulation of patients with uniformly poor outcomes. Oh et al. describe their reliance on a single EEG channel as a potential limitation, and others have called for validation of simplified EEG montages before widespread use [23]. To our knowledge, our work is the first to support this strategy. The degree of spatial correlation we demonstrate between individual EEG leads in this population demonstrates that simplified montages are unlikely to result in information loss about SR, although other qEEG measures may differ. This lack of spatial heterogeneity between hemispheres may be a reflection of the relatively diffuse brain injury, in contrast to the more focal lesions found after cerebrovascular accident or brain trauma. Similarly, the lack of other regional variation in spectral power, for example between frontal and occipital regions, may reflect a relatively static (over the 36-h observation period we selected) and diffuse post-anoxic cortical network failure in contrast to that observed in focal brain trauma or in response to sedation [24].
Currently, guidelines recommend delaying neurological prognostication for at least 72 h after CA because, prior to this time, no clinical sign, test, or combination of findings short of progression to brain death preclude a favorable outcome [25–32]. Our work strengthens the assertion that qEEG, in combination with clinical findings, might shorten the time to accurate neurological prognostication. While patients following trajectory Group 4 had no favorable outcomes, the 95 % confidence interval for our point estimate was 0–6 %. Withdrawal of life-sustaining therapy is uniformly fatal in this population, so new methods must be thoroughly evaluated to prevent avoidable mortality resulting from inaccurate prognostication and subsequent withdrawal. EEG and qEEG are two of multiple modalities available to inform accurate prognostication, and SR is just one quantitative metric that can be derived from the complex and information-rich EEG signal. Further work is also needed to elucidate which of many qEEG metrics are the most informative, alone or in combination, for prognostication. Before consideration of prognostication earlier than 72 h after CA, our results must be replicated by others to establish external validity and narrow confidence intervals around the final point estimate of outcome. To avoid self-fulfilling prophecies, this validation should be prospective, and carried out in a cohort of patients who are consistently monitored for at least 36 h without exposure to withdrawal of life-sustaining therapy based on perceived neurological prognosis.
Our findings also suggest the significance of baseline EEG suppression after CA may be limited. Most of our subjects fell into trajectories with baseline SR above 50 %. Although baseline SR was associated with outcome, improvement in SR over the first 36 h portended significantly better outcomes than persistent suppression. This is consistent with non-quantitative analyses by from Cloostermans et al. [5], which demonstrate favorable outcomes in some patients with early burst suppression that resolves over 18–24 h. The reason for this phenomenon remains unclear. EEG activity may be suppressed by early, reversible neurological injury from ischemia and reperfusion, sedation, hypothermia, or a combination of these factors. We note, for example, that the dynamic periods in temperature trajectories corresponding to rewarming (Supplemental Fig. 3) coincide with the epochs of maximum change in SR trajectories. SR can also be affected by metabolic confounders such as evolving renal function, malignant EEG patterns such as seizures, sedation, and antiepileptic therapy (Supplemental Table 2), and cerebral hypoperfusion. GBTM is not well suited in its current stage of development to explore these potentially important covariates in robust adjusted analyses. Future longitudinal analyses may address the effects of concurrent potential confounders.
The ability to rapidly and accurately identify patients at high risk of future neurological deterioration or death has clear importance for clinical research, particularly interventional trials. Our findings suggest that qEEG evolution over time can improve risk stratification in this population, as previously proposed by Friberg et al. [23]. Such analysis holds the promise of allowing targeted therapies to be initiated for selected patients in response to real-time EEG changes or titrated based on dynamic EEG responsive to therapy. For example, energy supply–demand mismatch resulting from cerebral hypoperfusion leads ultimately to energetic failure, loss of membrane potential, and suppression of electrical activity (i.e., increased SR) [33–35]. If prolonged or severe, this can result in neuronal apoptosis and/or necrosis and ultimately irrecoverable injury. Thus, increased SR might provide an actionable warning of early energy imbalance that could be corrected before irreversible damage occurs. This type of EEG-guided titration of care is somewhat akin to titrating vasoactive medications in response to continuous measures of arterial pressure and end-organ perfusion, rather than infrequent, discrete blood pressure measurements. Such a concept merits future investigation.
Our study has several limitations. Our primary outcome of interest was neurological outcome at hospital discharge, which can be confounded by withdrawal of life-sustaining therapy based on anticipated prognosis. Care limitations create the risk of self-fulfilling prophecies, whereby qEEG characteristics such as high SR might prompt clinicians to limit life-sustaining therapy, inadvertently increasing mortality in those subjects who follow a trajectory of prolonged EEG suppression. We note that median length of stay did not differ across trajectory groups, suggesting that life-sustaining therapy was not systematically withdrawn earlier in patients following specific trajectories of SR, nor did the proportion of subjects exposed to withdrawal for neurological prognosis differ across trajectories. Second, since GBTM requires equal length observations across subjects, we excluded subjects with <36 h of data available from our final analyses. This may limit the generalizability of our findings to the broader post-CA patient population. However, baseline characteristics did not differ between the entire cohort and those with >36 h of data, suggesting against biased sampling. The single-center design of our study limits generalizability. We established hospital-wide care protocols including routine use of targeted temperature management, continuous EEG, aggressive seizure control, and best-practice critical care [17]. This decreased variability in care improves the internal validity of our study, but our results must be replicated in other care systems.
In conclusion, we have described a methodological framework to analyze intensively sampled, time-series qEEG data and demonstrated the value added by using GBTM to model SR after CA. We identified strongly prognostic SR trajectories, which if validated could substantially shorten the time to accurate neurological prognostication, be used to enroll high-risk subjects in clinical research or identify dynamic treatment responsiveness. More broadly, these methods leverage the power of high-resolution data and are likely to be increasingly utilized in biomedical research.
References
Coppler PJ, Elmer J, Calderon L, Sabedra A, Doshi AA, Callaway CW, et al. Validation of the Pittsburgh Cardiac Arrest Category illness severity score. Resuscitation. 2015. doi:10.1016/j.resuscitation.2015.01.020.
Laver S, Farrow C, Turner D, Nolan J. Mode of death after admission to an intensive care unit following cardiac arrest. Intensive Care Med. 2004;30(11):2126–8. doi:10.1007/s00134-004-2425-z.
Rittenberger JC, Popescu A, Brenner RP, Guyette FX, Callaway CW. Frequency and timing of nonconvulsive status epilepticus in comatose post-cardiac arrest subjects treated with hypothermia. Neurocrit Care. 2012;16(1):114–22. doi:10.1007/s12028-011-9565-0.
Rossetti AO, Carrera E, Oddo M. Early EEG correlates of neuronal injury after brain anoxia. Neurology. 2012;78(11):796–802. doi:10.1212/WNL.0b013e318249f6bb.
Cloostermans MC, van Meulen FB, Eertman CJ, Hom HW, van Putten MJ. Continuous electroencephalography monitoring for early prediction of neurological outcome in postanoxic patients after cardiac arrest: a prospective cohort study. Crit Care Med. 2012;40(10):2867–75. doi:10.1097/CCM.0b013e31825b94f0.
Crepeau AZ, Rabinstein AA, Fugate JE, Mandrekar J, Wijdicks EF, White RD, et al. Continuous EEG in therapeutic hypothermia after cardiac arrest: prognostic and clinical value. Neurology. 2013;80(4):339–44. doi:10.1212/WNL.0b013e31827f089d.
Mani R, Schmitt SE, Mazer M, Putt ME, Gaieski DF. The frequency and timing of epileptiform activity on continuous electroencephalogram in comatose post-cardiac arrest syndrome patients treated with therapeutic hypothermia. Resuscitation. 2012;83(7):840–7. doi:10.1016/j.resuscitation.2012.02.015.
Rossetti AO, Urbano LA, Delodder F, Kaplan PW, Oddo M. Prognostic value of continuous EEG monitoring during therapeutic hypothermia after cardiac arrest. Crit Care. 2010;14(5):R173. doi:10.1186/cc9276.
Foreman B, Claassen J. Quantitative EEG for the detection of brain ischemia. Crit Care. 2012;16(2):216. doi:10.1186/cc11230.
Rundgren M, Westhall E, Cronberg T, Rosen I, Friberg H. Continuous amplitude-integrated electroencephalogram predicts outcome in hypothermia-treated cardiac arrest patients. Crit Care Med. 2010;38(9):1838–44. doi:10.1097/CCM.0b013e3181eaa1e7.
Oh SH, Park KN, Kim YM, Kim HJ, Youn CS, Kim SH, et al. The prognostic value of continuous amplitude-integrated electroencephalogram applied immediately after return of spontaneous circulation in therapeutic hypothermia-treated cardiac arrest patients. Resuscitation. 2013;84(2):200–5. doi:10.1016/j.resuscitation.2012.09.031.
Wennervirta JE, Ermes MJ, Tiainen SM, Salmi TK, Hynninen MS, Sarkela MO, et al. Hypothermia-treated cardiac arrest patients with good neurological outcome differ early in quantitative variables of EEG suppression and epileptiform activity. Crit Care Med. 2009;37(8):2427–35. doi:10.1097/CCM.0b013e3181a0ff84.
Seder DB, Fraser GL, Robbins T, Libby L, Riker RR. The bispectral index and suppression ratio are very early predictors of neurological outcome during therapeutic hypothermia after cardiac arrest. Intensiv Care Med. 2010;36(2):281–8. doi:10.1007/s00134-009-1691-1.
Selig C, Riegger C, Dirks B, Pawlik M, Seyfried T, Klingler W. Bispectral index (BIS) and suppression ratio (SR) as an early predictor of unfavourable neurological outcome after cardiac arrest. Resuscitation. 2014;85(2):221–6. doi:10.1016/j.resuscitation.2013.11.008.
Tjepkema-Cloostermans MC, van Meulen FB, Meinsma G, van Putten MJ. A Cerebral Recovery Index (CRI) for early prognosis in patients after cardiac arrest. Crit Care. 2013;17(5):R252. doi:10.1186/cc13078.
Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annu Rev Clin Psychol. 2010;6:109–38. doi:10.1146/annurev.clinpsy.121208.131413.
Rittenberger JC, Guyette FX, Tisherman SA, DeVita MA, Alvarez RJ, Callaway CW. Outcomes of a hospital-wide plan to improve care of comatose survivors of cardiac arrest. Resuscitation. 2008;79(2):198–204. doi:10.1016/j.resuscitation.2008.08.014.
Rittenberger JC, Tisherman SA, Holm MB, Guyette FX, Callaway CW. An early, novel illness severity score to predict outcome after cardiac arrest. Resuscitation. 2011;82(11):1399–404. doi:10.1016/j.resuscitation.2011.06.024.
Frisch A, Reynolds JC, Condle J, Gruen D, Callaway CW. Documentation discrepancies of time-dependent critical events in out of hospital cardiac arrest. Resuscitation. 2014;85(8):1111–4. doi:10.1016/j.resuscitation.2014.05.002.
Rittenberger JC, Martin JR, Kelly LJ, Roth RN, Hostler D, Callaway CW. Inter-rater reliability for witnessed collapse and presence of bystander CPR. Resuscitation. 2006;70(3):410–5. doi:10.1016/j.resuscitation.2005.12.015.
Pencina MJ, D’Agostino RB Sr, D’Agostino RB Jr, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27(2):157–72. doi:10.1002/sim.2929 discussion 207–12.
Oh SH, Park KN, Shon YM, Kim YM, Kim HJ, Youn CS, et al. Continuous amplitude-integrated electroencephalographic monitoring is a useful prognostic tool for hypothermia-treated cardiac arrest patients. Circulation. 2015. doi:10.1161/CIRCULATIONAHA.115.015754.
Friberg H, Westhall E, Rosen I, Rundgren M, Nielsen N, Cronberg T. Clinical review: continuous and simplified electroencephalography to monitor brain recovery after cardiac arrest. Crit Care. 2013;17(4):233. doi:10.1186/cc12699.
Chennu S, O’Connor S, Adapa R, Menon DK, Bekinschtein TA. brain connectivity dissociates responsiveness from drug exposure during propofol-induced transitions of consciousness. PLoS Comput Biol. 2016;12(1):e1004669. doi:10.1371/journal.pcbi.1004669.
Kamps MJ, Horn J, Oddo M, Fugate JE, Storm C, Cronberg T, et al. Prognostication of neurologic outcome in cardiac arrest patients after mild therapeutic hypothermia: a meta-analysis of the current literature. Intensiv Care Med. 2013;39(10):1671–82. doi:10.1007/s00134-013-3004-y.
Bouwes A, Binnekade JM, Kuiper MA, Bosch FH, Zandstra DF, Toornvliet AC, et al. Prognosis of coma after therapeutic hypothermia: a prospective cohort study. Ann Neurol. 2012;71(2):206–12. doi:10.1002/ana.22632.
Rossetti AO, Koenig MA. Prognostication after cardiac arrest: a tale of timing, confounders, and self-fulfillment. Neurology. 2011;77(14):1324–5. doi:10.1212/WNL.0b013e318231533b.
Cronberg T, Horn J, Kuiper MA, Friberg H, Nielsen N. A structured approach to neurologic prognostication in clinical cardiac arrest trials. Scand J Trauma Resusc Emerg Med. 2013;21:45. doi:10.1186/1757-7241-21-45.
Cronberg T, Brizzi M, Liedholm LJ, Rosen I, Rubertsson S, Rylander C, et al. Neurological prognostication after cardiac arrest–recommendations from the Swedish Resuscitation Council. Resuscitation. 2013;84(7):867–72. doi:10.1016/j.resuscitation.2013.01.019.
Wijdicks EF, Hijdra A, Young GB, Bassetti CL, Wiebe S. Quality Standards Subcommittee of the American Academy of N. Practice parameter: prediction of outcome in comatose survivors after cardiopulmonary resuscitation (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2006;67(2):203–10. doi:10.1212/01.wnl.0000227183.21314.cd.
Sandroni C, Cariou A, Cavallaro F, Cronberg T, Friberg H, Hoedemaekers C, et al. Prognostication in comatose survivors of cardiac arrest: an advisory statement from the European Resuscitation Council and the European Society of Intensive Care Medicine. Resuscitation. 2014;85(12):1779–89. doi:10.1016/j.resuscitation.2014.08.011.
Golan E, Barrett K, Alali AS, Duggal A, Jichici D, Pinto R, et al. Predicting neurologic outcome after targeted temperature management for cardiac arrest: systematic review and meta-analysis. Crit Care Med. 2014;42(8):1919–30. doi:10.1097/CCM.0000000000000335.
Hofmeijer J, Tjepkema-Cloostermans MC, van Putten MJ. Burst-suppression with identical bursts: a distinct EEG pattern with poor outcome in postanoxic coma. Clin Neurophysiol. 2014;125(5):947–54. doi:10.1016/j.clinph.2013.10.017.
Niedermeyer E, Sherman DL, Geocadin RJ, Hansen HC, Hanley DF. The burst-suppression electroencephalogram. Clin Electroencephalogr. 1999;30(3):99–105.
Thomke F, Brand A, Weilemann SL. The temporal dynamics of postanoxic burst-suppression EEG. J Clin Neurophysiol. 2002;19(1):24–31.
Acknowledgments
Dr. Elmer’s research time was supported by NIH Grant 5K12HL109068.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts of interest to report.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Elmer, J., Gianakas, J.J., Rittenberger, J.C. et al. Group-Based Trajectory Modeling of Suppression Ratio After Cardiac Arrest. Neurocrit Care 25, 415–423 (2016). https://doi.org/10.1007/s12028-016-0263-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-016-0263-9