Abstract
Extracorporeal membrane oxygenation is a potentially lifesaving intervention for children with severe cardiac or respiratory failure. It is used with increasing frequency and in increasingly more complex and severe diseases. Neurological injuries are important causes of morbidity and mortality in children treated with extracorporeal membrane oxygenation and include ischemic stroke, intracranial hemorrhage, hypoxic-ischemic injury, and seizures. In this review, we discuss the epidemiology and pathophysiology of neurological injury in patients supported with extracorporeal membrane oxygenation, and we review the current state of knowledge for available modalities of monitoring neurological function in these children. These include structural imaging with computed tomography and ultrasound, cerebral blood flow monitoring with near-infrared spectroscopy and transcranial Doppler ultrasound, and physiological monitoring with electroencephalography and plasma biomarkers. We highlight areas of need and emerging advances that will improve our understanding of neurological injury related to extracorporeal membrane oxygenation and help to reduce the burden of neurological sequelae in these children.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Extracorporeal membrane oxygenation (ECMO) is a form of extracorporeal life support that is used to treat patients with severe cardiac or pulmonary failure refractory to conventional interventions. The first child treated with ECMO was a neonate with respiratory failure reported by Dr. Bartlett and colleagues in 1976 [1]. The use of ECMO technology has increased tremendously since then. The Extracorporeal Life Support Organization registry currently contains more than 172,000 ECMO runs in its history, of which approximately 50% are in children [2]. Indications for ECMO include respiratory diseases such as pediatric acute respiratory distress syndrome [3, 4], severe cardiovascular dysfunction with inadequate oxygen delivery in children with congenital heart disease or acquired heart disease [5], or a rapid deployment measure to provide circulatory support in the setting of extracorporeal cardiopulmonary resuscitation (ECPR) [6].
ECMO uses either a roller or centrifugal pump to circulate blood back to the patient after it has passively been removed by indwelling catheters with an intervening oxygenator that uses a hollow fiber membrane for gas exchange (Fig. 1). The circuit accesses blood from the patient via a large venous cannula. Blood is pumped through an oxygenator, which supplies O2 and removes CO2, and the newly oxygenated blood is returned to the patient in either a vein or artery depending on the mode of ECMO. Although ECMO can provide lifesaving cardiopulmonary support for days to months, it is associated with significant risk of neurological injury. Children supported with ECMO are at risk for seizures, intracranial hemorrhage (ICH), and ischemic stroke. These complications are associated with increased mortality as well as long-term mobidity in survivors [7,8,9]. The most foundational principle when deciding on ECMO eligibility is identifying children with potentially reversible diseases who would otherwise have a high probability of mortality or severe morbidity without ECMO support. Many different factors play into the decision of who is most likely to benefit from ECMO. Predictive models have emerged with reasonable test characteristics for respiratory as well as cardiac ECMO support [10,11,12].
Typical pediatric V-A ECMO circuit with cannulation of the right common carotid artery and the right jugular vein. Blood is pumped from the right atrium through the oxygenator, which removes CO2 and adds O2 before returning the blood to the patient’s systemic circulation via the arterial cannula. ECMO, extracorporeal membrane oxygenation, V-A, veno-arterial
Modes of ECMO
Extracorporeal membrane oxygenation can be deployed in many configurations and modes based on location of the drainage and reinfusion cannulas. The two most common modes are veno-venous (V-V) and veno-arterial (V-A). V-V ECMO is used primarily for respiratory support and can be accomplished by using a dual lumen cannula or via two single lumen cannulas in different veins. V-A ECMO is used primarily for cardiac support and typically entails the use of two cannulas, one venous drainage cannula and one arterial return cannula.
If cervical (neck) cannulation is used for either V-V or V-A ECMO the internal jugular vein is used, most often on the right side. This may cause some degree of obstruction to venous drainage from the brain and lead to increased intracranial pressure and lower cerebral perfusion pressure [13]. Some centers use a cephalad drain in smaller patients to decompress cerebral venous drainage; however, analysis of this practice has not shown benefit [14].
Of note, the rate of neurological complications is higher in children supported with V-A compared with V-V ECMO [15]. Air or thrombotic emboli from the circuit can obstruct cerebral vessels leading to ischemic stroke. If the arterial cannula is located in the carotid artery, cerebral perfusion will rely on the contralateral carotid artery and the presence of an intact circle of Willis to provide perfusion to the cerebral hemisphere on the side ipsilateral to the arterial cannulation site [16, 17]. It has been shown that carotid artery cannulation is associated with higher rates of neurological complications compared with femoral artery cannulation [18]. At the end of a V-A ECMO course with carotid artery cannulation, the carotid artery may be ligated or repaired. Repair allows for bilateral carotid flow and recannulation of the same artery should repeat ECMO be needed in the future [19, 20].
Pathophysiology of neurological injury on ECMO
Cerebral Perfusion
The pathophysiology of neurological injury in patients on ECMO is complex and multifactorial. The brain is exquisitely sensitive to perturbations in cerebral blood flow. ECMO disrupts cerebral blood flow in multiple ways. Ligation of the right common carotid artery and right internal jugular vein diminishes anterograde flow through the right carotid artery while increasing flow through the left carotid artery [21]. This also affects venous outflow. Under these circumstances, perfusion of the right hemisphere relies on an intact circle of Willis, but anatomic variations exist that may not support robust collateral flow. Nonpulsatile flow as seen in V-A ECMO has been associated with altered cerebrovascular reactivity and microcirculatory perfusion deficits in both animal models and humans [22,23,24]. Under physiological conditions, autoregulation of the cerebral arterioles ensures adequate cerebral blood flow over a range of systemic perfusion pressures, but ECMO may impair cerebral autoregulation, rendering the brain vulnerable to ischemic and hemorrhagic injury [25].
In infants undergoing ECMO, transcranial Doppler (TCD) provided some of the earliest observations of altered cerebral hemodynamics. These early studies found that the mean pulsatility index (PI) decreased with ECMO initiation and over time at high ECMO flows but actually increased at low ECMO flow [26, 27]. The investigators postulated that this increase in PI correlated with increased cerebral blood flow (CBF) that could lead to ICH. In contrary though, other studies have demonstrated significantly lower CBF velocities (CBFVs) in children on ECMO compared with healthy or other critically ill children, as well as age-related variability [28, 29]. These findings may in part be related to reduced cerebral metabolic demand secondary to sedation frequently used in pediatric patients on ECMO.
Inflammation
In addition to directly altering CBF, ECMO is associated with a profound inflammatory response. The extensive exposure of a patient’s blood to foreign surfaces of the circuit induces a cascade akin to systemic inflammatory response syndrome, compounding the inflammatory response to critical illness that is already present preceding cannulation [30]. On ECMO initiation, interaction between blood and the surfaces of the ECMO circuit activates the complement system, with early elevations of activated C3 and tumor necrosis factor-α [31, 32]. Activated C3 is one of the effector molecules of the complement cascade, collectively termed “anaphylotoxins,” that result in vasodilation, recruitment of immune cells, and triggering of other proinflammatory responses [33]. Elevations in many cytokines, including tumor necrosis factor-α, interleukin-6, and interleukin-8, have been demonstrated in children on ECMO [34,35,36,37]. In addition to these inflammatory mediators, ECMO also results in activation of the contact pathway through activation of factor XII, thus bridging inflammatory and coagulation cascades [38].
Thrombophilia
Nonhemorrhagic brain injury in patients on ECMO is associated with a particularly poor prognosis and warrants special attention [39]. ECMO induces a procoagulant state due to extensive exposure of the blood to artificial materials. Platelet activation, tissue factor release, and activation of the contact system shift the homeostatic balance toward clotting and an increased risk of thrombosis [40,41,42,43]. Thrombosis in the circuit can lead to oxygenator dysfunction, circuit failure, and circuit-induced disseminated intravascular coagulopathy (DIC). Circuit DIC often leads to patient DIC and bleeding complications. Thrombosis in the circuit distal to the oxygenator is particularly worrisome because clots can embolize into the patient’s arterial circulation if on V-A ECMO. There is a need for anticoagulation in ECMO because of the prothrombotic nature of the circuit. The optimal strategy for anticoagulation on ECMO is still unknown; the best drug, dose, method of monitoring, and thresholds for transfusions of blood products are not clear [41, 44]. Unfractionated heparin infusion with activated clotting time and, more recently, antifactor Xa monitoring has become standard practice. Bivalirudin infusion with activated partial thromboplastin time monitoring has emerged as an alternative to unfractionated heparin.
Epidemiology of Acute Brain Injury on ECMO
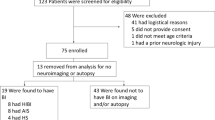
Children on ECMO are at risk for neurological injury due to pre-ECMO events (e.g., hypoxia, hypotension, acidosis, cardiac arrest), comorbidities, and factors associated with ECMO itself. The incidence of neurological injury is reported as high as 25% [45,46,47,48,49]. The most commonly reported neurological complications of ECMO are seizures, intracranial hemorrhage (ICH), and ischemic stroke (Table 1).
Seizures
It is common for children to develop seizures while on ECMO, with reported rates varying widely from about 6% up to 23% [2, 8, 46, 48,49,50,51,52,53]. Some of the variability in seizure incidence may be due to differing monitoring standards at different institutions. Lower rates of seizures of 7% to 8.4%, depending on indication and age group, are reported in the Extracorporeal Life Support Organization registry [2]. Conversely, in single center studies conducted at institutions with extensive video electroencephalography (EEG) monitoring programs, the rate of electrographic and electroclinical seizures was higher, 11% to 23% [8, 50,51,52]. Subclinical seizures in these studies were common, occurring in up to 83% of patients with seizures, suggesting that subclinical seizures are likely underdiagnosed clinically and highlighting the need for neuromonitoring during ECMO [51].
Most seizures started within the first 48 h of ECMO with the first seizure rarely occurring after 72 h on ECMO [8, 51, 52]. Across multiple studies about half of the patients who developed seizures had status epilepticus. Risk factors for the development of seizures in children on ECMO include cardiac indications, ECPR, pre-ECMO cardiac arrest, hypoplastic left heart syndrome, ischemic stroke, and lactic acidosis [8, 9, 51, 54].
The causes of seizures in children on ECMO are multiple. It is common for seizure onset to be the first sign that a structural injury such as ICH or ischemic stroke has occurred. Seizures are also commonly associated with poorer outcomes in children on ECMO, although these studies typically did not adjust for the concomitant presence of structural brain injury [8, 51, 54].
Intracranial Hemorrhage
Anticoagulation is necessary for patients treated with ECMO, and ICH is one of the most feared complications, with a reported incidence of 4–16% [5, 55]. The occurrence of ICH in children on ECMO presents difficult decisions regarding interrupting anticoagulation or adjusting anticoagulation goals, prognosis, and whether to continue ECMO support. There is no standard practice for neuroimaging, leading to variability in detection of ICH [56]. When detected acutely, ICH is often symptomatic and catastrophic, with survival as low at 20% [9, 57]. This low survival, however, may be in part due to a self-fulfilling prophecy, as the historical teaching was that large ICHs would require discontinuation of ECMO support and redirection of care if the child was not able to survive off ECMO. On the other hand, intracranial microbleeds have been shown to be very common in ECMO survivors when assessed by magnetic resonance imaging (MRI) and have unclear clinical significance [58]. Further prospective studies to detect subclinical ICH in children treated with ECMO would provide better prognostic information to inform clinical decisions.
Ischemic Injury
Ischemic injury on ECMO has multiple causes, but two general patterns are seen: global hypoxic-ischemic injury from a low perfusion state, and focal arterial ischemic stroke due to thromboembolic mechanisms (e.g., in situ thrombus formation with artery-to-artery embolus, emboli from the ECMO circuit). Children on ECMO who suffer an ischemic injury have higher mortality, with about 25% lower survival rate compared with those who do not suffer an ischemic stroke [9].
Ischemic injury has been documented in 2% to 17% of children supported on ECMO [9, 49, 59]. The true rate may very well be higher given the lack of standardized protocols for neuroimaging in patients on ECMO and a lower sensitivity for detecting ischemic injury with computed tomography (CT) and ultrasound modalities compared with MRI [9]. Prospective studies using standardized, universal imaging would be helpful for understanding the true incidence but are challenging, given the inherent risks of transporting critically ill patients and the lack of widely available portable technologies.
In a 10-year retrospective study of 81 neonates who underwent routine brain MRI following ECMO, 6% had infarctions primarily in arterial vascular territories, with no difference in infarction rate between V-A and V-V ECMO recipients [60]. In an 8-year retrospective review of 878 adult patients on V-A ECMO, ECMO-related neurological injury was diagnosed in nearly 8% of patients, with 5% suffering ischemic strokes [61]. In a large retrospective cohort of 677 neonates, ischemic stroke occurred in 5%, including 30 patients with arterial ischemic stroke and 4 patients with venous sinus thrombosis [62]. In another institutional study of 179 patients on ECMO, 82 underwent at least one CT scan and 49 exhibited brain injury with 27 of these being ischemic [9]. Of these patients, 41% had bilateral infarctions whereas 15% had isolated right side and 15% had isolated left side infarctions [9]. Distribution of ischemic injury in patients on ECMO has been variable in reported case series, and hypothesized factors influencing this include the site of cannulation and the presence of a complete circle of Willis, which may influence venous pressure and cerebral perfusion.
Outcomes
Children with severe respiratory or cardiac failure supported with ECMO have a substantially higher risk of mortality than the general intensive care unit population. Survival to hospital discharge varies by age and indication; it is lowest for neonatal and pediatric ECPR (42%) and highest for neonatal respiratory ECMO (73%) [2].
Children supported on ECMO who survive to hospital discharge frequently suffer from long-term deficits due to neurological injuries acquired during hospitalization for ECMO [63]. Cognitive deficits, behavioral problems, motor impairments, and lower health-related quality of life have been described in 10% to as many as 60% of survivors of critical illness requiring ECMO support [63]. Improving neurological monitoring of children supported on ECMO could lead to identification of at-risk physiological states and earlier detection of neurological injury. The next step would be to then identify interventions directed toward modifying those states to reduce morbidity and improve neurological outcome.
Neuromonitoring in Patients on ECMO
Neurological Examination
Although the neurological examination is the gold standard of determining neurological function, a reliable examination is often not available in patients treated with ECMO. Sedation and paralysis may be required to protect the patient and catheter safety while on the ECMO circuit, particularly in children. Even if awake, reversible alterations in mental status including encephalopathy and delirium due to metabolic derangements and intensive care unit environment frequently confound the clinical assessment of the patient. Highlighting the importance of the neurological examination, some centers advocate for sedation holidays or “neurologic wake up tests.” While providing the ability to directly assess the patient’s neurological function, there are potential concerns with this practice, including increasing patient distress and pain as well as increasing intracranial pressure and cerebral perfusion pressure, although evidence suggests that this does not necessarily translate to alterations of energy metabolism and oxygenation in patients with brain injury [64,65,66]. Neurologic wake up tests can only be performed intermittently, and there certainly may be times when a patient’s condition precludes weaning of sedation to any significant degree. For this reason, clinicians often rely on ancillary assessments of neurological function through a variety of modalities [67].
Quantitative Pupillometry
Although the neurological examination is often limited in patients during ECMO treatment, the pupillary reflex remains accessible, and automated pupillometry is being more widely used and studied in neurocritical care patients. Quantitative pupillometry reliably and sensitively assesses both static and dynamic aspects of the pupillary reflex, with normative data established in pediatric patients [68, 69]. A study of 28 pediatric patients with acute brain injury or encephalopathy included 1,171 measurements of intracranial pressure (ICP) and found that the Neurological Pupil index (NPi), a proprietary algorithm combining measures of pupil reactivity, percent change in pupil size, constriction velocity, and dilation velocity were all lower when intracranial pressure was elevated (greater than or equal to 20 mm Hg) [70]. Although pupil reactivity had an inverse correlation with concurrent ICP measurements, the NPi was not consistently predictive of patients who, with normal ICP at enrollment, would go on to develop increased ICP [70]. When evaluated within the first 72 h, the abnormal NPi (less than 3) has also been associated with poor neurological outcome in adult patients with severe brain injury [71]. In a study of 100 consecutive adult patients treated with VA-ECMO, an NPi less than 3 at any time from 24 to 72 h from ECMO initiation was 100% specific for 90 day mortality [72]. Other emerging uses for quantitative pupillometry include assessment of pain in sedated children [73], but further research is still necessary to understand all the factors that influence pupil reactivity in these patient populations who frequently have numerous potential confounders such as pharmacologic treatments and metabolic conditions [74].
Structural Imaging
Ultrasound
Cranial ultrasound is currently the most common portable, noninvasive imaging technique for children supported on ECMO and as such has become part of the routine neuromonitoring techniques in clinical practice. The current Extracorporeal Life Support Organization neuromonitoring guidelines recommend cranial ultrasound on a regular cadence; daily for the first 3–5 days followed by variable intervals based on clinical concerns such as new onset seizures or sudden decline in hemoglobin [75, 76]. Despite their appeal, cranial ultrasounds have several limitations including age limitation given the need for an open anterior fontanelle in addition to field of view limitations and variability in diagnostic criteria [77]. Secondly, to date, cranial ultrasound abnormalities have shown limited associations with long-term neurodevelopmental outcomes in survivors and are typically predictive only with severe lesions [78, 79]. Evaluation of 50 post-ECMO neonatal brain MRI studies showed inconsistency between MRI and ultrasound findings, with half of the patients with normal ultrasound findings noted to have MRI abnormalities [15]. As such, cranial ultrasounds continue to be utilized as primarily neuroimaging screening modalities with the need for confirmatory testing with CT or post-ECMO MRI.
Abnormalities detected on cranial ultrasound can be categorized as vessel occlusion abnormalities including arterial ischemic strokes or sinus venous thrombosis, primary hemorrhage including parenchymal, extracerebral and choroid plexus, and other abnormalities including focal dysplasia, hydrocephalus, evolving hematoma, periventricular leukomalacia, cortical laminar necrosis, lenticulostriate vasculopathy, and diffuse hypoxic-ischemic encephalopathy [62, 77]. Spectral Doppler flow assessments also allow evaluation of the resistance in intracranial vessels, resistive index, including the internal carotid and basilar arteries, the circle of Willis as well as the superior sagittal sinus, vein of Galen, and straight sinus. There is preliminary evidence that a greater than 10% variability in the resistive index with gentle compression of the anterior fontanelle is associated with neurological complications on ECMO [80].
CT
Head CT continues to be the imaging modality of choice on ECMO for older children in whom cranial ultrasound cannot be obtained. CT provides a full detailed view of the brain with the ability to identify ICH with high sensitivity and minimal interoperator variability (Fig. 2a). CT however is less sensitive at identifying early ischemic injury (Fig. 2b) [9]. There is evidence for higher detection of these abnormalities with more CT use, with associated concern for underreporting of intracranial complications occurring during the ECMO course [81]. Detection of these abnormalities, depending on their severity, has the potential to significantly impact patient care with alterations in anticoagulation management or even efforts to discontinue extracorporeal support [82].
Examples of head CT abnormalities on ECMO. a Head CT of a 4-year-old patient with failed Fontan physiology on ECMO day 3 following cardiac arrest showing large predominantly intraparenchymal hemorrhage centered in the left frontal and left parietal lobes. There is spillage into both lateral ventricles and small volume subarachnoid hemorrhage surrounding the large intraparenchymal hemorrhage. b Head CT image of a 6-month-old patient with dilated cardiomyopathy on day 26 of ECMO with evidence of bilateral posterior cerebral artery territory infarcts, larger and more well-defined on the left without evidence of mass effect or midline shift. CT, computed tomography, ECMO, extracorporeal membrane oxygenation
In the absence of portable CT, one of the major limitations of head CT is the need for intrahospital transport and the associated potential complications, thus limiting its use to clinical suspicion of an acute neurological injury [83]. Additionally, CT is associated with the risk of radiation exposure, another factor weighed in the decision making of obtaining head CT on ECMO. While contrast-enhanced CT can be used for studying blood flow through angiography and perfusion imaging, the altered hemodynamics in patients on ECMO can significantly impact the accuracy and interpretation of such imaging [84].
CBF Monitoring
TCD Sonography
Transcranial Doppler sonography provides a noninvasive, portable, and inexpensive means of monitoring CBFV in real time. Insonation through different acoustic windows can provide measurements of CBFV and PI in all the large cerebral arteries around the circle of Willis. PI reflects downstream vascular resistance and may be altered by impaired cerebral perfusion or autoregulation, intracranial hypertension/poor brain compliance, or distal stenosis [85]. General applications of TCD include assessment of intracranial pressure, measurement of cerebrovascular autoregulation, evaluation of vasospasm, and detection of cerebral embolization or large vessel occlusion. ECMO produces predictable alterations in TCD waveforms, but these applications remain investigational in patients undergoing ECMO therapy.
Variable associations have been identified between CBFVs and neurological injury in children treated with ECMO, likely reflecting small patient numbers in most of these case series [28, 86]. In one study of 27 patients, there was no statistically significant association between CBFVs and neurological injury, defined as focal deficits on clinical exam, seizures, or severe EEG abnormalities [28]. In contrast another study of 18 children found elevated CBFVs in patients who suffered intracerebral hemorrhage, with the increased velocities occurring 2–6 days prior to recognition of the injury.
In addition to providing information about cerebral hemodynamics in children on ECMO, TCD has the potential to be used in real time to rapidly identify causes of neurological injury that may be amenable to intervention, such as emboli leading to stroke (Fig. 3) [87, 88]. TCD has several limitations. About 10–20% of patients will not have adequate acoustic windows for reliable insonation. Performance of this technique relies on skilled operators and thus is limited by their availability. These characteristics make TCD more suitable to intermittent evaluation rather than continuous monitoring.
Elementary school aged boy presented with fever and purpura fulminans due to Staphylococcal toxic shock syndrome and developed refractory shock requiring V-A ECMO. TCD study of the left (a) and right (b) MCA showed mean CBFVs that were 6 and 3 standard deviations below normal for age [89], respectively. There is a 35% side-to-side asymmetry in mean CBFV, with relatively increased mean, peak systolic, and end-diastolic velocity in the right MCA. Neurologic examination 10 days after decannulation off sedation was notable for left upper extremity plegia. Brain MRI (c) the following day showed patchy edema (partially facilitated, partially restricted in diffusion) in the right insula, right superior temporal gyrus, right basal ganglia, and inferior right parietal lobe consistent with subacute infarctions in the right MCA. CBFV, cerebral blood flow velocity, ECMO, extracorporeal membrane oxygenation, EDV, HR, MCA, xxx, MRI, magnetic resonance imaging, PI, pulsatility index, RI, resistive index, S/D, xxx, TCD, transcranial Doppler, V-A, veno-arterial
Microvascular Imaging
Microvascular imaging is an emerging Doppler sonography technique that can provide high-resolution visualization of microvasculature in both deep and superficial brain structures in infants with an open fontanelle [90]. This method can identify tortuosity in the vessels, perfusion heterogeneity or asymmetry, and vascular engorgement [91]. A study of 30 patients demonstrated the feasibility of this technique, and while there was no association of basal ganglia abnormalities with neurological outcome, white matter vascular engorgement showed a statistically significant association with poor neurological outcome defined as death, seizure, or cerebrovascular injury [92].
Physiological Monitoring
Cerebral Oximetry
Near-infrared spectroscopy (NIRS) offers a means to continuously monitor regional cerebral oxygen saturation (crSO2). In infants and children, NIRS has demonstrated reductions in the concentration of oxyhemoglobin and concomitant increases in the concentration of deoxyhemoglobin immediately after cannulation onto ECMO, with return to baseline or even over the first hour [93, 94]. Recent studies have analyzed the association between NIRS monitoring and neurologic outcome. In a series of 34 neonates, crSO2 < 50% and a change of at least 20% from baseline (ΔcrSO2) were associated with death or brain injury [95]. This was confirmed in the largest study to date of 153 infants and children at a single academic center, in which both criteria were again associated with poor outcome at hospital discharge (either death or survival with Pediatric Cerebral Performance Category [PCPC] score > 2 at discharge, with decline from baseline PCPC) [96]. Another study of 63 patients found similar associations using a slightly different outcome definition that included any evident neurological injury, providing positive predictive values of 78% and 80% for crSO2 < 50% and ΔrScO2 > 20%, respectively [97].
Another active area of investigation and promise for cerebral oximetry measures is in the determination of cerebral autoregulation. In six newborns on V-A ECMO, decreasing ECMO flows were associated with loss of cerebrovascular autoregulation demonstrated by wavelet cross-correlation between multisite oxyhemoglobin concentration and mean arterial blood pressure [98]. A more recent pilot study of 29 children treated with either V-A or V-V ECMO demonstrated feasibility of continuous assessment of cerebral autoregulation. The investigators found that children with acute neurological events while on ECMO had both a higher mean cerebral oxygenation reactivity index and a greater percentage of time with impaired autoregulation, indicated by cerebral oxygenation reactivity index greater than 0.3 [99].
Measuring cerebral oximetry with NIRS has the distinct benefit of providing continuous monitoring that can easily be integrated into multimodal monitoring systems. The limitations of NIRS include the highly restricted area that is monitored, namely the frontal lobes. Thus, NIRS provides only a regional measure of cerebral oxygen saturation. While the utility of continuous monitoring of cerebral oxygenation and autoregulation is promising, further work is needed to determine whether interventions based upon these measures can influence outcome.
EEG
Electroencephalography provides direct information regarding brain physiology through the measurement of cortical electrical activity. It has become more widely used in critically ill children, providing the benefit of continuous noninvasive monitoring. Unlike regional information provided by cerebral oximetry, full EEG electrode arrays provide information about global cortical function. In addition to demonstrating electrographic seizures, EEG background can provide indirect information about CBF. As cerebral perfusion decreases, the EEG initially shows loss of faster frequencies, followed by an increase in slow frequency activity, and ultimately suppression of activity [100]. These changes are detectable even in states of critical illness, when the baseline EEG tracing is already abnormal due to sedation and other factors [101].
One of the largest case series of EEG monitoring studied 112 children on ECMO, of whom 99 received continuous video EEG (cEEG) monitoring for at least 1 day, identifying seizures in 16% of patients. Of the patients who had seizures, most were only electrographic-without clinical correlate, and more than half exhibited electrographic status epilepticus [51]. In this cohort, mortality and poor neurologic outcome were more common in patients with electrographic seizures. Another study of 70 children on ECMO who received cEEG monitoring identified electrographic seizures in 23%, with electrographic status epilepticus in 7% [52]. A third smaller case series of 19 patients further supported these findings with 21% of patients having electrographic seizures, all of which were subclinical [102]. In these studies, the majority of seizures were detected within the first 48 h of ECMO initiation.
Changes in EEG background may also be predictive of neurological injury. Lin et al. identified focal background abnormalities in 12% of patients on ECMO, most of which correlated to acute neuroimaging abnormalities [51]. Focal slowing and focal attenuation of the EEG signal were also commonly associated with injury on neuroimaging in a study by Piantino et al. [102]. In all studies the occurrence of seizures was also highly correlated to subsequent detection of neurological injury [51, 52, 102].
Amplitude-integrated EEG is a simpler method to monitor the brain’s electrical activity. It uses a reduced montage of electrodes to provide a time-compressed EEG tracing. Most commonly used in neonates, it has become a standard of care in monitoring during hypothermia for neonatal hypoxic-ischemic encephalopathy [103,104,105,106,107,108]. One study found that a background score of > 17 (out of 32) for the first 24 h of aEEG was highly predictive of poor outcome (positive predictive value 95%) [109]. Although the reduced electrode montage of aEEG reduces the sensitivity and ability to localize abnormalities, the relative simplicity and ease of use and interpretability make this an appealing alternative to full montage cEEG.
Continuous EEG offers tremendous promise for neuromonitoring during ECMO, but it is not without challenges. Most cEEG monitoring is recorded continuously but analyzed intermittently, thus detecting changes in real time is not always realistic. The vast array of equipment in a critical care setting can create electrical artifacts in the recordings which requires troubleshooting. Lead attachment and maintenance can also be difficulty in these children, particularly given poor perfusion states and edema. Thus, while cEEG provides extremely valuable information, obtaining a reliable study requires skilled and experienced technicians.
Plasma Biomarkers
Plasma biomarkers have been extensively studied in critical illness, and data are beginning to emerge in pediatric patients on ECMO, as well. Prospective studies of 22 and 80 children in one pediatric intensive care unit identified associations between peak levels of GFAP, MCP1, NSE, and S100b and unfavorable outcome (death or survival with neurological disability determined by PCPC) [37, 110]. A two-center observational cohort did not identify any associations between inflammatory biomarkers and long-term neurobehavioral outcome, but levels of interleukin-6 and plasminogen activator inhibitor-1 were elevated in children who died compared with those who survived to discharge [36].
Plasma biomarkers offer the advantage of specifically probing pathophysiological cascades, and the potential to identify modifiable factors that may improve outcome after ECMO. Differentiating between central nervous system and systemic contributions to peripherally measured biomarkers remains a confounder in determining the specific relevance to neurological injury versus critical illness in general. Also measuring peripheral biomarkers relies on disruption of the blood brain barrier, a pathophysiological process that occurs with injury but may not be directly correlated with severity and may not be consistent from patient to patient. Further studies of plasma biomarkers in this population will help to clarify some of these issues.
Knowledge Gaps and Future Directions
Increasing use of neuromonitoring strategies has provided a deeper understanding of the physiological changes that occur on ECMO and predispose to neurological injury. This has mostly been applied to determining predictors of neurologic outcome, but with further refinement neuromonitoring strategies have the potential to allow precision medicine in patients on ECMO, tailoring our care to provide individually optimized cerebral perfusion and reduce the incidence of neurological injury. For instance, significant decrease in the arterial partial pressure of CO2 at ECMO initiation has been consistently associated with adverse neurological events and mortality [111,112,113]. Arterial partial pressure of CO2 has important cerebrovascular effects, and technical modifications in the ECMO circuit such as adjusting flow rates or sweep to change the amount of CO2 removed from the blood may offer a means to proactively alter CBF for neuroprotective purposes [114]. Neuromonitoring data could also be used to target blood pressures within the range of autoregulation [99, 115]. Modifications to add pulsatility to ECMO flow may also be a means of improving hemodynamics and reducing microcirculatory damage [116].
One step toward achieving these goals will be developing more continuous monitoring strategies. Of the current widely used technologies, NIRS and EEG allow for continuous monitoring, though both are typically continuously recorded but only intermittently evaluated. The development of automated algorithms that can detect important changes in these neuromonitoring modalities will be useful in furthering this cause. Quantitative EEG is one example of this, extracting trends from the background of the EEG to provide prognostic values. Given significant limitations to the clinical neurological examination in patients on ECMO, we also rely on imaging studies to confirm acute injury. Transport of patients on ECMO is not a trivial endeavor, and further optimization and adoption of portable bedside imaging modalities may facilitate the ability to detect acute injury. To date clinicians have had to rely on CT scan or ultrasound for brain imaging, modalities that have limited temporal and spatial resolution for detecting acute injury. Evolving technologies including MRI that is portable and compatible with the ECMO circuit may eventually further enhance our capability for detecting neurological injury [117].
Conclusions
Extracorporeal membrane oxygenation is a lifesaving procedure for children with catastrophic cardiorespiratory failure, but neurological injury remains a significant complication that negatively impacts long-term outcome. Multiple factors including, but not limited to, critical illness and the need for sedation limit the ability to clinically monitor for neurological injury or deterioration. As we have reviewed here, there are numerous modalities available for neuromonitoring in these patients, each with their own uses and limitations. Increasing the systematic use of such technologies will continue to further our understanding of neurological injury that occurs in patients on ECMO, provide the ability to predict such injury, and ultimately tailor therapeutic strategies to improve outcome.
References
Bartlett RH, Gazzaniga AB, Jefferies MR, Huxtable RF, Haiduc NJ, Fong SW. Extracorporeal membrane oxygenation (ECMO) cardiopulmonary support in infancy. Trans Am Soc Artif Intern Organs. 1976;22:80–93.
International Summary - April, 2022. 2022. (Accessed 2 June 2022, at https://elso.org/Registry/InternationalSummaryandReports/InternationalSummary.aspx.)
Maratta C, Potera RM, van Leeuwen G, Castillo Moya A, Raman L, Annich GM. Extracorporeal life support organization (ELSO): 2020 pediatric respiratory ELSO guideline. ASAIO J. 2020;66:975–9.
Khemani RG, Smith L, Lopez-Fernandez YM, et al. Paediatric acute respiratory distress syndrome incidence and epidemiology (PARDIE): an international, observational study. Lancet Respir Med. 2019;7:115–28.
Barbaro RP, Paden ML, Guner YS, et al. Pediatric extracorporeal life support organization registry international report 2016. ASAIO J. 2017;63:456–63.
Conrad SA, Broman LM, Taccone FS, et al. The extracorporeal life support organization maastricht treaty for nomenclature in extracorporeal life support. A position paper of the extracorporeal life support organization. Am J Respir Crit Care Med. 2018;198:447–51.
Bembea MM, Felling RJ, Caprarola SD, et al. Neurologic outcomes in a two-center cohort of neonatal and pediatric patients supported on extracorporeal membrane oxygenation. ASAIO J. 2020;66:79–88.
Hassumani DO, Shan M, Mastropietro CW, Wing SE, Friedman ML. Seizures in children with cardiac disease on extracorporeal membrane oxygenation. Neurocrit Care. 2022;36:157–63.
LaRovere KL, Vonberg FW, Prabhu SP, et al. Patterns of head computed tomography abnormalities during pediatric extracorporeal membrane oxygenation and association with outcomes. Pediatr Neurol. 2017;73:64–70.
Bailly DK, Reeder RW, Zabrocki LA, et al. Development and validation of a score to predict mortality in children undergoing extracorporeal membrane oxygenation for respiratory failure: pediatric pulmonary rescue with extracorporeal membrane oxygenation prediction score. Crit Care Med. 2017;45:e58–66.
Barbaro RP, Bartlett RH, Chapman RL, et al. Development and validation of the neonatal risk estimate score for children using extracorporeal respiratory support. J Pediatr. 2016;173(56–61):e3.
Barbaro RP, Boonstra PS, Paden ML, et al. Development and validation of the pediatric risk estimate score for children using extracorporeal respiratory support (Ped-RESCUERS). Intensive Care Med. 2016;42:879–88.
Weber TR, Kountzman B. The effects of venous occlusion on cerebral blood flow characteristics during ECMO. J Pediatr Surg. 1996;31:1124–7.
Skarsgard ED, Salt DR, Lee SK. Venovenous extracorporeal membrane oxygenation in neonatal respiratory failure: Does routine, cephalad jugular drainage improve outcome? J Pediatr Surg. 2004;39:672–6.
Rollins MD, Hubbard A, Zabrocki L, Barnhart DC, Bratton SL. Extracorporeal membrane oxygenation cannulation trends for pediatric respiratory failure and central nervous system injury. J Pediatr Surg. 2012;47:68–75.
Matsumoto JS, Babcock DS, Brody AS, Weiss RG, Ryckman FG, Hiyama D. Right common carotid artery ligation for extracorporeal membrane oxygenation: cerebral blood flow velocity measurement with Doppler duplex US. Radiology. 1990;175:757–60.
Raju TN, Kim SY, Meller JL, Srinivasan G, Ghai V, Reyes H. Circle of Willis blood velocity and flow direction after common carotid artery ligation for neonatal extracorporeal membrane oxygenation. Pediatrics. 1989;83:343–7.
Teele SA, Salvin JW, Barrett CS, et al. The association of carotid artery cannulation and neurologic injury in pediatric patients supported with venoarterial extracorporeal membrane oxygenation*. Pediatr Crit Care Med J Soc Crit Care Med World Feder Pediatr Intensive Crit Care Soc. 2014;15:355–61.
Baumgart S, Streletz LJ, Needleman L, et al. Right common carotid artery reconstruction after extracorporeal membrane oxygenation: vascular imaging, cerebral circulation, electroencephalographic, and neurodevelopmental correlates to recovery. J Pediatr. 1994;125:295–304.
DeAngelis GA, Mitchell DG, Merton DA, et al. Right common carotid artery reconstruction in neonates after extracorporeal membrane oxygenation: color Doppler imaging. Radiology. 1992;182:521–5.
Lohrer RM, Bejar RF, Simko AJ, Moulton SL, Cornish JD. Internal carotid artery blood flow velocities before, during, and after extracorporeal membrane oxygenation. Am J Dis Child. 1992;146:201–7.
O’Neil MP, Fleming JC, Badhwar A, Guo LR. Pulsatile versus nonpulsatile flow during cardiopulmonary bypass: microcirculatory and systemic effects. Ann Thorac Surg. 2012;94:2046–53.
Veraar CM, Rinosl H, Kuhn K, et al. Non-pulsatile blood flow is associated with enhanced cerebrovascular carbon dioxide reactivity and an attenuated relationship between cerebral blood flow and regional brain oxygenation. Crit Care. 2019;23:426.
Salameh A, Kuhne L, Grassl M, et al. Protective effects of pulsatile flow during cardiopulmonary bypass. Ann Thorac Surg. 2015;99:192–9.
Short BL, Walker LK, Bender KS, Traystman RJ. Impairment of cerebral autoregulation during extracorporeal membrane oxygenation in newborn lambs. Pediatr Res. 1993;33:289–94.
van de Bor M, Walther FJ, Gangitano ES, Snyder JR. Extracorporeal membrane oxygenation and cerebral blood flow velocity in newborn infants. Crit Care Med. 1990;18:10–3.
Taylor GA, Catena LM, Garin DB, Miller MK, Short BL. Intracranial flow patterns in infants undergoing extracorporeal membrane oxygenation: preliminary observations with Doppler US. Radiology. 1987;165:671–4.
Rilinger JF, Smith CM, deRegnier RAO, et al. Transcranial doppler identification of neurologic injury during pediatric extracorporeal membrane oxygenation therapy. J Stroke Cerebrovasc Dis Off J Natl Stroke Assoc. 2017;26:2336–45.
O’Brien NF, Buttram SDW, Maa T, Lovett ME, Reuter-Rice K, LaRovere KL. Cerebrovascular physiology during pediatric extracorporeal membrane oxygenation: a multicenter study using transcranial doppler ultrasonography. Pediatr Crit Care Med J Soc Crit Care Med World Feder Pediatr Intensive Crit Care Soc. 2019;20:178–86.
Millar JE, Fanning JP, McDonald CI, McAuley DF, Fraser JF. The inflammatory response to extracorporeal membrane oxygenation (ECMO): a review of the pathophysiology. Crit Care. 2016;20:387.
Plotz FB, van Oeveren W, Bartlett RH, Wildevuur CR. Blood activation during neonatal extracorporeal life support. J Thorac Cardiovasc Surg. 1993;105:823–32.
Graulich J, Sonntag J, Marcinkowski M, et al. Complement activation by in vivo neonatal and in vitro extracorporeal membrane oxygenation. Mediators Inflamm. 2002;11:69–73.
Dunkelberger JR, Song WC. Complement and its role in innate and adaptive immune responses. Cell Res. 2010;20:34–50.
Mildner RJ, Taub N, Vyas JR, et al. Cytokine imbalance in infants receiving extracorporeal membrane oxygenation for respiratory failure. Biol Neonate. 2005;88:321–7.
Mc IRB, Timpa JG, Kurundkar AR, et al. Plasma concentrations of inflammatory cytokines rise rapidly during ECMO-related SIRS due to the release of preformed stores in the intestine. Lab Invest. 2010;90:128–39.
Caprarola SD, Ng DK, Carroll MK, et al. Pediatric ECMO: unfavorable outcomes are associated with inflammation and endothelial activation. Pediatr Res. 2021;92:549–56.
Bembea MM, Rizkalla N, Freedy J, et al. Plasma biomarkers of brain injury as diagnostic tools and outcome predictors after extracorporeal membrane oxygenation. Crit Care Med. 2015;43:2202–11.
Wendel HP, Scheule AM, Eckstein FS, Ziemer G. Haemocompatibility of paediatric membrane oxygenators with heparin-coated surfaces. Perfusion. 1999;14:21–8.
Iacobelli R, Fletcher-Sandersjoo A, Lindblad C, Keselman B, Thelin EP, Broman LM. Predictors of brain infarction in adult patients on extracorporeal membrane oxygenation: an observational cohort study. Sci Rep. 2021;11:3809.
Annich G, Adachi I. Anticoagulation for pediatric mechanical circulatory support. Pediatr Crit Care Med J Soc Crit Care Med World Feder Pediatr Intensive Crit Care Soc. 2013;14:S37–42.
Barton R, Ignjatovic V, Monagle P. Anticoagulation during ECMO in neonatal and paediatric patients. Thromb Res. 2019;173:172–7.
Callaghan S, Cai T, McCafferty C, et al. Adsorption of blood components to extracorporeal membrane oxygenation (ECMO) surfaces in humans: a systematic review. J Clin Med. 2020;9:3272.
Yaw HP, Van Den Helm S, MacLaren G, Linden M, Monagle P, Ignjatovic V. Platelet phenotype and function in the setting of pediatric extracorporeal membrane oxygenation (ECMO): a systematic review. Front Cardiovasc Med. 2019;6:137.
Ozment CP, Scott BL, Bembea MM, et al. Anticoagulation and transfusion management during neonatal and pediatric extracorporeal membrane oxygenation: a survey of medical directors in the United States. Pediatr Crit Care Med J Soc Crit Care Med World Feder Pediatr Intensive Crit Care Soc. 2021;22:530–41.
Barrett CS, Bratton SL, Salvin JW, Laussen PC, Rycus PT, Thiagarajan RR. Neurological injury after extracorporeal membrane oxygenation use to aid pediatric cardiopulmonary resuscitation. Pediatr Crit Care Med J Soc Crit Care Med World Feder Pediatr Intensive Crit Care Soc. 2009;10:445–51.
Hervey-Jumper SL, Annich GM, Yancon AR, Garton HJ, Muraszko KM, Maher CO. Neurological complications of extracorporeal membrane oxygenation in children. J Neurosurg Pediatr. 2011;7:338–44.
Mehta A, Ibsen LM. Neurologic complications and neurodevelopmental outcome with extracorporeal life support. World J Crit Care Med. 2013;2:40–7.
Polito A, Barrett CS, Rycus PT, Favia I, Cogo PE, Thiagarajan RR. Neurologic injury in neonates with congenital heart disease during extracorporeal membrane oxygenation: an analysis of extracorporeal life support organization registry data. ASAIO J. 2015;61:43–8.
Polito A, Barrett CS, Wypij D, et al. Neurologic complications in neonates supported with extracorporeal membrane oxygenation. An analysis of ELSO registry data. Intensive Care Med. 2013;39(9):1594–601. https://doi.org/10.1007/s00134-013-2985-x.
Cook RJ, Rau SM, Lester-Pelham SG, et al. Electrographic seizures and brain injury in children requiring extracorporeal membrane oxygenation. Pediatr Neurol. 2020;108:77–85.
Lin JJ, Banwell BL, Berg RA, et al. Electrographic seizures in children and neonates undergoing extracorporeal membrane oxygenation. Pediatr Crit Care Med J Soc Crit Care Med World Feder Pediatr Intensive Crit Care Soc. 2017;18:249–57.
Okochi S, Shakoor A, Barton S, et al. Prevalence of seizures in pediatric extracorporeal membrane oxygenation patients as measured by continuous electroencephalography. Pediatr Crit Care Med J Soc Crit Care Med World Feder Pediatr Intensive Crit Care Soc. 2018;19:1162–7.
Yuliati A, Federman M, Rao LM, Chen L, Sim MS, Matsumoto JH. Prevalence of seizures and risk factors for mortality in a continuous cohort of pediatric extracorporeal membrane oxygenation patients. Pediatr Crit Care Med J Soc Crit Care Med World Feder Pediatr Intensive Crit Care Soc. 2020;21:949–58.
Bauer Huang SL, Said AS, Smyser CD, Lin JC, Guilliams KP, Guerriero RM. Seizures are associated with brain injury in infants undergoing extracorporeal membrane oxygenation. J Child Neurol. 2021;36:230–6.
Bembea MM, Ng DK, Rizkalla N, et al. Outcomes after extracorporeal cardiopulmonary resuscitation of pediatric in-hospital cardiac arrest: a report from the get with the guidelines-resuscitation and the extracorporeal life support organization registries. Crit Care Med. 2019;47:e278–85.
Cvetkovic M, Chiarini G, Belliato M, et al. International survey of neuromonitoring and neurodevelopmental outcome in children and adults supported on extracorporeal membrane oxygenation in Europe. Perfusion. 2021. https://doi.org/10.1177/02676591211042563.
Dalton HJ, Reeder R, Garcia-Filion P, et al. Factors associated with bleeding and thrombosis in children receiving extracorporeal membrane oxygenation. Am J Respir Crit Care Med. 2017;196:762–71.
Liebeskind DS, Sanossian N, Sapo ML, Saver JL. Cerebral microbleeds after use of extracorporeal membrane oxygenation in children. J Neuroimag Off J Am Soc Neuroimag. 2013;23:75–8.
Pinto VL, Pruthi S, Westrick AC, Shannon CN, Bridges BC, Le TM. Brain magnetic resonance imaging findings in pediatric patients post extracorporeal membrane oxygenation. ASAIO J. 2017;63:810–4.
Wien MA, Whitehead MT, Bulas D, et al. Patterns of brain injury in newborns treated with extracorporeal membrane oxygenation. AJNR Am J Neuroradiol. 2017;38:820–6.
Le Guennec L, Cholet C, Huang F, et al. Ischemic and hemorrhagic brain injury during venoarterial-extracorporeal membrane oxygenation. Ann Intensive Care. 2018;8:129.
Raets MM, Dudink J, Ijsselstijn H, et al. Brain injury associated with neonatal extracorporeal membrane oxygenation in the Netherlands: a nationwide evaluation spanning two decades. Pediatr Crit Care Med J Soc Crit Care Med World Feder Pediatr Intensive Crit Care Soc. 2013;14:884–92.
Boyle K, Felling R, Yiu A, et al. Neurologic outcomes after extracorporeal membrane oxygenation: a systematic review. Pediatr Crit Care Med J Soc Crit Care Med World Feder Pediatr Intensive Crit Care Soc. 2018;19:760–6.
Skoglund K, Hillered L, Purins K, et al. The neurological wake-up test does not alter cerebral energy metabolism and oxygenation in patients with severe traumatic brain injury. Neurocrit Care. 2014;20:413–26.
Skoglund K, Enblad P, Hillered L, Marklund N. The neurological wake-up test increases stress hormone levels in patients with severe traumatic brain injury. Crit Care Med. 2012;40:216–22.
Skoglund K, Enblad P, Marklund N. Effects of the neurological wake-up test on intracranial pressure and cerebral perfusion pressure in brain-injured patients. Neurocrit Care. 2009;11:135–42.
Bembea MM, Felling R, Anton B, Salorio CF, Johnston MV. Neuromonitoring during extracorporeal membrane oxygenation: a systematic review of the literature. Pediatr Crit Care Med J Soc Crit Care Med World Feder Pediatr Intensive Crit Care Soc. 2015;16:558–64.
Boev AN, Fountas KN, Karampelas I, et al. Quantitative pupillometry: normative data in healthy pediatric volunteers. J Neurosurg. 2005;103:496–500.
Couret D, Boumaza D, Grisotto C, et al. Reliability of standard pupillometry practice in neurocritical care: an observational, double-blinded study. Crit Care. 2016;20:99.
Freeman AD, McCracken CE, Stockwell JA. Automated pupillary measurements inversely correlate with increased intracranial pressure in pediatric patients with acute brain injury or encephalopathy. Pediatr Crit Care Med J Soc Crit Care Med World Feder Pediatr Intensive Crit Care Soc. 2020;21:753–9.
Romagnosi F, Bernini A, Bongiovanni F, et al. Neurological pupil index for the early prediction of outcome in severe acute brain injury patients. Brain Sci. 2022;12:609.
Miroz JP, Ben-Hamouda N, Bernini A, et al. Neurological pupil index for early prognostication after venoarterial extracorporeal membrane oxygenation. Chest. 2020;157:1167–74.
Tosi F, Gatto A, Capossela L, et al. Role of the pupillometer in the assessment of pain in the sedation of pediatric patients. Eur Rev Med Pharmacol Sci. 2021;25:6349–55.
Opic P, Ruegg S, Marsch S, Gut SS, Sutter R. Automated quantitative pupillometry in the critically Ill: a systematic review of the literature. Neurology. 2021;97:e629–42.
Wild KT, Rintoul N, Kattan J, Gray B. Extracorporeal life support organization (ELSO): guidelines for neonatal respiratory failure. ASAIO J. 2020;66:463–70.
ELSO guidelines: Patient Care Practice Guidelines. 2015. at https://www.elso.org/Resources/Guidelines.aspx.)
Svrckova P, Meshaka R, Holtrup M, et al. Imaging of cerebral complications of extracorporeal membrane oxygenation in infants with congenital heart disease - ultrasound with multimodality correlation. Pediatr Radiol. 2020;50:997–1009.
Glass P, Bulas DI, Wagner AE, et al. Severity of brain injury following neonatal extracorporeal membrane oxygenation and outcome at age 5 years. Dev Med Child Neurol. 1997;39:441–8.
Lazar EL, Abramson SJ, Weinstein S, Stolar CJH. Neuroimaging of brain injury in neonates treated with extracorporeal membrane oxygenation: lessons learned from serial examinations. J Pediatr Surg. 1994;29(2):186–91. https://doi.org/10.1016/0022-3468(94)90315-8.
Zamora CA, Oshmyansky A, Bembea M, et al. Resistive index variability in anterior cerebral artery measurements during daily transcranial duplex sonography: a predictor of cerebrovascular complications in infants undergoing extracorporeal membrane oxygenation? J Ultrasound Med Off J Am Instit Ultrasound Med. 2016;35:2459–65.
Lidegran MK, Mosskin M, Ringertz HG, Frenckner BP, Linden VB. Cranial CT for diagnosis of intracranial complications in adult and pediatric patients during ECMO: clinical benefits in diagnosis and treatment. Acad Radiol. 2007;14:62–71.
Said AS, Guilliams KP, Bembea MM. Neurological monitoring and complications of pediatric extracorporeal membrane oxygenation support. Pediatr Neurol. 2020;108:31–9.
LaRovere KL, Brett MS, Tasker RC, Strauss KJ, Burns JP. Head computed tomography scanning during pediatric neurocritical care: diagnostic yield and the utility of portable studies. Neurocrit Care. 2012;16:251–7.
Aboul Nour H, Poyiadji N, Mohamed G, et al. Challenges of acute phase neuroimaging in VA-ECMO, pitfalls and alternative imaging options. Interv Neuroradiol. 2021;27:434–9.
LaRovere KL, O’Brien NF. Transcranial doppler sonography in pediatric neurocritical care: a review of clinical applications and case illustrations in the pediatric intensive care unit. J Ultrasound Med Off J Am Instit Ultrasound Med. 2015;34:2121–32.
O’Brien NF, Hall MW. Extracorporeal membrane oxygenation and cerebral blood flow velocity in children. Pediatr Crit Care Med J Soc Crit Care Med World Federat Pediatr Intensive Crit Care Soc. 2013;14:e126–34.
Mattioni A, Cenciarelli S, Eusebi P, et al. Transcranial Doppler sonography for detecting stenosis or occlusion of intracranial arteries in people with acute ischaemic stroke. Cochrane Database Syst Rev. 2020;2:CD010722.
Burgin WS, Malkoff M, Felberg RA, et al. Transcranial doppler ultrasound criteria for recanalization after thrombolysis for middle cerebral artery stroke. Stroke J Cerebral Circulat. 2000;31:1128–32.
Bode H, Wais U. Age dependence of flow velocities in basal cerebral arteries. Arch Dis Child. 1988;63:606–11.
Hwang M, Haddad S, Tierradentro-Garcia LO, Alves CA, Taylor GA, Darge K. Current understanding and future potential applications of cerebral microvascular imaging in infants. Br J Radiol. 2022;95:20211051.
Barletta A, Balbi M, Surace A, et al. Cerebral superb microvascular imaging in preterm neonates: in vivo evaluation of thalamic, striatal, and extrastriatal angioarchitecture. Neuroradiology. 2021;63:1103–12.
Tierradentro-Garcia LO, Stern JA, Dennis R, Hwang M. Utility of cerebral microvascular imaging in infants undergoing ECMO. Children. 2022;9:1827.
Liem KD, Hopman JC, Oeseburg B, de Haan AF, Festen C, Kollee LA. Cerebral oxygenation and hemodynamics during induction of extracorporeal membrane oxygenation as investigated by near infrared spectrophotometry. Pediatrics. 1995;95:555–61.
Ejike JC, Schenkman KA, Seidel K, Ramamoorthy C, Roberts JS. Cerebral oxygenation in neonatal and pediatric patients during veno-arterial extracorporeal life support. Pediatr Crit Care Med J Soc Crit Care Med World Federat Pediatr Intensive Crit Care Soc. 2006;7:154–8.
Clair MP, Rambaud J, Flahault A, et al. Prognostic value of cerebral tissue oxygen saturation during neonatal extracorporeal membrane oxygenation. PLoS One. 2017;12:e0172991.
Tsou PY, Garcia AV, Yiu A, Vaidya DM, Bembea MM. Association of cerebral oximetry with outcomes after extracorporeal membrane oxygenation. Neurocrit Care. 2020;33:429–37.
Vedrenne-Cloquet M, Levy R, Chareyre J, et al. Association of cerebral oxymetry with short-term outcome in critically ill children undergoing extracorporeal membrane oxygenation. Neurocrit Care. 2021;35:409–17.
Papademetriou MD, Tachtsidis I, Elliot MJ, Hoskote A, Elwell CE. Multichannel near infrared spectroscopy indicates regional variations in cerebral autoregulation in infants supported on extracorporeal membrane oxygenation. J Biomed Opt. 2012;17:067008.
Joram N, Beqiri E, Pezzato S, et al. Continuous monitoring of cerebral autoregulation in children supported by extracorporeal membrane oxygenation: a pilot study. Neurocrit Care. 2021;34:935–45.
Foreman B, Claassen J. Quantitative EEG for the detection of brain ischemia. Crit Care. 2012;16:216.
Diedler J, Sykora M, Bast T, et al. Quantitative EEG correlates of low cerebral perfusion in severe stroke. Neurocrit Care. 2009;11:210–6.
Piantino JA, Wainwright MS, Grimason M, et al. Nonconvulsive seizures are common in children treated with extracorporeal cardiac life support. Pediatr Crit Care Med J Soc Crit Care Med World Federat Pediatr Intensive Crit Care Soc. 2013;14:601–9.
Al Naqeeb N, Edwards AD, Cowan FM, Azzopardi D. Assessment of neonatal encephalopathy by amplitude-integrated electroencephalography. Pediatrics. 1999;103:1263–71.
Dilena R, Raviglione F, Cantalupo G, et al. Consensus protocol for EEG and amplitude-integrated EEG assessment and monitoring in neonates. Clin Neurophysiol Off J Int Feder Clin Neurophysiol. 2021;132:886–903.
Shellhaas RA, Soaita AI, Clancy RR. Sensitivity of amplitude-integrated electroencephalography for neonatal seizure detection. Pediatrics. 2007;120:770–7.
ter Horst HJ, Sommer C, Bergman KA, Fock JM, van Weerden TW, Bos AF. Prognostic significance of amplitude-integrated EEG during the first 72 h after birth in severely asphyxiated neonates. Pediatr Res. 2004;55:1026–33.
Toet MC, Hellstrom-Westas L, Groenendaal F, Eken P, de Vries LS. Amplitude integrated EEG 3 and 6 h after birth in full term neonates with hypoxic-ischaemic encephalopathy. Arch Dis Child Fetal Neonatal Ed. 1999;81:F19–23.
van Laerhoven H, de Haan TR, Offringa M, Post B, van der Lee JH. Prognostic tests in term neonates with hypoxic-ischemic encephalopathy: a systematic review. Pediatrics. 2013;131:88–98.
Chahine A, Chenouard A, Joram N, Berthomieu L, Pont-Thibodeau GD, Leclere B, Liet J-M, Maminirina P, Leclair-Visonneau L, Breinig S, Bourgoin P. Continuous amplitude-integrated electroencephalography during neonatal and pediatric extracorporeal membrane oxygenation. J Clin Neurophysiol. 2021. https://doi.org/10.1097/WNP.0000000000000890.
Bembea MM, Felling RJ, Caprarola SD, et al. Neurologic outcomes in a two-center cohort of neonatal and pediatric patients supported on extracorporeal membrane oxygenation. ASAIO J 2019.
Bembea MM, Lee R, Masten D, et al. Magnitude of arterial carbon dioxide change at initiation of extracorporeal membrane oxygenation support is associated with survival. J Extra Corpor Technol. 2013;45:26–32.
Cavayas YA, Munshi L, Del Sorbo L, Fan E. The early change in PaCO2 after extracorporeal membrane oxygenation initiation is associated with neurological complications. Am J Respir Crit Care Med. 2020;201:1525–35.
Joram N, Rozé J-C, Tonna JE, et al. Association between early change in arterial carbon dioxide tension and outcomes in neonates treated by extracorporeal membrane oxygenation. ASAIO J. 2022. https://doi.org/10.1097/MAT.0000000000001838.
Strassmann S, Merten M, Schafer S, et al. Impact of sweep gas flow on extracorporeal CO(2) removal (ECCO(2)R). Intensive Care Med Exp. 2019;7:17.
Tanaka D, Shimada S, Mullin M, Kreitler K, Cavarocchi N, Hirose H. What is the optimal blood pressure on veno-arterial extracorporeal membrane oxygenation? Impact of mean arterial pressure on survival. ASAIO J. 2019;65:336–41.
Li G, Zeng J, Liu Z, Zhang Y, Fan X. The pulsatile modification improves hemodynamics and attenuates inflammatory responses in extracorporeal membrane oxygenation. J Inflamm Res. 2021;14:1357–64.
Cho SM, Wilcox C, Keller S, et al. Assessing the SAfety and FEasibility of bedside portable low-field brain magnetic resonance imaging in patients on ECMO (SAFE-MRI ECMO study): study protocol and first case series experience. Crit Care. 2022;26:119.
Funding
This work was supported by the funding from the National Institute of Neurological Disorders and Stroke of the National Institutes of Health under Award Number R01NS106292 (MMB).
Author information
Authors and Affiliations
Contributions
All listed authors have met the requirements for authorship, including the following: substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published; and agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no other conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Felling, R.J., Kamerkar, A., Friedman, M.L. et al. Neuromonitoring During ECMO Support in Children. Neurocrit Care 39, 701–713 (2023). https://doi.org/10.1007/s12028-023-01675-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-023-01675-8