Abstract
Extracorporeal membrane oxygenation (ECMO) is used to provide cardiac and/or pulmonary support in patients refractory to conventional therapies. It is increasingly used in various clinical acute settings and associated with cerebrovascular complications responsible for high morbidity and mortality.
Studies have shown alterations in cerebral blood flow (CBF) during ECMO support are potentially associated with neurological complications. Early detection of cerebral hemodynamics changes could improve patient’s prognosis, and various neuromonitoring tools are available to assess CBF during ECMO support. Transcranial Doppler (TCD) has numerous advantages, as it is a noninvasive procedure, available at bedside, and able to detect cerebral hemodynamic changes in real time and microembolism.
The aim of this chapter is to review literature concerning dynamic monitoring of CBF by TCD during ECMO and to give practical considerations.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Extracorporeal membrane oxygenation
- ECMO
- Cerebrovascular complications
- Cerebral blood flow
- Transcranial Doppler
-
1.
Nonpulsatile blood flow caused by the ECMO pump might affect cerebral autoregulation through the alteration of the myogenic response.
-
2.
The addition of an IABP influences CBF depending on the systolic antegrade blood flow by spontaneous cardiac function. It decreases CBF in patients with cardiac stun because of transient end-diastolic reversal of intracranial blood flow induced by this device.
-
3.
Too-rapid hypercapnia correction after VV ECMO cannulation might lead to cerebral vasoconstriction and cerebrovascular complications.
-
4.
No correlation has been made yet, neither between MES and ECMO flow rate nor between MES and neurological outcome.
-
5.
TCD/TCCS is a good tool to assess cerebral circulatory arrest during ECMO only in patients with an LVEF higher than 20%.
1 Introduction
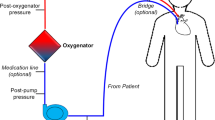
Extracorporeal membrane oxygenation (ECMO) is an emergency support procedure used to provide cardiac and/or pulmonary support in patient refractory to conventional therapies [1]. Over recent years, the number of patients treated with ECMO has increased [2, 3] and risk–benefit balance ratio has improved [3, 4]. ECMO circuit is either in a veno-venous (VV) configuration or in a veno-arterial (VA) configuration. It is associated to a centrifugal pump, which provides a continuous flow in the circuit, and to a membrane oxygenator. VV ECMO is used in acute respiratory distress syndrome (ARDS), and VA ECMO in refractory cardiogenic shock and cardiac arrest.
In VA ECMO, the circuit includes an inflow cannula, which drains blood from the venous system, and an outflow cannula, which delivers the warmed oxygenated blood back into the arterial system in order to restore a circulatory flow [5]. It is used for refractory cardiac dysfunction, regardless of the underlying cardiac pathology (myocarditis, cardiomyopathy, postcardiotomy heart failure, primary graft failure after heart transplantation, ventricular dysfunction in patients with acute coronary syndrome, acute intoxications due to cardiotropic drugs, cardiac arrest) [5]. Intra-aortic balloon pump (IABP) is often added in those patients to protect against hydrostatic pulmonary edema [6], or to improve coronary bypass graft flows and cardiac function in refractory postoperative cardiogenic shock [7, 8]. It reduces left ventricular afterload, improves coronary perfusion, and provides a pulsatile blood flow [9, 10].
In VV ECMO, the outflow cannula delivers oxygenated and decarboxylated blood to the vena cava and the right atrium. The aim of this configuration is to insure a normal blood gas exchange during ARDS refractory to conventional therapy [5, 11].
The Extracorporeal Life Support Organization (ELSO) collects data since 2002 from 359 centers managing with ECMO worldwide [12]. ELSO reported overall outcomes in 2018 in 35,632 adult patients, among which 15,686 were VV ECMO with a survival rate of 66% and 15,201 were VA ECMO with a survival rate of 55%; there were also 4745 extracorporeal cardiopulmonary resuscitation with a survival rate of 38% [12]. These data show that survival rate is higher in VV than in VA ECMO.
Use of ECMO is associated with several cerebrovascular complications (anoxic cerebral injury, ischemic stroke and cerebral hemorrhage, epileptic seizures, coma and brain death) [13,14,15], responsible for high morbidity and mortality [13, 16]. Many pre-ECMO factors are associated with neurological injury, but during the course of ECMO, the modality used is also diversely associated to nervous system complication. Stroke occurs mainly during VA ECMO [15], whereas cerebral hemorrhage is mostly observed during VV ECMO [14, 17]. These complications have an important impact in terms of outcome, and consequently on multidisciplinary team decisions.
It is likely that both VA and VV ECMO affect cerebral blood flow (CBF) and impact cerebral hemodynamics, resulting in neurological impairment [15, 17,18,19,20]. IABP might also play a role in CBF modification in patients with cardiac failure [10]. Early detection and specific care for neurological complications could improve the prognosis of these patients. Indeed, because of the critical condition of those patients and the use of deep sedation and anesthesia, it can be difficult to diagnose a neurological event under ECMO. Moreover, those neurological complications may be underestimated because of the difficulty to transfer these patients to other wards and to perform neuroimaging examinations.
As transcranial Doppler (TCD)/transcranial color-coded duplex sonography (TCCS) is a noninvasive monitoring procedure able to detect cerebral hemodynamic changes in real-time, microembolism, and has been used extensively in neurological and neurosurgical patients to monitor CBF velocities, there is an increasing literature about its usefulness in ECMO patients to detect as soon as possible ECMO-related cerebrovascular complication.
The aim of this chapter is to review literature concerning dynamic monitoring of CBF by TCD during ECMO and to give practical considerations.
2 Cerebral Hemodynamics
2.1 Physiological Mechanisms
The three processes responsible of cerebral hemodynamics regulation are the cerebrovascular responses to: (1) brain metabolism, called neurovascular coupling; (2) autonomic neurogenic regulation; and (3) changes in cerebral perfusion pressure (CPP), called cerebral autoregulation (CA).
Neurovascular coupling aim is to increase the CBF in response to regional or global brain metabolic demands. This metabolic regulation is effected by vasoactive mediators concentration changes in the perineuronal space such as CO2, O2, lactate, NO, K+, Ca2+, H+, and adenosine [21,22,23,24].
Neurogenic regulation of the vascular tone is triggered by perivascular sympathetic and cholinergic nerves that originate from peripheral nerve ganglia and intrinsic brain neurons [25]. This mechanism depends on autonomic nervous system reactivity and, for example, plays an important role in the pathophysiology of the migraine [26].
CA is the ability of cerebral arterioles to maintain stable CBF while mean arterial blood pressure (MAP) and CPP vary [27]. The CPP is defined as the difference between the MAP and the intracranial pressure, which is the pressure of the cerebrospinal fluid in the subarachnoid space. The constant CBF is obtained by vasodilation and vasoconstriction of cerebral arterioles. This mechanism allows to maintain proper brain perfusion and to supply the brain with the necessary oxygen and energy substrates under physiological and pathological conditions. Indeed, changes in perfusion pressure occur under normal conditions, as exercise or during a change in posture, or may result from pathological conditions such as subarachnoid hemorrhage (SAH), traumatic brain injury, stroke, or drugs administration. The myogenic response observed in CA process is the intrinsic ability of small arteries and pial arterioles smooth muscle cells to respond to changes in transmural vascular pressure resulting from MAP or CPP modification. This innate myogenic mechanism is not regulated by the autonomic nervous system. It is responsible for myogenic tone and subsequently cerebral vascular resistance.
Segmental and regional heterogeneity within the brain can result in varying levels of CBF in different regions of the brain, over the same range of CPP [28].
In pathological conditions, cerebral hemodynamics may become dysfunctional. Several disease states resulting in impaired CA are known, such as traumatic brain injury [29, 30], ischemic stroke [31, 32], intracerebral hemorrhage [33, 34], and subarachnoid hemorrhage [35, 36].
2.2 Regulation During ECMO
In adult patients, there is limited literature about CA impairment during ECMO.
Although pre-ECMO factors, such as hypoxia, hypercapnia, hypoperfusion, or hypertension, can disrupt systemic blood flow regulation, leaving the brain vulnerable to changes in blood pressure [37], it has been shown that cannulation of great blood vessels and alterations of pulsatile flow during the course of ECMO also affect CA [38, 39]. Most of those studies have been done in pediatric patients and have used near infrared spectrophotometry (NIRS) to assess this impairment. Thus, both pre- and ECMO factors may contribute to cerebrovascular complications commonly seen in ECMO.
2.2.1 VA ECMO
Various factors can alter CBF during ECMO. One of the main hypotheses is that the laminar blood flow caused by the ECMO pump affects CA through the myogenic response. The effect of nonpulsatile flow on the brain has been of concern first in cardiopulmonary bypass (CPB). An experimental animal study in the 1980s compared pulsatile and nonpulsatile bypass in a canine stroke model and found that pulsatile flow increased CBF significantly over nonpulsatile flow, showing the importance of pulsatile blood flow in ischemic brain disease [40]. In adult patients undergoing CPB, the mean lower limit of autoregulation, under which a drop in CPP results in a loss of CBF, has been found to be the MAP at 66 mmHg [41], but instead of targeting a specific MAP, CA monitoring using cerebral oximetry index to individualize optimal blood pressure is widely used to prevent neuronal injury [42].
During VA ECMO, CA has been evaluated in the early 1990s in newborn lambs [43]. Nonpulsatile roller-pump were used in this work. CA was evaluated during the course of ECMO by lowering the CPP via an increase in intracranial pressure through infusion of artificial cerebrospinal fluid into the lateral ventricle. CA was found to be impaired in lamb on VA ECMO (flow rates of 120–150 mL/kg/min) compared to control animals with right jugular vein and carotid artery ligation.
Multiple studies using NIRS and neuroimaging have shown abnormal CA in infants undergoing VA ECMO [20, 44, 45], but those studies are lacking in adult patients. Indeed, in neonates, the outflow arterial cannulation site can be the carotid artery, which can itself impact on CBF, whereas outflow arterial cannulation site in adult is often the femoral artery. However, when the outflow arterial cannula is the femoral artery, clinicians fear that the brain receives hypoxemic and undercarboxylated blood ejected from a residual activity of the left ventricle, in patient with poor lung function. This upper body differential hypoxemia defined as “Harlequin syndrome” [46] is usually detected by the monitoring of oxygen saturation within the right upper limb and could also impact CA.
The addition of an IABP in conjunction with VA ECMO to protect against hydrostatic pulmonary edema [6], or to improve coronary bypass graft flows and cardiac function in refractory postoperative cardiogenic shock [7, 8, 47], has also been shown to modify cerebral hemodynamics. Indeed, one study has shown, in patients with refractory cardiogenic shock after cardiac surgery requiring VA ECMO, that the addition of an IABP influences CBF depending on the systolic antegrade blood flow by spontaneous cardiac function. In this study, the addition of an IABP to VA ECMO support decreased the CBF in patients with cardiac stun, and it increased CBF in patients without cardiac stun [48].
2.2.2 VV ECMO
The main metabolic factors known to cause significant changes in CBF are PaCO2 and pH. These parameters can rapidly change during VV ECMO [49]. Intracranial bleeding is the most frequent cerebrovascular complication during VV ECMO, and it has been found that a decrease in PaCO2 after ECMO cannulation was independently associated with this complication [17]. However, because rapid decrease in PaCO2 leads to cerebral vasoconstriction, the relationship between PaCO2 change and cerebral bleeding is difficult to understand. One hypothesis could be that those cerebral bleeding was in fact secondary hemorrhagic transformation after cerebral infarction due to a cerebral vasoconstriction induced by VV ECMO.
Another factor that could impair cerebral hemodynamic during VV ECMO is the internal jugular vein occlusion due to the inflow cannula, which can cause cerebral venous hypertension, resulting in a decreased CBF within the first hours of cannulation, as it has been described in newborn [50]. In those studies, this effect tends to disappear after 24 h of VV ECMO, with normalization of the CBF [50, 51].
We can see that various factors can alter CBF during both VA and VV ECMO, and noninvasive monitoring procedures able to detect those cerebral hemodynamic changes in real time might be useful in everyday medical practice.
3 Transcranial Doppler Monitoring
TCD/TCCS is the reference tool to monitor CBF velocities. It is broadly used by neurointensivists. Briefly, it emits pulse wave ultrasounds that penetrate brain parenchyma and are reflected back after being scattered by circulating red blood cells. The frequency of this echo is then proportional to red blood cells velocity. Measurement of the pulsatility index (PI) (calculated as systolic velocity – diastolic velocity)/mean velocity), which reflects vascular resistance, is then performed to evaluate cerebral blood. In physiological condition, PIs ranges approximately from 0.8 to 1.4 depending on patient’s age.
Studies looking at TCD/TCCS on adult patients treated with ECMO are very limited in literature. However, this tool can be useful to assess CA during ECMO and has numerous advantages compared to other modalities, as it is a noninvasive technique, available at bedside, and repeatable without any risk of radiation.
3.1 VA ECMO
In 2016, a study in eight VA ECMO patients without IABP, implanted for cardiogenic shock or cardiac arrest, has shown a correlation between lowering of PIs and left ventricular ejection fraction (LVEF) [19]. Indeed, as the heart systolic function gives rise to the upstroke observed on TCDs, patients with a severely reduced LVEF displayed lower or noncomputable PIs. In this study, an ejection fraction (EF) of less than 10% resulted in a nonpulsatile TCD waveform. Moreover, in those patients, the measurement of the diastolic phase during TCD for calculation of PIs corresponded to the nonpulsatile flow generated by the ECMO circuit. In an expected manner, when the EF increased during recovery or following placement of total artificial heart and ECMO decannulation, the systolic upstroke increases in amplitude, resulting in higher PIs values, and returns to normal. This study shows that low or noncomputable PIs and lack of systolic upstroke should not be mistaken with cerebral vasodilation in VA ECMO patients with laminar flow, and that rising of their PIs during the course of ECMO can be related to a cardiac recovery. However, focal or asymmetrical PIs modifications still suggest changes of vascular resistance and should evoke cerebrovascular disease [52, 53].
As IABP is increasingly used in addition to VA ECMO to improve coronary bypass graft flows and cardiac function, and protects against hydrostatic pulmonary edema in critically ill patients [6,7,8], some studies have evaluated the impact of this combination on CBF. As a reminder, the effect of IABP alone on CBF is controversial, and there are some examples of contradictions in literature. For example, a study in patients with IABP support alone after cardiac surgery found that this device caused a small but significant increase in systolic antegrade mean flow velocity in the middle cerebral artery, but because 30% of those patients displayed transient end-diastolic reversal of intracranial blood flow induced by this device, the resulting average flow velocity was not influenced by the IABP [54]. An older study has also shown in 56 patients on IABP assistance alone a reduction of 11.6% in the ocular blood flow measured by ocular pneumoplethysmography [55].
However, the effect of the combination of VA ECMO and IABP on the CBF is not well known. Only one prospective study has investigated with TCD the effect of IABP in addition to VA ECMO on the CBF, analyzing the blood flow of the bilateral middle cerebral arteries [48].
In this work, 12 adult patients receiving VA ECMO and IABP support for refractory postcardiotomy cardiogenic shock after coronary artery bypass were analyzed. The IABP was implanted before VA ECMO. The CBF velocity were measured once every 12 h, under “turned on” IABP and “turned off” IABP support. Patients provided their own control values through the “turned off” IABP condition. All 12 patients were successfully weaned from the IABP and VA ECMO, 8 patients were able to be discharged from the hospital, and survival rate was 66.7%. Cerebrovascular complications were not observed in this study. Concerning their CBF, no statistically significant differences for the mean CBFs were observed between VA ECMO alone and VA ECMO with IABP support, but the authors divided patients into two groups, considering their cardiac functional state and their basal pulsatile pressure without IABP support. Their conclusions were that the addition of an IABP to VA ECMO significantly decreased the mean CBF in patients with basal pulsatile pressure under 10 mmHg and led to a significant increase in the mean CBF values in patients with basal pulsatile pressure higher than 10 mmHg. The CBF decrease in cardiac-stunned patient with VA ECMO and IABP seems to be due to the diastolic inflation of the IABP, which might intermittently compromise the retrograde flow, as it has been described in patients with cardiogenic shock and IABP alone [54].
Finally, in a recent retrospective study performed in 20 VA ECMO patients implanted for cardiogenic shock and/or cardiac arrest, 4 different TCD/TCCS waveform were correlated to LVEF values and IABP support [56]: (1) double systolic peak pattern in patients with both cardiac systole and IABP waves detectable; (2) Normal waveform pattern in patient with detectable cardiac systole wave with no IABP or IABP turned off; (3) systolic IABP peak into a continuous demodulate waveform pattern in patient with undetectable cardiac systolic wave; (4) continuous and nonpulsatile flow corresponding to VA ECMO flow in patient without detectable cardiac systole and no IABP, or IABP turned off. In that study, cardiac systolic peaks could be detected by TCD/TCSS when LVEF was above 20%.
Figure 48.1 shows patterns of TCD/TCCS waveforms of VA ECMO with IABP from our center.
3.2 VV ECMO
Concerning VV ECMO , a pediatric study [51] has shown in 19 newborns infants, among which 1 developed intracranial hemorrhage, that, except in this case of cerebral hemorrhage where the velocity in each of the cerebral arteries was higher compared with cases without cerebral complications, the CBF was either maintained or gradually increased before and during ECMO. Because most of these newborns were treated with double-lumen cannula, introduced into the right internal jugular vein, CBF trends to decrease within the first hours of cannulation, probably because of a transitory cerebral venous hypertension [50]. As described before, this effect trends to disappeared in the first day of VV ECMO, with normalization of the CBF.
Patterns of TCD waveforms of VA ECMO and VA ECMO with IABP patients, depending on their LVEF. Patient with LVEF of 30% and PP of 20 mmHg with VA ECMO and IABP. TCD monitoring of the right proximal segment of the middle cerebral artery of the right median cerebral artery showing (a) IABP off: Detectable cardiac systolic peak within a continuous demodulate waveform pattern. (b) IABP on: Double systolic peak corresponding to cardiac systole and IABP peak. ECMO extracorporeal membrane oxygenation, VA veno-arterial, LVEF left ventricular ejection fraction, PP pulsatile pressure, IABP intra-aortic balloon pump
4 TCD/TCCS: Cerebrovascular Complications During ECMO
ECMO use is associated with cerebrovascular diseases. In this paragraph, we focus on ischemic stroke and cerebral hemorrhage during ECMO and the contribution of TCD/TCCS in their early detection and specific care. We also discuss about brain death, even if this complication is mainly due to pre-ECMO factors, because of the specific management of brain-dead donor supported by this device, and the potential usefulness of TCD/TCCS in this particular situation. Algorithm resumes TCD/TCCS patterns depending on ECMO type.
4.1 Ischemic Stroke
4.1.1 VA ECMO
Ischemic strokes are more commonly observed in VA ECMO patients [15]. In 2016, a series of 137 patients with VA ECMO reported its incidence, diagnosed by brain imaging, at 10% [57]. However, this number was estimated at 50% in a 2006 study in which a cerebral magnetic resonance imaging (MRI) was performed systematically during the longitudinal follow-up of survivors, with median follow-up at 5 years [15]. Finally, in a study of 84 patients undergoing VA ECMO, where a brain autopsy was performed in 25% of non-survivors (10 patients), ischemic brain lesions were found in 70% of them, although neurological disorder was not notified during their stay [13].
Regarding the risk factors for ischemic stroke, a recent study of 171 patients including 80% of VA ECMO reported that a lactate level >10 mmol/L before ECMO cannulation was an independent risk factor of their occurrence [58].
4.1.2 VV ECMO
Ischemic stroke is less common in patients with VV ECMO compared to VA ECMO. The largest cohort that investigates neurological complications in patients undergoing VV ECMO has reported its incidence at 2% [17]. In this study, ischemic strokes occurred after a median of 21 days after ECMO implantation [17].
In 2006, a study in which a brain MRI was performed in survivors, no ischemic injury was found [15]. Studies with brain autopsy of patients undergoing VV ECMO have not been published so far.
4.1.3 Pathophysiological Mechanisms and TCD/TCCS Contribution
Mechanisms responsible for ischemic strokes are most likely to be different depending on the ECMO type. Regarding the mechanism of ischemic injury in patients undergoing VA ECMO, no study has analyzed their origin, but considering that these patients are more prone to ischemic stroke because of their underlying heart disease that motivates ECMO cannulation, the main cause seems to be cardioembolic stroke.
The role of the ECMO circuit itself in those strokes remains unclear, but it is likely that, regardless of the underlying disease, the presence of an ECMO may itself be a source of embolism. Indeed, the shear stress imposed by the flow pump generates an increased platelet activation, which causes their aggregation [59]. This is particularly observed with centrifugal pumps, widely used nowadays because of a decreased hemolysis compared to old roller-pump systems [59].
Another mechanism that can explain the high frequency of ischemic stroke in VA ECMO patients is cerebral hypoperfusion during initial cardiogenic shock. In this situation, cerebral infarctions have a particular topography, called “watershed cerebral infarction,” also known as “border zone infarcts,” because they occurred at the border between cerebral vascular territories where the tissue is farthest from arterial supply, and thus most vulnerable to reductions in perfusion. They are observed at the level of anastomoses between the different cerebral arterial territories, anterior, middle, and posterior.
For patients under VV ECMO, stroke physiopathology is less obvious than for VA ECMO. A mechanism involving a paradoxical embolism, responsible for 2% of ischemic strokes [60], could be evoked during VV ECMO, especially in ARDS patients with elevation of right atrial pressures induced by ultraprotective mechanical ventilation and high level of positive end-expiratory pressure, responsible for a reopening of their foramen ovale, and therefore, a higher risk of venous thromboembolism toward the arterial circulation. Finally, too-rapid correction of hypercapnia can result in respiratory alkalemia in these patients and may be responsible for cerebrovascular vasoconstriction and reduction in CBF that may cause ischemic injury [61].
TCD/TCCS can be used to identifying vessel occlusions and to monitor stroke response to treatment [62]. It is also used for microembolic signals (MES) detection [63]. MES are high-intensity transient signals detected by TCD/TCCS and have been shown to correspond to microemboli made of air, platelet, fibrinogen, or atheromatous material [63]. Their detection is correlated with recurrent ischemic stroke in patient with acute cerebral infarction [64]. They are also used as predictors of cerebral events in patients with symptomatic and asymptomatic carotid disease [65].
As cerebral infarctions might be caused by microemboli created in the arterial line during the ECMO support, studies have investigated if TCD/TCCS can aid in detecting microemboli arising from the ECMO circuit [66, 67]. In a 2010 study, six VA ECMO patients were evaluated for MES [66]. Among them, four had refractory postcardiotomy cardiogenic shock, and two were implanted because of cardiac arrest. All patients were assisted with IABP and with continuous renal replacement therapy. The authors reported a correlation between MES count and high flow rate of ECMO support (≥4 l/min). In 2016, a largest study in 55 patients with VA, VV ECMO, and extracorporeal CO2 removal (ECCO2R) had been performed and investigated if MES could be correlated to neurological outcome [67]. In this study, MES count was higher in VA ECMO patient than other, but no correlation was made, neither between MES and ECMO flow rate nor between MES and neurological outcome.
4.2 Intracerebral Hemorrhage
It is important to note that it can be difficult to distinguish between primary cerebral hemorrhage and secondary hemorrhagic transformation after cerebral infarction, which is correlated with the size of cerebral infarction [68].
4.2.1 VA ECMO
In 2013, the ELSO registry reported a rate of intracranial hemorrhage of 2% in patients undergoing VA ECMO. In 1999, a retrospective study searching for risk factors of cerebral hemorrhage during VA ECMO reported that neither the underlying disease nor the site of cannulation was associated with an increased risk of cerebral hemorrhage, as well as MAP, ECMO flow rate, or ECMO duration [69]. In addition, there was no evidence of a link between high activated clotting time (ACT) or low prothrombin time (PTT) and intracranial hemorrhage. In contrast, thrombocytopenia <50,000/mm3 was an independent risk factor associated with a high risk of cerebral hemorrhage. Acute renal failure and hemodialysis were also associated with risk of intracranial bleeding. Unexpectedly, female sex was an independent risk factor for cerebral hemorrhage [69].
4.2.2 VV ECMO
In 2013, the ELSO registry reported a higher rate of HIC in patients under VV ECMO at 4% [14], and this number was up to 15% in a recent study with 25 patients [70]. The largest series specifically dealing with cerebrovascular complications in VV ECMO reported a rate of brain bleeding of 7.5% [17]. In this study, the average duration of onset of cerebral bleeding was 3 days after VV ECMO implantation. Intracranial hemorrhage was independently associated with acute renal failure upon admission to intensive care, too-rapid correction of PaCO2 upon VV ECMO initiation, and was not associated with patient’s age or hemostasis disorders.
4.2.3 Pathophysiological Mechanisms and TCD/TCCS Contribution
In the same way as for ischemic stroke, it is likely that pathophysiological mechanisms causing brain bleeding are different depending on the type of ECMO.
In VA ECMO patients, sudden restoration of brain flow could lead to intracranial edema, equivalent to a cerebral hyperperfusion syndrome, leading to hemorrhagic transformation, particularly in patients with previous ischemic stroke, by analogy with what is observed in patients undergoing carotid endarterectomy [71].
For VV ECMO, rapid correction of hypercapnia is an independent factor of the occurrence of cerebral hemorrhage [17]. Cerebral vasoconstriction induced by this too-rapid decline in PaCO2 at the initiation of VV ECMO could be responsible for cerebral edema, with initial ischemic lesions evolving rapidly to and hemorrhagic transformation [61].
No study has yet investigated the usefulness of TCD/TCCS to prevent and monitor intracranial hemorrhage during VA or VV ECMO.
4.3 Brain Death During ECMO
Brain death is in 84% of cases directly related to pre-ECMO factors and cerebral edema secondary to cardiac arrest in ECMO patients [72]. Other causes are represented by ischemic strokes or intracranial bleeding occurring during ECMO support, representing respectively 4% and 12% of brain death during ECMO [72]. Patients on ECMO, and particularly patients implanted for refractory cardiac arrest, are increasingly regarded as potential organ donors, but high plasma levels of sedative drugs and hypothermia in those critically ill patients can make electroencephalogram examination unreliable and can delay brain death confirmation of brain death, as well as neurovascular imaging, because of the difficulty to transport these patients to radiology. TCD/TCCS could overcome all these limitations. To confirm a cerebral circulatory arrest with TCD/TCCS, several patterns are mandatory as a reverberating flow, systolic spikes, and absence of signal, while mean flow velocity value detection is not required [73].
In 2018, a retrospective analysis has been performed in 25 patients (20 VA ECMO and 5 CPB) to evaluate the feasibility of cerebral circulatory arrest diagnosis by TCD during the circulatory support [56]. Indeed, TCD/TCCS is a worldwide accepted technique for cerebral circulatory arrest diagnosis for brain death confirmation [74]. In that study, brain death occurred in five patients. Those patients with VA ECMO were either assisted with IABP or had a LVEF higher than 20%. TCD/TCCS brain death patterns were found in all five patients. The lack of brain dead patients without IABP or with very low cardiac output in this study is highlighted by their authors as a major limitation to conclude whether TCD/TCCS can be used to confirm cerebral circulatory arrest in patients with laminar , nonpulsatile arterial flow.
5 Practical Considerations and Limitations
The specific management of these cerebrovascular complications remains the same as that of brain-damaged patients [75]. However, the evolution of patients on ECMO support during their stay in intensive care unit includes events that impose several constraints, for example, on patient’s coagulation and oxygenation state, thus limiting specific therapeutic possibilities of these cerebrovascular complications. Even if TCD/TCCS is a practical tool to be informed about cerebral hemodynamics state in patients on ECMO support, the therapeutic impact of TCD/TCCS monitoring can be limited due to the many restrictions imposed by this circulatory device. Indeed, the heterogeneity of patients under ECMO requires individualized therapeutic strategies concerning ECMO flow rate or IABP use, which can rely on extra-neurological failures.
In the following paragraphs, we will exemplify two situations where TCD/TCCS findings should not be followed by circulatory device support parameter changes.
5.1 VA ECMO
As said previously, IABP is often added to VA ECMO, particularly in nonpulsatile patient with very low LVEF, in order to off-load the left ventricle and to protect against hydrostatic pulmonary edema [6]. TCD/TCCS has shown that in this subpopulation, IABP activation decreases CBF due to a transient end-diastolic reversal of intracranial blood flow during the diastolic inflation of the IABP [48]. Common sense should therefore avoid this device in patient with cardiac stun, but without an IABP, the probability that those VA ECMO patients develop severe hydrostatic pulmonary edema and ARDS is high. During the cardiac recovery process on ECMO, the heart might eject desaturated blood from the left ventricle, and evolve toward an “Harlequin syndrome” [46] which is deleterious for the brain, and might be responsible for hypoxic-ischemic encephalopathy.
Therefore, IABP should be added in those VA ECMO patients with cardiac stun, even if TCD/TCCS finds a reduction in CBF.
5.2 VV ECMO
Some severe ARDS patients develop severe hypercapnia with respiratory acidosis and consequently, display cerebral vasodilatation patterns and a decreased CBF on TCD/TCCS monitoring [76]. After VV ECMO cannulation of these patients, common sense would tend to restore a normal PaCO2 in order to restore a physiological pH and a normal CBF, but as told previously, intracranial bleeding is the most frequent cerebrovascular complication during VV ECMO, associated with rapid hypercapnia correction due to too-high extracorporeal gas flow on the circuit after cannulation [17].
Therefore, hypercapnia after cannulation should be respected within the first hours of VV ECMO, even if TCD/TCCS shows a vasodilatation pattern with a decreased CBF.
6 Conclusion
TCD/TCCS studies of patient undergoing ECMO are mandatory, and due to the lack of evidence regarding its usefulness during this circulatory report, it is not yet recommended as a regular and systematic monitoring tool during the follow-up of those patients for early detection or specific care of ECMO-induced neurological complications.
However, TCD/TCCS can represent a useful bedside tool to detect cerebral hemodynamic changes in real time in sedated and critically ill patients, in which clinical examination can hardly diagnose a neurological complication. Indeed, some medical centers, as “Baylor St. Luke’s Medical Center” in Houston (Texas, USA), have established a neuromonitoring protocol for patients on ECMO support, in which daily TCD/TCCS are performed [77].
References
Davies A, et al. Extracorporeal membrane oxygenation for 2009 influenza A(H1N1) acute respiratory distress syndrome. JAMA. 2009;302(17):1888–95.
Luyt CE, et al. Long-term outcomes of pandemic 2009 influenza A(H1N1)-associated severe ARDS. Chest. 2012;142(3):583–92.
Combes A, et al. Position paper for the organization of extracorporeal membrane oxygenation programs for acute respiratory failure in adult patients. Am J Respir Crit Care Med. 2014;190(5):488–96.
Abrams D, et al. Position paper for the organization of ECMO programs for cardiac failure in adults. Intensive Care Med. 2018;44(6):717–29.
Marasco SF, et al. Review of ECMO (extra corporeal membrane oxygenation) support in critically ill adult patients. Heart Lung Circ. 2008;17(Suppl 4):S41–7.
Brechot N, et al. Intra-aortic balloon pump protects against hydrostatic pulmonary oedema during peripheral venoarterial-extracorporeal membrane oxygenation. Eur Heart J Acute Cardiovasc Care. 2018;7(1):62–9.
Madershahian N, et al. The acute effect of IABP-induced pulsatility on coronary vascular resistance and graft flow in critical ill patients during ECMO. J Cardiovasc Surg. 2011;52(3):411–8.
Madershahian N, et al. The impact of intraaortic balloon counterpulsation on bypass graft flow in patients with peripheral ECMO. J Card Surg. 2009;24(3):265–8.
Ma P, et al. Combining ECMO with IABP for the treatment of critically ill adult heart failure patients. Heart Lung Circ. 2014;23(4):363–8.
Chung ES, et al. Results of extracorporeal membrane oxygenation (ECMO) support before coronary reperfusion in cardiogenic shock with acute myocardial infarction. Korean J Thorac Cardiovasc Surg. 2011;44(4):273–8.
Combes A, et al. Extracorporeal membrane oxygenation for severe acute respiratory distress syndrome. N Engl J Med. 2018;378(21):1965–75.
Extracorporeal Life Support Organization. Registry report for all ECLS cases.
Mateen FJ, et al. Neurological injury in adults treated with extracorporeal membrane oxygenation. Arch Neurol. 2011;68(12):1543–9.
Mehta A, Ibsen LM. Neurologic complications and neurodevelopmental outcome with extracorporeal life support. World J Crit Care Med. 2013;2(4):40–7.
Risnes I, et al. Cerebral outcome in adult patients treated with extracorporeal membrane oxygenation. Ann Thorac Surg. 2006;81(4):1401–6.
Lewandowski K, et al. High survival rate in 122 ARDS patients managed according to a clinical algorithm including extracorporeal membrane oxygenation. Intensive Care Med. 1997;23(8):819–35.
Luyt CE, et al. Brain injury during venovenous extracorporeal membrane oxygenation. Intensive Care Med. 2016;23:23.
O’Brien NF, Hall MW. Extracorporeal membrane oxygenation and cerebral blood flow velocity in children. Pediatr Crit Care Med. 2013;14(3):e126–34.
Kavi T, et al. Transcranial Doppler changes in patients treated with extracorporeal membrane oxygenation. J Stroke Cerebrovasc Dis. 2016;25(12):2882–5.
Papademetriou MD, et al. Multichannel near infrared spectroscopy indicates regional variations in cerebral autoregulation in infants supported on extracorporeal membrane oxygenation. J Biomed Opt. 2012;17(6):067008.
Lassen NA, Christensen MS. Physiology of cerebral blood flow. Br J Anaesth. 1976;48(8):719–34.
Kuschinsky W, Wahl M. Local chemical and neurogenic regulation of cerebral vascular resistance. Physiol Rev. 1978;58(3):656–89.
Winn HR, et al. Brain adenosine production in rat during sustained alteration in systemic blood pressure. Am J Phys. 1980;239(5):H636–41.
Wei EP, Kontos HA. Increased venous pressure causes myogenic constriction of cerebral arterioles during local hyperoxia. Circ Res. 1984;55(2):249–52.
Hamel E. Perivascular nerves and the regulation of cerebrovascular tone. J Appl Physiol (1985). 2006;100(3):1059–64.
Waeber C, Moskowitz MA. Migraine as an inflammatory disorder. Neurology. 2005;64(10 Suppl 2):S9–15.
McHenry LC, et al. Cerebral autoregulation in man. Stroke. 1974;5(6):695–706.
Faraci FM, Mayhan WG, Heistad DD. Segmental vascular responses to acute hypertension in cerebrum and brain stem. Am J Phys. 1987;252(4 Pt 2):H738–42.
Bouma GJ, et al. Blood pressure and intracranial pressure-volume dynamics in severe head injury: relationship with cerebral blood flow. J Neurosurg. 1992;77(1):15–9.
Czosnyka M, et al. Cerebral autoregulation following head injury. J Neurosurg. 2001;95(5):756–63.
Powers WJ, et al. Autoregulation after ischaemic stroke. J Hypertens. 2009;27(11):2218–22.
Panerai RB, et al. Dynamic cerebral autoregulation following acute ischaemic stroke: comparison of transcranial Doppler and magnetic resonance imaging techniques. J Cereb Blood Flow Metab. 2016;36(12):2194–202.
Oeinck M, et al. Dynamic cerebral autoregulation in acute intracerebral hemorrhage. Stroke. 2013;44(10):2722–8.
Ma H, et al. Temporal course of dynamic cerebral autoregulation in patients with intracerebral hemorrhage. Stroke. 2016;47(3):674–81.
Budohoski KP, et al. Impairment of cerebral autoregulation predicts delayed cerebral ischemia after subarachnoid hemorrhage: a prospective observational study. Stroke. 2012;43(12):3230–7.
Otite F, et al. Impaired cerebral autoregulation is associated with vasospasm and delayed cerebral ischemia in subarachnoid hemorrhage. Stroke. 2014;45(3):677–82.
Short BL. The effect of extracorporeal life support on the brain: a focus on ECMO. Semin Perinatol. 2005;29(1):45–50.
Liem KD, et al. Cerebral oxygenation and hemodynamics during induction of extracorporeal membrane oxygenation as investigated by near infrared spectrophotometry. Pediatrics. 1995;95(4):555–61.
Fenik JC, Rais-Bahrami K. Neonatal cerebral oximetry monitoring during ECMO cannulation. J Perinatol. 2009;29(5):376–81.
Tranmer BI, et al. Pulsatile versus nonpulsatile blood flow in the treatment of acute cerebral ischemia. Neurosurgery. 1986;19(5):724–31.
Joshi B, et al. Predicting the limits of cerebral autoregulation during cardiopulmonary bypass. Anesth Analg. 2012;114(3):503–10.
Hori D, et al. Hypotension after cardiac operations based on autoregulation monitoring leads to brain cellular injury. Ann Thorac Surg. 2015;100(2):487–93.
Short BL, et al. Impairment of cerebral autoregulation during extracorporeal membrane oxygenation in newborn lambs. Pediatr Res. 1993;33(3):289–94.
Tian F, et al. Impairment of cerebral autoregulation in pediatric extracorporeal membrane oxygenation associated with neuroimaging abnormalities. Neurophotonics. 2017;4(4):041410.
Tian F, et al. Wavelet coherence analysis of dynamic cerebral autoregulation in neonatal hypoxic-ischemic encephalopathy. Neuroimage Clin. 2016;11:124–32.
Cakici M, et al. Controlled flow diversion in hybrid venoarterial-venous extracorporeal membrane oxygenation. Interact Cardiovasc Thorac Surg. 2018;26(1):112–8.
Doll N, et al. Five-year results of 219 consecutive patients treated with extracorporeal membrane oxygenation for refractory postoperative cardiogenic shock. Ann Thorac Surg. 2004;77(1):151–7. discussion 157
Yang F, et al. Effects of intra-aortic balloon pump on cerebral blood flow during peripheral venoarterial extracorporeal membrane oxygenation support. J Transl Med. 2014;12:106.
Meng L, Gelb AW. Regulation of cerebral autoregulation by carbon dioxide. Anesthesiology. 2015;122(1):196–205.
Weber TR, Kountzman B. The effects of venous occlusion on cerebral blood flow characteristics during ECMO. J Pediatr Surg. 1996;31(8):1124–7.
Fukuda S, et al. Comparison of venoarterial versus venovenous access in the cerebral circulation of newborns undergoing extracorporeal membrane oxygenation. Pediatr Surg Int. 1999;15(2):78–84.
Taylor GA, et al. Intracranial flow patterns in infants undergoing extracorporeal membrane oxygenation: preliminary observations with Doppler US. Radiology. 1987;165(3):671–4.
van de Bor M, et al. Extracorporeal membrane oxygenation and cerebral blood flow velocity in newborn infants. Crit Care Med. 1990;18(1):10–3.
Schachtrupp A, et al. Influence of intra-aortic balloon pumping on cerebral blood flow pattern in patients after cardiac surgery. Eur J Anaesthesiol. 2005;22(3):165–70.
Gee W, et al. Assessment of intra-aortic balloon pumping by ocular pneumoplethysmography. Am Surg. 1986;52(9):489–91.
Marinoni M, et al. Retrospective analysis of transcranial Doppler patterns in veno-arterial extracorporeal membrane oxygenation patients: feasibility of cerebral circulatory arrest diagnosis. ASAIO J. 2018;64(2):175–82.
Nasr DM, Rabinstein AA. Neurologic complications of extracorporeal membrane oxygenation. J Clin Neurol. 2015;11(4):383–9.
Omar HR, et al. Incidence and predictors of ischemic cerebrovascular stroke among patients on extracorporeal membrane oxygenation support. J Crit Care. 2016;32:48–51.
Meyer AD, et al. Platelet-derived microparticles generated by neonatal extracorporeal membrane oxygenation systems. ASAIO J. 2015;61(1):37–42.
Foster PP, et al. Patent foramen ovale and paradoxical systemic embolism: a bibliographic review. Aviat Space Environ Med. 2003;74(6 Pt 2):B1–64.
Stocchetti N, et al. Hyperventilation in head injury: a review. Chest. 2005;127(5):1812–27.
Brunser AM, et al. The role of TCD in the evaluation of acute stroke. J Neuroimaging. 2016;26(4):420–5.
Muehrcke DD, et al. Complications of extracorporeal life support systems using heparin-bound surfaces. The risk of intracardiac clot formation. J Thorac Cardiovasc Surg. 1995;110(3):843–51.
Jiang J, et al. Microembolic signal monitoring of TOASTclassified cerebral infarction patients. Mol Med Rep. 2013;8(4):1135–42.
Best LM, et al. Transcranial Doppler ultrasound detection of microemboli as a predictor of cerebral events in patients with symptomatic and asymptomatic carotid disease: a systematic review and meta-analysis. Eur J Vasc Endovasc Surg. 2016;52(5):565–80.
Zanatta P, et al. Microembolic signals and strategy to prevent gas embolism during extracorporeal membrane oxygenation. J Cardiothorac Surg. 2010;5:5.
Marinoni M, et al. Cerebral microemboli detected by transcranial doppler in patients treated with extracorporeal membrane oxygenation. Acta Anaesthesiol Scand. 2016;60(7):934–44.
Hornig CR, Dorndorf W, Agnoli AL. Hemorrhagic cerebral infarction–a prospective study. Stroke. 1986;17(2):179–85.
Kasirajan V, et al. Risk factors for intracranial hemorrhage in adults on extracorporeal membrane oxygenation. Eur J Cardiothorac Surg. 1999;15(4):508–14.
Martucci G, Lo Re V, Arcadipane A. Neurological injuries and extracorporeal membrane oxygenation: the challenge of the new ECMO era. Neurol Sci. 2016;19:19.
Hingorani A, et al. Causes of early post carotid endartectomy stroke in a recent series: the increasing importance of hyperperfusion syndrome. Acta Chir Belg. 2002;102(6):435–8.
Giani M, et al. Apnea test during brain death assessment in mechanically ventilated and ECMO patients. Intensive Care Med. 2016;42(1):72–81.
Sloan MA, et al. Assessment: transcranial Doppler ultrasonography: report of the Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology. Neurology. 2004;62(9):1468–81.
Wahlster S, et al. Brain death declaration: practices and perceptions worldwide. Neurology. 2015;84(18):1870–9.
Pugin D, Woimant F. Stroke care in the ICU: general supportive treatment. Experts’ recommendations. Rev Neurol (Paris). 2012;168(6–7):490–500.
Atkinson JL, Anderson RE, Sundt TM. The effect of carbon dioxide on the diameter of brain capillaries. Brain Res. 1990;517(1–2):333–40.
Kazmi SO, et al. Cerebral pathophysiology in extracorporeal membrane oxygenation: pitfalls in daily clinical management. Crit Care Res Pract. 2018;2018:3237810.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Algorithm
Algorithm

ABCD airway-breathing-circulation-disability, GCS Glasgow coma score, LVEF left ventricular ejection fraction, CBF Cerebral blood flow, MV mechanical ventilation, IABP Intra-aortic blood pump, PI pulsatility index, EDV end-diastolic velocity, FA femoral artery, SCA subclavian artery, AAo aortic, CBV cerebral blood volume, FO foramen ovale, AKI acute renal injury, CPP cerebral perfusion pressure
Rights and permissions
Copyright information
© 2022 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Le Guennec, L., Combes, A. (2022). ECMO Patient in Intensive Care Unit: Usefulness of Neurosonology in Neurologic Monitoring. In: Rodríguez, C.N., et al. Neurosonology in Critical Care . Springer, Cham. https://doi.org/10.1007/978-3-030-81419-9_48
Download citation
DOI: https://doi.org/10.1007/978-3-030-81419-9_48
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-81418-2
Online ISBN: 978-3-030-81419-9
eBook Packages: MedicineMedicine (R0)