Abstract
Background
Acute brain injury (ABI) is a frequent complication of pediatric extracorporeal membrane oxygenation (ECMO) that could be detected by continuous neuromonitoring. Cerebral near-infrared spectroscopy (NIRS) allows monitoring of cerebral oxygenation.
Objective
To assess whether an impaired cerebral oxygenation was associated with short-term outcome during pediatric ECMO.
Methods
We conducted a single-center retrospective study in a pediatric intensive care unit. Children under 18 years old were included if receiving veno-venous or veno-arterial ECMO with concurrent NIRS monitoring. Cerebral saturation impairment was defined as rScO2 under 50% or 20% from the baseline for desaturation, and above 80%. Cerebral imaging (magnetic resonance imaging or CT scan) was performed in case of neurological concern. A radiologist blinded for patient history identified ABI as any hemorragic or ischemic lesion, then classified as major or minor. Primary endpoint was the outcome at hospital discharge. Poor outcome was defined as death or survival with a pediatric cerebral performance category scale (PCPC) score ≥ 3 and/or a major ABI. Good outcome was defined as survival with a PCPC score ≤ 2 and/or a minor or no ABI. Secondary endpoint was mortality before PICU discharge.
Results
Sixty-three patients met inclusion criteria; 48 (76%) had veno-arterial ECMO. Mortality rate was 51%. Forty-eight of sixty-three patients (76%) evolved with a poor outcome, including 20 major ABI. Mean rScO2 in the right/left hemisphere was 73 ± 9%/75 ± 9%. Cerebral desaturation and decline of rScO2 below 20% from the baseline, regardless of side, were each associated with poor outcome (multivariable-adjusted odds ratio (OR), 4 [95%CI 1.2; 15.1], p = 0.03, and 3.9 [95%CI 1.1; 14.9], p = 0.04, respectively), as well as a mean right rScO2 < 70% during the ECMO course (adjusted OR, 5.6 [95%CI 1.3; 34], p = 0.04). Left rSCO2 ≥ 80% was inversely correlated with hospital mortality (adjusted OR of 0.14 [95%CI 0.02; 0.8], p = 0.04).
Conclusions
Cerebral desaturation attested by NIRS was associated with a poor short-term outcome in children of all ages undergoing ECMO, and rScO2 > 80% seemed to be protective. NIRS monitoring might be included within multimodal neuromonitoring to assess the risk of the brain injury related to pediatric ECMO.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Extracorporeal membrane oxygenation (ECMO) is an increasingly used technique that provides temporary cardiopulmonary support. Neurological complications are frequent [1, 2] and associated with increased hospital mortality [2]. Children’s growing brain exposes them to acute brain injury (ABI) [3] Hence, pediatric stroke may occur in 5 to 22% during ECMO [2, 4, 5] with a higher prevalence in neonates and young infants [4, 6]. In this population, ABI is of difficult diagnosis because of sedation and curarization that strongly limit clinical examination accuracy. Continuous cerebral monitoring is therefore a matter of importance. Near-infra red spectroscopy (NIRS) offers a continuous and noninvasive cerebral saturation monitoring [7] that might reflect cerebral oxygenation and cerebral blood flow [8]. NIRS monitoring is routinely used in pediatric [9] and adult patients [10] undergoing cardiopulmonary bypass: cerebral oxygenation optimization driven by NIRS may reduce the incidence of post-operative complications [10] and stroke [11]. In patients under prolonged ECMO, the use of NIRS as a neuromonitoring tool may allow early detection of cerebrovascular events [12, 13]. Two pediatric studies including mostly neonates found an association between cerebral desaturation and hospital mortality or ABI defined by imaging [4] or by a poor neurological clinical score [14]. Data are lacking addressing older pediatric range, and no study addressed the impact of cerebral hyperoxia [15]. We aimed to assess if an impaired cerebral oxygenation was associated with mortality and ABI in children under ECMO.
Methods
Design and Population
We conducted a retrospective single-center study in a French pediatric intensive care unit (PICU), being an ECMO-center since 2014. Study was approved by the hospital institutional review board. ECMO management is described in the supplemental material.
All patients less than 18 years old receiving veno-venous (V–V) or veno-arterial (V-A) ECMO from January 2014 to December 2018 who had concurrent cerebral oxymetry monitoring for more than 6 h were included in the study.
NIRS Monitoring
Cerebral tissue oxygen saturation (rScO2) was continuously recorded using a 4-wavelength cerebral oxymeter (EQUANOX 7600®, Nonin, Eurocare) or a 2-wavelength cerebral oxymeter (INVOS 5100C®, Covidien, Medtronics, USA). Two sensors were placed on both sides of the patient’s forehead to allow for screening of unilateral lesions. Cerebral desaturation was defined as a decrease in rScO2 value under the threshold of 50%, or >20% from baseline [4, 16]. We also recorded increases in rScO2 value above the threshold of 80% [17]. Baseline rScO2 was defined as the first value recorded after ECMO cannulation. We abstracted all rScO2 recordings at each hour, from the first 6 h after initiation of ECMO until its discontinuation. We then calculated mean rScO2 and divided the cumulative spent time with rScO2 under or above the defined threshold by the duration of ECMO support (in hours) to obtain the time percentage.
Data Collection and Definitions
Baseline demographic and ECMO data were collected for all patients. Severity scores and comorbidities were assessed using the vasoactive-inotropic score (VIS), the Pediatric Index of Mortality-3 score (PIM-3), the Pediatric Logistic Organ Dysfunction-2 score (PELOD-2), and blood gas and lactate analyses. We recorded the lowest pH and the highest lactate and aterial PaCO2. We calculated PaCO2 variation between immediate pre- and post-ECMO initiation (delta = PaCO2 before ECMO – PaCO2 after initiation of ECMO).
Outcomes
For all survivors, a pediatric neurologist (MK) systematically performed a complete clinical examination before hospital discharge as part of our institutional practice. Pediatric Cerebral Performance Category Scale (PCPC) was calculated. Brain imaging was performed if neurological concern was raised, because of neurological acute events (including seizures), altered neurological examination, and/or suspicion of a patient’s history suggesting cerebral prolonged hypoxia or lesion (i.e., known neurological comorbidities, extracorporeal cardiopulmonary resuscitation (ECPR) prolonged more than 15 min, severe hemodynamic disability despite ECMO requiring high doses of inotropes or vasoactive drugs, deep anemia and/or disseminated intravascular coagulation and/or hemorragic shock). Cerebral tomography (CT) scan was used during ECMO, while magnetic resonance imaging (MRI) was performed after its discontinuation. A pediatric radiologist (RL), blind to the procedure and the patient’s outcome, reviewed retrospectively all images. Patients without neurological concern at PICU discharge were considered free of ABI, even in the absence of cerebral imaging.
The primary endpoint was an outcome composite criteria assessed at hospital discharge: (1) good outcome was defined as survival with a PCPC score ≤ 2 with no ABI or minor ABI on imaging; (2) poor outcome was defined as death or survival with a PCPC score ≥ 3 and/or a major ABI on imaging. ABI was defined as any hemorragic or ischemic lesion on cerebral imaging (CT scan or MRI) or on autopsy when performed. Lesions were classified using a previously described radiological classification [6]. Ischemic lesions were classified as minor or major according to their size (respectively ≤ 1 cm or > 1 cm). Minor hemorragic lesions included extra-axial hemorrhage without mass effect, parenchymal hemorrhage ≤ 1 cm (including microbleeds, which are common after ECMO [18]), and grade 1 or 2 intraventricular hemorrhage. Other subtypes of hemorrhage were classified as major.
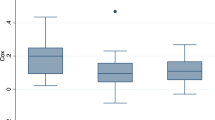
Statistical Analysis
Results are presented as means ± standard deviations (SD) or medians and interquartile range (IQR) for continuous variables depending on their normality and numbers, and percentages for categorical variables. Continuous variables were compared using Student’s T test or Wilcoxon rank sum test. Categorical variables were compared using Chi-squared or a Fisher test. Patients’ severity and cerebral oxymetry were tested in univariate analysis for association with outcome and death. We conducted multivariable regression analyses to adjust for the potential confounders. We retained variables achieving p < 0.1 in the univariate analysis and previously reported to be associated with outcome [14]. Variables were tested for colinearity and excluded of the model in case of association with another one. We considered rScO2 as a binary variable using the pre-defined thresholds. Mean rScO2 was dichotomized in a two classes of categorical variable based on prior works [4, 14] and on the results of the univariate analysis. A p value < 0.05 defined statistical significance. Data were analyzed using R programming software.
Results
Patients’ Characteristics and Evolution
Between January 2014 and December 2018, we treated 71 patients with ECMO. Among them, 63 patients had concurrent NIRS monitoring and were included in this study. Median [IQR] age was 1.1 [0.2; 4.3] years old. V-A ECMO was the most common type of extracorporeal assistance (76% (n = 48) versus 24% (n = 15) for V–V ECMO), all implanted with a jugulo-carotid cannulation. The median duration of ECMO therapy was 9 [5, 13] days. Patients’ characteristics are presented in Table 1 (Table 1). NIRS monitoring duration was 8 [4, 12] days. Regardless of side, cerebral desaturation occurred in 42 (68%) patients, and rSCO2 > 80% in 54 (87%) patients. On the right side (n = 62), baseline and mean rScO2 were, respectively, 70 ± 13% and 73 ± 9%. On the left side (n = 61), baseline and mean rScO2 were, respectively, 73 ± 13% and 75 ± 9%. There was no difference between both sides.
Neurological evolution and classification of patient outcomes are presented in Fig. 1. Thirty-two patients (51%) died before hospital discharge. Five patients were brain dead and 15 died following a withdrawal of life-sustaining treatments. Twenty of the deceased patients did not have cerebral imaging or autopsy. Detailed reasons for these deaths are summarized in the supplemental (table S1). Neurological concern was raised in (49%) of survivors (19/31), leading to diagnosis of major ABI in 10, minor one in 8, and no ABI in 1. Clinical and radiological features of the nine patients with minor or no ABI are described in the supplemental (table S2). Overall, 42 (67%) patients had poor outcome at hospital discharge (Fig. 1). Survivors with poor and good outcomes had a median PCPC score at 2 [1.25; 2] and 1 [1; 1.25], respectively. In patients with major ABI, lesions were mostly bilateral (16 bilateral lesions versus 4 right-located and 2 left-located).
Evolution of patients based on the study’s outcome definition. Grey boxes represent patients with a good outcome; dotted boxes represent patients with a poor outcome. * The total number of patients is lower than the number of lesions because some patients presented both ischemic and hemorrhagic lesions. ABI: acute brain injury; CT: cerebral tomodensitometry; MRI: magnetic resonance imaging
Cerebral Oxygenation and Short-Term Outcome
The proportion of patients with cerebral desaturation, regardless of side, was significantly higher in patients with a poor outcome. This difference seemed to be present in the left hemisphere and due to the drop in rScO2 below 20% from the baseline. Contrarily, episodes of rScO2 > 80% and the proportion of time with impaired cerebral oxygenation did not differ between groups (Table 2). In the multivariable regression logistic model adjusted on age, ECMO indication (cardiac or respiratory), ECMO duration, and maximum blood lactate, global cerebral desaturation and decline of rScO2 > 20% from the baseline, regardless of side, remained significantly associated with poor outcome (adjusted OR [CI95%] of 4 [1.2; 15.1] for any cerebral desaturation, p = 0.03, and of 3.9 [1.1; 14.9] for decline of 20% from baseline, p = 0.04) (Table 3). The sensitivity of cerebral oxymetry to predict poor outcome seemed enhanced by the threshold of 20% decline from baseline (Table 4). A mean right rScO2 of less than 70% during the ECMO course was significantly associated with poor outcome (Adjusted OR [CI95%] of 5.6 [1.3; 34], p = 0.04) (Table 3).
Cerebral Oxygenation and Mortality
Cerebral oxymetry did not differ between groups addressing cerebral desaturation. Conversely, survivors presented more episodes of rScO2 > 80% than non-survivors on both hemispheres, without difference addressing proportion of time spent with rScO2 above 80% (Table 2). In the multivariable regression logistic model adjusted on age, ECMO indication (cardiac or respiratory), ECMO duration, minimum pCO2, and maximum blood lactate, only left rSCO2 ≥ 80% remained significantly inversely correlated with mortality (adjusted OR [CI95%] of 0.14 [0.02; 0.8] p = 0.04).
Neurological involvement was uncertain in 4/20 deceased patients without imaging (2 patients had refractory shock at weaning and 2 deceased consecutively to a decision of withdrawing life support treatments because of refractory respiratory compromise) (supplemental table S1). Results were not modified when we performed secondary analysis excluding them.
Cerebral Oxygenation in V-A and V–V ECMO
Comparison of the outcome in patients under V-A and V–V ECMO is presented in the supplemental (tables S3 and S4). Twenty-three patients/48 (48%) treated with V-A ECMO died before hospital discharge, 15 (31%) had good outcome. Their NIRS monitoring showed similar patterns with the global population. Nine patients/15 (60%) treated with V–V ECMO deceased before hospital discharge; 6 (40%) evolved with good outcome. Baseline rScO2 measured at the beginning of V–V ECMO was lower in non-survivors (58% [56; 70] versus 78% [72; 81.8] in the survivors groups, p = 0.04), conversely cerebral oxymetry did not differ during the course of ECMO.
We sought to investigate the variation in PaCO2 before and after starting V–V ECMO (∆PaCO2): ∆PaCO2 tended to be higher in patients with major cerebral bleeding (p = 0.05) (supplemental S5).
Discussion
We report herein our single-center experience of continuous cerebral oxymetry monitoring during prolonged pediatric ECMO. We found an association between cerebral desaturation and poor outcome. Conversely, a higher rScO2 was associated with a better survival, with a specific trend in patients under V–V ECMO.
Almost half of our population developed an ABI. This proportion might therefore have been underestimated because some patients had no imaging. ABI under ECMO ranges from 8 to 50% and is variable across studies [5, 14], mostly because of heterogeneous populations and definitions. A higher proportion of unilateral lesions is reported in children [6], due to impaired cerebral autoregulation and to the ligation of the carotid artery and jugular vein induced by cannulation in infants under V-A ECMO, that can alter cerebral blood flow and drainage. In contrast with previous pediatric studies [4, 14], we included more children with previous complex genetic diseases or immunodeficiency, but we had a few neonates. This different population may explain the high rate of ABI.
Mortality and patients’ severity were similar to that previously described in pediatric prolonged ECMO [4, 14, 19]. Proportion of ischemic or hemorragic lesions depending on the type of ECMO was in accordance with literature [18, 20]. Anticoagulation in children under ECMO remains challenging [21]. A lower anticoagulation under V–V ECMO might avoid cerebral bleeding events. The high prevalence of cerebral bleeding in our study may be explained because we deliberately chose to include in this definition all types of bleeding including microbleeds as minor ABI. Cerebral microbleeds have been described in adults [18] and children [22] under ECMO with seemingly little effect on survival, but no study has investigated their impact on neurological outcome.
Despite the lack of randomized trials in the field of neuromonitoring during ECMO, several observational studies have now assessed the specific value of cerebral oxymetry in children [4, 14] and adults [12, 13]. All have shown an association between cerebral desaturation and poor neurological outcome. In our study, the impact of cerebral desaturation on outcome seemed to differ between hemispheres. Some hypotheses might explain this laterality: First, in patients with right jugulo-carotid V-A ECMO, collateral vascularization might lead either to a contralateral hyperhemia (similar to a brain ischemia–reperfusion syndrome) with subsequent left cerebral lesion [23] or to a right cerebral hypoperfusion with subsequent right cerebral ischemic lesion. The association found only in the right hemisphere between a lower mean rScO2 during the ECMO course and poor outcome relies with that latter hypothesis. Second, left rScO2 reflects the adequacy of systemic perfusion and oxygen delivery through both the circuit and systemic circulation. In this situation and in patients with cardiac failure, left cerebral desaturation would be more reliant on the ECMO circuit. We cannot conclude about these assumptions because we did not perform concomitant transcranial Doppler ultrasound and because data (SaO2, SvO2, mean arterial pressure) were insufficient to indicate circuit performance or systemic perfusion/oxygen delivery in a retrospective design. Moreover, the trends observed for a rather left-sided desaturation in the univariate analysis were not confirmed when adjusting on the confounders, and more probably might be due to chance.
Unfortunately, our study was not designed to investigate the significance of asymmetric cerebral desaturation. Moreover, patients had mainly bilateral lesions, so we cannot conclude about a direct link between the side of the rScO2 decrease and the occurrence of lateralized ischemic or hemorrhagic stroke.
We have to be cautious interpreting the association between cerebral desaturation and neurological outcome. First, mortality might not be entirely attributed to brain injury in our study. Patients needing ECMO often present in a very precarious state. When looking at the reasons for deaths in the 20 patients without imaging, 8/20 deceased from multiple organ dysfunction syndrome, which could uncertainly induce neurological injury, and 15 deaths were consecutive to a decision of withdrawing life-support treatments (supplemental). In those cases, the role of cerebral desaturation is uncertain. Nevertheless, neurological involvement seemed too obtuse only in 4/20 patients who did not appear to affect the results.
Second, cerebral desaturation as defined by our study was of accurate sensitivity to predict poor outcome, but the proportion of patients with good outcome and cerebral desaturation was important. It cannot be ruled out that our results would have differed in a less severe population.
Third, as developed in the previous paragraph, precluding any direct and independent link between cerebral desaturation and cerebral injury would probably lead to erroneous conclusion. Cerebral oxygenation depends on multiple parameters [24] including an optimal adequation between oxygen demand and delivery both at the systemic and the regional levels. Cerebral blood flow is maintained thanks to the cardiac output and/or ECMO rate flow, arterial pressure, and cerebral vasoreactivity, which in turn might be impacted by PaCO2 variations and cerebral oxygen consumption. Because we lack some of these data, we cannot conclude that the decrease in rScO2 alone was responsible for the brain lesions we observed. PaCO2 concentration has a well-known impact on cerebral autoregulation that may influence cerebral oximetry. High vasoconstriction induced by hypocapnia may lead to brain ischemic lesions in patients with low PaCO2 and rScO2, especially in children under V-A ECMO [25]. Prompt PaCO2 variations at the beginning of ECMO may alter cerebral blood flow and cerebral oxygenation and are known to be a risk factor of cerebral bleeding in V–V and V-A ECMO [18, 20]. In our study and in the V–V ECMO group, the level of PaCO2 variation tended to be higher in patients with major cerebral bleeding, although proportion of cerebral hyperoxia was higher. This suggests that NIRS alone does not allow interpretation of cerebral hemodynamics.
In contrast to others, cerebral desaturation was not associated with mortality in our study [4, 12, 13]. We chose a different threshold of rScO2 to define cerebral desaturation [12, 13] that was validated in children under cardiac or general surgery [16, 26, 27] and in neonates [4, 14, 17].
Unexpectedly, rScO2 > 80% was associated with a better survival. This difference seemed to be prominent in patients under V–V ECMO. Conversely, deceased patients had a lower baseline rScO2 at the initiation of ECMO, suggesting that a protective impact of cerebral hyperoxia might be present after implantation of ECMO. Hyperoxia is known to be deleterious on the immature brain in experimental studies [28] and represents an independent risk factor for mortality under pediatric ECMO [25]. However, no previous study has investigated the role of cerebral hyperoxia on neurological outcome and mortality. One explanation of our result could be that survivors in patients under V–V ECMO were less hypoxemic than non-survivors. Their survival might be due to a less serious illness rather than a better cerebral oxygenation. Oxygen transport to the living tissues depends on the arterial oxygen content, which is determined among others by arterial oxygen saturation and hemoglobin. Thus, rScO2 may vary because of SaO2 modifications without hemodynamic disorders [29]. This preliminary result encourages further studies to replicate investigations on the impact of high cerebral saturation in this setting, taking into account systemic oxygenation and a stricter definition (i.e., rScO2 > 85%).
Our study presented some limitations. First, population was small, especially in the V–V ECMO group. Second, NIRS monitoring was not designed for the study. We used two different NIRS devices along the study period, with different number of wavelengths and spectrum emission that could induce variations in rScO2 estimation overtime due to different measured concentrations of oxy and deoxyhemoglobin. NIRS sensors were placed on the forehead of the patients, which gives cerebral oxygenation for the frontal cortex only, yet we could have missed an event in patients with parieto-temporal lesion, which is more frequent in ECMO population. This constitutes one of the limits of the NIRS technique to predict the occurrence of a focalized lesion. Electroencephalogram (EEG) monitoring could be of interest in this situation, but our retrospective study was not designed to take EEG recordings into account. Because of the procedure for data collection, we may have missed some events during the entire NIRS monitoring. As the proportion of time with cerebral desaturation in relation to the total time under ECMO ranges only for several minutes in children [4], we believe that this bias was minimized by the long time our patients were recorded and by the averaging of rScO2. Another limit of the NIRS technology is the poor accuracy of the rScO2 measure in case of modifications of the underlying tissue, which might lead misinterpretation. Therefore, the intrinsic variations of rScO2 (20% decrement from the baseline value) are more important to take into account than the rScO2’s fall under absolute values.
Third, at the time of the study no systematic radiological neurological follow-up of ECMO patients had been implemented. Consequently, we may have underestimated the prevalence of brain lesions in patients who did not undergo brain imaging because of satisfactory clinical examination. On the other hand, short-term evaluation might be misinterpreted because of adjunctive sedative therapies and may have missed long-term disabilities. A systematic clinical and radiological long-term follow-up including quality of life evaluation is encouraged in children after ECMO.
This study is still one of the only pediatric studies that investigate the impact of cerebral oxygenation impairment on all age groups children under ECMO, and the first to assess the association between cerebral hyperoxia and outcome. NIRS monitoring alone is insufficient to predict unfavorable outcome for pediatric patients under ECMO. Nevertheless, a cerebral desaturation might reflect an impaired systemic oxygenation and hemodynamics, and a low rScO2 has to alert about possible brain suffering. In this situation, intensivists should complete their neurohemodynamic assessment (including transcranial Doppler ultrasound, electroencephalogram, and therefore, brain imaging in case of potent neurological concerns) and rapidly correct any systemic oxygenation or hemodynamic disturbance, aiming at preventing cerebral injury. Further prospective studies with long-term outcome are needed to assess first the feasibility and then the impact of a multimodal neurological monitoring including NIRS in children under ECMO.
References
Lorusso R, Barili F, Mauro MD, Gelsomino S, Parise O, Rycus PT, et al. In-hospital neurologic complications in adult patients undergoing venoarterial extracorporeal membrane oxygenation: results from the extracorporeal life support organization registry. Crit Care Med. 2016;44:e964–72.
Nasr DM, Rabinstein AA. Neurologic complications of extracorporeal membrane oxygenation. J Clin Neurol Seoul Korea. 2015;11:383–9.
Moretti R, Pansiot J, Bettati D, Strazielle N, Ghersi-Egea J-F, Damante G, et al. Blood-brain barrier dysfunction in disorders of the developing brain. Front Neurosci. 2015;9:40.
Clair M-P, Rambaud J, Flahault A, Guedj R, Guilbert J, Guellec I, et al. Prognostic value of cerebral tissue oxygen saturation during neonatal extracorporeal membrane oxygenation. PLoS ONE. 2017;12:e0172991.
Barbaro RP, Paden ML, Guner YS, Raman L, Ryerson LM, Alexander P, et al. Pediatric extracorporeal life support organization registry international report 2016. ASAIO J. 2017;63:456–63.
Wien MA, Whitehead MT, Bulas D, Ridore M, Melbourne L, Oldenburg G, et al. Patterns of brain injury in newborns treated with extracorporeal membrane oxygenation. AJNR Am J Neuroradiol. 2017;38:820–6.
Myers DE, Anderson LD, Seifert RP, Ortner JP, Cooper CE, Beilman GJ, et al. Noninvasive method for measuring local hemoglobin oxygen saturation in tissue using wide gap second derivative near-infrared spectroscopy. J Biomed Opt. 2005;10:034017.
Taussky P, O’Neal B, Daugherty WP, Luke S, Thorpe D, Pooley RA, et al. Validation of frontal near-infrared spectroscopy as noninvasive bedside monitoring for regional cerebral blood flow in brain-injured patients. Neurosurg Focus. 2012;32:E2.
Zulueta JL, Vida VL, Perisinotto E, Pittarello D, Stellin G. Role of intraoperative regional oxygen saturation using near infrared spectroscopy in the prediction of low output syndrome after pediatric heart surgery. J Card Surg. 2013;28:446–52.
Fischer GW, Lin H-M, Krol M, Galati MF, Di Luozzo G, Griepp RB, et al. Noninvasive cerebral oxygenation may predict outcome in patients undergoing aortic arch surgery. J Thorac Cardiovasc Surg. 2011;141:815–21.
Goldman S, Sutter F, Ferdinand F, Trace C. Optimizing intraoperative cerebral oxygen delivery using noninvasive cerebral oximetry decreases the incidence of stroke for cardiac surgical patients. Heart Surg Forum. 2004;7:E376–81.
Pozzebon S, Blandino Ortiz A, Franchi F, Cristallini S, Belliato M, Lheureux O, et al. Cerebral near-infrared spectroscopy in adult patients undergoing veno-arterial extracorporeal membrane oxygenation. Neurocrit Care. 2018;29:94–104.
Khan I, Rehan M, Parikh G, Zammit C, Badjatia N, Herr D, et al. Regional cerebral oximetry as an indicator of acute brain injury in adults undergoing veno-arterial extracorporeal membrane oxygenation-a prospective pilot study. Front Neurol. 2018;9:993.
Tsou P-Y, Garcia AV, Yiu A, Vaidya DM, Bembea MM. Association of cerebral oximetry with outcomes after extracorporeal membrane oxygenation. Neurocrit Care. 2020;33(2):429–37.
Roberts BW, Kilgannon JH, Hunter BR, Puskarich MA, Pierce L, Donnino M, et al. Association between early hyperoxia exposure after resuscitation from cardiac arrest and neurological disability: prospective multicenter protocol-directed cohort study. Circulation. 2018;137:2114–24.
Michelet D, Arslan O, Hilly J, Mangalsuren N, Brasher C, Grace R, et al. Intraoperative changes in blood pressure associated with cerebral desaturation in infants. Pediatric Anesthesia. 2015;25:681–8.
Hyttel-Sorensen S, Pellicer A, Alderliesten T, Austin T, van Bel F, Benders M, et al. Cerebral near infrared spectroscopy oximetry in extremely preterm infants: phase II randomised clinical trial. BMJ. 2015;350:g7635.
Luyt C-E, Bréchot N, Demondion P, Jovanovic T, Hékimian G, Lebreton G, et al. Brain injury during venovenous extracorporeal membrane oxygenation. Intens Care Med. 2016;42:897–907.
Jenks CL, Raman L, Dalton HJ. Pediatric extracorporeal membrane oxygenation. Crit Care Clin. 2017;33:825–41.
Le Guennec L, Cholet C, Huang F, Schmidt M, Bréchot N, Hékimian G, et al. Ischemic and hemorrhagic brain injury during venoarterial-extracorporeal membrane oxygenation. Ann Intens Care. 2018;8:129.
Barton R, Ignjatovic V, Monagle P. Anticoagulation during ECMO in neonatal and paediatric patients. Thromb Res. 2019;173:172–7.
Liebeskind DS, Sanossian N, Sapo ML, Saver JL. Cerebral microbleeds after use of extracorporeal membrane oxygenation in children. J Neuroimaging. 2013;23:75–8.
Mendoza JC, Shearer LL, Cook LN. Lateralization of brain lesions following extracorporeal membrane oxygenation. Pediatrics. 1991;88:1004–9.
Garvey AA, Dempsey EM. Applications of near infrared spectroscopy in the neonate. Curr Opin Pediatr. 2018;30:209–15.
Cashen K, Reeder R, Dalton HJ, Berg RA, Shanley TP, Newth CJL, et al. Hyperoxia and hypocapnia during pediatric extracorporeal membrane oxygenation: associations with complications, mortality, and functional status among survivors. Pediatr Crit Care Med. 2018;19:245–53.
Scheeren TWL, Schober P, Schwarte LA. Monitoring tissue oxygenation by near infrared spectroscopy (NIRS): background and current applications. J Clin Monit Comput. 2012;26:279–87.
Austin EH, Edmonds HL, Auden SM, Seremet V, Niznik G, Sehic A, et al. Benefit of neurophysiologic monitoring for pediatric cardiac surgery. J Thorac Cardiovasc Surg. 1997;114(707–15):717 (discussion 715–716).
Yiş U, Kurul SH, Kumral A, Cilaker S, Tuğyan K, Genç S, et al. Hyperoxic exposure leads to cell death in the developing brain. Brain Dev. 2008;30:556–62.
Kredel M, Lubnow M, Westermaier T, Müller T, Philipp A, Lotz C, et al. Cerebral tissue oxygenation during the initiation of venovenous ECMO. ASAIO J. 2014;60:694–700.
Funding
This research received no specific funding.
Author information
Authors and Affiliations
Contributions
All the authors contributed substantially to the conception and design of the study, the acquisition, analysis and interpretation of the data, drafted or provided critical revision of the article, and approved final version of this manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Authors have no conflict of interest regarding this study.
Ethical approval
This retrospective study was approved by our hospital ethic committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Vedrenne-Cloquet, M., Lévy, R., Chareyre, J. et al. Association of Cerebral Oxymetry with Short-Term Outcome in Critically ill Children Undergoing Extracorporeal Membrane Oxygenation. Neurocrit Care 35, 409–417 (2021). https://doi.org/10.1007/s12028-020-01179-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-020-01179-9