Abstract
Background
Cerebral mitochondrial dysfunction is prominent in the pathophysiology of severe bacterial meningitis. In the present study, we hypothesize that the metabolic changes seen after intracisternal lipopolysaccharide (LPS) injection in a piglet model of meningitis is compatible with mitochondrial dysfunction and resembles the metabolic patterns seen in patients with bacterial meningitis.
Methods
Eight pigs received LPS injection in cisterna magna, and four pigs received NaCl in cisterna magna as a control. Biochemical variables related to energy metabolism were monitored by intracerebral microdialysis technique and included interstitial glucose, lactate, pyruvate, glutamate, and glycerol. The intracranial pressure (ICP) and brain tissue oxygen tension (PbtO2) were also monitored along with physiological variables including mean arterial pressure, blood glucose, lactate, and partial pressure of O2 and CO2. Pigs were monitored for 60 min at baseline and 240 min after LPS/NaCl injection.
Results
After LPS injection, a significant increase in cerebral lactate/pyruvate ratio (LPR) compared to control group was registered (p = 0.01). This increase was due to a significant increased lactate with stable and normal values of pyruvate. No significant change in PbtO2 or ICP was registered. No changes in physiological variables were observed.
Conclusions
The metabolic changes after intracisternal LPS injection is compatible with disturbance in the oxidative metabolism and partly due to mitochondrial dysfunction with increasing cerebral LPR due to increased lactate and normal pyruvate, PbtO2, and ICP. The metabolic pattern resembles the one observed in patients with bacterial meningitis. Metabolic monitoring in these patients is feasible to monitor for cerebral metabolic derangements otherwise missed by conventional intensive care monitoring.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite declining incidence over the last two decades, acquired bacterial meningitis remains a devastating disease with a mortality as high as 25% and neurological morbidity as high as 50% despite critical care therapy and introduction of adjunct anti-inflammatory drugs [1, 2].
The pathophysiological mechanism of bacterial meningitis is complex and involves inflammation, vasculitis with intravascular coagulation, metabolic failure, and disruption of the blood–brain–barrier (BBB) leading to cerebral edema and cellular necrosis—all factors that contributes to poor cerebral outcome [3,4,5,6].
Antibiotics are obviously the cornerstone in the treatment of bacterial meningitis. Dexamethasone has been introduced as the only adjunctive therapy for bacterial meningitis and has been shown to reduce short-term neurological complications [7]. Despite this, the risk of neurological sequelae remains high after bacterial meningitis [8].
The mitochondria are essential for aerobic metabolism and obtaining cellular homeostasis. Consequently, dysfunctional mitochondria may lead to cellular energy crisis, loss of cell homeostasis, and cell death. It has been shown that mitochondrial dysfunction indeed plays a role in the pathogenesis of bacterial meningitis [9].
Recently, it has been shown that cerebral metabolic derangements are common in bacterial meningitis and that these episodes might occur independently from increased intracranial pressure (ICP) and perturbations in other physiological parameters [10]. In fact, it was suggested that some of these episodes were due to mitochondrial dysfunction. It is likely that the derangements contribute to the ultimate outcome and neurological sequelae. Hence, critical care of patients with bacterial meningitis should include focus on identifying patients with cerebral metabolic disturbance. Accordingly, experimental translational models mimicking the cerebral metabolism of bacterial meningitis are important to identify the various cerebral metabolic patterns associated with meningitis.
Lipopolysaccharide (LPS) is a potent endotoxin that has been shown to induce disruption of the BBB, cerebral edema, and metabolic changes [11,12,13,14,15,16,17,18]. In the present study of experimental meningitis, we evaluate the metabolic response to intracisternal LPS injection as a model of bacterial meningitis. The cerebral metabolism is evaluated by monitoring of chemical variables related to energy metabolism obtained by microdialysis technique. We hypothesize that the changes in cerebral energy metabolism induced by LPS injection resembles the metabolic changes observed during cerebral mitochondrial dysfunction.
Further, we propose that the results from the present study can be directly translated to the bedside in the critical care of patients with bacterial meningitis.
Materials and Methods
All experiments were approved by the local ethics committee and carried out in accordance with the Danish “Animal Experiment Inspectorate” (Dyreforsøgstilsynet) and the ARRIVE guidelines. The chosen model has previously been established in a study focusing on brain edema caused by LPS injection [16].
Animals and Anesthesia
Twelve female piglets (Danish Landrace) approximately 4 months old weighing 41.4 ± 3.7 kg were included in the study. All animals had free access to water, but were deprived of food for 24 h before the start of the experiments. Sedation was achieved with a mixture of medetomidine 0.05 mg/kg, midazolam 0.25 mg/kg, and atropine 0.25 mg/kg. Anesthetics used were midazolam 0.625 mg/kg and ketamine 12.5 mg/kg and maintained by infusion of fentanyl 5 µg/kg/time and midazolam 5 mg/kg/h. The animals were intubated and ventilated with a tidal volume of 10 L/kg with a FiO2 of 0.3. A continuous infusion of 5 ml/kg/h isotonic glucose 2.5% intravenously (i.v.) kept blood glucose within physiological range. PaCO2 was kept between 4–6 kPa and body temperature around 38.5 °C by heating blanket.
Surgical Procedures
The surgical procedures were performed under sterile conditions. With the pig in supine position, the femoral arteries on left side were catheterized for arterial blood pressure monitoring and blood gas analysis. With the animal in prone position, the skull was exposed from 2 cm below eyelevel to the arc of C1. The atlanto-occipital membrane was exposed for injection of LPS or NaCl into the cisterna magna. Two burr-holes were placed parasagittal in the parietal lobe behind the coronal suture and intraparenchymal microdialysis (CMA 70, Microdialysis AB, Sweden), and Licox® probe (CCISB, Integra Neurosciences Ltd., Plainsboro, New Jersey, USA) for brain tissue oxygen tension (PbtO2) monitoring was implanted.
Through a right side frontal burr-hole, a Camino® catheter (Integra Neurosciences Ltd.) was implanted for ICP monitoring. ICP data from one animal was discarded due to technical issues.
Monitoring
Temperature, mean artery pressure, ICP, and PbtO2 were monitored continuously and registered every 10 min. Microdialysis catheters were perfused with artificial cerebrospinal fluid by a rate of 0.3 μl/min (CMA 106 MD pump, Microdialysis AB, Sweden). Dialysate was collected in capped microvials and analyzed every 30 min on Iscus Flex Analyzer (Microdialysis AB, Sweden) for glucose, glutamate, glycerol, lactate, and pyruvate. Arterial blood gas was registered at baseline and after LPS or NaCl injection.
Eight pigs were included in the LPS group and received injection with LPS (lipopolysaccharides from Escherichia coli 0111:B4, L5293 Sigma-Aldrich, lot#025M4091V) 200 or 400 µg dissolved in vehicle (0.2 ml isotone NaCl) into the cisterna magna through the atlanto-occipital membrane. A lumbar needle was inserted into the cisterna magna, and 0.6 ml cerebrospinal fluid (CSF) was extracted; then, 0.2 ml LPS was injected followed by injection of 0.4 ml CSF. Thus, there was no net change in injected volume. Two different doses of LPS were used. The first 4 animals were used as pilots to investigate whether there was a dose effect of LPS on cerebral metabolism. However, both concentrations showed quantitative identical metabolic patterns. Thus, the data were pooled and subsequent experiments were conducted with the lower concentration (200 µg).
Four animals were included in the control group. In this group, the same procedure as above was followed with the exception that no LPS was added to the vehicle. Hence, only isotonic NaCl was injected.
By the end of the experiments, the animals were euthanized by an injection of 200 mg/ml sodium pentobarbital in concentrated ethanol.
Course of Experiment
Once stable variables were obtained, a 60-min baseline (designated “baseline”) was established. Then, either LPS or NaCl was injected in the cisterna magna and the animal was monitored for 240 min hereafter (designated “experimental period”) with no interventions in this time period.
Statistics
Results are displayed as mean ± SD. Paired t test was used to compare means between baseline and experimental period. Differences between LPS and NaCl groups were explored utilizing a mixed effect model for repeated measurements with each individual animal as fixed effect and time and group as random effect. Data were analyzed using STATA 11.2 (College Station, TX, USA). A p value < 0.05 was considered statistically significant.
Results
Physiological variables for baseline and experimental period, respectively, are shown in Table 1. Except for PaO2, there were no differences between the groups in either time period. However, in the NaCl group the PaO2 was significantly higher during the experimental period.
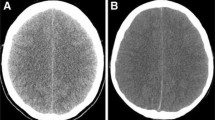
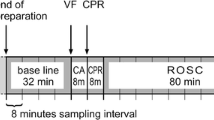
Table 2 shows mean values for microdialysis variables, PbtO2, and ICP during baseline and experimental period, respectively. All baseline values were within normal limits [19]. After injection of LPS, interstitial glucose in the LPS group showed a slight but significant decrease (Table 2) from 3.1 ± 1.2 to 1.7 ± 1.5 mmol/L during baseline and experimental period, respectively. This decrease was not observed in the control group, and glucose in the LPS group was significantly lower after LPS injection (p < 0.001). However, glucose remained within normal limits in both groups [19]. Interstitial lactate increased significantly from baseline after LPS injection from 2.3 ± 1.0 to 4.0 ± 2.0 mmol/L during the experimental period, whereas interstitial pyruvate remained stable and within normal values (Table 2, Fig. 1). The marked increase in lactate elicited a significant increase in LP ratio after LPS (Table 2, Figs. 2, 4) from 19 ± 9 during baseline to 48 ± 52 during experimental period. No change in LP ratio was observed in the control group. Also, compared to the control group both lactate and LP ratio increased significantly in the LPS group during the experimental period (p < 0.001 and p = 0.01, respectively).
Time course of the interstitial lactate and pyruvate concentration at baseline (0–60 min) and after LPS injection (60–300 min). Note the marked increase in lactate concentration after LPS injection paralleled by a slight increase in the pyruvate with subsequent decrease to sub-baseline but within normal limits [19]
Glycerol exhibited an increased tendency after LPS injection in the LPS group and was also markedly elevated above the NaCl group after LPS injection (p < 0.001) (Table 2, Suppl. Figure 1). No changes in glutamate in either group were observed after LPS injection (Table 2, Suppl. Figure 1).
A temporary increase in PbtO2 was observed immediately after LPS injection (Fig. 2). The PbtO2 then returned to baseline after approximately 1.5 h. Overall, neither group showed any significant change in PbtO2 after LPS or NaCl injection (Table 2). There was a significant difference in baseline PbtO2 between the two groups (Table 2). However, when correcting for this there were no significant differences between the groups.
In both groups, ICP tended to increase after treatment (Table 2, Fig. 3). The increase in the LPS group was more pronounced than in the control group but did not reach statistical significance (p = 0.08). Also, the changes were modest and ICP remained within normal values throughout the study.
Discussion
The present study describes the cerebral changes in the biochemical variables related to cerebral metabolism after LPS-induced meningitis in a translational model. Reference levels for the biochemical markers of metabolism have been established in humans [19]. These values are widely accepted as applicable to pig models and hence used for reference in the present paper.
The balance between interstitial lactate and pyruvate (LP ratio) reflects the redox state in the cellular interstitial space and is determined by the oxygen availability and oxidative metabolism, i.e., mitochondrial function.
Cerebral Metabolism and Oxygen Tension
In the present study, intrathecal injection of LPS caused a significant increase in LP ratio (Fig. 2). This increase was not observed in the control group (Fig. 4). The increase was due to a marked increase in lactate with a normal level of pyruvate (Fig. 1). The increase in lactate levels with normal levels of pyruvate was not observed in the control group where LP ratio, lactate, and pyruvate remained stable (Table 2, Fig. 4). Glucose showed a slightly decreasing tendency in the LPS group, but values remained within normal limits (Table 2).
In recent years, the changes in biochemical substances related to energy metabolism during mitochondrial dysfunction have been elaborated in both the experimental and clinical setting [20,21,22,23,24]. In brief, the metabolic pattern of mitochondrial dysfunction is characterized by increased LP ratio with marked increased lactate and normal or elevated levels of pyruvate. Further, it is distinguished from ischemia by normal levels of pyruvate. This metabolic pattern is similar to the one observed in the present study. The decrease in glucose is interpreted as a compensatory hyperglycolysis to increase the ATP generation through anaerobic metabolism.
In both groups, PbtO2 remained stable after LPS or NaCl injection compared to baseline (Table 2, Fig. 2). PbtO2 primarily reflects the product of CBF and arteriovenous oxygen difference [25]. Thus, no signs of decreased blood flow or oxygen delivery were observed. This supports the conclusion of non-ischemic metabolic derangement. We found a marked difference in PbtO2 between the groups. The normal level of brain tissue oxygen tension is variable and reported as low as 5 mmHg in white matter of healthy subjects [26]. Further, we have previously reported that the lower threshold for PbtO2 under which the cerebral metabolism is jeopardized can be as low as 10 mmHg [27]. This point is illustrated in our results as the lower baseline values for PbtO2 in the LPS group was accompanied by normal metabolism and LP ratio (Table 2).
Two studies have focused on cerebral metabolic changes after cisternal LPS injection in animal models [16, 28]. In the study by Jungner et al., they did not find any change in LP ratio after LPS injection. On the other hand, Gärdenfors et al. found a significant increase in LP ratio due to a marked increase in lactate and normal pyruvate levels after LPS injection [16] in accordance with our results.
The impact of LPS on cerebral mitochondrial function has been studied in detail. It has been proposed that LPS exerts its effect on the mitochondria through an inflammation-induced oxidative stress on the mitochondrial membrane potential and complex activity [13,14,15, 29]. The action is thought to be mediated through nitric oxide and is rapid in onset after LPS administration [15]. In the present experiment, the signs of mitochondrial dysfunction were observed approximately 1 h after LPS injection (Fig. 2). In this context, we propose that the observed metabolic changes observed in response to intrathecal LPS injection are due to mitochondrial dysfunction.
Glutamate is considered a robust marker of energy failure as elevated interstitial glutamate indicates that metabolic rate is insufficient to ensure glutamate reuptake from the synaptic cleft [30]. In the present study, baseline glutamate was somewhat higher in the LPS group than in the NaCl group (Table 2, Suppl. Figure 1). However, in both groups glutamate remained stable after LPS or NaCl injection. In LPS group, this observation indicates that the anaerobic metabolism was sufficient to obtain cell homeostasis.
Cell damage and subsequent membrane degradation and cell death increase the interstitial glycerol levels [31, 32]. In the present series, a slight yet significant increase in glycerol was observed (Table 2, Suppl. Figure 1). However, the values remained within normal levels. Hence, our data do not support that LPS injection leads to cell damage in the present series.
Immune Response to LPS
Intrathecal injection of LPS elicits a marked immune response with invasion of immune cells into the neuronal tissue [16]. Further, it has been shown that LPS suppresses the oxidative metabolism in macrophages and switches their metabolism toward glycolysis [33, 34]. Hence, the observed increase in LP ratio might also arise from hyperglycolytic immune cells. This contribution to the increase in LP ratio cannot be distinguished from the contribution from mitochondrial dysfunction in our study. However, in the original characterization of the present model the immune cells gathered in the subarachnoid space on the cortex as a response to LPS injection [16]. As the microdialysis probes sit in the white matter and only collect interstitial fluid from a few mm3 of tissue, we consider it likely that the chemical substances harvested by the microdialysis probe primarily reflect the metabolism of glial cells and neurons and to a lesser degree immune cells. The ratio of glial cells to neurons in white matter is about 2–4 and outnumbers other cell types [35]. Hence, the metabolic pattern most likely primarily represents the metabolism of these two cell types.
Besides eliciting a marked immune response and affecting the neuronal and glial tissue, it has been shown that LPS also impairs the mitochondrial function of the endothelial cells, thereby disturbing the integrity of the tight junctions causing disruption of the BBB [11, 16, 36]. This leads to cerebral edema and potentially increased intracranial pressure and decreasing perfusion pressure.
Intracranial Pressure
In both groups, the ICP had an increasing tendency over time with a tendency toward a more pronounced increase in the LPS group (Fig. 3). However, in both groups the ICP remained within normal limits and there was no significant difference between the groups. Others have reported a moderate increase in ICP after cisternal LPS injection [16, 28] and a slight increase after NaCl injection [16]. The observed increase in ICP in the NaCl group after 200 min might be due to increased stress response during the end of the experiment combined with higher infusion rate of 2.5% glucose i.v. leading to higher blood glucose levels (Table 1). Hence, signs of mitochondrial dysfunction can occur independent of the intracranial pressure. This view is supported by clinical data. In one study, metabolic signs of mitochondrial dysfunction were observed with normal ICP [10]. In another study on bacterial meningitis, ICP was increased in only approximately one-third of critical care patients [37] but was associated with a worse outcome. Accordingly, metabolic disturbances and potential energy failure might be missed with conventional monitoring of intracranial pressure and perfusion pressure in the critical care setting.
Clinical Implications
In a clinical study of 15 patients with bacterial meningitis published by our group, we found that one-third of the patients exhibited signs of cerebral metabolism identical to the pattern found in the present study [10]. Consequently, we propose that the model used in the present paper possesses translational properties necessary for evaluating the effect of intensive care treatment.
In summary, the metabolic picture presented in this paper is compatible with LPS-induced disturbance in oxidative metabolism that might in turn be contributed to mitochondrial dysfunction without severe energy failure leading to significant cell death. The latter should be interpreted in the light of the very controlled conditions under which the present experiments were conducted. In a clinical setting, the patient might be faced with systemic stress and systemic inflammatory response syndrome that further burdens the cerebral metabolism, and under these conditions, the metabolic rate might not be adequate to meet the metabolic demands. Hence, cell death might occur leading to neurological sequelae. We propose that disturbance in the cerebral oxidative metabolism is common after bacterial meningitis and, in part, due to mitochondrial dysfunction but does not always contribute to neuronal death. However, the disturbance renders the tissue more vulnerable to further metabolic stress. Consequently, critical care of patients with meningitis should focus not only on intracranial pressure and perfusion pressure monitoring as these variables do not reflect the metabolic state of the tissue. We propose that monitoring cerebral metabolism in critical care patients with meningitis will optimize the critical care by directly monitoring the metabolic adverse effect of systemic metabolic stress and episodes of hypotension, hypoxia, and intracranial hypertension. Further, metabolic monitoring might open possibilities for monitoring effects of treatments directed toward ameliorating oxidative stress, thereby preserving mitochondrial function [38].
Limitations
The present study only represents the metabolic changes after LPS-induced BBB disruption and inflammation. In the clinical setting, bacterial meningitis most likely induces a much more widespread response due to the inflammatory reaction toward other bacterial proteins. Hence, the pathophysiological mechanisms are probably much more complex and widespread than presented in this study.
As we did not perform in vitro studies of the mitochondrial function, the present study cannot elaborate on the exact mechanism of mitochondrial malfunction. Hence, the term “mitochondrial dysfunction” should be interpreted in its broadest view, signifying the inability of the mitochondrial oxidative metabolism to meet the metabolic demands of the tissue. Further, the present study does not clarify which cell types exhibit mitochondrial dysfunction. As discussed, activated immune cells might contribute to the metabolic pattern observed in the present study.
Conclusions
The metabolic response to intracisternal LPS injection mimics the metabolic changes observed during severe bacterial meningitis in the clinical setting. The metabolic changes are compatible with disturbances in the oxidative metabolism and partly due to mitochondrial dysfunction. The metabolic derangement can be observed in the absence of perturbations in conventional neuromonitoring, i.e., cerebral perfusion pressure and intracranial pressure. We propose that cerebral metabolic monitoring should be included in the monitoring of critically ill patients suffering from bacterial meningitis to optimize the intensive care and to monitor response to future treatment trials for severe bacterial meningitis.
References
Edberg M, Furebring M, Sjolin J, Enblad P. Neurointensive care of patients with severe community-acquired meningitis. Acta Anaesthesiol Scand. 2011;55(6):732–9.
Auburtin M, Porcher R, Bruneel F, Scanvic A, Trouillet JL, Bedos JP, et al. Pneumococcal meningitis in the intensive care unit: prognostic factors of clinical outcome in a series of 80 cases. Am J Respir Crit Care Med. 2002;165(5):713–7.
Liechti FD, Grandgirard D, Leib SL. Bacterial meningitis: insights into pathogenesis and evaluation of new treatment options: a perspective from experimental studies. Future Microbiol. 2015;10(7):1195–213.
Scheld WM, Koedel U, Nathan B, Pfister HW. Pathophysiology of bacterial meningitis: mechanism(s) of neuronal injury. J Infect Dis. 2002;186(Suppl 2):S225–33.
Gerber J, Nau R. Mechanisms of injury in bacterial meningitis. Curr Opin Neurol. 2010;23(3):312–8.
Lucas MJ, Brouwer MC, van de Beek D. Neurological sequelae of bacterial meningitis. J Infect. 2016;73(1):18–27.
Brouwer MC, McIntyre P, Prasad K, van de Beek D. Corticosteroids for acute bacterial meningitis. Cochrane Database Syst Rev. 2015(9):CD004405.
Bijlsma MW, Brouwer MC, Kasanmoentalib ES, Kloek AT, Lucas MJ, Tanck MW, et al. Community-acquired bacterial meningitis in adults in the Netherlands, 2006-14: a prospective cohort study. Lancet Infect Dis. 2016;16(3):339–47.
Barichello T, Savi GD, Simoes LR, Generoso JS, Fraga DB, Bellettini G, et al. Evaluation of mitochondrial respiratory chain in the brain of rats after pneumococcal meningitis. Brain Res Bull. 2010;82(5–6):302–7.
Poulsen FR, Schulz M, Jacobsen A, Andersen AB, Larsen L, Schalen W, et al. Bedside Evaluation of Cerebral Energy Metabolism in Severe Community-Acquired Bacterial Meningitis. Neurocrit Care. 2015;22(2):221–8.
Temesvari P, Abraham CS, Speer CP, Kovacs J, Megyeri P. Escherichia coli 0111 B4 lipopolysaccharide given intracisternally induces blood-brain barrier opening during experimental neonatal meningitis in piglets. Pediatr Res. 1993;34(2):182–6.
Tunkel AR, Rosser SW, Hansen EJ, Scheld WM. Blood-brain barrier alterations in bacterial meningitis: development of an in vitro model and observations on the effects of lipopolysaccharide. Vitro Cell Dev Biol. 1991;27A(2):113–20.
Noh H, Jeon J, Seo H. Systemic injection of LPS induces region-specific neuroinflammation and mitochondrial dysfunction in normal mouse brain. Neurochem Int. 2014;69:35–40.
Yao SY, Natarajan C, Sriram S. nNOS mediated mitochondrial injury in LPS stimulated oligodendrocytes. Mitochondrion. 2012;12(2):336–44.
Chuang YC, Tsai JL, Chang AY, Chan JY, Liou CW, Chan SH. Dysfunction of the mitochondrial respiratory chain in the rostral ventrolateral medulla during experimental endotoxemia in the rat. J Biomed Sci. 2002;9(6 Pt 1):542–8.
Gardenfors A, Nilsson F, Skagerberg G, Ungerstedt U, Nordstrom CH. Cerebral physiological and biochemical changes during vasogenic brain oedema induced by intrathecal injection of bacterial lipopolysaccharides in piglets. Acta Neurochir (Wien). 2002;144(6):601-8; discussion 8-9.
Burroughs M, Cabellos C, Prasad S, Tuomanen E. Bacterial components and the pathophysiology of injury to the blood-brain barrier: does cell wall add to the effects of endotoxin in gram-negative meningitis? J Infect Dis. 1992;165(Suppl 1):S82–5.
Wispelwey B, Lesse AJ, Hansen EJ, Scheld WM. Haemophilus influenzae lipopolysaccharide-induced blood brain barrier permeability during experimental meningitis in the rat. J Clin Invest. 1988;82(4):1339–46.
Reinstrup P, Stahl N, Mellergard P, Uski T, Ungerstedt U, Nordstrom CH. Intracerebral microdialysis in clinical practice: baseline values for chemical markers during wakefulness, anesthesia, and neurosurgery. Neurosurgery. 2000;47(3):701-9; discussion 9-10.
Nielsen TH, Bindslev TT, Pedersen SM, Toft P, Olsen NV, Nordstrom CH. Cerebral energy metabolism during induced mitochondrial dysfunction. Acta Anaesthesiol Scand. 2013;57(2):229–35.
Nielsen TH, Olsen NV, Toft P, Nordstrom CH. Cerebral energy metabolism during mitochondrial dysfunction induced by cyanide in piglets. Acta Anaesthesiol Scand. 2013;57(6):793–801.
Nordstrom CH, Nielsen TH, Schalen W, Reinstrup P, Ungerstedt U. Biochemical indications of cerebral ischaemia and mitochondrial dysfunction in severe brain trauma analysed with regard to type of lesion. Acta Neurochir (Wien). 2016;158(7):1231–40.
Jacobsen A, Nielsen TH, Nilsson O, Schalen W, Nordstrom CH. Bedside diagnosis of mitochondrial dysfunction in aneurysmal subarachnoid hemorrhage. Acta Neurol Scand. 2014;130(3):156–63.
Nielsen TH, Schalen W, Stahl N, Toft P, Reinstrup P, Nordstrom CH. Bedside Diagnosis of Mitochondrial Dysfunction After Malignant Middle Cerebral Artery Infarction. Neurocrit Care. 2014;21(1):35–42.
Rosenthal G, Hemphill JC 3rd, Manley G. Brain tissue oxygen tension is more indicative of oxygen diffusion than oxygen delivery and metabolism in patients with traumatic brain injury. Crit Care Med. 2009;37(1):379–80.
Pennings FA, Schuurman PR, van den Munckhof P, Bouma GJ. Brain tissue oxygen pressure monitoring in awake patients during functional neurosurgery: the assessment of normal values. J Neurotrauma. 2008;25(10):1173–7.
Nielsen TH, Engell SI, Johnsen RA, Schulz MK, Gerke O, Hjelmborg J, et al. Comparison Between Cerebral Tissue Oxygen Tension and Energy Metabolism in Experimental Subdural Hematoma. Neurocrit Care. 2011;15(3):585–92.
Jungner M, Bentzer P, Grande PO. Intracranial pressure following resuscitation with albumin or saline in a cat model of meningitis. Crit Care Med. 2011;39(1):135–40.
Kaizaki A, Tien LT, Pang Y, Cai Z, Tanaka S, Numazawa S, et al. Celecoxib reduces brain dopaminergic neuronaldysfunction, and improves sensorimotor behavioral performance in neonatal rats exposed to systemic lipopolysaccharide. J Neuroinflammation. 2013;10:45.
Samuelsson C, Hillered L, Zetterling M, Enblad P, Hesselager G, Ryttlefors M, et al. Cerebral glutamine and glutamate levels in relation to compromised energy metabolism: a microdialysis study in subarachnoid hemorrhage patients. J Cereb Blood Flow Metab. 2007;27(7):1309–17.
Ungerstedt U, Bäckström T, Hallstrom A. Microdialysis in normal and injured human brain. In: Kinney JM, Tucker HN, editors. Physiology, stress and malnutrition: functional correlates, nutritional intervention. New York: Lippincott-Raven; 1997. p. 361–74.
Hillered L, Valtysson J, Enblad P, Persson L. Interstitial glycerol as a marker for membrane phospholipid degradation in the acutely injured human brain. J Neurol Neurosurg Psychiatry. 1998;64(4):486–91.
Tannahill GM, Curtis AM, Adamik J, Palsson-McDermott EM, McGettrick AF, Goel G, et al. Succinate is an inflammatory signal that induces IL-1beta through HIF-1alpha. Nature. 2013;496(7444):238–42.
Mills EL, Kelly B, Logan A, Costa ASH, Varma M, Bryant CE, et al. Succinate Dehydrogenase Supports Metabolic Repurposing of Mitochondria to Drive Inflammatory Macrophages. Cell. 2016;167(2):457-70 e13.
von Bartheld CS, Bahney J, Herculano-Houzel S. The search for true numbers of neurons and glial cells in the human brain: a review of 150 years of cell counting. J Comp Neurol. 2016;524(18):3865–95.
Doll DN, Hu H, Sun J, Lewis SE, Simpkins JW, Ren X. Mitochondrial crisis in cerebrovascular endothelial cells opens the blood-brain barrier. Stroke. 2015;46(6):1681–9.
Larsen L, Poulsen FR, Nielsen TH, Nordstrom CH, Schulz MK, Andersen AB. Use of intracranial pressure monitoring in bacterial meningitis: a 10-year follow up on outcome and intracranial pressure versus head CT scans. Infect Dis (Lond). 2017;49(5):356–64.
Barichello T, Collodel A, Generoso JS, Simoes LR, Moreira AP, Ceretta RA, et al. Targets for adjunctive therapy in pneumococcal meningitis. J Neuroimmunol. 2015;278:262–70.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.

Supplementary Fig. 1
Glutamate and glycerol at baseline (0-60 min) and after LPS or NaCl injection in the LPS and Control group respectively. For glutamate, no difference from baseline was found in either group. Glycerol tended to increase in the LPS group after LPS injection. The increase was not significant (JPEG 226 kb)
Rights and permissions
About this article
Cite this article
Munk, M., Poulsen, F.R., Larsen, L. et al. Cerebral Metabolic Changes Related to Oxidative Metabolism in a Model of Bacterial Meningitis Induced by Lipopolysaccharide. Neurocrit Care 29, 496–503 (2018). https://doi.org/10.1007/s12028-018-0509-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-018-0509-9