Abstract
Background
An experimental swine model (n = 7) simulating an acute subdural hematoma (ASDH) was employed (1) to explore the relation between the brain tissue oxygenation (PbtO2) and the regional cerebral energy metabolism as obtained by microdialysis, and (2) to define the lowest level of PbtO2 compatible with intact energy metabolism.
Methods
ASDH was produced by infusion of 7 ml of autologous blood (infusion rate 0.5 ml/min) by a catheter placed subdurally. PbtO2 and microdialysis probes were placed symmetrically in the injured (“bad-side”) and non-injured (“good-side”) hemispheres. Intracranial pressure (ICP) was monitored in the “good-side.”
Results
ICP, cerebral perfusion pressure (CPP), PbtO2, glucose, lactate, pyruvate, lactate-pyruvate ratio (LP ratio), glutamate, and glycerol were recorded at baseline (60 min) and post trauma (360 min). After the creation of the ASDH, PbtO2 decreased significantly in both the hemispheres (P < 0.001). No significant difference was found between the sides post trauma. The LP ratio, glutamate, and glycerol in the “bad-side” increased significantly over the “good-side” where the values remained within the normal limits. A PbtO2 value below approximately 25 mmHg was found to be associated with disturbed energy metabolism in the “bad-side” but not in the “good-side.” No correlation was found between the LP ratio and PbtO2 in either hemisphere.
Conclusions
PbtO2 monitoring accurately describes tissue oxygenation but does not disclose whether the oxygen delivery is sufficient for maintaining cerebral energy metabolism. Accordingly, it may not be possible to define a threshold level for PbtO2 below which energy failure and permanent tissue damage occurs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During neurocritical care, cerebral ischemia is a relatively common and potentially serious complication. It may occur as a global phenomenon—e.g., due to an increase in intracranial pressure (ICP) causing a decrease in cerebral perfusion pressure (CPP)—or locally due to a regional restriction of blood flow, e.g., due to the vasoconstriction as seen in patients with vasospasms after subarachnoid hemorrhage or around a focal mass lesion in patients with traumatic brain injury. The acute changes in the cerebral levels of chemical compounds related to energy metabolism occurring during severe ischemia are well known [1, 2].
Techniques are now available for bed-side monitoring of brain tissue oxygenation (PbtO2) as well as for chemical analysis of the composition of cerebral interstitial fluid utilizing microdialysis [3]. Both the techniques give information from a small volume of the tissue surrounding the probe (approx. 10–15 mm3). Microdialysis with bed-side enzymatic analyses of the perfusates gives information regarding the delivery of substrate (glucose), the red-ox state of the tissue (lactate/pyruvate ratio, LP ratio), the efficacy of energy metabolism (glutamate), and the degradation of cellular membranes (glycerol) [4]. Monitoring of PbtO2 gives on-line information regarding tissue oxygenation. Knowledge of PbtO2 has been proposed to give an early warning of impending ischemia in neurointensive care patients, to serve as guidance for CPP management, and to be able to predict the prognosis for patients with traumatic brain injuries [5]. However, the relationship between cerebral energy metabolism and PbtO2 is still uncertain, and data are lacking regarding the lowest level of PbtO2 compatible with preserved cerebral energy metabolism [6].
To our knowledge, no study has investigated the relationship between the regional metabolism and tissue oxygen tension in a controlled experimental setting. The present study was designed a) to explore the correlation between PbtO2 and cerebral energy metabolism expressed by the LP ratio, and b) to define the lowest PbtO2 level compatible with intact energy metabolism.
The study was conducted in an animal model simulating an acute subdural hematoma (ASDH) adapted from Timaru-Kast et al. [7]. This model of focal cerebral damage has been shown to give a reproducible increase in ICP and decrease in PbtO2, as well as a significant impact on the cerebral energy metabolism similar to that seen in human traumatic brain injury.
Materials and Methods
Animals and Anesthesia
All experiments were approved by the local ethics committee and carried through in accordance with the Danish “Animal Experiment Inspectorate” (Dyreforsøgstilsynet). Ten female pigs (Danish Breed), weighing 49.1 ± 8.2 kg, were included in the study. The animals were sedated with i.m. medetomidine 0.04 mg/kg, midazolam 0.2 mg/kg, and atropine 0.05 mg/kg. Anesthesia was induced with propofol 10 mg/ml i.v. until adequate sedation was achieved. The animals received oral endotracheal intubation and were ventilated mechanically. Anesthesia was maintained with 2.5–3.5% sevoflurane in an oxygen-air mixture adapted to maintain PaO2, PaCO2, and pH within physiological limits (FiO2 ≅ 40%). The temperature was held constant at 36.6 ± 0.1°C. A continuous slow infusion of isotonic glucose i.v. kept blood glucose within physiological range.
After establishing anesthesia, a bladder catheter was inserted, and the right femoral artery was cannulated for blood pressure monitoring, blood gas sampling, and withdrawal of blood for the ASDH. The skull was exposed and a craniotomy (∅ = 15 mm) was carefully drilled over the left frontal cortex, the center of the craniotomy lying 1 cm ventral of the coronal suture, and 1 cm lateral of the sagittal suture. This side was denoted “bad-side” (in terms of regional metabolism).
After exposing the dura, a small incision was made, and a catheter (∅ = 1.5 mm) was inserted subdurally 5 mm for later creation of the ASDH. At a distance of 1.5 cm posterior to the center of the craniotomy, two burr holes (∅ = 2.7 mm) were made for the implantation of the PbtO2 and the microdialysis probes. Directly opposite in the contralateral hemisphere (denoted as “good-side,” again in terms of regional metabolism) two additional burr holes were made for implantation of microdialysis and PbtO2 probes. A burr hole was placed frontally in the “good-side” for ICP monitoring (Fig. 1). The craniotomy and the burr holes were closed with bone-wax, which also served the purpose of fixating the catheter as well as the microdialysis and PbtO2 probes. At the end of experiment, the animals were killed with an i.v. injection of sodium pentobarbital 200 mg/ml in concentrated ethanol (Veterinærapoteket, Københavns Universitet), Copenhagen, Denmark.
Multimodal Monitoring
Heart rate, mean arterial blood pressure (MAP), and pharyngeal temperature were measured continuously. Arterial blood gases (PaCO2, PaO2, and pH) and blood glucose were measured hourly.
For ICP measuring, a Camino® catheter (Integra Neurosciences Ltd., New Jersey, USA) was placed 15 mm into the brain parenchyma fixated with the Camino® bolt. Data was collected by a CAM01 monitor (Integra Neurosciences Ltd. New Jersey, USA), and ICP was monitored continuously. CPP was calculated as MAP-ICP. Data for ICP and CPP are given for every 10 min, except during the first 30 min after the creation of the ASDH when they are given for every minute. PbtO2 was measured with a Licox® probe (Licox CCISB, Integra Neurosciences Ltd. New Jersey, USA) placed 15 mm into the brain parenchyma. Data were collected using the AC3.1 monitor (Integra Neurosciences Ltd.) and recorded every 20 s. Microdialysis probes (CMA70/CMA71, CMA, Stockholm, Sweden) were perfused with artificial CSF (CMA, Stockholm, Sweden) at a rate of 0.3 μl/min (CMA 106 MD pump, CMA, Stockholm, Sweden). The dialyzates were collected in microvials and analyzed for glucose, lactate, pyruvate, glutamate, and glycerol every 20 min using an Iscus Flex analyzer (CMA, Stockholm, Sweden). After insertion, all probes were allowed a minimum of 2 h for stabilization. The base-line levels for the various variables were established during the subsequent 60 min.
Acute Subdural Hematoma
7 ml of autologous blood was withdrawn from the femoral arterial line. The blood was infused through the subdural catheter at a rate of 0.5 ml/min to produce the ASDH. The volume of 7 ml had been determined in a pilot study by using different volumes and infusion rates to cause a substantial increase in ICP without creating signs of fatal brain stem herniation.
Statistical Analysis
All values are expressed as mean ± standard deviation (SD). Baseline mean values and physiological mean values were compared using non-parametric Wilcoxon signed-rank test. Differences between “good-side” and “bad-side” in LP ratio, glutamate, glycerol, and PbtO2 were evaluated using a mixed effect model for repeated measurements with time, side, and baseline as fixed effects and each individual animal and side as random effects. Correlation between LP ratio and PbtO2 and CPP and PbtO2 were investigated using Spearman rank correlation. Since the risk of infarction is related to both depth and duration of cerebral hypoxia [1], area under the curve for each individual animal was calculated for PbtO2 and CPP from 0 to 40 min post trauma. These values were used for the correlations. For the correlation between PbtO2 and LP ratio, the LP at 40 min post trauma was used. Data was analyzed using STATA 11.1 software (StataCorp LP, College Station, USA).
Results
Data obtained from 7 out of 10 experimental animals were included in the analysis. One animal was excluded due to severe arterial hypoglycemia. One animal died approximately 2 h after induction of ASDH. The third animal was excluded as the subdural blood infusion for unknown reasons caused only a minimal increase in ICP.
The baseline levels and post-traumatic levels of blood glucose, PaCO2, PaO2, and arterial pH are presented in Table 1. All variables remained within normal ranges throughout the experiments and did not change significantly.
Baseline levels of ICP and CPP are also presented in Table 1. Immediately after creation of the ASDH, ICP increased significantly and CPP dropped significantly (P < 0.05 for both parameters, Wilcoxon signed-rank sum test).
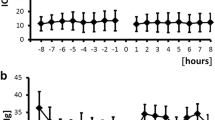
Baseline values of PbtO2 were 37.0 ± 9.8 mmHg and 27.9 ± 7.5 mmHg for “bad-side” and “good-side,” respectively. The difference was statistically significant. After induction of the ASDH, the PbtO2 immediately decreased significantly in both sides (P < 0.001 for both sides, mixed effect model). No statistical difference in PbtO2 between the two sides was found post trauma (Fig. 2a). Owing to the significant differences in baseline values, we also analyzed the time course of PbtO2 as the relative change from baseline. No significant difference between the sides after creation of the ASDH was found using this method (Fig. 2b).
a Change in brain tissue oxygen tension (PbtO2) in “good-side” (solid line) and “bad-side” (dashed line) at baseline and after creation of the ASDH. The ASDH was induced at 60 minutes (arrow). Mixed effect P-values for comparison between the sides after induction of ASDH are given in the figure. Data are shown as mean ± SD indicated by gray shadows. b Relative change in brain tissue oxygen tension (PbtO2 (%)) in “good-side” (solid line) and “bad-side” (dashed line) at baseline and after creation of the ASDH. The ASDH was induced at 60 minutes (arrow). Mixed effect P-values for comparison between the sides after induction of ASDH are given in the figure. Data are shown as mean ± SD indicated by gray shadows
“Good-side” baseline values for LP ratio, glutamate, and glycerol were 14 ± 4, 7 ± 5, and 32 ± 22 μM, respectively. Baseline levels for the “bad-side” were as follows (LP ratio, glutamate, and glycerol): 16 ± 3, 11 ± 5, and 22 ± 12 μM, respectively. There were no statistically significant differences between the two sides in any of the baseline microdialysis variables, and all baseline values were within physiological limits [8]. After induction of the ASDH, the LP ratio, glutamate, and glycerol in the “bad-side” increased significantly over the “good-side” (Figs. 3, 4a,b).
Figure 5 shows the relation between the PbtO2 and LP ratio for the “bad-side” and for the “good-side.” The shaded areas indicate the normal range for the LP ratio. The figure also gives the limit for PbtO2 indicating cerebral ischemia as suggested by the authors listed in the figure [9–17].
The relationship between PbtO2 and LP ratio during the first 120 minutes after creation of ASDH for “good-side” (triangle) and “bad-side” (square). The values are given as the mean PbtO2 value for the corresponding calculated LP ratio values at any given point of time. Horizontal shaded area indicates the physiological limits of the LP ratio in normal brain [8]. The interrupted lines indicate the ischemic threshold for PbtO2 suggested by the authors shown
There was a significant correlation between CPP and PbtO2 in the “bad-side” (r = 0.89, P = 0.02) but not in the “good-side” (r = 0.60, P = 0.21). No significant correlation between PbtO2 and LP ratio was found in either side (r = −0.54, P = 0.22 and r = −0.07, P = 0.87 for bad side and good- side, respectively) (Fig. 6).
The correlation between the area under the curve for PbtO2 and LP ratio in “good-side” (triangle) and “bad-side” (square). The best-fitted regression line is indicated by the solid and dashed lines. The r value is the Spearman rho coefficient. The area under the curve for PbtO2 is calculated in the period 0–40 min post trauma. The LP ratio represents the value obtained at 40 min post trauma
Discussion
The present study was undertaken in an experimental model of focal brain damage, monitored in metabolically both intact and affected tissue. No significant correlation between the PbtO2 and LP ratio could be demonstrated and a lower threshold for PbtO2 under which energy metabolism fails could not be definitely established.
The LP ratio is the balance between cytoplasmatic lactate and pyruvate and can be expressed in terms of the lactate dehydrogenase equilibrium:
During ischemia, the insufficient delivery of oxygen will cause an instantaneous increase in the cytoplasmatic (and interstitial) LP ratio due to the shift in the lactate dehydrogenase equilibrium reaction (Eq. 1). The LP ratio is independent of perfusion flow rate and recovery and is considered to be a robust marker of tissue ischemia [1, 2], but should be interpreted in the light of other markers of tissue ischemia.
Glutamate is the main excitatory transmitter of the central nervous system. After its release into the synaptic cleft, it is rapidly taken up by an energy demanding transport system into the surrounding astrocytes and stored in the transmitter vesicles [18]. Since glutamate is normally rapidly reabsorbed, a significant increase in the intercellular space is a sensitive indicator of jeopardized cerebral energy metabolism and impending cell damage [19]. Accordingly, in the present experiments the increase in interstitial glutamate concentration in the “bad-side” to levels significantly higher than in the “good-side” is interpreted as indicating insufficient energy production while in the “good side” energy metabolism was sufficient (Fig. 4a).
Glycerol is considered as a valuable indicator of cell membrane degradation in the brain [20, 21]. In the present study, the significant increase in the interstitial glycerol concentration in the “bad side” over “good-side,” is interpreted as indicating degradation of cellular membranes while in the “good side” no such degradation was observed (Fig. 4b).
The chemical variables obtained by the microdialysis technique in this study give a comprehensive picture of cerebral energy metabolism and cell membrane degradation. Since the variables measured are not directly chemically interrelated the complete picture obtained can be regarded as a true indicator of impending energy crisis and tissue damage during ischemia. This well-proved method of measuring regional energy metabolism may then be used as a reference for comparing the LP ratio and PbtO2 obtained simultaneously from the same region.
At baseline, the level of PbtO2 was significantly higher in the “bad-side” than in the “good-side.” Since it has been repeatedly shown that PbtO2 is correlated to regional CBF [22], we tentatively assume that the regional CBF was higher on the “bad-side.” The observation is probably explained by the fact that a craniotomy and insertion of the subdural catheter had been performed on this side. Subsequent to the creation of the ASDH, PbtO2 in both sides decreased significantly and almost equally, with no significant difference between the sides (Fig. 2a, b). Inspite of this fact, the LP ratio exhibited a marked and significant increase in the “bad-side” compared with the “good-side” in the same period (Fig. 3). The observed increase in the LP ratio in “bad-side” is paralleled by marked changes in all biochemical variables (Fig. 4a, b). The discrepancy between the PbtO2 values and the LP-ratio obtained in the present study after the creation of the ASDH might be explained if in the “bad-side” the metabolic demands were higher than in the “good-side.” Recent experimental and clinical studies indicate that this is probably the case. The studies have shown that energy-demanding spreading depolarization cycles occur in the penumbra zones surrounding the core lesion (e.g., in traumatic brain lesions, intracerebral hematoma, etc.) and might cause progressive growth of the ischemic region [23]. Under clinical conditions, it has been documented that spreading depolarization causes a decrease in interstitial glucose and increase in lactate [24].
Several authors have, based mainly on clinical observations, suggested a threshold for PbtO2 below which hypoxic/ischemic cerebral damage occurs [9–14]. Their opinions differ from a PbtO2 threshold as high as 23 mmHg [12] down to a critical level at 8.5 mmHg [10] or even 5 mmHg [14]. The suggested threshold levels are compared with the LP ratio of the present study in Fig. 5. As shown in the figure, a PbtO2 of approximately 25 mmHg was found to be related to failing energy metabolism in the “bad-side,” whereas we recorded PbtO2 values as low as 8 mmHg on the “good-side” without increase in the LP ratio.
Figure 6 depicts the AUC value for PbtO2 calculated from 0 to 40 min post trauma plotted against the LP ratio obtained at 40 min post trauma. It has been shown that the risk of unfavorable outcome after severe traumatic brain injury is related to both the depth and duration of episodes with low PbtO2 [14]. We therefore calculated the AUC values in the acute phase after the trauma (0–40 min post trauma), a value that is representative of both the depth and duration of decrease in PbtO2. The figure includes the best-fitted regression line. As shown, no significant correlation exists between the two variables in either side. In the “bad-side” the fitted values describe a tendency toward increasing LP ratio with decreasing AUC. However, in the “good-side,” the fitted line is almost horizontal and does not describe any known physiological relationship (e.g., the intracranial pressure–volume curve or CBF autoregulation curve). It was recently demonstrated that PbtO2 primarily reflects the product of CBF and arteriovenous oxygen tension difference (AVTO2) [25]. These variables do not take regional metabolic rate and the oxygen demand into consideration and therefore explains the lack of relationship between the PbtO2 and energy metabolism.
In the experimental studies, normal values between 15 mmHg and 42 mmHg have been reported [26–28], and tissue oxygen tensions below 5 mmHg have been reported in uninjured rat cortex [1]. In humans, normal values of 48 mmHg [29] were reported during neurosurgical procedures in anesthetized patients. In awake patients undergoing functional neurosurgery, PbtO2 has been shown to be 23.1 ± 6.6 mmHg [30]. The lowest recorded value in that study was 9 mmHg occurring without any clinical signs of regional ischemia. In our study, we recorded baseline values between 19 mmHg and 53 mmHg. The explanation for this great variability in PbtO2 is probably the great physiological variations in CBF between different tissues (white and gray matter) [1] and microvascularity [31]. These observations might further explain the lack of relationship between the tissue oxygen tension and regional metabolism.
A relatively large number of clinical studies have suggested a relation between measured PbtO2 levels and mortality following traumatic brain injuries (TBI) [9–14, 32, 33]. Many of these studies also aimed at defining the thresholds for PbtO2 discussed previously. Some clinical studies have reported a correlation between the regional PbtO2 levels and the functional outcome after TBI [14, 32, 34]. These studies have led to the hypothesis that PbtO2 monitoring could be used for targeting and improving intensive care in severe TBI [34–36]. These reports have recently received support from a study examining whether PbtO2-based therapy was superior to a retrospective series of patients treated according to an ICP/CPP-based therapy [37]. However, two recent publications found that PbtO2-guided therapy did not reduce mortality [38] and was associated with higher use of vasopressors and higher cumulative fluid balance leading to higher ICP and pulmonary edema [39]. The discrepancy might be explained by the results of the present study, showing that the relationship between brain tissue oxygen tension and regional energy metabolism seems to be differentiated depending on probe location and underlying pathology. Yet, another explanation may be that reported PbtO2 values often reflect a global level of oxygenation or CPP. Several authors have documented a close relation between the oxygen saturation of jugular venous blood (SjO2) and PbtO2 [10, 40, 41], and in the present study, we found a significant correlation between PbtO2 and CPP in the “bad-side” (P = 0.02) during the acute phase after creation of the ASDH.
Our study documents that the threshold values for PbtO2 under which energy metabolism fails is variable and most likely depending on the metabolic demands of the tissue. I.e., brain tissue oxygen tension monitoring accurately describes the tension of oxygen in the tissue determined by the blood flow, the blood oxygen tension, and oxygen diffusion through the tissue, but may not under all circumstances disclose whether this oxygen tension is sufficient for maintaining adequate metabolism or not. Under some conditions, PbtO2 might reflect global values such as CPP and global level of oxygenation rather than cerebral energy metabolism. Accordingly, it may not be possible to definitely establish an ischemic threshold for PbtO2 under which energy metabolism fails.
The present study furthermore underlines the importance of defining the positions of catheters used for regional, cerebral, physiological, and biochemical monitoring in relation to the local pathophysiological condition. The data obtained are relevant for this defined location but should not be extrapolated to the whole brain.
Conclusions
The present study in an animal model of focal brain damage demonstrated compromised energy metabolism in a “metabolic penumbra zone” surrounding a focal brain lesion while energy metabolism remained essentially intact in the contralateral hemisphere. While a PbtO2 level of approximately 25 mmHg seemed to be related to failing energy metabolism in the injured side, no such relationship was found in the uninjured side where the PbtO2 levels decreased to equally low values as in the injured side after the brain trauma. Further, no significant correlation between PbtO2 and energy metabolism could be demonstrated. The results indicate that PbtO2 reflects the delivery of oxygen to the tissue but PbtO2 does not under all circumstances disclose whether oxygen delivery is sufficient for energy metabolism or not. Accordingly, we conclude that it may not be possible to define a threshold level for PbtO2 below which energy failure and permanent tissue damage occurs.
References
Siesjö BK. Brain energy metabolism. Chichester [Eng.]; New York: Wiley; 1978.
Amer-Wahlin I, Nord A, Bottalico B, et al. Fetal cerebral energy metabolism and electrocardiogram during experimental umbilical cord occlusion and resuscitation. J Matern Fetal Neonatal Med. 2010;23:158–66.
Bhatia A, Gupta AK. Neuromonitoring in the intensive care unit. II. Cerebral oxygenation monitoring and microdialysis. Intensive Care Med. 2007;33:1322–8.
Nordstrom CH. Cerebral energy metabolism and microdialysis in neurocritical care. Childs Nerv Syst. 2010;26:465–72.
Mazzeo AT, Bullock R. Monitoring brain tissue oxymetry: will it change management of critically ill neurologic patients? J Neurol Sci. 2007;261:1–9.
Nortje J, Gupta AK. The role of tissue oxygen monitoring in patients with acute brain injury. Br J Anaesth. 2006;97:95–106.
Timaru-Kast R, Meissner A, Heimann A, Hoelper B, Kempski O, Alessandri B. Acute subdural hematoma in pigs: role of volume on multiparametric neuromonitoring and histology. J Neurotrauma. 2008;25:1107–19.
Reinstrup P, Stahl N, Mellergard P, Uski T, Ungerstedt U, Nordstrom CH. Intracerebral microdialysis in clinical practice: baseline values for chemical markers during wakefulness, anesthesia, and neurosurgery. Neurosurgery. 2000;47:701–9. discussion 9–10.
van Santbrink H, Maas AI, Avezaat CJ. Continuous monitoring of partial pressure of brain tissue oxygen in patients with severe head injury. Neurosurgery. 1996;38:21–31.
Kiening KL, Unterberg AW, Bardt TF, Schneider GH, Lanksch WR. Monitoring of cerebral oxygenation in patients with severe head injuries: brain tissue PO2 versus jugular vein oxygen saturation. J Neurosurg. 1996;85:751–7.
Zauner A, Doppenberg EM, Woodward JJ, Choi SC, Young HF, Bullock R. Continuous monitoring of cerebral substrate delivery and clearance: initial experience in 24 patients with severe acute brain injuries. Neurosurgery. 1997;41:1082–91. discussion 91–3.
Doppenberg EM, Zauner A, Watson JC, Bullock R. Determination of the ischemic threshold for brain oxygen tension. Acta Neurochir Suppl. 1998;71:166–9.
Valadka AB, Gopinath SP, Contant CF, Uzura M, Robertson CS. Relationship of brain tissue PO2 to outcome after severe head injury. Crit Care Med. 1998;26:1576–81.
van den Brink WA, van Santbrink H, Steyerberg EW, et al. Brain oxygen tension in severe head injury. Neurosurgery. 2000;46:868–76. discussion 76–8.
Johnston AJ, Steiner LA, Coles JP, et al. Effect of cerebral perfusion pressure augmentation on regional oxygenation and metabolism after head injury. Crit Care Med. 2005;33:189–95. discussion 255–7.
Menon DK, Coles JP, Gupta AK, et al. Diffusion limited oxygen delivery following head injury. Crit Care Med. 2004;32:1384–90.
Spiotta AM, Stiefel MF, Gracias VH, et al. Brain tissue oxygen-directed management and outcome in patients with severe traumatic brain injury. J Neurosurg. 2010;113(3):571–80.
Nedergaard M, Takano T, Hansen AJ. Beyond the role of glutamate as a neurotransmitter. Nat Rev Neurosci. 2002;3:748–55.
Samuelsson C, Hillered L, Zetterling M, et al. Cerebral glutamine and glutamate levels in relation to compromised energy metabolism: a microdialysis study in subarachnoid hemorrhage patients. J Cereb Blood Flow Metab. 2007;27:1309–17.
Ungerstedt U, Bäckström T, Hallstrom A. Microdialysis in normal and injured human brain. In: Kinney JM, Tucker HN, editors. Physiology, stress and malnutrition: functional correlates, nutritional intervention. New York: Lippincott-Raven; 1997. p. 361–74.
Hillered L, Valtysson J, Enblad P, Persson L. Interstitial glycerol as a marker for membrane phospholipid degradation in the acutely injured human brain. J Neurol Neurosurg Psychiatry. 1998;64:486–91.
Maloney-Wilensky E, Le Roux P. The physiology behind direct brain oxygen monitors and practical aspects of their use. Childs Nerv Syst. 2010;26:419–30.
Nakamura H, Strong AJ, Dohmen C, et al. Spreading depolarizations cycle around and enlarge focal ischaemic brain lesions. Brain. 2010;133:1994–2006.
Feuerstein D, Manning A, Hashemi P, et al. Dynamic metabolic response to multiple spreading depolarizations in patients with acute brain injury: an online microdialysis study. J Cereb Blood Flow Metab. 2010;30:1343–55.
Rosenthal G, Hemphill JC III, Manley G. Brain tissue oxygen tension is more indicative of oxygen diffusion than oxygen delivery and metabolism in patients with traumatic brain injury. Crit Care Med. 2009;37:379–80.
Manley GT, Pitts LH, Morabito D, et al. Brain tissue oxygenation during hemorrhagic shock, resuscitation, and alterations in ventilation. J Trauma. 1999;46:261–7.
Maas AI, Fleckenstein W, de Jong DA, van Santbrink H. Monitoring cerebral oxygenation: experimental studies and preliminary clinical results of continuous monitoring of cerebrospinal fluid and brain tissue oxygen tension. Acta Neurochir Suppl (Wien). 1993;59:50–7.
Hemphill JC III, Knudson MM, Derugin N, Morabito D, Manley GT. Carbon dioxide reactivity and pressure autoregulation of brain tissue oxygen. Neurosurgery. 2001;48:377–83. discussion 83–4.
Meixensberger J, Dings J, Kuhnigk H, Roosen K. Studies of tissue PO2 in normal and pathological human brain cortex. Acta Neurochir Suppl (Wien). 1993;59:58–63.
Pennings FA, Schuurman PR, van den Munckhof P, Bouma GJ. Brain tissue oxygen pressure monitoring in awake patients during functional neurosurgery: the assessment of normal values. J Neurotrauma. 2008;25:1173–7.
Scheufler KM, Rohrborn HJ, Zentner J. Does tissue oxygen-tension reliably reflect cerebral oxygen delivery and consumption? Anesth Analg. 2002;95:1042–8. Table of contents.
Chang JJ, Youn TS, Benson D, et al. Physiologic and functional outcome correlates of brain tissue hypoxia in traumatic brain injury. Crit Care Med. 2009;37:283–90.
Maloney-Wilensky E, Gracias V, Itkin A, et al. Brain tissue oxygen and outcome after severe traumatic brain injury: a systematic review. Crit Care Med. 2009;37:2057–63.
Meixensberger J, Renner C, Simanowski R, Schmidtke A, Dings J, Roosen K. Influence of cerebral oxygenation following severe head injury on neuropsychological testing. Neurol Res. 2004;26:414–7.
Meixensberger J, Jaeger M, Vath A, Dings J, Kunze E, Roosen K. Brain tissue oxygen guided treatment supplementing ICP/CPP therapy after traumatic brain injury. J Neurol Neurosurg Psychiatry. 2003;74:760–4.
Narotam PK, Morrison JF, Nathoo N. Brain tissue oxygen monitoring in traumatic brain injury and major trauma: outcome analysis of a brain tissue oxygen-directed therapy. J Neurosurg. 2009;111:672–82.
Spiotta AM, Stiefel MF, Gracias VH, et al. Brain tissue oxygen-directed management and outcome in patients with severe traumatic brain injury. J Neurosurg. 2010;113:571–80.
Martini RP, Deem S, Yanez ND, et al. Management guided by brain tissue oxygen monitoring and outcome following severe traumatic brain injury. J Neurosurg. 2009;111:644–9.
Fletcher JJ, Bergman K, Blostein PA, Kramer AH. Fluid balance, complications, and brain tissue oxygen tension monitoring following severe traumatic brain injury. Neurocrit Care. 2010;13:47–56.
Gupta AK, Hutchinson PJ, Al-Rawi P, et al. Measuring brain tissue oxygenation compared with jugular venous oxygen saturation for monitoring cerebral oxygenation after traumatic brain injury. Anesth Analg. 1999;88:549–53.
Gopinath SP, Valadka AB, Uzura M, Robertson CS. Comparison of jugular venous oxygen saturation and brain tissue Po2 as monitors of cerebral ischemia after head injury. Crit Care Med. 1999;27:2337–45.
Acknowledgments
This study was supported by grants from “The Foundation for Medical Research in The County of Funen Island” and “Surgical Training and Research Program at the Faculty of Health Science, University of Southern Denmark.” Licox probes were provided by Mediplast ncnielsen A/S, Denmark. The authors wish to thank the personnel at Biomedical Laboratory, Faculty of Health Science, University of Southern Denmark, for their great assistance and cooperation during the experiments.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nielsen, T.H., Engell, S.I., Johnsen, R.A. et al. Comparison Between Cerebral Tissue Oxygen Tension and Energy Metabolism in Experimental Subdural Hematoma. Neurocrit Care 15, 585–592 (2011). https://doi.org/10.1007/s12028-011-9563-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-011-9563-2