Abstract
Background
Mortality and morbidity have remained high in bacterial meningitis. Impairment of cerebral energy metabolism probably contributes to unfavorable outcome. Intracerebral microdialysis is routinely used to monitor cerebral energy metabolism, and recent experimental studies indicate that this technique may separate ischemia and non-ischemic mitochondrial dysfunction. The present study is a retrospective interpretation of biochemical data obtained in a series of patients with severe community-acquired meningitis.
Methods
Cerebral energy metabolism was monitored in 15 patients with severe community-acquired meningitis utilizing intracerebral microdialysis and bedside biochemical analysis. According to previous studies, cerebral ischemia was defined as lactate/pyruvate (LP) ratio >30 with intracerebral pyruvate level <70 µmol L−1. Non-ischemic mitochondrial dysfunction was defined as LP-ratio >30 at a normal or increased interstitial concentration of pyruvate (≥70 μmol L−1). Patients with LP-ratios <30 were classified as no mitochondrial dysfunction.
Results
The biochemical pattern was in 8 patients (10 microdialysis catheters) classified as no mitochondrial dysfunction, in 5 patients classified as non-ischemic mitochondrial dysfunction, and in 2 patients (3 catheters) classified as ischemia.
Conclusions
In patients with severe community-acquired meningitis, compromised cerebral energy metabolism occurs frequently and was diagnosed in 7 out of 15 cases. A biochemical pattern of non-ischemic mitochondrial dysfunction appears to be a more common underlying condition than cerebral ischemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Community-acquired bacterial meningitis is a medical emergency that may require a multidisciplinary approach. In western world studies, the incidence of meningitis has declined to 4–6 cases per 100,000 adults [1]. However, despite adequate antibiotic therapy, mortality has remained high (20–30 %) [2–4]. The incidence of bacterial meningitis in Sweden was 1.15 cases per 100,000 in 1999, and the same year mortality was reported to be 13 % [5]. As a consequence of the remaining high mortality, several studies have advocated that patients with severe bacterial meningitis should be admitted to departments of critical care medicine with facilities for cerebral multimodal monitoring [5–9].
Various complications contribute to mortality and morbidity in bacterial meningitis [10, 11]. It has been documented that—especially in meningitis caused by Streptococcus pneumoniae—cerebrovascular complications and cerebral infarction occur relatively frequently [10, 12–14]. Further, in animal experiments, septicemia has been shown to cause mitochondrial dysfunction [15, 16] and this has also been demonstrated in experimental pneumococcal meningitis [17, 18]. Under clinical conditions, an association between mitochondrial dysfunction and survival of septic shock has been documented [19].
By utilizing intracerebral microdialysis, it is possible to monitor cerebral energy metabolism bedside [20]. The biochemical pattern of cerebral ischemia has been well documented in experimental as well as clinical studies [21, 22]. We have recently defined the biochemical pattern during experimentally induced mitochondrial dysfunction [23, 24]. We have reported a similar pattern of cerebral energy metabolites in patients with large, re-perfused cerebral infarcts [25] and in patients with subarachnoid hemorrhage (SAH) [26]. In the present patient material, intracerebral microdialysis was used as a part of routine multimodal monitoring. The primary aim of the study was to examine whether disturbance of cerebral energy metabolism occurs in community-acquired bacterial meningitis. The biochemical interpretation of ischemia versus non-ischemic mitochondrial dysfunction was performed retrospectively when experimental studies had defined these patterns [23, 24]. To the best of our knowledge, this is the first bedside study of cerebral energy metabolism in patients with severe community-acquired meningitis.
Materials and Methods
Patient Population
This retrospective, observational study includes all 15 patients with bacterial meningitis who were admitted to the Department of Neurosurgery, Lund University Hospital during 2000–2009. Due to the severity of the clinical picture, these patients were selected from a much larger group with community-acquired meningitis and transferred from local hospitals to a department specialized for neurocritical care. All patients were subjected to multimodality monitoring including continuous monitoring of intracranial pressure (ICP) and cerebral perfusion pressure (CPP) as well as intracerebral microdialysis with bedside biochemical analysis (Table 1). As the incidence of community-acquired meningitis in Sweden during the studied period was estimated to 1.15 cases per 100,000 [5] and as the catchment area for the department of neurosurgery had about 1.3 million inhabitants, the patients included represent about 10 % of the total number of patients with bacterial meningitis in the region. ICP was in all patients recorded with an intraventricular catheter, and mean arterial blood pressure (MAP) was continuously recorded intra-arterially. CPP was calculated as CPP = MAP − ICP. At admittance, all patients were unconscious according to the Glasgow Coma Score (GCS ≤ 8) [27]. All patients were sedated, intubated, and treated with controlled normoventilation (PaCO2 4.0–5.0 kPa; PaO2 11–13 kPa) prior to insertion of the intraventricular catheter as well as the microdialysis catheters. No complications or side-effects caused by the intraventricular or the microdialysis catheters were noted. Doppler ultrasound measurements of blood flow velocity were not performed in the present series of patients. No patient exhibited clinical signs of stroke during the hospitalization.
In four patients, antibiotic therapy started before lumbar puncture (Table 1). In these patients, the responsible physician refrained from initial lumbar puncture as—due to the clinical symptoms—a very high ICP with an increased risk of transtentorial brainstem herniation was suspected. In all patients, intraventricular cerebrospinal fluid (CSF) was sampled for bacteriological culture at insertion of the ventricular catheter.
Management Protocol
Antibiotic therapy was in 14 patients initiated with i.v. infusion of cefotaxim. One patient (patient 7) was initially given meropenem i.v. When indicated the antibiotic therapy was later changed according to the results of bacteriological cultures. Simultaneously with or immediately before the start of antibiotic therapy, all patients were given corticosteroids.
All patients were sedated and intubated with controlled normo-ventilation during the monitoring period. Neuromuscular blockade was not used. Stress response was reduced by liberal use of midazolam (5–20 mg h−1) and fentanyl (2–5 µg kg−1 h−1). Increased ICP was treated according to the protocol (“Lund concept”) used in the department [27, 28]. A CPP of 60–70 mm Hg was usually considered optimal in patients with elevated ICP. During episodes of high ICP and low CPP i.v., infusion of dihydroergotamine was used in three patients [28, 29]. Diuretics (furosemide) and albumin infusion were used to achieve a balanced or moderately negative fluid balance. During the initial 24 h, the patients were given parenteral fluid including glucose containing solutions. All patients were later given a low calorie enteral nutrition. Insulin was administered i.v. to achieve a blood sugar level below 8 mmol L−1 (144 mg dL−1). The principles for treatment of increased ICP as well as the choice of antibiotics were unchanged during the study period.
Cerebral Microdialysis
The microdialysis catheters were inserted into brain tissue via a separate burr-hole in 12 patients. In three patients, two intracerebral microdialysis catheters were inserted simultaneously with hemi- or bifrontal craniectomy. In the patient subjected to bifrontal craniectomy (patient 13), the catheters were placed bilaterally in the frontal lobes.
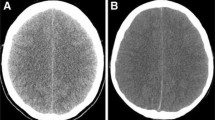
Microdialysis was performed utilizing CMA 70 catheters (cut-off 20 kDa; CMA Microdialysis, Stockholm, Sweden) as described previously [20]. Since 2001 the catheters are equipped with radiopaque gold tips. The positions of the catheters were in these patients (N = 14) verified by post-operative CT-scanning. The microdialysis catheters were perfused (Perfusion Fluid, CMA Microdialysis) at a rate of 0.3 μL min−1, and the perfusates were collected in capped microvials at one-hour intervals. The samples were immediately analyzed for glucose, pyruvate, lactate, glutamate, and glycerol utilizing conventional enzymatic techniques (CMA 600 or ISCUS Microdialysis Analyzer), and the results were displayed on a bedside monitor. The calculated lactate/pyruvate ratio (LP ratio) was used for evaluation of the cytoplasmatic redox state. All data obtained from cerebral microdialysis were integrated with global biochemical and physiological data utilizing a specially developed computer program (ICU-pilot, CMA Microdialysis, Stockholm, Sweden). The Ethical Committee of Lund University Medical Faculty approved the use of multiple intracerebral microdialysis catheters in 1991, and since 1995 intracerebral microdialysis has been used as a routine technique during neurocritical care.
Baseline (normal) biochemical levels for the variables were obtained from published data regarding normal human cerebral tissue [20]. The biochemical pattern obtained was used to classify the patients into the three groups of ischemia, non-ischemic mitochondrial dysfunction, and no mitochondrial dysfunction, respectively. These classifications were based on previous data obtained during experimentally induced mitochondrial dysfunction [23, 24]. The group of no mitochondrial dysfunction was defined as patients with LP ratios within normal mean level +2 SD (LP-ratio ≤30). Ischemia was defined as a pathological increase in LP ratio (LP-ratio >30) simultaneously with interstitial pyruvate concentration below normal level −2 SD (LP-ratio >30; pyruvate <70 μmol L−1). Non-ischemic mitochondrial dysfunction was defined as a pathological increase in LP-ratio (LP-ratio >30) simultaneously with a normal or increased interstitial concentration of pyruvate (pyruvate ≥70 μmol L−1). The study includes 1,212 microdialysis samples and approximately 6,000 bedside biochemical analyses. Microdialysis with bedside biochemical analysis was performed during altogether 1,090 h (min. 20 h; max. 145 h).
Statistical Analysis
All values are expressed as median (interquartile rage). Statistical comparison of the median levels of microdialysis variables between the group defined as non-ischemic mitochondrial dysfunction (N = 5) and the group defined as no mitochondrial dysfunction (N = 10) was performed by utilizing the non-parametric Wilcoxon Rank-Sum test. A p value below 0.05 was considered significant. As the p values are to be considered exploratory, no adjustment for generating multiple p values was performed. Stata 11 statistical software package (StataCorp LP, College Station, TX, USA) was used for data analysis.
Results
Basic Clinical Data
Basic clinical data are presented in Table 1. Median age for the patients included was 26 year (interquartile range 10 and 58 year). In eight of the patients, focal neurological symptoms were observed. One patient of the 15 patients died within 24 h after arrival to the department of neurosurgery. This patient (patient 13) deteriorated rapidly after lumbar puncture in the local hospital, and at arrival to the department of neurosurgery, he was GCS 3 with wide, non-reacting pupils. In addition to the non-surgical therapy described above this, patient was treated with bifrontal craniectomy. He was declared dead approximately 24 h after arrival. Two additional patients were subjected to hemicraniectomy due to intractable increase in ICP (patients 6 and 11). In one case (patient 8), a subdural empyema was evacuated.
Median ICP at insertion of the ventricular catheter was 11 mmHg (interquartile range 8 and 26 mmHg) (Table 1). In five patients, the initial ICP after insertion of the ventricular catheter was >20 mmHg. The changes over time for mean CPP ± SEM and mean ICP ± SEM during the initial 48 h are shown in Fig. 1. The tendency to increase in mean ICP during the time period 12–24 h was caused by the pronounced elevation of ICP in patient 13. During the initial 48 h median, CPP was 78 mmHg (interquartile range 68 and 85 mmHg). For ICP the corresponding figure was 7 mmHg (interquartile range 4 and 13 mmHg).
In seven patients, the meningitis was caused by S. pneumoniae, in two patients it was caused by Neisseria meningitidis, and in two patients the etiology remained unknown (Table 1). In one patient (patient 9), the diagnosis of meningitis was delayed for 24 h as the initial clinical picture and CT-scanning was initially interpreted as SAH.
Pattern of Biochemical Variables Obtained by Microdialysis
According to the definitions given previously, the biochemical pattern was in 8 patients (10 microdialysis catheters) classified as no mitochondrial dysfunction, in 5 patients classified as non-ischemic mitochondrial dysfunction, and in 2 patients (3 catheters) classified as ischemia. In one of the patients of the latter group, the pattern of ischemia occurred during the initial 4 h of monitoring. In all but one of the patients classified as non-ischemic mitochondrial dysfunction, the LP ratio normalized during the observation period. In three of the patients in this group, the increase of the LP ratio was associated with a marked increase in intracerebral glycerol level, and in two of these patients the level of glutamate was simultaneously elevated. Table 2 gives the median levels of the variables and the interquartile range during the time periods the patients fulfilled the definitions of the three groups. The pattern classified as non-ischemic mitochondrial dysfunction was recorded during altogether 182 h. The pattern of ischemia was observed during 27 h.
For the group defined as no mitochondrial dysfunction, all five biochemical variables as well as the calculated LP ratio were close to the corresponding data from normal human brain [20]. By definition the LP ratio was significantly increased in the group defined as non-ischemic mitochondrial dysfunction. In this group, interstitial pyruvate concentration was not significantly different from the group of no mitochondrial dysfunction but the concentration of lactate was significantly increased (Table 2). Median interstitial glucose level was lower, and glycerol and glutamate were increased in patients classified as non-ischemic mitochondrial dysfunction but the differences reached statistical significance only for glutamate.
In two patients, the biochemical pattern was classified as ischemia. In the first patient, (patient 13) pyruvate level was close to detection level and, accordingly, the calculated LP ratio was very high. Interstitial glucose was close to detection level; lactate concentration was increased, and the levels of glycerol and glutamate were very high. The time courses for some of the monitored variables are shown in Fig. 2 illustrating the time course of progressive ischemia. In spite of bifrontal craniectomy and pharmacological therapy, ICP and LP ratio were above normal levels, and CPP was low (33 mmHg) already at initiation of monitoring. With increasing ICP, the LP ratio increased to a very high level and a few hours after the pronounced increase of the LP ratio glycerol and glutamate increased markedly. Later than 8 h after start of monitoring, CPP was below 20 mmHg. The second patient (patient 15) exhibited a biochemical pattern of ischemia during the initial 3 h with a median LP ratio of 35 and a median pyruvate level of 46 µmol L−1. During this period, CPP was quite low (50–55 mmHg) due to an initially very high ICP (30–40 mmHg). The biochemical pattern normalized when ICP—due to the therapy presented above—was reduced below 20 mmHg. Within 5 days, the patient’s clinical state had recovered completely.
The pattern of progressive ischemia (patient 13) illustrated by the increase in intracranial pressure (ICP) and the simultaneous changes in lactate/pyruvate (LP) ratio as well as interstitial changes in the levels of glycerol and glutamate obtained by intracerebral microdialysis. The normal ranges (mean ± SD) for the variables according to Reinstrup et al. [20] are indicated on the y axis
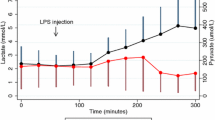
A biochemical pattern typical of non-ischemic mitochondrial dysfunction is shown in Fig. 3 (patient 14). During the 36 h period illustrated in the figure median ICP was 8 mmHg (interquartile range 6 and 10 mmHg). During this period, median LP ratio was 40 (min/max 31/48), median glucose was 1.0 mmol L−1 (min/max 0.6/1.4 mmol L−1), median pyruvate 159 µmol L−1 (min/max 120/223 µmol L−1), and median glutamate 87 µmol L−1 (min/max 71/118 µmol L−1).
The pattern of non-ischemic mitochondrial dysfunction (patient 14) illustrated by the lactate/pyruvate (LP) ratio as well as interstitial changes in the levels of glucose, pyruvate and glutamate obtained by intracerebral microdialysis. The normal ranges (mean ± SD) for the variables according to Reinstrup et al. [20] are indicated on the y axis
Discussion
In this study, we use the levels of lactate and pyruvate obtained from intracerebral microdialysis to diagnose and separate cerebral ischemia and non-ischemic mitochondrial dysfunction bedside. The intracellular LP ratio reflects the cytoplasmatic redox state which is primarily determined by mitochondrial function. An increase of the LP ratio occurs during insufficient blood supply (ischemia) due to a decrease of oxygen as well as substrate resulting in a very low level of pyruvate [21, 22, 30]. An increase of the LP ratio also occurs during arterial hypoxia and primary mitochondrial dysfunction. In both of these situations blood supply and delivery of substrate continues and, accordingly, the concentration of pyruvate will increase or remain normal due to the increased rate of anaerobic glycolysis [23–25, 31, 32]. As routine analysis of arterial pO2 reveals arterial oxygenation microdialysis and bedside biochemical analysis of lactate and pyruvate can be used to diagnose and separate cerebral ischemia and non-ischemic mitochondrial dysfunction under clinical conditions.
In the present study, this method of analysis was used in a group of patients with severe community-acquired cerebral meningitis. As shown in Table 1, the bacteriological etiology in our selected group of patients corresponded to the distribution observed in large studies [1]. The severity of the conditions is documented by the fact that all patients were unconscious (GCS ≤ 8) at admittance and that many patients exhibited serious focal neurological symptoms (Table 1). In spite of the severity of the clinical state initial, ICP was above 20 mmHg in only five patients and median ICP was normal (11 mmHg). Since all patients were sedated and intubated with controlled normoventilation before insertion of the ventricular catheters, these interventions are probably often sufficient to control elevated ICP in severe bacterial meningitis.
Microdialysis reflects the biochemical condition of the interstitial space, and the LP ratio obtained is supposed to reflect the cytoplasmatic redox state. Lactate and pyruvate pass cell membranes by proton-linked monocarboxylate transporters (MCTs) [33]. The efficacy of the MTCs in transmembrane transport of lactate and pyruvate appears to be high: it is well documented that cerebral ischemia causes an instantaneous increase in interstitial LP ratio that reflects the intracellular shift in redox state. As the capacity of the H+-monocarboxylate transporter across cell membranes is very high, the LP ratio obtained from cellular interstitial fluid by microdialysis reflects the intracellular redox state [30].
In the present study, a pattern of cerebral ischemia was observed only during increased ICP. The pattern of cerebral ischemia was paralleled by increases in glutamate and glycerol (Table 2; Fig. 2). Interstitial glutamate concentration is under normal circumstances kept at a very low level due to an energy demanding re-uptake into surrounding astrocytes [33, 35]. Increase in interstitial glutamate concentration may thus be interpreted as a sign of energy deficiency [36]. During cell membrane degradation, the glycerophospholipids of the cell membranes are split into glycerol and free fatty acids. Cerebral interstitial glycerol level may accordingly be used as a marker of degradation of cellular elements [37, 38].
In patients classified as non-ischemic mitochondrial dysfunction, LP ratio was above normal and significantly higher than in the group of no mitochondrial dysfunction due to a marked increase in lactate concentration while pyruvate was within normal limits (Table 2). The biochemical pattern of mitochondrial dysfunction was observed when ICP was within normal limits. The significant increase in glutamate and the tendency to increase glycerol levels may indicate that these patients are at risk for secondary cellular damage e.g., during a temporary decrease in CPP.
The mechanisms underlying non-ischemic mitochondrial dysfunction in severe bacterial infections are incompletely understood. Since long it has been known that in experimental sepsis the yield of cytochromes b, c, and a (a3) is markedly decreased in muscle mitochondria and that ATP synthesis rate is significantly reduced [15]. Recent experimental studies have shown that pneumococcal meningitis induces mitochondrial chain complex I inhibition in the brain that was interpreted as causing impairment of energy metabolism contributing to the pathogenesis [18]. In septic patients, an association between mitochondrial dysfunction and ATP depletion has been reported to be related to organ failure and impaired clinical outcome [17]. However, opinions differ regarding the clinical importance of mitochondrial dysfunction in these conditions. In a recent review, it was pointed out that mitochondrial function is highly variable in sepsis and that data from young, healthy animals have not supported the view that mitochondrial dysfunction is the general denominator for multiple organ failure [16].
The metabolic patterns in the present study may be compared with observations in patients with severe brain trauma and SAH. In pericontusional tissue, increased LP ratio is frequently not caused by a reduction of regional blood flow, and accordingly ischemia is probably only part of the explanation of disturbed energy metabolism. In patients with SAH, a metabolic pattern indicating mitochondrial dysfunction was recently described as more common than that of ischemia [26].
Limitations of the Study
The study included a selected group of patients with severe bacterial meningitis. It is likely that the frequency of impaired cerebral energy metabolism is higher in this group than in the larger group of patients with less severe clinical symptoms. As the microdialysis technique gives biochemical information selectively from a narrow zone surrounding the catheter and cerebral ischemia occurring outside this zone will not be detected. Although cerebral ischemia may be more frequent than observed in this study, it is reasonable to assume that mitochondrial dysfunction occurs more often than ischemia.
Conclusions
In patients with severe community-acquired meningitis, compromised cerebral energy metabolism appears to be relatively frequent and was observed in 7 out of 15 cases. In these patients, a biochemical pattern indicating non-ischemic mitochondrial dysfunction was more common than a pattern cerebral ischemia. The clinical relevance of non-ischemic mitochondrial dysfunction in bacterial meningitis and its influence on clinical outcome remain to be clarified.
References
Van de Beek D, de Gans J, Tunkel AR, Wijdicks EFM. Community-acquired bacterial meningitis in adults. N Engl J Med. 2006;354:44–53.
Lindvall P, Ahlm C, Ericsson M, Gothefors L, Naredi S, Koskinen LO. Reducing intracranial pressure may increase survival among patients with bacterial meningitis. Clin Infect Dis. 2004;38:384–90.
Aronin S, Peduzzi P, Quagliarello VJ. Community-acquired bacterial meningitis: risk stratification for adverse clinical outcome and effect of antibiotic timing. Ann Intern Med. 1998;129:862–9.
Durand ML, Calderwood SB, Weber DJ, et al. Acute bacterial meningitis in adults. a review of 493 episodes. N Engl J Med. 1993;328:21–8.
Van de Beek D, de Gans J, Spanjaard L, Weisfelt M, Reitsma JB, Vermeulen M. Clinical features and prognostic factors in adults with bacterial meningitis. N Engl J Med. 2004;351:1849–59.
Flores-Cordero JM, Amaya-Villar R, Rincón-Ferrari MD, et al. Acute community-acquired meningitis in adults admitted to the intensive care unit: clinical manifestations, management and prognostic factors. Int Care Med. 2003;29:1967–73.
Zimmerli W. Acute bacterial meningitis: time for a better outcome. Int Care Med. 2003;29:1868–70.
Baussart B, Cheisson G, Compain M, et al. Multimodal cerebral monitoring and decompressive surgery for the treatment of severe bacterial meningitis with increased intracranial pressure. Acta Anaesthesiol Scand. 2006;50:762–5.
Edberg M, Furebring M, Sjölin J, Enblad P. Neurointensive care of patients with severe community-acquired meningitis. Acta Anaesthesiol Scand. 2011;55:732–9.
Kastenbauer S, Pfister HW. Pneumococcal meningitis in adults. Spectrum of complications and prognostic factors in a series of 87 cases. Brain. 2003;126:1015–25.
Weisfelt M, van de Beek D, Spanjaard L, Reitsma JB, de Gans J. A risk score for unfavourable outcome in adults with bacterial meningitits. Ann Neurol. 2008;63:90–7.
Katchanov J, Heuschmann PU, Endres M, Weber JR. Cerebral infarction in bacterial meningitis: predictive factors and outcome. J Neurol. 2010;257:716–20.
Vergouwen MDI, Schut ES, Troost D, van de Beek D. Diffuse cerebral intravascular coagulation and cerebral infarction in pneumococcal meningitis. Neurocrit Care. 2010;13:217–27.
Shut ES, Lucas MJ, Brouwer MC, Vergouwen MDI, van der Ende A, van de Beek D. Cerebral infarction in adults with bacterial meningitis. Neurocrit Care. 2012;16:421–7.
Tavakoli H, Mela L. Alterations of mitochondrial metabolism and protein concentrations in subacute septicemia. Infect Immun. 1982;38:536–41.
Brealey D, Brand M, Hargreavens I, et al. Association between mitochondrial dysfunction and severity and outcome of septic shock. Lancet. 2002;360:219–23.
Barichello T, Savi GD, Simöes LR, et al. Evaluation of mitochondrial respiratory chain in the brain of rats after pneumococcal meningitis. Brain Res Bull. 2010;82:302–7.
Barichello T, Generoso JS, Collodel A, Moreira AP, de Almeida SM. Patophysiology of acute meningitis caused by Streptococcus pneumoniae and and junctive therapy approaches. Arq Neuropsiquiatr. 2012;70:366–72.
Jeger W, Djafarzadeh S, Jakob SM, Takala J. Mitochondrial function in sepsis. Eur J Clin Invest. 2013;43:532–42.
Reinstrup P, Stahl N, Mellergard P, et al. Intracerebral microdialysis in clinical practice: baseline values for chemical markers during wakefulness, anesthesia, and neurosurgery. Neurosurgery. 2000;47:701–9.
Amer-Wahlin I, Nord A, Bottalico B, et al. Fetal cerebral energy metabolism and electrocardiogram during experimental umbilical cord occlusion and resuscitation. J Matern Fetal Neonatal Med. 2010;23:158–66.
Ståhl N, Mellergård P, Hallström Å, Ungerstedt U, Nordström CH. Intracerebral microdialysis and bedside biochemical analysis in patients with fatal traumatic brain lesions. Acta Anaesthesiol Scand. 2001;45:977–85.
Nielsen TH, Bindslev TT, Pedersen SM, Toft P, Olsen NV, Nordstrom CH. Cerebral energy metabolism during induced mitochondrial dysfunction. Acta Anaesthesiol Scand. 2013;57:229–35.
Nielsen TH, Olsen NV, Toft P, Nordström CH. Cerebral energy metabolism during mitochondrial dysfunction induced by cyanide in piglets. Acta Anaesthesiol Scand. 2013;57:793–801.
Nielsen TH, Schalén W, Ståhl N, Toft P, Reinstrup P, Nordström CH. Bedside diagnosis of mitochondrial dysfunction after malignant middle cerebral artery infarction. Neurocrit Care. 2013. doi:10.1007/s12028-013-9875-5.
Jacobssen A, Nielssen TH, Nilsson O, Schalén W, Nordström CH. Bedside diagnosis of mitochondrial dysfunction in subarachnoid hemorrhage. Acta Neurol Scand. 2014. doi:10.1111/ane.12258.
Teasdale G, Jennett B. Assessment of coma and impaired consciousness: a practical scale. Lancet. 1974;7872:81–4.
Asgeirsson B, Grände PO, Nordström CH. A new therapy of post-trauma brain oedema based on haemodynamic principles for brain volume regulation. Intensive Care Med. 1994;20:260–7.
Grände PO, Asgeirsson B, Nordström CH. Volume targeted therapy of increased intracranial pressure: the Lund concept unifies surgical and non-surgical treatments. Acta Anaesthesiol Scand. 2002;46:929–41.
Siesjö BK. Brain energy metabolism. Chichester: Wiley; 1978.
Nordström CH, Rehncrona S, Siesjö BK. Restitution of cerebral energy state, as well as of glycolytic metabolites, citric acid cycle intermediates and associated amino acids after 30 minutes of complete ischemia in rats anaesthetized with nitrous oxide or phenobarbital. J Neurochem. 1978;30:479–86.
Nordström CH, Rehncrona S, Siesjö BK. Effects of phenobarbital in cerebral ischemia. Part II: restitution of cerebral energy state, as well as of glycolytic metabolites, citric acid cycle intermediates and associated amino acids after pronounced incomplete ischemia. Stroke. 1978;9:335–43.
Pierre K, Pellerin L. Monocarboxylate transporters in the central nervous system: distribution, regulation and function. J Neurochem. 2005;94:1–14.
Anderson CM, Sanson RA. Astrocyte glutamate transport: review of properties, regulation and physiological function. Glia. 2000;32:1–14.
Nedergaard M, Takano T, Hansen AJ. Beyond the role of glutamate as a neurotransmitter. Nat Rev Neurosci. 2002;3:748–55.
Samuelsson C, Hillered L, Zetterling M, et al. Cerebral glutamine and glutamate levels in relation to compromised energy metabolism: a microdialysis study in subarachnoid hemorrhage patients. J Cereb Blood Flow Metab. 2007;27:1309–17.
Ungerstedt U, Bäckström T, Hallström Å, Grände PO, Mellergård P, Nordström CH. Microdialysis in normal and injured human brain. In: Kinney JM, Tucker HN, editors. Physiology, stress, and malnutrition: functional correlates. Philadelphia NY: Nutritional Intervention. Lippincott-Raven Publishers; 1997. p. 361–74.
Hillered L, Valtysson J, Enblad P, Persson L. Interstitial glycerol as a marker for membrane phospholipid degradation in the acutely injured human brain. J Neurol Neurosurg Psychiatry. 1998;64:486–91.
Vespa PM, O’Phelan K, McArthur D, et al. Pericontusional brain tissue exhibits persistent elevation of lactate/pyruvate ratio independent of cerebral perfusion. Crit Care Med. 2007;35:1153–60.
Acknowledgments
We thank Katarina Nielsen, Department of Neurosurgery, Lund University Hospital, for help with the microdialysis equipment and the biochemical analyses. The study was supported by grants from Lund University Hospital, Odense University Hospital and University of Southern Denmark.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Poulsen, F.R., Schulz, M., Jacobsen, A. et al. Bedside Evaluation of Cerebral Energy Metabolism in Severe Community-Acquired Bacterial Meningitis. Neurocrit Care 22, 221–228 (2015). https://doi.org/10.1007/s12028-014-0057-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-014-0057-x