Abstract
Background
Targeted temperature management (TTM) represents the standard of care in comatose survivors after cardiac arrest (CA) and may be applied targeting 33° or 36 °C. While multimodal prognostication has been extensively tested for 33 °C, scarce information exists for 36 °C.
Methods
In this cohort study, consecutive comatose adults after CA treated with TTM at 36 °C between July 2014 and October 2016 were included. A combination of neurological examination, electrophysiological features, and serum neuron-specific enolase (NSE) was evaluated for outcome prediction at 3 months (mortality; good outcome defined as cerebral performance categories (CPC) score of 1–2, poor outcome defined as CPC 3–5).
Results
We analyzed 61 patients. The presence of two or more predictors out of, unreactive electroencephalogram (EEG) background, epileptiform EEG, absent pupillary and/or corneal reflex, early myoclonus, bilaterally absent cortical somatosensory evoked potentials, and serum NSE >75 μg/l, had a high specificity for predicting mortality (positive predictive value [PPV] = 1.00, 95% CI 0.87–1.00) and poor outcome (PPV = 1.00, 95% CI 0.80–1.00). Reactive EEG background was highly sensitive for predicting good outcome (0.95, 95% CI 0.74–0.99).
Conclusions
Prediction of outcome after CA and TTM targeting 36 °C seems valid in adults using the same features tested at 33 °C. A reactive EEG under TTM appears highly sensitive for good outcome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiac arrest (CA) has an annual incidence of 50-110/100000 [1], with an approximately 10% successful resuscitation rate [2] and a remarkable mortality decrease in hospitalized patients in the last few years [3]. Targeted temperature management (TTM), with therapeutic hypothermia (TH) to 33 °C [4] or more recently targeting 36 °C [5], has likely contributed to this trend [6]. In this setting, clinicians are expected to quickly and accurately provide predictions of survivors’ outcome.
Several predictors have been standardized following TH. Specifically, bilateral absence of brainstem reflexes, absence of motor response to pain and treatment-resistant myoclonus [7–10], unreactive or discontinuous electroencephalogram (EEG) background activity [10–12], bilateral absence of N20 somatosensory evoked potentials (SSEP) [7], and high serum neuron-specific enolase (NSE) [13] is related to poor neurological recovery. However, during TH, sedative medications, and possibly the temperature itself may delay prognostication decision up to several days, especially regarding motor signs [14].
After showing no difference in mortality between survivors treated with TH to 33 °C and survivors treated with 36 °C [5, 15], guidelines for care after CA are changing and foresee the use of TTM, either targeting 33 or 36 °C, depending on patients’ profiles [16]. The above-mentioned predictors (especially clinical examination, possibly also neurophysiological tests, and NSE) are potentially influenced by the temperature degree and associated sedation and myorelaxant medication; therefore, they have been thoroughly tested in patients treated with TTM at 36 °C and showed, individually, their validity in this condition [17–19].
Independently of the TTM target, a multimodal approach of the above-mentioned tests is strongly advocated in order to provide an early and accurate outcome prediction. Our group has focused on this strategy since the TH era and already validated the use of a protocol combining clinical examination and neurophysiological features for making decisions related to continuation of intensive treatment [10, 20]. Relatively little is known, however, regarding such an approach in patients undergoing 36 °C. The aim of our study was to assess accuracy of this multimodal prognostic panel in patients treated with 36 °C.
Methods
Study Subjects and TTM
In this cohort study, we prospectively collected consecutive patients older than 18 years successfully resuscitated after CA (in-hospital: out-of-hospital CA ratio was 1:10), who were managed with TTM in the medical-surgical intensive care unit at the University Hospital of Lausanne, between July 2014 and October 2016. Patients that died within 24 h after CA were excluded. Our institutional ethic committee fully approved this study. Patients were managed with TH until July 2014, then with either TH or 36 °C [5], depending on the patient context until May 2016, and thereafter exclusively with 36 °C. According to our protocol (in analogy to 33 °C) [10], 36 °C target temperature was applied for 24 h using ice packs and intravenous ice-cold fluids together with a surface cooling device (Arctic Sun System, Medivance, Louisville). Passive rewarming began at 24 h. Midazolam (0.1 mg/kg/h) and fentanyl (1.5 μg/kg/h) were given for analgesia-sedation, and vecuronium for shivering.
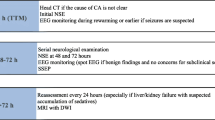
Neurological and Outcome Assessment
Neurological examination, including principal brainstem reflexes (pupillary, oculocephalic, corneal) and motor reactivity to pain stimulation, was assessed by a certified neurologist after interruption of TTM and weaning of pharmacological sedation (at least twice between 36 and 72 h after CA, or more often if needed). EEG recordings were assessed during (at least 6 h after CA, under TTM and sedation), and early after TTM, at the time of clinical examination. EEG background reactivity interpretation was performed by two experienced electroencephalographers (JN, AOR). Bilateral median nerve SSEP were recorded at least 24 h after CA. Serum NSE was measured at 24 and 48 h after CA and analyzed with an automated immunofluorescent assay (Thermo Scientific Brahms NSE Kryptor Immunoassay, Hennigsdorf, Germany). Withdrawal of care was decided using a multidisciplinary approach if two or more of the following criteria were present after TTM and after sedation was withdrawn [10]: 1. Unreactive EEG background 2. Treatment-resistant myoclonus, 3. Bilateral absence of N20 in SSEP, or 4. Incomplete return of brainstem reflexes.
Outcome at 3 months was assessed through a semi-structured phone interview using cerebral performance categories (CPC) [21, 22]: CPC 1 indicates full recovery; CPC 2 moderate disability; CPC 3 severe disability; CPC 4 coma or persistent vegetative state; and CPC 5 death. Poor neurological outcome was defined as CPC 3–5.
Data Collection and Variable Definitions
CA etiology was dichotomized as cardiac and non-cardiac, and initial arrest rhythm as ventricular fibrillation (VF) and non-VF (asystole and pulseless electrical activity). Time to return of spontaneous circulation was based on paramedics’ reports. The best clinical features of the clinical assessments performed within the first 72 h were used for analysis. Early myoclonus was retained if occurred in the first 24 h after weaning of sedation, or if seen earlier. Treatment-resistant myoclonus was defined as persistent despite treatment with at least two antiepileptic drugs [23]. EEG reactivity was assessed with bilateral nipple pinching and was defined as a reproducible change in amplitude or frequency, excluding stimulus-induced rhythmic, periodic, or irritative discharges and muscle artifacts [24, 25]; epileptiform activity as any repetitive periodic or rhythmic spikes, or sharp waves, or spike-waves [26]. The N20 (cortical) responses on SSEP were categorized as present or bilaterally absent, regardless of the amplitude. The NSE peak level was considered for the purpose of this study. All variables were collected prospectively according to the Utstein style [27].
Statistical Analysis
The cohort was analyzed using Fischer, Student’s t and Mann–Whitney U tests as needed. Specificity, sensitivity, positive predictive value (PPV), and negative predictive value (NPV) were assessed for poor outcome (CPC 3–5), using an exact binomial 95% confidence interval (CI), for unreactive first (during TTM) EEG background, epileptiform first EEG, absence of pupillary and/or corneal reflex, early myoclonus, bilaterally absent N20 on SSEP, and NSE level above 75 μg/l [20]. To evaluate the performance of all above-mentioned variables, both for mortality and poor neurological outcome, unweighted accuracies and areas under receiver operating characteristic (ROC) curves were calculated. Finally, we explored the value of a reactive first EEG background for good (CPC 1–2) outcome. Calculations were performed with Stata software, version 12 (College Station, TX). Significance was set at p < 0.05.
Results
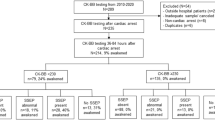
From July 2014 to October 2016, 137 patients have been successfully resuscitated after CA and admitted to our intensive care unit; 61 of them (the object of this study) were treated with TTM at 36 °C, and the other 76 were treated at 33 °C. Table 1 shows their demographics and clinical characteristics.
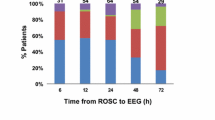
Table 2 illustrates predictors of poor outcome: All had high PPV but early myoclonus, epileptiform EEG, bilaterally absent N20, and NSE level above 75 μg/l correlated with no false positivity. On the other hand, a reactive EEG background activity represented a sensitive predictor of good outcome for both groups as shown in Table 3.
Testing the multimodal approach, the presence of two or more of the above-mentioned parameters had a high specificity for predicting both poor outcome and mortality (Table 4). This was confirmed by the ROC curves (Table 4a, b, Fig. 1).
Prognostic value of the multimodal approach for prediction poor outcome using the receiver operator characteristic (ROC) curves (presence of two or more variables among unreactive first EEG background, epileptiform first EEG, absent pupillary and/or corneal reflex, early myoclonus bilaterally absent SSEP, and NSE > 75 μg/l). EEG Electroencephalogram, NSE Neuron-specific enolase, SSEP Somatosensory evoked potentials
Discussion
These findings suggest that early multimodal prediction of mortality and poor functional outcome in survivors after CA is reliable in patients after TTM at 36 °C with parameters routinely used at 33 °C. Furthermore, a reactive EEG under TTM at 36 °C and sedation seems highly sensitive for predicting good outcome in both conditions.
Medical decisions in this clinical setting should never be based on isolated tests, and the need of a multimodal approach is widely recommended [28–30]. Recent studies assessed outcome predictors comparing 33 versus 36 °C, mostly generated by the TTM trial [5, 31] (for a detailed discussion, see below); however, they focused on isolated tests and not on multimodality. Our findings show high specificity of a first unreactive EEG background for predicting poor outcome at 36 °C. Besides background amplitude [32, 33], reactivity has been repeatedly described [10, 12, 25, 34, 35]; however, as opposed to this study, those descriptions rely on patients treated with 33 °C, and the first EEG recorded during TTM is generally not included as a predictor in current recommendations [29, 36]. We acknowledge that lack of standardized stimulations [24] remains a relevant limitation. On the other hand, early epileptiform EEG features during TTM accurately predicted poor outcome, with no false positives. This is already known after TTM at 33 °C [10, 11], and during hypothermia and sedative medications with antiepileptic effect [20, 28, 37]. The role of EEG background reactivity for good outcome has recently been shown after 33 °C [10, 20, 35] and this study confirms the same for the 36 °C group. Finally, bilateral absence of the N20 response in SSEP is highly correlated with poor outcome after CA and TTM [7, 20]; this study’s findings confirm with these previous results in both temperature groups.
Clinical examination represents a paramount test in this setting. Bilateral absence of pupillary or corneal reflexes as well as early myoclonus are already recognized outcome predictors after 33 °C [8, 10, 31] and are confirmed by this study for 36 °C. The absence of a motor response to pain represented an important test before TTM era [8], but its early evaluation in TTM is altered from myorelaxant or sedative medication [10, 38]. Early myoclonus is consistently associated with poor outcome [8, 9], but a careful assessment is necessary in order to avoid wrong therapeutic decisions in patients with treatable postanoxic Lance-Adams syndrome. Furthermore, some isolated cases of good prognosis after treatment have been described [23, 39], underscoring the importance of multimodality.
High serum NSE levels reflect the degree of brain damage after CA. Prior to the TH era, a level above 33 μg/l at 48 h after CA was considered robustly predictive of poor outcome [40]. During TTM, this cutoff value has been questioned and a high predictive value of poor outcome has been reported independent of target temperature and with values consistently higher than 33 μg/l [19]. Given the difficulty in identifying clear cutoffs, independent of settings, laboratories, and sedations/temperatures, NSE is currently not routinely used as a core test after CA [28]. Our findings confirm a cutoff of >75 μg/l for poor outcome in TTM at 36 °C with no false positives, in line with our previous work [20].
The presence of two or more of the above-analyzed variables accurately predicted both poor functional outcome and mortality, with very high accuracy in adult patients undergoing TTM at 36 °C. The previously described multimodal approach for predicting poor outcome was based on EEG recorded after TTM and off sedation [10] (even though, subsequently, EEG during TH was find to be even more accurate [20]) and incomplete brainstem reflexes, and did not take into account epileptiform EEG features or NSE values. Furthermore, the previous method was tested only in patients treated at 33 °C. In view of the present findings, it seems that this approach can be used also in controlled TTM targeting 36 °C.
This study has limitations. In our registry, we unfortunately lack data allowing identification of patients who had decisions of withdrawal of intensive care support, and we recognize that a self-fulfilling prophecy was potentially at play, as several predictors described here were used in practice for decisions on discontinuation of intensive care support. However, this should not apply to EEG (we routinely consider EEG after TTM, but not during TTM) and serum NSE; this should limit the self-fulfilling impact on these variables, albeit—admittedly—all results were available to clinicians. Unfortunately, this sort of problem is inherent to virtually all studies conducted in this clinical setting [10, 27]. We believe that a well-structured multimodal approach represents the only strategy to counteract this problem. Even if it seems highly accurate in the acute phase, this multimodal approach may not be absolutely specific in view of the relatively low number of patients and the 95% confidence intervals. Rapid conclusions should be avoided, especially in doubtful cases. Moreover, this multimodal assessment did not explore which combination of tests was the most accurate, as for this a larger cohort would be necessary. Finally, the serum NSE cutoff value of 75 μg/l was identified a priori [20].
References
Wnent J, Masterson S, Grasner JT, et al. EuReCa ONE—27 Nations, ONE Europe, ONE Registry: a prospective observational analysis over one month in 27 resuscitation registries in Europe—the EuReCa ONE study protocol. Scand J Trauma Resusc Emerg Med. 2015;23:7.
Berdowski J, Berg RA, Tijssen JG, Koster RW. Global incidences of out-of-hospital cardiac arrest and survival rates: systematic review of 67 prospective studies. Resuscitation. 2010;81:1479–87.
Fugate JE, Brinjikji W, Mandrekar JN, et al. Post-cardiac arrest mortality is declining: a study of the US national inpatient sample 2001 to 2009. Circulation. 2012;126:546–50.
Hypothermia after Cardiac Arrest Study G. Mild therapeutic hypothermia to improve the neurologic outcome after cardiac arrest. N Engl J Med. 2002;346:549–56.
Nielsen N, Wetterslev J, Cronberg T, et al. Targeted temperature management at 33 degrees C versus 36 degrees C after cardiac arrest. N Engl J Med. 2013;369:2197–206.
Scirica BM. Therapeutic hypothermia after cardiac arrest. Circulation. 2013;127:244–50.
Bouwes A, Binnekade JM, Kuiper MA, et al. Prognosis of coma after therapeutic hypothermia: a prospective cohort study. Ann Neurol. 2012;71:206–12.
Wijdicks EF, Hijdra A, Young GB, Bassetti CL, Wiebe S. Quality Standards Subcommittee of the American Academy of N. Practice parameter: prediction of outcome in comatose survivors after cardiopulmonary resuscitation (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2006;67:203–10.
Fugate JE, Wijdicks EF, Mandrekar J, et al. Predictors of neurologic outcome in hypothermia after cardiac arrest. Ann Neurol. 2010;68:907–14.
Rossetti AO, Oddo M, Logroscino G, Kaplan PW. Prognostication after cardiac arrest and hypothermia: a prospective study. Ann Neurol. 2010;67:301–7.
Westhall E, Rossetti AO, van Rootselaar AF, et al. Standardized EEG interpretation accurately predicts prognosis after cardiac arrest. Neurology. 2016;86:1482–90.
Thenayan EA, Savard M, Sharpe MD, Norton L, Young B. Electroencephalogram for prognosis after cardiac arrest. J Crit Care. 2010;25:300–4.
Cronberg T, Rundgren M, Westhall E, et al. Neuron-specific enolase correlates with other prognostic markers after cardiac arrest. Neurology. 2011;77:623–30.
Dragancea I, Rundgren M, Englund E, Friberg H, Cronberg T. The influence of induced hypothermia and delayed prognostication on the mode of death after cardiac arrest. Resuscitation. 2013;84:337–42.
Cronberg T, Lilja G, Horn J, et al. Neurologic function and health-related quality of life in patients following targeted temperature management at 33 degrees C vs 36 degrees C after out-of-hospital cardiac arrest: a randomized clinical trial. Jama Neurol. 2015;72:634–41.
Donnino MW, Andersen LW, Berg KM, et al. Temperature management after cardiac arrest: an advisory statement by the advanced life support task force of the international liaison committee on resuscitation and the american heart association emergency cardiovascular care committee and the council on cardiopulmonary, critical care, Perioperative and Resuscitation. Resuscitation. 2016;98:97–104.
Golan E, Barrett K, Alali AS, et al. Predicting neurologic outcome after targeted temperature management for cardiac arrest: systematic review and meta-analysis. Crit Care Med. 2014;42:1919–30.
Sandroni C, Cavallaro F, Callaway CW, et al. Predictors of poor neurological outcome in adult comatose survivors of cardiac arrest: a systematic review and meta-analysis. Part 1: patients not treated with therapeutic hypothermia. Resuscitation. 2013;84:1310–23.
Stammet P, Collignon O, Hassager C, et al. Neuron-specific enolase as a predictor of death or poor neurological outcome after out-of-hospital cardiac arrest and targeted temperature management at 33 degrees C and 36 degrees C. J Am Coll Cardiol. 2015;65:2104–14.
Oddo M, Rossetti AO. Early multimodal outcome prediction after cardiac arrest in patients treated with hypothermia. Crit Care Med. 2014;42:1340–7.
Booth CM, Boone RH, Tomlinson G, Detsky AS. Is this patient dead, vegetative, or severely neurologically impaired? Assessing outcome for comatose survivors of cardiac arrest. JAMA. 2004;291:870–9.
Morrison LJ, Visentin LM, Kiss A, et al. Validation of a rule for termination of resuscitation in out-of-hospital cardiac arrest. N Engl J Med. 2006;355:478–87.
Rossetti AO, Oddo M, Liaudet L, Kaplan PW. Predictors of awakening from postanoxic status epilepticus after therapeutic hypothermia. Neurology. 2009;72:744–9.
Tsetsou S, Novy J, Oddo M, Rossetti AO. EEG reactivity to pain in comatose patients: importance of the stimulus type. Resuscitation. 2015;97:34–7.
Fantaneanu TA, Tolchin B, Alvarez V, et al. Effect of stimulus type and temperature on EEG reactivity in cardiac arrest. Clin Neurophysiol. 2016;127:3412–7.
Hirsch LJ, LaRoche SM, Gaspard N, et al. American Clinical Neurophysiology Society’s standardized critical care EEG terminology: 2012 version. J Clin Neurophysiol. 2013;30:1–27.
The European Resuscitation Council, American Heart Association, Heart and Stroke Foundation of Canada, Australian Resuscitation Council. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest (new abridged version) The “Utstein style”. Br Heart J. 1992;67:325–33.
Rossetti AO, Rabinstein AA, Oddo M. Neurological prognostication of outcome in patients in coma after cardiac arrest. Lancet Neurol. 2016;15:597–609.
Sandroni C, Cariou A, Cavallaro F, et al. Prognostication in comatose survivors of cardiac arrest: an advisory statement from the European Resuscitation Council and the European Society of Intensive Care Medicine. Resuscitation. 2014;85:1779–89.
Nolan JP, Soar J, Cariou A, et al. European resuscitation council and european society of intensive care medicine guidelines for post-resuscitation Care 2015: section 5 of the European resuscitation council guidelines for resuscitation 2015. Resuscitation. 2015;95:202–22.
Dragancea I, Horn J, Kuiper M, et al. Neurological prognostication after cardiac arrest and targeted temperature management 33 degrees C versus 36 degrees C: results from a randomised controlled clinical trial. Resuscitation. 2015;93:164–70.
Sivaraju A, Gilmore EJ, Wira CR, et al. Prognostication of post-cardiac arrest coma: early clinical and electroencephalographic predictors of outcome. Intensive Care Med. 2015;41:1264–72.
Hofmeijer J, Beernink TM, Bosch FH, Beishuizen A, Tjepkema-Cloostermans MC, van Putten MJ. Early EEG contributes to multimodal outcome prediction of postanoxic coma. Neurology. 2015;85:137–43.
Logi F, Pasqualetti P, Tomaiuolo F. Predict recovery of consciousness in post-acute severe brain injury: the role of EEG reactivity. Brain Inj. 2011;25:972–9.
Tsetsou S, Oddo M, Rossetti AO. Clinical outcome after a reactive hypothermic EEG following cardiac arrest. Neurocrit Care. 2013;19:283–6.
Callaway CW, Donnino MW, Fink EL, et al. Part 8: post-cardiac arrest care: 2015 American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S465–82.
Sadaka F, Doerr D, Hindia J, Lee KP, Logan W. Continuous electroencephalogram in comatose postcardiac arrest syndrome patients treated with therapeutic hypothermia: outcome prediction study. J Intensive Care Med. 2015;30:292–6.
Al Thenayan E, Savard M, Sharpe M, Norton L, Young B. Predictors of poor neurologic outcome after induced mild hypothermia following cardiac arrest. Neurology. 2008;71:1535–7.
Elmer J, Rittenberger JC, Faro J, et al. Clinically distinct electroencephalographic phenotypes of early myoclonus after cardiac arrest. Ann Neurol. 2016;80:175–84.
Zandbergen EG, Hijdra A, Koelman JH, et al. Prediction of poor outcome within the first 3 days of postanoxic coma. Neurology. 2006;66:62–8.
Acknowledgements
The authors thank Christine Stähli, RN, and Elsa Juan, PhD, for help in data acquisition.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Tsetsou, S., Novy, J., Pfeiffer, C. et al. Multimodal Outcome Prognostication After Cardiac Arrest and Targeted Temperature Management: Analysis at 36 °C. Neurocrit Care 28, 104–109 (2018). https://doi.org/10.1007/s12028-017-0393-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-017-0393-8