Abstract
The aim of the study was to establish if the null cell adenoma (NCA) forms a distinct subgroup with unique clinicopathological characteristics within the nonfunctioning pituitary adenoma group particularly in relation to the silent gonadotroph adenomas (SGAs). We identified 31 patients with the pathological diagnosis of NCA verified by routine histology and immunohistochemistry with distinct differentiation from SGAs by an established negative testing for SF-1 at the Toronto Western Hospital between December 2004 and August 2010. We reviewed their demographic data, clinical features, magnetic resonance imaging, and the histologic variables: MIB-1, FGFR4, and P27. We compared these to 63 SGAs identified within the same period. All the NCAs were macroadenomas with diameter ranging from 15—57 mm and tumor volumes between 1.95–53.5 mm3. Preoperative cavernous sinus tumor growth was able to predict the presence of a residual after surgery (p = 0.023). Furthermore, preoperative cavernous sinus extension (p = 0.002) and negative P27 expression (p = 0.035) were able to independently predict the subsequent growth of the postoperative tumor residual. Comparing the NCA to SGA, we found that MIB-1 was higher in NCA (mean ± SD = 3.43 ± 2.76 %) compared to SGAs (mean ± SD = 2.49 ± 1.41 %) (p = 0.044). The preoperative and postoperative tumor volume doubling times (TVDTs) displayed a negative correlation in the SGA (r = −0.855, p = 0.002) while in the NCA, a positive correlation was evident (r = 0.718, p = 0.029). Our study suggests that the NCAs are a distinct group with differing behavioral characteristics from the SGAs. It also appears that the finding of cavernous sinus extension on preoperative imaging and a negative P27 expression on immunohistochemistry in NCAs may be valuable tools in predicting residual tumor growth which may impact on postoperative care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Clinically nonfunctioning pituitary adenomas (CNFPAs) are a varied group of tumors with different morphology and biologic characteristics constituting about a third of all pituitary adenomas [1]. They are characterized by the absence of symptoms or signs secondary to hormonal hypersecretion [2]. They are usually macroscopic and generally present with compressive symptoms affecting the visual apparatus and pituitary gland resulting in varying levels of hypopituitarism [2–4]. These tumors can also result in an apoplectic event with varying presentations from headache to visual impairment, often necessitating urgent surgical intervention. Tumor apoplexy poses long-term risk of endocrinological and visual sequelae [5, 6].
The classification of CNFPAs is based on immunoreactivity with further clarification using ultrastructural features when need be [6, 7]. This has yielded two groups: the “silent” group which consists of tumors that are positive for one of the anterior adenohypophyseal hormones though not in active amounts, and these include the silent somatotrophs, silent corticotrophs, silent lactotrophs, and silent gonadotroph adenomas (SGAs). The other group includes those tumors that are negative for any of the anterior adenohypophyseal hormones such as the null cell adenoma (NCA), oncocytoma, and the subtype 3 corticotrophs. The oncocytomas are essentially NCAs exhibiting oncocytic change with more mitochondrial activity on electron microscopy [6].
The NCA has been described as the rare tumor that is completely negative for all hormones and transcription factors [1, 7, 8]. The NCA is differentiated from the hormone-immunonegative gonadotroph adenomas using appropriate pituitary transcription factors, steroidogenic factor-1 (SF-1) and estrogen receptor-alpha (ER-α) [6]. The NCAs have often been lumped together with the silent gonadotrophs or merely evaluated in the larger context of CNFPAs. This is due either to the belief that they are or behave exactly like SGAs and/or to the inability to subclassify this group using immunohistochemistry, and this may explain the paucity of literature on this subgroup of CNFPAs as a distinct entity [1, 7].
The need for the optimum care of the patients with CNFPAs has necessitated appropriate stratification within this group based on a definition of the aggressiveness and invasive characteristics of each subtype. The silent group has received considerable focus with a number of studies documenting the more aggressive nature of the silent corticotroph and subtype 3 corticotroph adenomas, establishing their tendency to early recurrence/regrowth, thus positing close follow-up with imaging postoperatively and recommending radiotherapy in patients with residual tumors or, in some instances, regrowth [3, 6, 7, 9]. It is interesting to note that some other studies, however, have shown contrary results suggesting the adoption of an initially more conservative follow-up surveillance with radiation delayed until there is clear evidence of tumor recurrence [10, 11]. All of these studies address pertinent issues and provide some form of guide in the management of this subgroup of CNFPAs.
The aim of our study was to review our series of NCAs and investigate their clinical, imaging, and pathological characteristics. We went further to compare these findings with those of our patients with SGAs over the same period. We chose the markers MIB-1, FGFR4, and P27 to explore possible correlation with the patients’ clinical characteristics: MIB-1 because it evaluates the Ki-67 antigen and has been well investigated as a proliferation marker and a predictor of tumor recurrence, FGFR4 for its involvement in pituitary oncogenesis (a strong cytoplasmic activity for FGFR4 has been associated with tumor invasion), and P27 because it is a tumor suppressor protein whose expression has been demonstrated to be low in pituitary tumors and absent in pituitary carcinomas [12].
Materials and Methods
Patient Population
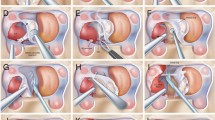
We obtained our institution’s research ethics board approval and retrospectively reviewed the charts of all patients with pituitary tumors who had surgery at the Toronto Western Hospital between December 2004 and August 2010. All surgeries were through the endoscopic route. We identified those with the pathological diagnosis of a NCA verified by routine histology and immunohistochemistry. All the NCAs were negative for all the adenohypophyseal hormones including LH and FSH and transcription factors. They also tested negative for SF-1 further distinguishing them from silent gonadotrophs. We reviewed their demographic data, clinical features, magnetic resonance imaging, and the histologic variables: MIB-1, FGFR4, and P27. A multidisciplinary team consisting of neurosurgeons, neuroendocrinologists, and neuropathologists reviews and manages these patients.
Imaging Analysis
All the patients included in the study had a minimum of two preoperative MR images that were at least a month apart except in the patients that presented with significant visual deterioration or with features suggestive of apoplexy. The two preoperative images that we selected were the first recorded image and the image just prior to surgery. We also reviewed two postoperative MR images with the first at least 3 months after surgery giving time resolution of postoperative surgical changes and correct evaluation of residual. The last follow-up MR image which is at least 12 months from the first postoperative image was evaluated for recurrence or growth of residual. The MRI studies were sella/pituitary-specific imaging protocols.
We carried out a volumetric assessment of each scan using the ITK-SNAP program (University of Pennsylvania, www.itksnap.org). This was done by uploading the MR images into the software followed by a manual contour slice by slice with eventual generation of the tumor volume as well as a three-dimensional reconstruction of the tumor. Our group has previously reported the use of this software [13]. The MR images were reviewed by at least three independent observers, and we recorded the interobserver consistency which was very acceptable with alpha values between .909 and .996.
Suprasellar extension was noted as extension beyond the diaphragm sella. Inferior extension was determined by erosion through the sellar floor into the sphenoid sinus. Cavernous extension was defined by the Knosp criteria [14]. Knosp criteria are divided into five grades (0–4) based on a series of lines drawn through the supracavernous and intracavernous segments of the carotid arteries as observed in midsella coronal sections. In our study, tumors extending to at least the lateral boundary of the intracavernous carotid segments (Knosp grade ≥2) were considered true extension into the CS as previously correlated to surgical findings.
The tumor volume doubling time (TVDT) was calculated using an established formula for tumor growth rate measurements: TVDT = t *log22 / log (V f/V 0) where t is the time interval between the first and second MRI examinations, V 0 is the initial tumor volume, and V f is the final volume. Preoperative and postoperative TVDTs were calculated. Tumor growth was recorded when there is >25 % increase in volume between the first and second scans, tumor regression when there is >25 % reduction in volume between the first and second scans, and stable if tumor growth is <25 %.
Statistical Analysis
Logistic regression was used to predict the presence or absence of residual in NCA and whether or not the residual grew or remained stable. T tests were used to compare mean differences among variables. Pearson’s correlation coefficient was used to establish possible correlations between NCAs and SGAs. Variables with p < 0.05 were considered statistically significant. All analysis was conducted using SPSS.
Result
Patient Characteristics
There were 31 patients with a confirmed diagnosis of NCA on histology and immunohistochemistry, all with established negative immunoreactivity to SF-1 differentiating them from gonadotrophs.
Our cohort included 13 male and 18 female subjects (1:1.3). The mean age was 57 years with the age range between 34 and 85 years. There were only three patients (9 %) who were 40 years and below while about 71 % of the patients were above 50 years. The major presenting symptoms were headaches and visual symptoms. Two patients (6 %) presented with apoplectic events and hypopituitarism. There were six (19 %) recurrent tumors with two of these having had prior radiotherapy. All of the tumors were macroadenomas defined as a tumor with a maximum diameter of >10 mm. The tumor diameters range from 15 to 57 mm, while the volumes range between 1.95 and 53.5 cm3.
All the patients underwent endoscopic transsphenoidal tumor resections with postop imaging confirmed gross total resection (GTR) in 14 patients and subtotal resections in 15 patients. The residual tumor varied from 0.31 to 5.89 cm3. There was no follow-up postop imaging in two of the patients to confirm the extent of resection recorded at surgery which was a subtotal resection in one and GTR in the other. The average follow-up postsurgery was 36 months (range is 7–71 months).
Predictors of Null Cell Residual and Growth
We carried out statistical evaluation using the following indices: age, gender, clinical presentation, optic chiasm compression (OC), Knosp classification, sphenoid sinus invasion, P27, FGFR4, MIB-1, and the preop and postop TVDTs. The significant finding was that the tumor that grew into the cavernous sinus preoperatively (p = 0.023) was able to predict the presence of a residual after surgery. Furthermore, preoperative cavernous sinus extension (p = 0.002) and negative P27 expression (p = 0.035) were able to independently predict the subsequent growth of the residual. Thus, with preoperative cavernous sinus extension and low P27 value, there was an increased risk of growth of the residual tumor.
Comparison of Null Cell with Gonadotroph
We compared the cohort of NCAs with a cohort of 63 SGAs, which were operated on during the same period (Table 1). With respect to the MIB-1 labeling index, we found that MIB-1 was higher in NCA (mean ± SD = 3.43 ± 2.76 %) compared to SGAs (mean ± SD = 2.49 ± 1.41 %) (p = 0.044).
In terms of tumor growth rate, the preoperative TVDT for the SGAs and NCAs was (mean ± SD) 1097 ± 668 and 1370 ± 1049 days, respectively. The corresponding postoperative TVDT for the SGAs and NCAs was 1117 ± 221 and 1899 ± 1542 days, respectively. The mean differences between the preoperative TVDT and postoperative TVDT for either tumor were not statistically significant (Figs. 1 and 2).
The preoperative and postoperative TVDTs were significantly correlated in both the SGAs and the NCAs. The preoperative and postoperative TVDTs displayed a negative correlation in the SGA (r = −0.855, p = 0.002) while in the NCA, a positive correlation was evident (r = 0.718, p = 0.029). This indicates that in the SGA group, tumors that grew rapidly preoperatively grew slowly after surgery while NCAs that grew rapidly prior to surgery continued to exhibit rapid postoperative growth (Figs. 3 and 4).
Discussion
The first designation of a group of tumors as NCAs was by Kovacs and his workers in 1980. They describe these tumors as pituitary adenomas that lack the histological, immunohistological, or ultrastructural markers that will permit the identification of their origin [15]. The NCA is postulated to arise from pluripotential precursor cells which can differentiate into different hormone-producing cell types [16–18]. There have been various attempts to describe the histological and functional characteristics of this group of tumors over the years with a general consensus that NCAs are negative for all hormones by immunohistochemistry [15, 17–20]. The study of the ultrastructure of NCA has however revealed that they have subcellular organelles for hormone synthesis and release and some of these tumors secrete glycoprotein subunits in vitro [17, 19–21]. These findings form the basis for the assumptions that NCAs are just an extension of SGAs and should therefore not be identified as a distinct group [20]. There have also been suggestions that they usually behave like gonadotrophs [8, 22]. However, a true NCA has been described as one which stains negative for all pituitary hormones and transcription factor such that the use of appropriate pituitary transcription factors (SF-1, ER-α) prevents hormone-immunonegative SGAs from being mistakenly diagnosed as NCAs [2, 6]. The NCA can thus be evaluated as a distinct group within the CNFPAs establishing the need to characterize their unique clinicopathological behavior.
Our study cohort had a mean age of 57 years with NCAs found in only 9 % of those below 40 years, which agrees with previous studies establishing that it is not a disease of the young [17, 23]. We found slight female predominance compared to data suggesting male predominance in CNFPAs [3]. All the tumors were macroadenomas and presented mainly with headache and visual symptoms, which included decrease or loss of visual acuity and visual field deficits.
In our study, we were able to establish that preoperative cavernous sinus extension predicts postoperative residual tumor in NCAs as has been found in other studies on CNFPAs [24–26]. However, we were also able to predict increased risk of growth of the residual tumor with preoperative cavernous sinus invasion (p = 0.002) and a low P27 value (p = 0.035). A previous report on CNFPAs, without specifics to the subtype, by Greenman et al. had found that tumors with cavernous sinus invasion before surgery and large postsurgical suprasellar remnants tended to have residual tumor growth after surgery [25]. They suggested this as a factor to consider in the stratification of patients for postoperative radiotherapy based on the risk for growth of the residual tumor. Though we did not study the risk of cavernous sinus extension within the subtypes of CNFPAs, Yamada and his co-workers had documented that cavernous sinus invasion within the NCA group was next to that seen in the silent corticotrophs and silent subtype 3 adenomas, more common than that seen in SGAs [27]. Thus, the consideration of this factor as a risk predictor for tumor growth in NCAs may be important and may influence the initiation of early adjuvant treatment such as radiotherapy.
There is a continuing effort at discovering molecular markers for predicting residual tumor growth in pituitary tumors. The focus has been on the Ki-67 antigen, which has been reported in some studies to have a positive correlation with residual tumor growth [28–34]. Some other reports have however found no usefulness for the Ki-67 antigen in predicting residual tumor growth [35, 36]. In our study, we explore the possibility of a relationship between the P27 protein and residual tumor growth and we found that a negative P27 independently predicts growth of the residual tumor. A previous study by Monsalves et al. did not find any correlation between the growth characteristics of pituitary tumors and the expression of P27 [13]. The P27 protein is a CDK inhibitor that blocks kinase activity in the G1 phase of the cell cycle. The overexpression of the protein prevents cells in the G1 phase from entering the S phase. The P27 protein has been demonstrated to occur in reduced expression levels in tumors derived from all pituitary cell types [37], and it has been investigated in the past as a predictor of invasiveness in pituitary adenomas [38]. Malignant transformation has been shown to lead to nearly complete loss of P27 immunoreactivity [3, 39]. Our study finding may indicate the possible importance of the protein as a predictive marker for residual tumor growth in NCAs.
The comparison of SGAs, surgically treated in our unit within the same period with our cohort of NCAs, showed that the Ki-67 LI (MIB) was higher in the NCA subtype (p = 0.044). Other studies have shown similar results with NCAs having higher MIB although there was no statistical difference [38, 40].
We also found that the preoperative TVDT and postoperative TVDT have a strong negative correlation in gonadotrophs (r = −0.855, p = 0.002): i.e., those tumors that grew slowly preoperatively grew quickly after surgery and vice versa. Interestingly, NCAs behaved in the opposite way even though the correlation was not significant (r = 0.533, p = 0.139). We do not understand what factors influence this behavior, and there is no certainty if this suggests certain unpredictability in the behavior of the SGAs when compared with the NCA. It is important to note that in our cohort, there were few residual tumors with which to compare preoperative and postoperative TVDTs, so these results must be interpreted with caution. A longer follow-up period may also have a modifying effect on our result.
Conclusion
Our study suggests tangible evidence that warrants the consideration of NCA as a distinct group with differing behavioral characteristics from the SGAs. It also appears that the finding of cavernous sinus invasion on preoperative imaging and a negative P27 expression on immunohistochemistry in NCAs may be valuable tools in predicting residual tumor growth and aid decisions regarding postop clinical and imaging surveillance and initiation of adjuvant therapy. We recognize that our study is limited by sample size and a larger study to corroborate these findings will be valuable.
References
Asa SL, Ezzat S (2009) The pathogenesis of pituitary tumors. Annual review of pathology 4: 97–126
Greenman Y, Stern N (2009) Non-functioning pituitary adenomas. Best Practice & Research Clinical Endocrinology & Metabolism 23: 625–638
Scheithauer BW, Gaffey TA, Lloyd RV, Sebo TJ, Kovacs KT, Horvath E, Yapcer Z, Young WF, Meyer FB, Kuroki T, Riehle DL, Laws ER (2006) Pathobiology of Pituitary Adenomas and Carcinomas. Neurosurgery 59: 341–353
Mahta A, Haghpanah V, Lashkari A, Heshmat R, Larijani B, Tavangar SM (2007) Non-functioning pituitary adenoma: immunohistochemical analysis of 85 cases. Folia neuropathologica/Association of Polish Neuropathologists and Medical Research Centre, Polish Academy of Sciences 45: 72–77
Bujawansa S, Thondam SK, Steele C, Cuthbertson DJ, Gilkes CE, Noonan C, Bleaney CW, Macfarlane IA, Javadpour M, Daousi C (2014) Presentation, management and outcomes in acute pituitary apoplexy: a large single-centre experience from the United Kingdom. Clinical endocrinology 80: 419–424
Mete O, Asa SL (2012) Clinicopathological correlations in pituitary adenomas. Brain pathology (Zurich, Switzerland) 22: 443–453
Al-Brahim NYY, Asa SL (2006) My approach to pathology of the pituitary gland. Journal of Clinical Pathology 59: 1245–1253
Asa SL (2008) Practical pituitary pathology: what does the pathologist need to know? Archives of pathology & laboratory medicine 132: 1231–1240
Miller BA, Rutledge WC, Ioachimescu AG, Oyesiku NM (2012) Management of large aggressive nonfunctional pituitary tumors: experimental medical options when surgery and radiation fail. Neurosurg Clin N Am 23: 587–594
Alahmadi H, Lee D, Wilson JR, Hayhurst C, Mete O, Gentili F, Asa SL, Zadeh G (2012) Clinical features of silent corticotroph adenomas. Acta Neurochir (Wien) 154: 1493–1498
Chen L, White WL, Spetzler RF, Xu B (2011) A prospective study of nonfunctioning pituitary adenomas: presentation, management, and clinical outcome. Journal of neuro-oncology 102: 129–138
Ramirez C, Cheng S, Vargas G, Asa SL, Ezzat S, Gonzalez B, Cabrera L, Guinto G, Mercado M (2012) Expression of Ki-67, PTTG1, FGFR4, and SSTR 2, 3, and 5 in nonfunctioning pituitary adenomas: a high throughput TMA, immunohistochemical study. The Journal of clinical endocrinology and metabolism 97: 1745–1751
Monsalves E, Larjani S, Loyola Godoy B, Juraschka K, Carvalho F, Kucharczyk W, Kulkarni A, Mete O, Gentili F, Ezzat S, Zadeh G (2014) Growth patterns of pituitary adenomas and histopathological correlates. The Journal of clinical endocrinology and metabolism: jc20133054
Knosp E, Steiner E, Kitz K, Matula C (1993) Pituitary adenomas with invasion of the cavernous sinus space: a magnetic resonance imaging classification compared with surgical findings. Neurosurgery 33: 610–617; discussion 617–618
Kovacs K, Horvath E, Ryan N, Ezrin C (1980) Null cell adenoma of the human pituitary. Virchows Archiv A, Pathological anatomy and histology 387: 165–174
Gittoes NJ (1998) Current perspectives on the pathogenesis of clinically non-functioning pituitary tumours. The Journal of endocrinology 157: 177–186
Holm R (1995) Null cell adenomas and oncocytomas of the pituitary gland. Pathology, research and practice 191: 348–352
Asa SL, Ezzat S (1998) The cytogenesis and pathogenesis of pituitary adenomas. Endocrine reviews 19: 798–827
Yamada S, Asa SL, Kovacs K (1988) Oncocytomas and null cell adenomas of the human pituitary: morphometric and in vitro functional comparison. Virchows Archiv A, Pathological anatomy and histopathology 413: 333–339
Sano T, Yamada S (1994) Histologic and immunohistochemical study of clinically non-functioning pituitary adenomas: special reference to gonadotropin-positive adenomas. Pathology international 44: 697–703
Al-Shraim M, Asa SL (2006) The 2004 World Health Organization classification of pituitary tumors: what is new? Acta neuropathologica 111: 1–7
Young WF, Jr., Scheithauer BW, Kovacs KT, Horvath E, Davis DH, Randall RV (1996) Gonadotroph adenoma of the pituitary gland: a clinicopathologic analysis of 100 cases. Mayo Clinic proceedings 71: 649–656
Yamada S, Kovacs K, Horvath E, Aiba T (1991) Morphological study of clinically nonsecreting pituitary adenomas in patients under 40 years of age. Journal of neurosurgery 75: 902–905
Losa M, Mortini P, Barzaghi R, Ribotto P, Terreni MR, Marzoli SB, Pieralli S, Giovanelli M (2008) Early results of surgery in patients with nonfunctioning pituitary adenoma and analysis of the risk of tumor recurrence. Journal of neurosurgery 108: 525–532
Greenman Y, Ouaknine G, Veshchev I, Reider G, II, Segev Y, Stern N (2003) Postoperative surveillance of clinically nonfunctioning pituitary macroadenomas: markers of tumour quiescence and regrowth. Clinical endocrinology 58: 763–769
Brochier S, Galland F, Kujas M, Parker F, Gaillard S, Raftopoulos C, Young J, Alexopoulou O, Maiter D, Chanson P (2010) Factors predicting relapse of nonfunctioning pituitary macroadenomas after neurosurgery: a study of 142 patients. European journal of endocrinology/European Federation of Endocrine Societies 163: 193–200
Yamada S, Ohyama K, Taguchi M, Takeshita A, Morita K, Takano K, Sano T (2007) A study of the correlation between morphological findings and biological activities in clinically nonfunctioning pituitary adenomas. Neurosurgery 61: 580–584; discussion 584–585
Steno A, Bocko J, Rychly B, Chorvath M, Celec P, Fabian M, Belan V, Steno J (2014) Nonfunctioning pituitary adenomas: association of Ki-67 and HMGA-1 labeling indices with residual tumor growth. Acta Neurochir (Wien) 156: 451–461
Widhalm G, Wolfsberger S, Preusser M, Fischer I, Woehrer A, Wunderer J, Hainfellner JA, Knosp E (2009) Residual nonfunctioning pituitary adenomas: prognostic value of MIB-1 labeling index for tumor progression. Journal of neurosurgery 111: 563–571
Matsuyama J (2012) Ki-67 expression for predicting progression of postoperative residual pituitary adenomas: correlations with clinical variables. Neurologia medico-chirurgica 52: 563–569
Nakabayashi H, Sunada I, Hara M (2001) Immunohistochemical analyses of cell cycle-related proteins, apoptosis, and proliferation in pituitary adenomas. The journal of histochemistry and cytochemistry: official journal of the Histochemistry Society 49: 1193–1194
Mizoue T, Kawamoto H, Arita K, Kurisu K, Tominaga A, Uozumi T (1997) MIB1 immunopositivity is associated with rapid regrowth of pituitary adenomas. Acta Neurochir (Wien) 139: 426–431; discussion 431–422
Honegger J, Prettin C, Feuerhake F, Petrick M, Schulte-Monting J, Reincke M (2003) Expression of Ki-67 antigen in nonfunctioning pituitary adenomas: correlation with growth velocity and invasiveness. Journal of neurosurgery 99: 674–679
Ekramullah SM, Saitoh Y, Arita N, Ohnishi T, Hayakawa T (1996) The correlation of Ki-67 staining indices with tumour doubling times in regrowing non-functioning pituitary adenomas. Acta Neurochir (Wien) 138: 1449–1455
Losa M, Franzin A, Mangili F, Terreni MR, Barzaghi R, Veglia F, Mortini P, Giovanelli M (2000) Proliferation index of nonfunctioning pituitary adenomas: correlations with clinical characteristics and long-term follow-up results. Neurosurgery 47: 1313–1318; discussion 1318–1319
Dubois S, Guyetant S, Menei P, Rodien P, Illouz F, Vielle B, Rohmer V (2007) Relevance of Ki-67 and prognostic factors for recurrence/progression of gonadotropic adenomas after first surgery. European journal of endocrinology/European Federation of Endocrine Societies 157: 141–147
Bamberger CM, Fehn M, Bamberger AM, Ludecke DK, Beil FU, Saeger W, Schulte HM (1999) Reduced expression levels of the cell-cycle inhibitor p27Kip1 in human pituitary adenomas. European journal of endocrinology/European Federation of Endocrine Societies 140: 250–255
Zhao D, Tomono Y, Nose T (1999) Expression of P27kip1 and Ki-67 in pituitary adenomas: an investigation of marker of adenoma invasiveness. Acta Neurochir (Wien) 141: 187–192
Korbonits M, Chahal HS, Kaltsas G, Jordan S, Urmanova Y, Khalimova Z, Harris PE, Farrell WE, Claret FX, Grossman AB (2002) Expression of phosphorylated p27(Kip1) protein and Jun activation domain-binding protein 1 in human pituitary tumors. The Journal of clinical endocrinology and metabolism 87: 2635–2643
Wolfsberger S, Wunderer J, Zachenhofer I, Czech T, Bocher-Schwarz HG, Hainfellner J, Knosp E (2004) Expression of cell proliferation markers in pituitary adenomas—correlation and clinical relevance of MIB-1 and anti-topoisomerase-IIalpha. Acta Neurochir (Wien) 146: 831–839
Conflict of Interest
The authors declare no conflict of interest
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Balogun, J.A., Monsalves, E., Juraschka, K. et al. Null Cell Adenomas of the Pituitary Gland: an Institutional Review of Their Clinical Imaging and Behavioral Characteristics. Endocr Pathol 26, 63–70 (2015). https://doi.org/10.1007/s12022-014-9347-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12022-014-9347-2