Abstract
Purpose
To clarify the invasiveness to surrounding structures and recurrence rate of each subtype of nonfunctioning pituitary neuroendocrine tumor (Pit-NETs) according to the WHO 2022 classification.
Methods
This retrospective study utilized data from 292 patients with nonfunctioning Pit-NETs treated with initial transsphenoidal surgery. Recurrence was evaluated on 113 patients who were available for a magnetic resonance imaging follow-up ≥ 60 months. All tumors were assessed by immunohistochemical staining for Pit-1, T-PIT, and GATA3. Invasiveness to surrounding structures was evaluated based on intraoperative findings.
Results
Cavernous sinus invasion was found in 47.5% of null cell tumors, 50.0% of Pit-1 lineage tumors, 31.8% of corticotroph tumors, and 18.3% of gonadotroph tumors. Dura mater defects in the floor of sellar turcica, indicating dural invasion, were found in 44.3% of null cell tumors, 36.4% of corticotroph tumors, 16.7% of Pit-1 lineage tumors, and 17.3% of gonadotroph tumors. In logistic regression analysis, Pit-1 (OR 5.90, 95% CI 1.71–20.4, P = 0.0050) and null tumors (OR 4.14, 95% CI 1.86–9.23, P = 0.0005) were associated with cavernous sinus invasion. Recurrence was found in 8 (4.9%) patients, but without significant differences between tumor subtypes. The presence of cavernous sinus invasion was correlated with recurrence (HR = 1.95, 95% CI 1.10–3.46, P = 0.0227).
Conclusion
Among nonfunctioning Pit-NETs, Pit-1 lineage tumors tend to invade the cavernous sinus, corticotroph tumors may produce dura mater defects, and null cell tumors tend to cause both. Pit-NETs with cavernous sinus invasion require a careful attention to recurrence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pituitary neuroendocrine tumors (Pit-NETs) are the third most frequent primary brain tumors and are frequently encountered clinically [1]. In the World Health Organization (WHO) 2022 classification, the diagnostic name changed from pituitary adenomas to Pit-NETs [2]. Although historically considered benign, 20%–55% of surgically removed Pit-NETs may exhibit evidence of local invasion to the dura matter, bone, and/or surrounding structures [3]. Such “invasiveness” makes achieving surgical total resection and/or postoperative complete remission challenging, and may result in tumor recurrence [4].
Pit-NETs are categorized as either functioning or nonfunctioning Pit-NETs, nonfunctioning Pit-NETs accounting for 14%–54% of all [5]. To determine the tumor subtype as well as various hormones, the WHO 2017 classification recommends immunostaining for transcription factors [6]. Previous reports have suggested that Pit-NETs which do not show immunoreactivity to pituitary hormone antibodies or those diagnosed as null cell tumors before 2017 are more likely to invade the cavernous sinus than silent gonadotroph tumors [7]. Conversely, most Pit-NETs diagnosed as null cell tumors before 2017 showed immunoreactivity for either T-PIT, Pit-1, or SF-1 [8]. Recently, Pit-NETs negative for all transcription factors, so-called “true null cell tumors,” have been shown to have a high rate of recurrence and cavernous sinus invasion [9]. However, the invasiveness and recurrence rate of tumors not subclassified as null cell tumors according to the latest WHO classification but diagnosed as null cell tumors before 2017 have not been clarified. Thus, this study aimed to determine the invasiveness to surrounding structures and recurrence rate for each Pit-NET subtype based on transcription factors, according to the latest WHO classification.
Materials & Methods
This retrospective study was approved by the institutional review board (E-2022), which waived the requirement for written informed consent due to the anonymous nature of the data used.
Patients
Between 2009 and 2022, 292 patients with nonfunctioning Pit-NETs underwent initial transsphenoidal surgery (TSS) at our institution. We retrieved their data from the medical records and analyzed age, sex, tumor volume, radiographical findings, operative findings, and pathological evaluations.
Radiological assessment
All patients underwent 3 T-MRI and head computed tomography within one month before surgery for tumor volume and shape assessment. Tumor volume (cm3) was calculated as Width × Height × Depth/2 [10]. Lateral tumor growth into the cavernous sinus was categorized according to the Knosp classification [11]. Total resection was defined as no residual tumor on MRI within three months after surgery. MRI was performed routinely at least once a year after surgery to evaluate the presence or absence of recurrence. MRI findings was assessed by independent senior authors (Y.K and F.Y). Differences in the evaluations were discussed and classified by consensus. Recurrence rate was assessed in 113 patients who had follow-up magnetic resonance imaging (MRI) data available for ≥ 60 months (median follow-up: 92 months, range 60–152 months). Therefore, patients who had follow-up period more than 5 years or who had recurrence within 5 years were included. A total of 140 patients were excluded (Supplemental Table 1). Four patients were excluded due to death unrelated to tumor recurrence within 5 years postoperatively. Other patients were lost to follow-up because they did not request follow-up or were not seen in the outpatient clinic.
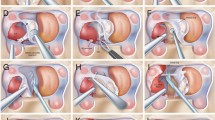
Surgical procedures
TSS was performed by two senior surgeons (A.To and Y.K) as an endoscopic procedure through one nostril, as previously described [12]. For this study, invasiveness was assessed by the following surgical findings: cavernous sinus invasion, sphenoid sinus invasion, dura matter defects in the floor of the sellar turcica indicating dural invasion, and erosion of bony parts in the floor of the sellar turcica [3]. Cavernous sinus invasion was evaluated by carefully observing the surgical field with reference to preoperative MRI findings. Differences in the evaluations were discussed and classified by consensus between the two senior surgeons.
Pathological diagnosis
Tumor histology was evaluated in formalin-fixed, paraffin-embedded, hematoxylin and eosin-stained tissue by two pathologists (V.J.A and Y.T). Immunohistochemical analyses for hormonal (anti-TSH, GH, prolactin, LH, FSH, and ACTH) secretion were performed as well. Additional immunohistochemical staining for transcription factors was performed using anti-Pit-1 [1:100, mouse monoclonal, clone:D7, Santa Cruz Biotehnologies Inc, Dallas, Texas, USA SC-393943 https://www.scbt.com/ja/p/pit-1-antibody-d-7?requestFrom=search], anti-GATA3 [prediluted, mouse monoclonal, clone:L50-823, Roche diagnostics, Rotkreuz, Switzerland https://elabdoc-prod.roche.com/eLD/web/jp/en/products/RTD000922?searchTerm=GATA&catalog=ProductCatalog&orderBy=Relevance], and anti-T-PIT [1:200; Anti-TBX19/HPA072686, Atlas Antibodies, RRID: AB_2732209, AB_2732209 https://antibodyregistry.org/search?q=AB_2732209]. Pathological diagnosis was based on WHO classification, 2022 edition [2]. Tumors without immunoreactivity for any antibodies were diagnosed as null cell tumors, tumors which showed immunoreactivity for Pit-1 were defined as Pit-1 lineage tumors, those with immunoreactivity for GATA3 and no immunoreactivity for Pit-1 were diagnosed as gonadotroph tumors, and tumors with immunoreactivity for T-PIT were diagnosed as corticotroph tumors. Gonadotroph tumors are generally diagnosed using the anti-SF-1 but the combination of GATA3 and Pit-1 enables an equivalent diagnosis quality [13, 14]. Hence, we used anti-GATA3 as surrogate marker.
Statistical analyses
The Shapiro–Wilk test was used to assess data normality; continuous variables are expressed as median [interquartile range] and categorical variables are represented as frequency (%). Continuous variables were compared using the Kruskal–Wallis test and one-way ANOVA, and categorical variables were compared using the Fisher’s exact test. A P-value < 0.05 (two-tailed) was deemed significant. Bonferroni correction was used to account for multiple comparisons. A logistic regression model was used to calculate the adjusted odds ratios (ORs) with 95% confidence intervals (CIs) to identify factors related to cavernous sinus invasion, and dura matter and bone defects in the sellar turcica. To avoid overfitting the model, seven covariates were selected for cavernous sinus invasion: age, sex, Knosp grade 3–4, tumor volume, null cell, PIT-1 and T-PIT expression, and dura matter defects in the sellar turcica: age, sex, tumor height, tumor volume, null cell, PIT-1, and T-PIT expression, respectively. Receiver operating characteristic (ROC) curves were generated to determine the sensitivity and specificity of various tumor height cutoff values for the dura matter defects in the sellar turcica. Cox proportional-hazards model was used to estimate the hazard ratios (HRs) and 95% CIs for factors related to recurrence. All statistical analyses were performed using JMP® version 16 (SAS Institute Inc., Cary, NC, USA).
Results
Tumor classification
Figure 1 presents the classification of the tumors in the present study. Gonadotroph tumors were the most common (65.4%); 32.5% showed immunoreactivity for FSH and/or LH. Among 22 (7.5%) cases classified as corticotroph tumors, 13 (4.4%) showed immunoreactivity for ACTH (“totally silent” corticotroph tumors) [15]. Among 18 cases classified into Pit-1 lineage tumors, 4 (1.4%) were subclassified into somatotroph tumors, 2 (0.7%) as lactotroph tumors, and 3 (1.0%) as thyrotroph tumors. There were nine cases (3.1%) without immunoreactivity for any pituitary hormone (Supplemental Table 2). One of three patients with thyrotroph tumors had primary hypothyroidism. Of all cases, 61 (20.9%) were classified as null cell tumors.
Breakdown of tumor subtypes. Since 2009, 461 patients underwent trans sphenoidal surgery for primary pituitary neuroendocrine tumors (Pit-NETs) at our institution. All patients were evaluated by endocrinological examinations, and 292 patients were diagnosed with nonfunctioning Pit-NETs. Among 191 patients with gonadotroph tumors, 95 cases were LH and/or FSH positive tumors and 96 cases were GATA-3 only positive tumors. Among 22 patients with corticotroph tumors, 13 cases were ACTH-positive and nine cases were T-PIT-only positive. Among 18 patients with Pit-1 lineage tumors, nine had GH, PRL, or TSH positive tumors and nine Pit-1 only positive tumors. Sixty-one patients had null cell tumors
Patient characteristics according to tumor subtype
Table 1 presents the characteristics of patients according to tumor subtype. Patients with Pit-1 lineage tumors were significantly younger than those with gonadotroph tumors (P < 0.0001) and tended to be younger than those with null cell and corticotroph tumors (P = 0.0197 and P = 0.0770). There were more male patients with gonadotroph tumors, but more female patients in the other three groups (P < 0.0001). Figure 2 shows a comparison of invasiveness between tumor subtypes. Null cell tumors showed more cavernous sinus invasion (P < 0.0001), dura mater (P < 0.0001) and bone (P < 0.0001) defects in the sellar turcica compared to gonadotroph tumors. The ratio of cavernous sinus invasion in Pit-1 lineage tumors was higher than in gonadotroph tumors (P = 0.0070), and the ratio of dura mater defects in the sellar turcica was higher in corticotroph tumors than in gonadotroph tumors (P = 0.044). No significant difference was observed in Knosp grade or the ratio of sphenoid sinus invasion. Neither was there any significant difference in total resection rate or MIB-1 index.
Invasiveness of different tumor subtypes. null cell tumors showed a higher rate of cavernous sinus invasion (P < 0.0001), dura mater (P < 0.0001) and bone (P < 0.0001) defects in the floor of the sellar turcica compared to gonadotroph tumors. Pit-1 lineage tumors showed a higher rate of cavernous invasion than gonadotroph tumors (P = 0.0070) and corticotroph tumors showed a higher rate of dura mater defects than gonadotroph tumors (P = 0.044)
Related factors of invasiveness of Pit-NETs
Table 2 shows the related factors of cavernous sinus invasion in multivariate analysis. Knosp grade 3–4, tumor volume, null cell tumor, and Pit-1 positive tumor were significantly associated with cavernous sinus invasion with adjusted ORs of 8.37 for Knosp grade 3–4 (95% CI 4.30–16.30, p < 0.0001), 4.14 for null cell tumor (95% CI 1.86–9.23, P = 0.0005), 5.90 for Pit-1 lineage tumor (95% CI 1.71–20.40, P = 0.0050), and 1.06 for tumor volume (95% CI 1.01–1.11, P = 0.0137). To exclude the tumor mass effect, cavernous sinus invasion was reassessed in 208 patients with Knosp grade 0–2. Cavernous sinus invasion was found in 33.3% of Pit-1 lineage tumors, 27.5% of null cell tumors, 9.7% of gonadotroph tumors, and in no corticotroph tumors.
Table 3 shows the related factors of dura matter defects in the sellar turcica obtained in multivariate analysis. Null cell tumors and tumor height were significantly associated with dura matter defects with adjusted ORs of 4.61 for null cell tumors (95% CI 2.13–9.99, P < 0.0001), and 1.10 for tumor height (95% CI 1.03–1.18, P = 0.0052). The optimal tumor height with dura mater defects was calculated using the ROC curve (Supplemental figure). We obtained the optimal relation between sensitivity (76.06%) and specificity (67.42%) at a cutoff value of 23.02 mm (AUC = 0.75225). To reduce the effect of tumor height, we reassessed the presence or absence of dura mater defects in each group at a height ≤ 23 mm. Accordingly, dura mater defects in the sellar turcica were found in 26.7% of corticotroph tumors, 22.6% of null cell tumors, 10.0% of Pit-1 lineage tumors, and 4.6% of gonadotroph tumors (Fig. 3).
Ratio of dura mater defects in the floor of the sellar turcica according to tumor subtype in tumor height ≤ 23 mm. To reduce the effect of tumor height, we evaluated the presence or absence of dura mater defects in each group at a height ≤ 23 mm. Dura mater defects were found in 22.6% of null cell tumors, 4.6% of gonadotroph tumors, 10.0% of Pit-1 lineage tumors, and 26.7% of corticotroph tumors
Recurrence
Table 4 shows the factors associated with recurrence. Among the 113 cases, 9 showed recurrence (null cell tumors: 4/27, gonadotroph tumors: 3/71, Pit-1 lineage tumors: 1/8, corticotroph tumors: 1/7, P = 0.2971). Eight of the nine cases showed "early recurrence" within 60 months. Cavernous sinus invasion and dura mater defects in the sellar turcica were more common in recurrent tumors (P = 0.0003 and P = 0.0243, respectively). Recurrence was also common in tumors with high MIB-1 index and large tumor volume (P = 0.0033 and P = 0.0439, respectively). Conversely, there was no correlation between tumor recurrence and subtype. However, no recurrence was observed in tumors showing immunoreactivity against FSH, LH, GH, PRL, TSH, and/or ACTH (P = 0.0554). Moreover, gonadotroph tumors tended to have less recurrence than non-Gonadotroph tumors (P = 0.0754). Cox proportional analysis was performed on six factors: age, sex, tumor volume, presence of cavernous sinus invasion, presence of dura mater defect in the sellar turcica and MIB-1 index. The presence of cavernous sinus invasion showed a strong correlation (HR = 1.95, 95% CI 1.10–3.46, P = 0.0227), and high MIB-1 index also showed a weak correlation (HR = 1.77, 95% CI 1.04–21.10, P = 0.0450).
Discussion
In this study we evaluated patient background and tumor characteristics of nonfunctioning Pit-NETs according the WHO 2022 classification. First, we found that cavernous sinus invasion and dura mater defects in the sellar turcica occur frequently in null cell pit-NETs. Next, we showed that Pit-1 lineage tumors were common in young patients and frequently showed cavernous sinus invasion as did null cell tumors. Furthermore, we demonstrated that, similar to null cell tumors, corticotroph tumors often exhibit the dura mater defects in the sellar turcica. In other words, in non-functioning Pit-NETs, Gonadotroph tumors showed less invasion into surrounding structures than non-Gonadotroph tumors. Due to the small number of cases, we could not find significant differences in recurrence rate among subtypes. However, non-Gonadotroph tumors and tumors with no-immunoreactivity to the pituitary hormone showed tendency to have a high recurrence rate.
Differences in origin among Pit-NETs subtypes and invasion to surrounding structures
The majority of silent corticotroph tumors are large at the time of diagnosis and known to cause frequent invasions at multiple sites [8, 16]. We confirmed for the first time that nonfunctioning corticotroph tumors had a high rate of dura mater defects in the sellar turcica, second only to null cell tumors. If tumors are large, the mass effect of the tumors on the bone and dura in the sellar turcica must be taken into account. However, in the actual clinical setting, relatively low-height Pit-NETs may also have bone and/or dural defects in the floor of sellar turcica. Therefore, in the present study, we also showed data that reduced the effect of height by re-analyzing only tumors with a height of 23 mm or less, and among these tumors, corticotroph tumors showed a tendency to have more dural mater defects. From an anatomical standpoint, normal corticotroph cells comprise about 15% of anterior pituitary cells and mostly cluster in the central mucoid wedge [17]. This cellular localization may explain why the relatively small coricotroph tumors caused more dura mater defects in the sellar turcica than other subtype tumors in the present study. In addition, corticotroph tumors with TP53 mutations, which constitute 6–10% of all pituitary tumors, have been reported to be more invasive and more malignant [18], comprising up to 45% of aggressive pituitary tumors and pituitary carcinomas [19].
Asmaro and colleagues reported that 53% of Pit-1 lineage Pit-NETs caused cavernous sinus invasion, with 44% of Knosp grade 0–2 Pit-1 lineage Pit-NETs showing cavernous sinus invasion [20]. In addition, 14% of Knosp grade 0–1 acromegaly patients are reported to have histologically cavernous sinus invasion [21]. Tumors with GH secretion but without acromegaly symptoms, the so-called silent somatotroph tumors, also frequently show cavernous sinus invasion [22]. From an anatomical perspective, normal somatotroph cells are primarily located in the lateral wings of the anterior lobe [17]. As for corticotroph tumors, the features of the tumor site of origin may correspond to the localization of normal cells. Thyrotroph tumors have a high tendency to invade the cavernous sinus [23,24,25]. Nonetheless, thyrotroph tumors frequently have GH-TSH co-secretion [24] and may contain immature Pit-1 lineage tumors [2]. Therefore, pure thyrotroph tumors may not be highly invasive to cavernous sinus. Lactotrophs tumors are common in young women, and cavernous sinus invasion influences the decline in surgical remission [26]. Cavernous sinus invasion is more common in lactotroph tumors in males than in females, as they are less likely symptomatic and their existence is only confirmed when already large [26]. A study of medial wall resection of the cavernous sinus at Pit-NETs showed lower effects for endocrinological remission in lactotrophs tumors than in somatotrophs tumors [27]. Therefore, it is controversial that cavernous sinus invasion has been common in Lactotroph tumors as well as Somatotroph tumors. Like thyroytroph tumors, immature Pit-1 lineage tumors must also be considered about lactotrophs with cavernous sinus invasion.
There are few tumors positive solely for Pit-1 and their detail biological behaviors have not been clarified [8, 28]. In this study, half Pit-1 lineage tumors were positive solely for Pit-1. Most patients with Pit-1 solely positive tumor were young and their tumors showed cavernous sinus invasion. A more primitive differentiated tumor is possible as well [28], as the lack of hormone secretion from the tumors makes it difficult to estimate the site of origin.
Tumors with negative for pituitary hormone have been known to exhibit a propensity for invasiveness to surroundings structures [7]. In the present study, we showed that true null cell tumors, which are also negative for transcription factors, account for about one-third of tumors negative for the pituitary hormone. They also exhibited a high degree of invasiveness to surroundings structures. Conversely, gonadotroph tumors showed less tendency of invasiveness than null cell tumors. Gonadotroph cells are scattered throughout the pars distalis, and null cells are scattered throughout the anterior pituitary [17]. Nevertheless, the fact that null cell tumors have higher invasive ability than gonadotroph tumors should be considered for factors of invasiveness other than the site of origin.
Based on the above, a combination of tumor site and subtype could result in easy invasion of surrounding structures. Therefore, nonfunctioning Pit-NETs that develop at a young age or that invade surrounding structures despite of a relatively small size should be suspected as somatotroph, corticotroph, null cell tumors, or Pit-1 only positive tumors.
Recurrence rate and tumors subtype
Silent Pit-NETs with dedicated differentiation along the transcription factors (SF-1, T-PIT, Pit-1) may constitute primitive tumors arising from cells that initiated adenohypophyseal lineage differentiation, yet experienced an arrest in maturation before reaching the maturity required for hormone production [28]. For example, among lactotroph tumors in male, which are often aggressive with a high risk of recurrence and malignancy [6], tumors with low PRL producing ability have a low expression rate of ERα, are prone to invasion, and are poorly differentiated [29]. Transcription factors such as ERα and others may be involved in tumor upregulation and could contribute to the aggressive behavior of malignant Pit-NETs [26]. “Totally silent” Pit-NETs are more aggressive than non-silent Pit-NETs but may still be less prone to recurrence than primitive differentiated Pit-NETs negative for pituitary hormone.
Complete resection of tumors with cavernous sinus invasion is difficult. It was also reported that 57% of tumors with direct contact to the medial wall of the cavernous sinus have histologically cavernous sinus invasion [30], and medial wall resection for nonfunctioning Pit-NETs is challenging for surgeons, considering the risk of massive bleeding. Cavernous sinus invasion was the most associated factor for recurrence in the present study. Regarding recurrence and subtype, a statistically accurate evaluation cannot be performed due to the small number of cases. Conversely, Zhao et al. reported that Pit-1 lineage tumors with no immunoreactivity for pituitary hormone were more associated with aggressiveness and recurrence [31]. A relation between the MIB-1 index and recurrence has also been reported [32, 33]. Although the present study showed a correlation between the MIB-1 index and recurrence, larger cohort studies are needed.
Limitations
Notwithstanding the above, this study has a few limitations. First, this study was a single-center review of nonrandomized patients, which limits its generalizability. For example, in this study, the proportion of null cell tumors was higher than that in other studies [8], and it cannot be denied that this may have influenced the results. Second, histological examination for cavernous sinus invasion was not performed. Because the tumors in this study were nonfunctioning Pit-NETs, we refrained from removing the medial wall of the cavernous sinus, which appeared to have a normal medial wall while allowing bleeding from the sinus. Although it is acceptable to evaluate cavernous sinus invasion using radiological diagnosis and careful observation by experienced surgeons, early regrowth of residual tumors and recurrence during long-term follow-up have been noted [34]. Third, the small number of cases included for evaluation of recurrence and regrowth made statistical evaluation difficult. In this study, we excluded patients with tumor regrowth from recurrence assessment. However, differentiation between recurrence after gross total resection and tumor regrowth from small residual tumor could be sometimes challenging. Therefore, further multicenter trials are needed. Despite the aforementioned issues, the data on invasiveness and recurrence are interesting clinical information; we believe that this study serves to expand the knowledge in the field of pituitary tumors.
Conclusion
In nonfunctioning Pit-NETs, Pit-1 lineage tumors tend to invade the cavernous sinus, corticotroph tumors tend to have defect of the dura mater in the floor of the sellar turcica, and null cell tumors tend to have both aspects. Cavernous sinus invasion was a significant factor associated with recurrence.
Data availability
Not applicable.
References
(2014) Brain tumor registry of Japan (2001–2004). Neurol Med Chir (Tokyo) 54(Suppl):1–102. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4740110/
Asa SL, Mete O, Perry A, Osamura RY (2022) Overview of the 2022 WHO classification of pituitary tumors. Endocr Pathol 33:6–26. https://doi.org/10.1007/s12022-022-09703-7
Nishioka H (2023) Aggressive pituitary tumors (PitNETs). Endocr J 70:241–248. https://doi.org/10.1507/endocrj.EJ23-0007
Trouillas J, Roy P, Sturm N et al (2013) A new prognostic clinicopathological classification of pituitary adenomas: a multicentric case-control study of 410 patients with 8 years post-operative follow-up. Acta Neuropathol 126:123–135. https://doi.org/10.1007/s00401-013-1084-y
Ntali G, Wass JA (2018) Epidemiology, clinical presentation and diagnosis of non-functioning pituitary adenomas. Pituitary 21:111–118. https://doi.org/10.1007/s11102-018-0869-3
Trouillas J, Jaffrain-Rea ML, Vasiljevic A, Raverot G, Roncaroli F, Villa C (2020) How to classify the pituitary neuroendocrine tumors (PitNET)s in 2020. Cancers (Basel) 12:514. https://doi.org/10.3390/cancers12020514
Yamada S, Ohyama K, Taguchi M et al (2007) A study of the correlation between morphological findings and biological activities in clinically nonfunctioning pituitary adenomas. Neurosurgery 61:580–584. https://doi.org/10.1227/01.NEU.0000290906.53685.79
Nishioka H, Inoshita N, Mete O et al (2015) The complementary role of transcription factors in the accurate diagnosis of clinically nonfunctioning pituitary adenomas. Endocr Pathol 26:349–355. https://doi.org/10.1007/s12022-015-9398-z
Haddad AF, Young JS, Oh T et al (2020) Clinical characteristics and outcomes of null-cell versus silent gonadotroph adenomas in a series of 1166 pituitary adenomas from a single institution. Neurosurg Focus 48:E13. https://doi.org/10.3171/2020.3.FOCUS20114
Taguchi A, Kinoshita Y, Tokumo K et al (2022) Usefulness of critical flicker fusion frequency measurement and its laterality for evaluating compressive optic neuropathy due to pituitary neuroendocrine tumors. Neurosurg Rev 46:4. https://doi.org/10.1007/s10143-022-01915-z
Knosp E, Steiner E, Kitz K, Matula C (1993) Pituitary adenomas with invasion of the cavernous sinus space: A magnetic resonance imaging classification compared with surgical findings. Neurosurgery 33:610–617. https://doi.org/10.1227/00006123-199310000-00008
Kinoshita Y, Tominaga A, Usui S et al (2016) The surgical side effects of pseudocapsular resection in nonfunctioning pituitary adenomas. World Neurosurg 93:430–435. https://doi.org/10.1016/j.wneu.2016.07.036
Mete O, Kefeli M, Çalışkan S, Asa SL (2019) GATA3 immunoreactivity expands the transcription factor profile of pituitary neuroendocrine tumors. Mod Pathol 32:484–489. https://doi.org/10.1038/s41379-018-0167-7
Turchini J, Sioson L, Clarkson A, Sheen A, Gill AJ (2020) Utility of GATA-3 expression in the analysis of pituitary neuroendocrine tumour (PitNET) transcription factors. Endocr Pathol 31:150–155. https://doi.org/10.1007/s12022-020-09615-4
Mayson SE, Snyder PJ (2014) Silent (clinically nonfunctioning) pituitary adenomas. J Neurooncol 117:429–436. https://doi.org/10.1007/s11060-014-1425-2
Jiang S, Zhu J, Feng M et al (2021) Clinical profiles of silent corticotroph adenomas compared with silent gonadotroph adenomas after adopting the 2017 WHO pituitary classification system. Pituitary 24:564–573. https://doi.org/10.1007/s11102-021-01133-8
Anat Ben-Shlomo SM (2011) Chapter 2: Hypothalamic regulation of anterior pituitary function. In: Anat Ben-Shlomo, Shlomo Melmed. (ed) The Pituitary (Third edition), pp. 21–45. Academic Press (2011), https://www.academia.edu/19700586/The_Pituitary_3rd_Edition. Accessed 22 June 2023.
Perez-Rivas LG, Simon J, Albani A et al (2022) TP53 mutations in functional corticotroph tumors are linked to invasion and worse clinical outcome. Acta Neuropathol Commun 10:139. https://doi.org/10.1186/s40478-022-01437-1
McCormack A, Dekkers OM, Petersenn S et al (2018) Treatment of aggressive pituitary tumours and carcinomas: results of a European Society of Endocrinology (ESE) survey 2016. Eur J Endocrinol 178:265–276. https://doi.org/10.1530/EJE-17-0933
Asmaro K, Zhang M, Rodrigues AJ et al (2023) Cytodifferentiation of pituitary tumors influences pathogenesis and cavernous sinus invasion. J Neurol Surg 28:1–9. https://doi.org/10.3171/2023.3.JNS221949
Nishioka H, Fukuhara N, Horiguchi K, Yamada S (2014) Aggressive transsphenoidal resection of tumors invading the cavernous sinus in patients with acromegaly: predictive factors, strategies, and outcomes. J Neurosurg 121:505–510. https://doi.org/10.3171/2014.3.JNS132214
Langlois F, Woltjer R, Cetas JS, Fleseriu M (2018) Silent somatotroph pituitary adenomas: an update. Pituitary 21:194–202. https://doi.org/10.1007/s11102-017-0858-y
Cossu G, Daniel RT, Pierzchala K et al (2019) Thyrotropin-secreting pituitary adenomas: a systematic review and meta-analysis of postoperative outcomes and management. Pituitary 22:79–88. https://doi.org/10.1007/s11102-018-0921-3
Taguchi A, Kinoshita Y, Yamasaki F, Arita K, Tominaga A (2021) Clinical characteristics and thyroid hormone dynamics of thyrotropin-secreting pituitary adenomas at a single institution. Endocrine 73:151–159. https://doi.org/10.1007/s12020-020-02556-2
Yamada S, Fukuhara N, Horiguchi K et al (2014) Clinicopathological characteristics and therapeutic outcomes in thyrotropin-secreting pituitary adenomas: a single-center study of 90 cases. J Neurosurg 121:1462–1473. https://doi.org/10.3171/2014.7.JNS1471
Trouillas J, Delgrange E, Wierinckx A et al (2019) Clinical, pathological, and molecular factors of aggressiveness in lactotroph tumours. Neuroendocrinology 109:70–76. https://doi.org/10.1159/000499382
Mohyeldin A, Katznelson LJ, Hoffman AR et al (2022) Prospective intraoperative and histologic evaluation of cavernous sinus medial wall invasion by pituitary adenomas and its implications for acromegaly remission outcomes. Sci Rep 12:9919. https://doi.org/10.1038/s41598-022-12980-1
Lee JC, Pekmezci M, Lavezo JL et al (2017) Utility of Pit-1 immunostaining in distinguishing pituitary adenomas of primitive differentiation from null cell adenomas. Endocr Pathol 28:287–292. https://doi.org/10.1007/s12022-017-9503-6
Lloyd RV, Landefeld TD, Maslar I, Frohman LA (1985) Diethylstilbestrol inhibits tumor growth and prolactin production in rat pituitary tumors. Am J Pathol 118:379–386
Ishida A, Shiramizu H, Yoshimoto H et al (2022) Resection of the cavernous sinus medial wall improves remission rate in functioning pituitary tumors: retrospective analysis of 248 consecutive cases. Neurosurgery 91:775–781. https://doi.org/10.1227/neu.0000000000002109
Zhao J, Ji C, Cheng H et al (2023) Digital image analysis allows objective stratification of patients with silent PIT1-lineage pituitary neuroendocrine tumors. J Pathol Clin Res 9:488–497. https://doi.org/10.1002/cjp2.340
Lenders NF, Earls PE, Wilkinson AC et al (2023) Predictors of pituitary tumour behaviour: an analysis from long-term follow-up in 2 tertiary centres. Eur J Endocrinol 189:106–114. https://doi.org/10.1093/ejendo/lvad079
Tadokoro K, Wolf C, Toth J et al (2022) Ki-67/MIB-1 and recurrence in pituitary adenoma. J Neurol Surg B Skull Base 83(Suppl 2):e580–e590. https://doi.org/10.1055/s-0041-1735874
Ng S, Messerer M, Engelhardt J et al (2021) Aggressive pituitary neuroendocrine tumors: current practices, controversies, and perspectives, on behalf of the EANS skull base section. Acta Neurochir (Wien) 163:3131–3142. https://doi.org/10.1007/s00701-021-04953-6
Acknowledgements
We gratefully acknowledge the work of past and present members of Hiroshima University Hospital. The authors would like to thank Enago (www.enago.jp) for the English language review.
Funding
This work was supported by JSPS Grant-in-Aid for Scientific Research (C) (Grant number [JP23K06697]).
Author information
Authors and Affiliations
Contributions
Conception and design: Akira Taguchi. Acquisition of data: Akira Taguchi, Yasuyuki Kinoshita, Shumpei Onishi, Atsushi Tominaga. Analysis and interpretation: Akira Taguchi, Fumiyuki Yamasaki, Yasuyuki Kinoshita, Vishwa Jeet Amatya, Shumpei Onishi, Yukari Go. Drafting the article: Akira Taguchi. Critically revising the article: Fumiyuki Yamasaki, Yasuyuki Kinoshita, Yukio Takeshima, Nobutaka Horie. Reviewed submitted version of manuscript: all authors. Statistical analysis: Akira. Taguchi, Yasuyuki Kinoshita, Fumiyuki Yamasaki. Administrative/technical/material support: Vishwa Jeet Amatya, Atsushi Tominaga, Yukio Takeshima. Study supervision: Fumiyuki Yamasaki, Nobutaka Horie.
Corresponding author
Ethics declarations
Ethics approval
This study was conducted retrospectively, utilized data obtained for clinical purposes, and was approved by the ethics committee of Hiroshima University Hospital (E-2022, May 18, 2020).
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Informed consent
As patient data in this study are completely anonymized, any identification of individuals is difficult. Pertinent research content is available in the homepage of our institution.
Research involving participants and/or animals
Not applicable.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Taguchi, A., Kinoshita, Y., Amatya, V.J. et al. Differences in invasiveness and recurrence rate among nonfunctioning pituitary neuroendocrine tumors depending on tumor subtype. Neurosurg Rev 46, 317 (2023). https://doi.org/10.1007/s10143-023-02234-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10143-023-02234-7