Abstract
To compare the clinical efficacy of tablet and oral liquid L-thyroxine (LT4) formulation in naïve hypothyroid subjects with Helicobacter pylori infection. Forty-seven adult naïve hypothyroid subjects with dyspeptic symptoms were investigated with upper endoscopy and divided into: 28 patients with Helicobacter pylori infection (Group A); 15 patients without gastric alterations (group B); 4 patients with autoimmune gastritis were excluded from the study. Subjects were randomly treated with a same dose of LT4 tablet (TAB) or oral liquid formulation (SOL), for 9 months on group A and 6 months on group B. Helicobacter pylori infection was eradicated after 3 months of LT4 treatment. On group A, after 3 months (before Helicobacter pylori eradication), subjects treated with SOL showed a greater thyroid-stimulating hormone reduction (ΔTSH3–0: TAB = −4.1 ± 4.6 mU/L; SOL = −7.7 ± 2.5 mU/L; p = 0.029) and a greater homogeneity in the thyroid-stimulating hormone values (TSH3mo: TAB = 5.7 ± 4.9 mU/L; SOL = 4.1 ± 2.0 mU/L; p = 0.025), compared to LT4 tablet. At 9 months (after 6 months of Helicobacter pylori eradication) mean thyroid-stimulating hormone values were lower in subjects treated with LT4 tablet (TSH9mo: TAB = 1.8 ± 1.2 mU/L; SOL = 3.2 ± 1.7 mU/L; p = 0.006). On group B no difference were observed, at each time point, in the mean thyroid-stimulating hormone values and thyroid-stimulating hormone variations between two LT4 formulations. LT4 liquid formulation may produce a better clinical response compared to the tablet formulation in hypothyroid subjects with Helicobacter pylori infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypothyroidism is a condition widely prevalent in the general population and its treatment is represented by L-thyroxine (LT4), which is characterized by simplicity of administration, ease of use and low cost. However, the long-lasting use of oral LT4 treatment needs an accurate dose management. The use of an individually tailored dose of LT4 adjusted by age, body weight or body mass index is recommended in clinical practice [1]. Despite these precautions, some patients fail to show an adequate chemical and clinical response to the designed dose of LT4 [2, 3], and frequently they are diagnosed malabsorption due to several gastrointestinal disorders on further examinations.
In recent years new formulations of LT4 have become available: the oral solution and the soft-gel capsule. In both cases the active ingredient is administered as a solute, therefore its intestinal absorption process differs from the traditional tablet formulation because of the absence of the dissolution phase [4].
In the case of LT4 tablet, structured as stable salt containing sodium, the dissolution phase is relevant for subsequent absorption and, an intact acid gastric pH, plays an essential role to dissolve the tablet by removing sodium ion and converting LT4 into a lipophilic molecule [5]. Many conditions, interfering with the normal acid-secretory activity of the stomach, may affect LT4 tablet absorption [6, 7]. Usually the acid environment of the stomach becomes altered in patients with Helicobacter pylori (H. pylori)-related gastritis, atrophic gastritis of the gastric body, or both, as well as in patients who are receiving long-term treatment with proton-pump-inhibitors (PPI) [8]. Also patients with gastrointestinal symptoms but with no evidence of structural disease (“functional dyspeptic patients”) should be taken into account while evaluating the effect of LT4 supplementation because they are more likely to be prescribed drugs that can alter gastric pH [9].
The relationship between H. pylori infection and drugs absorption is due to the close link that exists between the bioavailability of a drug and the level of gastric acidity (pH) that is in turn influenced by H. pylori presence [10]. Once in the stomach, the molecular structure of each drug is modified by the levels of acidity in the gastric environment, if the pH of the stomach is modified there is uncertainty about the dose that is absorbed.
Notwithstanding the fact that this infection can potentially alter the bioavailability of any drug, those who are part of a therapy designed to compensate for a lack or deficiency arising from inadequate nutrition, dysfunctions or losses (replacement therapies) are more likely to be affected by its presence and are potentially of an high clinical interest due to the close relationship between the drug effect and the dose administered [11].
It has been clearly demonstrated that patients with impaired acid secretion require an increased dose of LT4: the daily requirement was higher (by 22–34 %) in patients with H. pylori related gastritis, atrophic gastritis or both conditions [12]. The absence of clear guidance on the use of LT4 in such conditions underlines the significance of performing further evaluations on this topic.
Our study aimed to compare the clinical efficacy of LT4 tablet and LT4 oral liquid solution in naïve subjects with primary hypothyroidism and altered gastrointestinal absorption due to infection of H. pylori.
Patients and methods
Patients and study design
The study was conducted from January 2013 to December 2015 in a tertiary outpatient Endocrinology Unit and Internal Medicine Unit. During this period 47 subjects (aged 23–68 years) newly diagnosed with primary hypothyroidism and dyspeptic symptoms [9] were consecutively examined. Inclusion criteria were: (1) first diagnosis of primary hypothyroidism due to chronic autoimmune thyroiditis (2) dyspeptic symptoms defined as “bothersome postprandial fullness”; “early satiation”; “epigastric pain” and “epigastric burning”. Exclusion criteria were: (1) pregnancy; (2) drugs or substances that can interfere with the metabolism of LT4 in the last 12 months [6, 7, 13]; (3) patients with BMI > 30; (4) presence of autoimmune gastritis; (5) previous intestinal surgery; (6) anamnestic and clinical signs of chronic malabsorption (chronic diarrhea, loss of weight, food restriction); (7) celiac disease; (8) lactose intolerance.
Diagnosis of hypothyroidism
The diagnosis of primary hypothyroidism was based on the presence of at least two consecutive serum thyroid-stimulating hormone (TSH) levels upper to 4.5 mU/L with normal/reduced serum free T4. The diagnosis of autoimmune thyroiditis (Hashimoto’s thyroiditis) was based on the presence of at least one of the following criteria: high titer of anti-thyroperoxidase antibodies (anti-TPOAb) and/or characteristic ultrasonographic pattern.
Evaluation of dyspeptic symptoms
All patients underwent: (1) accurate medical history assessment to investigate the presence of chronic diarrhea, rectal bleeding, previous gastro-intestinal interventions or lactose intolerance; (2) upper endoscopy; (3) measurement of anti-gastric parietal cell antibodies and gastrin in all subjects with histological evidence of gastric atrophy; (4) measurement of anti-gliadin antibodies, anti-endomysium antibodies in subjects with macroscopic evidence of altered duodenal mucosa or with sign, symptom or clinical history suspicious for celiac disease.
43 patients fulfilled inclusion criteria and they were subsequently divided into two groups: Group A (28 patients) dyspeptic patients with H. pylori positive gastritis; Group B (15 patients) functional dyspeptic patients (concomitant presence of dyspeptic symptoms but no evidence of structural disease at upper endoscopy that can explain the symptoms).
All patients underwent upper endoscopy with biopsy specimens taken for histology (2 samples from the antrum, 1 sample from the incisura angularis, 2 samples from the corpus) and 1 additional sample from the antrum for a rapid urease test as routinely performed in our center. In H. pylori positive patients two additional biopsy specimens were taken from the antrum to perform bacterial culture.
Treatment groups
Patients were divided into two groups according to their histological findings: (A) H. pylori positive gastritis; (B) functional dyspeptic patients (concomitant presence of dyspeptic symptoms but no evidence of structural disease that can explain the symptoms).
Subjects of group A and B were randomized to receive two different formulations of LT4: tablet (Eutirox, Bracco, Milan, Italy) or oral liquid formulation (Tirosint, IBSA, Lugano, Switzerland). According to the most recent clinical indications [1], LT4 replacement therapy was started at a dose of 1.6 mcg/kg/day, which was maintained for all the study duration. After 3 months of LT4 treatment, subjects of Group A underwent eradication therapy for H. pylori infection and the observation was continued for an additional 6 months. Subjects of Group B were observed for 6 months since the start of LT4 treatment. Compliance to the treatments was checked at each time point by a self-reported questionnaire.
On group A, the assessment of serum TSH and free T4 levels was performed on blood samples at first examination (before starting LT4 supplementation), at 3 months (before eradication of H. pylori infection) and at 6 and 9 months of LT4 treatment (respectively 3 and 6 months after H. pylori eradication). On group B the assessment of serum TSH and free T4 level on blood samples was performed at first examination (before starting LT4 supplementation) and at 3 and 6 months of LT4 treatment. Bloods samples were collected at the morning (8.00–9.00 a.m.), after a 12 h overnight fast and before assumption of LT4 treatment.
Eradication of H. Pylori infection
H. pylori positive patients underwent eradication treatment with sequential regimen (esomeprazole 40 mg, amoxicillin 1 gr twice daily for the first 5 days, then esomeprazole 40 mg, clarithromycin 500 mg, tinidazole 500 mg twice daily for other 5 days). Compliance was considered good when more than 90 % of drugs were taken. Treatment success was evaluated by using a standard 13C urea breath test (UBT) performed 6–8 weeks after treatment ended. The UBT was performed after an overnight fast. A baseline breath sample was obtained, and 75 mg of 13C urea with citric acid (1.5 g) was administered as an aqueous solution. Another breath sample was collected after 30 min. The results of the test were considered positive if the difference between the baseline sample and the 30-min sample exceeded 4.5 parts per 1000 of 13CO2 [14].
Laboratory assays
Serum TSH levels were assayed with an automated method (IMMUNOLITE 2000 analyzer, SIEMENS—DPC, Erlangen, Germany). TSH normal range: 0.27–4.2 mU/L; sensitivity: 0.04 mU/L; intra-assay and inter-assay variation were 2.4 and 4.0 % respectively. Serum free-T4 levels were assayed with an automated method (IMMUNOLITE 2000 analyzer, SIEMENS—DPC, Erlangen, Germany). Free-T4 normal range: 9–17 pg/mL. Serum anti-thyroid peroxidase antibodies (anti-TPOAb) were assayed with an automated method (IMMUNOLITE 2000 analyzer, SIEMENS—DPC, Erlangen, Germany). Anti-TPOAb normal range: <34 U/mL.
Statistical analysis
Frequencies, mean ± standard deviation (SD) were calculated for each relevant variable. Normal distribution was checked by the Kolmogorov-Smirnov test. Comparisons between continuous variables [TSH, variation of TSH (ΔTSH), free T4 and variation of free T4 (ΔfT4)] were performed by Multivariate Analysis of Variance (MANOVA) adjusted for age, BMI and gastric histological findings. A test of Homogeneity of Variances (Levene’s test) was also performed in order to compare continuous variables (TSH, ΔTSH) between different therapies or groups. Two-tailed p-values of <0.05 were considered significant.
Statistical analyses were performed using SPSS Statistics for Windows v13.0 software (SPSS, Inc., Chicago, IL).
Ethical issues
The study has been approved by the local Ethical Committee (S. Orsola-Malpighi Hospital, Bologna, Italy). Written informed consent was obtained from all patients included in the study.
Results
Patient’s baseline characteristics
All patients with primary hypothyroidism and dyspeptic symptoms were consecutively enrolled in the study. The gastroenterological work-up identified: 28 patients with H. pylori related gastritis (group A); 15 patients with no evidence of gastric structural alterations (group B) and, finally, 4 patients with chronic atrophic gastritis associated with positivity of anti-gastric parietal cell antibodies (group C) that did not fulfill the inclusion criteria. The clinical and biochemical basal characteristics of the remaining 43 patients are described in Table 1.
Subjects were randomized for the two LT4 formulations as follow: on group A, 14 subjects were treated with the tablet formulation (TAB), 14 patients with the oral liquid formulation (SOL); on group B, 8 patients were treated with TAB and 7 patients with SOL.
In patients of group A no difference were observed in the distribution of the histological findings between patients treated with different LT4 formulations (14 patients of Group A treated with TAB: 9 subjects with superficial gastritis, 4 with gastric atrophy and 1 subject with erosive gastritis; 14 patients of Group A treated with SOL: 10 subjects with superficial gastritis and 4 with gastric atrophy).
TSH and fT4 response to LT4 treatment
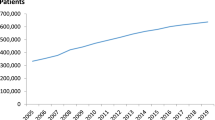
The mean values of TSH at each time point of the study, and the mean variation of TSH (ΔTSH) between different time point, in all subjects, separated by group and LT4 formulation are summarized on Table 2. Mean basal TSH values were not significantly different between patients randomized to receive different LT4 formulations on each group. On group A (H. pylori positive patients), after 3 months of treatment with LT4 (before H. pylori eradication) the mean TSH reduction from the baseline was significantly higher in subjects treated with SOL. At 6 months of treatment (after 3 months of H. pylori eradication), no difference where observed on mean TSH values or mean TSH variation between two LT4 formulations. At 9 months of treatment (after 6 months of H. pylori eradication) the mean TSH values were significantly lower in subjects treated with TAB (Fig. 1). There were no statistical significant differences on mean fT4 values and mean fT4 variation all around the observation period between two LT4 formulations (data not showed).
On group B (dyspeptic patients with no evidence of H. pylori infection), after 3 and 6 months of treatment there were no significant differences on mean TSH values and TSH variations between two LT4 formulations. (Fig. 2). Moreover there were no significant differences on mean fT4 values and mean fT4 variation from baseline all around the study observation (data not showed).
Patients treated with the same LT4 formulation were also compared between group A and group B: no difference were observed in the mean TSH or in the mean TSH variation values at each time points between groups.
We compared the homogeneity of TSH values after the start of LT4 treatment, between two formulations. On group A, at the third month (before H. pylori eradication), patients treated with SOL showed a bigger homogeneity of TSH values compared to subjects treated with TAB (TSH3mo: TAB = 5.7 ± 4.9 mU/L; SOL = 4.1 ± 2.0 mU/L; p = 0.025); this difference was instead not observed after the eradication of H. pylori infection at the 6 and 9 month of treatment (Fig. 3). On group B the homogeneity of TSH values after 3 and 6 months of LT4 treatment was similar between two formulations.
On group A we finally compared mean TSH, ΔTSH, freeT4 and ΔfT4 between patients with superficial gastritis and gastric atrophy treated with the same LT4 formulation, and no differences were observed. When considering only subjects with superficial gastritis or with gastric atrophy, the response between different LT4 formulations was similar to how described above: in both different histological groups, patients treated with SOL showed a significantly lowering of TSH since baseline and a bigger homogeneity of TSH at the control performed at 3 months (before eradication of H. pylori) with respect to subjects treated with TAB. After 3 months since the eradication of H. pylori, mean TSH values were similar between two formulations, while after 6 months mean TSH values were slightly but significantly lower in subjects treated with TAB (Table 3).
Discussion
Beside the traditional LT4 tablet, different formulations are now day available for the treatment of hypothyroidism (liquid oral solution, soft-gel capsules) [4, 6]. Current guideline for the treatment of hypothyroidism [1] do not give clear indication for the use of oral liquid formulation as an alternative to tablet, although this topic is largely debated [15] and an increased number of publications have been available in recent years. So far the liquid oral solution has shown a better therapeutic effect than tablets in patients undergoing bariatric surgery [16], with congenital hypothyroidism [17], under PPI treatment [18] or when administered with breakfast [19, 20], in case of autoimmune atrophic gastritis [21] and even in subjects without malabsorption [22].
In the present study we observed that a first line therapy based on LT4 liquid formulation administered to naïve hypothyroid patients with H. pylori infection and dyspeptic symptoms, provided a better therapeutic response than tablet LT4 formulation. This better response is characterized by an increased mean TSH reduction from baseline and by a better homogeneity of TSH values during H. pylori infection.
H. pylori has been already suggested as a causal agent of drug malabsorption: there is a robust evidence that this infection is one of the principal determinants of altered gastric acid secretion whose severity depends on the extension of the distribution of the infection in the stomach and on the duration of the disease. If the infection is mainly localized in the corpus, there is a decrease in acid secretion due to the effect of pro-inflammatory products (cytokines) on gastric parietal cell, but this process could still be reverted if the infection is detected and the pathogen is eradicated [23]. If the infection persists and becomes chronic, it leads to the complete loss of parietal cells (gastric atrophy) that determines a permanent acid reduction [24]. These modifications, related to H. pylori infection, are held responsible of altered drugs absorption due to the close link that exists between the bioavailability of a drug and the level of gastric acidity (pH). The dissolution phase of the LT4 tablet formulation is an essential step for its subsequent absorption from the gut and this phase is highly dependent on the gastric pH [2, 5]; the presence of H. pylori infection can lead to a malabsorption and to an increased requirement of LT4 if administered in tablet formulation [12]. LT4 liquid formulations, whose mechanism of absorption is instead not strictly dependent on gastric pH, can overcome this problem as showed recently on LT4 soft gel capsule formulation [25] and, according to our findings, similar results can be obtained with oral liquid solution of LT4.
It has been already shown that switching to a LT4 liquid formulation lead to a reversible normalization of serum TSH levels in patients with autoimmune atrophic gastritis who received LT4 in tablet form [21]. In our study, the comparison between different LT4 formulations, if performed separately in subjects of group A with superficial gastritis or with gastric atrophy, showed similar results: higher mean TSH reduction from baseline and a better homogeneity of TSH values on subjects treated with LT4 oral liquid formulation with respect to tablet formulation. This finding could be explained by the mechanisms of impairment of acid production induced by H. pylori infection that is not only related to the potential development of gastric atrophy but also to the effect of pro-inflammatory products (cytokines) on gastric parietal cell [23].
In a previous systematic review Lanher et al. [11] provided evidence of a relationship between H. pylori infection and the absorption of different drugs (LT4, L-dopa and delaviridine). Drugs who are part of replacement therapies are more likely to be affected by its presence and are potentially of an high clinical interest due to the close relationship between the drug effect and the dose administered. An example of the potential damage of the uncertainty about the drug absorbed dose in the presence of H. pylori infection has been demonstrated by Bugdaci et al. [26]; who evaluated the potential interference of H. pylori in patients with hypothyroidism under hormonal replacement therapy with LT4, in whom normal TSH levels could not be achieved despite treatment with high doses of tablet LT4. They conclude that not only H. pylori gastritis is responsible for an inadequate response to the treatment but also that, after eradication, cases receiving high doses of LT4 have a higher risk for developing factitious thyrotoxicosis.
According to previous findings, in the present study we confirmed that eradication of H. pylori infection improves the clinical efficacy of the LT4 tablet formulation; this is demonstrated not only by the reduction of the mean TSH values, but also by the reduction of the heterogeneity of TSH values after the eradication. With the LT4 oral liquid formulation we instead observed a similar mean TSH values and TSH homogeneity all around the treatment period regardless of the eradication of H. pylori infection. This is an interesting finding that could solve the problem of maintaining an adequate clinical efficacy in all hypothyroid subjects who have to undergo treatment for the eradication of H. pylori infection.
In conclusion our study confirm that H. pylori infection is able to cause malabsorption of LT4 tablet formulation that is restored by its eradication, therefore an accurate evaluation of all hypothyroid patients with dyspeptic symptoms is recommended in order to rapidly identify and treat the infection. It also shows that the oral liquid LT4 formulation is more effective than the traditional LT4 tablet formulation if administered in the presence of H. pylori infection. In addition, H. pylori eradication does not change, in contrast to what observed with the tablet formulation, its effectiveness. These results should be taken into account while evaluating dyspeptic hypothyroid patients in the clinical practice.
References
J. Jonklaas, A.C. Bianco, A.J. Bauer, K.D. Burman, A.R. Cappola, F.S. Celi, D.S. Cooper, B.W. Kim, R.P. Peeters, M.S. Rosenthal, A.M. Sawka; American Thyroid Association Task Force on Thyroid Hormone Replacement, Guidelines for the treatment of hypothyroidism: prepared by the american thyroid association task force on thyroid hormone replacement. Thyroid. 24, 1670–1751 (2014)
S. Benvenga, L. Bartolone, S. Squadrito, F. Lo Giudice, F. Trimarchi, Delayed intestinal absorption of levothyroxine. Thyroid. 5, 249–253 (1995)
C.L. Perez, F.S. Araki, H. Graf, G.A. de Carvalho, Serum thyrotropin levels following levothyroxine administration at breakfast. Thyroid. 23, 779–784 (2013)
R. Vita, P. Fallahi, A. Antonelli, S. Benvenga, The administration of L-thyroxine as soft gel capsule or liquid solution. Expert. Opin. Drug. Deliv. 11, 1103–1111 (2014)
K.W. Wenzel, H.E. Kirschsieper, Aspects of the absorption of oral L-thyroxine in normal man. Metabolism. 26, 1–8 (1977)
M. Centanni, Thyroxine treatment: absorption, malabsorption, and novel therapeutic approaches. Endocrine. 43, 8–9 (2013)
L. Liwanpo, J.M. Hershman, Conditions and drugs interfering with thyroxine absorption. Best. Pract. Res. Clin. Endocrinol. Metab. 23, 781–792 (2009)
G. Sachs, J.M. Shin, K. Munson, O. Vagin, N. Lambrecht, D.R. Scott, D.L. Weeks, K. Melchers, Review article: the control of gastric acid and Helicobacter pylori eradication. Aliment. Pharmacol. Ther. 14, 1383–1401 (2000)
Rome III Diagnostic Criteria for FGIDs (2016), http://www.romecriteria.org/assets/pdf/19_RomeIII_apA_885-898.pdf Accessed 18 Jul 2016.
E. Lahner, B. Annibale, G. Delle Fave, Systematic review: impaired drug absorption related to the co-administration of antisecretory therapy. Aliment. Pharmacol. Ther. 29, 1219–1229 (2009a)
E. Lahner, B. Annibale, G. Delle Fave, Systematic review: helicobacter pylori infection and impaired drug absorption. Aliment. Pharmacol. Ther. 29, 379–386 (2009b)
M. Centanni, L. Gargano, G. Canettieri, N. Viceconti, A. Franchi, G. Delle Fave, B. Annibale, Thyroxine in goiter, helicobacter pylori infection, and chronic gastritis. N. Engl. J. Med. 354, 1787–1795 (2006)
M.I. Surks, R. Sievert, Drugs and thyroid function. N. Engl. J. Med. 333, 1688–1694 (1995)
N. Vakil, A. Zullo, C. Ricci, C. Hassan, D. Vaira, Duplicate breath testing to confirm eradication of Helicobacter pylori: incremental benefit and cost in 419 patients. Aliment. Pharmacol. Ther. 28, 1304–1308 (2008)
A.M. Formenti, G. Mazziotti, R. Giubbini, A. Giustina, Treatment of hypothyroidism: all that glitters is gold? Endocrine. 52, 411–413 (2016)
I. Pirola, A.M. Formenti, E. Gandossi, F. Mittempergher, C. Casella, B. Agosti, C. Cappelli, Oral liquid L-thyroxine (l-T4) may be better absorded compared to l-T4 tablets following bariatric surgery. Obes. Surg. 23, 1493–1496 (2013)
A. Cassio, S. Monti, A. Rizzello, I. Bettocchi, F. Baronio, G. D’Addabbo, M.O. Bal, A. Balsamo, Comparison between liquid and tablet formulations of levothyroxine in the initial treatment of congenital hypothyroidism. J. Pediatr. 162, 1264–1269 (2013)
R. Vita, G. Saraceno, F. Trimarchi, S. Benvenga, Switching levothyroxine from the tablet to the oral solution formulation corrects the impaired absorption of levothyroxine induced by proton-pump inhibitors. J. Clin. Endocrinol. Metab. 12, 4481–4486 (2014)
C. Cappelli, I. Pirola, L. Daffini, A. Formenti, C. Iacobello, A. Cristiano, E. Gandossi, E. Agabiti Rosei, M. Castellano, A double-blind placebo-controlled trial of liquid thyroxine Ingested at breakfast: results of the TICO study. Thyroid. 26, 197–202 (2016)
S. Morelli, G. Reboldi, S. Moretti, E. Menicali, N. Avenia, E. Puxeddu, Timing of breakfast does not influence therapeutic efficacy of liquid levothyroxine formulation. Endocrine. 52, 571–578 (2016)
P. Fallahi, S.M. Ferrari, I. Ruffilli, A. Antonelli: Reversible normalisation of serum TSH levels in patients with autoimmune atrophic gastritis who received L-T4 in tablet form after switching to an oral liquid formulation: a case series. BMC Gastroenterol (2016). doi:10.1186/s12876-016-0439-y
P. Fallahi, S.M. Ferrari, A. Antonelli, Oral L-thyroxine liquid versus tablet in patients with hypothyroidism without malabsorption: a prospective study. Endocrine. 52, 597–601 (2016)
K.E. McColl, Helicobacter pylori and dyspepsia. Pro and against. Dig. Liver. Dis. 32, 199–201 (2000)
M. Feldman, B. Cryer, E. Lee, Effects of Helicobacter pylori gastritis on gastric secretion in healthy human beings. Am. J. Physiol. 274, 1011–1017 (1998)
M.G. Santaguida, C. Virili, S.C. Del Duca, M. Cellini, I. Gatto, N. Brusca, C. De Vito, L. Gargano, M. Centanni, Thyroxine softgel capsule in patients with gastric-related T4 malabsortion. Endocrine. 49, 51–57 (2015)
M.S. Bugdaci, S.S. Zuhur, M. Sokmen, B. Toksoy, B. Bayraktar, Y. Altuntas, The role of Helicobacter pylori in patients with hypothyroidism in whom could not be achieved normal thyrotropin levels despite treatment with high doses of thyroxine. Helicobacter. 16, 124–130 (2011)
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Ribichini, D., Fiorini, G., Repaci, A. et al. Tablet and oral liquid L-thyroxine formulation in the treatment of naïve hypothyroid patients with Helicobacter pylori infection. Endocrine 57, 394–401 (2017). https://doi.org/10.1007/s12020-016-1167-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-016-1167-3