Abstract
No consistent data are present in literature about the effectiveness of levothyroxine (l-T4) liquid formulation in patients without malabsorption. The aim of this study is to compare the effectiveness of l-T4 liquid formulation, with l-T4 tablets, in hypothyroid patients without malabsorption or drug interference. One hundred and fifty two patients were recruited. Patients were switched from the l-T4 therapy in tablets, to liquid l-T4 at the same dosage, 30 min before breakfast. Serum thyrotropic hormone (TSH), free thyroxine (FT4), and free triiodothyronine (FT3) were re-evaluated after 1–3 months (first control) and 5–7 months (second control) from the switch. TSH values significantly declined with respect to the basal value after the switch to liquid l-T4 both at the first control (P < 0.05) and at the second control (P < 0.01); FT4 and FT3 levels were not significantly changed. We show that liquid l-T4 is more effective than l-T4 tablet in controlling TSH levels in hypothyroid patients without malabsorption, gastric disorders, or drug interference.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Levothyroxine (l-T4) is one of the most prescribed drugs, because hypothyroidism is a relatively common disorder and its frequency increases with age [1, 2].
On average, 70 % of the orally ingested l-T4 is absorbed, the absorption occurring in the upper intestine (duodenum, jejunum, and ileum) [3]; an acid intragastric pH is required for optimal dissolution of the l-T4 tablet [4, 5].
There are a number of conditions of the digestive system and a number of drugs/supplements/beverages that cause l-T4 malabsorption [6–9]. These conditions include Helicobacter pylori-associated gastritis, autoimmune gastritis, and even simple positivity for parietal cell autoantibodies, lactose intolerance, celiac disease, intestinal parasitic diseases, operations of bariatric surgery, and even coffee [10–16].
Traditionally, thyroxine is used worldwide in tablet (also generic) form, but new formulations in soft gel capsule or liquid formulation are now available.
Many reports have shown an increased absorption rate with liquid l-T4 formulation as opposed to tablet form both in adults and in children [17].
Cassio et al. have recently observed, in a small number of infants with congenital hypothyroidism, a more frequent suppression of thyrotropic hormone (TSH) among patients treated with liquid formulation, suggesting that liquid form is more efficacious than tablet form which has to be crushed and thereby undergoing a process that might cause some loss of the drug [18].
Failure of l-T4 treatment to reach target serum TSH levels generally prompts the physicians to increase l-T4 daily dose. However, in vivo studies have demonstrated that the liquid formulation is capable of solving the l-T4 tablet malabsorption caused by certain drugs, bariatric surgery, or coffee. These new formulations may be attractive also for patients who cannot/do not want to change their (improper) habits of l-T4 ingestion. Finally, the l-T4 oral solution could be suitable for patients who cannot swallow the solid formulations [14, 19–22].
However, until now, to the best of our knowledge, no consistent data are present in literature about the effectiveness of l-T4 liquid formulation in patients without malabsorption [23, 24].
The aim of this study is to compare the effectiveness of l-T4 liquid formulation, with l-T4 tablets, in hypothyroid patients without malabsorption or drug interference.
Patients and methods
This is an observational, prospective study that has enrolled patients treated with l-T4 in tablet, for the substitutive therapy of hypothyroidism from November 2013 to January 2015.
Inclusion criteria were as follows: a-substitutive therapy of hypothyroidism for autoimmune thyroiditis or after near-total thyroidectomy for benign nodular or mutinodular goiter for a period longer than 1 year; b-age between 18 and 75 years; c-TSH values at last control (within 1 month) between 0.8 and 4 μIU/mL, under stable dosage of l-T4 in tablet, in the last year; and d-consensus of the patients to participate in the study.
Exclusion criteria were as follows: major psychiatric disorders; patients unable to understand the scope of the study and adhere to it; patients unable to give a valid consensus; abuse of alcohol or drugs; patients with thyroid nodules Thyr3–Thyr4–Thyr5 [25]; allergy or intolerance to the studied drugs; history of neoplastic disorders under therapy in the last 5 years; hepatitis C or B; hepatic disorders and dysfunction (increase of alanine aminotransferase or aspartate transaminase); impaired renal function [Modification of Diet in Renal Disease (MDRD) < 29 mL/min/1.73 mq]; history of myocardial infarction, atrial fibrillation, or other tachyarrhythmias; severe anemia [hemoglobin (Hb) < 10 g/dL)]; history and presence of atrophic gastritis, gastritis associated with H. Pylori infection, lactose intolerance, celiac disease, and intestinal malabsorption; previous bariatric surgery, or gastric or intestinal surgery; pregnancy; concomitant therapy with proton pump inhibitors, or amiodarone, beta-blockers, lithium, orlistat, raloxifene, cholestyramine, interferons, and antacids; and urinary iodine >250 μg/dL.
Patients were screened for other gastrointestinal diseases to avoid bias in the assessment of T4 malabsorption: (a) clinically by excluding anemia caused by cobalamin deficiency or iron deficiency; long-standing uninvestigated dyspepsia, as indicated by bloating, fullness, or burning; or a combination of these conditions; or diarrhea; (b) furthermore, the screening was performed by measuring gastrin, antiparietal cell antibodies, anti-tissue transglutaminase IgG and IgA antibodies, antiendomysial IgG and IgA antibodies, and H. pylori antigen in the stool [12]; only patients with negative results were included in the study.
One hundred and fifty two patients were recruited. Patients were switched from the l-T4 therapy in tablets, to liquid l-T4 (Tirosint® fiala monouso, IBSA Farmaceutici Italia) at the same dosage.
Patients agreed to take thyroxine under fasting conditions, abstaining from eating or drinking anything other than water for at least 30 min after treatment (before breakfast), both with l-T4 therapy in tablets or with liquid l-T4. Serum TSH, free thyroxine (FT4), and free triiodothyronine (FT3) were re-evaluated after 1–2 and 5–7 months from the switch. The study was approved by the local ethical committee.
Serum FT4 (normal range 0.7–1.7 ng/dL), FT3 (normal range 2.7–4.7 pg/mL), and serum TSH (normal range 0.4–4 μIU/mL) were determined in all samples by electrochemiluminescence immunoassay (Roche Corporation, Indianapolis, IN, USA). The concentration of each hormone at baseline, and after the switch, was calculated as a mean of the two samples collected before the l-T4 dose. Antithyroperoxidase antibodies (AbTPO) and antithyroglobulin antibodies (AbTg) (ICN Pharmaceuticals, USA; positivity was set at >100 IU/mL) were evaluated.
Data analysis
The values are given as mean ± SD for normally distributed variables, otherwise as median and interquartile range [IQR1–IQR3]. Group values were compared using one-way ANOVA for normally distributed variables [age and body mass index (BMI)]. Post hoc comparisons on normally distributed variables were carried out using the Bonferroni–Dunn test, or Fisher PLSD. Not normally distributed variables (TSH, l-T4 dosage, etc.) were compared by Kruskal–Wallis test (>3 groups), or by Mann–Whitney test (2 groups). Proportions were compared by the χ 2 test.
Results
Among the 152 recruited patients, 11 switched back to l-T4 tablets because of some discomfort in taking liquid l-T4 and were lost to follow up.
The 141 remaining patients were evaluated both at 1–3 months and at 5–7 months from the switch [116 females, 25 males; mean age 51.3 ± 14.3 years; 98 with autoimmune hypothyroidism [thyroid volume, median 14 mL, IQR1–IQR3 6–28 mL; AbTPO, median 323 IU/mL, IQR1-IQR3 75–752 IU/mL; AbTg, median 202 IU/mL, IQR1–IQR3 58–542 IU/mL]; 43 with near-total thyroidectomy].
The first evaluation (1–3 months) was made after 45 ± 7 days from the initial switch, while the second evaluation (5–7 months) was made after 175 ± 17 days. Body weight was not significantly changed (BMI, base 24.1 ± 2.6 kg/m2, first control 24.4 ± 2.7 kg/m2, second control 24.3 ± 2.5 kg/m2).
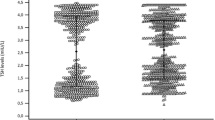
TSH values significantly declined with respect to the basal value after the switch to liquid l-T4 both at the first control (P < 0.05) and at the second control (P < 0.01) (Fig. 1). FT4 and FT3 levels were not significantly changed (data not shown). A similar decline of TSH was observed in patients aged ≤50 or >50 years (Table 1), even if the l-T4 dosage was higher in the younger patients [18 ≤ age ≤ 50, T4 dose of 1.51 μg/kg/day (IQR1–IQR3 1.34–1.67 μg/kg/day); 50 < age ≤ 75, T4 dose of 1.39 μg/kg/day (IQR1–IQR3 1.21–1.48 μg/kg/day); P < 0.05].
After the switch no patient has hypothyroid. TSH values between 3 and 4 μIU/L were present in 12 % of patients at baseline, in 5 % at the first control, and in 4 % at the second control (χ 2 = 7.96, P = 0.023), suggesting a better control of TSH by liquid formulation in these patients. No patient had a TSH < 0.2 μIU/L after the switch at both controls.
A similar decline of TSH values, with respect to the basal value, after the switch to liquid l-T4, was observed both in patients affected by autoimmune thyroiditis (Fig. 2a) as well as in the thyroidectomized patients (Fig. 2b), with no significant difference between the two groups; the l-T4 dosage was higher in the thyroidectomized patients [thyroidectomized, T4 dose of 1.63 μg/kg/day (IQR1–IQR3 1.43–1.81 μg/kg/day); autoimmune thyroiditis, T4 dose of 1.41 μg/kg/day (IQR1–IQR3 1.19–1.57 μg/kg/day; P < 0.05].
Discussion
The obtained results first show that liquid l-T4 is more effective than l-T4 tablet in controlling TSH levels in hypothyroid patients without malabsorption, gastric disorders, or drug interference. Considering that there was no change in the drug dosage, we hypothesize that the TSH decline could be related to an increased absorption of l-T4 with the liquid formulation; the involved mechanisms need to be further studied.
Normal gastric acid secretion is necessary for effective absorption of l-T4 [4] by dissolution of tablets, and drug dissolution and solubility may be altered by restrictive procedures that increase gastric pH in the newly created stomach pouch; this may occur in gastric bypass [26]. It has been also shown that the liquid formulation of l-T4 is extremely effective to circumvent the problem of incomplete absorption of the l-T4 caused by proton pump inhibitors [27]. Indeed, our patients had no malabsorption or gastric disorders, nor drug interference.
However, previous pharmacokinetic studies showed that liquid l-T4 has a clearly faster onset of absorption, with respect to tablets (area under the curve from 0 to 2 h greater than 50 %; time to maximum concentration faster by a mean of 30 min), and as a consequence it does not need gastric dissolution and enters directly into the small bowel where l-T4 is absorbed [28–31].
Furthermore, the presence of alcohol in the l-T4 liquid formulation could also play a key role in thyroxine absorption. Oral mucosal is highly vascularised, and drugs that are partially absorbed through the oral mucosa directly enter the systemic circulation, bypassing the gastrointestinal tract [32]. Further studies are needed to clarify these intriguing points.
Our results are in agreement with a retrospective study (Brancato et al.) that evaluated 53 outpatients on l-T4 replacement therapy (consumed within 1 h before breakfast) who switched from l-T4 tablets to l-T4 oral solution without changing the daily dose, showing that TSH level 60–90 days after the switch was significantly decreased [23]. However, in that study in the group of patients whose TSH dropped, it was observed an increased frequency of factors interfering with l-T4 absorption that are absent in our series of patients.
Another study was aimed to explore whether l-T4 liquid formulation (monodose vials or drops) affects TSH stability values and to assess its ability to maintain TSH within the normal range compared to tablets. A total of 100 hypothyroid patients on replacement treatment with l-T4 liquid solution were enrolled (Liquid Group) and the results were compared with those of 100 hypothyroid patients on replacement treatment with l-T4 tablets (Tablet Group). At the follow-up visit, 19 patients of the Tablet Group and 8 patients of the Liquid Group had abnormal TSH values. Weekly and daily l-T4 dosage per kilogram were higher in Tablet Group. This study suggested that the use of l-T4 liquid formulation is more effective to maintain the euthyroid state in hypothyroid patients [24]. However, no standardization of tablet treatment was reported in that study.
Interestingly, after the switch no patient has hypothyroid in our study. TSH values between 3 and 4 μIU/L that is not at optimal target were present in 12 % of patients at baseline, while only in 5 % at the first control and in 4 % at the second control, suggesting a better control of TSH by liquid formulation in these patients.
It has to be noticed also that the similar decline of TSH values both in patients affected by autoimmune thyroiditis as well as in the thyroidectomized patients suggests that the etiology of the hypothyroidism, per se, is not relevant to the final effect of the liquid formulation.
In conclusion, to the best of our knowledge, this is the first prospective study that shows that liquid l-T4 is more effective than l-T4 tablets in controlling TSH levels in hypothyroid patients without malabsorption, gastric disorders, or drug interference. Our results suggest that liquid l-T4 may overcome some absorption problems of l-T4 tablets when drug is taken half an hour before breakfast. A role of drug absorption directly in the oral mucosa by liquid l-T4 cannot be excluded. Other studies are needed to clarify these points.
References
J.R. Garber, R.H. Cobin, H. Gharib, J.V. Hennessey, I. Klein, J.I. Mechanick, R. Pessah-Pollack, P.A. Singer, K.A. Woeber, American Association of Clinical Endocrinologists and American Thyroid Association Taskforce on Hypothyroidism in Adults, Clinical practice guidelines for hypothyroidism for hypothyroidism in adults: cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Thyroid. 22, 1200–1235 (2012)
A. Antonelli, S.M. Ferrari, A. Corrado, A. Di Domenicantonio, P. Fallahi, Autoimmune thyroid disorders. Autoimmun. Rev. 14, 174–180 (2015)
S. Benvenga, L. Bartolone, S. Squadrito, F. Lo Giudice, F. Trimarchi, Delayed intestinal absorption of levothyroxine. Thyroid. 5, 249–253 (1995)
M. Centanni, L. Gargano, G. Canettieri, N. Viceconti, A. Franchi, G. Delle Fave, B. Annibale, Thyroxine in goiter, Helicobacter pylori infection, and chronic gastritis. N. Engl. J. Med. 354, 1787–1795 (2006)
S. Checchi, A. Montanaro, L. Pasqui, C. Ciuoli, V. De Palo, M.C. Chiappetta, F. Pacini, l-thyroxine requirement in patients with autoimmune hypothyroidism and parietal cell antibodies. J. Clin. Endocrinol. Metab. 93, 465–469 (2008)
S. Benvenga, When thyroid hormone replacement is ineffective? Curr. Opin. Endocrinol. Diabetes Obes. 20, 467–477 (2013)
P. Colucci, C. Seng Yue, M. Ducharme, S. Benvenga, A review of the pharmacokinetics of levothyroxine for the treatment of hypothyroidism. Eur. Endocrinol. 9, 40–47 (2013)
G. Barbesino, Drugs affecting thyroid function. Thyroid. 20, 763–770 (2010)
L. Liwanpo, J.M. Hershman, Conditions and drugs interfering with thyroxine absorption. Best. Pract. Res. Clin. Endocrinol. Metab. 23, 781–792 (2009)
M. Centanni, Thyroxine treatment: absorption, malabsorption, and novel therapeutic approaches. Endocrine 43, 8–9 (2013)
M.G. Santaguida, C. Virili, S.C. Del Duca, M. Cellini, I. Gatto, N. Brusca, C. De Vito, L. Gargano, M. Centanni, Thyroxine softgel capsule in patients with gastric-related T4 malabsorption. Endocrine 49, 51–57 (2015)
M. Cellini, M.G. Santaguida, I. Gatto, C. Virili, S.C. Del Duca, N. Brusca, S. Capriello, L. Gargano, M. Centanni, Systematic appraisal of lactose intolerance as cause of increased need for oral thyroxine. J. Clin. Endocrinol. Metab. 99, E1454–1458 (2014)
C. Virili, G. Bassotti, M.G. Santaguida, R. Iuorio, S.C. Del Duca, V. Mercuri, A. Picarelli, P. Gargiulo, L. Gargano, M. Centanni, Atypical celiac disease as cause of increased need for thyroxine: a systematic study. J. Clin. Endocrinol. Metab. 97, E419–E422 (2012)
I. Pirola, A.M. Formenti, E. Gandossi, F. Mittempergher, C. Casella, B. Agosti, C. Cappelli, Oral liquid l-thyroxine (l-T4) may be better absorbed compared to l-T4 tablets following bariatric surgery. Obes. Surg. 23, 1493–1496 (2013)
S. Benvenga, L. Bartolone, M.A. Pappalardo, A. Russo, D. Lapa, G. Giorgianni, G. Saraceno, F. Trimarchi, Altered intestinal absorption of l-thyroxine caused by coffee. Thyroid. 18, 293–301 (2008)
R. Vita, G. Saraceno, F. Trimarchi, S. Benvenga, A novel formulation of l-thyroxine (l-T4) reduces the problem of l-T4 malabsorption by coffee observed with traditional tablet formulations. Endocrine 43, 154–160 (2013)
R. Vita, P. Fallahi, A. Antonelli, S. Benvenga, The administration of l-thyroxine as soft gel capsule or liquid solution. Expert Opin. Drug Deliv. 11, 1103–1111 (2014)
A. Cassio, S. Monti, A. Rizzello, I. Bettocchi, F. Baronio, G. D’Addabbo, M.O. Bal, A. Balsamo, Comparison between liquid and tablet formulations of levothyroxine in the initial treatment of congenital hypothyroidism. J. Pediatr. 162, 1264–1269, 1269.e1–2 (2013)
M. Giusti, L. Mortara, N. Machello, E. Monti, G. Pera, M. Marenzana, Utility of a liquid formulation of levo-thyroxine in differentiated thyroid cancer patients. Drug. Res. (Stuttg) 65, 332–336 (2015)
I. Pirola, L. Daffini, E. Gandossi, D. Lombardi, A. Formenti, M. Castellano, C. Cappelli, Comparison between liquid and tablet levothyroxine formulations in patients treated through enteral feeding tube. J. Endocrinol. Invest. 37, 583–587 (2014)
K.M. Harper, E. Tunc-Ozcan, E.N. Graf, E.E. Redei, Intergenerational effects of prenatal ethanol on glucose tolerance and insulin response. Physiol. Genomics 46, 159–168 (2014)
E. Peroni, M.C. Vigone, S. Mora, L.A. Bassi, C. Pozzi, A. Passoni, G. Weber, Congenital hypothyroidism treatment in infants: a comparative study between liquid and tablet formulations of levothyroxine. Horm. Res. Paediatr. 81, 50–54 (2014)
D. Brancato, A. Scorsone, G. Saura, L. Ferrara, A. Di Noto, V. Aiello, M. Fleres, V. Provenzano, Comparison of TSH levels with liquid formulation versus tablet formulations of levothyroxine in the treatment of adult hypothyroidism. Endocr. Pract. 20, 657–662 (2014)
R. Negro, R. Valcavi, D. Agrimi, K.A. Toulis, Levothyroxine liquid solution versus tablet for replacement treatment in hypothyroid patients. Endocr. Pract. 20, 901–906 (2014)
American Thyroid Association (ATA) Guidelines Taskforce on Thyroid Nodules and Differentiated Thyroid Cancer, D.S. Cooper, G.M. Doherty, B.R. Haugen, R.T. Kloos, S.L. Lee, S.J. Mandel, E.L. Mazzaferri, B. McIver, F. Pacini, M. Schlumberger, S.I. Sherman, D.L. Steward, R.M. Tuttle, Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 19, 1167–1214 (2009)
R. Padwal, D. Brocks, A.M. Sharma, A systematic review of drug absorption following bariatric surgery and its theoretical implications. Obes. Rev. 11, 41–50 (2010)
Saraceno, G., Vita, R., Trimarchi, F., Benvenga, S.: A liquid formulation of l-thyroxine (l-T4) solves problems of incomplete normalization/suppression of serum TSH caused by proton pump inhibitors (PPI) on conventional tablet formulations of l-T4. in Presented at European Society of Endocrinology ICE/ECE, Florence, IT, 2012, p. 1626 (Abstract 29)
I. Walter-Sack, C. Clanget, R. Ding, C. Goeggelmann, V. Hinke, M. Lang, J. Pfeilschifter, Y. Tayrouz, K. Wegscheider, Assessment of levothyroxine sodium bioavailability: recommendations for an improved methodology based on the pooled analysis of eight identically designed trials with 396 drug exposures. Clin. Pharmacokinet. 43, 1037–1053 (2004)
R. Koytchev, R. Lauschner, Bioequivalence study of levothyroxine tablets compared to reference tablets and an oral solution. Arzneimittelforschung 54, 680–684 (2004)
N. Yannovits, E. Zintzaras, A. Pouli, G. Koukoulis, S. Lyberi, E. Savari, S. Potamianos, F. Triposkiadis, I. Stefanidis, E. Zartaloudis, A. Benakis, A bioequivalence study of levothyroxine tablets versus an oral levothyroxine solution in healthy volunteers. Eur. J. Drug Metab. Pharmacokinet. 31, 73–78 (2006)
C.S. Yue, C. Scarsi, M.P. Ducharme, Pharmacokinetics and potential advantages of a new oral solution of levothyroxine vs. other available dosage forms. Arzneimittelforschung 62, 631–636 (2012)
H. Zhang, J. Zhang, J.B. Streisand, Oral mucosal drug delivery: clinical pharmacokinetics and therapeutic applications. Clin. Pharmacokinet. 41, 661–680 (2002)
Funding
The authors have nothing to declare.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in this study.
Rights and permissions
About this article
Cite this article
Fallahi, P., Ferrari, S.M. & Antonelli, A. Oral l-thyroxine liquid versus tablet in patients with hypothyroidism without malabsorption: a prospective study. Endocrine 52, 597–601 (2016). https://doi.org/10.1007/s12020-015-0836-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12020-015-0836-y