Abstract
Many studies focused on the association between thyroid disease and pregnancy outcomes. The present study explored the effect of iodine nutrition during the first trimester on pregnancy outcomes. One thousand five hundred sixty-nine pregnant, euthyroid women at ≤12 weeks of gestation in an iodine-sufficient area in China were recruited. According to the World Health Organization (WHO) criteria for iodine nutrition during pregnancy, participants were divided into four groups: adequate iodine (median urinary iodine concentration (UIC), 150–249 μg/L), mild deficiency (UIC, 100–150 μg/L), moderate and severe deficiency (UIC, <100 μg/L), and more than adequate and excessive (UIC, ≥250 μg/L) groups. Pregnancy outcomes, including abortion, gestational hypertension, pre-eclampsia, gestational diabetes mellitus (GDM), placenta previa, placental abruption, preterm labor, low birth weight infants, macrosomia, breech presentation, and cord entanglement, were obtained during follow-up. The results showed that there was no significant difference in general characteristics, including age, body mass index, abdominal circumference, systolic blood pressure, diastolic blood pressure, heart rate, smoking rate, and drinking rate, among the four groups. In the more than adequate and excessive group, thyroid-stimulating hormone (TSH) was greater and free thyroxine (FT4) was lower than any other groups but still within normal range. The thyroglobulin (Tg) level was greater in the moderate and severe deficiency group. The incidence of GDM was significantly greater in women with mild iodine deficiency than in women with adequate iodine nutriture (18.38 vs. 13.70%, p < 0.05). Compared with the adequate group, incidence of macrosomia was significantly greater in the more than adequate and excessive group (12.42 vs. 9.79%, p < 0.05). Mild iodine deficiency was an independent risk factor for GDM (odds ratio = 1.566, 95% confidence interval = 1.060–2.313, p = 0.024); more than adequate and excessive iodine was an independent risk factor for macrosomia (OR = 1.917, CI = 1.128–3.256, p = 0.016). In summary, during 1st trimester, both mild iodine deficiency and excessive iodine intake had adverse impacts on pregnancy outcomes in an iodine-sufficient area.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The iodine status of pregnant women is important for fetal growth and development, as maternal iodine is the only source of iodine for fetal thyroid hormone synthesis. Pregnant women are susceptible to iodine deficiency (ID) due to increased renal clearance and additional fetal requirements. Insufficient maternal iodine intake is associated with poor pregnancy outcomes, such as abortion, low birth weight infants, and impaired fetal growth. Considering the adverse effects of iodine deficiency, the World Health Organization (WHO) recommends a daily dosage of 250 μg of iodine for pregnant women [1]. Iodine deficiency disorders (IDD) can be partially reversible by iodine repletion.
The Chinese government has implemented a universal salt iodization (USI) policy since 1996. In the past two decades, China has almost eradicated IDD, and the iodine status of the population is adequate; the median urinary iodine concentration (UIC) is 239 μg/L (according to the Iodine Global Network, http://www.ign.org/index.cfm). Although severe ID in pregnant women is no longer a problem in China, maternal ID has persisted, especially mild-to-moderate ID. According to the WHO standard of sufficient iodine status during pregnancy, the proportion of iodine insufficiency (UIC <150 μg/L) in pregnant Chinese women is approximately 50% [2]. Meanwhile, iodine excess has attracted public concern due to its association with an increased prevalence of thyroid diseases. The potential hazards of excessive iodine intake during early pregnancy have not been adequately studied. We designed a cohort study to explore the association of maternal iodine status with pregnancy outcomes in an iodine-sufficient area. We used UIC as a biochemical marker to assess iodine nutrition in pregnant women. This article provides evidence to understand the importance of iodine status in pregnancy outcomes.
Methods and Materials
Subjects
A study on subclinical hypothyroidism in early pregnancy (SHEP) was conducted from 2012 to 2014 in Liaoning Province, which is an iodine-sufficient area in China. A total of 1569 euthyroid and primapara women in the SHEP study were recruited to participate in this prospective cohort study. Recruitment criteria included women aged 18–45 years with a singleton pregnancy at 4–12 weeks of gestation and residence in the city for more than 10 years. Women with a history of thyroid disease or other chronic diseases were excluded.
Methods
Spot-urine and blood specimens were collected from each subject in the morning after all-night fasting. UICs were measured using the ammonium persulfate method based on the Sandell-Kolthoff reaction. Intra- and inter-assay coefficients of variation (CV) were 3–4 and 4–6% at 66 μg/L, respectively, and 2–5 and 3–6% at 230 μg/L, respectively. The median week of gestation when spot urine was obtained at 7. The subjects were divided into four groups according to the WHO criteria for assessing iodine nutrition during pregnancy: UIC 150–249 μg/L (iodine adequate, N = 562); UIC 100–149 μg/L (mild iodine deficiency, N = 419); UIC <100 μg/L (moderate-to-severe iodine deficiency, N = 247); and UIC ≥250 μg/L (more than adequate-to-excessive iodine, N = 314) [1].
Concentrations of serum TSH, free T4 (FT4), thyroglobulin (Tg), thyroperoxidase antibody (TPOAb), and thyroglobulin antibody (TgAb) levels were determined using the electrochemiluminescence immunoassay method. The intra- and inter-assay CV values of serum TSH, FT4, TPOAb, TgAb, and Tg were based on a previous study [2].
Defining Thyroid Dysfunction
Pregnant trimester-specific reference ranges of TSH and FT4 were based on the National Academy of Clinical Biochemistry (NACB) standards. During the first trimester, the reference range of TSH was 0.21–4.8 mIU/L and FT4 was 12.79–20.22 pmol/L. According to the diagnostic criteria, we excluded pregnant women with thyroid disorders including overt hypothyroidism, TSH >4.8 mIU/L and FT4 < 12.79 pmol/L, subclinical hypothyroidism, TSH >4.8 mIU/L with normal FT4, isolated hypothyroxinemia, FT4 < 12.79 pmol/L with normal TSH, negative TPOAb and TgAb, and positive TPOAb >100 IU/mL. Individuals with thyroid diseases were excluded to eliminate the effects of thyroid hormone and antibodies on pregnancy outcomes.
Pregnancy Outcomes
Pregnancy outcomes were recorded during telephone follow-up by two fixed persons. Maternal outcomes included abortion, gestational hypertension, pre-eclampsia, gestational diabetes mellitus (GDM), placenta previa, and placental abruption. Neonatal outcomes included preterm labor, birth weight, low birth weight infants, macrosomia, breech presentation, and cord entanglement. Pregnancy outcomes were managed by obstetricians. The diagnostic criteria are shown in Table 1.
Statistical Analysis
Data analysis was performed using SPSS (version 21.0, SPSS Inc., Chicago, IL, USA). A value of p < 0.05 was considered significant.
Ethics Committee Approval
The Ethics Committee of China Medical University approved this experimental procedure (2011–32-4), and the experiments adhered to guidelines established by the Declaration of Helsinki. All participants signed informed consent.
Results
Characteristics of Subjects
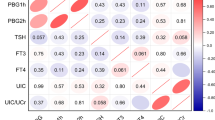
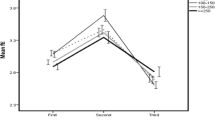
Table 2 shows the laboratory tests and general characteristics of the different groups of women by UIC. The data collected for subjects failed the normality test. Consequently, parameters were compared among four groups with the Kruskal-Wallis test, and pairwise comparisons were assessed using the Mann-Whitney test. No differences were found in age, body mass index (BMI), abdominal circumference (AC), systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate, smoking rate, and drinking rate among the four groups. Thyroid function of all subjects was within pregnancy-specific reference ranges. The greatest concentration of TSH and the least concentration of FT4 was observed in the group with UIC ≥250 μg/L. The Tg level was remarkably greater in the group with UIC <100 μg/L than both UIC 150–249 μg/L group and UIC 100–149 μg/L group (both p<0.05); additionally, the relationship between UIC and Tg corresponded to a U-shaped curve. No difference was found in TPOAb, TgAb values or TgAb- positive percentage in different groups based on UIC. The Wolff -Chaikoff effect was initiated to avoid iodine-induced hyperthyroidism when the iodine concentration increased [4]. The median UIC value of 159.59 μg/L (average, 188.95 μg/L) suggested that subjects in the cohort had a sufficient iodine status during their first trimester.
Prevalence of Pregnancy Outcomes
Table 3 shows the prevalence of pregnancy outcomes according to iodine status. Chi-square test was used to compare the prevalence of pregnancy outcomes in different groups. Compared with the women in the UIC 150–249 μg/L group, the prevalence of GDM among the women in the UIC 100–149 μg/L group was greater (13.70 vs. 18.38%; p = 0.046). Prevalence of placental abruption was considerably greater among the women in the UIC <100 μg/L group than in those women in the UIC 150–249 μg/L group (1.09 vs. 0%; p = 0.035). Nevertheless, placental abruption cases were rare due to the low morbidity rate. Compared with the newborns in the UIC 150–249 μg/L group, birth weight in the UIC ≥250 μg/L group was significantly increased (1756 ± 252 vs. 1710 ± 257; p = 0.010) by means of the Kruskal-Wallis test. No significant difference was found in 1-min Apgar score among four groups. Although there was no difference, the prevalence of macrosomia was greater among the women in the UIC ≥250 μg/L group than those in the UIC 150–249 μg/L group.
Multivariate Statistical Analysis
To further assess the confounding factors, a multiple logistic regression analysis was used to evaluate risk factors for pregnancy outcomes and complications. Mild iodine deficiency among women with UIC 100–149 μg/L acted as a risk factor for GDM (adjusted by age, BMI, SBP, DBP, TSH, FT4, TPOAb, TgAb, Tg, and smoking), and the odds ratio (OR) was 1.67. Additionally, women in the more than adequate-to-excessive iodine group (UIC ≥250 μg/L) had a 2.12-fold increased risk of macrosomia (adjusted by age, BMI, SBP, DBP, GDM, TSH, FT4, TPOAb, TgAb, Tg, and smoking) than those in the adequate iodine group (Table 4). None of the groups of women in the different iodine status levels had a risk factor for placental abruption (data not shown).
Discussion
Most studies of the effects of iodine nutrition on pregnancy outcomes were implemented in iodine-deficient areas. Cumulatively, severe iodine deficiency is related to maternal and fetal hypothyroidism and neurological impairment of the fetus [5]. However, little is known about the effects of mild iodine deficiency and iodine excess on pregnancy outcomes, which have become urgent issues because these conditions are now prevalent. The present study explored the correlations between iodine status and pregnancy outcomes in an iodine-sufficient region. After adjusting for possible confounding variables, mild iodine deficiency during the first trimester was associated with an elevated risk of GDM. Simultaneously, more than adequate-to-excessive iodine intake was linked to an increased risk of macrosomia.
For the first time, we report that pregnant women with mild iodine deficiency have a higher risk of GDM. We noted that the prevalence of GDM in recent years increased in different regions in China (16.8% in Shenyang, 11.63 to 31.63% in Guangzhou, and 24.7% in Qingdao) [6,7,8]. These articles did not discuss the local maternal iodine status due to the lack of UIC data. The accepted risk factors for GDM include age, overweight status or obesity, family history of diabetes, and a history of abnormal delivery [9]. Chen et al. demonstrated insulin resistance and β cell function were inversely correlated with TSH [10]. As TSH increased, thyroid hormones decreased and insulin antagonistic effect was weakened. Al-Attas et al. examined UIC in type 2 diabetes mellitus (T2DM) patients and found that the UIC was markedly lower in T2DM than in the healthy control group (84.6 ± 2.3 μg/L vs. 119.4 ± 3.4 μg/L, p < 0.001), but neither TSH nor thyroxine (T3) was significantly different between the two groups [11]. The role of iodine in the development of diabetes may involve other mechanisms apart from decreasing thyroid hormones. Hyperglycemia is associated with increased oxidative stress and decreased antioxidant status. Kurku et al. found that children with moderate iodine deficiency were exposed to more oxidative burden than children with mild iodine deficiency or iodine sufficiency [12]. Iodine could act directly as an antioxidant or induce indirectly antioxidative enzymes [13]. To sum up, we speculated that the underlying mechanism of iodine in GDM was mediated by an imbalance between antioxidant and oxidation systems. A well-designed trial to study the effect of iodine nutrition on GDM with adjusted confounding factors is warranted in the future.
A prospective cohort study in Bangladesh found that a maternal UIC up to 1.0 mg/L in early pregnancy was positively associated with birth weight, length, and head circumference in male newborns. The median UIC obtained at 8 weeks gestation from 1617 women was 300 μg/L. For male fetuses, a 0.5-mg/L increase in maternal UIC corresponded with an increase in fetal birth weight, body length, and head circumference of 70 g (p = 0.019), 0.41 cm (p = 0.013), and 0.28 cm (p = 0.031), respectively [14]. Unfortunately, this study did not measure maternal thyroid function, although the authors speculated that most participants might maintain normal thyroid function during the study. Another Spanish prospective cohort study showed an inverse association of FT4 concentration during the first half of pregnancy with birth weight. However, maternal UIC (median UIC, 128 μg/L; N = 1908) was not related to birth weight, small or large size for gestational age (SGA/LGA), or preterm labor [15]. In our study, the prevalence of macrosomia was significantly greater in the UIC ≥250 μg/L group; additionally, the UIC ≥250 μg/L group had the lowest FT4 level. These data suggested a positive correlation between maternal iodine status and birth weight. The relationship between UIC and birthweight warrants additional research to resolve this conflict.
Researchers in Pakistan performed a study to investigate the effect of maternal iodine supplementation on pregnancy outcomes in goiter endemic areas. Pregnant women were enrolled in this investigation at 6–8 weeks of gestation. The authors reported three still births, two spontaneous abortions, and one case of cretinism in the women with severe iodine deficiency (median UIC, 63–64 μg/L; N = 154) and one still birth in the women with mild iodine deficiency (median UIC, 102 μg/L; N = 156). In the women with severe iodine deficiency in the iodine supplement group (N = 150), none of the adverse outcomes mentioned above were reported [16]. In our study, we observed that an increased prevalence of abortion, placenta previa, placental abruption, and low birth weight occurred among the women in the UIC <100 μg/L group (median UIC, 79.21 μg/L; N = 274); however, these results were not significant. If we included moderate-to-severe iodine deficiency group, we might obtain significantly different results.
Previous studies had drawn controversial conclusions regarding the relationship between thyroid function and blood pressure. A study in the Netherlands found that both hyperthyroidism and high-normal FT4 levels during early pregnancy (mean 13.5 weeks) were risk factors for hypertensive disorders. Hyperthyroidism is associated with an increased risk of pregnancy-induced hypertension (OR, 4.18; 95% CI, 1.57–11.1; p = 0.004). High-normal FT4 levels are associated with an increased risk of pre-eclampsia (OR, 2.06; 95% CI, 1.04–4.08; p = 0.04). The median UIC was 221 μg/L (N = 5153), indicating an iodine-sufficient status of pregnant women [17]. In contrast, a retrospective cohort study in the USA including 223,512 pregnant women indicated that both hyper- and hypothyroidism increased the risk of pre-eclampsia [18]. In our study, although the FT4 level increased in the UIC 150–249 μg/L group, we did not observe an increased prevalence of hypertensive disorders. Because no acknowledged standard exists for pregnancy-specific thyroid parameters, normal reference ranges were variable among the different studies.
The underlying mechanism of the adverse effects of iodine on pregnancy is still unclear. Maternal micronutrients may interfere with pregnancy outcomes by regulating oxidative stress, enzyme function, signal transduction, and transcriptional activity, especially during conception, implantation, placentation, and the embryogenesis period of early pregnancy [19]. Moreover, iodine mainly influences pregnancy outcomes through the thyroid axis, which is driven by the thyroid hormone. In our study, thyroid function of all recruited women was within the normal range. Most pregnant women in iodine-sufficient areas have sufficient iodine reserves, which might sustain thyroid hormone synthesis during the entire pregnancy. A slight variation in thyroid function within the normal range may lead to adverse pregnancy outcomes. Additionally, the placenta has a self-regulatory mechanism to accommodate changes in the extra uterine iodine status and in thyroid hormone levels, such as regulating the expression of sodium iodide symporter (NIS), iodothyronine deiodinase, and thyroid hormone receptor, to prevent dramatic fluctuations in thyroid hormone levels [20].
There are several limitations in the current study. First, we used UICs from spot-urine samples to assess the iodine nutrition in pregnant women. UIC is not considered a suitable marker to assess individual iodine excretion due to variations in urine output and iodine intake. Moreover, we did not find any deleterious effects of severe iodine deficiency on pregnancy outcomes. The number of subjects in the UIC <100 μg/L group was likely insufficient; thus, we should increase the size of the study population. Another limitation was that subsequent iodine status of all participants in the second and third trimesters was unknown. Selenium (Se) status has been associated with adverse pregnancy outcomes [21]. In our previous investigations, these areas were sufficient in Se (unpublished data), so we did not measure serum Se in all pregnant women. Finally, these results were based on an observational study. Randomized controlled trials (RCTs) are required to find out whether the negative effects of iodine deficiency and iodine excess on pregnancy outcomes can be prevented by appropriate iodine intake before conception. The ongoing SHEP Phase II Study, a prospective RCT, has enrolled more than 5000 females of childbearing age before conception in iodine-sufficient areas. We expect that this large RCT will address these issues in the future.
Our study emphasized the importance of optimal iodine status during early pregnancy. Despite the above limitations, iodine deficiency and iodine excess have deleterious effects on pregnancy outcomes. Clearly, iodine prophylaxis programs need to be carefully monitored for both iodine deficiency and excess. In iodine-deficient areas, USI policy should be implemented to alleviate mild-to-moderate deficiency in pregnant females. Iodine supplements should be given to pregnant women as early as possible to ensure successful pregnancy outcomes. Pregnancy-specific guidelines for daily iodine intake should be established according to local iodine status. More scientific evidence is needed to provide optimal and safe upper limit of iodine intake for pregnant women.
References
Andersson M, de Benoist B, Delange F, Zupan J (2007) Prevention and control of iodine deficiency in pregnant and lactating women and in children less than 2-years-old: conclusions and recommendations of the technical consultation. Public Health Nutr 10(12A):1606–1611. doi:10.1017/s1368980007361004
Shi X, Han C, Li C, Mao J, Wang W, Xie X, Li C, Xu B, Meng T, Du J, Zhang S, Gao Z, Zhang X, Fan C, Shan Z, Teng W (2015) Optimal and safe upper limits of iodine intake for early pregnancy in iodine-sufficient regions: a cross-sectional study of 7190 pregnant women in China. J Clin Endocrinol Metab 100(4):1630–1638. doi:10.1210/jc.2014-3704
Xie X, Gou W (2013) The eighth edition of obstetrics and gynecology. People’s Medical Publishing House (article in Chinese)
Wolff J, Chaikoff IL (1948) Plasma inorganic iodide as a homeostatic regulator of thyroid function. J Biol Chem 174(2):555–564
Zimmermann MB (2012) The effects of iodine deficiency in pregnancy and infancy. Paediatr Perinat Epidemiol 26(Suppl 1):108–117. doi:10.1111/j.1365-3016.2012.01275.x
Yu J, Luan H, Li Y (2013) Gestational diabetes mellitus status in Shenyang. Chin Pract J Rural Dr(article In Chinese) 21:27–28
Hao B, Shen J, Wan H, Lv M, Li Y, Li J et al (2014) A retrospective survey of the incidence of gestational diabetes mellitus in Guangzhou Tianhe district. Chinese Journal of Diabetes (article in Chinese) 22(7):620–621
Cui Z, Cui X, Xu J (2016) Incidence and clinical data analysis of gestational diabetes mellitus in Qingdao area. Chinese Journal of Woman and Child Health Research (article in Chinese) 27(3):348–351
Yang H, Wei Y, Gao X, Xu X, Fan L, He J, Hu Y, Liu X, Chen X, Yang Z, Zhang C (2009) Risk factors for gestational diabetes mellitus in Chinese women: a prospective study of 16,286 pregnant women in China. Diabetic Medicine: a Journal of the British Diabetic Association 26(11):1099–1104. doi:10.1111/j.1464-5491.2009.02845.x
Chen G, Wu J, Lin Y, Huang B, Yao J, Jiang Q, Wen J, Lin L (2010) Associations between cardiovascular risk, insulin resistance, beta-cell function and thyroid dysfunction: a cross-sectional study in She ethnic minority group of Fujian Province in China. Eur J Endocrinol 163(5):775–782. doi:10.1530/EJE-10-0710
Al-Attas OS, Al-Daghri NM, Alkharfy KM, Alokail MS, Al-Johani NJ, Abd-Alrahman SH, Yakout SM, Draz HM, Sabico S (2012) Urinary iodine is associated with insulin resistance in subjects with diabetes mellitus type 2. Exp Clin Endocrinol Diabetes 120(10):618–622. doi:10.1055/s-0032-1323816
Kurku H, Gencer A, Pirgon O, Buyukinan M, Aslan N (2016) Increased oxidative stress parameters in children with moderate iodine deficiency. J Pediatr Endocrinol Metab 29(10):1159–1164. doi:10.1515/jpem-2016-0077
Moser M, Buchberger W, Mayer H, Winkler R (1991) Influence of an iodine-drinking cure on the antioxidative status of diabetic patients. Wien Klin Wochenschr 103(6):183–186
Rydbeck F, Rahman A, Grander M, Ekstrom EC, Vahter M, Kippler M (2014) Maternal urinary iodine concentration up to 1.0 mg/L is positively associated with birth weight, length, and head circumference of male offspring. J Nutr 144(9):1438–1444. doi:10.3945/jn.114.193029
Leon G, Murcia M, Rebagliato M, Alvarez-Pedrerol M, Castilla AM, Basterrechea M, Iniguez C, Fernandez-Somoano A, Blarduni E, Foradada CM, Tardon A, Vioque J (2015) Maternal thyroid dysfunction during gestation, preterm delivery, and birthweight. The Infancia y Medio Ambiente cohort. Spain Paediatric and Perinatal Epidemiology 29(2):113–122. doi:10.1111/ppe.12172
Anees M, Anis RA, Yousaf S, Murtaza I, Sultan A, Arslan M, Shahab M (2015) Effect of maternal iodine supplementation on thyroid function and birth outcome in goiter endemic areas. Curr Med Res Opin 31(4):667–674. doi:10.1185/03007995.2015.1011779
Medici M, Korevaar TI, Schalekamp-Timmermans S, Gaillard R, de Rijke YB, Visser WE, Visser W, de Muinck Keizer-Schrama SM, Hofman A, Hooijkaas H, Bongers-Schokking JJ, Tiemeier H, Jaddoe VW, Visser TJ, Peeters RP, Steegers EA (2014) Maternal early-pregnancy thyroid function is associated with subsequent hypertensive disorders of pregnancy: the generation R study. J Clin Endocrinol Metab 99(12):E2591–E2598. doi:10.1210/jc.2014-1505
Mannisto T, Mendola P, Grewal J, Xie Y, Chen Z, Laughon SK (2013) Thyroid diseases and adverse pregnancy outcomes in a contemporary US cohort. J Clin Endocrinol Metab 98(7):2725–2733. doi:10.1210/jc.2012-4233
Ramakrishnan U, Grant F, Goldenberg T, Zongrone A, Martorell R (2012) Effect of women's nutrition before and during early pregnancy on maternal and infant outcomes: a systematic review. Paediatr Perinat Epidemiol 26(Suppl 1):285–301. doi:10.1111/j.1365-3016.2012.01281.x
Akturk M, Oruc AS, Danisman N, Erkek S, Buyukkagnici U, Unlu E, Tazebay UH (2013) Na+/I- symporter and type 3 iodothyronine deiodinase gene expression in amniotic membrane and placenta and its relationship to maternal thyroid hormones. Biol Trace Elem Res 154(3):338–344. doi:10.1007/s12011-013-9748-y
Rayman MP (2012) Selenium and human health. Lancet 379(9822):1256–1268
Acknowledgments
We gratefully acknowledged the residents who participated in this study. The study was supported by the National Science and Technology Support Program (grant number 2014BAI06B02); Chinese National Natural Science Foundation (grant numbers 81170730 and 81570709); Research Foundation of Key Laboratory of Endocrine Diseases, Department of Education in Liaoning Province of China (grant number LZ2014035); and Key Platform Foundation of Science and Technology for the Universities in Liaoning Province of China (grant number 16010).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Xiao, Y., Sun, H., Li, C. et al. Effect of Iodine Nutrition on Pregnancy Outcomes in an Iodine-Sufficient Area in China. Biol Trace Elem Res 182, 231–237 (2018). https://doi.org/10.1007/s12011-017-1101-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-017-1101-4