Abstract
Iodine is essential for the production of thyroid hormones, and its deficiency during pregnancy may be associated with poor obstetric outcomes. The aim of this study was to investigate the relationship between maternal iodine statuses with pregnancy outcomes among pregnant Iranian women, considering their baseline thyrotropin (TSH) status. We used data from the Tehran Thyroid and Pregnancy Study (TTPS), a two-phase population-based study carried out among pregnant women receiving prenatal care. By excluding participants with overt thyroid dysfunction and those receiving levothyroxine, the remaining participants (n = 1286) were categorized into four groups, according to their urine iodine status: group 1, urine iodine concentration (UIC) < 100 μg/L; group 2, UIC between 100 and 150 μg/L; group 3, UIC between 150 and 250 μg/L; and group 4, UIC ≥ 250 μg/L. Primary outcome was preterm delivery. Preterm delivery occurred in 29 (9%), 19 (7%), 15 (5%), and 8 (4%) women, and neonatal admission was documented in 22 (7%), 30 (12%), 28 (11%), and 6 (3%) women of groups 1, 2, 3, and 4, respectively. Generalized linear regression model (GLM) demonstrated that the odds ratio of preterm delivery was significantly higher in women with urinary iodine < 100 μg/L and TSH ≥ 4 μIU/mL than those with similar urinary iodine with TSH < 4 μIU/mL (OR 2.5 [95% CI 1.1, 10], p = 0.024). Adverse pregnancy outcomes are increased among women with UIC < 100 μg/L, with serum TSH concentrations ≥ 4 μIU/mL.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Iodine, an essential trace element for synthesis of thyroid hormones, plays a vital role in early growth and development of most organs, especially in the central nervous and reproductive systems [1,2,3]. A active transportation of iodine from the blood into the thyroid is regulated by the thyroid-stimulating hormone (TSH) from the pituitary gland and by the concentration of iodine in the blood [4]. Iodine status may influence growth through its effects on the thyroid axis [5,6,7], and both iodine deficiency and its excess affect thyroid hormones. Sufficient maternal iodine is required for the production of thyroid hormones for the normal development of the fetus and the neonate [8].
The need for iodine in pregnancy is increased [9] due to an increase in maternal thyroxin production to maintain maternal euthyroidism and for transfer of thyroid hormones to the fetus in early pregnancy, before the fetal thyroid begins functioning [10]. Also, maternal glomerular filtration rate (GFR) is increased during pregnancy resulting in increased renal loss of ingested iodine [11]. Adequate iodine consumption is essential for production of thyroid hormones and prevention of any possible feto-maternal complications [1, 12]. Women with iodine deficiency may start pregnancy with inadequate intrathyroidal iodine stores that cannot meet the increasing demands of pregnancy [13,14,15], and this unmet need for iodine leads to pathological changes that may adversely affect maternal and fetal health [16]. Even mild-to-moderate iodine deficiency during pregnancy can cause maternal and fetal hypothyroidism, resulting in adverse feto-maternal and neonatal effects [4, 16,17,18]. Severe iodine deficiency in pregnant women has been associated with serious adverse health effects, including cretinism and growth retardation and impaired neurological development of the fetus and increased rates of pregnancy loss, stillbirth, and perinatal, neonatal, and infant mortality [14, 19, 20].
Iodine deficiency is one of the most prevalent disorders, especially during pregnancy [17, 18]. Severe maternal iodine deficiency may be associated with both maternal and fetal hypothyroidism and with adverse pregnancy outcomes, including spontaneous abortion, congenital anomalies, growth retardation, stillbirth and perinatal mortality, recurrent miscarriage, preterm delivery, and perinatal and infant mortality; significant improvements however have been documented observed with iodine supplementation [16,17,18, 21,22,23,24]. Potential adverse effects of severe iodine deficiency in pregnancy are believed to be due to alteration of maternal thyroid function and possibly fetal thyroid function as well, since iodine is an essential component of thyroid hormones [19, 25].
Following implementation of universal salt iodization in 1989, the Islamic Republic of Iran was declared to be a country free of iodine deficiency disorders (IDD) [26]. Despite consumption of iodized salt in Iran, studies conducted in 2013 showed inadequate iodine nutrition both in pregnant and in non-pregnant women in Tehran [27, 28]. Given the lack of sufficient data regarding the impact of mild-to-moderate iodine deficiency on pregnancy outcomes, we aimed to investigate the relationship of maternal iodine and TSH status with pregnancy outcomes in these women.
Materials and Methods
Study Design and Participants
We used data from the Tehran Thyroid and Pregnancy Study, a two-phase population-based study, conducted from September 2013 through February 2016. Details of the study protocol have previously been published [29]. Using a cluster sampling method, a total of 1671 pregnant women in their first trimester were selected (calculated by the date of last menstrual period or sonography), from among those receiving prenatal care in centers under coverage of Shahid Beheshti University of Medical Sciences, which provides health services to over two-thirds of Tehran’s population.
After obtaining a written informed consent from participants, a comprehensive questionnaire including demographic, reproductive, medical, and prenatal histories was completed during face-to-face interviews. Fasting blood samples were collected for thyroid hormonal assessment including thyroxine (T4), Resin T-uptake (RTU), thyrotropin (TSH), and thyroid peroxidase antibody (TPOAb) to determine the thyroid status of participants. Two additional fasting blood samples were collected in the second (20–24 weeks of gestation) and third (30–34 weeks of gestation) trimesters. Following centrifugation, samples were stored at − 80 °C till the end of the study to measure serum levels of TSH, T4, and RTU.
Women with subclinical hypothyroidism (TPO-Ab+ or TPO-Ab−) were invited for the second phase of the study and randomly assigned into two groups (treated with levothyroxine (LT4) and without treatment). Euthyroid TPOAb− women served as the healthy controls and were followed till delivery. Pregnancy outcomes in terms of height, weight, and head circumference of newborns, neonatal TSH levels and preterm delivery, placenta abruption, stillbirth, and neonatal admission were compared between groups.
For the purpose of the present study, pregnant women with twin pregnancies (n = 21), those with overt thyroid dysfunction (hyperthyroidism or hypothyroidism) (n = 78), and those who had used levothyroxine during pregnancy (previous consumers or those selected as interventional group in the second phase of the study) or those using iodine-containing supplement (n = 286) were excluded; finally, a total of 1286 pregnant women were included in the present study; none of whom consumed iodine-containing supplement during pregnancy.
Since the World Health Organization (WHO) recommends analysis of urinary iodine concentration (UIC) on spot urine samples for assessment of iodine status of a population [23], at the first prenatal visit, participants were asked to collect three casual morning urine samples (5–10 mL) on an every other day basis for measurement of UIC. Spot urine samples were collected and stored at − 20 °C. The levels of serum hormones and urinary iodine were measured at the Research Institute of Endocrine Sciences of the Shahid Beheshti University of Medical Sciences. Urinary iodine was measured in three urine samples to obtain the median. Pregnant women were divided into four groups according to urine iodine status, and pregnancy outcomes were compared between groups.
The study was approved by the ethics committee of the Research Institute of Endocrine Sciences (RIES), approval no: IR.SBMU.ENDOCRINE.REC.1397.273.
Outcomes
In this study, the primary outcome was preterm delivery and secondary outcomes were height, weight, and head circumference of newborns, neonatal TSH levels, placental abruption, stillbirth, and neonatal admission.
Laboratory Determination
T4 was measured by radioimmunoassay (RIA) using commercial kits (Izotop Kit, Budapest Co, Hungary) and TSH was measured by the immunoradiometric assay (IRMA) using the gamma counter (Dream Gamma-10, Goyang-si, Gyeonggi-do, South Korea). TPOAb and RTU were measured by the immunoenzymometric assay (IEMA) (Monobind Kit, Costa Mesa, CA, USA) and enzyme immunoassay (EIA) (DiaPlus Kit, San Francisco, CA, USA), respectively, using a calibrated ELISA reader (Sunrise, Tecan Co., Salzburg, Austria). Intra- and inter-assay coefficients of variation (CVs) for T4, TSH, RTU, and TPOAb were 1.1% and 3.9%, 1.9% and 4.7%, 2.2% and 4.3%, and 1.0% and 1.6%, respectively. Since free T4 immunoassays may be affected by changes of serum thyroxine-binding globulin and albumin during pregnancy, Free Thyroxine Index (FT4I) was used [30].
UIC was determined using a manual method, based on the Sandell–Kolthoff technique [23]. The intra-assay CVs in three ranges of 3.4, 12.5, and 37.1 μg/L were 8.5, 7.2, and 9.6%, respectively, and inter-assay CV percentages were 9.1, 8.6, and 12.3%, respectively.
Definition of Terms
Overt hyperthyroidism was defined as TSH levels < 0.1 μIU/mL and FT4I > 4.5. Overt hypothyroidism was defined as TSH > 10 μIU/mL or TSH levels > 2.5 μIU/mL and FT4I < 1.
Subclinical hypothyroidism was defined by a normal FT4I (1–4.5), despite elevated TSH (4–10 mIU/L). TPOAb > 50 IU/mL was considered to be TPOAb positivity.
Group 1 included pregnant women with UIC < 100 μg/L; group 2, UIC 100–150 μg/L; group 3, UIC 150–250 μg/L; and group 4, UIC ≥ 250 μg/L.
Preterm delivery was defined as babies born alive before 37 weeks of pregnancy [31]; placental abruption was defined as the placenta separation from the wall of the uterus, prior to the birth of the baby, and was diagnosed by clinical or histological findings [32]. Fetal death or stillbirth was defined as a baby born with no signs of life after a given threshold (20 weeks gestation) [33]; newborn admission was defined as the admission of a newborn to the neonatal unit, mainly due to icterus or fetal distress.
Sample Size
The sample size is calculated using the following formula:\( {n}_i=2{\left(\frac{z_{1-\frac{\alpha }{2}}+{z}_{1-\beta }}{Es}\right)}^2 \); α = 0.05 is assumed and the test power is considered to be 1 − β = 0.8; the effect size is calculated as follows: \( Es=\frac{\mid {P}_1-{P}_2\mid }{\sqrt{P\left(1-P\right)}} \) and \( P=\frac{P_1+{P}_2}{2} \). P1 and P2 are the proportion of individuals in each group that is expected to produce the desired outcome, and P is the overall proportion.
In this study, a 40% increase in the outcome ratio of iodine deficient individuals is clinically meaningful; hence, with a sample size of 543 people in each group and with a power of 80%, this difference can be identified in groups (mothers with different iodine statuses).
Statistical Analysis
Post hoc power calculation indicated that with at least a 240-sample size for each subgroup of UIC, this study had a 96% power to determine a 1.5% difference in the prevalence of our primary outcome (preterm labor) among pregnant women, of the four UIC categories.
Normality assumption was checked via the Kolmogorov–Smirnov and Shapiro–Wilk tests. Continuously distributed variables are reported as mean ± standard deviation for the normal and median (IQR) for the non-normal variables. ANOVA and Kruskal–Wallis tests were applied to detect significant differences in normally and non-normally distributed variables. Post hoc analysis was applied to make pairwise comparisons using the Dunn–Bonferroni and Tukey tests. Categorical variables are reported as N% of positive events and were tested using the chi-squared test.
Generalized linear regression model (GLM) via logit and linear link function for binary outcomes (preterm delivery and newborn admission) and continuous outcomes (head circumference, weight, and height) were applied to estimate odds ratio and mean difference in subgroups of UIC levels, respectively.
TSH-stratified multivariate-generalized estimating equation (GEE) method [34] was adjusted for age, body mass index (BMI), and TPOAb+ status, with linear link function and exchangeable working correlation; the matrix method was employed to estimate the overall effect of UIC on FTI and T4 and their trend over the pregnancy period. Statistical analyses were performed using SPSS version 19.0 (SPSS, Inc., Chicago, IL, USA).
Results
In the present study, median (interquartile range) UIC in a total of 1286 participants was 142.3 (133.6) μg/L; results showed 370 (28.8%), 315 (24.5%), 359 (27.9%), and 242 (18.8%) of participants had UIC < 100, 100–150, 150–250, and ≥ 250 μg/L, respectively. In these pregnant women, 6.6% (n = 85) and 4.8% (n = 62) had TSH ≥ 4.0 and TPO > 50, respectively. Ranges of neonatal TSH concentrations, head circumference, weight, and height of the newborns were 0.1–11.5 μIU/mL, 27–43 cm, 1470–4700 g, and 41–62 cm, respectively. Table 1 shows the characteristics of the study population based on their urinary iodine subgroups; we found no significant differences in maternal age among different subgroups of UIC, whereas maternal weight and BMI were significantly different between these subgroups (p value = 0.037 and 0.013, respectively). Preterm delivery in group 4 (UIC ≥ 250 μg/L) was significantly lower than in group 1 (UIC < 100) (8 [4%] vs. 29 [9%], p < 0.05), and neonatal admission in group 4 was significantly lower than in groups 1, 2, and 3 (6 [3%] vs. 22 [7%], 30 [12%], 28 [11%]; p = 0.005, respectively). There were no significant differences in the rates of placental abruption and stillbirth between the four study groups.
Table 2 presents the results of age, BMI, and TPOAb+ adjusted GLM analysis for pregnancy outcomes in the study groups based on the TSH cutoff value of 4.0 μIU/mL and different urinary iodine concentrations. Regardless of TSH levels, the results of GLM showed a higher odds ratio for preterm delivery in group 1 versus group 4 (OR 2.4; 95% CI 1.1, 5.0; p = 0.035); the odds ratio of preterm delivery in the subgroup of women with UIC < 100 μg/L and TSH ≥ 4 μIU/mL was 2.5 times higher than of those with similar urinary iodine but TSH < 4 μIU/mL (OR 2.5; 95% CI 1.1, 10.0; p = 0.024).
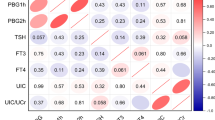
Table 3 presents the results of GEE analysis for FTI and T4, considering cutoff values of 4.0 μIU/mL for TSH and different subgroups of UIC, after the adjustment for age, BMI, and TPOAb+ status. Regardless of TSH level, the interaction of UIC and gestational trimester revealed that in comparison with those with UIC 150–250 μg/L, FTI was decreased by 0.1 unit (95% CI − 0.2, − 0.004; p = 0.041). This decreasing trend for UIC < 100 μg/L decelerated in pregnant women with TSH < 4 μIU/mL by − 0.08 unit (95% CI − 0.183, 0.015; p = 0.097) and accelerated by − 0.49 (95% CI − 0.818, − 0.158; p = 0.004) in pregnant women with TSH ≥ 4 μIU/mL. Trends of FTI and T4 over gestational time in different subgroups of UIC based on a TSH cutoff value of 4.0 μIU/mL are presented in Figs. 1, 2, 3, and 4, respectively.
Discussion
In this study conducted in an area with iodine sufficiency, despite the consumption of iodized salt, median UIC of 142.3 mIU/L, results showed mild iodine deficiency among our pregnant cohort, considering a WHO cutoff value of 150 mIU/L for the pregnancy period. We found that adverse pregnancy outcomes in terms of preterm delivery increased 2.5-fold (95% CI 1.1, 10.0; p = 0.024) in women with UIC < 100 μg/L and TSH ≥ 4 μIU/mL, compared with those with similar iodine concentrations and TSH < 4 μIU/mL; studies demonstrate that excessive iodine intake, especially in pregnant women with positive TPOAb, can induce a feedback loop to increase TSH levels and directly increase TSH levels by the action of the pituitary gland and the hypothalamus [35].
The present study showed an increased odds ratio of preterm delivery in pregnant women with deficiency of iodine (UIC < 100), in particular in those with TSH ≥ 4, compared with pregnant women with UIC ≥ 250, a finding consistent with the results of previous studies which show that adverse effects of iodine deficiency on pregnancy outcomes are higher in women with subclinical hypothyroidism [36, 37]. Charoenratana et al. demonstrated that in a severe iodine deficiency area, iodine status was an independent risk factor of preterm birth [38], and the Chaouki et al.’s study from Algeria showed that rates of abortion, stillbirth, and prematurity were significantly lower among women given oral iodized oil 1–3 months before conception or during pregnancy, than among untreated women in a severe iodine deficiency area [21]. On the contrary, Leon et al. (2015) reported UICs were not significantly related to preterm delivery in a mildly iodine deficient region [39].
Studies have documented associations between iodine deficiency, subclinical hypothyroidism, and adverse obstetric outcomes such as placental abruption and stillbirth, although the mechanisms behind these associations are unclear [40, 41]; our study did not show significant differences in the rates of these outcomes among different groups of iodine concentration. It has been suggested that a disturbance in thyroid hormones, viz. hypothyroidism, can lead to impaired endothelial function, increased arterial intimal media thickness, and insulin resistance, processes which may all result in placental insufficiency. Maternal thyroid status is important for trophoblastic function and to maintain pregnancy [40, 42]. However, in agreement with our study, Torlinska et al. [25] and Zhou et al. [43] also reported that maternal iodine status was not associated with adverse pregnancy outcomes in a mild-to-moderate iodine-deficient pregnant population. In contrast, Dillon et al. (2000) showed an increased risk of repeated miscarriages and stillbirth, which were related to severe iodine deficiency [41].
Differences in these results could be due to the method of assessing iodine status. Whereas we used three urine samples on different days of the week, Dillon et al. [41] and Leon et al. [39] assessed only one urine sample to determine iodine status in pregnant women. Considering the day-to-day and within-day variations in urinary iodine excretion, this method may not be reliable for determining iodine status. Even three urine samples, as we used, may not precisely define the individual iodine status, as demonstrated by König F et al., a reliable estimation of individual iodine status requires at least 10 urinary spot samples or 24-h samples [44]. These contradictory results may partly be explained by the timeline of recruitment. More than half of women in the present study were recruited after 8 weeks of gestation, and majority of miscarriages occur before 8 weeks of gestation. It is therefore possible that the study may have inadvertently excluded women with adverse pregnancy outcomes such as early miscarriages, and therefore, this data was not collected.
This study showed that regardless of TSH level, neonatal admission in pregnant women with UIC ≥ 250 μg/L was significantly lower than in those with UIC < 250 μg/L. Since most of the neonatal admissions can be due to prematurity, this finding seems logical. Similarly, Ozdemir et al. found that babies of pregnant women with hypothyroidism needed more frequent NICU admission, mainly due to preterm delivery [45]. In contrast, a randomized controlled trial conducted by Zhou et al. [43] did not detect any significant difference in the rate of NICU admissions between groups treated with 150 μg/L iodine supplement or placebo; their results however need to be interpreted with caution due to lack of adequate sample size. Another randomized, placebo-controlled trial conducted by Gowachirapant et al. [46] did not also detect any significant differences between the groups (receiving 200 μg iodine orally once a day or placebo until delivery) in the rate of serious adverse events in terms of death/hospital admission of either mother or baby for a cause other than delivery. Nevertheless, adequately powered randomized controlled trials with separate subgroups of iodine concentration are needed to provide conclusive evidence regarding the effect of iodine supplementation during pregnancy on neonatal admission rates.
The changing trend of FTI during pregnancy in the present study is in agreement with that reported by Azizi et al., markedly increasing in the first trimester, reaching a peak in the second trimester, and then falling in the third trimester [30]. Soldin et al. observed that in a region of iodine sufficiency, FT4 concentrations were significantly associated with a decline in the third trimester of pregnancy [47]. Khalil et al. also reported TSH values were lowest in the first-trimester group and increased in the second- and third-trimester groups, while FT4 levels showed the opposite trend [48], a finding similar to that of the current study. As pregnancy progressed, a decreasing trend of FTI was detected in women with UIC > 100 μg/L, compared with those with UIC < 100 μg/L per gestational trimester; although this negative trend was observed in both groups of pregnant women, regardless of baseline TSH cutoff value of 4 μIU/mL (− 0.1), it was more prominent in those with TSH ≥ 4 μIU/mL than in women with TSH < 4 μIU/mL (− 0.49 vs. − 0.08). These findings demonstrate the critical role of iodine deficiency in subclinical hypothyroidism in terms of decrease of FTI overtime throughout gestation.
According to WHO recommendations, the 2017 guidelines of the American Thyroid Association (ATA), and the European Thyroid Association (ETA), all pregnant women should ingest approximately 250 μg iodine daily, i.e., about 100 μg above their non-pregnant status. To ensure a daily consumption of 250 μg iodine, strategies may vary based on country of origin and iodine sufficiency levels [49]. Universal salt iodization is one of the most cost-effective ways of delivering iodine and improving maternal and infant health [20, 49]. In Iran, despite concerted attempts to ensure appropriate intake of adequate iodine in this population using strategies such as the universal iodization of salt and nutrition education programs, studies conducted on pregnant women shown that due to the increased need for iodine during pregnancy, urinary iodine concentration is below the recommended WHO level, demonstrating the need for increased iodine intake during pregnancy [50]. Similar to previous studies from Iran [28, 50, 51], in the current study, approximately a third (28.8%) of the pregnant population had urinary iodine concentrations < 100 μg/L (moderate-to-severe iodine deficiency), indicating that intakes of iodized salt in these women were inadequate and did not meet the iodine requirements of pregnancy.
The main strength of this study is its methodology, as a population-based study conducted mainly on first-trimester pregnant women with repeated assessments of thyroid status throughout the pregnancy period. Since in individuals, urinary iodine excretion can vary somewhat from day to day and even within a given day, median urinary iodine is the main indicator used to assess iodine status of a population [23]. In this study, collecting of urine samples on 3 different days of the week may partially remove the bias that may otherwise have occurred, in the precise evaluation of iodine status (due to day-to-day variations in urinary iodine excretion).
However, our study also had some limitations. First, the number of samples was insufficient to examine other rare pregnancy complications, e.g., preeclampsia and stillbirth. Second, not observing significant differences on miscarriage rates may be due to the non-timely recruitment of the study participants, and hence needs to be interpreted with caution. Third, lack of knowledge regarding some other risk factors of pregnancy outcomes could influence the results of this study. Fourth, changes in iodine status throughout the pregnancy cannot be assessed by use of single baseline assessment. Nutritional habits throughout pregnancy have not been evaluated, and their effects were not modified in analysis or interpretation of the results.
In conclusion, despite implementation of iodized salt strategies in Iran, mild iodine deficiency among our pregnant cohort indicates that iodine supplementation needs to be implemented for pregnant women. Considering the adverse pregnancy outcomes due to iodine deficiency, especially in women with TSH ≥ 4 μIU/mL, monitoring of urinary iodine concentration at the population level and iodine replacement may be needed during pregnancy, even in areas of iodine sufficiency.
References
Perez-Lopez FR (2007) Iodine and thyroid hormones during pregnancy and postpartum. Gynecol Endocrinol 23(7):414–428 http://www.ncbi.nlm.nih.gov/pubmed/17701774
Delange F (2007) Iodine requirements during pregnancy, lactation and the neonatal period and indicators of optimal iodine nutrition. Public Health Nutr 10:1571–1580 discussion 1581–1573. http://www.ncbi.nlm.nih.gov/pubmed/18053281
Delange F (2001) Iodine deficiency as a cause of brain damage. Postgrad Med J 77:217–220 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1741987/
Yarrington CD, Pearce EN (2011) Dietary iodine in pregnancy and postpartum. Clin Obstet Gynecol 54:459–470 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3134395/
Crew MD, Spindler SR (1986) Thyroid hormone regulation of the transfected rat growth hormone promoter. J Biol Chem 261:5018–5022 http://www.ncbi.nlm.nih.gov/pubmed/2420797
Samuels MH, Wierman ME, Wang C, Ridgway EC (1989) The effect of altered thyroid status on pituitary hormone messenger ribonucleic acid concentrations in the rat. Endocrinology 124:2277–2282 http://www.ncbi.nlm.nih.gov/pubmed/2707156
Hochberg Z, Bick T, Harel Z (1990) Alterations of human growth hormone binding by rat liver membranes during hypo- and hyperthyroidism. Endocrinology 126:325–329 http://www.ncbi.nlm.nih.gov/pubmed/2293991
Pearce EN (2012) Effects of iodine deficiency in pregnancy. J Trace Elem Med Biol 26:131–133 http://www.ncbi.nlm.nih.gov/pubmed/22565014
Glinoer D (2006) Iodine nutrition requirements during pregnancy. Thyroid 16:947–948 http://www.ncbi.nlm.nih.gov/pubmed/17042676
Glinoer D (1997) The regulation of thyroid function in pregnancy: pathways of endocrine adaptation from physiology to pathology. Endocr Rev 18:404–433 http://www.ncbi.nlm.nih.gov/pubmed/9183570
Dafnis E, Sabatini S (1992) The effect of pregnancy on renal function: physiology and pathophysiology. Am J Med Sci 303:184–205 http://www.ncbi.nlm.nih.gov/pubmed/1595782
Glinoer D (2004) The regulation of thyroid function during normal pregnancy: importance of the iodine nutrition status. Best Pract Res Clin Endocrinol Metab 18:133–152 http://www.ncbi.nlm.nih.gov/pubmed/15157832
Hershman JM (2004) Physiological and pathological aspects of the effect of human chorionic gonadotropin on the thyroid. Best Pract Res Clin Endocrinol Metab 18:249–265 http://www.ncbi.nlm.nih.gov/pubmed/15157839
Dunn JT, Delange F (2001) Damaged reproduction: the most important consequence of iodine deficiency. J Clin Endocrinol Metab 86:2360–2363 https://academic.oup.com/jcem/article/86/6/2360/2848412
Elnagar B, Eltom A, Wide L, Gebre-Medhin M, Karlsson FA (1998) Iodine status, thyroid function and pregnancy: study of Swedish and Sudanese women. Eur J Clin Nutr 52:351–355 http://www.ncbi.nlm.nih.gov/pubmed/9630385
Zimmermann MB (2009) Iodine deficiency. Endocr Rev 30:376–408 https://www.liebertpub.com/doi/abs/10.1089/thy.2007.0108
Hetzel BS (1983) Iodine deficiency disorders (IDD) and their eradication. Lancet 2:1126–1129 https://www.sciencedirect.com/science/article/pii/S0140673683906360?via%3Dihub
Zimmermann MB, Jooste PL, Pandav CS (2008) Iodine-deficiency disorders. Lancet 372(9645):1251–1262 http://www.ncbi.nlm.nih.gov/pubmed/18676011
Pearce EN, Lazarus JH, Moreno-Reyes R, Zimmermann MB (2016) Consequences of iodine deficiency and excess in pregnant women: an overview of current knowns and unknowns. Am J Clin Nutr 104(Suppl 3):918S–923S http://www.ncbi.nlm.nih.gov/pubmed/27534632
Zimmermann MB (2012) The effects of iodine deficiency in pregnancy and infancy. Paediatr Perinat Epidemiol 26(Suppl 1):108–117 http://www.ncbi.nlm.nih.gov/pubmed/22742605
Chaouki ML, Benmiloud M (1994) Prevention of iodine deficiency disorders by oral administration of lipiodol during pregnancy. Eur J Endocrinol 130:547–551 http://www.ncbi.nlm.nih.gov/pubmed/8205252
DeLong GR, Leslie PW, Wang SH, Jiang XM, Zhang ML, Rakeman M, Jiang JY, Ma T, Cao XY (1997) Effect on infant mortality of iodination of irrigation water in a severely iodine-deficient area of China. Lancet 350:771–773 http://www.ncbi.nlm.nih.gov/pubmed/9297997
International Council for Control of Iodine Deficiency Disorders (2007) Assessment of iodine deficiency disorders and monitoring their elimination: a guide for programme managers. World Health Organization, Geneva
McMichael A, Potter J, Hetzel B (1980) Iodine deficiency, thyroid function and reproductive failure. In Endemic Goitre and Endemic Cretinism. Wiley Medical, New York
Torlinska B, Bath SC, Janjua A, Boelaert K, Chan S-Y (2018) Iodine status during pregnancy in a region of mild-to-moderate iodine deficiency is not associated with adverse obstetric outcomes; results from the Avon Longitudinal Study of Parents and Children (ALSPAC). Nutrients 10:291 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5872709/
Azizi F, Sheikholeslam R, Hedayati M, Mirmiran P, Malekafzali H, Kimiagar M, Pajouhi M (2002) Sustainable control of iodine deficiency in Iran: beneficial results of the implementation of the mandatory law on salt iodization. J Endocrinol Investig 25:409–413 https://springerlink.bibliotecabuap.elogim.com/article/10.1007/BF03344029
Amouzegar A, Azizi F (2013) Variations of urinary iodine during the first trimester of pregnancy in an iodine-replete area. Comparison with non-pregnant women. Hormones 12:111–118 http://www.ncbi.nlm.nih.gov/pubmed/23624137
Mirmiran P, Nazeri P, Amiri P, Mehran L, Shakeri N, Azizi F (2013) Iodine nutrition status and knowledge, attitude, and behavior in Tehranian women following 2 decades without public education. J Nutr Educ Behav 45:412–419 https://linkinghub.elsevier.com/retrieve/pii/S1499-4046(13)00083-3
Nazarpour S, Ramezani Tehrani F, Simbar M, Tohidi M, Azizi F (2016) Thyroid and pregnancy in tehran, Iran: objectives and study protocol. Int J Endocrinol Metab 14:e33477 http://www.ncbi.nlm.nih.gov/pubmed/27279833
Azizi F, Mehran L, Amouzegar A, Delshad H, Tohidi M, Askari S, Hedayati M (2013) Establishment of the trimester-specific reference range for free thyroxine index. Thyroid 23:354–359 http://www.ncbi.nlm.nih.gov/pubmed/23167270
Suff N, Story L, Shennan A, editors (2018) The prediction of preterm delivery: what is new? Semin Fetal Neonatal Med Elsevier 28: S1744-165X(18)30111-2. https://www.sciencedirect.com/science/article/pii/S1744165X18301112?via%3Dihub
Elsasser DA, Ananth CV, Prasad V, Vintzileos AM, Investigators NJ-PAS (2010) Diagnosis of placental abruption: relationship between clinical and histopathological findings. Eur J Obstet Gynecol Reprod Biol 148:125–130 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2814948/
Blencowe H, Cousens S, Jassir FB, Say L, Chou D, Mathers C, Hogan D, Shiekh S, Qureshi ZU, You D, Lawn JE, Lancet Stillbirth Epidemiology Investigator G (2016) National, regional, and worldwide estimates of stillbirth rates in 2015, with trends from 2000: a systematic analysis. Lancet Glob Health 4(2):e98–e108 http://www.ncbi.nlm.nih.gov/pubmed/26795602
Diggle P, Diggle PJ, Heagerty P, Heagerty PJ, Liang K-Y, Zeger S (2002) Analysis of longitudinal data, 2nd edn. Oxford University Press, UK
Sang ZN, Wei W, Zhao N, Zhang GQ, Chen W, Liu H, Shen J, Liu JY, Yan YQ, Zhang WQ (2012) Thyroid dysfunction during late gestation is associated with excessive iodine intake in pregnant women. J Clin Endocrinol Metab 97:E1363–E1369 https://academic.oup.com/jcem/article/97/8/E1363/2823030
Casey BM, Dashe JS, Wells CE, McIntire DD, Byrd W, Leveno KJ, Cunningham FG (2005) Subclinical hypothyroidism and pregnancy outcomes. Obstet Gynecol 105:239–245 http://www.ncbi.nlm.nih.gov/pubmed/15684146
Nazarpour S, Ramezani Tehrani F, Simbar M, Tohidi M, Minooee S, Rahmati M, Azizi F (2018) Effects of levothyroxine on pregnant women with subclinical hypothyroidism, negative for thyroid peroxidase antibodies. J Clin Endocrinol Metab 103:926–935 http://www.ncbi.nlm.nih.gov/pubmed/29126290
Charoenratana C, Leelapat P, Traisrisilp K, Tongsong T (2016) Maternal iodine insufficiency and adverse pregnancy outcomes. Matern Child Nutr 12:680–687 http://www.ncbi.nlm.nih.gov/pubmed/26332721
León G, Murcia M, Rebagliato M, Álvarez-Pedrerol M, Castilla AM, Basterrechea M, Iñiguez C, Fernández-Somoano A, Blarduni E, Foradada CM (2015) Maternal thyroid dysfunction during gestation, preterm delivery, and birthweight. The Infancia y Medio Ambiente Cohort, S pain. Paediatr Perinat Epidemiol 29:113–122. https://doi.org/10.1111/ppe.12172
Breathnach FM, Donnelly J, Cooley SM, Geary M, Malone FD (2013) Subclinical hypothyroidism as a risk factor for placental abruption: evidence from a low-risk primigravid population. Aust N Z J Obstet Gynaecol 53:553–560. https://doi.org/10.1111/ajo.12131
Dillon JC, Milliez J (2000) Reproductive failure in women living in iodine deficient areas of West Africa. BJOG 107:631–636 http://www.ncbi.nlm.nih.gov/pubmed/10826578
Ohara N, Tsujino T, Maruo T (2004) The role of thyroid hormone in trophoblast function, early pregnancy maintenance, and fetal neurodevelopment. J Obstet Gynaecol Can 26:982–990 http://www.ncbi.nlm.nih.gov/pubmed/15560861
Zhou SJ, Skeaff SA, Ryan P, Doyle LW, Anderson PJ, Kornman L, McPhee AJ, Yelland LN, Makrides M (2015) The effect of iodine supplementation in pregnancy on early childhood neurodevelopment and clinical outcomes: results of an aborted randomised placebo-controlled trial. Trials 16:563 http://www.ncbi.nlm.nih.gov/pubmed/26654905
König F, Andersson M, Hotz K, Aeberli I, Zimmermann MB (2011) Ten repeat collections for urinary iodine from spot samples or 24-hour samples are needed to reliably estimate individual iodine status in women–4. J Nutr 141:2049–2054 https://academic.oup.com/jn/article/141/11/2049/4630581
Ozdemir H, Akman I, Coskun S, Demirel U, Turan S, Bereket A, Bilgen H, Ozek E (2013) Maternal thyroid dysfunction and neonatal thyroid problems. Int J Endocrinol 2013:987843 http://www.ncbi.nlm.nih.gov/pubmed/23737782
Gowachirapant S, Jaiswal N, Melse-Boonstra A, Galetti V, Stinca S, Mackenzie I, Thomas S, Thomas T, Winichagoon P, Srinivasan K, Zimmermann MB (2017) Effect of iodine supplementation in pregnant women on child neurodevelopment: a randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol 5:853–863 http://www.ncbi.nlm.nih.gov/pubmed/29030199
Soldin OP, Tractenberg RE, Hollowell JG, Jonklaas J, Janicic N, Soldin SJ (2004) Trimester-specific changes in maternal thyroid hormone, thyrotropin, and thyroglobulin concentrations during gestation: trends and associations across trimesters in iodine sufficiency. Thyroid 14:1084–1090 http://www.ncbi.nlm.nih.gov/pubmed/15650363
Khalil AB, Salih BT, Chinengo O, Bardies MRD, Turner A, Wareth LOA (2018) Trimester specific reference ranges for serum TSH and free T4 among United Arab Emirates pregnant women. Pract Lab Med 12. https://www.sciencedirect.com/science/article/pii/S2352551717300112
Alexander EK, Pearce EN, Brent GA, Brown RS, Chen H, Dosiou C, Grobman WA, Laurberg P, Lazarus JH, Mandel SJ, Peeters RP, Sullivan S (2017) 2017 guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and the postpartum. Thyroid 27:315–389 http://www.ncbi.nlm.nih.gov/pubmed/28056690
Nazeri P, Zarghani NH, Mirmiran P, Hedayati M, Mehrabi Y, Azizi F (2016) Iodine status in pregnant women, lactating mothers, and newborns in an area with more than two decades of successful iodine nutrition. Biol Trace Elem Res 172:79–85 https://springerlink.bibliotecabuap.elogim.com/article/10.1007%2Fs12011-015-0575-1
Delshad H, Amouzegar A, Mirmiran P, Mehran L, Azizi F (2012) Eighteen years of continuously sustained elimination of iodine deficiency in the Islamic Republic of Iran: the vitality of periodic monitoring. Thyroid 22:415–421 http://www.ncbi.nlm.nih.gov/pubmed/22409203
Acknowledgments
The authors wish to acknowledge Ms. Niloofar Shiva for critical editing of English grammar and syntax of the manuscript. The authors would also like to thank the laboratory staff of RIES for their cooperation and assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study was approved by the ethics committee of the Research Institute of Endocrine Sciences (RIES), approval no: IR.SBMU.ENDOCRINE.REC.1397.273.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nazarpour, S., Ramezani Tehrani, F., Amiri, M. et al. Maternal Urinary Iodine Concentration and Pregnancy Outcomes: Tehran Thyroid and Pregnancy Study. Biol Trace Elem Res 194, 348–359 (2020). https://doi.org/10.1007/s12011-019-01812-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12011-019-01812-5