Abstract
Purpose of Review
Over the past two decades, significant progress has been made to untangle the etiology of inflammation and new bone formation (NBF) associated with axial spondyloarthritis (axSpA). However, exact mechanisms as to how the disease initiates and develops remain elusive.
Recent Findings
Type 3 immunity, centered around the IL-23/IL-17 axis, has been recognized as a key player in the pathogenesis of axSpA. Multiple hypotheses associated with HLA-B*27 have been proposed to account for disease onset and progression of axSpA, potentially by driving downstream T cell responses. However, HLA-B*27 alone is not sufficient to fully explain the development of axSpA. Genome-wide association studies (GWAS) identified several genes that are potentially relevant to disease pathogenesis leading to a better understanding of the immune activation seen in axSpA. Furthermore, gut microbiome studies suggest an altered microbiome in axSpA, and animal studies suggest a pathogenic role for immune cells migrating from the gut to the joint. Recent studies focusing on the pathogenesis of new bone formation (NBF) have highlighted the importance of endochondral ossification, mechanical stress, pre-existing inflammation, and activated anabolic signaling pathways during the development of NBF.
Summary
Despite the complex etiology of axSpA, recent studies have shed light on pivotal pieces that could lead to a better understanding of the pathogenic events in axSpA.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
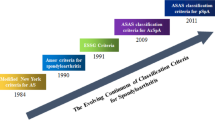
Introduction
Axial spondyloarthritis (axSpA) is a chronic rheumatic disease that affects the spine, sacroiliac joints (SIJs), eyes (uveitis), gut (ileitis), and skin (psoriasis). The spectrum of AxSpA includes patients with (i) ankylosing spondylitis (AS) who have structural changes detectable by X-rays, fulfilling the modified New York criteria [1], and (ii) non-radiographic axSpA where inflammation is captured by MRI but no definitive changes on x-rays.
Over the past two decades, significant progress has been made in untangling the pathogenesis of axSpA. Genetic susceptibility, epigenetic modification, gut microbiome, and other environmental factors play important roles in the immunopathology of axSpA, especially for the activation of type 3 immunity [2]. Importantly, these factors likely contribute in consort for the development of axSpA, as likely none of these factors can independently induce disease.
Here, we discuss recent advances in our understanding of the immunological mechanisms underlying the onset and the potential sequence of events in the development of axSpA.
Genetics of AS
The importance of hereditary factors in the pathogenesis of AS was reported in the early 1960s [3]. Monozygotic twins who have greater gene sharing have higher concordance of AS (63%) compared to dizygotic twins (12.5%) [4]. Among genetic variants identified in axSpA, HLA-B*27 is the strongest gene associated with AS [5]. However, the contribution of HLA-B*27 has been reported to be only ~ 20% of the overall heritability of AS [6]. In addition, the vast majority of healthy HLA-B*27 + individuals do not develop AS. This demonstrates that additional genes and genetic regions are involved in the development of AS. With the help of large GWAS studies, we have identified several genetic variants which may play critical roles in the pathogenesis of axSpA.
HLA-B*27
The prevalence of HLA-B*27 varies in the general populations across countries. It is more common in indigenous populations of Western Canada/Alaska (40–50% of prevalence) and European descent (~ 8%) than Middle East/North African (2–5%) [7]. Among over 160 subtypes of HLA-B*27, HLA-B*27:02 and B27:05 have frequently been reported to have the disease association with AS [8]. Other subtypes also appear to be implicated in different regions; for instance, HLA-B*27:03 and HLA-B*27:04 being associated with axSpA/AS in sub-Sahara/Middle Eastern and Chinese and Asian populations, respectively [9, 10].
The pathogenic roles of HLA-B*27 has been investigated in rodent models of SpA. The presence of a high gene copy number of HLA-B*27:05 in HLA-B*27/human β2-microglobulin (hβ2m) transgenic rats spontaneously induces SpA-like disease with arthritis, enthesitis, spondylitis, and NBF. The model also exhibits increased levels of key pathogenic cytokines including IL-17 [11,12,13]. Although hβ2m is part of MHC class I, its pathogenic role seems to be less important than HLA-B*27:05, as the transgenic rats still display the SpA-like phenotypes even in the lack of h β2m expression [14]. In addition, administration of the human class I heavy chain-specific monoclonal antibody (mAb: HC10) is sufficient to ameliorate the disease [15]. Intriguingly, HLA-B27:05 transgenic mice do not develop spontaneous SpA-like features potentially due to altered function of HLA-B27:05 in the presence of mouse β2m [16].
In humans, the precise pathological role of HLA-B27 remains unclear. Some potential mechanisms of how HLA-B*27 may be implicated in the pathogenesis of AS were previously suggested, including presentation of arthritogenic peptides, formation of aberrant HLA-B*27 (free heavy chains) structures, and accumulation of HLA-B*27 misfolded protein in the endoplasmic reticulum (ER) [17]. Recently, a study published by Yang et al. provides strong evidence supporting the involvement of T cell receptors (TCRs) and peptide presentation [18••]. Specifically, the study identified a unique TCR consistently pairing with the alpha chain variable region AV21, which was found to be clonally expanded in the joints of AS patients and in the eyes of acute anterior uveitis (AAU) patients. Notably, these TCRs isolated from AS and AAU patients exhibited cross-reactivity with both self-peptides and microbial peptides [18••], suggesting a shared binding motif in these antigens and highlighting the potential role of TCRs and peptide presentation in the development of HLA-B27-associated diseases.
Other Genes
GWAS studies have identified over 100 susceptibility loci for SpA spectrum diseases, such as AS, Crohn’s disease (CD), and psoriasis [6]. The genetic polymorphisms in the aminopeptidases, endoplasmic reticulum aminopeptidase 1 and 2 (ERAP1 and ERAP2), are strongly associated with AS [19]. Enzymatic activities of ERAP1 and ERAP2 aid in trimming peptides for presentation on MHC-I molecules. Based on this function, ERAP1 and ERAP2 variants could directly affect peptide-HLA-B*27 complex formation. However, the potential role of ERAP in previous studies show mixed results, possibly due to the difference in the experimental designs, methods, cell lines, or others. For instance, it was reported that the silencing of ERAP1 expression enhanced the accumulation of HLA-B*27 open conformations on the cell membrane [20, 21], while others showed that dysfunction of ERAP1 decreased the expression of open conformations [22]. With regard to ERAP2, the higher expression of HLA-B*27 open conformations on the surface of PBMCs has been shown in HLA-B*27 positive axSpA patients lacking ERAP2 [23]. The same study also showed that ERAP2 suppression in a HLA-B*27 cell line led to increased levels of HLA-B*27 open conformations and activation of the unfolded protein response (UPR) [23]. These results suggest that impaired peptide processing and antigen presentation could contribute to the pathogenesis of axSpA in a multitude of ways.
Gut Microbiome
Alterations in the composition of gut microbiome may contribute to the pathogenesis of autoimmune diseases. Gut microbiome, through activation of immune responses and impaired intestinal permeability, is reported to be associated with disease activity of autoimmune diseases. Gut inflammation is one of the major extra-articular manifestations in SpA, affecting up to 70% of patients including those who have subclinical inflammation [24]. Changes of gut microbiota have been reported in patients with axSpA and recent studies demonstrate that HLA-B*27 play a role in the bacterial flora even in healthy individuals [25, 26]. In addition, microbiome differences were seen in HLA-B*27/ hβ2m transgenic rats compared to wild type rats [27]. These data suggest that disrupted microbiome in axSpA may be the cause rather than a consequence of disease.
Dysbiosis in the gut causes a pathogenic microenvironment where inflammatory mediators are overproduced [28]. The SKG mouse (Zap70 mutation), a well-established SpA mouse model, exhibits ileitis after the administration of fungal component β-glucans with increased production of IL-23 [29]. IL-23 activates IL-23 receptor bearing cells such as conventional CD4 + T cells, γδ T cells, and group 3 innate lymphoid cells, all of which are identified in human spinal entheses [30,31,32]. As an IL-23 overexpression mouse model displays enthesitis [33], it is conceivable that upregulated production of IL-23 in the gut tissues activates entheseal resident immune cells and stromal cells, leading to the enhancement of the IL-23/IL-17 axis.
Although a distinct composition of microbiota has been postulated in axSpA, this does not necessarily indicate an activated immune response in the gut. To detect microbiota evoking an immune response in the gut, a recent study labeled and sorted IgA-coated and uncoated bacteria from fecal homogenates of CD-associated SpA patients [34••]. This study found an abundant IgA-coated Escherichia coli (E. coli) in CD-SpA patients and the E. coli were similar in genotype and phenotype to an adherent-invasive E. coli (AIEC) pathotype. CD-SpA–derived AIEC induced systemic Th17 immunity and promoted joint inflammation. These data suggest that the specific bacterial pathogen enhances the adaptive IgA response to induce Th17-mediated immune response. Previous reports showed increased levels of serum IgA in SpA patients including axSpA [35,36,37], which may corroborate this etiology.
The migration of activated immune cells in the gut to joint tissues have been proposed in axSpA, yet the corroborating evidence is still sparse. However, a recent study demonstrated evidence that may link arthritis with gut inflammation in the CIA mouse model [38••]. This study showed that effector T cells migrate from the lamina propria of the leaky gut towards the synovial tissues in the joint where they induced arthritis. The authors also showed that the increased permeability in the intestinal epithelium may be caused by increased expression of zonulin that disrupts gut tight junctions in arthritis patients and mouse models. Restoration of the intestinal barrier function with zonulin antagonist suppressed the development of arthritis in this mouse model. Although further studies focusing on how immune cells are activated and migrate into the joints are needed, this study demonstrates an important perspective of immune cell migration from gut to joint tissues through the impaired gut barrier function.
Gender
Historically, AS was commonly considered a condition primarily impacting men, with a male-to-female ratio of 3.6 to 6.1: 1 [39]. However, recent studies indicate that a substantial number of AS patients are women, with a male-to-female ratio of less than 2: 1 [40, 41]. Regarding nr-axSpA, the prevalence appears to be similar between the genders [42]. Previous studies showed that men are more likely to have greater radiographic changes and MRI inflammation in the sacroiliac joints and spinal progression (syndesmophyte formation) assessed by mSASSS (The modified Stoke Ankylosing Spondylitis Spinal Score) scores compared to women [43,44,45]. Despite more extensive spinal damage in men, the quality of life (QOL) assessed by patient-reported outcomes are poorer in women than in men with early axSpA [45]. Key elements in QOL such as fatigue, axial pain, and functional scores (BASFI) are significantly poorer in women [45]. A more recent real-world study further showed the similar results in which overall disease burden was greater in women compared to men with axSpA, despite lesser spinal immobilization than men [46]. These data indicate that gender is one of the determinants for disease phenotypes in axSpA.
The reasons for the distinct phenotypes between males and females are likely multifactorial such as genetic, immunological, and hormonal differences. In men but not women with AS, upregulated expression was observed in genes such as IL17RA, MEFV, and NLRP12 [47]. Likewise, the serum level of IL-17A and the frequency of Th17 cells in blood were increased in men but not in women with AS, compared to healthy controls [47]. Hormonal gender differences may also be responsible for part of distinct immune responses between men and women. Estrogen increases production of IL-1, IL-6, and tumor necrosis factor-alpha (TNF-α) [48], while testosterone decreases TNF-α production but increases the production of anti-inflammatory IL-10 [49]. Given men have more radiographic changes, these cytokine profiles do not seem to fully account for spinal progression in axSpA, and the etiology is likely more complicated.
Other Potential Factors
Smoking has been reported as a risk factor of spinal progression in AS [50]. A previous study showed that current smoking status was significantly associated with incident self-reported axSpA in logistic regression adjusted for possible confounders [51]. Interestingly, smoking was an independent factor associated with MRI-assessed inflammation in sacroiliac joints in a cohort for axSpA patients [52]. Although the mechanism as to how smoking induces worse spinal outcomes has not been determined, these data suggest that smoking has harmful effects on the spinal progression in patients with axSpA.
Despite sparse evidence, lower levels of vitamin D, compared to healthy controls, are not uncommon in AS patients and may contribute to increased risks of active disease, impaired function, radiographic severity, and bone mineral loss [53]. Conversely, another study showed that there were not any significant correlations between serum levels of vitamin D and the severity of disease in SpA patients, although serum vitamin D levels were lower in SpA patients compared to healthy controls [54]. An overview of potential contributors driving inflammation in axSpA is shown in Fig. 1.
Potential factors driving inflammation in axial spondyloarthritis (axSpA). Factors such as genetic, gender, and environmental factors (smoking and diet) activate immune response in axSpA. Gut inflammation caused by microbiome alteration (dysbiosis), barrier dysfunction, and specific pathogens also activates systemic inflammation. The activated immune response chiefly driven by type 3 immunity causes inflammation in the joint, spine, and entheseal tissues. Immune cells activated in the gut may migrate into the joint and spine. ERAP, endoplasmic reticulum aminopeptidase 1; ER, endoplasmic reticulum; UPR, unfolded protein response. The figure was created with BioRender (BioRender.com)
Development of NBF in AS
Besides the understanding of the activation of immune response that provokes inflammation in axSpA, the sequential development of NBF has rigorously been studied, and its pathogenesis has gradually been unveiled.
Endochondral Ossification
Endochondral ossification in axSpA spinal ligaments has been described as an essential process during the development of NBF in axSpA [55]. During this process, a cartilage template is first formed by chondrocytes which is then replaced by osteoblasts to create mature bone. Yu et al. found increased Col II + chondrocyte differentiation and cartilage formation in the spinal ligaments of patients with early AS [56••]. The same study identified endochondral ossification in these sites where hypertrophied chondrocytes calcified and subsequently recruited osteoclasts [56••]. Similar to acquired heterotopic ossification, these osteoclasts secreted transforming growth factor beta (TGF-β) which in-turn attracted osteoblasts to these sites to produce mature heterotopic bone [56••]. Moreover, a study by Cui et al. highlighted the importance of another chemokine, CXCL12, in the recruitment of osteoprogenitor cells to the entheseal sites of NBF [57]. They showed that CXCL12 was overexpressed in the ligaments and entheseal regions of both human and mouse models of AS. CXCL12 was found to be expressed mainly by CD45 + immune cells in early disease and by Col2a1 + cells in later stages. When CXCL12 was overexpressed in Col2a1 + cells in DBA mice, severe ankylosis, higher bone volume of osteophytes, and earlier onset of new bone formation were observed [57].
Other studies also highlight the importance of endochondral ossification in axSpA. A study showed that tenascin C, a large molecular extracellular matrix glycoprotein, promotes chondrogenesis in bone marrow derived mesenchymal stem cells (BM-MSCs) [58]. This protein is overexpressed in AS ligaments and entheseal tissues in both humans and animal models [58, 59]. Inhibition of tenascin C systemically, showed an overall amelioration of pathogenic NBF in proteoglycan-induced arthritis mice [58]. In another study, antagonism of the calcium-sensing receptor (CaSR) was shown to downregulate chondrogenic genes such as Sox9 and Col2a1 in mouse chondrocytes [60]. These studies demonstrate the importance of chondrogenesis as one of the initial processes of NBF, which may serve as a potential therapeutic target to prevent NBF at an early stage.
Interestingly, a recent study has reported an interesting aspect of TNF related to endochondral ossification in SpA [61••]. Transmembrane TNF (tm TNF) was found to be elevated in synovial tissues from SpA patients compared to those from rheumatoid arthritis (RA) patients. Conversely, soluble TNF (sTNF) is more abundant in SF from RA compared to SF from SpA, possibly due to deceased activity of ADAMTS17 (TACE) in SpA patients [61••]. As tm TNF-overexpressing mice clearly exhibit NBF through endochondral ossification, the balance between tm TNF and sTNF may determine the phenotypic difference between RA and SpA. Therefore, therapies targeting tmTNF, rather than sTNF, may offer a novel treatment avenue to prevent or delay NBF in axSpA.
Contribution of Mechanical Stress and Inflammation to NBF
Previous studies proposed the potential relationship between mechanical loading and proinflammatory processes in axSpA joints and entheses. Studies in collagen antibody induced arthritis (CAIA) mouse models show that voluntary running induced mechanical stress impaired the resolution of arthritis, by upregulating the complement system and inhibiting the immune suppressing activity of T regulatory cells (Tregs) [62]. Another recent study done in TNFΔARE mouse models showed that hindlimb unloading by tail suspension ameliorated clinical signs of peripheral arthritis and led to the development of decreased new bone formation by inactivating the ERK1/2 pathway [63]. This pathway has been shown to upregulate osteogenic and proinflammatory markers in AS [64, 65]. A recent study showed that Peizo-1, a mechanosensitive calcium channel, was overexpressed in human AS and CAIA mouse entheseal samples [66]. Moreover, when mice were tail suspended to prevent mechanical stress induced NBF, the administration of a Peizo-1 agonist Yoda1 rescued osteophyte formation in CAIA mice [66].
In vitro studies that stretch stimulated osteoblasts and chondrocytes showed increases in osteogenic BMP2 and proinflammatory mediators such as IL-6 and prostaglandin E2 (PGE2) [67]. Furthermore, mechanical loading was also shown to be responsible for the onset of joint specific inflammation from systemic autoimmunity by leading to the overexpression of monocyte homing markers such as CXCL1 and CCL2. This can promote bone specific damage by osteoclast conversion and inflammation through the secretion of cytokines [68].
Although the sequential event from inflammation to NBF has not been fully delineated yet, NBF tends to develop at inflamed vertebral edges in human AS [69]. In addition, previous MRI studies suggested that NBF likely develops in resolved inflammatory spinal lesions with fat metaplasia [70, 71]. Pro-inflammatory cytokines themselves, especially the IL23/IL-17 axis, contribute to NBF in AS [72]. While both IL-17 and IL-23 have been shown to have a positive effect on osteoclastogenesis [72,73,74], evidence also exists on these cytokines’ ability to induce bone formation as well. In human periosteal derived cells treated with IL-17A and IL-17F, increased RUNX2, BMP2, and matrix mineralization was observed [75]. Similar results were achieved in mesenchymal stem cells (MSCs) cultured with IL17A, whereby osteogenesis was enhanced over adipogenesis [76]. Furthermore, IL-37, a member of the IL-1 family, upregulated matrix mineralization and osteoblast markers in MSCs through PI3K/AKT signaling [77]. Research has also shown that IL-1β, IL-17A, IL-22, IL-23, and TNF-α were able to induce the expression of calcium sensing receptor (CaSR) in osteoblasts cell lines [60]. CaSR is a G protein coupled receptor that is critical in modulating Ca2+ homeostasis. Inhibition of this receptor diminished osteoblast maturation and matrix mineralization in vivo and inhibited spinal ankylosis and pathogenic bone formation in a proteoglycan-induced arthritis mouse model [60]. Furthermore, increased levels of CaSR + osteoblasts accumulated in bone formation sites like the entheses and spinal ligaments in axSpA patients compared to healthy controls [60]. Finally, macrophage inhibitory factor (MIF) was recently identified as an osteogenic cytokine that induced mineralization in a mature osteoblast cell line in vitro. MIF was elevated in AS serum compared to controls and positively associated with radiographic progression as assessed by mSASSS scores [78•]. Taken together, the recent evidence shows that mechanical stress in axSpA/AS joints and entheses promotes a proinflammatory environment which in turn recruits osteoclastic, osteogenic and progenitor cells to these sites. This drives NBF through the anabolic pathways described below.
Signaling Pathways Associated with NBF
Wnt/β-Catenin Pathway
The Wnt pathway regulates important cellular activities and plays a vital role during skeletal development [79]. When this pathway is activated by secreted Wnt proteins, cytosolic β-catenin is rescued from phosphorylation and subsequent proteasomal degradation and is translocated into the nucleus to transcribe target genes. This pathway is also critically important to bone homeostasis and NBF [79]. In AS, Wnt proteins are highly expressed in the spinal ligament tissue of axSpA patients compared to healthy controls [80]. When osteoblasts were treated with supernatant from monocytes that were treated constitutively with low doses of TNF-α, increased levels of osteogenesis were observed. This was reversed with the knock down of β-catenin in osteoblasts or Wnt proteins in monocytes [80]. Other studies show that Wnt pathway inhibitors such as DKK-1 and sclerostin (SOST) could be differentially expressed and regulated in AS to promote aberrant NBF [81, 82]. However, there is some disagreement in literature on the exact nature of their involvement [83,84,85]. Further investigation is warranted to determine the clinical importance and nature of Wnt pathway inhibitors in AS. Finally, recent studies have elucidated the role of ankylosis progressive homolog (ANKH) in AS [86, 87]. ANKH is a transmembrane protein that transports intracellular pyrophosphate to the extracellular milieu. This protein was downregulated in AS spinal ligament tissues when compared to those from spinal fracture controls. In vitro studies showed that overexpression of ANKH in AS fibroblasts inhibited mineralization and ossification by promoting β-catenin phosphorylation and degradation [86]. Another study showed that miR-17-5p was significantly upregulated in fibroblasts and ligament tissue from AS patients compared to HC and inhibits ANKH by targeting its 3’ untranslated region [87]. Indeed, the knockdown of miR-17-5p reduced fibroblast osteogenesis and sacroiliitis in rats with AS [87].
Other microRNAs can also regulate the Wnt pathway in AS. miR-96 levels are elevated in AS and have been reported to inhibit sclerostin [88]. Administration of miR-96 mimics to AS mouse models resulted in increased levels of inflammatory cytokines such as IL-6, IL-1, and TNF-α. It also resulted in increased levels of Wnt1, β-catenin, and osteoblast lineage markers such as Runx2, osteoprotegerin (OPG) and osteocalcin (OC) which contributed to increased osteoblast differentiation and calcium mineralization [88]. Additionally, miR-29a was also upregulated in AS PBMCs and is positively associated with mSASSS and disease duration [89]. It has been shown to upregulate the Wnt pathway by downregulating its inhibitor DKK-1 [90, 91].
BMP Pathway
Bone morphogenic proteins (BMPs) are growth factors and cytokines that belong to the TGF superfamily [92]. It is one of the most critical among cell signaling pathways in the body for skeletal development and growth. BMPs can activate the Smad pathway by binding to its cell surface receptor, which subsequently phosphorylates Smad1/5/8, translocating Smad4 into the nucleus to modulate gene expression. In AS, multiple studies have shown that the involvement and upregulation of BMPs is necessary for disease pathogenesis. Specifically, serum levels of BMP2 and BMP4 have been associated with spinal progression [93,94,95].
In a 3D cell culture system that was meant to model the bone microenvironment in AS, MSCs derived from AS patients had higher osteogenic potential than those from healthy controls [96]. This could be reversed by inhibiting BMP-2 or Smad1/5/8 pathway molecules [96]. In another study, osteogenesis in AS fibroblasts could be downregulated by inhibiting matrix metallopeptidase-2 (MMP-2) which acts by downregulating BMP2, Smad1/5/8, and Smad 4 [97]. Similarly, in supraspinous ligament fibroblasts, BMP2 and TGF-β1 overexpression significantly activated Smad signaling, which upregulated the expression of Runx2 to induce osteogenesis. Knockdown of the BMP and TGF receptor TβRIII in these fibroblasts, was able to reverse this effect [98]. Lastly, miR-214-3p was found to be downregulated in AS fibroblasts [99]. Overexpression of this microRNA led to the inhibition of alkaline phosphatase activity and calcium nodule formation in culture. This study showed that miR-214-3p inhibits BMP-2 and blocks Smad signaling to prevent fibroblast osteogenic differentiation [99].
HLA-B27 and NBF
A recent study highlights the potential contribution of HLA-B*27 to the development of NBF in axSpA [100]. However, the specific role of HLA-B*27 in NBF remains controversial [55, 101,102,103]. In an experimental animal model, HLA-B*27 has been shown to have no significant role in either chondrogenesis or osteoblastogenesis in CAIA models of arthritis [104]. Furthermore, in vitro experiments in models of chondrogenesis (ATDC5), osteogenesis (human periosteal derived cells) and endochondral ossification (lim bud cells) also showed no significant difference between HLA-B*27 transduced cells and controls [104]. Contrastingly, in human AS MSCs isolated from the entheses, HLA-B*27 misfolding was shown to activate the UPR inositol-requiring 1 (IRE1)/spliced X-box–binding protein 1 (sXBP1) pathway [105••]. This was shown to subsequently upregulate the expression of tissue non-specific alkaline phosphate (TNAP), which enhances mineralization by hydrolyzing anti-mineral factor pyrophosphate into inorganic phosphate. Inhibiting TNAP or pathway molecules ameliorated matrix mineralization by MSCs. Furthermore, bone specific TNAP (BAP) was shown to be significantly upregulated in AS serum and an independent predictor of radiographic progression [105••]. Therefore, it is possible that targeting this pathway could be a potential therapeutic avenue for NBF in AS (Fig. 2).
Potential mechanisms of new bone formation (NBF) in axial spondyloarthritis (axSpA). Mechanical stress in the joints leads to pro-inflammatory processes in the tendons and ligaments through tenocyte cell death. This can recruit immune cells (e.g., monocytes and T cells) into the inflamed tissues and local mesenchymal stem cells (MSCs) directly differentiate into bone forming osteoblasts or chondrocytes. During the process of endochondral ossification, chondrocytes recruit TGFβ-secreting osteoclasts, which in turn promotes osteoblast-mediated NBF through various signaling pathways and microRNA regulation. CaSR, calcium sensing receptor; tmTNF, transmembrane tumor necrosis factor; Wnt, wingless related integration site; BMP2, bone morphogenic protein 2; TNAP, tissue non-specific alkaline phosphatase; ANKH, ankylosis progressive homolog; MSC, mesenchymal stem cells; TGFβ, transforming growth factor beta; MIF, macrophage migration inhibitory factor; TNFα, tumor necrosis factor alpha; DKK-1, Dickkopf-related protein 1; MMP2, matrix metallopeptidase 2; UPR, unfolded protein response. The figure was created with BioRender (BioRender.com)
Future Directions
Although recent studies including both human ex vivo and experimental animal models have revealed that genetic factors combined with environmental factors and gut dysbiosis appear to activate immune response leading to chronic inflammation in axSpA, there are still many questions that remain unresolved. The exact role of HLA-B*27 in the pathogenesis of axSpA needs to be refined. Specific immune cell populations responsible for disease initiation and progression in spinal tissues of axSpA patients remain elusive. In addition, the gut-joint axis seems to be critical in the pathogenesis of axSpA, yet immune cells migrating from the gut to the joint in humans has not been defined. Endochondral ossification is a critical process during the development of NBF in axSpA, and several regulatory factors have been identified; however, the complex regulatory network is still unclear. Moreover, newly identified therapeutic targets need to be validated for efficacy and safety in different pre-clinical animal models prior to clinical trials. To better delineate the pathogenesis and sequence of events in axSpA, future studies on exploring specific roles of genetic associations, animal and human ex vivo studies, will be warranted.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
van der Linden S, Valkenburg HA, Cats A. Evaluation of diagnostic criteria for ankylosing spondylitis. A proposal for modification of the New York criteria. Arthritis Rheum. 1984;27:361–8.
Nakamura A, Haroon N. Recent updates in the immunopathology of type 3 immunity-mediated enthesitis. Curr Rheumatol Rep. 2021;23:31. https://doi.org/10.1007/s11926-021-00995-y.
de Blecourt J, Polman A, de Blecourt-Meindersma T. Hereditary factors in rheumatoid arthritis and ankylosing spondylitis. Ann Rheum Dis. 1961;20:215–20.
Brown MA, Kennedy LG, MacGregor AJ, Darke C, Duncan E, Shatford JL, et al. Susceptibility to ankylosing spondylitis in twins: the role of genes, HLA, and the environment. Arthritis Rheum. 1997;40:1823–8.
Brewerton DA, Hart FD, Nicholls A, Caffrey M, James DC, Sturrock RD. Ankylosing spondylitis and HL-A 27. Lancet. 1973;1:904–7.
Ellinghaus D, Jostins L, Spain SL, Cortes A, Bethune J, Han B, et al. Analysis of five chronic inflammatory diseases identifies 27 new associations and highlights disease-specific patterns at shared loci. Nat Genet. 2016;48:510–8.
Kopplin LJ, Mount G, Suhler EB. Review for disease of the year: epidemiology of HLA-B27 associated ocular disorderS. Ocul Immunol Inflamm. 2016;24:470–5.
Brown MA, Pile KD, Kennedy LG, Calin A, Darke C, Bell J, et al. HLA class I associations of ankylosing spondylitis in the white population in the United Kingdom. Ann Rheum Dis. 1996;55:268–70.
Luo F, Zhao Z, Zhang J, Leng J. Comparison of HLA-B*27 subtypes between Chinese patients with ankylosing spondylitis and non-ankylosing spondylitis carriers. J Int Med Res. 2019;47:3171–8.
Yang M, Xu M, Pan X, Hu Z, Li Q, Wei Y, et al. Epidemiological comparison of clinical manifestations according to HLA-B*27 carrier status of Chinese ankylosing spondylitis patients. Tissue Antigens. 2013;82:338–43.
Glatigny S, Fert I, Blaton MA, Lories RJ, Araujo LM, Chiocchia G, et al. Proinflammatory Th17 cells are expanded and induced by dendritic cells in spondylarthritis-prone HLA-B27-transgenic rats. Arthritis Rheum. 2012;64:110–20.
DeLay ML, Turner MJ, Klenk EI, Smith JA, Sowders DP, Colbert RA. HLA-B27 misfolding and the unfolded protein response augment interleukin-23 production and are associated with Th17 activation in transgenic rats. Arthritis Rheum. 2009;60:2633–43.
Milia AF, Ibba-Manneschi L, Manetti M, Benelli G, Messerini L, Matucci-Cerinic M. HLA-B27 transgenic rat: an animal model mimicking gut and joint involvement in human spondyloarthritides. Ann N Y Acad Sci. 2009;1173:570–4.
Khare SD, Luthra HS, David CS. Spontaneous inflammatory arthritis in HLA-B27 transgenic mice lacking beta 2-microglobulin: a model of human spondyloarthropathies. J Exp Med. 1995;182:1153–8.
Stam NJ, Spits H, Ploegh HL. Monoclonal antibodies raised against denatured HLA-B locus heavy chains permit biochemical characterization of certain HLA-C locus products. J Immunol. 1986;137:2299–306.
Braem K, Lories RJ. Insights into the pathophysiology of ankylosing spondylitis: contributions from animal models. Joint Bone Spine. 2012;79:243–8.
Nakamura A, Boroojeni SF, Haroon N. Aberrant antigen processing and presentation: key pathogenic factors leading to immune activation in Ankylosing spondylitis. Semin Immunopathol. 2021;43:245–53.
•• Yang X, Garner LI, Zvyagin I V, Paley MA, Komech EA, Jude KM, et al. Autoimmunity-associated T cell receptors recognize HLA-B*27-bound peptides. Nature. 2022;612: 771–7. (This study identified a subset of pathogenic CD8 TCRs with a shared alpha chain that was expanded in the joints in axSpA and AUU suggesting that pathogenic peptides presented by HLA-B27 may be disease inducing.)
Burton PR, Clayton DG, Cardon LR, Craddock N, Deloukas P, Duncanson A, et al. Association scan of 14,500 nonsynonymous SNPs in four diseases identifies autoimmunity variants. Nat Genet. 2007;39:1329–37.
Haroon N, Tsui FW, Uchanska-Ziegler B, Ziegler A, Inman RD. Endoplasmic reticulum aminopeptidase 1 (ERAP1) exhibits functionally significant interaction with HLA-B27 and relates to subtype specificity in ankylosing spondylitis. Ann Rheum Dis. 2012;71:589–95.
Tran TM, Hong S, Edwan JH, Colbert RA. ERAP1 reduces accumulation of aberrant and disulfide-linked forms of HLA-B27 on the cell surface. Mol Immunol. 2016;74:10–7. https://doi.org/10.1016/j.molimm.2016.04.002.
Chen L, Ridley A, Hammitzsch A, Al-Mossawi MH, Bunting H, Georgiadis D, et al. Silencing or inhibition of endoplasmic reticulum aminopeptidase 1 (ERAP1) suppresses free heavy chain expression and Th17 responses in ankylosing spondylitis. Ann Rheum Dis. 2016;75:916–23.
Zhang Z, Ciccia F, Zeng F, Guggino G, Yee K, Abdullah H, et al. Brief Report: Functional Interaction of Endoplasmic Reticulum Aminopeptidase 2 and HLA-B27 Activates the Unfolded Protein Response. Arthritis Rheumatol. 2017;69:1009–15.
Mielants H, Veys EM, Goemaere S, Goethals K, Cuvelier C, De Vos M. Gut inflammation in the spondyloarthropathies: clinical, radiologic, biologic and genetic features in relation to the type of histology. A prospective study J Rheumatol. 1991;18:1542–51.
Asquith M, Sternes PR, Costello M-E, Karstens L, Diamond S, Martin TM, et al. HLA alleles associated with risk of ankylosing spondylitis and rheumatoid arthritis influence the gut microbiome. Arthritis Rheumatol. 2019;71:1642–50.
Breban M, Tap J, Leboime A, Said-Nahal R, Langella P, Chiocchia G, et al. Faecal microbiota study reveals specific dysbiosis in spondyloarthritis. Ann Rheum Dis. 2017;76:1614–22.
Lin P, Bach M, Asquith M, Lee AY, Akileswaran L, Stauffer P, et al. HLA-B27 and human β2-microglobulin affect the gut microbiota of transgenic rats. PLoS ONE. 2014;9:e105684. https://doi.org/10.1371/journal.pone.0105684.
Mousa WK, Chehadeh F, Husband S. Microbial dysbiosis in the gut drives systemic autoimmune diseases. Front Immunol. 2022;13:906258. https://doi.org/10.3389/fimmu.2022.906258.
Ruutu M, Thomas G, Steck R, Degli-Esposti MA, Zinkernagel MS, Alexander K, et al. beta-glucan triggers spondylarthritis and Crohn’s disease-like ileitis in SKG mice. Arthritis Rheum. 2012;64:2211–22.
• Watad A, Rowe H, Russell T, Zhou Q, Anderson LK, Khan A, et al. Normal human enthesis harbours conventional CD4+ and CD8+ T cells with regulatory features and inducible IL-17A and TNF expression. Ann Rheum Dis. 2020;79:1044–1054. (This study shows that conventional CD4+ and CD8+ T cells exist in human axial entheses and have an ability to produce IL-17A and TNF.)
••Cuthbert RJ, Watad A, Fragkakis EM, Dunsmuir R, Loughenbury P, Khan A, et al. Evidence that tissue resident human enthesis γδT-cells can produce IL-17A independently of IL-23R transcript expression. Ann Rheum Dis. 2019;78:1559–65. (This study provides the first evidence of IL-17 producing γδ T cells independent of IL-23 in human axial entheses, which may be the reason for the ineffectiveness of IL-23 monoclonal antibodies in patients with ankylosing spondylitis.)
Cuthbert RJ, Fragkakis EM, Dunsmuir R, Li Z, Coles M, Marzo-Ortega H, et al. Brief report: group 3 innate lymphoid cells in human enthesis. Arthritis Rheumatol. 2017;69:1816–22.
Reinhardt A, Yevsa T, Worbs T, Lienenklaus S, Sandrock I, Oberdörfer L, et al. Interleukin-23-dependent γ/δ T cells produce interleukin-17 and accumulate in the enthesis, aortic valve, and ciliary body in mice. Arthritis Rheumatol. 2016;68:2476–86.
••. Viladomiu M, Kivolowitz C, Abdulhamid A, Dogan B, Victorio D, Castellanos JG, et al. IgA-coated E. coli enriched in Crohn’s disease spondyloarthritis promote T(H)17-dependent inflammation. Sci Transl Med. 2017; 9:eaaf9655. https://doi.org/10.1126/scitranslmed.aaf9655. (This study found an abundant IgA-coated Escherichia coli (E. coli) in Crohn’s disease (CD)-SpA patients, and the E. coli were similar in genotype and phenotype to an adherent-invasive E. coli (AIEC) pathotype. CD-SpA-derived AIEC induced systemic Th17 immunity and promoted joint inflammation.)
Franssen MJ, van de Putte LB, Gribnau FW. IgA serum levels and disease activity in ankylosing spondylitis: a prospective study. Ann Rheum Dis. 1985;44:766–71.
Salas-Cuestas F, Bautista-Molano W, Bello-Gualtero JM, Arias I, Castillo DM, Chila-Moreno L, et al. Higher levels of secretory IgA are associated with low disease activity index in patients with reactive arthritis and undifferentiated spondyloarthritis. Front Immunol. 2017;8:476. https://doi.org/10.3389/fimmu.2017.00476.
Stoll ML, Kumar R, Morrow CD, Lefkowitz EJ, Cui X, Genin A, et al. Altered microbiota associated with abnormal humoral immune responses to commensal organisms in enthesitis-related arthritis. Arthritis Res Ther. 2014;16:486. https://doi.org/10.1186/s13075-014-0486-0.
••Tajik N, Frech M, Schulz O, Schälter F, Lucas S, Azizov V, et al. Targeting zonulin and intestinal epithelial barrier function to prevent onset of arthritis. Nat Commun. 2020;11:1995. https://doi.org/10.1038/s41467-020-15831-7. (The authors also showed that the increased permeability in the intestinal epithelium may be caused by increased expression of zonulin that induces impaired barrier function in arthritis patients and mouse models.)
Gran JT, Ostensen M, Husby G. A clinical comparison between males and females with ankylosing spondylitis. J Rheumatol. 1985;12:126–9.
Baumberger H, Khan M. SAT0417 Gradual progressive change to equal prevalence of ankylosing spondylitis among males and females in Switzerland: data from the Swiss ankylosing spondylitis society (SVMB). Poster Presentations. 2017;76:929. BMJ Publishing Group Ltd and European League Against Rheumatismhttps://doi.org/10.1136/annrheumdis-2017-eular.3961
Haroon NN, Paterson JM, Li P, Haroon N. Increasing proportion of female patients with ankylosing spondylitis: a population-based study of trends in the incidence and prevalence of AS. BMJ Open. 2014;4:e006634. https://doi.org/10.1136/bmjopen-2014-006634.
Sieper J, van der Heijde D. Review: Nonradiographic axial spondyloarthritis: new definition of an old disease? Arthritis Rheum. 2013;65:543–51.
Deminger A, Klingberg E, Geijer M, Göthlin J, Hedberg M, Rehnberg E, et al. A five-year prospective study of spinal radiographic progression and its predictors in men and women with ankylosing spondylitis. Arthritis Res Ther. 2018;20:162. https://doi.org/10.1186/s13075-018-1665-1.
Ward MM, Hendrey MR, Malley JD, Learch TJ, Davis JCJ, Reveille JD, et al. Clinical and immunogenetic prognostic factors for radiographic severity in ankylosing spondylitis. Arthritis Rheum. 2009;61:859–66.
Tournadre A, Pereira B, Lhoste A, Dubost JJ, Ristori JM, Claudepierre P, et al. Differences between women and men with recent-onset axial spondyloarthritis: results from a prospective multicenter French cohort. Arthritis Care Res (Hoboken). 2013;65:1482–9.
Mease PJ, McLean RR, Dube B, Liu M, Rebello S, Glynn M, et al. Comparison of men and women with axial spondyloarthritis in the US-based corrona psoriatic arthritis/spondyloarthritis registry. J Rheumatol. 2021;48:1528–36.
Gracey E, Yao Y, Green B, Qaiyum Z, Baglaenko Y, Lin A, et al. Sexual dimorphism in the Th17 Signature of ankylosing spondylitis. Arthritis Rheumatol. 2016;68:679–89.
Fish EN. The X-files in immunity: sex-based differences predispose immune responses. Nat Rev Immunol. 2008;8:737–44.
Mohamad N-V, Wong SK, Wan Hasan WN, Jolly JJ, Nur-Farhana MF, Ima-Nirwana S, et al. The relationship between circulating testosterone and inflammatory cytokines in men. Aging Male. 2019;22:129–40.
Kong W, Jefferies C, Learch TJ, Gan X, Zhu F, Zhang N, et al. Risk factors for spinal structural damage in a chinese cohort with ankylosing spondylitis. J Clin Rheumatol. 2022;28:e118–24. https://doi.org/10.1097/RHU.0000000000001658.
Videm V, Cortes A, Thomas R, Brown MA. Current smoking is associated with incident ankylosing spondylitis – the HUNT population-based Norwegian health study. J Rheumatol. 2014;41:2041–8.
Nikiphorou E, Ramiro S, Sepriano A, Ruyssen-Witrand A, Landewé RBM, van der Heijde D. Do smoking and socioeconomic factors influence imaging outcomes in axial spondyloarthritis? Five-year data from the DESIR cohort. Arthritis Rheumatol. 2020;72:1855–62.
Elolemy G, Hassan W, Nasr M, Baraka E. Hypovitaminosis D in patients with ankylosing spondylitis: frequency and consequences. Curr Rheumatol Rev. 2021;17:365–72.
Kolahi S, Khabbazi A, Kazemi N, Malek MA. Does vitamin D deficiency contribute to higher disease activity in patients with spondyloarthritis? Immunol Lett. 2019;212:1–5.
Nakamura A, Talukdar A, Nakamura S, Pathan E, Haroon N. Bone formation in axial spondyloarthritis: is disease modification possible? Best Pract Res Clin Rheumatol. 2019;33:101491. https://doi.org/10.1016/j.berh.2020.101491.
••Yu T, Zhang J, Zhu W, Wang X, Bai Y, Feng B, et al. Chondrogenesis mediates progression of ankylosing spondylitis through heterotopic ossification. Bone Res. 2021;9:19. https://doi.org/10.1038/s41413-021-00140-6. (This study shows that endochondral ossification is a critical process during NBF in AS spine and revealed pivotal regulators in this process.)
Cui H, Li Z, Chen S, Li X, Chen D, Wang J, et al. CXCL12/CXCR4-Rac1-mediated migration of osteogenic precursor cells contributes to pathological new bone formation in ankylosing spondylitis. Sci Adv. 2022;8:eabl8054 https://doi.org/10.1126/sciadv.abl8054
Li Z, Chen S, Cui H, Li X, Chen D, Hao W, et al. Tenascin-C-mediated suppression of extracellular matrix adhesion force promotes entheseal new bone formation through activation of Hippo signalling in ankylosing spondylitis. Ann Rheum Dis. 2021;80:891–902.
Gupta L, Bhattacharya S, Aggarwal A. Tenascin-C, a biomarker of disease activity in early ankylosing spondylitis. Clin Rheumatol. 2018;37:1401–5.
Li X, Chen S, Hu Z, Chen D, Wang J, Li Z, et al. Aberrant upregulation of CaSR promotes pathological new bone formation in ankylosing spondylitis. EMBO Mol Med. 2020;12:e12109 https://doi.org/10.15252/emmm.202012109
••Kaaij MH, van Tok MN, Blijdorp IC, Ambarus CA, Stock M, Pots D, et al. Transmembrane TNF drives osteoproliferative joint inflammation reminiscent of human spondyloarthritis. J Exp Med. 2020;217: e20200288 https://doi.org/10.1084/jem.20200288. (This study revealed the increased level of transmembrane TNF in the joint tissue of SpA patients compared to that of rheumatoid arthritis patients, which appears to facilitate TNF-driven osteo-proliferative changes in AS.)
Cambré I, Gaublomme D, Schryvers N, Lambrecht S, Lories R, Venken K, et al. Running promotes chronicity of arthritis by local modulation of complement activators and impairing T regulatory feedback loops. Ann Rheum Dis. 2019;78:787–95.
Jacques P, Lambrecht S, Verheugen E, Pauwels E, Kollias G, Armaka M, et al. Proof of concept: enthesitis and new bone formation in spondyloarthritis are driven by mechanical strain and stromal cells. Ann Rheum Dis. 2014;73:437–45.
Xie Z, Wang P, Li J, Li Y, Wang S, Wu X, et al. MCP1 triggers monocyte dysfunctions during abnormal osteogenic differentiation of mesenchymal stem cells in ankylosing spondylitis. J Mol Med (Berl). 2017;95:143–54.
Ding M, Guan T-J, Wei C-Y, Chen B-H. Identification of pathways significantly associated with spondyloarthropathy/ankylosing spondylitis using the sub-pathway method. Mol Med Rep. 2018;18:3825–33.
Chen S, Li Z, Chen D, Cui H, Wang J, Li Z, et al. Piezo1-mediated mechanotransduction promotes entheseal pathological new bone formation in ankylosing spondylitis. Ann Rheum Dis. 2022;82:533–45. https://doi.org/10.1136/ard-2022-223428.
Briolay A, El Jamal A, Arnolfo P, Le Goff B, Blanchard F, Magne D, et al. Enhanced BMP-2/BMP-4 ratio in patients with peripheral spondyloarthritis and in cytokine- and stretch-stimulated mouse chondrocytes. Arthritis Res Ther. 2020;22:234. https://doi.org/10.1186/s13075-020-02330-9.
Cambré I, Gaublomme D, Burssens A, Jacques P, Schryvers N, De Muynck A, et al. Mechanical strain determines the site-specific localization of inflammation and tissue damage in arthritis. Nat Commun. 2018;9:4613. https://doi.org/10.1038/s41467-018-06933-4.
van der Heijde D, Machado P, Braun J, Hermann K-GA, Baraliakos X, Hsu B, et al MRI inflammation at the vertebral unit only marginally predicts new syndesmophyte formation: a multilevel analysis in patients with ankylosing spondylitis. Ann Rheum Dis. 2012;71:369–73
Maksymowych WP, Morency N, Conner-Spady B, Lambert RG. Suppression of inflammation and effects on new bone formation in ankylosing spondylitis: evidence for a window of opportunity in disease modification. Ann Rheum Dis. 2013;72:23–8.
Chiowchanwisawakit P, Lambert RGW, Conner-Spady B, Maksymowych WP. Focal fat lesions at vertebral corners on magnetic resonance imaging predict the development of new syndesmophytes in ankylosing spondylitis. Arthritis Rheum. 2011;63:2215–25.
Chisălău BA, Crînguș L-I, Vreju FA, Pârvănescu CD, Firulescu SC, Dinescu Ștefan C, et al. New insights into IL-17/IL-23 signaling in ankylosing spondylitis (review). Exp Ther Med. 2020;20:3493–7.
Chen L, Wei X-Q, Evans B, Jiang W, Aeschlimann D. IL-23 promotes osteoclast formation by up-regulation of receptor activator of NF-kappaB (RANK) expression in myeloid precursor cells. Eur J Immunol. 2008;38:2845–54.
Song L, Tan J, Wang Z, Ding P, Tang Q, Xia M, et al. Interleukin-17A facilitates osteoclast differentiation and bone resorption via activation of autophagy in mouse bone marrow macrophages. Mol Med Rep. 2019;19:4743–52.
Shah M, Maroof A, Gikas P, Mittal G, Keen R, Baeten D, et al. Dual neutralisation of IL-17F and IL-17A with bimekizumab blocks inflammation-driven osteogenic differentiation of human periosteal cells. RMD Open. 2020;6:e001306. https://doi.org/10.1136/rmdopen-2020-001306.
Russell T, Watad A, Bridgewood C, Rowe H, Khan A, Rao A, et al. IL-17A and TNF modulate normal human spinal entheseal bone and soft tissue mesenchymal stem cell osteogenesis, adipogenesis, and stromal function. Cells. 2021;10:341. https://doi.org/10.3390/cells10020341.
Ye C, Zhang W, Hang K, Chen M, Hou W, Chen J, et al. Extracellular IL-37 promotes osteogenic differentiation of human bone marrow mesenchymal stem cells via activation of the PI3K/AKT signaling pathway. Cell Death Dis. 2019;10:753. https://doi.org/10.1038/s41419-019-1904-7.
•Ranganathan V, Ciccia F, Zeng F, Sari I, Guggino G, Muralitharan J, et al. Macrophage migration inhibitory factor induces inflammation and predicts spinal progression in ankylosing spondylitis. Arthritis Rheumatol. 2017;69:1796–1806. (This study shows elevated MIF levels in axSpA progressors vs. non-progressors and its role in new bone formation as well as inflammation.)
Xie W, Zhou L, Li S, Hui T, Chen D. Wnt/β-catenin signaling plays a key role in the development of spondyloarthritis. Ann N Y Acad Sci. 2016;1364:25–31.
Li X, Wang J, Zhan Z, Li S, Zheng Z, Wang T, et al. Inflammation intensity-dependent expression of osteoinductive Wnt proteins is critical for ectopic new bone formation in ankylosing spondylitis. Arthritis Rheumatol. 2018;70:1056–70.
Kwon S-R, Lim M-J, Suh C-H, Park S-G, Hong Y-S, Yoon B-Y, et al. Dickkopf-1 level is lower in patients with ankylosing spondylitis than in healthy people and is not influenced by anti-tumor necrosis factor therapy. Rheumatol Int. 2012;32:2523–7.
Appel H, Ruiz-Heiland G, Listing J, Zwerina J, Herrmann M, Mueller R, et al. Altered skeletal expression of sclerostin and its link to radiographic progression in ankylosing spondylitis. Arthritis Rheum. 2009;60:3257–62.
Wu M, Chen M, Ma Y, Yang J, Han R, Yuan Y, et al. Dickkopf-1 in ankylosing spondylitis: review and meta-analysis. Clin Chim Acta. 2018;481:177–83.
Saad CGS, Ribeiro ACM, Moraes JCB, Takayama L, Goncalves CR, Rodrigues MB, et al. Low sclerostin levels: a predictive marker of persistent inflammation in ankylosing spondylitis during anti-tumor necrosis factor therapy? Arthritis Res Ther. 2012;14:R216. https://doi.org/10.1186/ar4055.
Shi J, Ying H, Du J, Shen B. Serum sclerostin levels in patients with ankylosing spondylitis and rheumatoid arthritis: a systematic review and meta-analysis. Biomed Res Int. 2017;2017:9295313. https://doi.org/10.1155/2017/9295313.
He X, Dong Y. Ankylosis progressive homolog upregulation inhibits cell viability and mineralization during fibroblast ossification by regulating the Wnt/β-catenin signaling pathway. Mol Med Rep. 2020;22:4551–60.
Qin X, Zhu B, Jiang T, Tan J, Wu Z, Yuan Z, et al. miR-17-5p regulates heterotopic ossification by targeting ANKH in ankylosing spondylitis. Mol Ther Nucleic Acids. 2019;18:696–707.
Ma S, Wang D-D, Ma C-Y, Zhang Y-D. MicroRNA-96 promotes osteoblast differentiation and bone formation in ankylosing spondylitis mice through activating the Wnt signaling pathway by binding to SOST. J Cell Biochem. 2019;120:15429–42.
Huang J, Song G, Yin Z, Fu Z, Zhang L. Altered expression of microRNAs targeting Dkk-1 in peripheral blood mononuclear cells of patients with ankylosing spondylitis. Cent Eur J Immunol. 2019;44:59–64.
Huang J, Song G, Yin Z, Luo X, Ye Z. Elevated miR-29a expression is not correlated with disease activity index in PBMCs of patients with ankylosing spondylitis. Mod Rheumatol. 2014;24:331–4.
Zhang F, Cao K, Du G, Zhang Q, Yin Z. miR-29a promotes osteoblast proliferation by downregulating DKK-1 expression and activating Wnt/β-catenin signaling pathway. Adv Clin Exp Med. 2019;28:1293–300.
Carter S, Braem K, Lories RJ. The role of bone morphogenetic proteins in ankylosing spondylitis. Ther Adv Musculoskelet Dis. 2012;4:293–9.
Chen H-A, Chen C-H, Lin Y-J, Chen P-C, Chen W-S, Lu C-L, et al. Association of bone morphogenetic proteins with spinal fusion in ankylosing spondylitis. J Rheumatol. 2010;37:2126–32.
Yang J, Xu S, Chen M, Yuan Y, Zhang X, Ma Y, et al. Serum sclerostin and bone morphogenetic protein-2 levels in patients with ankylosing spondylitis: a meta-analysis. Calcif Tissue Int. 2019;105:37–50.
Liao H-T, Lin Y-F, Tsai C-Y, Chou T-C. Bone morphogenetic proteins and Dickkopf-1 in ankylosing spondylitis. Scand J Rheumatol. 2018;47:56–61.
Zheng G, Xie Z, Wang P, Li J, Li M, Cen S, et al. Enhanced osteogenic differentiation of mesenchymal stem cells in ankylosing spondylitis: a study based on a three-dimensional biomimetic environment. Cell Death Dis. 2019;10:350.
Yuan B, Wu Z. MMP-2 silencing reduces the osteogenic transformation of fibroblasts by inhibiting the activation of the BMP/Smad pathway in ankylosing spondylitis. Oncol Lett. 2018;15:3281–6.
Zhang Y, Chen W-G, Yang S-Z, Qiu H, Hu X, Qiu Y-Y, et al. Up-regulation of TβRIII facilitates the osteogenesis of supraspinous ligament-derived fibroblasts from patients with ankylosing spondylitis. J Cell Mol Med. 2021;25:1613–23.
Ding L, Yin Y, Hou Y, Jiang H, Zhang J, Dai Z, et al. microRNA-214-3p suppresses ankylosing spondylitis fibroblast osteogenesis via BMP-TGFβ axis and BMP2. Front Endocrinol (Lausanne). 2020;11:609753. https://doi.org/10.3389/fendo.2020.609753.
Coates LC, Baraliakos X, Blanco FJ, Blanco-Morales EA, Braun J, Chandran V, et al. The phenotype of axial spondyloarthritis: is it dependent on HLA-B27 status? Arthritis Care Res (Hoboken). 2021;73:856–60.
Ramiro S, Stolwijk C, van Tubergen A, van der Heijde D, Dougados M, van den Bosch F, et al. Evolution of radiographic damage in ankylosing spondylitis: a 12 year prospective follow-up of the OASIS study. Ann Rheum Dis. 2015;74:52–9.
Lories RJ, Haroon N. Bone formation in axial spondyloarthritis. Best Pract Res Clin Rheumatol. 2014;28:765–77.
van Tubergen A, Ramiro S, van der Heijde D, Dougados M, Mielants H, Landewé R. Development of new syndesmophytes and bridges in ankylosing spondylitis and their predictors: a longitudinal study. Ann Rheum Dis. 2012;71:518–23.
Neerinckx B, Kollnberger S, Shaw J, Lories R. No evidence for a direct role of HLA-B27 in pathological bone formation in axial SpA. RMD Open. 2017;3:e000451. https://doi.org/10.1136/rmdopen-2017-000451.
••Liu C-H, Raj S, Chen C-H, Hung K-H, Chou C-T, Chen I-H, et al. HLA-B27-mediated activation of TNAP phosphatase promotes pathogenic syndesmophyte formation in ankylosing spondylitis. J Clin Invest. 2019;129:5357–73. (This study suggests that HLA-B*27 is involved in the development of NBF associated with AS through the activation of TNAP phosphatase.)
Funding
This article was supported by grants to NH from the Canadian Institute of Health Research (CIHR) and Arthritis Society (Canada). SA is a recipient of the Queen Elizabeth II/Edward Dunlop Foundation Graduate Scholarships in Science and Technology (University of Toronto). AN is a recipient of CIHR fellowship, Spondyloarthritis Research and Treatment Network (SPARTAN) fellowship, Spondyloarthritis Research Consortium of Canada (SPARCC) fellowship, Edward Christie Stevens fellowship, S. Fenwick Research fellowship, and Krembil Research Institute fellowship (Canada). Figures 1 and 2 were created with BioRender (BioRender.com).
Author information
Authors and Affiliations
Contributions
A.S., A.N., and N.H. wrote the main manuscript text and A.S. and A.N. prepared figures 1-2. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
A.N. has received a speaking honorarium from AbbVie and Novartis. N.H. has received consulting fees from Abbvie, Amgen, Eli Lilly, Janssen, Merck, Novartis and UCB.
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This manuscript is published thanks to collaboration with the SPARTAN group.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Srinath, A., Nakamura, A. & Haroon, N. Sequence of Events in the Pathogenesis of Axial Spondyloarthritis: A Current Review—2023 SPARTAN Meeting Proceedings. Curr Rheumatol Rep 26, 133–143 (2024). https://doi.org/10.1007/s11926-024-01136-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11926-024-01136-x