Abstract
Purpose of Review
The goal of this review is to summarize recent findings on marrow adipose tissue (MAT) function and to discuss the possibility of targeting MAT for therapeutic purposes.
Recent Findings
MAT is characterized with high heterogeneity which may suggest both that marrow adipocytes originate from multiple different progenitors and/or their phenotype is determined by skeletal location and environmental cues. Close relationship to osteoblasts and heterogeneity suggests that MAT consists of cells representing spectrum of phenotypes ranging from lipid-filled adipocytes to pre-osteoblasts. We propose a term of adiposteoblast for describing phenotypic spectrum of MAT. Manipulating with MAT activity in diseases where impairment in energy metabolism correlates with bone functional deficit, such as aging and diabetes, may be beneficial for both. Paracrine activities of MAT might be considered for treatment of bone diseases.
Summary
MAT has unrecognized potential, either beneficial or detrimental, to regulate bone homeostasis in physiological and pathological conditions. More research is required to harness this potential for therapeutic purposes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Until two decades ago, marrow cells filled with lipids were considered an obscure type of cells, often disregarded as adipocytes and referred to cells of unknown origin and function. Recent appreciation of adipocyte endocrine function shed a new spotlight on marrow adipocytes and their possible endocrine/paracrine function supporting skeletal and hematopoietic processes in marrow environment.
Adipocytes reside in the bone marrow of all mammals and their number increases during both skeletal growth, which is associated with bone acquisition and sexual development, and aging, which is associated with bone loss and decline in gonadal activity. Initially, an interest in marrow adipose tissue (MAT) was focused on anatomical location and expansion in marrow cavity as a result of involution of hematopoiesis and/or a response to temperature gradient [1]. From pathologic perspective, MAT was considered as a source of fat embolism accompanying severe anemia and fractures [2]. The major breakthrough consisted a demonstration in 1990s that marrow adipocytes originate from the same mesenchymal precursor as osteoblasts [3]. This led to a hypothesis of inverse relationship between osteoblast and adipocyte differentiation; so one type of cell would differentiate from the same precursor at the expense of other type of cell. This idea has been extensively tested in different cellular and animal models, and led to the current hypothesis that MAT is a heterogeneous tissue which constitutes fat-laden cells of various origins including common progenitors with osteoblasts (reviewed in [4]). On the functional level, MAT heterogeneity is reflected by diverse effects on bone which may be either beneficial or detrimental for bone homeostasis. This review speculates on possibility of harnessing MAT potential to treat bone diseases.
Marrow Adipocyte Origin
There is a certain controversy on marrow adipocyte origin with some models supporting shared progenitor with osteoblasts, while others negating it. It appears that both cell lineages originate from a common Myf5-negative progenitor and determination of their fate is under control of retinoblastoma protein (pRB) [5]. Myf5-negative progenitor is also common for peripheral “white” and “beige” adipocytes, with exception of “brown” thermogenic adipocytes which are Myf5-positive and related to muscle cells. Recent analysis by Ambrosi et al. provides the most comprehensive up-to-date profiling of marrow adipocytes [6]. It has been demonstrated that marrow adipocytes are derived from cells negative for both hematopoietic CD45 and endothelial CD31 markers but positive for mesenchymal Sca1 marker. These CD45−CD31−Sca1+ mesenchymal stroma cells have high potential for adipocytic differentiation and rather limited potential for osteochondrogenic differentiation. In contrast, CD45−CD31−Sca1− cells have relatively low potential to differentiate to adipocytes but high to differentiate to osteoblasts. Interestingly, a subpopulation of CD45−CD31−Sca1+ cells which are also positive for CD24 and PDGFRα has characteristics of multipotential cells signified by high proliferation capability and robust differentiation toward adipocytic, osteoblastic, and chondrocytic lineages [6]. The origin of marrow adipocytes has been also studied by lineage tracing using the mTomato/eGFP “flipping” system [7]. Thus, crossing mice carrying mTomato/eGFP with mice carrying Cre recombinase under lineage-specific control permits switch from red to green fluorescence only in cells where studied gene has been transcriptionally active at any given time point during development. Use of this system allowed for confirmation that marrow adipocytes have non-hematopoietic origin and finding that MAT consists of cells which trace to Myf5− and Osterix+ precursors [7]. Moreover, it has been shown that, in contrast to white adipose tissue (WAT) and brown adipose tissue (BAT), only a fraction of marrow adipocytes is PDGFRα+ suggesting that they may originate from multiple precursors.
Other studies demonstrated that marrow adipocytes are derived from leptin receptor-positive (LepR+) skeletal stem cells which have also potential to differentiate to osteoblasts and can support hematopoietic niche by producing stem cell factor (SCF) [8, 9]. In addition, it has been shown that MAT contains a population of adipocytes derived from pair-related homeobox-positive (Prx1+) and parathyroid hormone receptor-positive (PTHr1+) osteoblastic progenitors which have a capacity to secrete RANKL cytokine, therefore supporting the role of MAT in regulation of bone resorption and bone remodeling [10]. In contrast to the above, studies by Worthley et al. showed that marrow adipocytes do not share the same musculoskeletal ancestor as osteoblasts, chondrocytes, and muscle cells by demonstrating that Gremlin 1-positive mesenchymal progenitors can differentiate into the above lineages but not into adipocytes [11]. Our profiling of marrow adipocyte in respect to expression of gene markers characteristic for white, brown, and beige adipocytes confirmed their unique phenotype [12•]. Marrow adipocytes do not express BAT-exclusive Zic1 marker, WAT-exclusive Tcf21 marker, and beige-specific Tmem26 marker, suggesting different phenotypes from peripheral white, brown, and beige adipocytes.
Such diverse phenotype suggests that either marrow adipocytes are derived from several different lineage-specific precursors, some of them closely related to osteoblasts or extramedullary adipocytes, or they have a common origin but are highly plastic and their terminal phenotype depends on skeletal location which determines their function.
MAT Function
Extramedullar fat is distributed throughout the body in depots which serve different functions including storing and releasing energy through the process of lipogenesis and lipolysis. However, with discovery that adipocytes produce specific hormones called adipokines, it became well appreciated that adipose tissue is also an endocrine organ regulating systemic energy metabolism. Both functions, lipid metabolism and endocrine activities, are characteristic for extramedullary adipocytes.
MAT is present in different skeletal sites including those with active bone remodeling and hematopoiesis and those where these processes are absent. In human red marrow with active hematopoiesis, marrow adipocytes constitute up to 45%, while in yellow marrow, hematopoiesis is absent up to 90% of cellular component. These proportions are different in rodents, but in general, adipocytes are less frequent in epiphysis/metaphysis of a long bone (e.g., proximal tibia, distal femur) where trabecular bone remodeling and hematopoiesis are juxtaposed, whereas they are densely packed and resemble yellow marrow in distal tibia and caudal vertebra where hematopoiesis and bone remodeling are absent. These differences in distribution correlate with different phenotypic profiles of MAT. As showed by Scheller et al., MAT located in the proximal tibia, referred by authors to reformed or rMAT, differs from MAT located in the distal part, referred to constitutive or cMAT, with regard to fatty acid composition, plasticity, and response to environmental cues [13••]. Lower content of unsaturated fatty acids in rMAT as compared to that in cMAT suggests different metabolic functions of these two MAT depots. Moreover, rMAT, but not cMAT, responds to the cold exposure with decrease in volume and to caloric restriction with increase in volume [13••]. These findings indicate that MAT differs by skeletal location; however, the question still remains whether these differences have any functional meaning or are just a mere response to environmental stimuli such as temperature gradient or blood perfusion.
Some of the clues may come from our studies correlating MAT metabolic phenotype and bone mass. First, it has been showed that MAT has mixed phenotype comprising WAT-like and BAT-like, and that BAT-like phenotype is compromised with aging and diabetes despite overall expansion in MAT volume [14]. Second, that MAT in the proximal tibia (pMAT) is characterized with higher expression of beige fat markers, including Prdm16, Dio2, and Tbx1, as compared to MAT located in the distal part (dMAT) in both males and females [12•]. Remarkably, pMAT in males has higher expression of beige markers as compared to that in females, which correlates with males’ higher trabecular bone mass in the same location. Third, ovariectomy increases volume of pMAT but attenuates its beige-like phenotype. Interestingly, an increase in pMAT volume with estrogen deficiency correlates positively with expansion of epididymal WAT suggesting that both fat depots are under suppressive control of estrogen. Indeed, estrogen replacement decreases MAT and WAT volume in mice and humans [15, 16]. In contrast, orchiectomy modestly increases MAT volume despite the wasting effect on peripheral fat including, epididymal WAT, implying that androgens have different effects on MAT and WAT. These characteristics indicate that there is a correlation between MAT phenotype and bone mass; however, it is unclear whether this relationship is functional or casual.
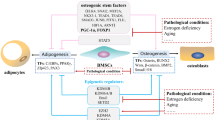
Although we refer to beige-like phenotype, however, it is upon discussion whether beige-like MAT acquires thermogenic function, which is characteristic for peripheral beige adipocytes. In regard to this and diverse origin, it is probably a scholastic exercise to follow “color-like” key applied for peripheral fat in naming MAT. Marrow adipocytes’ close relationship to osteoblasts and their heterogeneity in respect to lineage-specific markers or metabolic phenotype may suggest that MAT consists of cells representing spectrum of different phenotypes ranging from lipid-filled adipocytes to pre-osteoblasts. In the view of this hypothesis, we propose a term of adiposteoblast for describing phenotypic spectrum of MAT (Fig. 1).
MAT Role in Regulation of Bone Mass
It is well documented that increase in MAT volume correlates with bone loss and fractures during aging and in diabetes, as well as a result of prolonged immobilization, malnutrition, and medications such as thiazolidinediones or glucocorticoids [17, 18]. This negative correlation between MAT and bone health encompasses reciprocal inverse relationship between MSCs differentiation toward osteoblasts and adipocytes, and MAT lipotoxic and pro-inflammatory effect including production of cytokines supporting bone resorption [19].
Nevertheless, we have demonstrated in several animal models that MAT which acquire beige-like characteristics as a result of either genetic or pharmacologic manipulation has a positive effect on bone mass. These manipulations include adipocyte-specific overexpression of FoxC2 transcription factor [20•] or manipulation with PPARγ transcriptional activity by either pharmacological use of selective agonists such as telmisartan [21, 22•] or by manipulation with protein phosphatase 5 (PP5) activity which controls phosphorylation and activity of both PPARγ and RUNX2 proteins [23•].
FoxC2, which belongs to a family of winged transcription factors, promotes brown/beige fat development by sensitizing adipocytic cells to the β-adrenergic cAMP-protein kinase A pathway and by stimulating mitochondrial biogenesis and their futile metabolism [24]. Mice overexpressing FoxC2 under the control of adipocyte-specific enhancer to aP2/Fabp4 gene have high bone mass and are resistant to obesity and glucose intolerance. Peripheral WAT and bone MAT have beige-like phenotype signified by increased expression of Ucp1, Dio2, and Prdm16 gene markers, and the secretome of these adipocytes, which includes WNT10b, IGF-1, IGFBP2, and BMP4 proteins, has pro-osteoblastic activity as demonstrated in co-culture experiments [20•].
Similarly, selective modulators of PPARγ activities, specifically those which protect Ser112 phosphorylation, induce beige-like profile in MAT and in peripheral WAT and have either neutral or positive effect on bone, in contrast to full agonists thiazolidinediones (TZDs) which dephosphorylate Ser112 and have a negative effect on bone [21, 22•, 25, 26]. As evidenced in humans and animals, administration of antidiabetic TZDs, rosiglitazone or pioglitazone, leads to bone loss and fractures partly due to suppressive effect on osteoblast differentiation and bone formation associated with extensive expansion of MAT [25, 27]. In contrast, PPARγ partial agonist telmisartan or inverse agonist SR10171 induces insulin-sensitizing activity associated with dephosphorylation of Ser273, but does not induce pro-adipocytic activity associated with dephosphorylation of Ser112 [21]. Mice receiving these modulators either do not loose bone or gain bone mass and this correlates with increased expression of beige gene markers in MAT [21, 22•].
Phosphorylation of Ser112 is under the control of PP5 phosphatase. Mice deficient in PP5 have phenotype almost identical as mice with the adipocyte-specific overexpression of FoxC2. They are protected from diet-induced obesity and glucose intolerance and have high bone mass [23•]. Most importantly, MAT and peripheral WAT of PP5-deficient mice acquire beige-like phenotype with increased expression of Wnt10b, Igf-1, Igfbp2, and Bmp4 and pro-osteoblastic secretome, as evidenced in co-culture experiments [23•].
Can MAT Be Targeted to Treat Bone Diseases?
Two options can be considered in targeting MAT to treat bone diseases. First option follows a belief that “fat loss is bone gain,” which is based on reciprocal and inverse relationship of osteoblast and adipocyte differentiation from a common mesenchymal precursor. Second option contemplates a possibility of changing MAT phenotype into the one supporting bone formation and bone remodeling.
Hormonal and chemical therapies can be discussed in regard to suppression of adipogenesis as a way to boost osteoanabolic effect to treat disorders where increase in MAT volume correlates with bone loss. Several approved hormonal therapies, among them with estrogen, PTH, and vitamin D, regulate both bone remodeling and marrow adipocyte differentiation. Although the main target of these therapies is activity of osteoblast and/or osteoclast, their suppressive effect on MAT may contribute to an increase in osteoblast number and quashing of lipotoxic and pro-inflammatory marrow microenvironment. Estrogen antagonizes pro-adipocytic activity of PPARγ probably through competition for the same coactivators [28], and beneficial effect of estrogen therapy on postmenopausal osteoporosis is associated with decreased MAT volume in affected skeletal sites [16]. Besides regulation of systemic calcium and phosphate homeostasis, PTH and vitamin D have a direct effect on MSC differentiation. PTH treatment reduces MAT volume in mice and deletion of PTH receptor 1 in Prx-positive mesenchymal cells increases MAT and renders it unresponsive to the PTH treatment [10]. One of the proposed mechanisms consists of downregulation of Zfp467 factor which is critical for MSC commitment toward adipogenic lineage [10]. Interestingly, in postmenopausal osteopenic women, teriparatide therapy lowers marrow adiposity without altering of abdominal fat accumulation [29]. Moreover, in males with idiopathic osteoporosis, intermittent PTH has been reported to reduce marrow adipocyte number without changing adipocyte size [10]. Less clear is a role in adipogenesis of vitamin D and its receptor which belongs to the same family of nuclear receptors and transcription factors as PPARγ and uses the same heterogenic partner retinoid X receptor (RXR). Vitamin D suppresses the expression of C/EBPα, PPARγ, and FABP4 and has a protective role toward Wnt signaling pathway in 3T3-L1 cells [30, 31]. Similarly, vitamin D reduces lipid accumulation and inhibits adipocyte differentiation and reverses TZD-induced adipogenesis in murine marrow stroma cells [32]. In contrast, vitamin D in a dose-dependent manner induces adipocyte differentiation in human MSCs [33], and however does not have an effect on body weight and body composition when used as a diet supplementation [34]. These discrepancies between humans and mice may be attributed to the differences in metabolism and function of vitamin D.
Among compounds which reduce adipogenesis, PPARγ antagonists and inverse agonists can be considered. Examples of such therapies include bisphenol-A-diglycidyl ether (BADGE), a synthetic PPARγ antagonist [35], and selective artificial and natural PPARγ modulators, among them the aforementioned SR10171 and oleuropein, a polyphenol found profusely in olive tree products [36]. Treatment of mice with BADGE reduced MAT volume and increased bone mass and quality, and circulating levels of bone formation markers [37]. Importantly, inhibiting PPARγ activity with BADGE increased vitamin D receptor (VDR) expression suggesting a possibility that inhibition of PPARγ aids in osteogenic response of bone to vitamin D [37]. Similarly, oleuropein inhibits PPARγ expression and adipogenesis in human MSCs and enhances their differentiation into osteoblast [36].
One of the unique features of MAT is simultaneous involvement in the regulation of energy metabolism and bone homeostasis which may, at least in part, explain skeletal response to pathologic changes in energy balance such as obesity, diabetes, caloric restriction, and anorexia nervosa. Bone metabolism and energy metabolism rely on the same hormonal signaling. For example, efferent signaling from periphery to bone includes insulin, IGF-1, adiponectin, and leptin, whereas afferent signaling from osteoblasts to periphery includes osteocalcin and lipocalin 2 [18, 38,39,40]. MAT contribution to the glucose metabolism comprises production of insulin-sensitizing adiponectin at the levels that significantly contribute to the circulating pools of this adipokine especially in conditions of decreased peripheral fat mass [41].
At the molecular level, bone and energy metabolism are coupled by the nuclear receptor PPARγ. The same posttranslational modifications (PTMs) of PPARγ protein that regulate insulin sensitivity and energy metabolism also regulate bone turnover [22•]. Thus, dephosphorylated Ser273 determines both insulin-sensitizing and pro-osteoclastic activities of PPARγ, whereas phosphorylated Ser112 protects against adipose tissue expansion and correlates with increased bone formation and MAT beiging [22•]. In other words, PPARγ activities that are necessary for balanced energy metabolism and insulin sensitivity are coherently tied to positive regulation of bone remodeling through stimulation of bone formation and bone resorption processes. In contrast, insulin resistance and obesity are associated at the PPARγ level with phosphorylation of Ser273 and dephosphorylation of Ser112, and decrease in bone remodeling at the level of bone resorption and formation. The feature of decreased bone turnover is characteristic for diabetic bone disease (reviewed in [42]). Thus, one can envision that stimulation of PPARγ insulin-sensitizing activity and beiging of adipocytes will be associated with increased bone resorption and bone formation, and will comprise a therapy to treat low bone turnover diseases, such as diabetic bone disease. The prototype of such therapeutic possibility is represented by SR10171 compound which acts as insulin sensitizer and inverse agonist for PPARγ pro-adipocytic activity.
Inhibition of PP5 activity, which controls PPARγ and RUNX2 phosphorylation, represents another therapeutic mean to induce beige phenotype in MAT and increase bone mass. PP5 is unique among other phosphatases because its activity is controlled by an autoinhibitory mechanism involving tetratricopeptide (TPR) domain and C-terminal αJ helix [43,44,45]. When the TPR domain of PP5 is bound to a steroid receptor or free fatty acid, e.g., arachidonic acid, the phosphatase domain is released from the interaction with C-terminus and becomes activated [46,47,48,49]. Thus, by analogy to nuclear receptors, PP5 activity may be modulated pharmacologically. Indeed, novel PP5 activators and inhibitors have been recently developed; however, their effects on MAT acquisition of bone anabolic secretome and regulation of PPARγ and RUNX2 activities have not been tested as yet [50, 51].
As mentioned earlier, manipulation with MAT beige-like phenotype and associated increase in bone mass correlates with acquiring by MAT, a secretome which is anabolic for bone [20•, 23•]. This provides a strong argument for beige-like MAT possessing beneficial for bone endocrine/paracrine activities. Thus, MAT futile metabolic phenotype correlates positively with bone health and negatively with bone loss. The possibility of pharmacological regulation of MAT phenotype opens the door to speculation whether we can harness or suppress, in controlled manner, different activities of MAT. In this respect, manipulation with MAT activities needs to be carefully considered in regard to other bone pathologies. For example, MAT support for angiogenesis may be beneficial for fracture healing but may also facilitate bone cancer metastasis. MAT activities supporting hematopoiesis seen after irradiation may have a detrimental effects on supporting development of leukemia. These different and contradicted effects need to be analyzed against MAT phenotype, whether it is WAT-like which is associated with lipid accumulation and lipotoxicity, or beige-like which is associated with futile metabolism and production of bone anabolic factors.
In summary, MAT has unrecognized potential to regulate bone homeostasis in physiological and pathological conditions. It requires more focused research to determine this potential and harness it for the beneficial but not harmful effects.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Tavassoli M. Marrow adipose cells and hemopoiesis: an interpretative review. Exp Hematol. 1984;12(2):139–46.
Rappaport H, Raum M, Horrell JB. Bone marrow embolism. Am J Pathol. 1951;27(3):407–33.
Beresford JN, Bennett JH, Devlin C, Leboy PS, Owen ME. Evidence for an inverse relationship between the differentiation of adipocytic and osteogenic cells in rat marrow stromal cell cultures. J Cell Sci. 1992;102(Pt 2):341–51.
Horowitz MC, Berry R, Holtrup B, Sebo Z, Nelson T, Fretz JA, et al. Bone marrow adipocytes. Adipocyte. 2017;6:1–12. https://doi.org/10.1080/21623945.2017.1367881.
Calo E, Quintero-Estades JA, Danielian PS, Nedelcu S, Berman SD, Lees JA. Rb regulates fate choice and lineage commitment in vivo. Nature. 2010;466(7310):1110–4.
Ambrosi TH, Scialdone A, Graja A, Gohlke S, Jank AM, Bocian C, et al. Adipocyte accumulation in the bone marrow during obesity and aging impairs stem cell-based hematopoietic and bone regeneration. Cell Stem Cell. 2017;20(6):771–84 e6. https://doi.org/10.1016/j.stem.2017.02.009.
Berry R, Rodeheffer MS, Rosen CJ, Horowitz MC. Adipose tissue residing progenitors (adipocyte lineage progenitors and adipose derived stem cells (ADSC)). Curr Mol Biol Rep. 2015;1(3):101–9. https://doi.org/10.1007/s40610-015-0018-y.
Yue R, Zhou BO, Shimada IS, Zhao Z, Morrison SJ. Leptin receptor promotes adipogenesis and reduces osteogenesis by regulating mesenchymal stromal cells in adult bone marrow. Cell Stem Cell. 2016;18(6):782–96. https://doi.org/10.1016/j.stem.2016.02.015.
Zhou BO, Yu H, Yue R, Zhao Z, Rios JJ, Naveiras O, et al. Bone marrow adipocytes promote the regeneration of stem cells and haematopoiesis by secreting SCF. Nat Cell Biol. 2017;19(8):891–903. https://doi.org/10.1038/ncb3570.
Fan Y, Hanai JI, Le PT, Bi R, Maridas D, DeMambro V, et al. Parathyroid hormone directs bone marrow mesenchymal cell fate. Cell Metab. 2017;25(3):661–72. https://doi.org/10.1016/j.cmet.2017.01.001.
Worthley DL, Churchill M, Compton JT, Tailor Y, Rao M, Si Y, et al. Gremlin 1 identifies a skeletal stem cell with bone, cartilage, and reticular stromal potential. Cell. 2015;160(1–2):269–84. https://doi.org/10.1016/j.cell.2014.11.042.
• Lecka-Czernik B, Stechschulte LA, Czernik PJ, Sherman SB, Huang S, Krings A. Marrow adipose tissue: skeletal location, sexual dimorphism, and response to sex steroid deficiency. Front Endocrinol (Lausanne). 2017;8:188. https://doi.org/10.3389/fendo.2017.00188. This study suggests metabolic diversity among MAT in different skeletal locations and correlation with bone mass and sex steroids status.
•• Scheller EL, Doucette CR, Learman BS, Cawthorn WP, Khandaker S, Schell B, et al. Region-specific variation in the properties of skeletal adipocytes reveals regulated and constitutive marrow adipose tissues. Nat Commun. 2015;6:7808. https://doi.org/10.1038/ncomms8808. These studies represent the first indication of diverse phenotype of MAT.
Krings A, Rahman S, Huang S, Lu Y, Czernik PJ, Lecka-Czernik B. Bone marrow fat has brown adipose tissue characteristics, which are attenuated with aging and diabetes. Bone. 2012;50(2):546–52.
Elbaz A, Rivas D, Duque G. Effect of estrogens on bone marrow adipogenesis and Sirt1 in aging C57BL/6J mice. Biogerontology. 2009;10(6):747–55. https://doi.org/10.1007/s10522-009-9221-7.
Syed FA, Oursler MJ, Hefferanm TE, Peterson JM, Riggs BL, Khosla S. Effects of estrogen therapy on bone marrow adipocytes in postmenopausal osteoporotic women. Osteoporos Int. 2008;19(9):1323–30.
Lecka-Czernik B, Stechschulte LA. Bone and fat: a relationship of different shades. Arch Biochem Biophys. 2014;561:124–9. https://doi.org/10.1016/j.abb.2014.06.010.
Lecka-Czernik B, Rosen CJ. Energy excess, glucose utilization, and skeletal remodeling: new insights. J Bone Miner Res. 2015;30(8):1356–61. https://doi.org/10.1002/jbmr.2574.
Elbaz A, Wu X, Rivas D, Gimble JM, Duque G. Inhibition of fatty acid biosynthesis prevents adipocyte lipotoxicity on human osteoblasts in vitro. J Cell Mol Med. 2010;14(4):982–91. https://doi.org/10.1111/j.1582-4934.2009.00751.x.
• Rahman S, Lu Y, Czernik PJ, Rosen CJ, Enerback S, Lecka-Czernik B. Inducible brown adipose tissue, or beige fat, is anabolic for the skeleton. Endocrinology. 2013;154(8):2687–701. These studies identify for the first time bone anabolic secretome of beige-like MAT.
Kolli V, Stechschulte LA, Dowling AR, Rahman S, Czernik PJ, Lecka-Czernik B. Partial agonist, telmisartan, maintains PPARgamma serine 112 phosphorylation, and does not affect osteoblast differentiation and bone mass. PLoS One. 2014;9(5):e96323. https://doi.org/10.1371/journal.pone.0096323.
• Stechschulte LA, Czernik PJ, Rotter ZC, Tausif FN, Corzo CA, Marciano DP, et al. PPARG post-translational modifications regulate bone formation and bone resorption. EBioMedicine. 2016;10:174–84. https://doi.org/10.1016/j.ebiom.2016.06.040. These studies demonstrated that SR10171 compound which acts as PPARγ inverse agonist has beneficial effect on bone and insulin sensitivity.
• Stechschulte LA, Ge C, Hinds TD Jr, Sanchez ER, Franceschi RT, Lecka-Czernik B. Protein phosphatase PP5 controls bone mass and the negative effects of rosiglitazone on bone through reciprocal regulation of PPARgamma (peroxisome proliferator-activated receptor gamma) and RUNX2 (runt-related transcription factor 2). J Biol Chem. 2016;291(47):24475–86. https://doi.org/10.1074/jbc.M116.752493. These studies identify PP5 for its inhibitory effect on RUNX2 activity and anabolic activity of beige-like MAT.
Cederberg A, Gronning LM, Ahren B, Tasken K, Carlsson P, Enerback S. FOXC2 is a winged helix gene that counteracts obesity, hypertriglyceridemia, and diet-induced insulin resistance. Cell. 2001;106(5):563–73.
Lazarenko OP, Rzonca SO, Hogue WR, Swain FL, Suva LJ, Lecka-Czernik B. Rosiglitazone induces decreases in bone mass and strength that are reminiscent of aged bone. Endocrinology. 2007;148(6):2669–80.
Marciano DP, Kuruvilla DS, Boregowda SV, Asteian A, Hughes TS, Garcia-Ordonez R, et al. Pharmacological repression of PPARgamma promotes osteogenesis. Nat Commun. 2015;6:7443. https://doi.org/10.1038/ncomms8443.
Kahn SE, Zinman B, Lachin JM, Haffner SM, Herman WH, Holman RR, et al. Rosiglitazone-associated fractures in type 2 diabetes: an analysis from a diabetes outcome progression trial (ADOPT). Diabetes Care. 2008;31(5):845–51.
Modder UI, Monroe DG, Fraser DG, Spelsberg TC, Rosen CJ, Gehin M, et al. Skeletal consequences of deletion of steroid receptor coactivator-2/transcription intermediary factor-2. J Biol Chem. 2009;284(28):18767–77.
Yang Y, Luo X, Xie X, Yan F, Chen G, Zhao W, et al. Influences of teriparatide administration on marrow fat content in postmenopausal osteopenic women using MR spectroscopy. Climacteric. 2016;19(3):285–91. https://doi.org/10.3109/13697137.2015.1126576.
Kong J, Li YC. Molecular mechanism of 1,25-dihydroxyvitamin D3 inhibition of adipogenesis in 3T3-L1 cells. Am J Physiol Endocrinol Metab. 2006;290(5):E916–24. https://doi.org/10.1152/ajpendo.00410.2005.
Lee H, Bae S, Yoon Y. Anti-adipogenic effects of 1,25-dihydroxyvitamin D3 are mediated by the maintenance of the wingless-type MMTV integration site/beta-catenin pathway. Int J Mol Med. 2012;30(5):1219–24. https://doi.org/10.3892/ijmm.2012.1101.
Kelly KA, Gimble JM. 1,25-Dihydroxy vitamin D3 inhibits adipocyte differentiation and gene expression in murine bone marrow stromal cell clones and primary cultures. Endocrinology. 1998;139(5):2622–8.
Narvaez CJ, Simmons KM, Brunton J, Salinero A, Chittur SV, Welsh JE. Induction of STEAP4 correlates with 1,25-dihydroxyvitamin D3 stimulation of adipogenesis in mesenchymal progenitor cells derived from human adipose tissue. J Cell Physiol. 2013;228(10):2024–36. https://doi.org/10.1002/jcp.24371.
Pathak K, Soares MJ, Calton EK, Zhao Y, Hallett J. Vitamin D supplementation and body weight status: a systematic review and meta-analysis of randomized controlled trials. Obes Rev. 2014;15(6):528–37. https://doi.org/10.1111/obr.12162.
Wright HM, Clish CB, Mikami T, Hauser S, Yanagi K, Hiramatsu R, et al. A synthetic antagonist for the peroxisome proliferator-activated receptor gamma inhibits adipocyte differentiation. J Biol Chem. 2000;275(3):1873–7.
Santiago-Mora R, Casado-Diaz A, De Castro MD, Quesada-Gomez JM. Oleuropein enhances osteoblastogenesis and inhibits adipogenesis: the effect on differentiation in stem cells derived from bone marrow. Osteoporos Int. 2011;22(2):675–84. https://doi.org/10.1007/s00198-010-1270-x.
Duque G, Li W, Vidal C, Bermeo S, Rivas D, Henderson J. Pharmacological inhibition of PPARgamma increases osteoblastogenesis and bone mass in male C57BL/6 mice. J Bone Miner Res. 2013;28(3):639–48. https://doi.org/10.1002/jbmr.1782.
Lecka-Czernik B, Rosen CJ. Skeletal integration of energy homeostasis: translational implications. Bone. 2016;82:35–41. https://doi.org/10.1016/j.bone.2015.07.026.
Liu JM, Rosen CJ, Ducy P, Kousteni S, Karsenty G. Regulation of glucose handling by the skeleton: insights from mouse and human studies. Diabetes. 2016;65(11):3225–32. https://doi.org/10.2337/db16-0053.
Mosialou I, Shikhel S, Liu JM, Maurizi A, Luo N, He Z, et al. MC4R-dependent suppression of appetite by bone-derived lipocalin 2. Nature. 2017;543(7645):385–90. https://doi.org/10.1038/nature21697.
Scheller EL, Burr AA, MacDougald OA, Cawthorn WP. Inside out: bone marrow adipose tissue as a source of circulating adiponectin. Adipocyte. 2016;5(3):251–69. https://doi.org/10.1080/21623945.2016.1149269.
Lecka-Czernik B. Diabetes, bone and glucose-lowering agents: basic biology. Diabetologia. 2017;60:1163–9. https://doi.org/10.1007/s00125-017-4269-4.
Chen MX, McPartlin AE, Brown L, Chen YH, Barker HM, Cohen PTA. Novel human protein serine/threonine phosphatase, which possesses four tetratricopeptide repeat motifs and localizes to the nucleus. EMBO J. 1994;13(18):4278–90.
Kang H, Sayner SL, Gross KL, Russell LC, Chinkers M. Identification of amino acids in the tetratricopeptide repeat and C-terminal domains of protein phosphatase 5 involved in autoinhibition and lipid activation. Biochemistry. 2001;40(35):10485–90.
Hinds TD Jr, Sanchez ER. Protein phosphatase 5. Int J Biochem Cell Biol. 2008;40(11):2358–62. https://doi.org/10.1016/j.biocel.2007.08.010.
Skinner J, Sinclair C, Romeo C, Armstrong D, Charbonneau H, Rossie S. Purification of a fatty acid-stimulated protein-serine/threonine phosphatase from bovine brain and its identification as a homolog of protein phosphatase 5. J Biol Chem. 1997;272(36):22464–71.
Hinds TD Jr, Stechschulte LA, Cash HA, Whisler D, Banerjee A, Yong W, et al. Protein phosphatase 5 mediates lipid metabolism through reciprocal control of glucocorticoid and PPAR{gamma} receptors. J Biol Chem. 2011;286(10):42911–22.
Cher C, Tremblay MH, Barber JR, Chung Ng S, Zhang B. Identification of chaulmoogric acid as a small molecule activator of protein phosphatase 5. Appl Biochem Biotechnol. 2010;160(5):1450–9. https://doi.org/10.1007/s12010-009-8647-3.
Ramsey AJ, Chinkers M. Identification of potential physiological activators of protein phosphatase 5. Biochemistry. 2002;41(17):5625–32.
Haslbeck V, Drazic A, Eckl JM, Alte F, Helmuth M, Popowicz G, Schmidt W, Braun F, Weiwad M, Fischer G, Gemmecker G, Sattler M, Striggow F, Groll M, Richter K Selective activators of protein phosphatase 5 target the auto-inhibitory mechanism. Biosci Rep. 2015;35(3), e00210. https://doi.org/10.1042/BSR20150042
Hong TJ, Park K, Choi EW, Hahn JS. Ro 90-7501 inhibits PP5 through a novel, TPR-dependent mechanism. Biochem Biophys Res Commun. 2017;482(2):215–20. https://doi.org/10.1016/j.bbrc.2016.11.043.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Beata Lecka-Czernik, Sudipta Baroi, Lance Stechschulte, and Amit Sopan Chougule declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects.
Additional information
This article is part of the Topical Collection on Bone Marrow and Adipose Tissue
Rights and permissions
About this article
Cite this article
Lecka-Czernik, B., Baroi, S., Stechschulte, L.A. et al. Marrow Fat—a New Target to Treat Bone Diseases?. Curr Osteoporos Rep 16, 123–129 (2018). https://doi.org/10.1007/s11914-018-0426-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-018-0426-z