Abstract
Purpose of Review
The term osteopetrosis refers to a group of rare skeletal diseases sharing the hallmark of a generalized increase in bone density owing to a defect in bone resorption. Osteopetrosis is clinically and genetically heterogeneous, and a precise molecular classification is relevant for prognosis and treatment. Here, we review recent data on the pathogenesis of this disorder.
Recent Findings
Novel mutations in known genes as well as defects in new genes have been recently reported, further expanding the spectrum of molecular defects leading to osteopetrosis.
Summary
Exploitation of next-generation sequencing tools is ever spreading, facilitating differential diagnosis. Some complex phenotypes in which osteopetrosis is accompanied by additional clinical features have received a molecular classification, also involving new genes. Moreover, novel types of mutations have been recognized, which for their nature or genomic location are at high risk being neglected. Yet, the causative mutation is unknown in some patients, indicating that the genetics of osteopetrosis still deserves intense research efforts.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
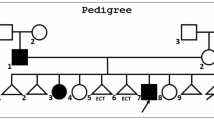
The term osteopetrosis describes a group of inherited skeletal rare disorders characterized by a marked increase in bone density owing to defective bone resorption by the osteoclasts, the cells specifically devoted to this function in the bone tissue [1••]. Three forms of osteopetrosis can be distinguished based on the pattern of inheritance: autosomal recessive (ARO), autosomal dominant (ADO), and X-linked.
ARO has an incidence of 1:250,000 births, but in specific geographic regions (i.e., Costa Rica, the Middle East, the Chuvash Republic of Russia, the Västerbotten county in Sweden) is more frequent because of a founder effect, geographic isolation, or high degree of parental consanguinity. ARO is also called malignant infantile, because it is diagnosed soon after birth and is often lethal in untreated patients [1••].
ADO has an incidence of 1:20,000 births, is also called adult since clinical manifestation typically occurs in adolescence or adulthood, and is generally considered benign since life expectancy is usually normal. However, this form displays highly variable severity, ranging from asymptomatic cases to severely affected individuals, where the disease is evident already in childhood [2].
Finally, X-linked osteopetrosis is an extremely rare form, with only very few unrelated patients reported thus far in literature [3,4,5,6,7].
Carbonic anhydrase II (CAII) deficiency was the first form of osteopetrosis with a recognized molecular pathogenesis [8]. The initial evidence came from the biochemical evaluation of the enzymatic activity in patients; afterwards, direct sequencing of the CAII gene allowed identifying the exact mutations [9]. Since 2000, the genetic bases of osteopetrosis have largely been elucidated, thus providing a genetic classification for about 90% of patients, while few cases still lack a precise diagnosis [1••]. In “pure” ARO, biallelic mutations in one of seven different genes lead to the disease: five of these disease genes (TCIRG1, CLCN7, OSTM1, SNX10, and PLEKHM1) encode proteins involved in the acidification of the resorption lacunae and/or in vesicular transport. Loss-of-function mutations in these genes lead to osteoclast-rich osteopetrosis, in which osteoclasts are abundant but not functional. On the other hand, mutations in TNFSF11 (RANKL) and its receptor TNFRSF11A (RANK) are associated with osteoclast-poor ARO, in which osteoclastogenesis is blocked [10].
In ADO, the types I and II differ for key clinical features (namely, the main sites of increased bone density and the susceptibility to fragility fractures) and for the genetic defect, which is located in the LRP5 and CLCN7 genes, respectively [11]. However, since ADO I derives from enhanced osteoblast activity due to reduced LRP5 affinity for the extracellular antagonists SOST and DKK1 and consequent increased Wnt canonical signaling, it would be more properly classified as a form of high bone mass. For this reason, recent literature regarding mutations in the LRP5 gene will not be addressed in this work.
Finally, X-linked osteopetrosis is ascribed to hypomorphic mutations in the NEMO (NF-κB essential modulator) gene [3,4,5,6,7].
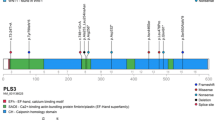
Here, we will review the most recent genetic findings that expand the spectrum of molecular defects leading to osteopetrosis. We will briefly describe the novel mutations identified in the abovementioned genes, with a specific focus on new types of mutations, which in some cases challenge commonly adopted criteria of variant selection during genetic investigation, and we will present new genes associated with osteopetrosis in single or few patients. The molecules and signaling pathways mentioned in the text as having a role in the pathogenesis of osteopetrosis are schematically depicted in Fig. 1 and summarized in Table 1.
Simplified representation of molecules involved in osteoclast differentiation and activation and playing a role in the pathogenesis of osteopetrosis. The well-known disease genes are in bold in black color, while the newly identified disease genes mentioned in this review are in bold in orange color
Mutations in Known Genes
TCIRG1
The TCIRG1 (T cell immune regulator 1) gene encodes the a3 subunit of the V0 domain of the ATP-dependent vacuolar proton pump V-ATPase [12]. It is mostly expressed in osteoclasts and in gastric parietal cells: in bone, the activity of the V-ATPase is required to achieve the low pH needed for the dissolution of the inorganic matrix and the degradation of the organic matrix by acid proteases; in the stomach, it determines the low pH required for dietary Ca2+ absorption. Overall, this explains the defect in bone mineralization and the co-occurrence of osteopetrosis and rickets (i.e., osteopetrorickets) deriving from TCIRG1 mutations [1••].
In addition to its proton-pump activity, the V0 complex is involved in vesicle trafficking; in fact, it interacts with microtubules and actin cytoskeleton, probably by means of the a3 subunit itself, and this is crucial for ruffled border formation [1••].
Mutations in TCIRG1 account for about 50% of ARO cases and are distributed along the entire gene, causing defects in the proton-pumping function of the V-ATPase and in vesicle trafficking/fusion in osteoclasts.
More than 120 different mutations have been described thus far in the TCIRG1 gene, comprising missense mutations, stop mutations, small insertions/deletions, large genomic deletions, and splicing defects, which demonstrates the high genetic heterogeneity of the TCIRG1-deficient ARO cohort [13,14,15]. This fact has been further underlined by recent reports of single patients or small groups of patients carrying novel TCIRG1 mutations [16••, 17, 18, 19••, 20]. On this topic, our group recently published particularly interesting data: in the first report, we described four different single nucleotide changes in intron 15 located about 150 nucleotides away from the closest canonical splicing site, thus named deep intronic mutations [16••]. These mutations impaired the splicing process because of the activation of a cryptic splicing site; at the same time, the correct splicing was not completely abrogated, thus likely explaining the milder phenotype displayed in the homozygous state. Overall, these data highlighted the need to carefully evaluate the possible effects of intronic changes in known disease genes.
In the second work, we described a synonymous mutation in TCIRG1 exon 12 which formed an internal acceptor splice site in exon 12 causing splicing aberration, frame shift, and premature termination, as demonstrated by in silico analysis and the minigene technology [19••]. We found a similar defect in a CLCN7-dependent ARO patient (see below). These results were in line with recent literature dealing with other human diseases claiming the nonneutral effect of synonymous changes in different genes.
CLCN7
The CLCN7 (chloride voltage-gated channel 7) gene encodes a ubiquitously expressed slowly voltage-gated 2Cl−/1H+ antiporter channel located on the membrane of late endosomes and lysosomes [21]. It mediates the exchange of chloride ions against protons, thus cooperating with the V-ATPase in the acidification of the resorption lacuna and of lysosomal vesicles. CLCN7 functions as a dimer: each monomer contains an ion translocation pathway with conserved gating glutamate residues, and conformational rearrangements outside the ion pathway lead to simultaneous gating of the two pores [22••].
Recessive mutations in the CLCN7 gene are responsible for about 17% of ARO cases, while dominant ones are responsible for most ADO II cases [2, 11, 23].
In the last few years, a number of novel CLCN7 mutations have been reported in patients of different geographic origin (i.e., Chinese, Taiwanese, Japanese, Ecuadorian, Italian-Moroccan) and associated with all the different forms of CLCN7-dependent osteopetrosis: recessive, dominant, and intermediate [24,25,26,27,28,29,30,31,32]. The majority of these novel mutations caused amino acid changes and was found in single patients or families. Actually, this might introduce some uncertainty in their interpretation, so the optimization of an easy and reliable assay to test the functional effect of CLCN7 mutations on the protein function is urgently needed, in order to definitely distinguish between rare polymorphisms and mutations, to draw genotype-phenotype correlations and phenotype prediction on the basis of genotype information. Furthermore, as above mentioned, a synonymous variant in CLCN7 exon 12 was reported too, and demonstrated to cause a partial splicing aberration with in-frame skipping of exon 12 [19••]. This finding prompted the hypothesis that some synonymous, not clearly pathogenic changes might modulate the phenotype of CLCN7 mutations. To verify this, the analysis of clinical and genetic data on large cohorts of CLCN7-dependent osteopetrotic individuals could be considered.
SNX10
The SNX10 (sorting nexin 10) gene encodes a protein belonging to the SNX family of cytoplasmic and membrane-bound proteins characterized by the presence of a phosphoinositide-binding domain, called PX domain [33]. In general, SNX proteins take part in protein sorting and membrane trafficking by establishing protein-protein and protein-lipid interactions. In particular, SNX10 interacts with the V-ATPase and regulates its subcellular trafficking; accordingly, SNX10-deficient ARO results from altered V-ATPase trafficking to the ruffled border and consequent defective osteoclast function. Very recently, SNX10 has also been suggested to play a role in trafficking and secretion of matrix metalloprotease 9 for degradation of the extracellular matrix [34].
Mutations in the SNX10 gene (NM_001199835.1) account for about 5% of ARO cases, comprising also the so-called Västerbottenian osteopetrosis, from the name of the Swedish County with a high incidence of the disease [35, 36, 37••, 38]. In particular, the SNX10 c.212+1G>T variant, causing activation of a cryptic splice site in intron 4 and aberrant splicing, has been confirmed as the shared mutation in this cohort of patients, with an impressive carrier frequency (1:93) in the general Vasterbottenian population [37••]. Interestingly, genealogical studies and haplotype analysis traced its origin back to a common ancestor in the early nineteenth century. At the cellular level, despite previous contradictory findings on the presence or absence of osteoclasts in SNX10-deficient ARO, Stattin and colleagues clearly demonstrated no defect in osteoclast differentiation from the patients’ PBMCs but impaired ruffled border formation [34, 37••]. On the other hand, whether in humans SNX10 inactivation leads to osteopetrorickets as reported in the mouse model remains an open question as only few patients display this peculiar phenotype [37••]. Very recently, induced pluripotent stem cells (iPSc) have been reprogrammed from the skin fibroblasts of a patient carrying the c.212+1G>T mutation. These iPSc will be a useful tool to help unraveling the unsolved aspects of SNX10-dependent osteopetrosis [39].
OSTM1
The OSTM1 (osteopetrosis-associated transmembrane protein 1) gene encodes a type I transmembrane protein localized mainly on endosomes and lysosomes. It has a highly glycosylated N-terminus which stabilizes CLCN7 and protects it from lysosomal degradation, and is important for CLCN7 2Cl−/1H+ exchange [21, 40]. The transmembrane domain is involved in ion exchange and CLCN7-dependent trafficking to the lysosomes. OSTM1 has been proposed to act also as an E3 ubiquitin ligase for the heterotrimeric G-protein Gαi3 and to potentiate WNT canonical signaling by modulating β-catenin/Lef1 interaction [41, 42].
Additional cytosolic OSTM1 binding partners have recently been identified, suggesting that OSTM1 might serve as an adaptor molecule within a cytosolic scaffolding multiprotein complex [43].
Mutations in the OSTM1 gene (NM_014028.3) account for about 5% of ARO cases and invariably cause an extremely severe phenotype with rapidly progressing primary neurodegeneration [44, 45]. Almost all the identified mutations in this gene are truncating defects. In this respect, a secreted form of truncated OSTM1 has been shown to inhibit in vitro osteoclast formation through downregulation of the BLIMP1-NFATc1 axis, thus providing a putative additional pathogenetic mechanism for OSTM1-deficient ARO [46•]. Moreover, through an ad hoc designed quantitative PCR strategy, two different homozygous microdeletions, respectively, spanning ~ 110 and ~ 10 kb and affecting the N-terminal portion of the OSTM1 gene, have been reported in two unrelated families of Arabic and Indian descent, comprising five severely sick patients [47]. Sequence analysis of the relevant genomic region identified AluSx-mediated recombination and nonrecurrent rearrangement followed by nonhomologous end joining, as respective underlying molecular mechanism.
Very recently, a patient has been described displaying osteopetrosis, early onset neurodegeneration and iron accumulation in specific brain regions, which is a very unusual finding [48]. Whole exome sequencing revealed the presence of the novel c.783+5G>T mutation in the OSTM1 gene, causing skipping of exon 4, and of the frameshift variant c.446dup at the homozygous state in the MANEAL gene. This latter encodes the mannosidase endo-alpha-like protein, which probably localizes at the Golgi and is potentially involved in glycoprotein metabolism; indeed, mannose tetrasaccharide molecules were found increased in the patient’s urine and cerebrospinal fluid. How this might relate to brain iron accumulation is not clear. Overall, the contribution of the mutation in the MANEAL gene to the phenotype driven by the OSTM1 requires further investigations.
PLEKHM1
The PLEKHM1 (pleckstrin homology domain-containing family M -with RUN domain-member 1) gene encodes a cytosolic protein implicated in endosomal trafficking pathways through the interaction with the small GTPases RAB7 and ARL8 [49, 50]. In addition, PLEKHM1 participates in the fusion of autophagosomes and lysosomes, required for clearance of diverse protein aggregates [51]. Accordingly, disruption of specific PLEKHM1 domains or loss of PLEKHM1 impairs vesicle distribution, secretion, and ruffled border formation, thus undermining osteoclast resorptive function [52].
PLEKHM1 is a large protein containing different functional domains: a RUN domain, where the mutation (NM_014798.2:c.296+1G>A) originally identified in two ARO siblings was located [53]; two pleckstrin homology (PH) domains separated from one another by an LC3-interacting region (LIR); a Rubicon homology (RH) domain and a C1 zinc finger, at the C terminus. Two different putatively dominant mutations in the PLEKHM1 gene have been reported in two unrelated patients: the c.2140C>T:p.Arg714Cys, not clearly associated with osteopetrosis, found in the second PH domain [54]; and the recently reported c.3051_3052delCA located in the RH domain and predicted to eliminate the zinc finger-like motif [55]. The RH domain is required for PLEKHM1 interaction with RAB7; accordingly, overexpression studies in HEK293T cells showed reduced interaction of the mutant protein with RAB7, resulting in abnormal intracellular localization and increased levels of autophagy. This recent work importantly contributed to the understanding of PLEKHM1 function in bone cell biology, even though some aspects, such as the relationship with autophagy, remain controversial and deserve further investigation.
CAII
The CAII gene codes the cytoplasmic enzyme that catalyzes the formation of H2CO3 using CO2 and H2O; then, H2CO3 dissociates into HCO3− and H+ ions. The generated H+ are extruded by the V-ATPase, while the HCO3− is taken up by a Cl−/HCO3− anion exchanger located in the basolateral membrane, which prevents cytoplasmic alkalinization and provides the Cl− ions required by the CLCN7/OSTM1 2Cl−/H+ antiporter [8, 56].
Besides in bone, the CAII gene is highly expressed in the kidney and brain, in fact patients with CAII deficit present osteopetrosis, renal tubular acidosis (RTA) and cerebral calcifications, and this triad per se makes the diagnosis [1••, 8, 9]. Interestingly, proximal RTA has recently been described also in an ADO II patient carrying the common p.Gly215Arg ADO II mutation and no additional mutation in genes associated with RTA; in this specific context, the exact pathogenetic mechanism is not clear yet [29].
Since the standardization of the conditions for genetic testing, about 30 different mutations have been identified in the CAII gene: missense, stop and splice site mutations (among these latter, the NM_000067.2:c.232+1G>A is the called Arabic mutation, since it is very common in patients of Arabic descent). The majority of patients are of Arab origin; however, also Caucasian, Hispanics, African-Americans, Asians, and more recently Chinese Han patients have been reported [57,58,59,60].
FERMT3
The FERMT3 (fermitin family member 3) gene encodes kindlin-3, a member of the kindlin family that comprises three different focal adhesion proteins involved in integrin activation. This is a process required for cell adhesion, spreading and migration, extracellular matrix organization, cell survival, proliferation, and differentiation [61]. Kindlin-3 is an intracellular protein linked to the actin cytoskeleton. It interacts with multiple integrin classes and mediates their adhesive function and inside-out signaling, which in bone is essential for osteoclast resorptive activity. Accordingly, kindlin-3 deficiency causes a severe morphological alteration of osteoclasts and impairs their ability to adhere to bone surfaces [62]. Interestingly, mutations in the FERMT3 gene are responsible for the rare autosomal recessive disease called leukocyte adhesion deficiency (LAD-III); few LAD-III patients also suffer from severe osteopetrosis (10 out of 23 published cases) [63, 64]. The mutations are mostly highly disruptive: truncating mutations, splicing defects, frame shifts; only two missense mutations have been reported. Unfortunately, since the number of cases published in literature is very limited, at present is not possible to draw genotype/phenotype correlations.
RANKL
The RANKL (receptor activator of nuclear kappa B ligand) gene codes for the essential osteoclastogenic cytokine that through binding to its receptor RANK determines the activation of the downstream signaling cascade driving osteoclast differentiation and activation [65]. An additional receptor for the RANKL molecule has been recently recognized, the leucine-rich repeat-containing G-protein coupled receptor 4 (LGR4), which upon ligand binding activates the GSK3 pathway, thus suppressing the expression of NFATc1 during osteoclastogenesis [66••]. Moreover, a new unexpected function of RANKL in the bone tissue has been unveiled, which is an important role in the osteogenic differentiation of mesenchymal stem cells probably through an autocrine loop [67•].
Overall, these data raise great interest on RANKL-deficient ARO, which constitutes a rare form of osteopetrosis accounting for about 2% of cases [10, 68, 69•]. Further investigations are needed to fully understand the elicited molecular mechanisms and their relevance in bone pathophysiology.
To the best of our knowledge, no additional patients and mutations besides the original ones have recently been published.
RANK
As mentioned above, the RANK (receptor activator of nuclear kappa B) gene codes for the functional receptor for RANKL. Binding to the ligand induces the receptor trimerization and recruitment of different adaptor molecules and activation of several signaling pathways such as c-Jun N-terminal kinase (JNK)/activator protein-1 (AP-1), nuclear factor kappa B (NF-kB) and nuclear factor of activated T cell c1 (NFATc1), Src and p38/MITF, Src and ERK, resulting in osteoclast differentiation, activation and survival [65].
Mutations in the RANK gene are responsible for about 5% of ARO cases [10, 70, 71•]. At variance with RANKL-deficient ARO, in which the bone defect is not corrected by hematopoietic stem cell transplantation (HSCT), RANK-deficient ARO is cured by HSCT, as further demonstrated by recent reports [72,73,74,75]. These works reported also novel mutations (NM_003839:c.376T>C:p.Cys126Arg and c.1063C>T:p.Gln355* in [72], and c.689_751del:p.Thr230Glyfs5* and c.414T>G:p.Cys126Gly in [75]).
SLC29A3
Dysosteosclerosis is a rare distinctive form of osteopetrosis presenting in infancy with typical skeletal features (expanded ends of the tubular bones and platyspondyly) and various skin lesions [76]. The clinical course and the prognosis seem to be rather benign. Scanty data are available in literature on the genetics of Dysosteosclerosis. The affected gene is the SLC29A3 (Solute carrier family 29 member 3), encoding a lysosomal nucleoside transporter highly expressed in cells of the myeloid lineage. The reported mutations (NM_018344:c.607T>C:p.Ser203Pro and c.1157G>A:p.Arg386Gln in patient 1, and c.1346C>G:p.Thr449Arg in patient 2 at the homozygous state, in [76]; c.303_320dup:p.102_107dup at the homozygous state in [77]) would impact on osteoclast function and differentiation, as suggested by reduced osteoclast numbers after in vitro differentiation from the patients’ PBMCs and in bone biopsy specimens from the patients [76]. Mutations in SLC29A3 are also associated with histiocytosis–lymphadenopathy plus syndrome, a group of conditions with little or no skeletal involvement. Thus, further investigations would be required to better elucidate its role in bone, and more in general in physiopathology.
CTSK
Pycnodysostosis is a rare autosomal recessive skeletal dysplasia (estimated prevalence 1:1.7 million individuals) included in the differential diagnosis of osteopetrosis because of the presence of increased bone density in long bones. Other clinical features typical of pycnodysostosis are short stature, variably responsive to growth hormone treatment; open fontanels and cranial sutures, fractures, obtuse mandibular angle, and acroosteolysis of the distal phalanges [78]. The affected gene is the CTSK, coding for cathepsin K, a cysteine peptidase of the papain superfamily exploited by osteoclasts for bone matrix degradation and endowed with the unique capacity to cleave collagen molecules at multiple sites [79]. Furthermore, cathepsin K has been recently shown to cleave and activate matrix metalloproteinase 9 in vitro, which would suggest the presence of a protease-signaling network likely relevant in a variety of physiopathological conditions [80]. More recently, cathepsin K has been shown to contribute to the regulation of bone modeling by degrading periostin, a matricellular protein of the cortical compartment essential for the periosteal bone formation mediated by the Wnt-β catenin pathway [81].
About 60 different mutations have been reported in literature so far, in patients of different geographic origin [78, 82,83,84,85,86,87,88,89]. Missense variants are the most frequent mutations; frameshifts, nonsense mutations, and splicing defects have been identified, too. Mutations mainly occur in the mature CTSK protein, where exons 5 and 6 appear to be hot spots. In addition, about 6% of mutations map in the preregion and 25% in the proregion, which are short N-terminal domains required for proper protein localization and protein folding and intracellular trafficking, respectively; the proregion is also needed to maintain the enzyme in an inactive state and is cleaved off at low pH. Nevertheless, genotype-phenotype correlations, possibly explaining also atypical presentations [84, 85, 89], have not been specifically investigated.
Genes Involved in Newly Recognized Syndromic Forms of Osteopetrosis
TRAF6
Among different adaptor molecules recruited by RANKL/RANK binding, TRAF6 (TNF receptor-associated factor 6) appears to be the most important. TRAF6 acts also downstream T and B cell receptor, leading to NF-kB activation [65]. Several years ago, TRAF6 gene inactivation in mouse was demonstrated to cause severe osteopetrosis, and very recently, similar evidence has been obtained in humans [90, 91•]. In fact, a 2064 Kb homozygous genomic deletion on chromosome 11 encompassing the 5′ region of TRAF6, RAG1, and RAG2 genes (the RAG proteins are essential for recombination of B and T cell receptors, and for the survival and differentiation of these cells) has been identified in two affected siblings displaying osteopetrosis and severe combined immunodeficiency (SCID) through chromosomal microarray analysis [91•]. The exact boundaries of the deletion have not been defined; for what pertains to TRAF6, this genomic deletion encompasses the region upstream of exon 1 and part of the noncoding sequences of exon 1. These regions are very likely regulatory, in fact at the protein level their deletion completely abolished TRAF6 production. The resulting phenotype was peculiar, since osteopetrosis was not generalized, but prominent in the pelvis and legs; since both affected siblings died at a very young age due to the severe immunological defect and no additional similar cases are known at present, foreseeing the evolution of the skeletal disease in this specific genetic background is difficult.
LRRK1
Osteosclerotic metaphyseal dysplasia is a form of osteopetrosis mainly affecting the metaphyses of long bones, the vertebral endplates, costal ends, and margins of flat bones, while the skull appears normal [92•]. Only five patients have been described; in one of them, the homozygous deletion of seven nucleotides in the last exon of the LRRK1 (leucine-rich repeat kinase 1) gene has recently been identified (NM_024652:c.5938_5944delGAGTGGT:p.Glu1980Alafs*66) and predicted to cause frameshift and premature termination, with loss of the seventh tryptophan-aspartic acid (WD) 40 domain. The WD40 domain, as well as other functional domains in the LRRK1 protein, mediates protein-protein interaction [93]. In particular, LRRK1 has been proposed to interact with components of the c-Src signaling pathway to achieve cytoskeletal rearrangement and ruffled border and podosome assembly. Accordingly, murine Lrrk1-deficient osteoclasts are flat and large, as they fail to properly reorganize the cytoskeleton and resorb bone. Overall, LRRK1 has raised great interest in bone biology and future work will precisely define its physiopathological role.
MITF
The microphthalmia-associated transcription factor (MITF) is a basic helix-loop-helix zipper transcription factor, which forms homo/heterodimers regulating gene expression in different tissues, so a range of phenotypes can be reasonably expected when it is mutated. In bone, MITF has been proposed to act along the RANKL/RANK signaling pathway downstream NFATc1 in order to amplify NFATc1-dependent osteoclastogenic signals [94]. Indeed, Mitfmi/mi mice are osteopetrotic due to a defect in the early stages of osteoclastogenesis [95].
Compound heterozygous mutations in the MITF gene have very recently been found in two unrelated patients displaying COMMAD syndrome, featuring coloboma, osteopetrosis, microphtalmia, macrocephaly, albinism, and deafness [96•]. The identified mutations (NM_198159.2:c.952_954delAGA:p.Arg318del and c.921G>C:p.Lys307Asn in proband I; c.952A>G:p.Arg318Gly and c.938-1G>A:p.Leu312fs* in proband II) did not alter MITF dimerization, but rather its nuclear migration and DNA binding properties. This finding expands the spectrum of phenotypes driven by MITF; in fact, at variance with recessive mutations, dominant ones are associated with Waardenburg syndrome type 2A and Tietz syndrome, which share the hallmark of deafness and pigmentation deficits. Overall, these data confirm the essential role of MITF in developmental processes, and in cell differentiation and survival.
NF-kB Signaling
NF-kB signaling involves a number of molecules (mainly kinases and transcription factors), which exert a crucial role in regulating gene expression in many organs and physiopathological conditions. In bone, this is demonstrated by the fact that hypomorphic mutations in the NEMO gene, which encodes a component of the IkB kinase complex required for inhibition of IkB-α and subsequent nuclear translocation of the released p65/p50 heterodimer, are responsible for X-linked osteopetrosis with ectodermal dysplasia and immunodeficiency [3,4,5,6,7]. These mutations are mainly located in the zinc finger domain of the protein and lead to osteopetrosis through alteration of the RANKL/RANK signaling pathway.
More recently, p65 (Rela) itself has been linked to a high bone mass phenotype [97•]. In fact, in a newborn suddenly died of unknown causes, the pathological increase in bone density found at postmortem analysis and attributed to increased osteoblast function, was associated to a de novo missense mutation in the RELA gene (NM_021975.3:c.1534_1535delinsAG:p.Asp512Ser). This mutation was demonstrated to impair NF-kB signaling in the patient’s fibroblasts, raising the hypothesis of possible alterations in diverse vital functions.
CSF1R
Together with RANKL, M-CSF is an essential osteoclastogenic molecule, as well demonstrated by the osteoclast-poor osteopetrosis in mice lacking this cytokine (the op/op mouse model). Mice deficient for the M-CSF receptor (CSF1R) display a similar osteopetrotic phenotype; in addition, both models have defects in innate immunity, fertility, and neurologic function [98]. Interestingly, dominant mutations in the CSF1R gene cause an adult form of encephalomyopathy, while very recently, a recessive mutation in this gene was suspected to be responsible for a lethal, complex phenotype in two affected siblings presenting with generalized osteopetrosis and severe brain malformation [99•]. Briefly, exome sequencing in the consanguineous parents of the deceased children identified a heterozygous truncating mutation (NM_001288705.1:c.1620C>T:p.Tyr540*) in the CSF1R gene predicted to give rise to a protein lacking the intracellular domain, which is required for ligand-dependent dimerization and autophosphorylation. In the absence of a DNA sample from the patients, homozygosity for the CSF1R mutation could not be demonstrated in the affected individuals; therefore, these findings were not conclusive. However, on their basis it would be interesting to analyze the gene in other patients with a similar phenotype, in order to try to identify additional mutations as a confirmation.
C16orf57
Several years ago, an Italian patient was described displaying osteopetrosis in association with poikyloderma and neutropenia (PN) [100]. PN is an inherited genodermatosis characterized by early onset poikiloderma, nail dystrophy, palmo-plantar hyperkeratosis, and persistent neutropenia leading to recurrent infections. Sometimes skeletal defects, such as osteopenia, craniofacial dysmorphisms, fractures, postnatal delay in skeletal maturation and growth, are present; thus, the case reported by Migliaccio et al. was really atypical. PN is due to mutations in the C16orf57 gene, coding for a phosphodiesterase responsible for modification and stabilization of the U6 small nuclear RNA (USB1), which is an essential element of the splicesome machinery [101]. More recently, the patient with osteopetrosis and PN was found to bear a homozygous stop mutation in the C16orf57 gene (ENSG00000103005:c.232C>T:p.Arg78*), predicted to severely damage the correct folding of the putative truncated protein [102•]. The elicited pathogenetic mechanism could be incomplete/aberrant splicing of specific classes of genes, as suggested with specific respect to neutropenia [103, 104]; however, further investigations targeted to skeletal cells are required to verify this hypothesis.
Current Therapies
At present, the only established cure for ARO is hematopoietic stem cell transplantation (HSCT): in fact, osteoclasts are cells of hematopoietic origin; thus, HSCT allows restoration of bone resorption by donor-derived cells. Here, we will not enter into details of this kind of approach, e.g., conditioning strategies, source of HSCs, type of donor, timing, and other undoubtedly important aspects, as they have been extensively reviewed by world experts in recent works (see for example [7, 72, 73, 105,106,107,108]). We will just briefly underline some concepts: first, molecular studies importantly contribute to define whether HSCT is appropriate. In fact, patients bearing mutations in the RANKL or OSTM1 gene are not candidate to this procedure: in the former group, the defect is not cell-autonomous, therefore cannot be corrected by HSCT; in the latter, severe neurological deficits are invariably present and preclude the patients any possibility of survival. For these patients, there is no approved cure at present.
Besides this, the severity of the clinical picture directs the treatment decision: mild forms, such as those associated with PLEKHM1, SLC29A3 or CTSK, or with CLCN7 dominant mutations, do not warrant all the risky and invasive procedures related to HSCT. In these cases, only symptomatic treatments to relieve the complications of the disease (such as fractures, dental defects, otorhinolaryngological problems) are applied. On the other hand, in CLCN7-deficient ARO, a careful neurological assessment is recommended in order to evaluate the suitability of HSCT: the ascertainment of progressive neurodegeneration should discourage transplantation. Unfortunately, at present, in this subgroup, there are no specific genotype-phenotype correlations able to identify patients eligible to HSCT on the basis of the pure molecular data.
Finally, in the newly identified forms of the disease, there is not sufficient knowledge and/or expertise to define specific treatment advice in addition to the general considerations above mentioned.
Conclusions
Recent reports confirm the genetic heterogeneity of osteopetrosis, which constitutes a challenge for molecular diagnosis. In fact, more than ten genes have been involved in the pathogenesis of osteopetrosis, also comprising large genes. In the most frequently affected, a high number of different mutations have been identified: some of them are reported in many patients of different origin, others in single cases, and still novel ones are identified. For these reasons, next-generation sequencing (NGS), including both whole exome sequencing (WES) and gene-targeted panels, has entered the clinic as a tool for routine diagnostic procedures [109] This has the clear advantage to greatly expedite the analysis, thus potentially getting to a precise molecular diagnosis, relevant for prognosis and treatment, in a shorter time as compared to classical Sanger sequencing of candidate genes. In addition, WES has identified in single patients with peculiar phenotypes mutations in new genes already known to play a role in bone homeostasis: TRAF6, LRRK1, MITF, CSF1R, and RELA; genetic data in a single patient point to a possible, as yet undefined role of C16orf57 in bone. In some cases, the underlying pathogenetic mechanism still has to be better elucidated, even though data in literature already provide sufficient rationale to suspect a detrimental effect of the identified mutation. On the other hand, two classes of mutations, namely deep intronic and synonymous changes, have come on stage highlighting a possible limitation of WES. As a matter of fact, even though many noncoding regions are actually targeted by WES, standard workflow for variant selection usually consider only intronic changes close to canonical splice sites; in particular, variants at the end of reads tend to be neglected. So, if a mutation is located in these regions, it can be missed. In fact, we clearly demonstrated in two unrelated families the pathogenic effect of the deep intronic single-nucleotide changes found in the TCIRG1 gene initially disregarded by WES [16••]. Similarly, synonymous changes are commonly filtered out in a standard workflow for WES; actually, they are usually ignored also when identified by classic Sanger sequencing, based on the assumption that they are silent changes. As demonstrated by our group and by others in the framework of diverse diseases, this assumption is absolutely wrong in some cases [19••].
In conclusion, huge advances have been made in the elucidation of the genetic bases of osteopetrosis. Nonetheless, about 10% of cases lack a molecular classification; in these patients, new, unexpected genes could be affected or known genes could harbor elusive defects. In order to fill the gap, we will need to find strategies integrating the technological power of NGS technologies and a better capacity to interpret genomic variations, allowing fishing out what is clinically relevant among the tens of thousands of variants in each single exome [110].
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
•• Sobacchi C, Schulz A, Coxon FP, Villa A, Helfrich MH. Osteopetrosis: genetics, treatment and new insights into osteoclast function. Nat Rev Endocrinol. 2013;9(9):522–36. This review offered a comprehensive overview of the genetics, clinical aspects, cellular pathogenesis and treatment of osteopetrosis.
Sobacchi C, Villa A, Schulz A, Kornak U. CLCN7-Related Osteopetrosis. In: Pagon RA, Adam MP, Ardinger HH, Wallace SE, Amemiya A, Bean LJH, Bird TD, Ledbetter N, Mefford HC, Smith RJH, Stephens K, editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993–2017. 2007 Feb 12 [updated 2016 Jun 9].
Döffinger R, Smahi A, Bessia C, Geissmann F, Feinberg J, Durandy A, et al. X-linked anhidrotic ectodermal dysplasia with immunodeficiency is caused by impaired NF-kappaB signaling. Nat Genet. 2001;27(3):277–85.
Dupuis-Girod S, Corradini N, Hadj-Rabia S, Fournet JC, Faivre L, Le Deist F, et al. Osteopetrosis, lymphedema, anhidrotic ectodermal dysplasia, and immunodeficiency in a boy and incontinentia pigmenti in his mother. Pediatrics. 2002;109(6):e97.
Roberts CM, Angus JE, Leach IH, McDermott EM, Walker DA, Ravenscroft JC. A novel NEMO gene mutation causing osteopetrosis, lymphoedema, hypohidrotic ectodermal dysplasia and immunodeficiency (OL-HED-ID). Eur J Pediatr. 2010;169(11):1403–7.
Carlberg VM, Lofgren SM, Mann JA, Austin JP, Nolt D, Shereck EB, et al. Hypohidrotic ectodermal dysplasia, osteopetrosis, lymphedema, and immunodeficiency in an infant with multiple opportunistic infections. Pediatr Dermatol. 2014;31(6):716–21.
Miot C, Imai K, Imai C, Mancini AJ, Kucuk ZY, Kawai T, et al. Hematopoietic stem cell transplantation in 29 patients hemizygous for hypomorphic IKBKG/NEMO mutations. Blood. 2017;130(12):1456–67.
Sly WS, Whyte MP, Sundaram V, Tashian RE, Hewett-Emmett D, Guibaud P, et al. Carbonic anhydrase II deficiency in 12 families with the autosomal recessive syndrome of osteopetrosis with renal tubular acidosis and cerebral calcification. N Engl J Med. 1985;313(3):139–45.
Hu PY, Ernst AR, Sly WS, Venta PJ, Skaggs LA, Tashian RE. Carbonic anhydrase II deficiency: single-base deletion in exon 7 is the predominant mutation in Caribbean Hispanic patients. Am J Hum Genet. 1994;54(4):602–8.
Villa A, Guerrini MM, Cassani B, Pangrazio A, Sobacchi C. Infantile malignant, autosomal recessive osteopetrosis: the rich and the poor. Calcif Tissue Int. 2009;84(1):1–12.
Bollerslev J, Henriksen K, Nielsen MF, Brixen K, Van Hul W. Autosomal dominant osteopetrosis revisited: lessons from recent studies. Eur J Endocrinol. 2013;69(2):R39–57.
Qin A, Cheng TS, Pavlos NJ, Lin Z, Dai KR, Zheng MH. V-ATPases in osteoclasts: structure, function and potential inhibitors of bone resorption. Int J Biochem Cell Biol. 2012;44(9):1422–35.
Frattini A, Orchard PJ, Sobacchi C, Giliani S, Abinun M, Mattsson JP, et al. Defects in TCIRG1 subunit of the vacuolar proton pump are responsible for a subset of human autosomal recessive osteopetrosis. Nat Genet. 2000;25(3):343–6.
Sobacchi C, Frattini A, Orchard P, Porras O, Tezcan I, Andolina M, et al. The mutational spectrum of human malignant autosomal recessive osteopetrosis. Hum Mol Genet. 2001;10(17):1767–73.
Pangrazio A, Caldana ME, Lo Iacono N, Mantero S, Vezzoni P, Villa A, et al. Autosomal recessive osteopetrosis: report of 41 novel mutations in the TCIRG1 gene and diagnostic implications. Osteoporos Int. 2012;23(11):2713–8.
•• Palagano E, Blair HC, Pangrazio A, Tourkova I, Strina D, Angius A, et al. Buried in the middle but guilty: intronic mutations in the TCIRG1 gene cause human autosomal recessive osteopetrosis. J Bone Miner Res. 2015;30(10):1814–21. This manuscript highlighted the possible involvement of deep intronic mutations in disease pathogenesis, with relevant implications for WES data analysis.
Demir K, Nalbantoglu O, Karaer K, Korkmaz HA, Yildiz M, Tunc S, et al. Genetic diagnosis using whole exome analysis in two cases with malignant osteopetrosis of infancy. J Clin Res Pediatr Endocrinol. 2015;7(4):356–7.
Bahr TL, Lund T, Sando NM, Orchard PJ, Miller WP. Haploidentical transplantation with post-transplant cyclophosphamide following reduced-intensity conditioning for osteopetrosis: outcomes in three children. Bone Marrow Transplant. 2016;51:1546–8.
•• Palagano E, Susani L, Menale C, Ramenghi U, Berger M, Uva P, et al. Synonymous mutations add a layer of complexity in the diagnosis of human osteopetrosis. J Bone Miner Res. 2017;32(1):99–105. This manuscript highlighted the possible involvement of synonymous but not silent mutations in disease pathogenesis, with relevant implications for WES data analysis.
Zhang X, He J, Fu W, Wang C, Zhang Z. Novel mutations of TCIRG1 cause a malignant and mild phenotype of autosomal recessive osteopetrosis (ARO) in four Chinese families. Acta Pharmacol Sin 2017.
Leisle L, Ludwig CF, Wagner FA, Jentsch TJ, Stauber T. ClC-7 is a slowly voltage-gated 2Cl(−)/1H(+)-exchanger and requires Ostm1 for transport activity. EMBO J. 2011;30(11):2140–52.
•• Ludwig CF, Ullrich F, Leisle L, Stauber T, Jentsch TJ. Common gating of both CLC transporter subunits underlies voltage-dependent activation of the 2Cl-/1H+ exchanger ClC-7/Ostm1. J Biol Chem. 2013;288(40):28611–9. This and the previous work essentially contributed to the dissection of ClC7/Ostm1 pathophysiology.
Kornak U, Kasper D, Bösl MR, Kaiser E, Schweizer M, Schulz A, et al. Loss of the ClC-7 chloride channel leads to osteopetrosis in mice and man. Cell. 2001;104(2):205–15.
Chen X, Zhang K, Hock J, Wang C, Yu X. Enhanced but hypofunctional osteoclastogenesis in an autosomal dominant osteopetrosis type II case carrying a c.1856C>T mutation in CLCN7. Bone Res. 2016;4:16035.
Deng H, He D, Rong P, Xu H, Yuan L, Li L, et al. Novel CLCN7 mutation identified in a Han Chinese family with autosomal dominant osteopetrosis-2. Mol Pain 2016;12.
González-Rodríguez JD, Luis-Yanes MI, Inglés-Torres E, Arango-Sancho P, Cabrera-Sevilla JE, Duque-Fernández MR, et al. Can acetazolamide be used to treat diseases involving increased bone mineral density? Intractable Rare Dis Res. 2016;5(4):284–9.
Ledemazel J, Plantaz D, Pagnier A, Girard P, Lasfargue M, Hullo E, et al. Malignant infantile osteopetrosis: case report of a 5-month-old boy. Arch Pediatr. 2016;23(4):389–93.
Pang Q, Chi Y, Zhao Z, Xing X, Li M, Wang O, et al. Novel mutations of CLCN7 cause autosomal dominant osteopetrosis type II (ADO-II) and intermediate autosomal recessive osteopetrosis (IARO) in Chinese patients. Osteoporos Int. 2016;27(3):1047–55.
Piret SE, Gorvin CM, Trinh A, Taylor J, Lise S, Taylor JC, et al. Autosomal dominant osteopetrosis associated with renal tubular acidosis is due to a CLCN7 mutation. Am J Med Genet A. 2016;170(11):2988–92.
Zeng B, Li R, Hu Y, Hu B, Zhao Q, Liu H, et al. A novel mutation and a known mutation in the CLCN7 gene associated with relatively stable infantile malignant osteopetrosis in a Chinese patient. Gene. 2016;576(1 Pt 1):176–81.
Zheng H, Shao C, Zheng Y, He JW, Fu WZ, Wang C, et al. Two novel mutations of CLCN7 gene in Chinese families with autosomal dominant osteopetrosis (type II). J Bone Miner Metab. 2016;34(4):440–6.
Okamoto N, Kohmoto T, Naruto T, Masuda K, Komori T, Imoto I. Novel CLCN7 compound heterozygous mutations in intermediate autosomal recessive osteopetrosis. Hum Genome Var. 2017;4:17036.
Worby CA, Dixon JE. Sorting out the cellular functions of sorting nexins. Nat Rev Mol Cell Biol. 2002;3(12):919–31.
Zhou C, Wang Y, Peng J, Li C, Liu P, Shen X. SNX10 plays a critical role in MMP9 secretion via JNK-p38-ERK signaling pathway. J Cell Biochem 2017.
Aker M, Rouvinski A, Hashavia S, Ta-Shma A, Shaag A, Zenvirt S, et al. An SNX10 mutation causes malignant osteopetrosis of infancy. J Med Genet. 2012;49(4):221–6.
Pangrazio A, Fasth A, Sbardellati A, Orchard PJ, Kasow KA, Raza J, et al. SNX10 mutations define a subgroup of human autosomal recessive osteopetrosis with variable clinical severity. J Bone Miner Res. 2013;28(5):1041–9.
•• Stattin EL, Henning P, Klar J, McDermott E, Stecksen-Blicks C, Sandström PE, et al. SNX10 gene mutation leading to osteopetrosis with dysfunctional osteoclasts. Sci Rep. 2017;7(1):3012. This work contributed to unravel the mechanism elicited by SNX10 mutation in the pathogenesis of osteopetrosis.
Amirfiroozy A, Hamidieh AA, Golchehre Z, Rezamand A, Yahyaei M, Beiranvandi F, et al. A novel mutation in SNX10 gene causes malignant infantile Osteopetrosis. Avicenna J Med Biotechnol. 2017;9(4):205–8.
Xu M, Stattin EL, Murphy M, Barry F. Generation of induced pluripotent stem cells (ARO-iPSC1–11) from a patient with autosomal recessive osteopetrosis harboring the c.212+1G>T mutation in SNX10 gene. Stem Cell Res. 2017;24:51–4.
Lange PF, Wartosch L, Jentsch TJ, Fuhrmann JC. ClC-7 requires Ostm1 as a beta-subunit to support bone resorption and lysosomal function. Nature. 2006;440(7081):220–3.
Fischer T, De Vries L, Meerloo T, Farquhar MG. Promotion of Gαi3 subunit down-regulation by GIPN, a putative E3 ubiquitin ligase that interacts with RGS-GAIP. Proc Natl Acad Sci. 2003;100:8270–5.
Feigin ME, Malbon CC. OSTM1 regulates beta-catenin/Lef1 interaction and is required for Wnt/beta-catenin signaling. Cell Signal. 2008;20(5):949–57.
Pandruvada SN, Beauregard J, Benjannet S, Pata M, Lazure C, Seidah NG, et al. Role of Ostm1 cytosolic complex with kinesin 5B in intracellular dispersion and trafficking. Mol Cell Biol. 2015;36(3):507–21.
Chalhoub N, Benachenhou N, Rajapurohitam V, Pata M, Ferron M, Frattini A, et al. Grey-lethal mutation induces severe malignant autosomal recessive osteopetrosis in mouse and human. Nat Med. 2003;9(4):399–406.
Pangrazio A, Poliani PL, Megarbane A, Lefranc G, Lanino E, Di Rocco M, et al. Mutations in OSTM1 (grey lethal) define a particularly severe form of autosomal recessive osteopetrosis with neural involvement. J Bone Miner Res. 2006;21(7):1098–105.
• Shin B, Yu J, Park ES, Choi S, Yu J, Hwang JM, et al. Secretion of a truncated osteopetrosis-associated transmembrane protein 1 (OSTM1) mutant inhibits osteoclastogenesis through down-regulation of the B lymphocyte-induced maturation protein 1 (BLIMP1)-nuclear factor of activated T cells c1 (NFATc1) axis. J Biol Chem. 2014;289(52):35868–81. This work described a possible mechanism elicited by OSTM1 truncated protein products in the pathogenesis of osteopetrosis.
Ott CE, Fischer B, Schröter P, Richter R, Gupta N, Verma N, et al. Severe neuronopathic autosomal recessive osteopetrosis due to homozygous deletions affecting OSTM1. Bone. 2013;55(2):292–7.
Herebian D, Alhaddad B, Seibt A, Schwarzmayr T, Danhauser K, Klee D, et al. Coexisting variants in OSTM1 and MANEAL cause a complex neurodegenerative disorder with NBIA-like brain abnormalities. Eur J Hum Genet. 2017;25(9):1092–5.
Fujiwara T, Ye S, Castro-Gomes T, Winchell CG, Andrews NW, Voth DE, et al. PLEKHM1/DEF8/RAB7 complex regulates lysosome positioning and bone homeostasis. JCI Insight. 2016;1(17):e86330.
Marwaha R, Arya SB, Jagga D, Kaur H, Tuli A, Sharma M. The Rab7 effector PLEKHM1 binds Arl8b to promote cargo traffic to lysosomes. J Cell Biol. 2017;216(4):1051–70.
McEwan DG, Popovic D, Gubas A, Terawaki S, Suzuki H, Stadel D, et al. PLEKHM1 regulates autophagosome-lysosome fusion through HOPS complex and LC3/GABARAP proteins. Mol Cell. 2015;57(1):39–54.
Witwicka H, Jia H, Kutikov A, Reyes-Gutierrez P, Li X, Odgren PR. TRAFD1 (FLN29) interacts with Plekhm1 and regulates osteoclast acidification and resorption. PLoS One. 2015;10(5):e0127537.
Van Wesenbeeck L, Odgren PR, Coxon FP, Frattini A, Moens P, Perdu B, et al. Involvement of PLEKHM1 in osteoclastic vesicular transport and osteopetrosis in incisors absent rats and humans. J Clin Invest. 2007;117(4):919–30.
Del Fattore A, Fornari R, Van Wesenbeeck L, de Freitas F, Timmermans JP, Peruzzi B, et al. A new heterozygous mutation (R714C) of the osteopetrosis gene, pleckstrin homolog domain containing family M (with run domain) member 1 (PLEKHM1), impairs vesicular acidification and increases TRACP secretion in osteoclasts. J Bone Miner Res. 2008;23(3):380–91.
Bo T, Yan F, Guo J, Lin X, Zhang H, Guan Q, et al. Characterization of a relatively malignant form of osteopetrosis caused by a novel mutation in the PLEKHM1 gene. J Bone Miner Res. 2016;31(11):1979–87.
Tolar J, Teitelbaum SL, Orchard PJ. Osteopetrosis. N Engl J Med. 2004;351:2839–49.
Shah GN, Bonapace G, Hu PY, Strisciuglio P, Sly WS. Carbonic anhydrase II deficiency syndrome (osteopetrosis with renal tubular acidosis and brain calcification): novel mutations in CA2 identified by direct sequencing expand the opportunity for genotype-phenotype correlation. Hum Mutat. 2004;24(3):272.
Alhuzaim ON, Almohareb OM. Sherbeeni SM carbonic anhydrase II deficiency in a Saudi woman. Clin Med Insights Case Rep. 2015;8:7–10.
Pang Q, Qi X, Jiang Y, Wang O, Li M, Xing X, et al. Two novel CAII mutations causing carbonic anhydrase II deficiency syndrome in two unrelated Chinese families. Metab Brain Dis. 2015;30(4):989–97.
Alsharidi A, Al-Hamed M, Alsuwaida A. Carbonic anhydrase II deficiency: report of a novel mutation. CEN Case Rep. 2016;5:108–12.
Rognoni E, Ruppert R, Fässler R. The kindlin family: functions, signaling properties and implications for human disease. J Cell Sci. 2016;129(1):17–27.
Schmidt S, Nakchbandi I, Ruppert R, Kawelke N, Hess MW, Pfaller K, et al. Kindlin-3-mediated signaling from multiple integrin classes is required for osteoclast-mediated bone resorption. J Cell Biol. 2011;192(5):883–97.
Crazzolara R, Maurer K, Schulze H, Zieger B, Zustin J, Schulz AS. A new mutation in the KINDLIN-3 gene ablates integrin-dependent leukocyte, platelet, and osteoclast function in a patient with leukocyte adhesion deficiency-III. Pediatr Blood Cancer. 2015;62(9):1677–9.
Palagano E, Slatter MA, Uva P, Menale C, Villa A, Abinun M, et al. Hematopoietic stem cell transplantation corrects osteopetrosis in a child carrying a novel homozygous mutation in the FERMT3 gene. Bone. 2017;97:126–9.
Liu W, Zhang X. Receptor activator of nuclear factor-κB ligand (RANKL)/RANK/osteoprotegerin system in bone and other tissues (review). Mol Med Rep. 2015;11(5):3212–8.
•• Luo J, Yang Z, Ma Y, Yue Z, Lin H, Qu G, et al. LGR4 is a receptor for RANKL and negatively regulates osteoclast differentiation and bone resorption. Nat Med. 2016;22(5):539–46. This work identified LGR4 as an additional receptor for the essential osteoclastogenic cytokine RANKL; the implications of these data in bone pathophysiology still have to be completely understood.
• Schena F, Menale C, Caci E, Diomede L, Palagano E, Recordati C, et al. Murine Rankl-/- Mesenchymal Stromal Cells display an osteogenic differentiation defect improved by a RANKL-expressing lentiviral vector. Stem Cells. 2017;35(5):1365–77. This work first described a defect in the osteoblast lineage due to RANKL absence; the implications of these data in bone pathophysiology still have to be clarified and might extend well beyond RANKL-deficient ARO.
Sobacchi C, Frattini A, Guerrini MM, Abinun M, Pangrazio A, Susani L, et al. Osteoclast-poor human osteopetrosis due to mutations in the gene encoding RANKL. Nat Genet. 2007;39(8):960–2.
• Lo Iacono N, Pangrazio A, Abinun M, Bredius R, Zecca M, Blair HC, et al. RANKL cytokine: from pioneer of the osteoimmunology era to cure for a rare disease. Clin Dev Immunol. 2013;2013:412768. This work described RANKL-deficient ARO patients; to the best of our knowledge, this remains the only subgroup of ARO in which the bone defect is not corrected by HSCT.
Guerrini MM, Sobacchi C, Cassani B, Abinun M, Kilic SS, Pangrazio A, et al. Human osteoclast-poor osteopetrosis with hypogammaglobulinemia due to TNFRSF11A (RANK) mutations. Am J Hum Genet. 2008 Jul;83(1):64–76.
• Pangrazio A, Cassani B, Guerrini MM, Crockett JC, Marrella V, Zammataro L, et al. RANK-dependent autosomal recessive osteopetrosis: characterization of five new cases with novel mutations. J Bone Miner Res. 2012;27(2):342–51. This work described RANK-deficient ARO patients and clearly highlighted the differences with the RANKL-dependent subgroup of osteoclast-poor ARO patients.
Porta F, Cavagnini S, Imberti L, Sottini A, Bolda F, Beghin A, et al. Partial depletion of TCR alpha/beta+/CD19+ cells in matched unrelated transplantation of three patients with osteopetrosis. Bone Marrow Transplant. 2015;50(12):1583–5.
Natsheh J, Drozdinsky G, Simanovsky N, Lamdan R, Erlich O, Gorelik N, et al. Improved outcomes of hematopoietic stem cell transplantation in patients with infantile malignant osteopetrosis using fludarabine-based conditioning. Pediatr Blood Cancer. 2016;63(3):535–40.
Simanovsky N, Rozovsky K, Hiller N, Weintraub M, Stepensky P. Extending the spectrum of radiological findings in patients with severe osteopetrosis and different genetic backgrounds. Pediatr Blood Cancer. 2016;63(7):1222–6.
Shamriz O, Shaag A, Yaacov B, NaserEddin A, Weintraub M, Elpeleg O, et al. The use of whole exome sequencing for the diagnosis of autosomal recessive malignant infantile osteopetrosis. Clin Genet. 2017;92(1):80–5.
Campeau PM, Lu JT, Sule G, Jiang MM, Bae Y, Madan S, et al. Whole-exome sequencing identifies mutations in the nucleoside transporter gene SLC29A3 in dysosteosclerosis, a form of osteopetrosis. Hum Mol Genet. 2012;21(22):4904–9.
Turan S, Mumm S, Gottesman GS, Abali S, Baş S, Atay Z, et al. Dysosteosclerosis from a unique mutation in SLC29A3. Presented at the 7th International Conference on Children’s Bone Health 2015, Salzburg, Austria. Bone Abstracts 4:97.
Gelb BD, Shi GP, Chapman HA, Desnick RJ. Pycnodysostosis, a lysosomal disease caused by cathepsin K deficiency. Science. 1996;273(5279):1236–8.
Novinec M, Lenarčič B. Cathepsin K: a unique collagenolytic cysteine peptidase. Biol Chem. 2013;394(9):1163–79.
Christensen J, Shastri VP. Matrix-metalloproteinase-9 is cleaved and activated by cathepsin K. BMC Res Notes. 2015;8:322.
Bonnet N, Brun J, Rousseau JC, Duong LT, Ferrari SL. Cathepsin K controls cortical bone formation by degrading periostin. J Bone Miner Res. 2017;32(7):1432–41.
Xue Y, Cai T, Shi S, Wang W, Zhang Y, Mao T, et al. Clinical and animal research findings in pycnodysostosis and gene mutations of cathepsin K from 1996 to 2011. Orphanet J Rare Dis. 2011;6:20.
Xue Y, Wang L, Xia D, Li Q, Gao S, Dong M, et al. Dental abnormalities caused by novel compound heterozygous CTSK mutations. J Dent Res. 2015;94(5):674–81.
Singh A, Cuevas-Covarrubias S, Pradhan G, Gautam VK, Messina-Baas O, Gonzalez-Huerta LM, et al. Novel mutation and white matter involvement in an Indian child with pycnodysostosis. Indian J Pediatr. 2015;82(5):471–3.
Huang X, Qi X, Li M, Wang O, Jiang Y, Xing X, et al. A mutation in CTSK gene in an autosomal recessive pycnodysostosis family of Chinese origin. Calcif Tissue Int. 2015;96(5):373–8.
Araujo TF, Ribeiro EM, Arruda AP, Moreno CA, de Medeiros PF, Minillo RM, et al. Molecular analysis of the CTSK gene in a cohort of 33 Brazilian families with pycnodysostosis from a cluster in a Brazilian northeast region. Eur J Med Res. 2016;21(1):33.
Mandal K, Ray S, Saxena D, Srivastava P, Moirangthem A, Ranganath P, et al. Pycnodysostosis: mutation spectrum in five unrelated Indian children. Clin Dysmorphol. 2016;25(3):113–20.
Rovira Martí P, Ullot FR. Orthopaedic disorders of pycnodysostosis: a report of five clinical cases. Int Orthop. 2016;40(11):2221–31.
Song HK, Sohn YB, Choi YJ, Chung YS, Jang JH. A case report of pycnodysostosis with atypical femur fracture diagnosed by next-generation sequencing of candidate genes. Medicine (Baltimore). 2017;96(12):e6367.
Lomaga MA, Yeh WC, Sarosi I, Duncan GS, Furlonger C, Ho A, et al. TRAF6 deficiency results in osteopetrosis and defective interleukin-1, CD40, and LPS signaling. Genes Dev. 1999;13(8):1015–24.
• Weisz Hubshman M, Basel-Vanagaite L, Krauss A, Konen O, Levy Y, Garty BZ, et al. Homozygous deletion of RAG1, RAG2 and 5′ region TRAF6 causes severe immune suppression and atypical osteopetrosis. Clin Genet. 2017;91(6):902–7. This work suggested a role for TRAF6 in the pathogenesis of human osteopetrosis.
• Iida A, Xing W, Docx MFK, Nakashima T, Wang Z, Kimizuka M, et al. Identification of biallelic LRRK1 mutations in osteosclerotic metaphyseal dysplasia and evidence for locus heterogeneity. J Med Genet. 2016;53:568–74. This work suggested a possible pathogenetic role of LRRK1 recessive mutations in a peculiar form of osteopetrosis.
Xing WR, Goodluck H, Zeng C, Mohan S. Role and mechanism of action of leucine-rich repeat kinase 1 in bone. Bone Res. 2017;5:17003.
Lu SY, Li M, Lin YL. Mitf regulates osteoclastogenesis by modulating NFATc1 activity. Exp Cell Res. 2014;328(1):32–43.
Steingrímsson E, Moore KJ, Lamoreux ML, Ferré-D'Amaré AR, Burley SK, Zimring DC, et al. Molecular basis of mouse microphthalmia (mi) mutations helps explain their developmental and phenotypic consequences. Nat Genet. 1994;8(3):256–63.
• George A, Zand DJ, Hufnagel RB, Sharma R, Sergeev YV, Legare JM, et al. Biallelic mutations in MITF cause coloboma, osteopetrosis, microphthalmia, macrocephaly, albinism, and deafness. Am J Hum Genet. 2016;99(6):1388–94. This work suggested a possible pathogenetic role of MITF recessive mutations in a peculiar form of osteopetrosis.
• Frederiksen AL, Larsen MJ, Brusgaard K, Novack DV, Thii Knudsen PJ, Daa Schroder H, et al. Neonatal high bone mass with first mutation of the NF-kB complex: heterozygous de novo missense (p.Asp512Ser) RELA (Rela/p65). J Bone Miner Res. 2016;31(1):163–72. This work suggested a possible pathogenetic role of a RELA mutation in a form of neonatal High Bone Mass.
Dai XM, Ryan GR, Hapel AJ, Dominguez MG, Russell RG, Kapp S, et al. Targeted disruption of the mouse colony-stimulating factor 1 receptor gene results in osteopetrosis, mononuclear phagocyte deficiency, increased primitive progenitor cell frequencies, and reproductive defects. Blood. 2002;99(1):111–20.
• Monies D, Maddirevula S, Kurdi W, Alanazy MH, Alkhalidi H, Al-Owain M, et al. Autozygosity reveals recessive mutations and novel mechanisms in dominant genes: implications in variant interpretation. Genet Med. 2017. This work suggested a possible pathogenetic role of CSF1R mutations in two ARO patients.
Migliaccio S, Luciani M, Taranta A, De Rossi G, Minisola S, El Hachem M, et al. Association of intermediate osteopetrosis with poikiloderma. J Bone Miner Res. 1999;14(5):834–6.
Mroczek S, Krwawicz J, Kutner J, Lazniewski M, Kuciński I, Ginalski K, et al. C16orf57, a gene mutated in poikiloderma with neutropenia, encodes a putative phosphodiesterase responsible for the U6 snRNA 3′ end modification. Genes Dev. 2012;26(17):1911–25.
• Colombo EA, Bazan JF, Negri G, Gervasini C, Elcioglu NH, Yucelten D, et al. Novel C16orf57 mutations in patients with Poikiloderma with Neutropenia: bioinformatic analysis of the protein and predicted effects of all reported mutations. Orphanet J Rare Dis. 2012;7:7. This work identified C16orf57 as the gene mutated in a patient displaying osteopetrosis, poikiloderma and neutropenia.
Colombo EA, Carra S, Fontana L, Bresciani E, Cotelli F, Larizza L. A zebrafish model of Poikiloderma with neutropenia recapitulates the human syndrome hallmarks and traces back neutropenia to the myeloid progenitor. Sci Rep. 2015;5:15814.
Patil P, Uechi T, Kenmochi N. Incomplete splicing of neutrophil-specific genes affects neutrophil development in a zebrafish model of poikiloderma with neutropenia. RNA Biol. 2015;12(4):426–34.
Schulz AS, Moshous D, Steward CG, Villa A, Sobacchi C. Osteopetrosis–Consensus Guidelines of the ESID and the EBMT Working Party Inborn Errors [online], https://esid.org/layout/set/print/content/view/full/14267.
Orchard PJ, Fasth AL, Le Rademacher J, He W, Boelens JJ, Horwitz EM, et al. Hematopoietic stem cell transplantation for infantile osteopetrosis. Blood. 2015;126(2):270–6.
Chiesa R, Ruggeri A, Paviglianiti A, Zecca M, Gónzalez-Vicent M, Bordon V, et al. Outcomes after unrelated umbilical cord blood transplantation for children with Osteopetrosis. Biol Blood Marrow Transpl. 2016;22(11):1997–2002.
Wu CC, Econs MJ, DiMeglio LA, Insogna KL, Levine MA, Orchard PJ, et al. Diagnosis and management of osteopetrosis: consensus guidelines from the Osteopetrosis Working Group. J Clin Endocrinol Metab. 2017;102(9):3111–23.
Jamuar SS, Tan EC. Clinical application of next-generation sequencing for Mendelian diseases. Hum Genomics. 2015;9:10.
Frebourg T. The challenge for the next generation of medical geneticists. Hum Mutat. 2014;35(8):909–11.
Acknowledgements
We acknowledge the many authors whose original contribution in the field could not be cited in this minireview for the sake of brevity.
Funding
This work was partially supported by the European Community’s Seventh Framework Program (FP7/2007–2013, SYBIL Project), by PRIN Projects (20102M7T8X_003 and 2015F3JHMB_004) to AV and by Programma Nazionale per la Ricerca-Consiglio Nazionale delle Ricerche Aging Project to AV, and by Ministero della Salute - Giovani Ricercatori (grant GR-2011-02348266) to CS.
Author information
Authors and Affiliations
Contributions
All the authors contributed to organize, draft, and revise the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Eleonora Palagano, Cristina Sobacchi, Anna Villa, and Ciro Menale declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Genetics
Rights and permissions
About this article
Cite this article
Palagano, E., Menale, C., Sobacchi, C. et al. Genetics of Osteopetrosis. Curr Osteoporos Rep 16, 13–25 (2018). https://doi.org/10.1007/s11914-018-0415-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-018-0415-2