Abstract
Purpose of the Review
Mounting evidence supports a role of low-grade inflammation in the pathophysiology of osteoarthritis (OA). We review and discuss the role of synovitis, complement activation, cytokines, and immune cell population in OA.
Recent Findings
Using newer imaging modalities, synovitis is found in the majority of knees with OA. Complement activation and pro-inflammatory cytokines play a significant role in the development of cartilage destruction and synovitis. Immune cell infiltration of OA synovial tissue by sub-populations of T cells and activated macrophages correlates with OA disease progression and pain.
Summary
The innate and acquired immune system plays a key role in the low-grade inflammation found associated with OA. Targets of these pathways my hold promise for future disease-modifying osteoarthritis drugs (DMOADs).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoarthritis (OA) is a degenerative multifactorial joint disease, characterized by progressive joint failure with pain and disability. OA involves breakdown and loss of articular cartilage, bone deformation, and synovial inflammation [1, 2]. Studies have shown a direct role for inflammatory factors in OA pathogenesis, which now define OA as no longer simply the result of “wear and tear” biomechanical processes [3]. The interaction between trauma and chronic inflammation has been described as a “triggering factor” that activates the immune responses in OA pathogenesis [4].
Synovial Inflammation and OA
OA has traditionally been considered a pathological response to abnormal joint loading and mechanics but low-grade synovitis is now recognized as a common finding [5•]. Many authors agree that in OA patients, the grade of synovitis is frequently associated with: increased local cartilage damage and pain [6]. Depending on the diagnostic technique and the selection criteria for OA patients, synovitis may occur in the majority of patients. Localized proliferative and inflammatory changes of synovium occur in up to 50% of OA patients suggested by arthroscopic studies [7]. The prevalence of synovial hypertrophy detected by ultrasound (US) in OA of the knees was analyzed by meta-analysis and found that synovial hypertrophy was present in 41.5% (95% CI 26.3 to57.7) of patients with knee OA compared to 14.5% (95% CI 0–58.81) of control subjects without OA [8]. MRI assessment of a thousand knee OA patients revealed synovial inflammation, measured by synovial hypertrophy and synovial enhancement, in 60% of OA patients [9]. Whether synovitis is causative of OA or a consequence of joint failure is still not clear; however, synovitis and bone marrow lesions, detected by contrast- enhanced MRI (ceMRI) or Doppler US, have revealed that synovitis and/or bone marrow lesions are predictive of incident OA and the severity of synovitis predicts OA progression [10,11,12,13,14,15,16]. These data are highly suggestive that synovitis may play a pathological role in OA.
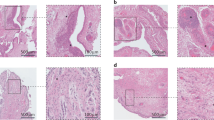
Histopathology of OA Synovium
Synovium is constructed of an outer layer, subintima, and an inner layer, intima, and functions to produce and retain synovial fluid in the joint. Typically, the subintima is composed of dense fibrous tissue, type I collagen, adipose tissue, and includes lymphatic vessels, nerve fibers, and microvascular blood vessels [17]. The intima is usually 1–4 cells thick and includes synoviocytes, macrophages, and fibroblasts [17]. In OA, synovial lining hyperplasia, sublining fibrosis, and neovascularization of the stroma occur with infiltration of predominantly macrophages and T cells and some mast cells, B cells, plasma cells, and NK cells [5•]. However, another study suggests that the grade of macrophage infiltration is increased in early OA [18]. Unlike RA synovitis, lymphoid aggregates and germinal center formation are rarely seen in OA synovial samples [19]. Cumulatively, these studies support a model of OA development that includes local damage to the articular cartilage, release of danger-associated molecular patterns (DAMPs) that stimulate macrophage activation, release of pro-inflammatory cytokine and chemokines that lead to recruitment of more macrophages and lymphocytes, increase in angiogenesis, and promotion of chondrocyte dysregulation that leads to secretion of metalloproteinases, pro-inflammatory cytokines, and prostaglandins that induce more cartilage destruction [20] (Fig. 1).
Components of low-grade inflammation associated with osteoarthritis. Multiple inflammatory pathways and mechanisms contribute to the pathogenesis of OA. Tissue injury from trauma, mechanical disturbances, and other mediators including obesity predispose the joint to complement activation and cartilage destruction releasing disease-associated molecular patterns (DAMPS) that can stimulate macrophages and chondrocytes via toll-like receptors (TLRs) to secrete chemokines like CCL2, aggrecanases, metalloproteinases, and pro-inflammatory cytokines like TNF-α and IL-1β. Additional macrophages, T cells, and mast cells are recruited leading to mild synovitis and continued cartilage degradation
The Role of Chemokines in OA
There are two well-documented events in OA and their manifestation as synovitis. The first is the infiltration of monocytes and macrophages in the synovial tissue and the second is the increase of cytokines and chemokines in the synovial tissue and synovial fluid [21, 22••]. The infiltration of immune cells in the synovium of OA primarily reflects migration rather than local proliferation and therefore is dependent on soluble mediators, especially chemokines [23]. Chemokines are a family of low-molecular-weight secretory proteins that induce immune cell migration as well as cell activation, angiogenesis, and pain responses and inflammation [23]. Currently, four subfamilies of chemokine receptors have been classified based on the chemokine ligands to which they bind. The relationship between chemokines and their receptors is complex because a given chemokine can bind to several receptors, and each receptor may bind to multiple chemokines. In OA, chemokines are produced by a variety of cells including synovial macrophages and fibroblasts, chondrocytes, and osteoblasts activated by inflammatory mediators or by mechanical stress [23]. Chemokines expressed by human chondrocytes include IL-8/CXCL-8, GROα/CXCL-1, MCP-1/CCL-2, RANTES/CCL-5, MIP-1α/CCL-3, and MIP-1β/CCL-4, and some of them are over-expressed in OA [24, 25].
CCL2 is also known as monocyte chemotactic protein 1 (MCP-1) and has been extensively studied in human OA and animal models of OA [26]. Synovial fluid levels of CCL2 positively correlate with pain and physical disability in patients with OA [27]. Similarly, OA-related pain is significantly decreased in mice deficient in the receptor for CCL2, CCR2, in a destabilized medial meniscus (DMM) model of OA [28]. In this study, cartilage damage and proteoglycan loss were not severe and were not significantly different between wild type and CCR2-deficient mice [28]. However, a recent study showed significant decreases in DMM-induced OA in mice lacking CCR2 or CCL2 [21]. Protection from DMM-induced OA was associated with significantly reduced joint macrophage infiltration [21]. Furthermore, synovial fluid from OA patients had significant levels of CCR2 ligands, including CCL2, CCL7, and CCL8, and synovial biopsies had abundant CCR2+ macrophages that lined, invaded, and were associated with OA cartilage erosions [21]. Importantly, blockade of CCL2/CCR2 signaling significantly attenuated macrophage accumulation, synovitis, and cartilage damage induced by DMM in mice [21]. A third study found that mice deficient in CCR2 or CCL2 had decreased synovial inflammation and delayed pain behavior but only CCR2-deficient mice were protected from developing OA at 20 weeks [29]. Human articular chondrocytes express CCR2, and CCL2 induces increased expression of MMP-3 and proteoglycan loss in vitro [26]. Highlighting the possible role of CCL2 in human OA, a single nucleotide polymorphism study of CCL2 gene found both OA disease-associated and OA protective variants [30]. Taken together, these data support a significant role for CCL2/CCR2 in trauma-induced OA but further studies are needed to establish a role of CCR2 in age or high-fat diet-induced OA.
CCR5 and its ligands CCL5 (RANTES), CCL4 (MIP-1β), and CCL3 (MIP-1α) have also been evaluated in OA [26]. CCL5 and CCL4 levels have been reported to be increased in the OA synovial fluid [31]. However, a more recent paper found no increase in CCL5 or CCL3 in OA samples that had high levels of CCL2 [21]. This study also showed that mice deficient in CCR5 or CCL5 were not protected from DMM-induced OA [21]. In contrast, Takebe et al. found that CCR5-deficient mice were partially protected from DMM-induced OA, with reduced cartilage damage but similar synovitis and bone changes as WT mice [32]. Further studies are needed to determine a role of CCR5 or its ligands in OA.
Other chemokines, such as CXCR2, may have a more homeostatic role in articular cartilage [33]. CXCR2 and its ligand CXCL6 are expressed in adult healthy articular cartilage; CXCL6 is retained in articular cartilage within the extracellular matrix and CXCL6 is not detected in advanced OA samples [33]. Mice with CXCR2 deficiency developed more severe DMM-induced OA with increased chondrocyte apoptosis compared to WT mice [33]. However, CXCR2-deficient mice did not develop spontaneous OA. Similarly, disruption of CXCR1/2 in human and CXCR2 signaling in mouse chondrocytes leads to decreased extracellular matrix production, reduced expression of chondrocyte differentiation markers, and increased chondrocyte apoptosis [34]. Additional studies are needed to determine if exogenous CXCL6 can restore articular chondrocyte health.
The Role of Complement in OA
The complement system is one of the “first lines of defense” in innate immunity, initiating a systemic danger response to cope with an insult [4]. It is composed by over 30 proteins, capable of inducing opsonization of pathogens, and initiating phagocytosis of its own cells and tissues when improperly regulated by inhibitors, autoantibodies, or mutations in complement components [35,36,37]. Complement activation can also increase vascular permeability, recruitment of phagocytic cells, augmentation of acute phase response, and stimulation of B and T lymphocytes [38, 39]. Three distinct pathways can activate the complement cascade. The classical and lectin pathways have their own specific pattern recognition molecules (PRMs), whereas the alternative pathway is activated by a spontaneous hydrolysis of C3 [40,41,42]. All pathways converge into the C3 and C5 convertases, enzymes responsible to mediate the formation of the membrane attack complex (MAC), composed by C5b-C9 [43]. This complex has been extensively demonstrated to lyse target cells through pore formation when deposited on cellular membranes [44]. Importantly, the complement system is involved in physiological and pathological processes in cartilage [45, 46].
Components of the classical (C1s and C4a) and alternative (factor B) pathways, C3 and C5, and the components of MAC are reported to be highly expressed in the synovial membrane and synovial fluid from OA patients with meniscal tears and cartilage degeneration [47,48,49,50,51]. The activation and deposition of complement factors are found in cartilage from OA patients as well as in animal models of OA [24]. Chondrocytes have been shown to synthesize complement components and synthesis can be upregulated by pro-inflammatory cytokines such as IL-1β and TNF-α in OA [51, 52]. Other components of the complement, such as C5a receptors, have been reported to be upregulated on the surface of chondrocytes in OA but not to the same extent as in RA [39]. MAC formation is induced in response to extracellular matrix (ECM) proteins, such as aggrecans, chondroadherin, fibromodulin, osteoadherin, COMP, and type II collagen [53, 54]. However, within the joint, MAC activation is directly or indirectly inhibited by proline/arginine-rich end leucine-rich repeat protein (PRELP), the NC4 domain of type IX collagen, biglycan, decorin, and COMP [42, 55]. This duality may explain why no correlation was seen between cartilage protein fragments and complement proteins in synovial fluid from patients with knee injury [40]. However, a series of recent studies clearly demonstrate the pathological function of the complement system in trauma-induced OA in mouse models.
DMM in mice deficient in C5 or C6 have reduced joint pathology, with less cartilage loss, osteophyte formation, and synovitis [53]. Chondrocytes from C5-deficient mice after DMM surgery also demonstrated lower mRNA expression levels of Jun and Fos pro-inflammatory transcriptional factors, whose expression is induced by MAC in OA [51, 56]. Mice deficient in MAC-inhibitor, CD59a, developed more severe OA as compared to WT mice using three mouse models of OA [53]. In addition, blocking complement activity with a pharmacological drug, such as CR2-fH, a fusion protein that inhibits activation of C3 and C5, attenuates the development of joint damage. In the same way, another study showed that carboxypeptidase B (CPB) appeared to have a protective effect against joint erosion in rheumatoid arthritis and OA by inactivating the complement system [57]. The same group observed that high levels of CPB in the synovial fluid from individuals with OA were associated with high levels of pro-inflammatory cytokines, and complement components which correlated positively with levels of MAC [53, 57]. Similar findings were seen in Cpb2-deficient mice that developed greater cartilage damage than WT mice and had a greater number of osteophytes and degree of synovitis [57]. In in vitro studies of complement activation assays, the CBP-treated serum suppressed the formation of MAC as well as MAC-induced hemolysis, suggesting that CPB has an anti-inflammatory role in OA [57]. Taken together, these data indicate that complement activation and regulation play a central role in trauma-induced OA.
The Role of Macrophages in OA
Macrophage infiltration is common in OA synovial hyperplasia and up to 90% of end-stage knee OA samples have significant infiltration of CD68+ macrophages [19]. Macrophages are the most abundant cells in OA synovium and produce pro-inflammatory cytokines including IL-1β and TNF-α known to induce cartilage breakdown [24]. Seventy-six percent of OA knees have accumulation of macrophages detected in vivo using etarfolatide labeling and SPECT-CT analysis of activated macrophages and the quantity of activated macrophages in the joint is significantly associated with knee pain (R = 0.60, p < 0.0001), joint space narrowing (R = 0.68, p = 0.007), and osteophytes (R = 0.66, p = 0.001) [58•]. These results are highly suggestive that synovitis with activated macrophage recruitment to the joint is pathogenic in OA.
Activated macrophages may develop in response to pathogen-associated molecular patterns (PAMPs) and endogenous DAMPS. Pattern recognition receptors (PRRs) are germ-line encoded innate immune receptors that recognize exogenous PAMPS and endogenous DAMPs. Major families of PRRs include Toll-like receptors (TLR), C-type lectin receptors (CLRs), nucleotide binding and oligomerization domain (NOD)-like receptor family, pyrin and HIN200 domain-containing (PYHIN) family, the RIG-1-like receptor (RLR) family, and oligoadenylate synthase (OAS) proteins. PRRs activate signaling pathways that collectively induce the production of cytokines as well as activation of NLR family, pyrin domain containing 3 (NALP3) inflammasomes, driving activation of caspase-1 and generating biologically active Il-1β and IL-18 and inducing pyroptosis or inflammatory cell death [59]. Dysregulated NALP3 inflammasome responses are commonly found in human diseases including Parkinson’s disease, Alzheimer’s disease, type 2 diabetes, gout, and obesity [59]. Multiple crystals, including uric acid (UA), calcium pyrophosphate, basic calcium phosphate (BCP) crystals such as hydroxyapatite (HA), activate inflammasomes leading to secretion of IL-1β and IL-18 within the joint and likely contributes to OA. NALP3 protein is over-expressed 5.4 fold in OA synovium compared to non-OA synovium [60]. HA crystal deposition and prevalence in joint fluid are found in up to 60% of OA patients and correlate with OA severity [61,62,63]. HA crystals activate the inflammasome in synovial macrophages, leading to IL-1β and IL-18 release into the synovial fluid targeting chondrocytes and synovial lining cells to up regulate cartilage-degrading enzymes and suppress extracellular matrix synthesis, resulting in joint destruction [64]. However, clinical trials using anti- IL-1β therapies have been disappointing [65]. Recent studies have shown that BCP crystals induce Syk, PI3K, and MAPK activation leading to IL-1β, MMP1, and generation of DAMP antigen S100A8 in human macrophages [66]. Syk inhibition effectively prevented these cellular responses and suggests that treatment with Syk inhibitors, several of which are currently in clinical trials for cancer and autoimmune disease, may be advantageous to prevent crystal- and DAMP- induced inflammation and cartilage damage.
The Role of T Cells in OA
A pathological role of T cells in OA is still uncertain but a significant body of literature indicates OA synovium has a rich population of T cells compared to healthy synovium [67, 68]. In OA synovium, T cells are second only to macrophages in frequency and may account for 20–25% of the inflammatory cells [69]. CD4+ T cells are enriched within synovial aggregates compared to CD8+ T cells [70] and OA synovial tissue has increased CD4+/CD8+ ratios approaching 5:1 in OA compared to 2:1 in healthy synovium [67, 68, 70, 71]. Unilateral versus bi-compartmental OA synovial membrane inflammatory cellular infiltrates also differ, with predominantly CD14+ macrophages in unilateral and both macrophages and CD4+ T cells in bilateral OA [72]. OA synovial T cells also have decreased expression of CD3zeta+ mRNA and protein compared to CD3epsilon suggesting that they are chronically stimulated [73]. When adjusted for age, sex, and body mass index (BMI), synovial CD4+ T cells, but not other immune cells, are associated with the pain visual analog scale (VAS) [74]. Peripherally, OA patients also have altered ratios of circulating CD4+/CD8+ T cell ratios [75]. Peripheral blood T cell populations are also altered in aged OA patients [71, 76, 77]. These data indicate that OA is associated with alterations in T cells locally within the joint and peripherally.
In both RA and OA, T regulatory (Tregs) cells (CD4+CD25+/high CD127/−) are increased in peripheral blood and synovial fluid, while Tregs are significantly elevated in RA synovium (p = 0.0335) compared to OA synovium [78]. Interestingly, the Tregs present in RA and OA synovium are very similar, displaying an activated effector memory phenotype (CD45RO + RA-, CD69, CD62L) and Treg functional markers CD152, CD154, CD274, CD279, and GITR [74]. However, despite the increased frequency of CD4 + CD25 + Foxp3+ Tregs in the blood of OA patients, these Tregs have lower secretion of IL-10, likely due to decreased expression of T cell inhibitory receptor T cell immunoglobulin and mucin domain-containing-3 (Tim-3) [79]. Another study found increased Tim-3 + CD4+ T cells in the peripheral blood of OA patients and found that galectin 9, a ligand for Tim-3, was increased in the synovial fluid in less severe grade 2 OA patients compared to grade 4 OA patients [80]. In the synovial fluid, surface Tim-3 was also higher on CD8+ T cells and CD14+ monocytes from grade 2 OA patients and lower in grade 4 OA patients [80]. Importantly, galectin 9 induced Tim-3 + CD4+ Th1 cell apoptosis, suggesting that galectin 9 may inhibit T cell-induced inflammation in early OA [80].
The role of effector T cells including Th1, Th2, Th9, Th22, and Th17 in OA has been recently reviewed [68]. Although pro-inflammatory Th1 cells, producing interferon-γ (IFN-γ) and TNF-α, are present in the sublining layer of synovial membranes of OA, they are much less frequent than in RA synovium [81,82,83]. Th2 cells, induced by IL-4, producing IL-10, IL-4, IL-5, and IL-13, are infrequent in OA synovium and synovial fluid [68]. There is controversy on alternations in OA synovium with some studies showing similar peripheral Th17 cell percentages as healthy controls [84, 85] and while another has shown an increased frequency or presence in OA synovium [77, 81]. Recent work investigated the percentage of T follicular helper (TFH) cells (CXCR5+, CD4+) and serum IL-21, IL-17A, and IFN-γ in 40 OA patients compared to 12 health controls [86]. CXCR5+, CD4+ TFH cell populations were increased in OA patients and the percent of TFH increased with OA grade [86]. Furthermore, OA patients compared to healthy controls had significantly elevated serum IL-21, IL-17A, and IFN-γ levels. Overall, the expression of IL-21 + TFH cells positively correlated with OA disease activity, CRP levels, and WOMAC. The newly described Th9 cells (CD4+ CD8- IL9+), producing IL-9, positively correlate with Western Ontario and McMaster Universities Osteoarthritis Index in OA patients and may represent a marker of disease activity [77]. Collectively, these studies are suggestive that T cells are dysregulated in OA but more data are needed to confirm a pathological role of individual subsets of T cells in OA.
The Role of Other Immune Cells in OA
OA synovial tissue includes other immune cells including B cells, plasma cells, mast cells, and NK cells [67, 74, 87]. While many studies have shown B cells present in low levels in OA, one study has shown moderate to strong B cell staining in 15% of OA patients while 54% had no B cell staining [88]. However, studies are lacking showing a correlation between B cell infiltration and OA progression or severity. NK cells are present in limited numbers in OA synovium and no evidence supports a significant role of NK cells in OA [89]. Synovial biopsies from 56 symptomatic OA and 49 RA patients revealed significantly more mast cells in the OA samples and a positive association between number of mast cells and KL grade [87]. Mechanical loading can induce mast cell degranulation [90]; however, activated mast cells as indicated by substance P are found in a minority (7%) of OA samples compared to 41% of RA synovial biopsies [91]. Additional studies are needed confirm a possible pathological role of mast cells or B cells in OA development.
Conclusion
Recent studies have provided significant mechanistic advances into the role of inflammation and immune cells in the pathophysiology of OA. Traumatic OA initiation clearly requires both complement activation and macrophage infiltration. Future studies aimed at testing local inhibition of complement activation or preventing macrophage infiltration in the immediate post-injury phase will help to determine if targeting these factors will reduce the progression to end-stage OA. Activated macrophages and T cell synovial infiltration predict pain and disease progression in OA but further studies are needed to identify how this low-level inflammation contributes to cartilage damage.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Litwic A, Edwards MH, Dennison EM, Cooper C. Epidemiology and burden of osteoarthritis. Br Med Bull. 2013;105:185–99.
Chen D, Shen J, Zhao W, Wang T, Han L, Hamilton JL, et al. Osteoarthritis: toward a comprehensive understanding of pathological mechanism. Bone research. 2017;5:16044.
Issa RI, Griffin TM. Pathobiology of obesity and osteoarthritis: integrating biomechanics and inflammation. Pathobiol Aging Age Relat Dis. 2012;2:2012.
Huber-Lang M, Kovtun A, Ignatius A. The role of complement in trauma and fracture healing. Semin Immunol. 2013;25(1):73–8.
• Mathiessen A, Conaghan PG. Synovitis in osteoarthritis: current understanding with therapeutic implications. Arthritis Res Ther. 2017;19(1):18. This is an excellent review of the various imaging modalities used to detect synovitis in OA as well as data on the longitudinal outcomes of OA symptoms as it relates to synovitis.
Liu-Bryan R, Terkeltaub R. Emerging regulators of the inflammatory process in osteoarthritis. Nat Rev Rheumatol. 2015;11(1):35–44.
Ayral X, Pickering EH, Woodworth TG, Mackillop N, Dougados M. Synovitis: a potential predictive factor of structural progression of medial tibiofemoral knee osteoarthritis—results of a 1 year longitudinal arthroscopic study in 422 patients. Osteoarthr Cartil. 2005;13(5):361–7.
Sarmanova A, Hall M, Moses J, Doherty M, Zhang W. Synovial changes detected by ultrasound in people with knee osteoarthritis—a meta-analysis of observational studies. Osteoarthr Cartil. 2016;24(8):1376–83.
Neogi T, Guermazi A, Roemer F, Nevitt MC, Scholz J, Arendt-Nielsen L, et al. Association of joint inflammation with pain sensitization in knee osteoarthritis: the Multicenter Osteoarthritis Study. Arthritis & rheumatology. 2016;68(3):654–61.
Wallace G, Cro S, Dore C, King L, Kluzek S, Price A, et al. Associations between clinical evidence of inflammation and synovitis in symptomatic knee osteoarthritis: a substudy of the VIDEO trial. Arthritis Care Res (Hoboken). 2016;
Jaremko JL, Jeffery D, Buller M, Wichuk S, McDougall D, Lambert RG, et al. Preliminary validation of the Knee Inflammation MRI Scoring System (KIMRISS) for grading bone marrow lesions in osteoarthritis of the knee: data from the Osteoarthritis Initiative. RMD Open. 2017;3(1):e000355.
Damman W, Liu R, Bloem JL, Rosendaal FR, Reijnierse M, Kloppenburg M. Bone marrow lesions and synovitis on MRI associate with radiographic progression after 2 years in hand osteoarthritis. Ann Rheum Dis. 2017;76(1):214–7.
Liu R, Damman W, Reijnierse M, Bloem JL, Rosendaal FR, Kloppenburg M. Bone marrow lesions on magnetic resonance imaging in hand osteoarthritis are associated with pain and interact with synovitis. Osteoarthr Cartil. 2017;
Mancarella L, Addimanda O, Cavallari C, Meliconi R. Synovial inflammation drives structural damage in hand osteoarthritis: a narrative literature review. Curr Rheumatol Rev. 2017;13(1):43–50.
Felson DT, Niu J, Neogi T, Goggins J, Nevitt MC, Roemer F, et al. Synovitis and the risk of knee osteoarthritis: the MOST Study. Osteoarthr Cartil. 2016;24(3):458–64.
Sharma L, Hochberg M, Nevitt M, Guermazi A, Roemer F, Crema MD, et al. Knee tissue lesions and prediction of incident knee osteoarthritis over 7 years in a cohort of persons at higher risk. Osteoarthr Cartil. 2017;25(7):1068–75.
Smith MD. The normal synovium. Open Rheumatol J. 2011;5:100–6.
Benito MJ, Veale DJ, FitzGerald O, van den Berg WB, Bresnihan B. Synovial tissue inflammation in early and late osteoarthritis. Ann Rheum Dis. 2005;64(9):1263–7.
Hugle T, Geurts J. What drives osteoarthritis?-synovial versus subchondral bone pathology. Rheumatology (Oxford, England). 2017;56(9):1461–71.
Berenbaum F. Osteoarthritis as an inflammatory disease (osteoarthritis is not osteoarthrosis)! Osteoarthr Cartil. 2013;21(1):16–21.
Raghu H, Lepus CM, Wang Q, Wong HH, Lingampalli N, Oliviero F, et al. CCL2/CCR2, but not CCL5/CCR5, mediates monocyte recruitment, inflammation and cartilage destruction in osteoarthritis. Ann Rheum Dis. 2017;76(5):914–22.
•• Rahmati M, Mobasheri A, Mozafari M. Inflammatory mediators in osteoarthritis: a critical review of the state-of-the-art, current prospects, and future challenges. Bone. 2016;85:81–90. This is an excellent and comprehensive review of inflammatory mediators, possible biomarkers, and cellular components of synovitis that mediate OA.
Bernardini G, Benigni G, Scrivo R, Valesini G, Santoni A. The multifunctional role of the chemokine system in arthritogenic processes. Curr Rheumatol Rep. 2017;19(3):11.
Haseeb A, Haqqi TM. Immunopathogenesis of osteoarthritis. Clinical immunology (Orlando, Fla). 2013;146(3):185–96.
Yang P, Tan J, Yuan Z, Meng G, Bi L, Liu J. Expression profile of cytokines and chemokines in osteoarthritis patients: proinflammatory roles for CXCL8 and CXCL11 to chondrocytes. Int Immunopharmacol. 2016;40:16–23.
Scanzello CR. Chemokines and inflammation in osteoarthritis: Insights from patients and animal models. Journal of orthopaedic research : official publication of the Orthopaedic Research Society. 2017;35(4):735–9.
Li L, Jiang BE. Serum and synovial fluid chemokine ligand 2/monocyte chemoattractant protein 1 concentrations correlates with symptomatic severity in patients with knee osteoarthritis. Ann Clin Biochem. 2015;52(Pt 2):276–82.
Miller RE, Tran PB, Das R, Ghoreishi-Haack N, Ren D, Miller RJ, et al. CCR2 chemokine receptor signaling mediates pain in experimental osteoarthritis. Proc Natl Acad Sci U S A. 2012;109(50):20602–7.
Miotla Zarebska J, Chanalaris A, Driscoll C, Burleigh A, Miller RE, Malfait AM, et al. CCL2 and CCR2 regulate pain-related behaviour and early gene expression in post-traumatic murine osteoarthritis but contribute little to chondropathy. Osteoarthr Cartil. 2017;25(3):406–12.
Hulin-Curtis SL, Bidwell JL, Perry MJ. Association between CCL2 haplotypes and knee osteoarthritis. International journal of immunogenetics. 2013;40(4):280–3.
Beekhuizen M, Gierman LM, van Spil WE, Van Osch GJVM, Huizinga TWJ, Saris DBF, et al. An explorative study comparing levels of soluble mediators in control and osteoarthritic synovial fluid. Osteoarthr Cartil. 2013;21(7):918–22.
Takebe K, Rai MF, Schmidt EJ, Sandell LJ. The chemokine receptor CCR5 plays a role in post-traumatic cartilage loss in mice, but does not affect synovium and bone. Osteoarthr Cartil. 2015;23(3):454–61.
Sherwood J, Bertrand J, Nalesso G, Poulet B, Pitsillides A, Brandolini L, et al. A homeostatic function of CXCR2 signalling in articular cartilage. Ann Rheum Dis. 2015;74(12):2207–15.
Karsdal MA, Bay-Jensen AC, Lories RJ, Abramson S, Spector T, Pastoureau P, et al. The coupling of bone and cartilage turnover in osteoarthritis: opportunities for bone antiresorptives and anabolics as potential treatments? Ann Rheum Dis. 2014;73(2):336–48.
Ricklin D, Hajishengallis G, Yang K, Lambris JD. Complement: a key system for immune surveillance and homeostasis. Nat Immunol. 2010;11(9):785–97.
Merle NS, Church SE, Fremeaux-Bacchi V, Roumenina LT. Complement system part i—molecular mechanisms of activation and regulation. Front Immunol. 2015;6:262.
Merle NS, Noe R, Halbwachs-Mecarelli L, Fremeaux-Bacchi V, Roumenina LT. Complement system part II: role in immunity. Front Immunol. 2015;6:257.
Carroll MC. The complement system in regulation of adaptive immunity. Nat Immunol. 2004;5(10):981–6.
Onuma H, Masuko-Hongo K, Yuan G, Sakata M, Nakamura H, Kato T, et al. Expression of the anaphylatoxin receptor C5aR (CD88) by human articular chondrocytes. Rheumatol Int. 2002;22(2):52–5.
Struglics A, Okroj M, Sward P, Frobell R, Saxne T, Lohmander LS, et al. The complement system is activated in synovial fluid from subjects with knee injury and from patients with osteoarthritis. Arthritis Res Ther. 2016;18(1):223.
Huber-Lang M, Ignatius A, Brenner RE. Role of complement on broken surfaces after trauma. Adv Exp Med Biol. 2015;865:43–55.
Happonen KE, Heinegard D, Saxne T, Blom AM. Interactions of the complement system with molecules of extracellular matrix: relevance for joint diseases. Immunobiology. 2012;217(11):1088–96.
Sturfelt G, Truedsson L. Complement in the immunopathogenesis of rheumatic disease. Nat Rev Rheumatol. 2012;8(8):458–68.
Scanzello CR, Goldring SR. The role of synovitis in osteoarthritis pathogenesis. Bone. 2012;51(2):249–57.
John T, Stahel PF, Morgan SJ, Schulze-Tanzil G. Impact of the complement cascade on posttraumatic cartilage inflammation and degradation. Histol Histopathol. 2007;22(7):781–90.
Ballanti E, Perricone C, di Muzio G, Kroegler B, Chimenti MS, Graceffa D, et al. Role of the complement system in rheumatoid arthritis and psoriatic arthritis: relationship with anti-TNF inhibitors. Autoimmun Rev. 2011;10(10):617–23.
Cantatore FP, Benazzo F, Ribatti D, Lapadula G, D’Amico S, Tursi A, et al. Early alteration of synovial membrane in osteoarthrosis. Clin Rheumatol. 1988;7(2):214–9.
Corvetta A, Pomponio G, Rinaldi N, Luchetti MM, Di Loreto C, Stramazzotti D. Terminal complement complex in synovial tissue from patients affected by rheumatoid arthritis, osteoarthritis and acute joint trauma. Clin Exp Rheumatol. 1992;10(5):433–8.
Konttinen YT, Ceponis A, Meri S, Vuorikoski A, Kortekangas P, Sorsa T, et al. Complement in acute and chronic arthritides: assessment of C3c, C9, and protectin (CD59) in synovial membrane. Ann Rheum Dis. 1996;55(12):888–94.
Gobezie R, Kho A, Krastins B, Sarracino DA, Thornhill TS, Chase M, et al. High abundance synovial fluid proteome: distinct profiles in health and osteoarthritis. Arthritis Res Ther. 2007;9(2):R36.
Orlowsky EW, Kraus VB. The role of innate immunity in osteoarthritis: when our first line of defense goes on the offensive. J Rheumatol. 2015;42(3):363–71.
Bradley K, North J, Saunders D, Schwaeble W, Jeziorska M, Woolley DE, et al. Synthesis of classical pathway complement components by chondrocytes. Immunology. 1996;88(4):648–56.
Wang Q, Rozelle AL, Lepus CM, Scanzello CR, Song JJ, Larsen DM, et al. Identification of a central role for complement in osteoarthritis. Nat Med. 2011;17(12):1674–9.
Melin Furst C, Morgelin M, Vadstrup K, Heinegard D, Aspberg A, Blom AM. The C-type lectin of the aggrecan G3 domain activates complement. PLoS One. 2013;8(4):e61407.
Kalchishkova N, Furst CM, Heinegard D, Blom AM. NC4 Domain of cartilage-specific collagen IX inhibits complement directly due to attenuation of membrane attack formation and indirectly through binding and enhancing activity of complement inhibitors C4B-binding protein and factor H. J Biol Chem. 2011;286(32):27915–26.
Freria CM, Velloso LA, Oliveira AL. Opposing effects of Toll-like receptors 2 and 4 on synaptic stability in the spinal cord after peripheral nerve injury. J Neuroinflammation. 2012;9:240.
Lepus CM, Song JJ, Wang Q, Wagner CA, Lindstrom TM, Chu CR, et al. Brief report: carboxypeptidase B serves as a protective mediator in osteoarthritis. Arthritis & Rheumatology. 2014;66(1):101–6.
• Kraus VB, McDaniel G, Huebner JL, Stabler TV, Pieper CF, Shipes SW, et al. Direct in vivo evidence of activated macrophages in human osteoarthritis. Osteoarthr Cartil. 2016;24(9):1613–21. This paper shows activated macrophages are very common in human OA in vivo.
Guo H, Callaway JB, Ting JPY. Inflammasomes: mechanism of action, role in disease, and therapeutics. Nat Med. 2015;21(7):677–87.
Clavijo-Cornejo D, Martinez-Flores K, Silva-Luna K, Martinez-Nava GA, Fernandez-Torres J, Zamudio-Cuevas Y, et al. The overexpression of NALP3 inflammasome in knee osteoarthritis is associated with synovial membrane prolidase and NADPH oxidase 2. Oxidative Med Cell Longev. 2016;2016:1472567.
Gibilisco PA, Schumacher HR Jr, Hollander JL, Soper KA. Synovial fluid crystals in osteoarthritis. Arthritis Rheum. 1985;28(5):511–5.
Fuerst M, Bertrand J, Lammers L, Dreier R, Echtermeyer F, Nitschke Y, et al. Calcification of articular cartilage in human osteoarthritis. Arthritis Rheum. 2009;60(9):2694–703.
Fuerst M, Niggemeyer O, Lammers L, Schafer F, Lohmann C, Ruther W. Articular cartilage mineralization in osteoarthritis of the hip. BMC Musculoskelet Disord. 2009;10:166.
Jin C, Frayssinet P, Pelker R, Cwirka D, Hu B, Vignery A, et al. NLRP3 inflammasome plays a critical role in the pathogenesis of hydroxyapatite-associated arthropathy. Proc Natl Acad Sci U S A. 2011;108(36):14867–72.
Robinson WH, Lepus CM, Wang Q, Raghu H, Mao R, Lindstrom TM, et al. Low-grade inflammation as a key mediator of the pathogenesis of osteoarthritis. Nat Rev Rheumatol. 2016;
Corr EM, Cunningham CC, Helbert L, McCarthy GM, Dunne A. Osteoarthritis-associated basic calcium phosphate crystals activate membrane proximal kinases in human innate immune cells. Arthritis Research & Therapy. 2017;19(1):23.
de Lange-Brokaar BJ, Ioan-Facsinay A, van Osch GJ, Zuurmond AM, Schoones J, Toes RE, et al. Synovial inflammation, immune cells and their cytokines in osteoarthritis: a review. Osteoarthr Cartil. 2012;20(12):1484–99.
Li YS, Luo W, Zhu SA, Lei GHT. Cells in osteoarthritis: alterations and beyond. Front Immunol. 2017;8:356.
Pessler F, Chen LX, Dai L, Gomez-Vaquero C, Diaz-Torne C, Paessler ME, et al. A histomorphometric analysis of synovial biopsies from individuals with Gulf War Veterans’ Illness and joint pain compared to normal and osteoarthritis synovium. Clin Rheumatol. 2008;27(9):1127–34.
Saito I, Koshino T, Nakashima K, Uesugi M, Saito T. Increased cellular infiltrate in inflammatory synovia of osteoarthritic knees. Osteoarthr Cartil. 2002;10(2):156–62.
Pawlowska J, Mikosik A, Soroczynska-Cybula M, Jozwik A, Luczkiewicz P, Mazurkiewicz S, et al. Different distribution of CD4 and CD8 T cells in synovial membrane and peripheral blood of rheumatoid arthritis and osteoarthritis patients. Folia Histochem Cytobiol. 2009;47(4):627–32.
Moradi B, Rosshirt N, Tripel E, Kirsch J, Barie A, Zeifang F, et al. Unicompartmental and bicompartmental knee osteoarthritis show different patterns of mononuclear cell infiltration and cytokine release in the affected joints. Clin Exp Immunol. 2015;180(1):143–54.
Sakkas LI, Koussidis G, Avgerinos E, Gaughan J, Platsoucas CD. Decreased expression of the CD3zeta chain in T cells infiltrating the synovial membrane of patients with osteoarthritis. Clin Diagn Lab Immunol. 2004;11(1):195–202.
Klein-Wieringa IR, de Lange-Brokaar BJ, Yusuf E, Andersen SN, Kwekkeboom JC, Kroon HM, et al. Inflammatory cells in patients with endstage knee osteoarthritis: a comparison between the synovium and the infrapatellar fat pad. J Rheumatol. 2016;43(4):771–8.
Hussein MR, Fathi NA, El-Din AM, Hassan HI, Abdullah F, Al-Hakeem E, et al. Alterations of the CD4(+), CD8 (+) T cell subsets, interleukins-1beta, IL-10, IL-17, tumor necrosis factor-alpha and soluble intercellular adhesion molecule-1 in rheumatoid arthritis and osteoarthritis: preliminary observations. Pathol Oncol Res. 2008;14(3):321–8.
Ponchel F, Burska AN, Hensor EM, Raja R, Campbell M, Emery P, et al. Changes in peripheral blood immune cell composition in osteoarthritis. Osteoarthr Cartil. 2015;23(11):1870–8.
Qi C, Shan Y, Wang J, Ding F, Zhao D, Yang T, et al. Circulating T helper 9 cells and increased serum interleukin-9 levels in patients with knee osteoarthritis. Clin Exp Pharmacol Physiol. 2016;43(5):528–34.
Moradi B, Schnatzer P, Hagmann S, Rosshirt N, Gotterbarm T, Kretzer JP, et al. CD4(+)CD25(+)/highCD127low/(-) regulatory T cells are enriched in rheumatoid arthritis and osteoarthritis joints—analysis of frequency and phenotype in synovial membrane, synovial fluid and peripheral blood. Arthritis Research & Therapy. 2014;16(2):R97.
Li S, Wan J, Anderson W, Sun H, Zhang H, Peng X, et al. Downregulation of IL-10 secretion by Treg cells in osteoarthritis is associated with a reduction in Tim-3 expression. Biomed Pharmacother. 2016;79:159–65.
Yang S, Wang J, Chen F, Liu G, Weng Z, Chen J. Elevated Galectin-9 Suppresses Th1 Effector Function and Induces Apoptosis of Activated CD4+ T Cells in Osteoarthritis. Inflammation. 2017;
Yamada H, Nakashima Y, Okazaki K, Mawatari T, Fukushi J, Oyamada A, et al. Preferential accumulation of activated Th1 cells not only in rheumatoid arthritis but also in osteoarthritis joints. J Rheumatol. 2011;38(8):1569–75.
Sakkas LI, Scanzello C, Johanson N, Burkholder J, Mitra A, Salgame P, et al. T cells and T-cell cytokine transcripts in the synovial membrane in patients with osteoarthritis. Clin Diagn Lab Immunol. 1998;5(4):430–7.
Ishii H, Tanaka H, Katoh K, Nakamura H, Nagashima M, Yoshino S. Characterization of infiltrating T cells and Th1/Th2-type cytokines in the synovium of patients with osteoarthritis. Osteoarthr Cartil. 2002;10(4):277–81.
Zhang L, Li JM, Liu XG, Ma DX, Hu NW, Li YG, et al. Elevated Th22 cells correlated with Th17 cells in patients with rheumatoid arthritis. J Clin Immunol. 2011;31(4):606–14.
Zhang L, Li YG, Li YH, Qi L, Liu XG, Yuan CZ, et al. Increased frequencies of Th22 cells as well as Th17 cells in the peripheral blood of patients with ankylosing spondylitis and rheumatoid arthritis. PLoS One. 2012;7(4):e31000.
Shan Y, Qi C, Liu Y, Gao H, Zhao D, Jiang Y. Increased frequency of peripheral blood follicular helper T cells and elevated serum IL21 levels in patients with knee osteoarthritis. Mol Med Rep. 2017;15(3):1095–102.
de Lange-Brokaar BJ, Kloppenburg M, Andersen SN, Dorjee AL, Yusuf E, Herb-van Toorn L, et al. Characterization of synovial mast cells in knee osteoarthritis: association with clinical parameters. Osteoarthr Cartil. 2016;24(4):664–71.
Da RR, Qin Y, Baeten D, Zhang YB. cell clonal expansion and somatic hypermutation of Ig variable heavy chain genes in the synovial membrane of patients with osteoarthritis. J Immunol. 2007;178(1):557–65.
Kummer JA, Tak PP, Brinkman BM, van Tilborg AA, Kamp AM, Verweij CL, et al. Expression of granzymes A and B in synovial tissue from patients with rheumatoid arthritis and osteoarthritis. Clin Immunol Immunopathol. 1994;73(1):88–95.
Fowlkes V, Wilson CG, Carver W, Goldsmith EC. Mechanical loading promotes mast cell degranulation via RGD-integrin dependent pathways. J Biomech. 2013;46(4):788–95.
Okamura Y, Mishima S, Kashiwakura JI, Sasaki-Sakamoto T, Toyoshima S, Kuroda K, et al. The dual regulation of substance P-mediated inflammation via human synovial mast cells in rheumatoid arthritis. Allergology international : official journal of the Japanese Society of Allergology. 2017;
Acknowledgements
This study was supported by Presbyterian Health Foundation (MBH) and Veterans Affairs PECASE (MBH).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Mary Beth Humphrey, Erika Barboza Prado Lopes, Adrian Filiberti, and Syed Ali Husain declare that they have no conflict of interest.
Human and Animal Rights
All report studies with human or animal subjects performed by the authors have been previously published and complied with all applicable ethical standards.
Additional information
This article is part of the Topical Collection on Osteoimmunology
Rights and permissions
About this article
Cite this article
Lopes, E.B.P., Filiberti, A., Husain, S.A. et al. Immune Contributions to Osteoarthritis. Curr Osteoporos Rep 15, 593–600 (2017). https://doi.org/10.1007/s11914-017-0411-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-017-0411-y