Abstract
Purpose of Review
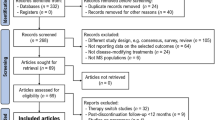
Long-term use of multiple sclerosis (MS) disease-modifying therapies (DMTs) is standard practice to prevent accumulation of disability. Immunosenescence and other age-related changes lead to an altered risk–benefit ratio for older patients on DMTs. This article reviews recent research on the topic of de-escalation and discontinuation of MS DMTs.
Recent Findings
Observational and interventional studies have shed light on what happens to patients who de-escalate or discontinue DMTs and the factors, such as age, treatment type, and presence of recent disease activity, that influence outcomes.
Summary
Though many questions remain, recent findings have been valuable for the development of an evidence-based approach to making de-escalation and discontinuation decisions in MS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The field of multiple sclerosis (MS) has experienced enormous advances in the last 30 years, exemplified by the introduction of over 20 disease-modifying therapies (DMTs), which have been shown in large-scale clinical trials to reduce the occurrence of relapses and slow the accumulation of disability. An individual diagnosed with MS now faces a significantly lower risk of reaching disability milestones compared to 30 years ago [1]. A drawback of these therapeutic advances is that patients are in most instances committed to a treatment course that may last many years, even decades. While maintenance medication is common to many chronic conditions, there are certain factors unique to MS and MS DMTs that argue against the type of therapeutic inertia in which indefinite treatment is seen as the default approach [2]. Escalating costs [3], the inconveniences of administration and monitoring (and in the US at least, of obtaining insurance authorization), side effects, and safety concerns associated with DMTs are burdens largely borne by patients and their families. As all presently available DMTs act in some fashion on the immune system, persistent treatment may make patients vulnerable to infections or other complications—risks that may increase with treatment duration or to which older people are particularly susceptible [4, 5]. In addition, medical comorbidities and disability may accumulate as people age, heightening the risks associated with certain DMTs. The COVID-19 pandemic was a wake-up call to many MS patients and their healthcare providers, putting into sharp relief the underappreciated dangers of a compromised immune system, and leading some to put DMTs on hold, temporarily or permanently. Older age [6, 7], greater levels of disability, and by some accounts certain MS DMTs [8, 9] were associated with worse outcomes in COVID-19 registries of MS patients, though COVID-19-associated morbidity and mortality have decreased since the early days of the pandemic.
Although some amount of risk may be unavoidable and outweighed by the advantages of DMT use, evidence from observational studies and interventional trials have shown that DMTs confer their greatest benefit in the first few years after disease onset, when overt signs of inflammation (relapses and new or active lesions on neuroimaging) occur with greatest frequency. Sub-group analyses from clinical trials of multiple MS DMTs show diminished efficacy in older age groups [10] (also reviewed by Jakimovski et al. [11] and Macaron et al. [12]). Despite the fact that about half of all people with MS in the US are at least 55 years of age, clinical trials of MS DMTs have mostly used an upper age limit of 55 in relapsing–remitting multiple sclerosis (RRMS), or up to 60 or 65 in some secondary progressive (SPMS) trials, thus limiting the conclusions one can draw about DMT safety and efficacy in older populations. With that caveat, a meta-analysis of DMT clinical trials involving 38 clinical trials and over 28,000 participants estimated that the average patient over age 53 does not benefit from DMT use in terms of disability progression [13]. Given the possibility of higher risk and lower benefit in older age and after years of DMT use, it is appropriate to ask whether continued treatment with expensive and potentially risky DMTs is in the best interest of some patients (not to mention health systems [14]). Doctors and patients are of course already making discontinuation decisions everyday: in MS studies involving large registries and healthcare claims databases, DMT use is consistently greater in younger patients compared to their older counterparts, many of whom presumably discontinued their DMT at some point (though others may have never been treated) [15,16,17]. Certainly, many MS providers can recall patients who have discontinued a DMT and remained stable at follow up visits. But when is it safe and appropriate for the neurologist to recommend permanent DMT discontinuation? What attributes of the patient, or of the treatment, suggest a higher likelihood of stability upon DMT discontinuation? Given the reluctance of many patients to discontinue a DMT altogether [18], are there safer or better tolerated strategies to de-escalate treatment, such as tapering the dose or extending the interval between treatments? This review aims to critically evaluate the literature of MS DMT discontinuation and de-escalation, introducing the reader to the different approaches to treating patients with MS over their lifetimes, exploring the concepts of aging and immunosenescence in MS, and examining outcomes from a variety of clinical studies on this topic. Where the evidence is murky or expert views diverge, we offer our opinion, recognizing that more research in this area is needed.
DMTs in Early Disease Course: Escalation vs Induction vs High-Efficacy Therapy
With more DMT options currently available and increasing recognition that disability accumulation frequently occurs independent of relapses (progression independent of relapse activity, or PIRA), even early in the course of MS and in the relapsing–remitting phase [19, 20], the initial choice of DMT is more important than ever. Evidence from multi-center cohort studies and population-based registries demonstrate that early initiation of high-efficacy DMTs appears to lead to better functional outcomes compared to lower efficacy DMTs, particularly in relapse-onset MS (these data largely predated the widespread use of high efficacy DMTs in primary progressive MS) [21,22,23,24,25]. Yet there remains some controversy about the optimal treatment algorithm for newly diagnosed patients, with some emphasizing an escalatory approach and others arguing for early use of high-efficacy DMTs [26, 27]. In the initial selection of DMT, drug availability may be limited by geographic location, regulatory structures, or payer authorization; patients may worry about the risk of possible adverse events; or prescribing options may simply be dictated by provider familiarity or risk aversion.
The need or desire to consider treatment de-escalation is frequently influenced by the specific DMT being used. One example of this is switching from natalizumab due to an increasing risk of progressive multifocal leukoencephalopathy (PML) with prolonged use [28] (more on this below). Some leukocyte-depleting MS DMTs also have a dose-dependent risk of toxicity (e.g. mitoxantrone, cladribine), so discontinuation or de-escalation becomes imperative. The decision to re-treat after an induction phase with a pulsed immune reconstitution therapy like alemtuzumab or cladribine may depend on whether disease reactivation has occurred [29, 30]. For example, in analysis of long-term outcomes of patients in the CLARITY/CLARITY Extension studies of cladribine, 46.9% (204/435) of participants had subsequent DMT use, mainly in the form of a platform DMT, at a median of 10.9 years since their last dose [31]. Similarly, while hematopoietic stem cell transplantation (HSCT) seemed to offer the promise of “one and done” with high rates of No Evidence of Disease Activity (NEDA) and event-free survival, some patients have nevertheless required subsequent DMT resumption [32]. By contrast, most traditional immunotherapies including glatiramer acetate, interferon β formulations, the fumarates (dimethyl fumarate, monomethyl fumarate, and diroximel fumarate), sphingosine-1-phosphate receptor (S1PR) modulators (fingolimod, siponimod, ozanimod, ponesimod), natalizumab, and anti-CD20 immunotherapies (rituximab, ocrelizumab, ublituximab, ofatumumab) require persistent administration to maintain efficacy. In the absence of safety or tolerability concerns, these DMTs might be continued for many years.
Aging and Immunosenescence in MS
Immunosenescence is defined as the age-related weakening of adaptive and innate immune systems including the differentiation and maturation of different immune subsets, immune cell functionality, and responsiveness to vaccinations [33,34,35,36,37]. Senescent immune cells change their secretory pattern to produce a more pro-inflammatory milieu (so-called “senescence-associated secretory phenotype” or SNAP), which in combination with accumulated cellular debris and self-antigens can lead to “inflammaging”—the low-grade inflammation present in older age that can contribute to tissue damage and degenerative diseases [33,34,35,36,37]. Alterations in B and T cell subsets, reduced diversity of B and T cell receptors, and diminished antibody production take place in older age, which helps to explain why extra vaccinations or higher vaccine doses are sometimes recommended in older populations. For example, in a single-center cohort study, reduced humoral response to hepatitis B vaccination was observed in older patients with MS, who were more likely to require a 4th vaccine dose to achieve seroprotection [38]. Aging resident central nervous system cells, such as astrocytes and microglia, lose their homeostatic functions and shift their secretory patterns toward a more pro-inflammatory profile [39, 40]. Remyelination efficiency diminishes with age as a result of failure of oligodendrocyte precursor cell recruitment and differentiation [41,42,43], which may be why older age is associated with worse recovery from MS relapses [44].
Age is the most consistently recognized modifier of MS disease course [33, 45]. Relapse rates are highest in the early years of the illness and seen at higher frequencies in pediatric MS than in adult-onset MS, and lowest rates in late-onset MS (with corresponding least to greatest proportions of primary progressive MS presentations in these age groups) [46,47,48,49]. After years of chronic inflammation and loss of neurological reserve, some relapse-onset MS patients transition to secondary progressive MS [45, 50, 51]. Atrophy occurs at an accelerated rate throughout the course of MS [52], though the MS-specific contribution wanes over time, specifically for whole brain and thalamic atrophy, while the contribution of normal aging to volume loss increases [53]. Consistent with these clinical and imaging observations, studies demonstrate evolution of pathological changes as patients age with MS [54,55,56]. The infiltration by B and T lymphocytes and formation of white matter plaques early in the disease process gives way to slow expansion of pre-existing lesions and gradual lymphocyte accumulation in connective tissue spaces of the brain such as the meninges and Virchow Robin spaces, while blood–brain barrier disruption subsides over time (seen on magnetic resonance imaging [MRIs] as reduced gadolinium-enhancing lesions with aging [57]). Age-associated changes in sex hormones, such as declines in testosterone levels in men and anti-Mullerian hormone in perimenopausal women, have been linked to brain atrophy and risk of disability progression in patients with MS, respectively [33].
Relative to controls, people with MS (particularly progressive MS) are at higher risk for infections and infection-associated hospitalizations, independent of DMTs, with absolute infection rates highest in the oldest age groups [58, 59]. Complicating this, use of MS DMTs, especially more immunosuppressive ones, can become riskier with longer use and in older individuals. As mentioned above, natalizumab-associated PML rates increase with longer treatment, particularly for those who test positive for antibodies to the JC virus [28]. JC virus seropositivity has been shown to increase with age [60]. In a study of the first 336 confirmed post-marketing cases of natalizumab-associated PML, older patients had a higher mortality [61], similar to what was found in a French population-based study of all PML cases from any cause over a 10-year span [62]. Meta-analyses of PML in MS have found earlier PML onset and worse outcomes in older patients [63, 64]. Prior to the availability of JC virus serological testing, many chose to de-escalate from natalizumab at the 2-year mark (after which PML risk rises faster), though our present practice is typically to continue natalizumab treatment beyond this point as long as the serum JC virus antibody remains negative with regular (e.g. at least every 6 months) blood monitoring. De-escalation from natalizumab, after JC virus seroconversion for example, was previously necessitated by the limited number of high efficacy alternatives; now with the availability of other effective options that carry lower risk of PML, “lateral moves” after natalizumab are possible.
Common medical co-morbidities such as diabetes, hypertension, and cardiac arrythmias become more prevalent in older individuals, potentially raising the risk for complications from fingolimod, for example. Though analysis of clinical trial data from 11 ocrelizumab clinical trials demonstrates an acceptable safety profile with up to 7 years of treatment [65], real world data suggest a higher risk of infections with B cell depletion with than other MS DMTs [66, 67]. Risk of infection increases with longer use of anti-CD20 immunotherapies and with hypogammaglobulinemia, itself a consequence of prolonged use of these DMTs [4, 68]. Wheelchair-bound patients taking rituximab are particularly susceptible to infections [4]. Whether newer anti-CD20 DMTs, such as ublituximab and ofatumumab, will face similar issues remains to be seen.
Certain MS DMTs impair the normal response to vaccinations, which may become increasingly important as people age (see Table 1). In a 2012 review of vaccinations in MS, the authors noted that large-scale and prospective studies of vaccinations with MS DMTs were scarce [69]. Studies have emerged to suggest largely preserved vaccine responses with interferon β, teriflunomide, alemtuzumab, and the fumarates, variably diminished responses with glatiramer acetate, and inadequate responses to various vaccinations with S1PR modulators, natalizumab, and anti-CD20 DMTs [38, 70,71,72,73,74,75]. Findings from a meta-regression of 45 MS clinical trials identified an age-dependent risk of neoplasm with use of depletive agents (alemtuzumab, cladribine, and ocrelizumab), particularly for patients older than 45 years [76]. Periodic reassessments of the DMT risk–benefit ratio in older individuals based on their unique risk factors would allow for a more personalized approach to care.
Discontinuation and De-escalation
Discontinuation
In 2018, the American Academy of Neurology issued practice guideline recommendations on MS DMTs, including a discussion of when to consider DMT discontinuation, but given the paucity of data in this area stopped short of making firm recommendations except for those with SPMS without recent disease activity and an Expanded Disability Status Scale (EDSS) of at least 7—unable to walk more than 5 m, largely restricted to a wheelchair— for 2 years (Level B) [77]. In an ideal world, patients contemplating DMT discontinuation would discuss the pros and cons with their neurologist before taking the leap. In the real world, these decisions are sometimes made independently by the patient and disclosed to the neurologist afterward (or not at all if the patient never returns). Treatment interruptions can occur as an intended step between two different DMTs (or for family planning purposes) and thus should be distinguished from a planned permanent discontinuation, though studies have historically not always made this distinction. (Discussion of DMTs and pregnancy is outside the scope of this review but is available elsewhere [78].) Patients choose to discontinue DMTs for a variety of reasons including cost, intolerable side effects, serious adverse events, (perceived or real) lack of efficacy, comorbid mental health disorders, and in our experience, the fact that taking a DMT reminds them of having MS [79,80,81,82,83,84]. Those with stable MS and minimal disability accrual over many years may in theory be good candidates for DMT discontinuation, though in a recent survey of 377 patients with MS, only 11.9% of respondents said they would consider DMT discontinuation if they had stable disease [18]. Patients who continue to progress despite DMTs tend to be the ones most interested in discontinuation. In the above survey, perceptions of DMT discontinuation appeared to be very influenced by the opinions of others, especially that of their neurologist. Regardless of how it happens, we have gained insights from the many patients who over the years have discontinued DMTs.
Observational cohort studies have identified cutoffs in middle-age after which DMT discontinuation is associated with a lower risk of disease activity. A small retrospective study of 22 DMT continuers and 13 DMT discontinuers over age 60 found that discontinuation did not influence clinical outcomes after a mean follow-up of 77.1 months [85]. In another small study, Yano et al. found that patients who discontinued after age 45 tended to have a stable course, while younger patients were more likely to experience clinical relapse or new MRI activity upon DMT discontinuation [86]. In an analysis of 132 DMT continuers and 366 discontinuers over age 50 followed for a median of 7 years, there was no difference in time to first relapse or time to disability progression between the groups, but discontinuation was associated with a higher risk of reaching an EDSS of 6 [87]. In a study of 100 SPMS discontinuers with a mean age of 47.2, annualized relapse rate remained stable at 1 and 3 years of follow up compared to on-treatment but 16 patients experienced an exacerbation and 19 had active lesions on MRI post-discontinuation [88]. A gadolinium-positive scan in the 3 years before discontinuation and EDSS < 6 were associated with relapse and/or MRI activity in this study. A study of the MSBase Registry found a similar time to first relapse between DMT continuers and propensity-score matched discontinuers, though time to disability progression was faster among discontinuers, driven by continued progression in those who had had progression prior to discontinuation [89]. In a subsequent study from the same MSBase Registry involving 4842 patients with a median age of 35.9 years, the risk of relapse following DMT discontinuation was higher in younger patients, female patients, and those with moderate disability and a relapse within 1 year of discontinuation [90]. A Dutch study of 130 patients who stopped first-line DMTs (87.7% with relapsing–remitting MS, with average age of 45.3 at DMT discontinuation) found an exceptionally high rate of disease activity—60% [91]. In this study, higher age was associated with lower risk and severity of MRI activity and lower risk of relapse: patients older than 45 had over 3 times lower risk of MRI activity compared to younger patients.
Hua et al. performed regression analyses for various longitudinal outcomes in a retrospective cohort of 600 patients of at least 60 years of age (178 of whom discontinued treatment) and found that stopping DMT appeared to have minimal effect on these outcomes, with very few (19) discontinuers subsequently reinitiating therapy [92]. A French cohort study of 232 discontinuers with a mean age of 52.8 years found that risk of disease reactivation varied by DMT: in the year after discontinuation of a first-line agent, fingolimod, or natalizumab, 6%, 9%, and 43% of patients suffered relapses, respectively [93]. Time to relapse after discontinuation did not differ in this study according to whether the patient was younger or older than 55, though time to first MRI activity was faster in the younger group. Examining discontinuation of high-efficacy therapy in MS patients 50 years and older, a separate French cohort study including 168 discontinuers and 1452 propensity-matched continuers found an increased risk of inflammatory activity in discontinuers, which was both age- and DMT-dependent [94]. In particular, discontinuers of natalizumab and fingolimod experienced a significant increased risk of disease reactivation, even among patients with inactive SPMS, whereas discontinuers of rituximab and ocrelizumab did not. A systematic review of 22 articles and 2942 patients who had discontinued DMTs for longer than 12 months found that the risk of relapse became negligible (defined as less than 1% per year) at about 60 years of age, and after either 10 years of DMT exposure, or 8 years of disease stability [95]. Since the average 60-year-old with MS has had a disease duration of 30 to 40 years, these studies are less relevant for individuals with late-onset MS, who in general are less likely to be treated with DMTs despite the fact that they reach disability milestones at faster rates than those with adult-onset MS [96]. The discrepancy in discontinuation ages among all these retrospective studies likely reflects cultural differences and heterogeneity in real-world prescribing practices; they also highlight the fact that age alone is insufficient to determine when to recommend DMT discontinuation.
In addition to age and disease duration, the recent presence of disease activity has been shown to predict likelihood of recurrence upon DMT discontinuation. Researchers using the large Innsbruck MS Database found that age greater than 45 years at discontinuation, absence of relapses for at least 4 years on DMT prior to discontinuation, and absence of contrast-enhancing lesions predicted freedom from relapses after discontinuation [97]. A follow-up study from the same group leveraging generation and validation datasets of DMT discontinuers confirmed the importance of age, MRI activity at discontinuation, and duration of clinical stability as independent risk factors for disease reactivation, and a predictive model consisting of these variables was able to robustly identify patients at high (83–85%), moderate (36–38%) and low (7%) risk of disease reactivation within 5 years [98]. Serological measurements of biomarkers such as neurofilament light (NfL) and glial fibrillary acidic protein (GFAP) may be helpful in predicting the likelihood of disease reactivation upon DMT cessation [99] though more research is needed in this area. More long-term observational discontinuation studies are also needed that include longer-acting agents such as anti-CD20 DMTs.
Until very recently, virtually all of the evidence for DMT discontinuation came from observational studies. The DISCOMS trial was the first multicenter randomized control trial (RCT) to test the hypothesis that DMT discontinuation was not inferior to treatment continuation in a typical population of middle-aged, stable MS patients [100]. Inclusion criteria specified at least 55 years of age, any MS subtype, no relapses in the preceding 5 years and no new MRI lesions in the prior 3 years. 6 (4.7%) of continuers and 16 (12.2%) of discontinuers had a relapse or new MRI activity during the trial. Given a non-inferiority margin of 8%, the null hypothesis was not rejected; discontinuation could not be declared non-inferior to continuation in this study. Nevertheless, the overall number of relapses in the trial was quite low—1 among continuers and 3 among discontinuers (no statistically significant difference on post-hoc analysis). Likewise, mean disability progression by EDSS or Symbol Digit Modality Test (SDMT, a cognitive test of psychomotor speed widely used in MS research) and number of individuals with confirmed disability progression did not differ between the two arms. At the start of the study, most participants felt “satisfied” or “very satisfied” (77% for continuers, 78% for discontinuers), and after 24 months, the proportion of satisfied participants remained stable among continuers while increasing to 91% among discontinuers (p = 0.0086). 15/22 (68.2%) of the events in DISCOMS consisted of 1–2 new brain lesions on MRI, with no association found between these and disability progression, raising a question about the clinical relevance of such radiographic changes.
The DOT-MS discontinuation RCT was halted prematurely in March 2023 after inflammatory activity (largely limited to MRI) emerged in 17.8% of the 45 participants who discontinued DMT, compared to none in those who continued DMT [101]. Like DISCOMS, the DOT-MS trial randomly assigned half the participants, who were stable for at least 5 years, to stop their DMTs, while the other half continued them. Compared to DISCOMS, DOT-MS enrolled participants who were an average of 9 years younger. Those who developed disease reactivation in DOT-MS were on average 8 years younger than those who remained stable, corroborating the effect of age on risk of disease activity.
STOP-I-SEP (NCT03653273) is an ongoing French multicenter RCT for patients with secondary progressive MS over age 50, with moderate baseline disability (EDSS ≥ 3), estimated to end in January 2028. The primary endpoint for this trial is the percentage of patients experiencing confirmed disability progression at 2 years. We are narrowing in on the optimal age for DMT discontinuation and will continue to gain insights about age and other factors associated with discontinuation success from this and future studies.
De-escalation and Rebound
As people age with MS, they may no longer experience any added benefit from high-efficacy DMTs but may still benefit from taking a low- or moderate-efficacy DMT. Analysis from our center found that younger patients tended to derive more benefit from highly effective DMTs (rituximab and natalizumab) compared to moderate efficacy oral agents (dimethyl fumarate and fingolimod), while patients older than 54.2 years benefitted equally with either approach [102] (in Weideman et al.’s meta-analysis, high-efficacy DMTs were superior to platform therapies only for those below 40.5 years [13]).
MS DMTs do not cause neurochemical changes like other medications or substances, such as opioids, whose discontinuation can unleash unopposed counter-regulatory forces and rapid withdrawal symptoms. Still, abrupt discontinuation of certain MS DMTs (or excessive gaps between DMTs) associated with lymphocyte trafficking or migration, such as natalizumab and the S1PR modulators, have been associated with the risk of rebound disease activity, even in those over age 50, though older patients may be at lower risk for disease reactivation [103,104,105,106,107] (see Fig. 1). De-escalation may not mitigate this risk. A prospective observational study of patients with MS transitioning from natalizumab to teriflunomide because of prior JC virus exposure found a low annualized relapse rate (ARR = 0.08) at 12 months, but 11 out of 55 (20%) had developed a new gadolinium-enhancing lesion [108]. Switching to interferon β from natalizumab resulted in the development of relapses in 22% and new T2 lesions in 75% of participants in a 1-year randomized pilot study [109]. The RESTORE trial, which randomly assigned patients who were stable on natalizumab for at least one year to continued natalizumab, placebo, or other therapies (interferon β-1a, glatiramer acetate, or methylprednisolone), reported 50/167 (30%) participants resuming natalizumab prior to week 28 because of disease activity [110]. The odds of developing higher numbers of gadolinium-positive lesions on MRI was 3.8 times greater (95% CI 1.71–8.56) in patients < 40 years compared to ≥ 40 years old in this trial [111]. Natalizumab Extended Interval Dosing (EID) has been implemented mainly to reduce the risk of PML, with encouraging efficacy data at an interval of 6 weeks [112,113,114,115]. EID of natalizumab does not seem to increase the rate of brain atrophy [116] or the levels of serum NfL [117] compared to standard interval dosing (SID). In the first phase of the NEXT-MS trial, which explored natalizumab dosing strategies based on trough levels, investigators found that personalized EID—in some cases out to 9 weeks—did not result in inferior clinical or radiographic outcomes compared to SID [118]. Whether such de-escalation strategies can lead to successful DMT discontinuation in older inactive MS patients is not yet known.
Most MS DMTs have only one or a limited number of approved dose strengths (lower doses available for initial titration, for example), but there have been some studies investigating off-label dosing regimens for some DMTs. Ghadiri et al. performed a systematic review of alternate day dosing of fingolimod, identifying 4 retrospective observational studies with a combined 296 on standard and 276 on alternate day dosing [119]. These studies differed in study populations, outcome measures, and methodologies. One study [120] found increased risk of relapses and MRI activity with every other day compared to standard dosing, but two others [121, 122] found similar rates of disease reactivation between the two regimens. The ASSESS trial, which separately compared daily doses of fingolimod 0.5mg or 0.25mg to glatiramer acetate (GA) 20mg, found that the higher fingolimod dose outperformed GA in annualized relapse rate, while the difference between the lower dose and GA was not statistically significant (The lower dose was statistically superior to GA on MRI measures of disease activity) [123]. GA exists in 20mg daily and 40mg three times weekly doses, though we have patients who prefer to take lower doses, for instance 40mg once or twice weekly; more evidence is needed to determine whether this kind of de-escalation strategy is valid. A monthly depot version of GA, not yet available as of this writing, may be attractive to older patients taking GA who are interested in limiting their injection burden, or even those taking other DMTs who want to de-escalate.
Using rituximab off-label for MS, neurologists initially adopted dosing practices from rheumatology and oncology, with 2 doses of 1000mg separated by 2 weeks, or 375mg weekly for 4 weeks, with repeated cycles every 6 months [124]. Our current practice is typically to administer single maintenance doses of 500mg once every 6 months, though after March 2020, many patients experienced longer gaps between rituximab (and ocrelizumab) infusions due to the COVID-19 pandemic. In a single-center French study of all MS patients who started or continued rituximab after 2019, EID with a median gap of 17 months did not produce an appreciable difference in the annualized relapse rate, with 97% of patients experiencing radiographic stability in the EID period, despite partial or complete peripheral B cell reconstitution in the vast majority [125]. A Swedish retrospective study of 225 MS patients treated with rituximab who had discontinued treatment or reduced the dose to < 1000mg/year found no differences in annualized relapse rates, new or enlarging T2 lesions or contrast-enhancing lesions between full dose, reduced dose, and treatment discontinuation over a mean (SD) follow-up period of 6.5 (2.0) years [126]. Similarly, in a Swedish prospective, non-randomized cohort of 718 rituximab-treated MS patients stratified by interval (< 8, ≥ 8 to 12, ≥ 12 to 18, and ≥ 18 months), there was no relationship between time since last infusion and clinical or radiographic disease activity, despite variable B cell repopulation kinetics [127]. The ongoing RIDOSE-MS study (NCT03979456) is a Swedish non-inferiority RCT comparing rituximab 500 mg dosed every 6 months versus yearly, estimated to finish in June 2025.
Data from the ocrelizumab phase II extension study suggest durable efficacy 12–18 months after last infusion and an apparent decline in risk of infection toward the end of the treatment-free period [128]. A multicenter German study of ocrelizumab given at SID and EID (EID defined as ≥ 4-week delay in treatment) found high rates of freedom from relapse and MRI activity and low rates of disability progression with both dosing schemes [129]. Ocrelizumab EID resulted in repopulation of a higher percentage of transitional, naïve, and regulatory B cells, but not of memory B cells or plasmablasts, compared to SID in an immunological study of B cell subsets in which EID and SID had similarly very low rates of disease activity [130]. In Italian observational studies of relapsing and progressive MS patients on ocrelizumab, there was no difference disease activity or disability progression between SID and EID [131, 132]. Given the absence of rebound and their favorable pharmacodynamic properties, EID of intravenous anti-B cell DMTs is an attractive strategy to “wean off” DMTs, especially for natalizumab and S1PR modulators. At a minimum, de-escalation in any form can provide a psychological bridge for patients who are reluctant to quit DMTs “cold turkey.”
Conclusion
The observational and prospective controlled studies described above have defined several factors that should be considered when discussing potential permanent DMT discontinuation or de-escalation, including age, disease duration, recent clinical or radiographic activity or progression, current DMT, medical comorbidities, risks and costs with continued treatment, and patient preferences. Even in the best possible scenario, clinicians and patients approaching this issue are often confronted with more questions than answers. What is the risk of disease activity when the DMT is reduced or eliminated? How much time will have to pass off therapy before we are “in the clear?” What symptom or event would support treatment re-initiation? Is any amount of disease activity, however small, acceptable? And relatedly, if small lesions appear on follow up brain MRIs of older discontinuers, how confident can we be that they are MS lesions and not microvascular changes? Given the greater benefits on relapses and MRI activity than on disability progression generally with MS DMTs, and the especially limited impact of presently available DMTs on progression in older patients, it is worth considering the inflammatory activity and PIRA axes separately when evaluating whether or not treatment discontinuation has been “successful.” The fact that someone experiences PIRA after DMT cessation does not necessarily mean that they would not have had the same progression had the DMT been continued.
Given the information available to date, we would conclude it is reasonable to begin having DMT de-escalation and discontinuation discussions with patients of any MS subtype fulfilling the following criteria: 1) Age 50 to 55 years; 2) Minimum time from last relapse or MRI change of 5 years; and 3) Disease duration of at least 15 years. Conversations may need to be continued over several visits. A stepwise de-escalation plan can be offered to those wishing to reduce DMT risk who are fearful of disease recurrence with abrupt discontinuation, though more research is needed to refine de-escalation strategies. We recommend that DMT discontinuers continue to be followed with periodic examinations and neuroimaging to evaluate for stability, for example, obtaining a brain MRI at the time of discontinuation and annually for 2 years and if stable as needed thereafter, and clinical follow up every 6 months for 2 years and if stable annually thereafter. Clinical or radiographic worsening should prompt reconsideration of the discontinuation decision, although data from DISCOMS indicate that one or two new lesions on brain MRI are not associated with significant risk of disability progression [105]. Fears of disease reactivation following DMT discontinuation should not be quickly dismissed regardless of a patient’s age or disease duration, since older patients may still have some (albeit low) risk of disease reactivation. Even a predicted 99% chance of success might be met with skepticism by someone currently content with their DMT. It is important to emphasize to the patient that discontinuation does not mean abandonment of care.
In general, there remains relatively limited research in MS patients over age 55 on the use of and de-escalation/ discontinuation from DMTs, especially involving long-term follow up. Future studies will be needed to pinpoint an individual’s optimal moment for permanent DMT discontinuation, to identify biomarkers (fluid, imaging) with stronger predictive power, to refine prognostic algorithms for de-escalation and discontinuation, and to gauge the benefits of DMT resumption in discontinuers following new MRI findings or clinical symptoms. Introduction of novel interventions such as CAR-T therapies or MS vaccines that tolerize the immune system in a more durable way may further reshape the concepts of DMT de-escalation and discontinuation. In a future that includes neuroprotective, remyelinating, and regenerative treatments in addition to standard immunotherapies, paradigms of DMT de-escalation and discontinuation will evolve: one might imagine an overlapping treatment framework prioritizing immunotherapies for the first several years, remyelinating/repair agents as needed (e.g. following a relapse) or until desired functional outcomes are achieved, and neuroprotective agents throughout the course.
Case
A 60-year-old woman with MS presented to our clinic to establish care. She was originally diagnosed with MS 36 years ago after an episode of diplopia and has had progressive decline in her gait beginning about 15 years ago, consistent with a secondary progressive phenotype. She began walking with a cane 10 years ago and more recently has become more reliant on a walker. 3.5 years ago after her partner’s death, her family became aware of how dependent she had become. Chronic symptoms included mild paraparesis, gait ataxia, urinary incontinence, and cognitive impairment. She has been receiving natalizumab infusions for the past 5 years. MRIs of the brain during this time have shown stable moderate burden of demyelinating lesions in the juxtacortical, deep, periventricular, and infratentorial white matter, with severe global volume loss and no gadolinium-enhancing lesions. 2 years ago, she was hospitalized for generalized seizures, now controlled with levetiracetam. At initial evaluation, her Expanded Disability Status Scale was 6.5. We agreed to discontinue natalizumab. At a return visit 7 months later, she reported worsened balance and falls. New noncontrast brain MRI revealed a new lesion in the left pons and middle cerebellar peduncle (see Fig. 1). Natalizumab was resumed without further relapses or MRI changes in the following 5 years, though she continued to experience slow decline, increasingly needing to use a wheelchair.
Lesson: Natalizumab discontinuation should be approached cautiously, even in older progressive patients, given the risk of disease reactivation. Extended interval dosing or switching to an anti-CD20 immunotherapy should be considered.
Key References
• Signori A, Schiavetti I, Gallo F, Sormani MP. Subgroups of multiple sclerosis patients with larger treatment benefits: a meta-analysis of randomized trials. Eur J Neurol. 2015;22(6):960–6. https://doi.org/10.1111/ene.12690.
-
Metaanalysis of MS clinical trials demonstrating reduced DMT benefit in older age based on subgroup analyses.
• Weideman AM, Tapia-Maltos MA, Johnson K, Greenwood M, Bielekova B. Meta-analysis of the Age-Dependent Efficacy of Multiple Sclerosis Treatments. Front Neurol. 2017;8:577. https://doi.org/10.3389/fneur.2017.00577.
-
Large meta-analysis of MS clinical trials that substantiates the notion that age is an essential modifier of DMT efficacy.
•Lewis S (Ed.) Monitoring, Switching, and Stopping MS Disease-Modifying Therapies. Robert Gross and John Corboy. Continuum: Lifelong Learning in Neurology. American Academy of Neurology: June 2019; 25(3):715–735.
-
Reviews different treatment paradigms in MS including escalation, induction, and early use of high-efficacy DMTs
• Graves JS, Krysko KM, Hua LH, Absinta M, Franklin RJ, Segal BM. Ageing and multiple sclerosis. Lancet Neurol. 2023;22:66–77. https://doi.org/10.1016/S1474-4422(22)00184-3.
-
Comprehensive overview of changes associated with aging in MS
References
Beiki O, Frumento P, Bottai M, Manoucherhinia A, Hillert J. Changes in the risk of reaching multiple sclerosis disability milestones in recent decades: A nationwide population-based cohort study in Sweden. JAMA Neurol. 2019;76:665–71. https://doi.org/10.1001/jamaneurol.2019.0330.
Abdelrahman A, Alvarez E. Advances in Multiple Sclerosis Neurotherapeutics, Neuroprotection, and Risk Mitigation Strategies. Neurol Clin. 2024;42(1):115–35. https://doi.org/10.1016/j.ncl.2023.08.002.
Hartung DM. Health economics of disease-modifying therapy for multiple sclerosis in the United States. Ther Adv Neurol Disord. 2021;14:1756286420987031.
Vollmer BL, Wallach AI, Corboy JR, Dubovskaya K, Alvarez E, Kister I. Serious safety events in rituximab-treated multiple sclerosis and related disorders. Ann Clin Transl Neurol. 2020;7(9):1477–87.
Tur C, Dubessy AL, Otero-Romero S, Amato MP, Derfuss T, Di Pauli F, et al. The risk of infections for multiple sclerosis and neuromyelitis optica spectrum disorder disease-modifying treatments: Eighth European Committee for Treatment and Research in Multiple Sclerosis Focused Workshop Review. April 2021. Mult Scler 2022;28(9):1424–1456. https://doi.org/10.1177/13524585211069068
Louapre C, Collongues N, Stankoff B, Giannesini C, Papeix C, Bensa C, et al. Clinical characteristics and outcomes in patients with coronavirus disease 2019 and multiple sclerosis. JAMA Neurol. 2020;77:1079–88. https://doi.org/10.1001/jamaneurol.2020.2581.
Chaudhry F, Bulka H, Rathnam AS, Said OM, Lin J, Lorigan H, et al. COVID-19 in multiple sclerosis patients and risk factors for severe infection. J Neurol Sci. 2020;418:117147.
Salter AGA. COViMS registry and UKMSR. Presented at 8th Joint European Committee for Treatment and Research in Multiple Sclerosis-Americas Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS-ACTRIMS) 2020; Washington DC, United States
Langer-Gould A, Smith JB, Li BH; KPSC MS Specialist Group. Multiple sclerosis, rituximab, and COVID-19. Ann Clin Transl Neurol 2021;8(4):938–943. https://doi.org/10.1002/acn3.51342
Signori A, Schiavetti I, Gallo F, Sormani MP. Subgroups of multiple sclerosis patients with larger treatment benefits: a meta-analysis of randomized trials. Eur J Neurol. 2015;22(6):960–6. https://doi.org/10.1111/ene.12690.
Jakimovski D, Eckert SP, Zivadinov R, Weinstock-Guttman B. Considering patient age when treating multiple sclerosis across the adult lifespan. Expert Rev Neurother. 2021;21(3):353–64. https://doi.org/10.1080/14737175.2021.1886082.
Macaron G, Larochelle C, Arbour N, Galmard M, Girard JM, Prat A, et al. Impact of aging on treatment considerations for multiple sclerosis patients. Front Neurol. 2023;14:1197212. https://doi.org/10.3389/fneur.2023.1197212.
Weideman AM, Tapia-Maltos MA, Johnson K, Greenwood M, Bielekova B. Meta-analysis of the Age-Dependent Efficacy of Multiple Sclerosis Treatments. Front Neurol. 2017;8:577. https://doi.org/10.3389/fneur.2017.00577.
Jalaleddini K, Bermel RA, Talente B, Weinstein D, Qureshi F, Rasmussen M, et al. A US payer perspective health economic model assessing value of monitoring disease activity to inform discontinuation and re-initiation of DMT in multiple sclerosis. Mult Scler. 2024;30(3):432–42. https://doi.org/10.1177/13524585241227372.
Zhang Y, Salter A, Jin S, Culpepper WJ 2nd, Cutter GR, Wallin M, et al. Disease-modifying therapy prescription patterns in people with multiple sclerosis by age. Ther Adv Neurol Disord. 2021;14:17562864211006500. https://doi.org/10.1177/17562864211006499.
Cisternas M, Bartolome L, Gitar B, Hulbert E, Trenz H, Patel V, et al. Health care resource utilization and disease modifying treatment use in multiple sclerosis patients by age and insurance type. Curr Med Res Opin. 2021;37(4):597–604. https://doi.org/10.1080/03007995.2021.1885367.
Goereci Y, Ellenberger D, Rommer P, Dunkl V, Golla H, Zettl U, et al. Persons with multiple sclerosis older than 55 years: an analysis from the German MS registry. J Neurol. 2024;271(6):3409–16. https://doi.org/10.1007/s00415-024-12286-4.
McGinley MP, Cola PA, Fox RJ, Cohen JA, Corboy JJ, Miller D. Perspectives of individuals with multiple sclerosis on discontinuation of disease-modifying therapies. Mult Scler. 2020;26(12):1581–9. https://doi.org/10.1177/1352458519867314.
Lublin FD, Häring DA, Ganjgahi H, Ocampo A, Hatami F, Čuklina J, et al. How patients with multiple sclerosis acquire disability. Brain. 2022;145(9):3147–61. https://doi.org/10.1093/brain/awac016.
Kappos L, Wolinsky JS, Giovannoni G, Arnold DL, Wang Q, Bernasconi C, et al. Contribution of Relapse-Independent Progression vs Relapse-Associated Worsening to Overall Confirmed Disability Accumulation in Typical Relapsing Multiple Sclerosis in a Pooled Analysis of 2 Randomized Clinical Trials. JAMA Neurol. 2020;77(9):1132–40. https://doi.org/10.1001/jamaneurol.2020.1568.
Brown JWL, Coles A, Horakova D, Havrdova E, Izquierdo G, Prat A, et al; MSBase Study Group. Association of Initial Disease-Modifying Therapy With Later Conversion to Secondary Progressive Multiple Sclerosis. JAMA 2019;321(2):175–187. https://doi.org/10.1001/jama.2018.20588
Harding K, Williams O, Willis M, Hrastelj J, Rimmer A, Joseph F, et al. Clinical Outcomes of Escalation vs Early Intensive Disease-Modifying Therapy in Patients With Multiple Sclerosis. JAMA Neurol. 2019;76(5):536–41. https://doi.org/10.1001/jamaneurol.2018.4905.
Buron MD, Chalmer TA, Sellebjerg F, Barzinji I, Danny B, Christensen JR, et al. Initial high-efficacy disease-modifying therapy in multiple sclerosis: A nationwide cohort study. Neurol. 2020;95(8):e1041–51. https://doi.org/10.1212/WNL.0000000000010135.
He A, Merkel B, Brown JWL, Zhovits Ryerson L, Kister I, Malpas CB, et al; MSBase study group. Timing of high-efficacy therapy for multiple sclerosis: a retrospective observational cohort study. Lancet Neurol 2020;19(4):307–316. https://doi.org/10.1016/S1474-4422(20)30067-3
Spelman T, Magyari M, Piehl F, Svenningsson A, Rasmussen PV, Kant M, et al. Treatment Escalation vs Immediate Initiation of Highly Effective Treatment for Patients With Relapsing-Remitting Multiple Sclerosis: Data From 2 Different National Strategies. JAMA Neurol. 2021;78(10):1197–204. https://doi.org/10.1001/jamaneurol.2021.2738.
Lewis S (Ed.) Monitoring, Switching, and Stopping MS Disease-Modifying Therapies. Robert Gross and John Corboy. Continuum: Lifelong Learning in Neurology. American Academy of Neurology: June 2019; 25(3):715–735.
Filippi M, Amato MP, Centonze D, Gallo P, Gasperini C, Inglese M, et al. Early use of high-efficacy disease-modifying therapies makes the difference in people with multiple sclerosis: an expert opinion. J Neurol. 2022;269(10):5382–94. https://doi.org/10.1007/s00415-022-11193-w.
Cortese I, Reich DS, Nath A. Progressive multifocal leukoencephalopathy and the spectrum of JC virus-related disease. Nat Rev Neurol. 2021;17(1):37–51. https://doi.org/10.1038/s41582-020-00427-y.
Coles AJ, Cohen JA, Fox EJ, Giovannoni G, Hartung HP, Havrdova E, et al; CARE-MS II and CAMMS03409 Investigators. Alemtuzumab CARE-MS II 5-year follow-up: Efficacy and safety findings. Neurol 2017;89(11):1117–1126. https://doi.org/10.1212/WNL.0000000000004354
Allen-Philbey K, De Trane S, MacDougall A, Adams A, Bianchi L, Campion T, et al. Disease activity 4.5 years after starting cladribine: experience in 264 patients with multiple sclerosis. Ther Adv Neurol Disord 2023;16:17562864231200627. https://doi.org/10.1177/17562864231200627
Giovannoni G, Boyko A, Correale J, Edan G, Freedman MS, Montalban X, et al. Long-term follow-up of patients with relapsing multiple sclerosis from the CLARITY/CLARITY Extension cohort of CLASSIC-MS: An ambispective study. Mult Scler. 2023;29(6):719–30. https://doi.org/10.1177/13524585231161494.
Rush CA, Atkins HL, Freedman MS. Autologous Hematopoietic Stem Cell Transplantation in the Treatment of Multiple Sclerosis. Cold Spring Harb Perspect Med. 2019;9(3):a029082. https://doi.org/10.1101/cshperspect.a029082.
Graves JS, Krysko KM, Hua LH, Absinta M, Franklin RJ, Segal BM. Ageing and multiple sclerosis. Lancet Neurol. 2023;22:66–77. https://doi.org/10.1016/S1474-4422(22)00184-3.
Crooke SN, Ovsyannikova IG, Poland GA, Kennedy RB. Immunosenescence: A systems-level overview of immune cell biology and strategies for improving vaccine responses. Exp Gerontol. 2019;124:110632. https://doi.org/10.1016/j.exger.2019.110632.
Dema M, Eixarch H, Villar LM, Montalban X, Espejo C. Immunosenescence in multiple sclerosis: the identification of new therapeutic targets. Autoimmun Rev 2021;20(9):102893, ISSN 1568–9972. https://doi.org/10.1016/j.autrev.2021.102893
Thakolwiboon S, Mills EA, Yang J, Doty J, Belkin MI, Cho T, et al. Immunosenescence and multiple sclerosis: inflammaging for prognosis and therapeutic consideration. Front Aging. 2023;4:1234572. https://doi.org/10.3389/fragi.2023.1234572.
Ostolaza Ibáñez A, Corroza Laviñeta J, Ayuso BT. Immunosenescence: the role of age in multiple sclerosis. Neurologia (Engl Ed). 2023May;38(4):284–90. https://doi.org/10.1016/j.nrleng.2020.05.023.
Faustino P, Coutinho M, Leitão L, Capela C, Brum M, Parra J, et al. Seroconversion rate following HBV vaccination in clinical practice: The role of age and DMT treatment. Mult Scler Relat Disord. 2021;50:102859. https://doi.org/10.1016/j.msard.2021.102859.
Salminen A, Ojala J, Kaarniranta K, Haapasalo A, Hiltunen M, Soininen H. Astrocytes in the aging brain express characteristics of senescence-associated secretory phenotype. Eur J Neurosci. 2011;34(1):3–11. https://doi.org/10.1111/j.1460-9568.2011.07738.x.
Angelova DM, Brown DR. Microglia and the aging brain: are senescent microglia the key to neurodegeneration? J Neurochem. 2019;151(6):676–88. https://doi.org/10.1111/jnc.14860.
Franklin RJ, Goldman SA. Glia Disease and Repair-Remyelination. Cold Spring Harb Perspect Biol. 2015;7(7):a020594. https://doi.org/10.1101/cshperspect.a020594.
Sim FJ, Zhao C, Penderis J, Franklin RJ. The age-related decrease in CNS remyelination efficiency is attributable to an impairment of both oligodendrocyte progenitor recruitment and differentiation. J Neurosci. 2002;22(7):2451–9. https://doi.org/10.1523/JNEUROSCI.22-07-02451.2002.
Neumann B, Segel M, Chalut KJ, Franklin RJ. Remyelination and ageing: Reversing the ravages of time. Mult Scler. 2019;25(14):1835–41. https://doi.org/10.1177/1352458519884006.
Conway BL, Zeydan B, Uygunoğlu U, Novotna M, Siva A, Pittock SJ, et al. Age is a critical determinant in recovery from multiple sclerosis relapses. Mult Scler. 2019;25(13):1754–63. https://doi.org/10.1177/1352458518800815.
Confavreux C, Vukusic S. Natural history of multiple sclerosis: a unifying concept. Brain. 2006;129:606–16.
Tremlett H, Zhao Y, Joseph J, Devonshire V; UBCMS Clinic Neurologists. Relapses in multiple sclerosis are age- and time-dependent. J Neurol Neurosurg Psychiatry. 2008; 79(12): 1368–1374
Gorman MP, Healy BC, Polgar-Turcsanyi M, Chitnis T. Increased relapse rate in pediatric-onset compared with adult-onset multiple sclerosis. Arch Neurol. 2009;66:54–9.
McKay KA, Hillert J, Manouchehrinia A. Long-term disability progression of pediatric-onset multiple sclerosis. Neurology. 2019Jun 11;92(24):e2764–73. https://doi.org/10.1212/WNL.0000000000007647.
Andersen MA, Buron MD, Magyari M. Late-onset MS is associated with an increased rate of reaching disability milestones. J Neurol. 2021;268(9):3352–60. https://doi.org/10.1007/s00415-021-10490-0.
Lassmann H, van Horssen J, Mahad D. Progressive multiple sclerosis: pathology and pathogenesis. Nat Rev Neurol. 2012;8(11):647–56. https://doi.org/10.1038/nrneurol.2012.168.
Vollmer TL, Nair KV, Williams IM, Alvarez E. Multiple Sclerosis Phenotypes as a Continuum: The Role of Neurologic Reserve. Neurol Clin Pract. 2021;11(4):342–51. https://doi.org/10.1212/CPJ.0000000000001045.
De Stefano N, Stromillo ML, Giorgio A, Bartolozzi ML, Battaglini M, Baldini M, Portaccio E, Amato MP, Sormani MP. Establishing pathological cut-offs of brain atrophy rates in multiple sclerosis. J Neurol Neurosurg Psychiatry. 2016;87(1):93–9. https://doi.org/10.1136/jnnp-2014-309903.
Azevedo CJ, Cen SY, Jaberzadeh A, Zheng L, Hauser SL, Pelletier D. Contribution of normal aging to brain atrophy in MS. Neurol Neuroimmunol Neuroinflamm. 2019;6(6):e616. https://doi.org/10.1212/NXI.0000000000000616.
Mahad DH, Trapp BD, Lassmann H. Pathological mechanisms in progressive multiple sclerosis. Lancet Neurol. 2015;14:183–93.
Frischer JM, Weigand SD, Guo Y, Kale N, Parisi JE, Pirko I, Mandrekar J, Bramow S, Metz I, Brück W, Lassmann H, Lucchinetti CF. Clinical and pathological insights into the dynamic nature of the white matter multiple sclerosis plaque. Ann Neurol. 2015;78(5):710–21. https://doi.org/10.1002/ana.24497.
Lassmann H. The contribution of neuropathology to multiple sclerosis research. Eur J Neurol. 2022;29(9):2869–77. https://doi.org/10.1111/ene.15360.
Tortorella C, Bellacosa A, Paolicelli D, Fuiani A, Di Monte E, Simone IL, et al. Age-related gadolinium-enhancement of MRI brain lesions in multiple sclerosis. J Neurol Sci. 2005;239(1):95–9. https://doi.org/10.1016/j.jns.2005.08.006.
Wijnands JM, Kingwell E, Zhu F, Zhao Y, Fisk JD, Evans C, et al. Infection-related health care utilization among people with and without multiple sclerosis. Mult Scler. 2017;23(11):1506–16. https://doi.org/10.1177/1352458516681198.
Brand JS, Smith KA, Piehl F, Olsson T, Montgomery S. Risk of serious infections in multiple sclerosis patients by disease course and disability status: Results from a Swedish register-based study. Brain Behav Immun Health. 2022;22:100470. https://doi.org/10.1016/j.bbih.2022.100470.
Egli A, Infanti L, Dumoulin A, Buser A, Samaridis J, Stebler C, et al. Prevalence of Polyomavirus BK and JC Infection and Replication in 400 Healthy Blood Donors. J Infect Dis. 2009;199(6):837–46. https://doi.org/10.1086/597126.
Dong-Si T, Gheuens S, Gangadharan A Wenten M, Philip J, McIninch J, et al. Predictors of survival and functional outcomes in natalizumab-associated progressive multifocal leukoencephalopathy. J Neurovirol 2015;21: 637–644. https://doi.org/10.1007/s13365-015-0316-4
Joly M, Conte C, Cazanave C, Le Moing V, Tattevin P, Delobel P, et al. Progressive multifocal leukoencephalopathy: epidemiology and spectrum of predisposing conditions. Brain. 2023;146(1):349–58. https://doi.org/10.1093/brain/awac237.
Prosperini L, Scarpazza C, Imberti L, Cordioli C, De Rossi N, Capra R. Age as a risk factor for early onset of natalizumab-related progressive multifocal leukoencephalopathy. J Neurovirol. 2017;23(5):742–9. https://doi.org/10.1007/s13365-017-0561-9.
Sriwastava S, Kataria S, Srivastava S, Kazemlou S, Gao S, Wen S, et al. Disease-modifying therapies and progressive multifocal leukoencephalopathy in multiple sclerosis: A systematic review and meta-analysis. J Neuroimmunol. 2021;360:577721. https://doi.org/10.1016/j.jneuroim.2021.577721.
Hauser SL, Kappos L, Montalban X, Craveiro L, Chognot C, Hughes R, et al. Safety of Ocrelizumab in Patients With Relapsing and Primary Progressive Multiple Sclerosis. Neurol. 2021;97(16):e1546–59. https://doi.org/10.1212/WNL.0000000000012700.
Luna G, Alping P, Burman J, Fink K, Fogdell-Hahn A, Gunnarsson M, et al. Infection Risks Among Patients With Multiple Sclerosis Treated With Fingolimod, Natalizumab, Rituximab, and Injectable Therapies. JAMA Neurol. 2020;77(2):184–91. https://doi.org/10.1001/jamaneurol.2019.3365.
Langer-Gould AM, Smith JB, Gonzales EG, Piehl F, Li BH. Multiple Sclerosis, Disease-Modifying Therapies, and Infections. Neurol Neuroimmunol Neuroinflamm. 2023;10(6):e200164. https://doi.org/10.1212/NXI.0000000000200164.
Perriguey M, Maarouf A, Stellmann JP, Rico A, Boutiere C, Demortiere S, et al. Hypogammaglobulinemia and infections in patients with multiple sclerosis treated with rituximab. Neurol Neuroimmunol Neuroinflamm. 2021;9(1):e1115.
Loebermann M, Winkelmann A, Hartung HP, Hengel H, Reisinger EC, Zettl UK. Vaccination against infection in patients with multiple sclerosis. Nat Rev Neurol. 2012;8(3):143–51. https://doi.org/10.1038/nrneurol.2012.8.
Tremblay MA, Vukusic S, Shanmugasundaram M, Bozin I, Levin S, Gocke A, Wipfler P. Vaccine response in people with multiple sclerosis treated with fumarates. Mult Scler J Exp Transl Clin. 2023;9(3):20552173231191170. https://doi.org/10.1177/20552173231191170.
Tornatore C, Wiendl H, Lublin AL, Geertsen SS, Chavin J, Truffinet P, et al. Vaccine Response in Patients With Multiple Sclerosis Receiving Teriflunomide. Front Neurol. 2022;13:828616. https://doi.org/10.3389/fneur.2022.828616.
Achiron A, Mandel M, Dreyer-Alster S, Magalashvili D, Menascu S, Warszawer Y, et al. In-depth characterization of long-term humoral and cellular immune responses to COVID-19m-RNA vaccination in multiple sclerosis patients treated with teriflunomide or alemtuzumab. Mult Scler Relat Disord. 2023;72:104616. https://doi.org/10.1016/j.msard.2023.104616.
Bar-Or A, Calkwood JC, Chognot C, Evershed J, Herman A, et al. Effect of ocrelizumab on vaccine responses in patients with multiple sclerosis: the VELOCE study. Neurol. 2020;95(14):e1999–2008. https://doi.org/10.1212/WNL.0000000000010380.
Ciotti JR, Valtcheva MV, Cross AH. Effects of MS disease-modifying therapies on responses to vaccinations: A review. Mult Scler Relat Disord. 2020;45:102439. https://doi.org/10.1016/j.msard.2020.102439.
Sormani MP, Inglese M, Schiavetti I, Carmisciano L, Laroni A, Lapucci C, et al; CovaXiMS study group on behalf of the Italian Covid-19 Alliance in MS. Effect of SARS-CoV-2 mRNA vaccination in MS patients treated with disease modifying therapies. EBioMedicine 2021;72:103581. https://doi.org/10.1016/j.ebiom.2021.103581
Prosperini L, Haggiag S, Tortorella C, Galgani S, Gasperini C. Age-related adverse events of disease-modifying treatments for multiple sclerosis: A meta-regression. Mult Scler. 2021;27(9):1391–402. https://doi.org/10.1177/1352458520964778.
Rae-Grant A, Day GS, Marrie RA, Rabinstein A, Cree BAC, Gronseth GS, et al. Practice guideline recommendations summary: Disease-modifying therapies for adults with multiple sclerosis: Report of the Guideline Development, Dissemination, and Implementation Subcommittee of the American Academy of Neurology. Neurol. 2018;90(17):777–88. https://doi.org/10.1212/WNL.0000000000005347.
Krysko KM, Bove R, Dobson R, Jokubaitis V, Hellwig K. Treatment of Women with Multiple Sclerosis Planning Pregnancy. Curr Treat Options Neurol. 2021;23(4):11. https://doi.org/10.1007/s11940-021-00666-4.
Tobin MO, Weinshenker BG. Stopping immunomodulatory medications in MS: frequency, reasons and consequences. Mult Scler Relat Disord. 2015;4:437–43.
Zettl UK, Schreiber H, Bauer-Steinhusen U, et al. Baseline predictors of persistence to first disease-modifying treatment in multiple sclerosis. Acta Neurol Scand. 2017;136:116–21. https://doi.org/10.1111/ane.12705.
Parks NE, Andreou P, Marrie RA, Fisk JD, Bhan V, Kirkland SA. Comorbidity and persistence of disease-modifying therapy use in relapsing remitting multiple sclerosis. Mult Scler Relat Disord. 2021;56:103249. https://doi.org/10.1016/j.msard.2021.103249.
Moccia M, Palladino R, Carotenuto A, et al. Predictors of long-term interferon discontinuation in newly diagnosed relapsing multiple sclerosis. Mult Scler Relat Disord. 2016;10:90–6. https://doi.org/10.1016/j.msard.2016.09.011.
Grytten N, Aarseth JH, Espeset K, Johnsen GB, Wehus R, Lund C, Haugstad RC. Stoppers and non-starters of disease-modifying treatment in multiple sclerosis. Acta Neurol Scand. 2013;127:133–40. https://doi.org/10.1111/j.1600-0404.2012.01708.x.
Hartung HP, Meuth SG, Miller DM, Comi G. Stopping disease-modifying therapy in relapsing and progressive multiple sclerosis. Curr Opin Neurol. 2021;34:598–603. https://doi.org/10.1097/WCO.0000000000000960.
Salavisa M, Serrazina F, Ladeira AF, Correia AS. Discontinuation of disease-modifying therapy in MS patients over 60 years old and its impact on relapse rates and disease progression. Clin Neurol Neurosurg. 2023;225:107612.
Yano H, Gonzalez C, Healy BC, Glanz BI, Weiner HL, Chitnis T. Discontinuation of disease-modifying therapy for patients with relapsing-remitting multiple sclerosis: Effect on clinical and MRI outcomes. Mult Scler Relat Disord. 2019;35:119–27. https://doi.org/10.1016/j.msard.2019.07.021.
Kaminsky AL, Omorou AY, Soudant M, Pittion-Vouyovitch S, Michaud M, Anxionnat R, et al. Discontinuation of disease-modifying treatments for multiple sclerosis in patients aged over 50 with disease inactivity. J Neurol. 2020;267:3518–27.
Bonenfant J, Bajeux E, Deburghgraeve V, Le Page E, Edan G, Kerbrat A. Can we stop immunomodulatory treatments in secondary progressive multiple sclerosis? Eur J Neurol. 2017;24(2):237–44. https://doi.org/10.1111/ene.13181.
Kister I, Spelman T, Alroughani R, et al. Discontinuing disease-modifying therapy in MS after a prolonged relapse-free period: a propensity score-matched study [published correction appears in J Neurol Neurosurg Psychiatry. 2019; 90: e2]. J Neurol Neurosurg Psychiatry. 2016; 87: 1133-1137https://doi.org/10.1136/jnnp-2016-313760
Kister I, Spelman T, Patti F, Duquette P, Trojano M, Izquierdo G, et al. Predictors of relapse and disability progression in MS patients who discontinue disease-modifying therapy. J Neurol Sci. 2018;391:72–6.
Coerver EME, Bourass A, Wessels MHJ, van Kempen ZLE, Jasperse MMS, Tonino BAR, et al. Discontinuation of first-line disease-modifying therapy in relapse onset multiple sclerosis. Mult Scler Relat Disord. 2023;74:104706. https://doi.org/10.1016/j.msard.2023.104706.
Hua LH, Harris H, Conway D, Thompson NR. Changes in patient-reported outcomes between continuers and discontinuers of disease modifying therapy in patients with multiple sclerosis over age 60. Mult Scler Rel Dis 2019;30:252–256.
Chappuis M, Rousseau C, Bajeux E, Wiertlewski S, Laplaud D, Le Page E, et al. Discontinuation of second- versus first-line disease-modifying treatment in middle-aged patients with multiple sclerosis. J Neurol. 2023;270(1):413–22. https://doi.org/10.1007/s00415-022-11341-2.
Jouvenot G, Courbon G, Lefort M, Rollot F, Casey R, Le Page E, et al. High-Efficacy Therapy Discontinuation in Patients 50 Years and Older With Nonactive MS. JAMA Neurol; Published online March 25, 2024. https://doi.org/10.1001/jamaneurol.2024.0395
Prosperini L, Haggiag S, Ruggieri S, Tortorella C, Gasperini C. Stopping disease-modifying treatments in multiple sclerosis: A systematic review and meta-analysis of real-world studies. CNS Drugs. 2023;37:915–27. https://doi.org/10.1007/s40263-023-01038-z.
Mouresan EF, Mentesidou E, Berglund A, McKay KA, Hillert J, Iacobaeus E. Clinical Characteristics and Long-Term Outcomes of Late-Onset Multiple Sclerosis: A Swedish Nationwide Study. Neurol. 2024;102(6):e208051. https://doi.org/10.1212/WNL.0000000000208051.
Bsteh G, Feige J, Ehling R, Auer M, Hegen H, Di Pauli F, et al. Discontinuation of disease-modifying therapies in multiple sclerosis – Clinical outcome and prognostic factors. Mult Scler. 2017;23:1241–8. https://doi.org/10.1177/1352458516675751.
Bsteh G, Hegen H, Riedl K, Altmann P, Auer M, Berek K, et al. Quantifying the risk of disease reactivation after interferon and glatiramer acetate discontinuation in multiple sclerosis: The VIAADISC score. Eur J Neurol. 2021;28:1609–16. https://doi.org/10.1111/ene.14705.
Bose G, Healy BC, Saxena S, Saleh F, Glanz BI, Bakshi R, et al. Increasing Neurofilament and Glial Fibrillary Acidic Protein After Treatment Discontinuation Predicts Multiple Sclerosis Disease Activity. Neurol Neuroimmunol Neuroinflamm. 2023;10(6):e200167. https://doi.org/10.1212/NXI.0000000000200167.
Corboy JR, Fox RJ, Kister I, Cutter GR, Morgan CJ, Seale R, et al; DISCOMS investigators. Risk of new disease activity in patients with multiple sclerosis who continue or discontinue disease-modifying therapies (DISCOMS): a multicentre, randomised, single-blind, phase 4, non-inferiority trial. Lancet Neurol 2023;22(7):568–577. https://doi.org/10.1016/S1474-4422(23)00154-0.
Coerver EME, Fung WH, Beukelaar JD, et al. Patient-reported outcomes in discontinuation of first-line disease-modifying therapy in stable multiple sclerosis (DOT-MS): results of a multicenter randomized controlled trial. Presented at: MSMilan; October 11–13, 2023; Milan, Italy. POSTER 791
Vollmer BL, Wolf AB, Sillau S, Corboy JR, Alvarez E. Evolution of Disease Modifying Therapy Benefits and Risks: An Argument for De-escalation as a Treatment Paradigm for Patients With Multiple Sclerosis. Front Neurol. 2022;12:799138. https://doi.org/10.3389/fneur.2021.799138.
O’Connor PW, Goodman A, Kappos L, Lublin FD, Miller DH, Polman C, et al. Disease activity return during natalizumab treatment interruption in patients with multiple sclerosis. Neurol. 2011;76(22):1858–65. https://doi.org/10.1212/WNL.0b013e31821e7c8a.
Hatcher SE, Waubant E, Nourbakhsh B, Crabtree-Hartman E, Graves JS. Rebound Syndrome in Patients With Multiple Sclerosis After Cessation of Fingolimod Treatment. JAMA Neurol. 2016;73(7):790–4. https://doi.org/10.1001/jamaneurol.2016.0826.
Fagius J, Feresiadou A, Larsson EM, Burman J. Discontinuation of disease modifying treatments in middle aged multiple sclerosis patients. First line drugs vs natalizumab. Mult Scler Relat Disord 2017; 12: 82–87. https://doi.org/10.1016/j.msard.2017.01.009
Malpas CB, Roos I, Sharmin S, Buzzard K, Skibina O, Butzkueven H, et al; MSBase Study Group. Multiple Sclerosis Relapses Following Cessation of Fingolimod. Clin Drug Investig 2022;42(4):355–364. https://doi.org/10.1007/s40261-022-01129-7
Prosperini L, Kinkel RP, Miravalle AA, Iaffaldano P, Fantaccini S. Post-natalizumab disease reactivation in multiple sclerosis: systematic review and meta-analysis. Ther Adv Neurol Disord. 2019;12:1756286419837809. https://doi.org/10.1177/1756286419837809.
Cohan SL, Edwards K, Lucas L, Gervasi-Follmar T, O’Connor J, Siuta J, et al. Reducing return of disease activity in patients with relapsing multiple sclerosis transitioned from natalizumab to teriflunomide: 12-month interim results of teriflunomide therapy. Mult Scler J Exp Transl Clin 2019;5(1). https://doi.org/10.1177/2055217318824618
Gobbi C, Meier DS, Cotton F, Sintzel M, Leppert D, Guttmann CR, et al. Interferon beta 1b following natalizumab discontinuation: one year, randomized, prospective, pilot trial. BMC Neurol. 2013;13:101. https://doi.org/10.1186/1471-2377-13-101.
Fox RJ, Cree BA, De Sèze J, Gold R, Hartung HP, Jeffery D, et al. MS disease activity in RESTORE: a randomized 24-week natalizumab treatment interruption study. Neurol. 2014;82:1491–8.
Kaufman M, Cree BA, De Sèze J, Fox RJ, Gold R, Hartung HP, et al. Radiologic MS disease activity during natalizumab treatment interruption: findings from RESTORE. J Neurol. 2015;262(2):326–36. https://doi.org/10.1007/s00415-014-7558-6.
Leurs CE, van Kempen ZL, Dekker I, Balk LJ, Wattjes MP, Rispens T, et al. Switching natalizumab to fingolimod within 6 weeks reduces recurrence of disease activity in MS patients. Mult Scler. 2018;24(11):1453–60. https://doi.org/10.1177/1352458517726381.
Vollmer B, Honce JM, Sillau S, Corboy JR, Vollmer T, Nair K, et al. The impact of very short transition times on switching from Natalizumab to Fingolimod on imaging and clinical effectiveness outcomes in multiple sclerosis. J Neurol Sci. 2018;390:89–93. https://doi.org/10.1016/j.jns.2018.04.021.
Foley JF, Defer G, Ryerson LZ, Cohen JA, Arnold DL, Butzkueven H, et al.; NOVA study investigators. Comparison of switching to 6-week dosing of natalizumab versus continuing with 4-week dosing in patients with relapsing-remitting multiple sclerosis (NOVA): a randomised, controlled, open-label, phase 3b trial. Lancet Neurol 2022;21(7):608–619. https://doi.org/10.1016/S1474-4422(22)00143-0.
Ryerson LZ, Foley JF, Defer G, Cohen JA, Arnold DL, Butzkueven H, et al. Exploratory clinical efficacy and patient-reported outcomes from NOVA: A randomized controlled study of intravenous natalizumab 6-week dosing versus continued 4-week dosing for relapsing-remitting multiple sclerosis. Mult Scler Relat Disord. 2023;72:104561. https://doi.org/10.1016/j.msard.2023.104561.
Toorop AA, Noteboom S, Steenwijk MD, Gravendeel JW, Jasperse B, Barkhof F, et al. Exploring the effects of extended interval dosing of natalizumab and drug concentrations on brain atrophy in multiple sclerosis. Mult Scler. 2024;30(2):266–71. https://doi.org/10.1177/13524585231225855.
Foley J, Xiong K, Hoyt T, Singh CM, Riddle E, de Moor C, et al. Serum neurofilament light levels in natalizumab-treated patients with multiple sclerosis who switch to extended interval dosing from every-4-week dosing in real-world clinical practice. Mult Scler. 2023;29(2):196–205. https://doi.org/10.1177/13524585221130949.
Toorop AA, van Lierop ZY, Gelissen LM, Hoitsma E, Zeinstra EM, van Rooij LC, et al. Prospective trial of natalizumab personalised extended interval dosing by therapeutic drug monitoring in relapsing-remitting multiple sclerosis (NEXT-MS). J Neurol Neurosurg Psychiatry 2023:jnnp-2023–332119. https://doi.org/10.1136/jnnp-2023-332119
Ghadiri F, Mirmosayyeb O, Sahraian MA, Moghadasi AN, Ghajarzadeh M. Alternate dosing of fingolimod in relapsing-remitting multiple sclerosis: A systematic review. Curr J Neurol. 2023;22(2):110–4. https://doi.org/10.18502/cjn.v22i2.13339.
Zecca C, Merlini A, Disanto G, Rodegher M, Panicari L, Romeo MAL, et al. Half-dose fingolimod for treating relapsing-remitting multiple sclerosis: Observational study. Mult Scler. 2018;24(2):167–74. https://doi.org/10.1177/1352458517694089.
Ramos-Lopes J, Batista S, Barradas P, Campelo I, Correia I, Nunes C, et al. Clinical effectiveness of reduced fingolimod dose in relapsing remitting multiple sclerosis-a Portuguese cohort. Neurol Sci. 2021;42(3):1039–43. https://doi.org/10.1007/s10072-020-04629-6.
Longbrake EE, Kantor D, Pawate S, Bradshaw MJ, von Geldern G, Chahin S, et al. Effectiveness of alternative dose fingolimod for multiple sclerosis. Neurol Clin Pract. 2018;8(2):102–7. https://doi.org/10.1212/CPJ.0000000000000434.
Cree BAC, Goldman MD, Corboy JR, Singer BA, Fox EJ, Arnold DL, et al; ASSESS Trial Investigators. Efficacy and Safety of 2 Fingolimod Doses vs Glatiramer Acetate for the Treatment of Patients With Relapsing-Remitting Multiple Sclerosis: A Randomized Clinical Trial. JAMA Neurol 2020;78(1):1–13. https://doi.org/10.1001/jamaneurol.2020.2950
Chisari CG, Sgarlata E, Arena S, Toscano S, Luca M, Patti F. Rituximab for the treatment of multiple sclerosis: a review. J Neurol. 2022;269:159–83. https://doi.org/10.1007/s00415-020-10362-z.
Claverie R, Perriguey M, Rico A, Boutiere C, Demortiere S, Durozard P, et al. Efficacy of Rituximab Outlasts B-Cell Repopulation in Multiple Sclerosis: Time to Rethink Dosing? Neurol Neuroimmunol Neuroinflamm. 2023;10(5):e200152. https://doi.org/10.1212/NXI.0000000000200152.
Boremalm M, Sundström P, Salzer J. Discontinuation and dose reduction of rituximab in relapsing-remitting multiple sclerosis. J Neurol. 2021;268(6):2161–8. https://doi.org/10.1007/s00415-021-10399-8.
Starvaggi Cucuzza C, Longinetti E, Ruffin N, Evertsson B, Kockum I, Jagodic M, et al. Sustained Low Relapse Rate With Highly Variable B-Cell Repopulation Dynamics With Extended Rituximab Dosing Intervals in Multiple Sclerosis. Neurol Neuroimmunol Neuroinflamm. 2022;10(1):e200056. https://doi.org/10.1212/NXI.0000000000200056.
Baker D, Pryce G, James LK, Marta M, Schmierer K. The ocrelizumab phase II extension trial suggests the potential to improve the risk: Benefit balance in multiple sclerosis. Mult Scler Relat Disord. 2020;44:102279. https://doi.org/10.1016/j.msard.2020.102279.
Rolfes L, Pawlitzki M, Pfeuffer S, Nelke C, Lux A, Pul R, et al. Ocrelizumab Extended Interval Dosing in Multiple Sclerosis in Times of COVID-19. Neurol Neuroimmunol Neuroinflamm. 2021;8(5):e1035. https://doi.org/10.1212/NXI.0000000000001035.
Rodriguez-Mogeda C, van Lierop ZYGJ, van der Pol SMA, Coenen L, Hogenboom L, Kamermans A, et al. Extended interval dosing of ocrelizumab modifies the repopulation of B cells without altering the clinical efficacy in multiple sclerosis. J Neuroinflamm. 2023;20:215. https://doi.org/10.1186/s12974-023-02900-z.
Guerrieri S, Bucca C, Nozzolillo A, Genchi A, Zanetta C, Cetta I, et al; SanRaf MS Study Group. Ocrelizumab extended-interval dosing in multiple sclerosis during SARS-CoV-2 pandemic: a real-world experience. Eur J Neurol 2023;30(9):2859–2864. https://doi.org/10.1111/ene.15891
Zanghì A, Ferraro D, Callari G, Valentino P, Granella F, Patti F, et al. Ocrelizumab Extended Interval Dosing in Primary Progressive Multiple Sclerosis: An Italian Experience. Curr Neuropharmacol. 2024;22(2):339–45. https://doi.org/10.2174/1570159X22666231002142709.
Author information
Authors and Affiliations
Contributions
R.G. and J.C. wrote the main manuscript text, prepared the figure and the table, and jointly reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflicts of interest/ Competing interests
RHG has no relevant financial or non-financial interests to disclose. JC reports personal fees from Annals of Neurology, personal fees from Rocky Mountain Multiple Sclerosis Center, grants from NIH/ Immune Tolerance Network, grants from EMD Serono, personal fees from Clene Biosciences, grants and personal fees from Bristol Myers Squib, and grants from National Multiple Sclerosis Society and Patient-Centered Outcomes Research Institute.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gross, R.H., Corboy, J. De-escalation and Discontinuation of Disease-Modifying Therapies in Multiple Sclerosis. Curr Neurol Neurosci Rep 24, 341–353 (2024). https://doi.org/10.1007/s11910-024-01355-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11910-024-01355-w