Abstract
Objective
To describe patient characteristics and assess the risk of disability worsening in patients of different age groups with focus on late-onset multiple sclerosis (LOMS) defined as disease onset after the age of 50 years.
Methods
The nationwide population-based Danish Multiple Sclerosis Registry served as data source. We described baseline characteristics and analyzed rates of reaching Expanded Disability Status Scale (EDSS) milestones.
Results
We identified 28,232 patients with MS with a known year of clinical onset, of which 2661 had LOMS. The LOMS group had a higher proportion of males and patients with primary progressive disease course, and they were less likely to receive disease-modifying therapy. The initial rate of reaching EDSS milestone 6 after diagnosis was higher in LOMS [hazard ratio (HR) 1.53; 95% confidence interval (CI) 1.14–2.06]; however, when assessing the risk of reaching EDSS 6 according to age, the HR was significantly lower for the LOMS group (HR 0.307; 95% CI 0.221–0.426).
Conclusion
The clinical characteristics and treatment approaches for patients with LOMS differ from their younger counterparts. Following diagnosis, patients with LOMS initially have an increased rate of reaching EDSS score 6; however, the risk of reaching EDSS score 6 at any given age is higher in patients with non-LOMS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple sclerosis (MS) has primarily been considered a disease of the younger population, though recent scientific reports have shown that the incidence, prevalence, and the mean age at onset of persons with MS are increasing [1, 2]. The increase in prevalence is likely due to the increased longevity of the general population and improved life expectancy in the MS population [3, 4]. Late-onset MS (LOMS), commonly defined as disease onset after the age of 50 years, is considered a rare phenomenon; however, the reported prevalence among patients with MS ranges between 4 and 10% in different studies [5,6,7]. A recent study investigating the incidence of MS over the last 60 years in Denmark found that the incidence of MS has doubled in women, and increased modestly in men—this increase was largely driven by an increase in LOMS among women [1].
Treatment of LOMS poses unique challenges. While effective in reducing neuroinflammation, the currently approved disease-modifying therapies (DMT) used in MS are not as effective in preventing the disability accumulation associated with neurodegeneration and progressive disease—both of which are dominating in older persons with MS [8], though a recent study has also shown that the effectiveness of DMT is reduced in patients with relapsing–remitting (RR) LOMS when compared to patients with onset earlier in life [9]. Clinical trials for the currently approved DMT have excluded individuals over 50–55 years with MS [10], making evidence on the safety and efficacy of DMT in elderly populations limited and based on observational studies. Despite this, treatment of LOMS with DMT is commonly initiated in daily clinical practice.
The aim of this study was to describe the demographics, disease characteristics and DMT usage for the Danish population with LOMS, and to assess the risk of reaching an Expanded Disability Status Scale (EDSS) score of 6 in persons with LOMS compared to their younger counterparts. Improved knowledge on the characteristics, prognosis and current treatment patterns concerning this growing group of patients is warranted.
Methods
Data sources
Data were provided by The Danish Multiple Sclerosis Registry (DMSR) [11]. The DMSR has collected data on the incidence of MS since 1948. All Danish Departments of Neurology treating patients with MS report data to the DMSR. Notification starts when MS is diagnosed and then at each visit in the clinic. Since 1996, with the introduction of the first DMT, it became mandatory to regularly collect data on all patients treated with DMT. During treatment, patients are monitored on clinical visits at regular intervals with recording of demographic, clinical and paraclinical data, as well as EDSS scores, relapses, side effects and data entered in an online notification platform.
Study population and outcomes
We included all patients diagnosed with MS having a known date or year of disease onset since the beginning of the data collection in 1948, and until date of data extraction on April 22nd, 2020. From these included patients, we defined 2 cohorts for the descriptive part of the study:
-
1.
A main cohort used for cross-sectional description of patient characteristics. All the above patients were included in this cohort.
-
2.
A sub-cohort used for cross-sectional description of treatment characteristics. Only patients diagnosed between 1st of January 2006 and 22nd of October 2019 (6 months before data extraction) with an initial disease course of relapsing-remitting MS (RRMS) were selected. Furthermore, patients were excluded if they had a history of receiving atypical or clinical trial drugs or if they were lacking information on whether they had received treatment or not. Atypical drugs were daclizumab, azathioprine, fampridine, intravenous immunoglobulins and cyclic corticosteroids. These filters were applied to reflect a representative and contemporary treatment-setting with availability of high-efficacy disease-modifying therapies (heDMT) in Denmark.
In calculation of statistics on changes to treatment within the first 5 years, patients were excluded if they started treatment within 5 years of data extraction or if they were terminated within 5 years of beginning treatment with DMT.
Lastly, we performed a longitudinal outcome analysis assessing the risk of reaching an EDSS milestone of 6 or above. This cohort included all patients with RRMS in the descriptive main cohort who, in addition, had any data on EDSS, had ever received DMT and had a valid baseline EDSS score less than 6. A valid baseline EDSS was defined as the first recorded EDSS score within 6 months of the date of diagnosis. If the date of diagnosis was recorded as either being the 1st of January or 1st of July, the date was assumed to be approximated according to clinical practice, and the first EDSS within 12 months of 1st of July on the given year was accepted as baseline EDSS. If a subsequent lower EDSS score was obtained within 12 months of the first, we assumed the first score to be reported unreliably high due to relapse activity and used the second value as the EDSS score at baseline. If a patient’s date of termination preceded their latest visit in the clinic, we assumed the date of termination to be unknown and the patient was excluded. Termination is defined as end of data collection due to patient-choice or due to a patient ending their medical service associated with any MS clinic in Denmark.
Statistical analysis
Main cohort: description of baseline characteristics according to age at onset
For the description of patient demographic and clinical characteristics in the main cohort, we grouped patients into five categories (< 18, 18–29, 30–39, 40–49 and ≥ 50 years of age) based on their age at disease onset. The characteristics are all presented as frequencies with corresponding percentages for categorical values, or as mean or median values with standard deviation (SD) or interquartile range (IQR) for continuous variables, as appropriate. As specified earlier, patients with missing data for a variable were not included when calculating descriptive statistics for that specific variable.
We calculated diagnostic delay as the time from clinical onset to the diagnosis of MS. If onset and diagnosis was reported to be simultaneous, onset was assumed to be approximated within same year and diagnostic delay was corrected to a quarter of a year following usual clinical practice.
We defined treatment delay as time from diagnosis of MS to initiation of DMT. Patients did not contribute to the calculation of treatment delay if they had an initial disease course other than RR, or if they never received DMT.
We defined onset symptom as multifocal if registered as: (a) multifocal or (b) optic pathway + any other symptom or (c) cerebellar + any other symptom or (d) brainstem + any other symptom or (e) sphincter + any other symptom that was not sensory or pyramidal.
The EDSS at diagnosis was defined according to the previous definition of a valid baseline EDSS.
For determining the disease course at presentation, we used a ranking model. This method was used in patients with multiple registered disease courses, since the disease course registered at time of diagnosis can be corrected after observing the patient over time. Our ranking was as follows, from low to high: (1) primary progressive MS (PPMS), (2) RRMS, (3) secondary progressive MS (SPMS). If multiple disease courses for a patient were registered, the lowest ranking course was assumed to be disease course at presentation.
Sub-cohort: treatment characteristics according to LOMS/non-LOMS
When describing treatment characteristics of this treated, contemporary sub-cohort, we grouped patients by age at onset (LOMS (≥ 50 years of age at onset) and non-LOMS (< 50 years of age at onset)) and sex (men, women and total). If a patient had received multiple treatments, all treatments could contribute to the descriptive analyses.
For classification of the initial treatment efficacy-tier, we classified the following therapies as moderate-efficacy DMT (meDMT): teriflunomide, interferon beta-1a, interferon beta-1b, glatiramer acetate and dimethyl fumarate. HeDMT were: fingolimod, alemtuzumab, cladribine, mitoxantrone, ocrelizumab, natalizumab, rituximab, methotrexate and treosulfane, ofatumumab and hematopoietic stem cell transplantation.
All switches during follow-up were recorded, so that every patient could contribute with more than one switch. We considered switching from a meDMT to a heDMT an escalation of treatment and a switch from a heDMT to a meDMT a de-escalation of treatment. We defined lateral switches as a switch between DMT within the same efficacy-tier.
Presented p values were calculated using χ2-tests for the categorical variables and using Mann–Whitney’s U test for differences in the duration of first treatment.
Longitudinal analysis: EDSS milestone analyses
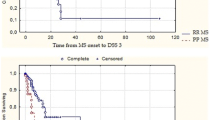
The probabilities of reaching a confirmed EDSS milestone of 6 were calculated using non-parametric Kaplan–Meier estimators. Confirmed EDSS milestone 6 was included as an event if the patient had two consecutive visits at least 6 months apart that met or exceeded an EDSS score of 6. The date of the initial worsening was chosen as the time of the event and not the confirming date. We performed analyses with two different underlying time-scales: using time since diagnosis and using age [12].
We assessed difference in rates of reaching EDSS 6 according to LOMS-status using univariate Cox-regression analyses as well as two multivariate Cox-regression analyses with LOMS-status as the exposure of interest, adjusted for potential confounders. The univariate model and the first multivariate model used time since diagnosis as time-scale, whereas the second multivariate model used age as time scale [13]. All Cox regression-models were checked for fulfillment of the relevant model assumptions (linearity of continuous covariates, interactions, proportional hazards). As baseline EDSS (categorical: 0, 1.0–2.5, 3.0–3.5, 4.0–4.5, > 5) and time from onset to treatment (categorical: < 2 years/ ≥ 2 years) did not fulfill the proportional hazards assumption, we stratified all multivariate Cox-regression analyses on these variables. The models further included the covariates: LOMS-status, sex and number of relapses 24 months prior to treatment start (continuous).
Patients were censored at time of death, emigration or termination. Furthermore, if a patient did not have a registered EDSS score for 3 years, the patient was censored at the date of the last registered EDSS score before this observational gap.
Standard protocol approvals, registrations, and patient consents
This study was approved by the Danish Data Protection Agency (approval number P-2019-734).
Ethics approval is not required in Denmark for non-interventional studies.
Data availability statement
Data will be shared upon request by any qualified investigator under approval from the Danish Data Protection Agency and the board of the Danish Multiple Sclerosis Group.
Results
Of 30,506 patients in the DMSR, we included 28,232 with a known date of disease onset (excluded: n = 149) and a diagnosis of MS in our cohort (excluded: n = 2125). A flow-chart depicting the final inclusion and exclusion counts for each of the analyzed cohorts can be seen in Fig. 1. The patient characteristics of the main cohort can be found in Table 1. Patients with higher age at onset tended to have a shorter diagnostic delay, a more recent calendar year of diagnosis, be less likely to have a multifocal onset, have a higher EDSS score, and have a higher probability of debuting with PPMS.
Of the 28,232 patients in the main cohort, a sub-cohort of 6411 patients diagnosed after 2006 was selected for investigating treatment characteristics according to LOMS-status. Table 2 shows the characteristics of this sub-cohort. The mean number of treatment switches was 1.85 switches per patient. Patients with late-onset RRMS were more likely to remain untreated and more likely to discontinue DMT. Furthermore, patients with LOMS were less likely to switch therapy, and those switching were less likely to escalate therapy to heDMT and more likely to perform lateral treatment switches.
Figure 2 shows the distribution of initial DMT in patients with non-LOMS (n = 5751) and LOMS (n = 418) for groups of 5 or more patients initiating the same DMT. Of the 97.39% patients with non-LOMS initiating DMT, 52.25% started on interferon beta-1a and 23.66% on teriflunomide. In the LOMS group 94.02% initiated DMT with 41.98% on interferon beta-1a and 36.13% on teriflunomide. We found only small differences between the sexes. Most notably we found a more frequent use of interferon beta-1a in men, and a slightly higher use of teriflunomide in women.
A total of 7016 patients were included in the longitudinal analysis investigating the risk of reaching EDSS 6. Total follow-up time was 42,373 (median 6.46) and 2067 (median 4.51) person-years for the non-LOMS and LOMS group, respectively. In accordance with the inclusion criteria, all patients contributing to this analysis were treated with DMT at some point during follow-up. To assess comparability between the groups, we calculated the percentage of follow-up time on treatment for each group. We found that on average the patients with non-LOMS were on treatment for 90.7% of the follow-up time, while on average, the patients with LOMS were on treatment for 91.6% of the follow-up time, which indicate similar cumulative treatment exposure across groups. Total follow-up time on treatment was 38,432 person-years for the non-LOMS group and 1893 person-years for the LOMS group.
We observed 496 events of 6-month confirmed EDSS 6 in the non-LOMS group and 49 events of 6-month confirmed EDSS 6 in the LOMS group.
Figure 3 shows the probability of reaching a 6-month confirmed EDSS 6 according to LOMS-status using time since onset as underlying time scale. Figure 4 shows the probability of reaching a 6-month confirmed EDSS 6 according to LOMS-status using age as the underlying time scale.
In both the univariate and multivariate Cox-regression analyses, all included covariates were associated with reaching a confirmed EDSS score of 6, except number of relapses 24 months prior to treatment in multivariate model 2. Results from the Cox-models are presented in Table 3. The adjusted Cox models confirmed the association observed from the Kaplan–Meier estimators. After confounder-adjustment, LOMS was associated with a 53% increase in the hazard of reaching EDSS 6 when using time since diagnosis as the underlying timescale, and a 69% decrease if using age as the underlying timescale. As baseline EDSS and time from onset to treatment did not fulfill the proportional hazards assumption, the multivariate Cox-models were stratified on these variables and we are not able to give an estimate of the effect from these. However, when stratifying the raw data, we observed increasing number of patients reaching EDSS 6 with increasing baseline EDSS (data not shown).
Discussion
We describe a nationwide population of patients with LOMS and compare them to their younger counterparts by analyzing data from the DMSR. We found a total of 9.43% of patients presenting with LOMS, which is similar to what has been reported in other cohorts [5, 7, 14, 15]. In line with our study, a previous report from the DMSR has shown that LOMS has been increasingly diagnosed in Denmark in recent years [1]. The same tendency has also been shown in the MSBase cohort [16].
Female sex was predominant in the LOMS group, though the female–male ratio was found to diminish with higher age, as seen previously [15]. Furthermore, patients with LOMS more often presented with PPMS when compared to the non-LOMS age groups. This is in line with previous knowledge, showing that higher age at onset is associated with primary progressive disease [17]. However, our study shows that RRMS is still the most common presentation among patients with LOMS.
We found a shorter diagnostic delay in patients with LOMS, possibly due to a combination of factors. The predominance of relapse activity in younger patients may provide a more precise time of onset, as opposed to patients with LOMS who less often experience relapses. This may lead to underestimation of the time since onset in patients with LOMS. Furthermore, older patients with neurologic symptoms are often diagnosed quickly due to concerns of stroke or cerebrovascular insult.
When considering time from diagnosis to treatment initiation, we see that, despite the lack of evidence from RCTs on clinical efficacy of DMT in persons with MS older than 50–55, physicians are prescribing DMT more rapidly after diagnosis for the patients with higher age at onset. Speculatively, this could be due to the higher mean EDSS score at diagnosis indicating that the elderly are initially more disabled, which could prompt a quicker treatment because of a perceived aggressive disease. However, it is also possible that the observation is a result of an evolving treatment strategy having increased emphasis on early treatment, as the mean year of diagnosis is higher for the patients with LOMS.
Furthermore, the relapsing–remitting patients with LOMS had a lower EDSS at diagnosis compared with the complete LOMS cohort, indicating that patients with PPMS and/or SPMS typically present with a higher EDSS at diagnosis, as expected. This tendency is not seen in the age groups with lower age at onset, though this could be because very few younger patients are diagnosed with progressive disease making a detection of difference difficult.
When comparing LOMS to non-LOMS in our sub-cohort, we found that men with LOMS were most likely to start on a high-efficacy DMT as initial treatment while having the longest adherence to treatment. This finding is somewhat unexpected as heDMT are usually prescribed to young people with high inflammatory activity [18]; however, our finding may simply be due to random variation caused by low sample size. Women with LOMS are very much alike their younger counterparts both regarding type of initial DMT and treatment adherence. Overall though, patients with LOMS are more likely to not start DMT (5.67% in LOMS vs 2.51% in non-LOMS), though surprisingly, the difference is very small despite the lack of evidence of DMT efficiency for this age category.
There is not much variation between the sexes with regards to switching or discontinuing treatment in the non-LOMS group. The male patients with LOMS look much alike the younger patients, while the female patients with LOMS have a ~ 23% lower tendency to switch to another treatment within 5 years and a ~ 16% higher tendency to stop treatment all together than the non-LOMS group.
Patients with non-LOMS were more prone to escalate treatment, which may partly be due to a combination of a higher proportion of patients with progressive disease course in LOMS, a lower inflammatory activity in older patients, and likely caution to prescribe DMT with possible serious adverse events to older patients. On the contrary, younger patients generally have more relapse activity [19], and therefore, a more aggressive treatment approach is often preferred.
When analyzing rates of reaching EDSS 6 with time since diagnosis as underlying time scale, we found that patients with RR LOMS had an about 53% higher rate of reaching the outcome. The results were similar in all types of analyzes. This indicates an accelerated initial rate of reaching EDSS 6 in patients with RR LOMS following diagnosis. Other studies has found similar results of increased rate of reaching EDSS 6 with higher age at onset [20, 21].
When analyzing rates of reaching EDSS 6 with age as the underlying time scale though, the rate was approximately 69% higher for patients with non-LOMS. This indicates that even though the initial rate of reaching EDSS 6 after diagnosis is higher in LOMS (as seen in the analysis with time since diagnosis as the timescale), the risk of reaching EDSS 6 at a given age is higher in patients with an earlier onset of disease. A longer disease duration in the non-LOMS group likely causes the more pronounced disability accumulation at a given age. A similar result was previously reported [22], showing a lower mean age at EDSS 6 for patients with younger age at onset, though the difference seen then could not be shown significant, possibly due to a smaller sample size.
A limitation of this study is that it assesses differences on the group-level but cannot predict the rate of disability worsening on the individual level. This means that the rates found does not apply for any single patient; however, on a group level, it is fair to assume that the tendencies found is reasonably generalizable to other populations owing to the nationwide nature of the study. Furthermore, our study only reports on results with an EDSS score of 6 as endpoint, though we found similar results for EDSS score 3, 3.5, 4 and 7 (data not shown).
Another limitation is the lack of standardized complete MRI data on patients, which could be used to adjust for disease activity. To alleviate this, we instead used clinically confirmed relapses in 2 years before treatment start as a measurement of disease activity.
An important strength of this study is the way data is collected into the DMSR. The Danish healthcare system is free for all Danish citizens and notification to DMSR is mandatory, thus we expect most cases of MS in Denmark to be represented in the registry. This gives a high data completeness but can also affect the validity. Patients presenting with progressive disease are often registered as RRMS at the slightest doubt of the disease course, since classification of the disease course as relapsing–remitting widens the possibility of treatment with DMT. We know that progressive disease is more frequent in the LOMS patient group and is, in the case of misclassification, therefore, a potential confounder that we cannot adjust for.
Another potentially unmeasured confounder when comparing age groups is a cohort effect resulting from different diagnostic criteria and availability of treatment at year of diagnosis—also known as the Will Rogers Phenomenon [23]. We found a slight difference in median year of diagnosis between the age groups with the higher age groups being diagnosed more recently. Patients diagnosed before the approval of the first DMT potentially had a longer disease duration before treatment start than those who had immediate access to DMT. However, limiting the longitudinal EDSS analyses to patients with onset from 2006 has likely mitigated most bias due to this.
Conclusion
Danish patients with LOMS have a higher chance of presenting with PPMS, a higher EDSS score at diagnosis and are less likely to switch DMT.
Patients with LOMS initially have an increased rate of reaching a disability milestone of EDSS 6; however, the risk of reaching EDSS 6 at any given age is higher in patients with non-LOMS, which is likely due to a longer disease duration and thus a longer time to accumulate disability.
Availability of data, code and material
Data and code will be shared upon request by any qualified investigator under approval from the Danish Data Protection Agency and the board of the Danish Multiple Sclerosis Group.
References
Koch-Henriksen N, Thygesen LC, Stenager E et al (2018) Incidence of MS has increased markedly over six decades in Denmark particularly with late onset and in women. Neurology 90:e1954–e1963. https://doi.org/10.1212/WNL.0000000000005612
D’Amico E, Patti F, Zanghì A et al (2018) Late-onset and young-onset relapsing-remitting multiple sclerosis: evidence from a retrospective long-term follow-up study. Eur J Neurol 25:1425–1431. https://doi.org/10.1111/ene.13745
Koch-Henriksen N, Laursen B, Stenager E, Magyari M (2017) Excess mortality among patients with multiple sclerosis in Denmark has dropped significantly over the past six decades: a population based study. J Neurol Neurosurg Psychiatry 88:626–631. https://doi.org/10.1136/jnnp-2017-315907
Lunde HMB, Assmus J, Myhr KM et al (2017) Survival and cause of death in multiple sclerosis: a 60-year longitudinal population study. J Neurol Neurosurg Psychiatry 88:621–625. https://doi.org/10.1136/jnnp-2016-315238
Martinelli V, Rodegher M, Moiola L, Comi G (2004) Late onset multiple sclerosis: clinical characteristics, prognostic factors and differential diagnosis. Neurol Sci 25:S350–S355. https://doi.org/10.1007/s10072-004-0339-8
Bove R, Chitnis T (2013) Sexual disparities in the incidence and course of MS. Clin Immunol 149:201–210
Polliack ML, Barak Y, Achiron A (2001) Late-onset multiple sclerosis. J Am Geriatr Soc 49:168–171. https://doi.org/10.1046/j.1532-5415.2001.49038.x
Peterson JW, Trapp BD (2005) Neuropathobiology of multiple sclerosis. Neurol Clin 23:107–129
Amato MP, Fonderico M, Portaccio E et al (2020) Disease-modifying drugs can reduce disability progression in relapsing multiple sclerosis. Brain 143:3013–3024. https://doi.org/10.1093/brain/awaa251
Trojano M, Tintore M, Montalban X et al (2017) Treatment decisions in multiple sclerosis—insights from real-world observational studies. Nat Rev Neurol 13:105–118. https://doi.org/10.1038/nrneurol.2016.188
Magyari M, Joensen H, Laursen B, Koch-Henriksen N (2020) The Danish Multiple Sclerosis Registry. Brain Behav. https://doi.org/10.1002/brb3.1921
Korn EL, Graubard BI, Midthune D (1997) Time-to-event analysis of longitudinal follow-up of a survey: choice of the time-scale. Am J Epidemiol 145:72–80. https://doi.org/10.1093/oxfordjournals.aje.a009034
Thiébaut ACM, Bénichou J (2004) Choice of time-scale in Cox’s model analysis of epidemiologic cohort data: a simulation study. Stat Med 23:3803–3820. https://doi.org/10.1002/sim.2098
Noseworthy J, Paty D, Wonnacott T et al (1983) Multiple sclerosis after age 50. Neurology 33:1537–1544. https://doi.org/10.1212/wnl.33.12.1537
Bove RM, Healy B, Augustine A et al (2012) Effect of gender on late-onset multiple sclerosis. Mult Scler J 18:1472–1479. https://doi.org/10.1177/1352458512438236
Kister I, Chamot E, Cutter G et al (2012) Increasing age at disability milestones among MS patients in the MSBase Registry. J Neurol Sci 318:94–99. https://doi.org/10.1016/j.jns.2012.03.017
Ontaneda D (2019) Progressive multiple sclerosis. Contin Lifelong Learn Neurol 25:736–752. https://doi.org/10.1212/CON.0000000000000727
Buron MD, Chalmer TA, Sellebjerg F et al (2020) Initial high-efficacy disease-modifying therapy in multiple sclerosis. Neurology 95:e1041–e1051. https://doi.org/10.1212/WNL.0000000000010135
Tremlett H, Zhao Y, Joseph J et al (2008) Relapses in multiple sclerosis are age- and time-dependent. J Neurol Neurosurg Psychiatry 79:1368–1374. https://doi.org/10.1136/jnnp.2008.145805
Alroughani R, Akhtar S, Ahmed S et al (2016) Is time to reach EDSS 6.0 faster in patients with late-onset versus young-onset multiple sclerosis? PLoS ONE. https://doi.org/10.1371/journal.pone.0165846
Guillemin F, Baumann C, Epstein J et al (2017) Older age at multiple sclerosis onset is an independent factor of poor prognosis: a population-based cohort study. Neuroepidemiology 48:179–187. https://doi.org/10.1159/000479516
Tremlett H, Devonshire V (2006) Is late-onset multiple sclerosis associated with a worse outcome? Neurology 67:954–959. https://doi.org/10.1212/01.wnl.0000237475.01655.9d
Sormani MP, Tintorè M, Rovaris M et al (2008) Will Rogers phenomenon in multiple sclerosis. Ann Neurol 64:428–433. https://doi.org/10.1002/ana.21464
Acknowledgements
We would like to acknowledge all neurology departments in Denmark for collecting data and the Danish Multiple Sclerosis Society for funding The Danish Multiple Sclerosis Registry.
Funding
This study was sponsored by Lundbækfonden.
Author information
Authors and Affiliations
Contributions
MAA: Danish Multiple Sclerosis Registry, Design and Conceptualization; Methodology; Software; Data analysis; Visualization; Drafting and revision for intellectual content. MDB: Danish Multiple Sclerosis Registry, Design and Conceptualization; Methodology; Software; Data analysis; Drafting and revision for intellectual content. MM: Danish Multiple Sclerosis Registry, Design and Conceptualization; Methodology; Drafting and revision for intellectual content, Supervision; Funding acquisition; Resources.
Corresponding author
Ethics declarations
Conflicts of interest
Mads Albrecht Andersen reports no disclosures. Dr. Buron has received support for congress participation from Roche. Dr. Magyari has served on scientific advisory board for Biogen, Sanofi, Roche, Novartis, Merck and AbbVie, has received honoraria for lecturing from Biogen, Merck, Novartis, Sanofi, Genzyme, has received research support and support for congress participation from Biogen, Genzyme, Teva, Roche, Merck and Novartis.
Standard protocol approvals, registrations, and patient consents
This study was approved by the Danish Data Protection Agency (approval number P-2019-734). Ethics approval is not required in Denmark for non-interventional studies.
Rights and permissions
About this article
Cite this article
Andersen, M.A., Buron, M.D. & Magyari, M. Late-onset MS is associated with an increased rate of reaching disability milestones. J Neurol 268, 3352–3360 (2021). https://doi.org/10.1007/s00415-021-10490-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00415-021-10490-0