Abstract
Infections of cerebrospinal fluid (CSF) shunts remain a common surgical complication causing significant morbidity in children with hydrocephalus. As most of the literature regarding these infections includes only small cohorts from a single institution’s experience, there remain large knowledge gaps and little support for the prevailing management strategies. Regarding the microbiology of shunt infections, little has changed in the past 10 years, other than the emergence of methicillin-resistant strains of coagulase-negative staphylococcus (CoNS) and Staphylococcus aureus, which remain the two predominant etiologic agents. Molecular diagnostics such as multiplex PCR have been used to identify the complex microflora of shunt infections and in the future could prove a useful adjunct for early diagnosis and targeting of antimicrobial therapy. Antibiotic-impregnated catheters for use in external ventricular drains and CSF shunts have been adopted into clinical practice and appear to reduce the risk of shunt infection by susceptible organisms.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In the early 1950s, a pediatric neurosurgeon named Eugene Spitz, with the help of John Holter, a patient’s father, developed the use of cerebrospinal fluid (CSF) shunts and revolutionized the treatment of hydrocephalus [1]. Ventriculoperitoneal (VP) shunts, the most common type used presently, serve to bypass obstructions in CSF circulation by diverting CSF directly to the peritoneal cavity. An estimated 40,000 such shunts are placed annually in the USA [2].
After more than 60 years of widespread use, infection remains a substantial complication of CSF shunting procedures. Approximately 8–10 % of all shunts placed become infected, resulting in thousands of shunt removals, replacements, and significant morbidity and mortality [3–5]. Despite the high incidence of CSF shunt infections, there remain no universal guidelines as to their management and significant variation in practice is found between institutions. Recent studies challenge the traditional treatment modalities through the use of adjunctive intraventricular antibiotics, shortened antibiotic courses, or use of antibiotics such as linezolid, which may better penetrate biofilms. Other research has centered on preventing infectious complications through standardized protocols directing perioperative technique and the use of antibiotic-impregnated catheters. This article will review the evolving microbiology of CSF shunt infections as well as the most recent evidence on the prevention and management of these challenging infections.
Challenges to the Study of CSF Shunt Infections
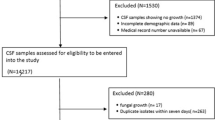
Literature on CSF shunt infections consists primarily of small retrospective cohort studies examining infection rate, risk factors for infection, pathogens identified, and occasionally outcomes from a single institution. There is a paucity of large, multi-center, and prospective randomized studies in children. It is therefore difficult to estimate the true incidence of CSF shunt infection, let alone make recommendations regarding its management.
Reported rates of CSF shunt infection between institutions vary greatly, due to different definitions used for shunt infection, different lengths of surveillance, and different patient populations and age groups studied as well as a variety of factors intrinsic to the study site. In one recent multi-center study of 41 US children’s hospitals, the CSF shunt infection rate ranged widely by hospital from 4.1 to 20.5 %. After adjusting for a collection of significant patient, hospital, and surgeon factors, the range narrows to between 8.8 and 12.8 % per patient. This indicates that much of the variability lies in the presence of known patient risk factors such as younger age, number of previous shunt revisions, and intraventricular hemorrhage (IVH) as the cause of hydrocephalus [5, 6].
The small size and heterogeneity of the pediatric patient population make it difficult to sufficiently power any prospective studies comparing interventions aimed at prevention and treatment of shunt infections. A few meta-analyses and multi-center reviews have sought to combine the experience of smaller institutions to help answer questions such as the efficacy of antibiotic-impregnated systems (AIS) [7•, 8, 9, 10••].
Pathogenesis and Risk Factors
It is traditionally accepted that most CSF shunt infections result from colonization of the shunt at the time of surgery. This conclusion is supported by both the timing of most shunt infections, which most commonly occur in the first few months following surgery, as well as the predominant isolation of causative microorganisms that are found to colonize the skin. This theory is supported by recent studies. In one retrospective cohort of 333 CSF shunt placements in children from Korea, 51.4 % of infections took place within 1 month of insertion and 91.4 % occurred within 3 months [11]. Of shunt infections in a series from Turkey, 71.4 % occurred within 4 months of shunt insertion [12].
Early identification and treatment of CSF shunt infections can reduce morbidity and mortality. This requires an understanding of the most common presenting clinical signs and symptoms of shunt infections and of the risk factors that help define the population at risk. Several of these risk factors for cerebrospinal fluid shunt infections are summarized in Table 1. A high index of suspicion is required for identifying VP shunt infections, as they can often be occult. Fever is almost universally present; however, more specific signs such as seizures, neurologic changes, or local inflammation may only be present in 30–40 % of cases [11, 12]. In cases of infections caused by low-virulence organisms such as Staphylococcus epidermidis, fever may be absent or low grade and lethargy may be the most common presenting sign, reflecting progressive shunt malfunction. Many laboratory tests have been evaluated for use in screening patients for VP shunt infections. In one series of 92 shunt infections, 98 % of cases had an elevated C-reactive protein (CRP), defined as >3 mg/L, indicating that a normal value may be useful in ruling out shunt infections [17].
Risk factors for shunt infection identified in the Korean cohort include post-hemorrhagic hydrocephalus and age <1 year at time of insertion [11]. Shunts placed in the first 12 months of life also had the highest complication rate in a study of children in Kosovo, supporting previous reports that show children, especially infants, are more likely than adults to develop CSF shunt infections [18]. This is most likely due to immaturity of the infant immune system and skin barrier and a higher density of bacteria colonizing the skin in neonates admitted to the intensive care unit [19, 20].
Past studies have identified previous shunt infection and shunt revision as risk factors for CSF shunt infection, again supporting the theory of contamination at the time of surgery. A recent study of repeated shunt infections in children reported that of those who develop a second shunt infection, 60 and 47 % will go on to develop a third and fourth shunt infection, respectively [21•]. In virtually all of these instances, multiple shunt hardware revisions are involved. Another look at the risk of infection following CSF shunt revision revealed a significantly higher risk of infection after revision when compared to the risk at initial placement (HR 3.0, 95 % CI 1.9–4.7) that increased with the number of revisions [13]. This creates a frustrating cycle of shunt infection or malfunction requiring revision, which can then be complicated by re-infection. A retrospective review of 64 pediatric patients who had VP shunts placed at the University of Rochester Medical Center from 1990 to 1996 showed that over the ensuing 20 years of follow-up, 84.5 % required one or more shunt revisions, 9 % of which were because of infection [22].
Traditional Microbiology
As previously noted, the microbiology of cerebrospinal shunt infections follows closely along the lines of bacteria that are likely to contaminate or colonize the shunt at the time of placement. Table 2 summarizes some of the larger studies in an attempt to illustrate some of the consistencies in microbiology isolates found in studies across decades and continents. In nearly every study, Staphylococcus species are the predominant isolates obtained. This likely reflects their role as prominent skin flora. CoNS have proven to be the most common pathogen accounting for nearly 75 % of infections in some series. These bacteria are the prototype for device-related infections secondary to their ability to create a biofilm on the catheter material that is able to evade the immune system and antimicrobials. Gram-negative bacteria are the next most common group of pathogens isolated. The presence of these bacteria most likely represent colonization from the intensive care setting as well as their role as common pathogens in the neonatal period. The finding of other classifications of other skin-colonizing bacteria such as diphtheroids and anaerobic bacteria is somewhat more variable. This may be a result of inconsistent culturing practices as well as variable antibiotic prophylaxis practices during the neurosurgical procedure.
There have been occurrences of VP shunt infections involving more than one organism. One major source of these polymicrobial infections is the gastrointestinal tract. In some cases, the distal end of the shunt catheter has been reported to perforate the bowel and result in contamination and infection of the peritoneal end of the catheter [30]. A major clue that this may have occurred is the microbiology of these infections. CSF cultures growing enterobacteriaceae and anaerobes such as Bacteroides fragilis should prompt clinicians to consider an enteric source of VP shunt infection and evaluate for the presence of a perforated viscus.
Current Trends in Management
Although there are no universally accepted guidelines for the management of CSF shunt infections, most cite the results of a meta-analysis by Schreffler et al., which pooled available data on therapy and outcomes from case reports, case series, and a single randomized control trial [31, 32]. The most conservative practice involved immediate removal of the shunt followed by placement of a temporary external ventricular drain (EVD) or use of serial ventricular taps and intravenous (IV) antibiotics with or without intraventricular antibiotics. This intervention was compared to immediate shunt replacement with IV antibiotics, again with or without intraventricular antibiotics; and both were compared to the use of IV antibiotics without shunt replacement. The most conservative approach emerged as the superior modality with a cure rate of 88 %, compared to 64 % in the immediate shunt replacement group and only 34 % of those who received antibiotics alone. To date, most non-surgical management approaches of CSF shunt infections have not been successful, most likely due to the ability of the most common pathogens to form biofilms on the shunt hardware, which limit antibiotic penetration [17].
The authors concluded that this approach of shunt removal followed by temporary CSF divergence using EVD would be the most effective method of CSF shunt infection treatment as long as the rate of EVD infection remained low [31]. A survey of 84 pediatric neurosurgeons demonstrated that approximately 2/3 practice shunt removal with EVD placement as first-line management of cerebrospinal fluid shunt infections; however, the same survey demonstrated marked variability in the duration of antibiotic treatment, ranging from 2–21 days of treatment from the first sterile culture for staphylococcal species and 2–37 days for infections with a gram-negative bacillus [33].
While there is little doubt about the morbidity associated with CSF shunt infections, the mortality associated with them is less clear. Some of the best data can be gleaned from the meta-analysis described above. In comparing the treatment groups, the conservative therapy group that underwent removal of the shunt and temporary CSF diversion experienced a 5.7 % mortality rate. Those who received antibiotic therapy with no surgical intervention had 20.4 % mortality rate. It should be noted, however, that a selection bias could be present, as the patients who did not undergo a surgical procedure may have been unusually complex with co-morbidities making them poor surgical candidates. Finally, the literature reminds us that infection alone is a predictor for morbidity and mortality. In Tuli’s review of 907 patients who received shunts over 10 years, the greatest predictor of death was the presence of infection with a hazard ratio of 1.66 [34].
Duration of systemic antibiotic treatment varies greatly, usually based on the organism isolated and how quickly the CSF becomes sterile. In this area, there are also no controlled prospective randomized trials comparing different regimens. In general, with common organisms such as CoNS, antimicrobial therapy is continued for 7–10 days after CSF cultures are negative before re-shunting, with some advocating for a 2–5-day interval off of antimicrobials before replacing the shunt to insure clearance of the infection [17, 35]. For more virulent and difficult to clear organisms such as S. aureus or gram-negative bacilli, recommendations range anywhere from 10 to 21 days of antimicrobial therapy following negative cultures before re-shunting [35, 36]. The length of time during which the shunt is externalized while the patient receives systemic antimicrobial therapy must be weighed against the significant risk of retrograde infection from the external ventricular drain, which increases with duration of ventriculostomy placement and approaches 5–8 % [37].
Perhaps no topic is more controversial than the use of intraventricular antibiotics as an adjunct therapy in the treatment of shunt infections. Several groups have demonstrated more rapid sterilization of the CSF and excellent overall treatment success rates with shorter durations of antimicrobials through a more aggressive approach using adjunctive intraventricular antimicrobials in addition to shunt externalization and intravenous antimicrobials [38, 39]. Historically, there is only one multi-center randomized controlled study evaluating the use of intraventricular antibiotics in pediatric patients. This study examined the role of intraventricular gentamicin in the treatment of neonatal meningitis due to gram-negative enteric bacilli, mostly Escherichia coli and Salmonella species. This study was terminated early secondary to higher mortality rates in the intraventricular antibiotic group [40]. Later analysis of the CSF from these patients noted higher levels of endotoxins and interleukin-1 beta concentrations in the CSF of the patients who received intraventricular antibiotics versus those who received intravenous antibiotics alone [41]. Other antibiotics have been associated with complications when administered intraventricularly. Reports of toxicity with cefazolin and nafcillin administration make the use of intraventricular beta-lactam antibiotics less acceptable [42, 43]. Conversely, more recent data suggests that intraventricular antibiotics may play a role in the treatment of shunt infections. James et al. reports on the development and deployment of a protocol that combines administration of intraventricular antibiotics for 2 weeks with intravenous antibiotics for 3 weeks for the management of complicated shunt infections. The authors report that when intraventricular antibiotics were used in combination with complete removal and replacement of the shunt, they achieved both short and long-term microbiologic and clinical cure in 25 consecutive patients with no morbidity attributable to the intraventricular antibiotics [39, 44]. Our group has had limited experience with the use of intraventricular antimicrobials, but reserve them for use in cases in which shunt removal is not possible or when CSF cultures have failed to clear with use of intravenous antimicrobials alone.
Emerging Microbiological Trends
The most common etiologic agents isolated from recent studies of CSF shunt infections are listed in Table 2 and remain largely unchanged from those traditionally reported. CoNS and S. aureus remain the predominant shunt infection pathogens isolated. However, the emergence of methicillin-resistant S. epidermidis (MRSE) (at rates reported between 70–80 % of all CoNS in some institutions) in addition to methicillin-resistant S. aureus (MRSA) is a significant trend and should be considered when choosing initial empiric antimicrobial therapy [11, 17].
In the past 10 years, the increased use of anaerobic culture techniques and prolonged incubation time have led to the increased recognition of diphtheroids, such as Propionibacterium acnes, as common pathogens responsible for shunt infection, causing as many as 17 % of shunt infections in one series [45, 46]. It has been suggested by some investigators that CSF cultures should be incubated for up to 10 days in order to grow fastidious organisms or those exposed to antibiotics prior to collection [47]. Fungal infections of cerebrospinal fluid shunts, especially Candida spp., remain rare, but have been rising, especially in patients with known risk factors for invasive fungal infection such as broad-spectrum antibiotic use, prematurity, immunocompromised state, steroid use, and indwelling bladder and central venous catheters [48].
Molecular diagnostics such as polymerase chain reaction (PCR) are being investigated as potential diagnostic tools for identifying pathogens in shunt infections. One early study of 86 CSF samples from shunts in adults found that out of 56 PCR-positive specimens, 42 had sterile cultures. Most of these culture-negative samples occurred after antibiotic use. P. acnes and S. aureus were the most commonly isolated pathogens by PCR [49]. A recent study utilized 16S rRNA gene amplification to evaluate the microbiota of CSF shunt infections in eight children. In addition to the usual bacterial pathogens, they were able to identify a large variety of bacterial and fungal organisms that were not recovered by conventional culture, some of which persisted after antimicrobial treatment. This highlights the importance of obtaining anaerobic and fungal cultures of CSF and utilizing prolonged incubation times to increase detection of shunt pathogens as well as a significant trend toward the use of molecular diagnostics in this field [50•].
Current and Investigational Therapies
Antimicrobial Therapy
Empiric antimicrobial therapy for CSF shunt infections should include agents that have bactericidal activity against the most common pathogens isolated as previously discussed and which possess the ability to penetrate into the central nervous system. Traditional use of anti-staphylococcal penicillins for empiric staphylococcal coverage and perioperative prophylaxis has been replaced by the use of vancomycin due to rising rates of MRSE and MRSA. Not surprisingly, the use of vancomycin was associated with a 20 % higher treatment success rate than the use of flucloxacillin in a recent study of CSF shunt infections from a center with a MRSE rate of 68 % [17]. Initial empiric antimicrobial therapy for CSF shunt infections should also include broad coverage for gram-negative bacilli, including Pseudomonas spp., with an agent such as ceftazidime, cefepime, or meropenem, depending on the patient’s own history and institutional prevalence of extended spectrum beta-lactamase-producing organisms. Table 3 includes suggested management techniques and antibiotic choices based on the organism isolated.
Although a complete shunt system removal is preferred in the management of CSF shunt infections, there are situations in which the patient cannot tolerate surgery to remove the shunt. Successful non-surgical treatment of CSF shunt infections with linezolid has been reported [51]. This prompted a look at the in vitro action of this drug, and other commonly used first-line antibiotics, on biofilms. Linezolid was shown to eliminate the biofilms of MRSE and MRSA at drug levels achievable by intravenous or oral administration. Vancomycin also showed lasting effects against staphylococcal biofilms, but only at the higher concentrations achievable by intraventricular administration. Neither drug however was effective against the biofilms of Enterococcus faecalis or Enterococcus faecium [2]. Although more clinical experience is necessary, the use of linezolid and/or intraventricular vancomycin may be useful alternative therapies for clearing shunt infections when surgery is not an option or adjuncts for use when CSF cultures remain persistently positive.
Operative Management
As the management of CSF shunt infections involves invasive surgery to remove the shunt and long courses of antibiotics, much research has been appropriately focused on developing institutional standardized protocols to prevent shunt colonization during its initial placement, targeting such practices as hand-washing, preoperative preparation of the patient’s head, double-gloving, and minimal handling of the shunt catheter, among others. In a small study from Saudi Arabia, the simple practice of double gloving and removing the outer set of gloves before handling the shunt demonstrated a statistically significant reduction in CSF shunt infection rate, from 16.33 to 3.77 % (P = 0.046); however, there was an alarmingly high infection rate in the control group [52]. A study by the Hydrocephalus Clinical Research Network (HCRN) at four pediatric hospitals demonstrated a 36 % relative risk reduction in CSF shunt infection rates, from 8.8 to 5.7 % (P = 0.003), through the institution of an 11-step protocol that standardized key components of CSF shunt placement, such as hand-washing technique, patient positioning, preoperative hair washing, and use of antibiotic-impregnated sutures [53•].
Traditional practice for shunt reinsertion following an infection is to avoid the ventricular entry site that became infected and create a new shunt track. However, in a review of recurrent shunt infections in one institution, reusing recently infected ventricular entry sites carried the same risk of re-infection as switching to a new entry site [54]. Efforts to improve surgical technique and the practices surrounding shunt placement are integral to infection control and minimizing surgical shunt infections, and more research into this area of practice is needed.
Antibiotic-Impregnated Catheters
One of the most-studied interventions to prevent CSF shunt infections in recent years has been the use of antibiotic-impregnated systems (AIS). In 2003, catheters impregnated with rifampicin plus either clindamycin or minocycline or with silver nanoparticles were introduced for use in EVD and CSF shunts, with the hopes of preventing bacterial colonization and infection. The release of antibiotics from these catheters into the lumen and surrounding tissues can last for approximately 50 days, which covers the period of highest risk for post-operative shunt infection. In preliminary in vitro and animal studies, these materials were shown to reduce catheter colonization [10••]. The outcomes of the largest, most significant studies evaluating the use of AIS in preventing EVD and VP shunt infections are summarized in Table 4.
One of the first, albeit small studies, to evaluate the use of antibiotic-impregnated shunt (AIS) systems in humans demonstrated a significant decrease in shunt infections with staphylococci organisms, with 10 present in the control group compared to none in the AIS group (P = 0.038) [56]. A prospective, double-blinded, randomized, controlled trial in adults compared plain catheters used for external ventricular drains (EVD) to those impregnated with silver. The risk of CNS infection in the silver group was 42.5 % lower than that of the plain EVD group (21.4 % vs 12.3 %, P = 0.043) [55••].
A prospective observational study of AIS at King’s College Hospital in pediatric and adult patients demonstrated a comparatively low infection rate of 3.2 %, including only 4 infections from among 125 shunt placements. All four infections were with rifampicin-resistant S. epidermidis, implying a selection of antibiotic resistant strains [57]. The largest set of data on the use of antibiotic-impregnated shunts in pediatric patients comes from a multi-center prospective observational study from three sites in the U.K.. The researchers compared infection rates in patients receiving antibiotic-impregnated shunts to historical controls with traditional shunts. Although the pooled data from the three sites demonstrated a significantly lower infection rate in the group receiving antibiotic-impregnated shunts (OR 0.60, 95 % CI 0.38–0.93), the confidence intervals from the individual sites had significant overlap [7•]. Several groups have reported lower infection rates with the use of antibiotic-impregnated catheters, but many studies are underpowered to show a significant difference or used historical controls instead of randomized controls, making them vulnerable to bias. Others used AIS combined with minimal handling protocols or other bundled interventions, and although these studies showed reductions in CSF shunt infections, it is difficult to independently evaluate the contribution of the AIS [58]. Although the collective evidence for a beneficial role of AIS in preventing shunt infections is promising, well-designed, adequately powered, double-blinded, randomized control trials are necessary before their benefit can be confirmed.
Conclusions
CSF shunt infections remain a significant and challenging complication in children with hydrocephalus. Although improvements in surgical technique, perioperative antibiotic prophylaxis, and early recognition and treatment of these infections have resulted in lowered infection rates and associated morbidity, CSF shunt infection rates remain unacceptably high. The microbiology of these infections is well established, but has been impacted by the emergence of multi-drug-resistant pathogens such as MRSE and MRSA. Molecular diagnostics, such as multiplex PCR, will likely play an increasing role in rapid and comprehensive identification of CSF shunt infection pathogens and may further identify previously less appreciated co-pathogens. Sufficiently powered, randomized control trials are urgently necessary to establish the best management practices relating to these infections, including the duration of antibiotic therapy, use of adjuvant intraventricular antimicrobials, and efficacy of AIS.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance and •• Of major importance
Downey SA. Eugene B. Spitz, 87; Developed a life-saving operation. The Philadelphia Inquirer. 2006 December 19, 2006.
Bayston R, Ullas G, Ashraf W. Action of linezolid or vancomycin on biofilms in ventriculoperitoneal shunts in vitro. Antimicrob Agents Chemother. 2012;56(6):2842–5. doi:10.1128/AAC.06326-11.
Kestle J, Drake J, Milner R, Sainte-Rose C, Cinalli G, Boop F, et al. Long-term follow-up data from the shunt design trial. Pediatr Neurosurg. 2000;33(5):230–6.
Kestle JR, Drake JM, Cochrane DD, Milner R, Walker ML, Abbott 3rd R, et al. Lack of benefit of endoscopic ventriculoperitoneal shunt insertion: a multicenter randomized trial. J Neursurg. 2003;98(2):284–90. doi:10.3171/jns.2003.98.2.0284.
Simon TD, Hall M, Riva-Cambrin J, Albert JE, Jeffries HE, Lafleur B, et al. Infection rates following initial cerebrospinal fluid shunt placement across pediatric hospitals in the United States. J Neurosurg Pediatr. 2009;4(2):156–65. doi:10.3171/2009.3.PEDS08215. Clinical article.
Prusseit J, Simon M, von der Brelie C, Heep A, Molitor E, Volz S, et al. Epidemiology, prevention and management of ventriculoperitoneal shunt infections in children. Pediatr Neurosurg. 2009;45(5):325–36. doi:10.1159/000257520.
Kandasamy J, Dwan K, Hartley JC, Jenkinson MD, Hayhurst C, Gatscher S, et al. Antibiotic-impregnated ventriculoperitoneal shunts—a multi-centre British paediatric neurosurgery group (BPNG) study using historical controls. Childs Nerv Syst. 2011;27(4):575–81. doi:10.1007/s00381-010-1290-z. This multi-center historical control study is the largest to evaluate the use of AIS in pediatric patients.
Ratilal B, Costa J, Sampaio C. Antibiotic prophylaxis for surgical introduction of intracranial ventricular shunts. Cochrane Database Syst Rev. 2006;3, CD005365. doi:10.1002/14651858.CD005365.pub2.
Steinbok P, Milner R, Agrawal D, Farace E, Leung GK, Ng I, et al. A multicenter multinational registry for assessing ventriculoperitoneal shunt infections for hydrocephalus. Neurosurgery. 2010;67(5):1303–10. doi:10.1227/NEU.0b013e3181f07e76.
Thomas R, Lee S, Patole S, Rao S. Antibiotic-impregnated catheters for the prevention of CSF shunt infections: a systematic review and meta-analysis. Br J Neurosurg. 2012;26(2):175–84. doi:10.3109/02688697.2011.603856. This large review of 12 studies on antibiotic-impregnated catheters in adult and pediatric shunt infections shows a significant trend toward their benefit.
Lee JK, Seok JY, Lee JH, Choi EH, Phi JH, Kim SK, et al. Incidence and risk factors of ventriculoperitoneal shunt infections in children: a study of 333 consecutive shunts in 6 years. J Korean Med Sci. 2012;27(12):1563–8. doi:10.3346/jkms.2012.27.12.1563.
Turgut M, Alabaz D, Erbey F, Kocabas E, Erman T, Alhan E, et al. Cerebrospinal fluid shunt infections in children. Pediatr Neurosurg. 2005;41(3):131–6. doi:10.1159/000085869.
Simon TD, Whitlock KB, Riva-Cambrin J, Kestle JR, Rosenfeld M, Dean JM, et al. Revision surgeries are associated with significant increased risk of subsequent cerebrospinal fluid shunt infection. Pediatr Infect Dis J. 2012;31(6):551–6. doi:10.1097/INF.0b013e31824da5bd.
Simon TD, Butler J, Whitlock KB, Browd SR, Holubkov R, Kestle JR, et al. Risk factors for first cerebrospinal fluid shunt infection: findings from a multi-center prospective cohort study. J Pediatr. 2014. doi:10.1016/j.jpeds.2014.02.013.
Kim JH, Desai NS, Ricci J, Stieg PE, Rosengart AJ, Hartl R, et al. Factors contributing to ventriculostomy infection. World Neurosurg. 2012;77(1):135–40. doi:10.1016/j.wneu.2011.04.017.
Topjian AA, Stuart A, Pabalan AA, Clair A, Kilbaugh TJ, Abend NS, et al. Risk factors associated with infections and need for permanent cerebrospinal fluid diversion in pediatric intensive care patients with externalized ventricular drains. Neurocrit Care. 2014. doi:10.1007/s12028-013-9946-7.
von der Brelie C, Simon A, Groner A, Molitor E, Simon M. Evaluation of an institutional guideline for the treatment of cerebrospinal fluid shunt-associated infections. Acta Neurochir (Wien). 2012;154(9):1691–7. doi:10.1007/s00701-012-1329-x.
Morina Q, Kelmendi F, Morina A, Morina D, Bunjaku D. Ventriculoperitoneal shunt complications in a developing country: a single institution experience. Med Arh. 2013;67(1):36–8.
James HE, Bejar R, Gluck L, Coen R, Merritt A, Mannino F, et al. Ventriculoperitoneal shunts in high risk newborns weighing under 2000 grams: a clinical report. Neurosurgery. 1984;15(2):198–202.
Pople IK, Bayston R, Hayward RD. Infection of cerebrospinal fluid shunts in infants: a study of etiological factors. J Neursurg. 1992;77(1):29–36. doi:10.3171/jns.1992.77.1.0029.
Tuan TJ, Thorell EA, Hamblett NM, Kestle JR, Rosenfeld M, Simon TD. Treatment and microbiology of repeated cerebrospinal fluid shunt infections in children. Pediatr Infect Dis J. 2011;30(9):731–5. doi:10.1097/INF.0b013e318218ac0e. A study demonstrating the significantly higher CSF shunt infection rate among children with a history of shunt infections.
Stone JJ, Walker CT, Jacobson M, Phillips V, Silberstein HJ. Revision rate of pediatric ventriculoperitoneal shunts after 15 years. J Neurosurg Pediatr. 2013;11(1):15–9. doi:10.3171/2012.9.PEDS1298.
Odio C, McCracken Jr GH, Nelson JD. CSF shunt infections in pediatrics. A seven-year experience. Am J Dis Child. 1984;138(12):1103–8.
Enger PO, Svendsen F, Wester K. CSF shunt infections in children: experiences from a population-based study. Acta Neurochir. 2003;145(4):243–8. doi:10.1007/s00701-002-1068-5. discussion 8.
Ronan A, Hogg GG, Klug GL. Cerebrospinal fluid shunt infections in children. Pediatr Infect Dis J. 1995;14(9):782–6.
Kontny U, Hofling B, Gutjahr P, Voth D, Schwarz M, Schmitt HJ. CSF shunt infections in children. Infection. 1993;21(2):89–92.
Mancao M, Miller C, Cochrane B, Hoff C, Sauter K, Weber E. Cerebrospinal fluid shunt infections in infants and children in Mobile. Ala Acta Paediatr. 1998;87(6):667–70.
McGirt MJ, Zaas A, Fuchs HE, George TM, Kaye K, Sexton DJ. Risk factors for pediatric ventriculoperitoneal shunt infection and predictors of infectious pathogens. Clin Infect Dis. 2003;36(7):858–62. doi:10.1086/368191.
Wang KW, Chang WN, Shih TY, Huang CR, Tsai NW, Chang CS, et al. Infection of cerebrospinal fluid shunts: causative pathogens, clinical features, and outcomes. Jpn J Infect Dis. 2004;57(2):44–8.
Brook I, Johnson N, Overturf GD, Wilkins J. Mixed bacterial meningitis: a complication of ventriculo- and lumboperitoneal shunts. J Neurosurg Pediatr. 1977;47(6):961–4. doi:10.3171/jns.1977.47.6.0961.
Schreffler RT, Schreffler AJ, Wittler RR. Treatment of cerebrospinal fluid shunt infections: a decision analysis. Pediatr Infect Dis J. 2002;21(7):632–6. doi:10.1097/01.inf.0000020964.43766.35.
James HE, Walsh JW, Wilson HD, Connor JD, Bean JR, Tibbs PA. Prospective randomized study of therapy in cerebrospinal fluid shunt infection. Neurosurgery. 1980;7(5):459–63.
Whitehead WE, Kestle JR. The treatment of cerebrospinal fluid shunt infections. Results from a practice survey of the American Society of Pediatric Neurosurgeons. Pediatr Neurosurg. 2001;35(4):205–10.
Tuli S, Tuli J, Drake J, Spears J. Predictors of death in pediatric patients requiring cerebrospinal fluid shunts. J Neurosurg. 2004;100(5 Suppl Pediatrics):442–6. doi:10.3171/ped.2004.100.5.0442.
Tunkel ARD, James M. Cerebrospinal fluid shunt infections. Mandell, Douglas, and Bennett’s principles and practice of infectious diseases. 7th ed. Philidelphia: Elsevier; 2010. p. 1231–6.
Chapman PH, Borges LF. Shunt infections: prevention and treatment. Clin Neurosurg. 1985;32:652–64.
Wong GK, Poon WS, Wai S, Yu LM, Lyon D, Lam JM. Failure of regular external ventricular drain exchange to reduce cerebrospinal fluid infection: result of a randomised controlled trial. J Neurol Neurosurg Psychiatry. 2002;73(6):759–61.
Arnell K, Enblad P, Wester T, Sjolin J. Treatment of cerebrospinal fluid shunt infections in children using systemic and intraventricular antibiotic therapy in combination with externalization of the ventricular catheter: efficacy in 34 consecutively treated infections. J Neurosurg. 2007;107(3 Suppl):213–9. doi:10.3171/PED-07/09/213.
James HE, Bradley JS. Aggressive management of shunt infection: combined intravenous and intraventricular antibiotic therapy for twelve or less days. Pediatr Neurosurg. 2008;44(2):104–11. doi:10.1159/000113111.
McCracken Jr GH, Mize SG, Threlkeld N. Intraventricular gentamicin therapy in gram-negative bacillary meningitis of infancy. Report of the Second Neonatal Meningitis Cooperative Study Group. Lancet. 1980;1(8172):787–91.
Mustafa MM, Mertsola J, Ramilo O, Saez-Llorens X, Risser RC, McCracken Jr GH. Increased endotoxin and interleukin-1 beta concentrations in cerebrospinal fluid of infants with coliform meningitis and ventriculitis associated with intraventricular gentamicin therapy. J Infect Dis. 1989;160(5):891–5.
Brozanski BS, Scher MS, Albright AL. Intraventricular nafcillin-induced seizures in a neonate. Pediatr Neurol. 1988;4(3):188–90.
Manzella JP, Paul RL, Butler IL. CNS toxicity associated with intraventricular injection of cefazolin. Report of three cases. J Neurosurg. 1988;68(6):970–1. doi:10.3171/jns.1988.68.6.0970.
James HE, Bradley JS. Management of complicated shunt infections: a clinical report. J Neurosurg Pediatr. 2008;1(3):223–8. doi:10.3171/PED/2008/1/3/223.
Brook I. Meningitis and shunt infection caused by anaerobic bacteria in children. Pediatr Neurol. 2002;26(2):99–105.
Arnell K, Cesarini K, Lagerqvist-Widh A, Wester T, Sjolin J. Cerebrospinal fluid shunt infections in children over a 13-year period: anaerobic cultures and comparison of clinical signs of infection with Propionibacterium acnes and with other bacteria. J Neurosurg Pediatr. 2008;1(5):366–72. doi:10.3171/PED/2008/1/5/366.
Desai A, Lollis SS, Missios S, Radwan T, Zuaro DE, Schwarzman JD, et al. How long should cerebrospinal fluid cultures be held to detect shunt infections? J Neurosurg Pediatr. 2009;4(2):184–9. doi:10.3171/2009.4.PEDS08279. Clinical article.
Montero A, Romero J, Vargas JA, Regueiro CA, Sanchez-Aloz G, De Prados F, et al. Candida infection of cerebrospinal fluid shunt devices: report of two cases and review of the literature. Acta Neurochir (Wien). 2000;142(1):67–74.
Banks JT, Bharara S, Tubbs RS, Wolff CL, Gillespie GY, Markert JM, et al. Polymerase chain reaction for the rapid detection of cerebrospinal fluid shunt or ventriculostomy infections. Neurosurgery. 2005;57(6):1237–43. discussion −43.
Simon TD, Pope CE, Browd SR, Ojemann JG, Riva-Cambrin J, Mayer-Hamblett N, et al. Evaluation of microbial bacterial and fungal diversity in cerebrospinal fluid shunt infection. PLoS One. 2014;9(1):e83229. doi:10.1371/journal.pone.0083229. A small study using 16s PCR to evaluate the complex microbiotia associated with shunt infections.
Yilmaz A, Dalgic N, Musluman M, Sancar M, Colak I, Aydin Y. Linezolid treatment of shunt-related cerebrospinal fluid infections in children. J Neurosurg Pediatr. 2010;5(5):443–8. doi:10.3171/2009.12.PEDS09421.
Rehman AU, Rehman TU, Bashir HH, Gupta V. A simple method to reduce infection of ventriculoperitoneal shunts. J Neurosurg Pediatr. 2010;5(6):569–72. doi:10.3171/2010.2.PEDS09151.
Kestle JR, Riva-Cambrin J, Wellons 3rd JC, Kulkarni AV, Whitehead WE, Walker ML, et al. A standardized protocol to reduce cerebrospinal fluid shunt infection: the Hydrocephalus Clinical Research Network Quality Improvement Initiative. J Neurosurg Pediatr. 2011;8(1):22–9. doi:10.3171/2011.4.PEDS10551. This multi-center study demonstrated the value of a standardized protocol for CSF shunt placement in reducing infection rates.
Winston KR, Ho JT, Dolan SA. Recurrent cerebrospinal fluid shunt infection and the efficacy of reusing infected ventricular entry sites. J Neurosurg Pediatr. 2013;11(6):635–42. doi:10.3171/2013.3.PEDS12478.
Keong NC, Bulters DO, Richards HK, Farrington M, Sparrow OC, Pickard JD et al. The SILVER (Silver Impregnated Line Versus EVD Randomized trial): a double-blind, prospective, randomized, controlled trial of an intervention to reduce the rate of external ventricular drain infection. Neurosurgery. 2012;71(2):394–403; discussion−4. doi:10.1227/NEU.0b013e318257bebb. One of few prospective, randomized studies of antimicrobial-impregnated catheters, this study demonstrated a reduced rate of EVD infection in the group receiving silver-impregnated EVDs.
Govender ST, Nathoo N, van Dellen JR. Evaluation of an antibiotic-impregnated shunt system for the treatment of hydrocephalus. J Neurosurg Pediatr. 2003;99(5):831–9. doi:10.3171/jns.2003.99.5.0831.
Demetriades AK, Bassi S. Antibiotic resistant infections with antibiotic-impregnated Bactiseal catheters for ventriculoperitoneal shunts. Br J Neurosurg. 2011;25(6):671–3. doi:10.3109/02688697.2011.575478.
Rivero-Garvia M, Marquez-Rivas J, Jimenez-Mejias ME, Neth O, Rueda-Torres AB. Reduction in external ventricular drain infection rate. Impact of a minimal handling protocol and antibiotic-impregnated catheters. Acta Neurochir. 2011;153(3):647–51. doi:10.1007/s00701-010-0905-1.
Compliance with Ethics Guidelines
Conflict of Interest
Michael Rajnik and Daniel Adams declare no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by the author.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the Topical Collection on Pediatric Infectious Diseases
Rights and permissions
About this article
Cite this article
Adams, D.J., Rajnik, M. Microbiology and Treatment of Cerebrospinal Fluid Shunt Infections in Children. Curr Infect Dis Rep 16, 427 (2014). https://doi.org/10.1007/s11908-014-0427-8
Published:
DOI: https://doi.org/10.1007/s11908-014-0427-8