Abstract
Purpose of Review
Gastroesophageal neuroendocrine neoplasms (NENs) are a rare entity. Recent 2019 WHO classifications reflect our understanding of tumor biology, namely, that distinct molecular characteristics underline tumor behavior and prognosis. Here, we reviewed the evidence for linking molecular findings with the clinicopathological features and treatment of gastroesophageal NENs.
Recent Findings
Degree of differentiation and Ki-67 proliferation index are required for accurate classification of neuroendocrine tumors and carcinomas but not sufficient to distinguish between the two entities. Resection remains the mainstay treatment for early-stage gastroesophageal neuroendocrine tumors. Additional perioperative therapy may benefit mitotically active tumors. There is a role for somatostatin analogues, especially in the setting of metastatic and symptomatic disease. New radiolabeled somatostatin analogues, immunotherapy, and embolization offer multimodality treatments for distant metastases.
Summary
We need to understand the specific underlying biology of the various subtypes of gastroesophageal NENs to provide tailored treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over 70% of all neuroendocrine neoplasms (NENs) are found in the digestive system. The stomach and esophagus are among the least common locations for NENs with incidence of 10% and < 1% at each site, respectively [1, 2].
Updated retrospective, population-based Surveillance, Epidemiology, and End Results (SEER) data reveal an increasing incidence of NENs at all gastrointestinal sites with an annual percentage rate change of over 5% between 1986 and 2015 [3]. Gastric NENs have had an overall 15-fold increase from 1973 to 2012, while esophageal NENs are too rare to be adequately analyzed. This increased incidence may be due to use of endoscopy and discovery of early-stage tumors, with improved imaging. Survival of patients with advanced staged tumors has also improved [4].
The 5th edition of the WHO classification, formulated in 2019, represents a significant improvement in clinicopathologic classification over the previous 2010 edition [5•].
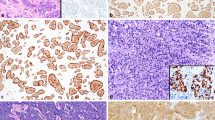
The updated definition includes separation of NENs into three distinct entities: neuroendocrine tumors (NETs), neuroendocrine carcinomas (NECs), and mixed neuroendocrine–non-neuroendocrine neoplasms (MINENs). There is an increased understanding of the interaction between histologic grade, tumor type, and molecular signature. It is now clear that Ki-67 proliferation index alone cannot be used to distinguish NETs from the more aggressive NECs.
The current WHO classification system uses replicative activity (Ki-67/mitotic rate) to assign grade (ranging from 1 to 3), with mitotic rates defined as < 2, 2–20, and > 20 mitoses/2 mm2 and Ki-67 indices defined as < 2%, 3–20%, and > 20%, respectively. The combination of grade and level of differentiation in the current system more clearly correlates with biologic behavior and outcomes.
Pathophysiology
Gastric NENs
Gastric NENs are thought to arise from neuroendocrine cell precursors, including enterochromaffin-like (ECL) cells found in the gastric fundus and antral D cells and G cells [1]. Each of these three precursor cells can give rise to characteristic types of NENs, which express and/or secrete histamine, somatostatin, and gastrin, respectively. A fourth precursor subtype, which expresses serotonin, is found throughout the gastric mucosa.
Normal ECL cells express gastrin receptors, which secrete histamine once activated. Histamine then stimulates acid secretion by parietal cells. Gastrin promotes the growth of ECL cells by interaction with a CCK2/gastrin receptor. Persistent gastrin stimulation can induce ECL cell hyperplasia as well as potentially lead to the development of dysplasia and ultimately to the formation of NENs. There has been interest in targeting this process with the orphan drug netazepide, a CCK2/gastrin receptor antagonist [6].
Some reports suggest medications that increase gastrin levels, such as proton pump inhibitors, may contribute to the risk of developing NENs, depending on chronicity of use, exposure, and both genetic/comorbid background determinants [7, 8]. The existence of familial G cell NETs associated with ATP4Ap.R703C mutation or the known autoimmune derangements present in atrophic gastritis are examples of other factors involved in the development of NENs [9]. A retrospective case-control study of more than 740 patients also suggests that both diabetes and a family history of cancer (non-NEN) are risk factors in women for the development of gastric NENs [10].
Gastric NENs have historically been “typed” according to clinicopathologic characteristics. Type I and type II gastric NETs are both associated with elevated gastrin levels [11]. Type I gastric NETs represent approximately 80% of all gastric NETs and are associated with chronic atrophic gastritis, which lead to a progressive decrease in gastrin acid production driving a negative feedback loop resulting in hypergastrinemia. Type II gastric NETs occur in association with G cell neoplasia or the presence of an ectopic gastrinoma—a tumor found as part of multiple endocrine neoplasia (MEN) type 1 or Zollinger-Ellison syndrome. A distinguishing clinical feature that separates these different mechanisms of hypergastrinemia is type I gastric NETs present with high gastric pH > 4, while type II have low gastric pH < 2. Most type I and type II gastric NETs are multifocal, relatively small tumors found throughout the gastric mucosa at sites corresponding to their precursor subtype. Type I and II NETs are usually either low or intermediate grade (G1 or G2) and typically behave in an indolent manner.
Type III gastric NETs have only been clearly defined by the WHO as a subgroup recently but remain a mystery. These tumors are typically sporadic, larger, and solitary with an unclear precursor and are not associated with hypergastrinemia. Most importantly, by WHO definitions, these are well differentiated but mitotically active G3 tumors. While only accounting for 20% of gastric NETs, they are commonly aggressive tumors with metastatic disease in up to 65% of cases at diagnosis.
NECs are a different entity from NETs and are uncommon in the stomach. Previously recognized as the most aggressive of NENs, the underlying reasons for this are now being elucidated. For example, mutations in MEN1, DAXX, and ATRX characterize pancreatic NETs of all grades, whereas pancreatic NECs usually have TP53 or RB1 mutations. NECs are all WHO G3 tumors and are distinguished by a poorly differentiated phenotype. Most of the time, they can be separated into large and small cell subtypes. Necrosis is significant and represents a diagnostic hallmark of NECs [5•].
Esophageal NENs
Esophageal NENs are most commonly located in the middle and lower esophagus [12•]. They are often associated with Barrett’s mucosa. More than 90% of esophageal NENs are NECs and present as large, bulky infiltrative tumors. Esophageal NECs represent approximately 2% of all esophageal cancers in Western populations, with a likely higher incidence in Asia. Amine precursor uptake and decarboxylase (APUD) and Merkel cells are thought to be the progenitors cells due to location [2]. In contrast, esophageal NETs are usually small submucosal lesions.
Gastroesophageal Mixed Neuroendocrine–Non-neuroendocrine Neoplasms (MINENs)
MINENs are a new entity defined by the WHO as a result of molecular and genomic profiling that have better delineated NECs from NETs. This term replaces the previous entity mixed adenoneuroendocrine carcinomas (MANECs). The new terminology reflects the many different permutations that this very rare tumor group may express, including mixtures of low/low, high/low, or high/high grade components of epithelial, glandular, and neuroendocrine types.
The appendix is the most common site of origin, representing 60% of all digestive system MINENs, while gastroesophageal MINENs comprise 12% [13]. Gastric MINENs may account for up to 25% of all gastric NEN and are admixtures of classic or mucinous adenocarcinoma with areas of NET or NEC. In a study of 88 patients with MINENs, even a 10% NEC component in a gastric adenocarcinoma rendered the clinical course significantly worse and akin to that of a “pure” NEC or gastric adenocarcinoma without NEC [14].
The true incidence of esophageal MINENs is difficult to quantify. These tumors may be mistakenly classified as adenocarcinomas (AC) or squamous cell carcinomas (SCC) with “neuroendocrine features.” Molecular studies have shown that in true MINENs, the adenocarcinoma and neuroendocrine components, usually NEC, share similar genomic abnormalities suggestive of a common progenitor. In fact, the existence of so-called “amphicrine” tumors with AC, SCC, and neuroendocrine components intermixed at a cellular level is most indicative of a single cell of origin whose progeny subsequently took different developmental pathways [15].
Staging
Both the American Joint Committee on Cancer (AJCC) and the European Neuroendocrine Tumor Society (ENETS) staging systems can be used for gastroesophageal NENs. The AJCC system is TNM-based and evaluates surgical resectability. As surgery is the mainstay for curative treatment, the AJCC system is used to estimate prognosis. Locally advanced disease, along with nodal and metastatic involvement, is associated with worse outcome [16]. Even though the 8th AJCC edition now incorporates grade by separating NET and NEC staging systems, it does not catch the emerging prognostic differences of various grades of NET nor does it address MINENs.
Given the unique biology of intermediate and high-grade NETs, there is growing interest in improving predictive models to reflect the relatively good long-term prognosis, even in stage IV disease. In an ideal model, the strongest prognostic staging would be one with both TMN and grade staging. Several nomograms have been published and seem to improve prognostic ability compared with classic systems [17••].
Treatment
Localized Disease
Gastric NENs
Resection, whether endoscopic or surgical, is the mainstay management of localized NETs, irrespective of site of origin (Table 1). Resection options for gastric NENs include endoscopic removal, wedge or local resection, or formal gastrectomy. Extent of lymphadenectomy differs by TNM stage, and grade should also be considered. However, in the setting of surgical resection, lymphadenectomy should be strongly considered specially to improve tumor staging. Antrectomy with surveillance has been advocated for some type I NETs given their reliance on elevated gastrin levels. Removal of antral G-cells can lead to normalization of serum gastrin levels and regression of some tumors; however, some ECL cells may become autonomous. Of note, type III gastric carcinoids have historically been treated with formal resection and lymphadenectomy; however, there are data to suggest that endoscopic or wedge resection may be adequate for low-grade tumors less than 2 cm without invasive features or poor differentiation [18, 19].
Endoscopic treatment is a valid approach for small G1 tumors, whether type I or II, but requires surveillance and observation at least every 2 years with resection of gastrinoma to address the underlying hypergastrinemia if feasible [20].
In a recent large retrospective review by the US-NETSG of 76 patients with gastric NENs treated between 2000 and 2016, tumor biology, rather than extent of resection, was the primary driver of prognosis. Most patients had type I and III NETs [21••]. Overall survival was significantly worse in those undergoing gastrectomy compared with local resection. Though not explicitly detailed, there could be a poor risk benefit ratio to performing gastrectomy for G1 NETs given the perioperative morbidity of a more extensive operation. Though type I tumors had the highest proportion of R0 resection, prognosis did not seem to be affected, again underscoring how biology rather than surgical margins governs outcomes.
The role of systemic therapy in localized NETs is unclear. G1 and G2 NETs are rarely treated with systemic therapy given their excellent prognosis with resection, though they have a propensity to recur and can metastasize as well. Somatostatin receptor–targeted therapy (SSRT), such octreotide or lanreotide, is used mainly to control the manifestations of hormonal excess in secretory NETs. Despite new data suggesting antiproliferative effects of these agents in the metastatic setting, they have not been studied perioperatively for surgically resectable disease. G3 NETs, as a relatively newly defined entity, have little data to suggest a standard treatment. Given a worse prognosis, more aggressive behavior, and higher proliferative index and metastatic potential, perioperative systemic therapy is usually considered.
The role of perioperative chemotherapy in gastric NECs is controversial despite the poor prognosis of these tumors. According to our 2018 National Cancer Database (NCDB) analysis, resection (either surgical or endoscopic) offers a survival advantage in poorly differentiated gastroesophageal tumors both in localized and metastatic disease (in metastatic disease, median survival 6.0 vs. 14.6 months, p < 0.001) [22••]. The addition of adjuvant chemotherapy and radiation did not appear to have any additive benefit (p = 0.39).
In gastric MINEN (mostly mixed adenoneuroendocrine carcinoma—high grade), a recent study of 69 patients found that neoadjuvant chemotherapy afforded improved overall survival compared with up-front surgery (p = 0.032) [23].
Esophageal NENs
While most esophageal NENs are high grade, the treatment—partial or total esophagectomy—is a highly morbid procedure. A recent large retrospective series using NCDB reviewed esophageal NENs from 2006 to 2014 and found that over 50% of patients had stage III disease [24]. This reflects the fact that an overwhelming majority of esophageal NENs are NECs, which have a high rate of lymph node and distant metastases. The most common pathology identified (44%) was “small cell.” There was clear recurrence-free and overall survival benefit with surgery for G1/G2 tumors in both stage I and II diseases. However, the data were not as robust for G3 tumors, especially in multivariate analysis (HR 0.78 (0.49–1.25); p = 0.303) [25, 26]. It is possible that G3 NETs and NECs may have been grouped together, which would explain the lack of benefit of resection for G3 tumors. The results may reflect that clinicians are correctly considering tumor biology when choosing surgery for NENs, with 81% of G1/G2 vs. 32% of G3 NENs undergoing resection.
Despite retrospective database analyses that suggest lack of benefit with perioperative therapy for gastroesophageal NECs, careful patient selection may allow some patients to benefit from a multimodality approach. In a subset of esophageal NECs that fulfilled the criteria of being both surgically resectable and having “limited disease,” surgery with or without adjuvant therapy showed a remarkably improved outcome in stage I and II compared with stage III esophageal NECs (median survival time 31.1 and 12.7 months, p < 0.001). These latter tumors were defined as “surgery nonresponse” and also did not benefit from adjuvant therapy, while the “surgery response” tumors did [27]. In a recent review of NECs from France, within which a small subset (16%) were gastroesophageal NECs, the overall and disease-free survival of the whole population with perioperative therapy (either neoadjuvant or adjuvant) were 24 and 9 months, respectively, suggesting improved outcomes with the addition of systemic therapy. Perioperative therapy consisted of a platinum-combination in the majority, with some cases being treated with capecitabine and radiation [28].
Another treatment approach for esophageal NECs is a combination of systemic and locoregional radiation therapy, most often delivered as concurrent or sequential chemoradiation. It has been shown that adding systemic therapy to local therapy improves outcomes. A retrospective study from Japan examined the outcomes of chemoradiation with cisplatin-based therapy in 23 patients with locally advanced esophageal NEC [29]. The overall response rate and clinical complete remission rate in all patients was 86.4% and 77.3%, respectively. The median progression-free survival and overall survival in all patients was 12.7 and 37.5 months, respectively, associated with a 5-year survival rate of 45.4%.
With respect to gastroesophageal MINEN, a Dutch retrospective analysis used PALGA, the Dutch national pathology registry and found that diagnosis remains a key problem in the management of mixed tumors [30]. Localized esophageal and gastric tumors were misdiagnosed on endoscopic biopsies in nearly 50% of cases. After resection, long-term survival was achieved in almost 40% of patients with neoadjuvant therapy. Therapy for MINENs remains an area of active interest with the goal of determining which component of these tumors needs to be targeted.
Distant Metastatic Disease
Though considered indolent tumors, even well-differentiated NENs can metastasize over time. Several locoregional treatment options exist for metastatic NENs depending on the site and the organs involved.
Most commonly, stage IV NETs are treated with endocrine suppression with somatostatin receptor–targeted therapy (SSRT), such as octreotide or its derivatives, which have been shown to improve disease-free survival in inoperable or metastatic NENs originating at non-gastroesophageal sites in the large PROMID and CLARINET studies [31,32,33]. At present, it is reasonable to extrapolate these results and adopt the use of long-acting octreotide or lanreotide in all G1 and G2, stage IV disease given similarities in histopathologic characteristics across NENs. Even G3 NET may benefit from SSRT. In a study, which included a few gastric NETs, median progression-free and overall survival were 9.6 and 19.9 months, respectively, and outcomes were even better in the setting of non-FDG avid disease [34]. Approximately 20% of G3 NETs in this study fit into this latter category, which is surprising given the high proliferative index of these tumors. The role of these analogues in MINENs is unknown. Given the dependency of SSRTs on receptor expression, it is unknown what role these analogues may have for NECs.
Multiple studies have shown that surgery can be beneficial in metastatic NETs.
In the largest series examining resection of the primary tumor alone in stage IV gastroesophageal and pancreatic NETs, overall survival was significantly higher after primary tumor resection irrespective of primary organ site or resectability of distant disease (21.2 months vs. 7.0 months for gastric subset, p < .001) [35•]. This suggests an abscopal oncologic effect of primary tumor resection.
In addition, liver transplant has been explored at several centers across the world with encouraging results. In a European liver transplant registry series of 213 cases of all types of NETs, reporting on outcomes over a 27-year period, 3-month postoperative mortality was 10%, while 5-year postoperative overall and disease-free survival were 52% and 30%, respectively [36]. Due to advances in transplant medicine and surgical techniques, as well as appropriate patient selection via the Milan-NETLM criteria, outcomes with NET liver metastasis have improved significantly [37]. A recent case series of 15 patients, including 1 gastric NET, estimated 1- and 5-year recurrence-free rates posttransplant to be 80% and 43%, respectively [38].
Embolization therapies including bland embolization, transarterial chemoembolization (TACE), and radioembolization (TARE) are newer techniques that improve disease control and progression-free survival in stage IV NETs with liver-only metastases by exploiting the hypervascular nature of these lesions. Guidelines support the use of these locoregional interventional approaches for control of liver metastases [39]. In a recent case series, both TACE and TARE were found to have comparable efficacy; however, there are no randomized data available so far to determine which modality is superior or to quantify the improvement in survival compared with systemic therapy alone. The RETNET trial, which attempts to compare locoregional therapies, exclusive of TARE, is an ongoing prospective trial [40, 41].
Radiolabeled SSRT or peptide receptor radionuclide therapy (PRRT), as 90Y-DOTATOC or 177Lu-Dotatate (Lutathera), uses therapeutic radionuclides that bind to tissues harboring somatostatin receptors and has been recently approved in the USA as therapy for malignant disease detectable by somatostatin receptor–based imaging techniques irrespective of site of origin. The NETTER-1 study, which lacked gastroesophageal NETs, showed improved progression-free survival and quality of life in metastatic NET using 177Lu-Dotatate, compared with high-dose long-acting octreotide alone [42].
Combination therapy has also shown efficacy. Surgery with SSRT may have additive benefits. In a series of 104 patients, SSRT and surgical resection in combination therapy was superior to both surgery and SSRT alone (10-year survival 60.6% vs. 51.8% surgery alone vs. 36.0% receiving SSRT alone (p < 0.0001)) [43]. Aggressive therapy with TARE following PPRT also appears feasible and efficacious in metastatic NETs, achieving over 90% disease control with tolerable toxicity despite over 50% grade 3–4 lymphopenia and elevation in liver enzymes [44].
Systemic therapies, such as cytotoxic chemotherapy or targeted molecular inhibitors, can be used in unresectable stage IV NETs with variable improvement in progression-free and overall survival. Platinum-based therapies are preferred for NECs. Most of these regimens have not been specifically evaluated for gastroesophageal NENs. For example, in the RADIANT-4 study evaluating everolimus in metastatic NETs, only 3% of tumors originated in the stomach, and none were recorded to be from esophageal origin.
Perhaps the most promising current treatment class is that of immunotherapy. Little is known about the immune response in NENs. There is immunohistochemical expression of the immunosuppressive molecule PDL1 in gastric NENs, and higher expression is correlated with worse outcome [45, 46]. This suggests that the PDL1/PD1 immune pathway may play a role in gastric NEN and checkpoint blockade therapy may be beneficial. A recent report from the ongoing SWOG 1609-DART basket study has been very encouraging in this regard [47]. The combination of checkpoint inhibitors ipilimumab plus nivolumab demonstrated a 44% overall response rate in patients with non-pancreatic NECs.
Prognosis
Type I/II G1 gastric NETs are often multifocal and indolent. G2 tumors can recur locally with approximately 5% incidence of lymph node and distant metastatic involvement. Type III gastric NETs show a higher incidence of locoregional nodal involvement and distant metastases, up to one quarter and one sixth of cases, respectively. Ki67 has been considered an important prognostic marker for GI NENs [48•]. In a series of gastric NET, however, the tumor type (I vs. III) and size (> 10 mm) were shown to be predictive of prognosis [49•]. This suggests that other biologic variables underlying NETs may drive their clinical course.
In a retrospectively analyzed case series of 119 Korean patients with gastric NETs or NECs, gastric NECs had a worse prognosis than the general population of gastric cancer patients [50]. Gastric NEC mirrors the biologic behavior of signet cell ring carcinoma, one of the most aggressive subtypes of epithelial gastric cancer. Interestingly, prognosis was worse even in early T1 or T2 staged tumors.
Esophageal NENs are larger and more aggressive tumors, with more local, nodal, and distant metastases, consistent with increased incidence of higher-grade NEC subtype [22••]. In a retrospective analysis of 802 patients with esophageal NEN, 97% of cases were NECs with a 68% male predominance [51]. Only 11% of patients with NEN underwent surgery, and almost 70% had perioperative therapy. Tumor > 4 cm and higher stages were associated with significantly worse overall survival, while esophagectomy and neoadjuvant therapy were predictors of better survival. The 5-year overall survival rate was 12% for all esophageal NEN, 89% for NET, and 9% for NEC. Compared with pancreatic NENs, esophageal NETs had improved overall survival, while NECs had a poorer survival.
The NORDIC-NEC study group showed that primary location significantly predicts survival in NECs, with survival of esophageal NECs being significantly worse than gastric NECs (OR 1.29 and 0.37, respectively) [48•]. Our own analysis of the NCDB interestingly showed that gastric NENs arising from the cardia have similar 5-year survival as esophageal NENs (11.2% vs. 9.8%), which was worse than non-cardia gastric NEN (22.8%) [22••]. This suggests that either gastric cardia NENs share similar biology as esophageal NENs or that surgical resection of the former is less effective compared with non-cardia NENs. In a retrospective multicenter study from China, gastroesophageal junction NENs have also been shown to be significantly larger, of higher grade, and with more distant metastasis than gastric NENs [52].
The prognosis of MINENs is intermediate between that of NECs and pure adenocarcinoma or squamous cell carcinoma of the esophagus; however, they have poorer prognosis than NETs. In the rare MINENs composed of NET (as opposed to NEC) and another subtype, it appears that prognosis is driven by the non-neuroendocrine component [53].
Conclusion
Our understanding of gastroesophageal NENs is evolving and is starting to be reflected in the updated 2019 WHO classifications. Further evaluation of various treatment strategies incorporating multimodality therapy with a focus on targeting underlying tumor biology is likely to improve disease outcomes.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Borch K, Ahren B, Ahlman H, Falkmer S, Granerus G, Grimelius L. Gastric carcinoids: biologic behavior and prognosis after differentiated treatment in relation to type. Ann Surg. 2005;242(1):64–73. https://doi.org/10.1097/01.sla.0000167862.52309.7d.
Deng HY, Ni PZ, Wang YC, Wang WP, Chen LQ. Neuroendocrine carcinoma of the esophagus: clinical characteristics and prognostic evaluation of 49 cases with surgical resection. J Thorac Dis. 2016;8(6):1250–6. https://doi.org/10.21037/jtd.2016.04.21.
Zheng Z, Chen C, Jiang L, Zhou X, Dai X, Song Y, et al. Incidence and risk factors of gastrointestinal neuroendocrine neoplasm metastasis in liver, lung, bone, and brain: a population-based study. Cancer medicine. 2019;8(17):7288–98.
Dasari A, Shen C, Halperin D, Zhao B, Zhou S, Xu Y, et al. Trends in the incidence, prevalence, and survival outcomes in patients with neuroendocrine tumors in the United States. JAMA Oncol. 2017;3(10):1335–42. https://doi.org/10.1001/jamaoncol.2017.0589.
• Nagtegaal ID, Odze RD, Klimstra D, Paradis V, Rugge M, Schirmacher P, et al. The 2019 WHO classification of tumours of the digestive system. Histopathology. 2020;76(2):182–8 New 2019 WHO classifications distinguishes between well differentiated NETs and poorly differentiated NECs in all sites based on molecular differences. Mixed NENs are now grouped as MINENs.
Boyce M, Moore AR, Sagatun L, Parsons BN, Varro A, Campbell F, et al. Netazepide, a gastrin/cholecystokinin-2 receptor antagonist, can eradicate gastric neuroendocrine tumours in patients with autoimmune chronic atrophic gastritis. Br J Clin Pharmacol. 2017;83(3):466–75. https://doi.org/10.1111/bcp.13146.
McCarthy DM. Proton pump inhibitor use, hypergastrinemia, and gastric carcinoids—what is the relationship? Int J Mol Sci. 2020;21(2):662.
Tatsuguchi A, Hoshino S, Kawami N, Gudis K, Iwakiri K. Sa1200–Hypergastrinemia secondary to long-term proton pump inhibitor treatment does not cause neuroendocrine tumor in stomach. Gastroenterology. 2019;156(6):S-305.
Benítez J, Marra R, Reyes J, Calvete O. A genetic origin for acid–base imbalance triggers the mitochondrial damage that explains the autoimmune response and drives to gastric neuroendocrine tumours. Gastric Cancer. 2020;23(1):52–63.
Hassan MM, Phan A, Li D, Dagohoy CG, Leary C, Yao JC. Risk factors associated with neuroendocrine tumors: a US-based case–control study. Int J Cancer. 2008;123(4):867–73.
Assarzadegan N, Montgomery E. What is new in 2019 World Health Organization (WHO) classification of tumors of the digestive system: review of selected updates on neuroendocrine neoplasms, appendiceal tumors, and molecular testing. Arch Pathol Lab Med. 2020.
• Ye L, Lu H, Wu L, Zhang L, Shi H, Wu HM, et al. The clinicopathologic features and prognosis of esophageal neuroendocrine carcinomas: a single-center study of 53 resection cases. BMC Cancer. 2019;19(1):1234. https://doi.org/10.1186/s12885-019-6420-8Pure esophageal NEC have worse prognosis compared to esophageal MINEN.
de Mestier L, Cros J, Neuzillet C, Hentic O, Egal A, Muller N, et al. Digestive system mixed neuroendocrine-non-neuroendocrine neoplasms. Neuroendocrinology. 2017;105(4):412–25.
Park JY, Ryu M-H, Park YS, Park HJ, Ryoo B-Y, Kim MG, et al. Prognostic significance of neuroendocrine components in gastric carcinomas. Eur J Cancer. 2014;50(16):2802–9.
La Rosa S, Sessa F, Uccella S. Mixed neuroendocrine-nonneuroendocrine neoplasms (MiNENs): unifying the concept of a heterogeneous group of neoplasms. Endocr Pathol. 2016;27(4):284–311.
Dolcetta-Capuzzo A, Villa V, Albarello L, Franchi GM, Gemma M, Scavini M, et al. Gastroenteric neuroendocrine neoplasms classification: comparison of prognostic models. Cancer. 2013;119(1):36–44. https://doi.org/10.1002/cncr.27716.
•• Hu P, Bai J, Liu M, Xue J, Chen T, Li R, et al. Trends of incidence and prognosis of gastric neuroendocrine neoplasms: a study based on SEER and our multicenter research. Gastric Cancer. 2020. https://doi.org/10.1007/s10120-020-01046-8Gastric NENs have increased in incidence since 1975. This study provides nomograms based on SEER data for 3- and 5- year survival for gastric NET and NEC.
Min BH, Hong M, Lee JH, Rhee PL, Sohn TS, Kim S, et al. Clinicopathological features and outcome of type 3 gastric neuroendocrine tumours. Br J Surg. 2018;105(11):1480–6. https://doi.org/10.1002/bjs.10901.
Saund MS, Al Natour RH, Sharma AM, Huang Q, Boosalis VA, Gold JS. Tumor size and depth predict rate of lymph node metastasis and utilization of lymph node sampling in surgically managed gastric carcinoids. Ann Surg Oncol. 2011;18(10):2826–32. https://doi.org/10.1245/s10434-011-1652-0.
Network NCC. NCCN clinical practice guidelines in oncology: neuroendocrine and adrenal tumors. Version 1.2019. 2019.
•• Crown A, Kennecke H, Kozarek R, Lopez-Aguiar AG, Dillhoff M, Beal EW, et al. Gastric carcinoids: does type of surgery or tumor affect survival? The American Journal of Surgery. 2019;217(5):937–42 Subtype of gastric NET has more impact on overall survival while type of surgery (formal gastrectomy v. local resection) does not change reoccurrence free survival.
•• Gray KD, Moore MD, Panjwani S, Elmously A, Afaneh C, Fahey TJ 3rd, et al. Predicting survival and response to treatment in gastroesophageal neuroendocrine tumors: an analysis of the National Cancer Database. Ann Surg Oncol. 2018;25(5):1418–24. https://doi.org/10.1245/s10434-018-6389-6Esophageal and gastric cardia NET have worse prognosis compared to gastric noncardia NET. No additional survival benefit with radiation or chemotherapy in poorly differentiated tumors.
Ma F, Wang B, Xue L, Kang W, Li Y, Li W, et al. Neoadjuvant chemotherapy improves the survival of patients with neuroendocrine carcinoma and mixed adenoneuroendocrine carcinoma of the stomach. J Cancer Res Clin Oncol. 2020:1–8.
Erdem S, Troxler E, Warschkow R, Tsai C, Yerokun B, Schmied B, et al. Is there a role for surgery in patients with neuroendocrine tumors of the esophagus? A contemporary view from the NCDB. Ann Surg Oncol. 2020;27(3):671–80.
Erdem S, Worni M. ASO author reflections: surgical resection of esophageal neuroendocrine tumors should be considered as an integral part of multimodal therapy in localized disease. Ann Surg Oncol. 2020;27(3):681–2.
Erdem S, Warschkow R, Worni M. Reply to the Editor:“Is There a Role of Surgery in Treating Localized Esophageal Neuroendocrine Tumor?”. Ann Surg Oncol. 2020;27(3):962.
Deng H-Y, Li G, Luo J, Li X-R, Alai G, Lin Y-D. The role of surgery in treating resectable limited disease of esophageal neuroendocrine carcinoma. World J Surg. 2018;42(8):2428–36.
Pellat A, Walter T, Augustin J, Hautefeuille V, Hentic O, Do Cao C, et al. Chemotherapy in resected neuroendocrine carcinomas of the digestive tract: a National Study from the French Group of Endocrine Tumours. Neuroendocrinology. 2020;110(5):404–12.
Honma Y, Nagashima K, Hirano H, Shoji H, Iwasa S, Takashima A, et al. Clinical outcomes of locally advanced esophageal neuroendocrine carcinoma treated with chemoradiotherapy. Cancer Med. 2019.
Van Der Veen A, Seesing M, Wijnhoven BP, Steur W, Henegouwen MI, Rosman C, et al. PS01. 202: Management of resectable esophageal and gastric (mixed adeno) neuroendocrine carcinoma: a nationwide cohort study. Diseases of the Esophagus. 2018;31(13).
Caplin ME, Pavel M, Cwikla JB, Phan AT, Raderer M, Sedlackova E, et al. Anti-tumour effects of lanreotide for pancreatic and intestinal neuroendocrine tumours: the CLARINET open-label extension study. Endocr Relat Cancer. 2016;23(3):191–9. https://doi.org/10.1530/ERC-15-0490.
Rinke A, Neary MP, Eriksson J, Hunger M, Doan T, Karli D, et al. Health-related quality of life for long-acting octreotide versus placebo in patients with metastatic midgut neuroendocrine tumors in the phase 3 PROMID trial. Neuroendocrinology. 2019;109(2):141–51. https://doi.org/10.1159/000499469.
Rinke A, Wittenberg M, Schade-Brittinger C, Aminossadati B, Ronicke E, Gress TM, et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors (PROMID): results of long-term survival. Neuroendocrinology. 2017;104(1):26–32. https://doi.org/10.1159/000443612.
Zhang J, Kulkarni HR, Singh A, Niepsch K, Müller D, Baum RP. Peptide receptor radionuclide therapy in grade 3 neuroendocrine neoplasms: safety and survival analysis in 69 patients. J Nucl Med. 2019;60(3):377–85.
• Tierney JF, Chivukula SV, Wang X, Pappas SG, Schadde E, Hertl M, et al. Resection of primary tumor may prolong survival in metastatic gastroenteropancreatic neuroendocrine tumors. Surgery. 2019;165(3):644–51. https://doi.org/10.1016/j.surg.2018.09.006Resection of primary tumors can improve surival in stage IV metastic gastroenteropancreatic NETs if they are low grade.
Le Treut YP, Gregoire E, Klempnauer J, Belghiti J, Jouve E, Lerut J, et al. Liver transplantation for neuroendocrine tumors in Europe-results and trends in patient selection: a 213-case European liver transplant registry study. Ann Surg. 2013;257(5):807–15. https://doi.org/10.1097/SLA.0b013e31828ee17c.
Mazzaferro V, Sposito C, Coppa J, Miceli R, Bhoori S, Bongini M, et al. The long-term benefit of liver transplantation for hepatic metastases from neuroendocrine tumors. Am J Transplant. 2016;16(10):2892–902. https://doi.org/10.1111/ajt.13831.
Korda D, Doros A, Piros L, Gerlei Z, Haboub-Sandil A, Mandli T, et al. Liver transplant for metastatic neuroendocrine tumors: a single-center experience in Hungary. Transplant Proc. 2019;51(4):1251–3. https://doi.org/10.1016/j.transproceed.2019.04.010.
Kennedy A, Bester L, Salem R, Sharma RA, Parks RW, Ruszniewski P, et al. Role of hepatic intra-arterial therapies in metastatic neuroendocrine tumours (NET): guidelines from the NET-liver-metastases consensus conference. HPB (Oxford). 2015;17(1):29–37. https://doi.org/10.1111/hpb.12326.
Egger ME, Armstrong E, Martin RC 2nd, Scoggins CR, Philips P, Shah M, et al. Transarterial chemoembolization vs radioembolization for neuroendocrine liver metastases: a multi-institutional analysis. J Am Coll Surg. 2020;230(4):363–70. https://doi.org/10.1016/j.jamcollsurg.2019.12.026.
Chen JX, Wileyto EP, Soulen MC. Randomized embolization trial for NeuroEndocrine tumor metastases to the liver (RETNET): study protocol for a randomized controlled trial. Trials. 2018;19(1):390. https://doi.org/10.1186/s13063-018-2782-5.
Strosberg J, El-Haddad G, Wolin E, Hendifar A, Yao J, Chasen B, et al. Phase 3 trial of (177)Lu-Dotatate for midgut neuroendocrine tumors. N Engl J Med. 2017;376(2):125–35. https://doi.org/10.1056/NEJMoa1607427.
Deutsch GB, Lee JH, Bilchik AJ. Long-term survival with long-acting somatostatin analogues plus aggressive cytoreductive surgery in patients with metastatic neuroendocrine carcinoma. J Am Coll Surg. 2015;221(1):26–36. https://doi.org/10.1016/j.jamcollsurg.2015.03.055.
Braat A, Ahmadzadehfar H, Kappadath SC, Stothers CL, Frilling A, Deroose CM, et al. Radioembolization with (90) Y resin microspheres of neuroendocrine liver metastases after initial peptide receptor radionuclide therapy. Cardiovasc Intervent Radiol. 2020;43(2):246–53. https://doi.org/10.1007/s00270-019-02350-2.
Yang MW, Fu XL, Jiang YS, Chen XJ, Tao LY, Yang JY, et al. Clinical significance of programmed death 1/programmed death ligand 1 pathway in gastric neuroendocrine carcinomas. World J Gastroenterol. 2019;25(14):1684–96. https://doi.org/10.3748/wjg.v25.i14.1684.
Wang C, Yu J, Fan Y, Ma K, Ning J, Hu Y, et al. The clinical significance of PD-L1/PD-1 expression in gastroenteropancreatic neuroendocrine neoplasia. Ann Clin Lab Sci. 2019;49(4):448–56.
Patel SP, Othus M, Chae YK, Giles FJ, Hansel DE, Singh PP, et al. A phase II basket trial of dual anti-CTLA-4 and anti-PD-1 blockade in rare tumors (DART SWOG 1609) in patients with non-pancreatic neuroendocrine tumors. Clin Cancer Res. 2020;26:2290–6.
• Sorbye H, Welin S, Langer SW, Vestermark LW, Holt N, Osterlund P, et al. Predictive and prognostic factors for treatment and survival in 305 patients with advanced gastrointestinal neuroendocrine carcinoma (WHO G3): the NORDIC NEC study. Ann Oncol. 2013;24(1):152–60. https://doi.org/10.1093/annonc/mds276Advanced GI NECs benefit from chemotherapy. Primary location predicts outcomes with gastric NECs having better prognosis than esophageal NECs.
• Panzuto F, Campana D, Massironi S, Faggiano A, Rinzivillo M, Lamberti G, et al. Tumour type and size are prognostic factors in gastric neuroendocrine neoplasia: a multicentre retrospective study. Dig Liver Dis. 2019;51(10):1456–60. https://doi.org/10.1016/j.dld.2019.04.016In gastric NENs, tumor subtype and size predict poor outcome whereas Ki67 does not.
Kim BS, Park YS, Yook JH, Kim B-S. Comparison of relapse-free survival in gastric neuroendocrine carcinoma (WHO grade 3) and gastric carcinoma. Ther Adv Gastroenterol. 2017;10(5):407–15.
Taherian M, Samankan S, Groman A, Yendamuri S, Bhalla A. Pathological prognostic factors for survival in neuroendocrine neoplasms of esophagus: results from the National Cancer Database. In: Laboratory Investigation; 2019: Nature Publishing Group 75 Varick St, 9th Flr, New York, Ny 10013–1917 Usa.
Zhang P, Wang W, Lu M, Zeng C, Chen J, Li E, et al. Clinicopathological features and outcome for neuroendocrine neoplasms of gastroesophageal junction: a population-based study. Cancer Med. 2018;7(9):4361–70. https://doi.org/10.1002/cam4.1702.
Frizziero M, Chakrabarty B, Nagy B, Lamarca A, Hubner RA, Valle JW, et al. Mixed neuroendocrine non-neuroendocrine neoplasms: a systematic review of a controversial and underestimated diagnosis. J Clin Med. 2020;9(1):273.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights
This article does not contain any studies with human or animal subject performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of Topical Collection on Stomach and Duodenum
Rights and permissions
About this article
Cite this article
Liu, M., Popa, E.C., Finnerty, B.M. et al. Clinicopathological Features of Gastroesophageal Neuroendocrine Neoplasms. Curr Gastroenterol Rep 22, 50 (2020). https://doi.org/10.1007/s11894-020-00788-w
Published:
DOI: https://doi.org/10.1007/s11894-020-00788-w