Abstract
Background
Esophageal neuroendocrine carcinoma (NEC) is a rare malignant tumor. The role of surgery in resectable limited disease of esophageal NEC remains unclear. How to select a specific group of limited disease of esophageal NEC who might benefit from surgery remains to be answered.
Methods
Patients undergoing esophagectomy for resectable limited disease of esophageal NEC in our department from January 2007 to June 2015 were analyzed. TNM staging system was applied to describe those patients, and according to their different long-term prognosis after surgery, those patients were subgrouped into surgery response limited disease (SRLD) group and surgery non-response limited disease (SNRLD) group. Both univariate and multivariate analyses were applied to identify potential prognostic factors.
Results
A total of 72 patients with resectable limited disease of esophageal NEC were identified for analysis. The median survival time of those patients was 21.5 months. There was no significant survival differences among stage I, stage IIA, and stage IIB patients, but all these patients had significantly longer survival than stage III patients. Therefore, stage I, stage IIA, and stage IIB patients were aggregated together as SRLD group, and stage III patients were aggregated as SNRLD group. SRLD patients obtained significantly longer survival than SNRLD patients in both univariate analysis and multivariate analysis. Moreover, adjuvant therapy could significantly benefit SRLD patients (P = 0.004) but could not benefit SNRLD patients (P = 0.136).
Conclusions
Different responses to surgery existed in resectable limited disease of esophageal NEC indicating the need of further subgrouping for those patients. The resectable limited disease of esophageal NEC could be further subgrouped into SRLD group and SNRLD group according to the TNM staging system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuroendocrine carcinoma (NEC), mainly consisting of small-cell carcinoma and large-cell carcinoma, is one kind of high-grade neuroendocrine neoplasms with poor differentiation [1]. It is characterized with a mitotic count of > 20 per 10 high power fields and/or a Ki-67 index > 20% [2]. Even though NEC was mainly found to arise from the gut and bronchopulmonary systems [3], NEC of the esophagus was extremely rare and poorly understood, as the incidence of esophageal NEC was reported to account for about 0.5–5.9% of all Chinese esophageal cancer patients and 1–2.8% in Western esophageal cancer patients [4]. Due to its rarity, there is no specific proposal staging system for esophageal NEC. However, in daily practice, the Veterans’ Administration Lung Study Group (VALSG) system, which is originally applied to primary small-cell lung cancer (SCLC), was widely adopted in staging esophageal NEC [5]. Depending on whether all known tumorous lesions locating in an anatomic region could be encompassed within a tolerable radiation field or not [6, 7], the VALSG staging system classified small-cell lung cancer only into two categories, namely the limited disease and extensive disease. However, esophageal NEC had different tumor behavior from SCLC [5], and even in SCLC, controversy still exists in the criteria for limited disease and extensive disease [8]. Up to date, the definition of limited disease stage of esophageal NEC was confusingly interpreted by various literatures. Some authors took it for granted that the limited disease of esophageal NEC equaled to resectable disease [9]. Although some authors have the consensus that limited disease of esophageal NEC also includes unresectable esophageal NEC, controversy still exists in to what extent the limited disease stage can invade out of the esophageal wall [10,11,12]: Some authors say that adjacent organ invasion can also be regarded as limited disease [10], while others believe that only peri-esophageal tissue invasion can be regarded as limited disease [12]. Therefore, it is not surprising that controversy exists in the role of surgery in treating limited disease of esophageal NEC. Accumulating evidence has supported the application of surgical resection as an effective treatment of esophageal NEC in limited disease stage of esophageal NEC [10, 13], but challenge to the role of surgery never stops [14]. Based upon literature reviews and our following clinical data, we found that limited disease of esophageal NEC includes both unresectable disease and resectable disease and that only a special portion of the resectable limited disease of esophageal NEC can benefit most from esophagectomy and we may call it “surgery response limited disease (SRLD).” In this report, we tried to use TNM staging system to subgroup the resectable limited disease of esophageal NEC and pick out that special portion of SRLD for the purpose of giving a preliminary description. To our knowledge, this is the first cohort study focusing on current topic with a relatively large sample size.
Patients and methods
We retrospectively reviewed and collected the data of patients with resectable limited disease of esophageal NEC who underwent esophagectomy with lymphadenectomy in our department from January 2007 to June 2015. Resectability was defined as: clinical T1-3, without regional lymph node metastasis or with regional lymph node metastasis but all lymph nodes were evaluated to be completely resectable on computed tomography scan. All those esophageal NEC patients were diagnosed pathologically and immunohistochemically according to the World Health Organization (WHO)’s diagnostic criteria [2]. Our study was approved by the Ethics Committee of West China Hospital, Sichuan University (No. 20161011). Since our study was a retrospective prognosis analysis and analyzed anonymously, the ethics committee waived the need for consent.
We collected the following data for analysis: demographic data, pathologic findings, TNM stage, adjuvant therapy, and survival time. The pathologic findings consisted of homology of the NEC, lymph node involvement, lymphovascular invasion, and tumor location. Tumor location was categorized into three parts according to the endoscopic findings: cervical/upper (15–25 cm from the incisor teeth), middle (25–30 cm), and lower (30–40 cm) segments of the esophagus. Those esophageal NEC patients were staged by both the VALSG system and the AJCC 2009 TNM staging system for ESCC. All patients were followed up every 3 months for the first 2 years, then every 6 months for the following 3 years, and annually thereafter. We conducted our last follow-up by telephone, outpatient department visit, or even visiting the patients’ home in October 2016 in order to minimize the rate of lost to follow-up as possible. Survival time was measured from the day of esophagectomy to the date of death or last follow-up.
Statistical analysis was performed by using SPSS 19.0 software (SPSS Corp, Chicago, IL, USA). Data were represented as the mean ± standard deviation for continuous variables or number (%) for categorical data. The survival time of all patients was calculated by the Kaplan–Meier analysis, and the log-rank test was used to estimate the association between eligible variables and survival time. The Cox’s hazard regression model was applied to explore the possible independent prognostic factors. A two-sided probability value of less than 0.05 was considered statistically significant.
Results
Patient characteristics
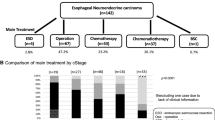
From January 2007 to June 2015, a total of 4275 patients undergoing esophagectomy with lymphadenectomy for esophageal cancer were registered in our database, seventy-two (72/4275: 1.7%) of which were resectable limited disease of esophageal NEC. Because those patients were preoperatively diagnosed as resectable disease (clinical stage I-III), none of them received any neoadjuvant therapy, and all of them were intended for radical esophagectomy with two-field lymphadenectomy. Because of the historical background of choosing left thoracotomy as a predominant approach for esophageal cancer in China, sixty-one patients underwent esophagectomy with two-field lymphadenectomy through the left thoracotomy, eight patients through Ivor-Lewis approach, and the other three patients through transhiatal approach. All those patients underwent R0 resection.
The baseline characteristics of those esophageal NEC patients are shown in Table 1. The mean age of those patients was 59.7 ± 8.3 years old (ranging from 42 to 76 years) with a male-to-female ratio of 3.2:1. The majority of the esophageal NEC was located in the middle (58.3%) and lower (33.3%) segment of esophagus. Pathologically, most of the esophageal NEC was found to be small-cell carcinoma (73.6%), and a quarter of the esophageal NEC were all mixed with ESCC. More than half of those patients (58.3%) were found to have positive lymph node metastasis, and eight patients were proved to have lymphovascular invasion. All those patients were staged as resectable limited disease. According to TNM stage system, fourteen patients were at stage I, nine patients at stage IIA, twenty patients at Stage IIB, and twenty-nine patients at stage III. There were only two patients suffering from major postoperative complications (one for severe pneumonia and another for anastomosis leakage). One patient died of esophagobronchial fistula within 30 days after surgery. Moreover, the rate of 90-day mortality was 4.2% for those patients. Patients with positive lymph node metastasis were all recommended for adjuvant therapy. Postoperatively, about half of those patients received adjuvant therapy (chemotherapy and/or radiotherapy), while several patients who were recommended for adjuvant therapy did not receive adjuvant therapy due to economic burdens or physical conditions.
Survival analysis and prognosis
Our last follow-up was conducted in October 2016 by telephone, outpatient department visit, or even patient visiting. After a median follow-up time of 54.8 months [95% confidence interval (CI) 52.4–57.2 months], fifty-one (70.8%) patients were decreased, while nineteen (26.4%) patients were still alive, but two (2.8%) patients were lost to follow-up. The median survival time of those patients was 21.5 months (95% CI 14.4–28.6 months), and the 1-, 3-, and 5-year survival rates for all those patients were 75.0, 33.4, and 28.4%, respectively (Fig. 1).
For prognostic analysis, the univariate analysis was initially applied. Patients with earlier TNM stage had significantly longer overall survival time than patients with relatively advanced stage disease (P = 0.001). Thanks to our large sample size, we were capable of comparing the survival between each pair of disease stages. Patients with stage I (P < 0.001), stage IIA (P = 0.021), and stage IIB (P = 0.039) diseases had significantly longer survival time than those with stage III, while there were no significant difference among patients with stage I, stage IIA, and stage IIB diseases (stage I vs. stage IIA: P = 0.716; stage I vs. stage IIB: P = 0.084; stage IIA vs. stage IIB: P = 0.485, Fig. 2a). Patients with negative lymph node metastasis also yielded significantly longer survival time than those with positive lymph node metastasis (median survival time 32.8 and 17.7 months, respectively; P = 0.008). Moreover, patients receiving adjuvant therapy obtained significantly longer overall survival than those without adjuvant therapy (median survival time 37.9 and 16.3 months, respectively; P = 0.001, Fig. 2b). Patients with mixed esophageal NEC tended to have longer survival time than those with pure esophageal NEC (median survival time 32.8 and 18.0 months, respectively; P = 0.106). However, there were no significant differences in survival time with regard to patients’ gender (P = 0.515), tumor location (P = 0.795), pathology type (P = 0.413), as well as lymphovascular invasion (P = 0.435) (shown in Table 2).
In the multivariate analysis, only TNM stage (P = 0.018) and adjuvant therapy (P = 0.002) were significant independent prognostic factors for overall survival (shown in Table 3). Patients with stage I [hazard ratio (HR) = 0.100; 95% CI 0.023–0.427; P = 0.002], stage IIA (HR = 0.230; 95% CI 0.056–0.941; P = 0.041), and stage IIB (HR = 0.387; 95% CI 0.168–0.895; P = 0.026) yielded significantly longer survival time than those with stage III (as a reference HR = 1). Moreover, adjuvant therapy significantly influenced the overall survival of esophageal NEC patients (HR = 0.326; 95% CI 0.159–0.668; P = 0.002).
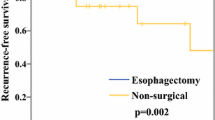
When stage I, stage IIA, and stage IIB patients were aggregated into the so-called SRLD group, these patients had significantly longer survival time than stage III patients, the so-called surgery non-response limited disease (SNRLD) group in univariate analysis (median survival time 31.1 and 12.7 months, respectively; P < 0.001, Fig. 3). Moreover, SRLD (HR = 0.385; 95% CI 0.164–0.906; P = 0.029) and adjuvant therapy (HR = 0.357; 95% CI 0.183–0.694; P = 0.002) were still found to be the only independent prognostic factors in the multivariate analysis. We further explored the role of adjuvant therapy in both SRLD and SNRLD patients. In SRLD group, patients receiving adjuvant therapy obtained significantly longer overall survival time than those without adjuvant therapy (median survival time 72.2 and 24.0 months, respectively; P = 0.004, Fig. 4a); While in SNRLD group, adjuvant therapy did not significantly increase the overall survival time (median survival time 18.0 and 12.5 months, respectively; P = 0.136, Fig. 4b).
Kaplan–Meier curves of the overall survival of esophageal neuroendocrine carcinoma patients stratified by TNM stage (P < 0.001). Note stage I, stage IIA, and stage IIB patients were aggregated as surgery response limited disease (SRLD), while stage III patients were called as surgery non-response limited disease (SNRLD)
Kaplan–Meier curves of the overall survival of esophageal neuroendocrine carcinoma patients with different TNM stage stratified by adjuvant therapy. a In patients with SRLD (P = 0.004); b in patients with SNRLD (P = 0.136). Note stage I, stage IIA, and stage IIB patients were aggregated as surgery response limited disease (SRLD), while stage III patients were called as surgery non-response limited disease (SNRLD)
Discussion
Esophageal NEC was an extremely rare type of malignant tumor originated from esophagus, which was reported to account for about 0.5–5.9% of all esophageal cancers [4]. Patients with esophageal NEC have an extremely poor prognosis, because the median survival time of those patients was reported to be about 8.0–28.5 months [4, 15,16,17,18,19]. Due to its rarity, the optimal therapeutic choices for esophageal NEC were not well established yet. For the convenience of therapeutic choices, the VALSG staging system, which was initially applied for SCLC, was applied to divided esophageal NEC roughly into limited disease and extensive disease [5]. However, the role of surgery in limited disease of esophageal NEC remained controversial [14], for the fact that the definition of limited disease in VALSG system was confusing in clinical practice. Our previous study proved that the 2009 AJCC TNM staging system for ESCC could also be applied to describe esophageal NEC [20], but how to select the unique subgroup of SRLD in resectable limited disease of esophageal NEC who can benefit most from surgery remains to be answered. Here in this report, we aimed to use TNM staging system to give a preliminary description of this unique subgroup. To our knowledge, this is the first study focusing on this topic with a relatively large sample size.
Although investigators advocated that esophageal NEC was a systemic disease similar to SCLC [18, 21] and that non-surgical approaches (chemotherapy, radiotherapy, or chemoradiotherapy) were recommended as the priority in therapeutic choices [14, 21], recent studies have shown that surgery could still benefit a unique portion of SCLC patients [22]. After a median follow-up time of 54.8 months, the median survival time for our surgical patients was only 21.5 months, indicating the aggressiveness of esophageal NEC. In the univariate analysis, TNM stage, lymph node metastasis, and adjuvant therapy were found to significantly influence the survival of esophageal NEC patients. When we investigated further, we found that although there was no significant survival differences among stage I, stage IIA, and stage IIB patients, those patients had significantly longer survival than stage III patients. Therefore, stage I, stage IIA, and stage IIB patients could be aggregated into one unique group of SRLD. Interestingly, stage III patients (median survival time 12.7 months) were found to have significantly shorter overall survival than SRLD group patients (median survival time 31.1 months) in both univariate and multivariate analyses, and we thus call the stage III patients as SNRLD group. Given the fact that the reported median survival time in patients with chemoradiotherapy alone was about 8.0–16.7 months [5, 18, 23], while in surgically resected esophageal NEC patients it was about 16.0–28.5 months [4, 16, 24], our data demonstrated that surgery could only benefit SRLD patients but could not benefit SNRLD patients. Accordingly, adjuvant therapy could only significantly increase the survival of SRLD patients (P = 0.004), but could not significantly bring survival benefits for SNRLD patients (P = 0.136). Therefore, the revised protocol for surgical treatment for esophageal NEC would be like this: First, use VALSG system to pick out limited disease of esophageal NEC; Secondly, evaluate their resectability by preoperative images; Thirdly, applying TNM staging system to subgroup resectable limited disease of esophageal NEC into SRLD group and SNRLD group; Finally, only select the SRLD group for surgery. As for the SNRLD group, direct surgical treatment is not recommended, and neoadjuvant therapy or chemoradiotherapy would be the prior choice.
Even though we draw our reasonable conclusions based on one of the largest surgical cohorts with a very low rate of lost to follow-up (2.8%), our study still had several limitations. First, the retrospective study design could affect our overall analysis. Another limitation is the lack of detailed information about adjuvant therapy due to a relatively long time gap. Moreover, due to selection bias of patients receiving adjuvant therapy, the causal relationship of adjuvant therapy and survival has not been well proven in our study. Finally, due to the fact that our patients were preoperatively diagnosed as resectable esophageal malignancies, none of them received neoadjuvant therapy. Therefore, the role of neoadjuvant therapy in downstaging still needs to be established in future studies. Therefore, further researches with larger sample size are needed to confirm and update our current conclusion.
Conclusion
Esophageal NEC is a rare and aggressively malignant tumor. The resectable limited disease of esophageal NEC could be further subgrouped into SRLD group and SNRLD group. For SRLD group, surgery combined with adjuvant therapy could be the prior therapy modality, while for SNRLD group, neoadjuvant therapy or chemoradiotherapy should be the optimal therapeutic strategy.
References
Kloppel G (2011) Classification and pathology of gastroenteropancreatic neuroendocrine neoplasms. Endocr Relat Cancer 18(Suppl 1):S1–16
Rindi G (2011) Wiedenmann B Neuroendocrine neoplasms of the gut and pancreas: new insights Nature reviews. Endocrinology 8:54–64
Modlin IM, Oberg K, Chung DC et al (2008) Gastroenteropancreatic neuroendocrine tumours. Lancet Oncol 9:61–72
Huang Q, Wu H, Nie L et al (2013) Primary high-grade neuroendocrine carcinoma of the esophagus: a clinicopathologic and immunohistochemical study of 42 resection cases. Am J Surg Pathol 37:467–483
Nakajima Y, Zenda S, Minashi K et al (2012) Non-surgical approach to small cell carcinoma of the esophagus: does this rare disease have the same tumor behavior as SCLC? Int J Clin Oncol 17:610–615
Diagnosis Stahel RA (1991) staging, and prognostic factors of small cell lung cancer. Curr Opin Oncol 3:306–311
Wang SY, Mao WM, Du XH et al (2013) The 2002 AJCC TNM classification is a better predictor of primary small cell esophageal carcinoma outcome than the VALSG staging system. Chin J Cancer 32:342–352
Micke P, Faldum A, Metz T et al (2002) Staging small cell lung cancer: veterans administration lung study group versus international association for the study of lung cancer–what limits limited disease? Lung Cancer (Amsterdam, Netherlands) 37:271–276
Situ D, Lin Y, Long H et al (2013) Surgical treatment for limited-stage primary small cell cancer of the esophagus. Ann Thorac Surg 95:1057–1062
Hou X, Wei JC, Wu JX et al (2013) Multidisciplinary modalities achieve encouraging long-term survival in resectable limited-disease esophageal small cell carcinoma. PloS One 8:e69259
Chen SB, Yang JS, Yang WP et al (2011) Treatment and prognosis of limited disease primary small cell carcinoma of esophagus. Dis Esophagus 24:114–119
Meng MB, Zaorsky NG, Jiang C et al (2013) Radiotherapy and chemotherapy are associated with improved outcomes over surgery and chemotherapy in the management of limited-stage small cell esophageal carcinoma. Radiother Oncol 106:317–322
Chen WW, Wang F, Chen S et al (2014) Detailed analysis of prognostic factors in primary esophageal small cell carcinoma. Ann Thorac Surg 97:1975–1981
Jatoi A, Miller RC (2008) Should we recommend surgery to patients with limited small cell carcinoma of the esophagus? J Thorac Oncol 3:1373–1376
Maru DM, Khurana H, Rashid A et al (2008) Retrospective study of clinicopathologic features and prognosis of high-grade neuroendocrine carcinoma of the esophagus. Am J Surg Pathol 32:1404–1411
Tanaka T, Matono S, Nagano T et al (2010) Surgical management for small cell carcinoma of the esophagus. Dis Esophagus 23:502–505
Chen SB, Yang JS, Yang WP et al (2011) Treatment and prognosis of limited disease primary small cell carcinoma of esophagus. Dis Esophagus 24:114–119
Yau KK, Siu WT, Wong DC et al (2007) Non-operative management of small cell carcinoma of esophagus. Dis Esophagus 20:487–490
Lu XJ, Luo JD, Ling Y et al (2013) Management of small cell carcinoma of esophagus in China. J Gastrointest Surg 17:1181–1187
Deng HY, Ni PZ, Wang YC et al (2016) Neuroendocrine carcinoma of the esophagus: clinical characteristics and prognostic evaluation of 49 cases with surgical resection. J Thorac Dis 8:1250–1256
Lv J, Liang J, Wang J et al (2008) Primary small cell carcinoma of the esophagus. J Thorac Oncol 3:1460–1465
de Hoyos A, DeCamp MM (2014) Surgery for small cell lung cancer. Thorac Surg Clin 24:399–409
Hudson E, Powell J, Mukherjee S et al (2007) Small cell oesophageal carcinoma: an institutional experience and review of the literature. Br J Cancer 96:708–711
Zou B, Li T, Zhou Q et al (2016) Adjuvant therapeutic modalities in primary small cell carcinoma of esophagus patients: a retrospective cohort study of multicenter clinical outcomes. Medicine 95:e3507
Funding
This work was supported by National Natural Science Foundation of China [Nos. 81672291; 31071210] (to Yi-Dan Lin).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interests
None.
Rights and permissions
About this article
Cite this article
Deng, HY., Li, G., Luo, J. et al. The Role of Surgery in Treating Resectable Limited Disease of Esophageal Neuroendocrine Carcinoma. World J Surg 42, 2428–2436 (2018). https://doi.org/10.1007/s00268-018-4475-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-018-4475-3