Abstract
Purpose of Review
Despite mounting interest in the non-operative management (NOM, also known as watchful waiting) of rectal adenocarcinoma, limited guidance exists regarding appropriate patient selection and procedures. In this literature review targeting patients with operable adenocarcinoma of the rectum, we sought to evaluate NOM in terms of patient selection, management approaches, and outcomes with regard to both quality of life (QoL) and oncologic outcomes.
Recent Findings
Despite a lack of randomized evidence comparing NOM (performed via active surveillance following neoadjuvant chemotherapy and radiation) to neoadjuvant therapy followed by planned surgery, given that the vast majority of local, regional, and distant recurrences occur early in follow-up, the available evidence points to similar oncologic outcomes and possible QoL improvement. Due to the high chance of surgical salvage in the case of locoregional recurrence, close multidisciplinary follow-up is essential.
Conclusions
Under the care of an experienced multidisciplinary lower gastrointestinal team, NOM is feasible, is safe, and has the potential for improved QoL. A potential algorithm for clinically implementing NOM is described within this review.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Decades of research have led to improvements in rectal cancer outcomes, with the German phase III CAO/ARO/AIO-94 trial setting a new standard management approach since its publication. Although it established the superiority of neoadjuvant long-course concurrent chemoradiation (LCRT) followed by surgery and then adjuvant chemotherapy over adjuvant LCRT [1], this treatment paradigm has been associated with significant long-term sequelae. With local recurrence rates occurring in only 0–8% of patients, evidence is increasing to support the hypothesis that only one local therapy is required for many patients to achieve optimal balance between treatment efficacy and quality of life (QoL) [1, 2••]. Although one strategy has been to eliminate radiation therapy (RT) for early stage rectal cancer patients [3, 4], another option gaining momentum is non-operative management (NOM, also known as “watch and wait”) following RT and chemotherapy. Although avoidance of a permanent stoma is a top priority for rectal cancer patients [5, 6], historically low pathologic complete response (pCR) rates on the order of 8–10% in rectal cancer likely delayed interest in such an approach [1, 7]. Habr-Gama and colleagues were the first to report long-term outcomes noting complete clinical response (cCR) rates exceeding historic pCR rates, with the majority of cCRs maintained and nearly all patients having successful surgical salvage in the setting of locoregional recurrence [8]. Data from randomized controlled trials (RCTs) confirming equivalent outcomes of NOM vs. neoadjuvant LCRT and surgery are not available, tempering the endorsement of NOM by many national guidelines [9]. The most recent version of the National Comprehensive Cancer Network (NCCN) guidelines currently does not include NOM as part of the main treatment algorithm, although the option is described in a footnote for cT3-4 N-any patients with or without a clear circumferential resection margin (CRM), appropriately suggesting this approach only being pursued by experienced multidisciplinary teams given the rigor and nuance of treatment and follow-up [10].
The purpose of this review is to increase physician familiarity with NOM as well as its potential benefits and risks. Survey data has indicated that knowledge of the literature has been correlated with physician comfort discussing and offering NOM with their patients [11]. Survey data also reveals increasing interest in NOM by both rectal cancer patients and their physicians, with one study indicating NOM as the option most patients preferred [6]. Patients have been found to be more comfortable than physicians with accepting higher risks of regrowth (defined as primary tumor recurrence following treatment in the setting of NOM), with patients willing to pursue the approach even if it was assumed this resulted in on average up to a 20% shorter overall survival (OS) [12]. Fortunately, although RCTs are lacking available data thus far, that does not suggest outcomes are compromised with NOM [2••, 13••, 14]. A survey of Asia-Pacific colorectal surgeons determined that over 80% support the option of NOM, with about 2/3 comfortable enough to offer it to their own patients [15]. However, in order to better inform patients of the risks and benefits of their various options, physicians must have a clear understanding of the rationale behind the various facets of NOM, as well as expected outcomes. The evidence contained within this review was assessed using the Population, Intervention, Comparator, Outcome, and Study design (PICOS) framework. For the population of operable patients with adenocarcinoma of the rectum, we sought to evaluate NOM in terms of patient selection, procedures, and outcomes with regard to QoL as well as disease control and survival metrics.
Methodology
Study types within this literature review consisted of RCTs, meta-analyses, and observational studies. With librarian assistance, we developed a literature search strategy using subject headings and combinations of keyword search terms (Appendix 1). To yield a comprehensive set of relevant articles, peer-reviewed journals indexed in Ovid Medline were searched covering the timeframe from 1/1/2015–9/7/2020. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses Literature Search Extension (PRISMA-S) guidelines were used to guide the identification of journal articles for this literature review [16]. Two authors (CA and PC) independently screened the literature search results and full-text articles to determine the final studies included in this review as detailed in Appendix 2. Any discrepancies between the reviewers were resolved by consensus. We reviewed the bibliographies of full articles for a comprehensive survey, and 8 additional studies were included meeting all inclusion criteria except publication date (6 published before 2015). Forward citation chaining via Web of Science was then performed on the selected documents to determine if any eligible articles published no later than 9/7/2020 had been missed by the initial search strategy, and 3 were discovered resulting in a final count of 80 references [1, 2••, 3,4,5,6,7,8,9, 11, 12, 13••, 14, 15, 17••, 18,19,20,21,22,23,24,25, 26•, 27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45, 46•, 47•, 48, 49•, 50,51,52,53,54,55,56,57, 58•, 59, 60, 61•, 62,63,64,65,66,67,68,69, 70•, 71,72,73,74,75,76, 77•, 78,79,80,81]. The remaining 6 references contained in this paper involve 3 guideline documents for context [10, 82, 83], PRISMA-S instructions [16], a key conference abstract [84], and the associated protocol design [85] to address important advances in NOM research. The PRISMA-S checklist is contained in Appendix 3, Table 4.
Patient Selection and Outcomes with Non-operative Management
To investigate factors predictive of tumor regrowth following cCR post-neoadjuvant LCRT, Chadi et al. performed a rigorous individual patient data meta-analysis assessing 20 core variables in 11 data sets across 10 centers for non-metastatic cT-any cN-any patients [17••]. The authors were careful to include studies with a definition of a cCR that was equivalent to São Paulo benchmarks pioneered by Dr. Habr-Gama (i.e., absence of residual ulceration, stenosis, or mass within the rectum using digital rectal exam (DRE) and endoscopic exam; of note, cross-sectional imaging was not required), with the initial cCR rate after ranging from 12 to 78%. To increase patient population homogeneity, patients receiving 5 Gy × 5 fraction (fx) short course radiation (SCRT), local excision (LE), or contact brachytherapy were excluded. The majority of series involved LCRT without induction (pre-LCRT) or consolidation (post-LCRT) chemotherapy. With a 3-year median follow-up, the 2- and 5-year local regrowth rates were 21.4% (95% confidence interval [CI], 15.3–27.6) and 28.0% (95% CI, 20.3–35.8). Of importance is that 93.4% of regrowths occurred within 3 years. Only T-stage was associated with regrowth, with rates of 19% (95% CI, 13–28), 31% (95% CI, 26–37), and 37% (95% CI, 21–60) for T1/2 (n = 125), T3 (n = 282), and T4 (n = 22) disease, respectively. Clinical variables such as nodal stage, carcinogenic embryonic antigen (CEA) level, and distance to the verge did not correlate with regrowth, indicating that these variables should not be used to exclude patients from NOM.
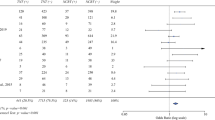
A major concern with NOM is missing the opportunity to cure a patient. Although one retrospective series showed an increased rate of distant metastases associated with regrowth [18], this has not been described in other studies [20,21,22,23, 39]. Table 1 describes the characteristics of key NOM studies, while Table 2 summarizes their outcomes. Available data including meta-analyses have revealed that NOM does not appear associated with any detriment to distant-metastases-free survival (DMFS), non-regrowth recurrence, or disease-specific survival (DSS) [2••, 13••, 14, 19,20,21,22,23]. In the meta-analysis by Dossa et al., it was found this holds true even when comparing NOM patients to those found to have a cCR pre-operatively or pCR at the time of surgery, a strong predictor of improved outcomes [2••]. DMFS rates were not significantly different and were ≤ 20% for all groups. Following local regrowth the pooled proportion of patients who had salvage therapy was 95.4% (95% CI, 89.6–99.3). Another pooled analysis noted an 88% salvage rate for all pelvic recurrences, of which 93% were R0 and 45% were sphincter-sparing [13••]. Retrospective analyses have not found any increased morbidity associated with delayed salvage surgery [24, 25]. Over 90% of locoregional and almost 80% of distant recurrences occurred within first 3 years [2••, 13••, 17, 23]. Despite shorter duration of follow-up compared to surgical series, most recurrences appear captured, and thus, NOM appears promising and on par with standard treatment with regard to oncologic outcomes.
Treatment Regimens
Radiation
In the aforementioned individual patient data meta-analysis, LCRT radiation doses ranged from 45 to 65 Gy and RT dose was not correlated with regrowth rate [17••]. In fact, the lowest rate involved a 50.4 Gy cohort. However, the question remains whether increasing the RT dose leads to an improved initial cCR rate. In the randomized, phase II RECTAL-BOOST study, increasing the dose from 50 to 65 Gy via a 5 × 3 Gy boost increased the initial near cCR or cCR rate from 45 to 69%, but the pCR rate or 2-year sustained cCR rate was not improved (38% vs. 36%, respectively) [26•]. In the setting of NOM, data from investigators out of São Paulo, Brazil, showed that for cT3 patients, the cCR rate was between 54 and 55% regardless of whether the regimen 50.4 Gy/28 fx (“standard” LCRT) or 54 Gy/30 fx with consolidation chemotherapy (“extended” LCRT, preferred by the group since 2006) was employed [27]. Surgery-free survival at 1 and 5 years was numerically but not significantly improved with extended LCRT (42% vs. 37.9% and 33.4% vs. 27.1%, respectively). In a separate retrospective analysis of 81 patients from the same group, they found that cT2 N0 patients were significantly more likely to have a cCR with extended LCRT vs. standard LCRT (85.7% vs. 56.6%, p < 0.001) [28]. However, consistent with the data in the individual patient data meta-analysis by Chadi et al. [17••], once a cCR has been attained, the surgery-free survival was similar between groups [28]. Because of the improved initial cCR rate, the 5-year organ preservation rate was higher with extended vs. standard LCRT (67% vs. 30%, p = 0.001). These two analyses offer insight as to why cross-trial comparisons regarding cCR rates should be approached with caution due to potential biases. While tempting to note that the prospective extended LCRT-only approach published in 2013 resulted in higher cCR rates (68%) than the standard LCRT approach (49%) assessed retrospectively in 2014 (see Table 1), multiple differences including patient population, study design, and methods of cCR assessment make such comparisons challenging [21, 22]. With regard to local excision, in the ACOSOG Z6041 trial, high toxicity was noted with 54 Gy, which was decreased to 50.4 Gy, resulting in improved tolerability. However, based on other trials that investigated the effects of concurrent oxaliplatin, radiosensitizing oxaliplatin was the more likely culprit for toxicity in ACOSOG as other prospective series have not reported increased toxicity with 54 Gy. Of note, data from a meta-analysis on patterns of failure note that the superior border of RT fields could be dropped to S2/3 to limit toxicity for cT1-2 patients [29]. In a study investigating the late dose-volume effects of RT specifically on the anorectal function in rectal cancer patients, the investigators assessed the frequency of low anterior rectal syndrome (LARS), one of the most common and challenging side effects occurring from the treatment of rectal cancer. It is defined as a constellation of symptoms defined by problems with fecal frequency, incontinence/seepage, and incomplete evacuation. One-third had major LARS in this series, and the most frequent reported complaints were clustering and fecal urgency. Trends towards worse long-term anorectal function were noted with a higher anal sphincter complex radiotherapy dose [30]. Since patients choosing NOM are clearly concerned about QoL, these data and patient concerns should be considered when deciding on RT dose.
There are less data when it comes to SCRT in the setting of organ preservation. A large, retrospective analysis of Dutch patients treated with either LCRT (n = 5070) or SCRT (n = 764) without further chemotherapy following an interval of 5–15 weeks revealed that significantly more patients had a pCR following LCRT (17.5%) as compared to SCRT (9.3%) [31]. An international retrospective series found that significantly more ypN+ disease was found with SCRT without neoadjuvant chemotherapy compared to LCRT, indicating SCRT alone may be inadequate to sterilize pelvic disease [32]. In a small retrospective series of patients who underwent SCRT followed by LE 8–10 weeks later, only 17% (5 of 29) of cT2 patients had a pCR as compared to 48% of cT1 patients (13 of 27) [33], with acute RT-related complications occurring in about 1/3 of patients. Other data noting QoL decreases with neoadjuvant RT +/- chemotherapy indicates LE alone is preferred whenever RT may be avoided [34]. Overall, these data indicate that SCRT alone is not an optimal strategy when NOM is the goal [31]. However, there are data noting similar outcomes between neoadjuvant SCRT and consolidation chemotherapy vs. LCRT +/- consolidation chemotherapy when treatment involves planned total mesorectal excision (TME) [35,36,37]. Given the current lack of data, NOM via SCRT with consolidation chemotherapy appears most appropriate in an investigative setting such as the phase 2 Non-Operative Management and Early Response Assessment in Rectal Cancer (NOM-ERA) study investigating this approach (NCT03904043). In summary, prescribing doses of 50–54 Gy in 25 fractions of 1.8–2 Gy appears most appropriate in the NOM setting. Further data, ideally gathered prospectively via RCT, is needed to allow improved personalization of the most appropriate RT dose.
Brachytherapy
To date, the highest reported cCR rate following neoadjuvant therapy was 78% in the series involving 65 Gy delivered via a 5 Gy high dose rate (HDR) brachytherapy boost after 60 Gy to the gross tumor. Fifty Gy was given to elective nodes via a simultaneous-integrated boost [38] (Table 2). Long-term follow-up revealed the 5-year regrowth at 31%, similar to series with standard RT dosing [17••, 39]. Although the majority of QoL patient-reported outcome (PRO) metrics did not vary between baseline and subsequent assessments, rectal bleeding deteriorated from baseline which was attributed to the brachytherapy boost. Outcomes with an alternative method to HDR have been described by small series of patients receiving 45–50 Gy RT + 90 Gy contact brachytherapy (CXB).These have shown initial cCR rates ranging from 64 to 98% with regrowth rates ranging from 11 to 12% and toxicity limited to the rectum [40, 41]. Although promising, the small size of the series, non-uniform technique and outcome reporting, and short follow-up limit the definitive conclusions about the effectiveness and safety of brachytherapy. However, these early results do indicate that integration of brachytherapy into the NOM regimen is worthy of further study. The Organ Preservation in Early Rectal Adeno (OPERA) (NCT 02505750) is a phase III study comparing 45 Gy + either 9 Gy/5 fx of RT or 90 Gy/3 fx of CXB. Although brachytherapy is not standard in NOM at present, to enable future comparisons and improvements, standardizing the reporting of endorectal brachytherapy RT dose, treatment volume specifications, and toxicity are necessary.
Chemotherapy
Although there are no published RCTs investigating the optimal treatment sequence and chemotherapy regimen for NOM, there are increasing relevant data to help guide practice. While there may be certain subsets of patients who may benefit from adjuvant chemotherapy following neoadjuvant LCRT and surgery [42], various meta-analyses have shown little to no benefit thus resulting in a shift to the development of total neoadjuvant therapy (TNT). Delivering all chemotherapy neoadjuvantly increases the chance of completing all treatment [43], and this theoretically may help combat distant and other patterns of recurrence. Pathologic complete response rates have been found to improve with increasing number of cycles of induction chemotherapy [44], with the TIMING study showing a pCR rate of 18% with LCRT alone, increasing to 25%, 30%, and 38% with 2, 4, and 6 q2week cycles of FOLFOX, respectively. However, toxicity increased as well, with the Grade 3+ side effects rate at just 5% with 1 month (2 cycles) of chemotherapy vs. 35% with 3 months (6 cycles). Further data are needed to determine the ideal balance between benefit and toxicity.
For cT1 or T2 patients, retrospective data from Habr-Gama et al. revealed that patients getting 50.4 Gy with 2 q3week concurrent cycles of 5-FU (standard LCRT) were less likely than those getting 54 Gy with 6 q3wk cycles of concurrent and consolidation chemotherapy (extended LCRT) to achieve a cCR (56% vs. 86%) and avoid definitive surgical resection at 5 years (30% vs. 67%) [28]. Similar to the findings of Chadi et al. [17••], for those who achieved a cCR regardless of dose group, surgery-free survival was similar [28]. No NOM patient required medical or surgical procedures for bleeding, strictures, or pain. This indicates that treatment up to 54 Gy with consolidation chemotherapy is a reasonable, safe approach for cT2 N0 patients. Emergent data includes that from the phase 2R Organ Preservation in Rectal Adenocarcinoma (OPRA) study (NCT02008656), where patients with MRI stage II or III disease were randomized to 4 months of induction or consolidation chemotherapy added to LCRT to 50–56 Gy [84, 85]. At a median follow-up of 2 years, there was equivalent chemotherapy compliance between the TNT approaches, with a median RT dose of 54 Gy. Three-year disease-free survival (DFS) (77–78%) and DMFS (81–83%) rates were equivalent, but there was significantly improved 3-year organ preservation with the consolidation chemotherapy as opposed to induction (58% vs. 43%, respectively (p = 0.01)). In the operative setting, improved ypCR findings with consolidation vs. induction chemotherapy of the phase 2R CAO/ARO/AIO-12 study lend further support to this treatment sequence [46•]. In summary, although there is no proven benefit to NOM with induction or consolidation chemotherapy, numerically, the best reported outcomes to date involve LCRT followed by consolidation chemotherapy with either FOLFOX or CAPOX. Often 4 months of consolidation therapy is considered reasonable, as this was used in OPRA and it formed the standard-of-care arm in NRG-GI002: A phase II clinical trial platform for total neoadjuvant therapy (TNT) in rectal cancer (NCT02921256). Concurrent 5-FU or capecitabine should accompany LCRT.
Integrating Local Excision into NOM
Following radiation and chemotherapy, options for organ preservation could include local excision (LE) rather than TME if there is an incomplete response. However, appropriate considerations include concerns for incompletely addressed nodal disease and/or local recurrence. In order to better understand how LE may be integrated into organ preservation strategies including NOM, it is important to review the 4 major trials that address LE following LCRT, including (1) the phase 3 GRECCAR-2 trial that involved neoadjuvant LCRT with good responders (defined as primary ≤ 3 cm post-LCRT) randomized to TME vs. local excision, (2) the phase 3 study by Lezoche et al. that randomized 100 cT2 N0 patients to either TME or LE following LCRT, (3) the single-arm phase 2 CARTS trial that involved LCRT followed by transanal endoscopic microsurgery (TEM), and (4) the phase 2 single-arm ACOSOG Z6041 trial that also involved LCRT followed by TEM [47•, 48, 49•, 50, 79]. The ACOSOG and Lezoche et al. trials only included cT2 N0 patients whereas the other two included cT3, with GRECCAR-2 also allowing node-positive patients. Despite the ACOSOG and Lezoche et al. trials not requiring a completion TME for concerning pathologic findings such as ypT2+ disease, there were no nodal failures. For Lezoche et al., although TME patients may have been overtreated, oncologic outcomes were equivalent between arms. In ACOSOG, the local failure rate was only 4%. Of significant interest is that the pCR rate at the time of LE in all trials was noted to be 40–44%, supporting NOM as a potential initial strategy rather than planned LE. In GRECCAR-2, only 8% of all TME specimens and 8% of those with ypT2 disease were ypN+ at TME, lower than expected based on prior other data that ypT2 disease in initially cT3-4 or cN+ patients was associated with a node-positivity rate up to 30% [51]. As might be expected, in GRECCAR-2 ypT3 disease was associated with a 40% nodal positivity rate at TME [49•]. Another series of patients with initial cT3-4 N0-1 disease noted nodal positivity of > 10% despite ypT0 at TME suggesting a pCR of the primary does not guarantee clearance of nodal disease [52]. In a retrospective series of cT3 or cN+ patients, 50 of 362 patients received LE due to an objective clinical response that was not quite a cCR due to the presence of a residual ulcer measuring ≤ 3 cm. However, of these 50 patients, 30% underwent a completion TME for adverse pathologic findings (≥ ypT2 or R1), and 27% had positive lymph nodes on final pathology [53]. In summary, given the lack of node positivity seen in ACOSOG and Lezoche et al., it may be surmised that the nodal positivity for ≥ ypT2 patients is driven by those with ≥ cT3 staging at diagnosis.
Because of the high rate of completion TME, in GRECCAR-2, QoL was not found to be improved compared to the LE group in the intention to treat analysis [49•]. Of importance is that patients who underwent neoadjuvant LCRT followed by LE who then required completion TME had a 78% chance of encountering major surgical morbidity (Grades III–IV of Dindo’s classification [54]) or severe side effects (definitive colostomy, anal incontinence, or impotence), as compared with only 38% who had a TME post-LCRT. As expected, the lowest rate of major toxicity (29%) was reported by patients whose treatment ended at LE following LCRT. Oncologic control did not differ between the 2 randomized groups. In the ACOSOG trial, completion TME was not required and QoL was preserved following LE [55]. In a study by Habr-Gama, it was noted that QoL and rectal function scores were improved with a NOM approach as compared to LE following LCRT [56].
In summary, these various data suggest very limited support for a LCRT and LE approach for patients with cT3+/cN+ disease at presentation. Given the risk of completion TME which is found to significantly increase the risk for poor QoL following LCRT, cT3+/N+ patients may be better advised to attempt organ preservation through NOM, with a plan for salvage with TME rather than LE for an incomplete response. The finding of ypT2 disease at LE for initial stage cT3+/N+ patients confers a higher risk of node positivity than ypT2 disease for patients who are cT2 N0 at diagnosis. For cT2 N0 patients who do not respond completely to LCRT during NOM and are found to have ≤ ypT2 disease at LE, favorable oncologic and QoL outcomes may be possible despite avoidance of a completion TME. This approach is not mentioned as an option in the current NCCN rectal guidelines [10], but it is a favored approach by the gastrointestinal expert American Radium Society™ Appropriate Use Committee [83].
Quality of Life
QoL benefits may be seen with NOM regardless of tumor location and the expected surgery. Of note, cancer patients’ participation in social, recreational, and civic activities has been found to be strongly associated with QoL, but these activities are not well integrated into cancer survivorship research or interventions [57]. Several matched controlled studies have shown major LARS occurs in about 2/3 of patients undergoing RT and surgery, but definitive LCRT is not without problems with 1/3 of patients suffering these symptoms [58•, 59]. Beyond fecal symptoms, additional benefits noted with NOM vs. planned surgery following neoadjuvant treatment include improved physical and cognitive function, improved physical and emotional roles, better global health status, and fewer problems with sexual/urinary tract function [58•, 60]. In the absence of randomized data comparing NOM with standard surgical therapy following LCRT, Markov Decision Analyses have been performed to compare outcomes [61•, 62]. These assessments have found similar DSS, but with the benefit of superior quality adjusted survival and decreased costs. Upfront TME was preferred only when the assumed expected rates of successful surgical salvage were lower than those actually reported in the literature, with the authors concluding that NOM is a reasonable option if patients undergo close monitoring for recurrence.
Assessment of Treatment Response
Much effort has also been put into correlating pCR with tumor response assessments following LCRT [63]. Typically, a cCR has been defined as follows: (1) DRE: no palpable tumor when initially palpable; (2) endoscopy: no residual tumor, with flat, white scar and/or telangiectasia acceptable but no ulcer or nodularity; (3) T2-weighted MRI (MRI-T2W): only dark and no intermediate T2 signal with no visible nodes; and (4) diffusion-weighted MRI (MRI-DW): no diffusion restriction (Table 1) [23, 85]. However, there are limitations to all methods of assessment, with uncertainty further compounded by heterogeneity in the timing and techniques of the various assessments thus limiting definitive conclusions. For example, pCRs have been noted despite mucosal abnormalities on endoscopy, mixed signal or tumor site irregularities on MRI-T2W, restriction on MRI-DW, and suspicious nodes indicating the possibility of false positives [64, 65]. Typically, MRI rarely alters the determination of whether a cCR is present based on endoscopic assessment [70•, 71]. Fortunately, advances are being made to further gastrointestinal radiologists’ ability to recognize a rectal cCR, including certain patterns of intermediate and low signal that indicate a cCR with high specificity rather than persistent disease (i.e., split scar sign) [81]. Biopsy should not be relied on as a means to rule out disease presence, with a negative predictive value (NPV) reported as low as 11% due to tumor scatter or submucosal persistence of disease [66]. The greatest value of MRI as well as CT at present lies in evaluating extraluminal recurrences. In a retrospective series involving 3 independent reviewers assessing the likelihood of a pCR based on endoscopic images following LCRT or SCRT, the ranges for sensitivity, specificity, positive predictive value (PPV), and NPV were 72–94%, 61–85%, 63–78%, and 80–89%, respectively [64]. A flat white scar was most predictive of a ypCR, with the PPV of small (< 1 cm) flat, large flat, and irregular ulcers at 40–50%, 29–33%, and 4–15%, respectively. In the setting of these ulcers, MRI often shows ambiguous findings such as heterogeneous T2 signal or small focal diffusion restriction and thus does not provide additional clarity [67]. In a prospective series of 124 patients evaluated pre-operatively 6–7 weeks post-LCRT by MRI and EUS, 75% of pCR patients had a mass in the rectal lumen or suspicious lymph nodes [68]. Therefore, for those with a near cCR, a repeat assessment 2–3 months later may be pursued. Figure 1 shows an example of a patient experiencing a cCR with resolution of all concerning clinical findings, whereas Fig. 2 illustrates MRI and endoscopic findings consistent with an incomplete response. Following LE, despite anatomic defects that may be introduced from the surgical procedure, MRI has shown utility with high T2W signal intensity and thickening of the rectal wall in recurrent disease, with DWI abnormalities also useful but slightly less sensitive [69].
66-year-old female with Stage IIIB, T3b N1b M0 adenocarcinoma of the rectum. Initial staging MRI demonstrated a centrally ulcerated left lateral wall mass (red arrows) which had intermediate intensity on T2W MRI (a), was hypointense on ADC map (b), and was hyperintense on DWI (c). Two mesorectal nodes were noted, and the extramural depth of invasion extended 4 mm. DRE and endoscopy (d) revealed a 2 cm mass 3 cm from the dentate line. Treatment involved LCRT to a prescription dose of 5400 cGy concurrent with capecitabine, followed 1 month later by 8 cycles of consolidation FOLFOX q2wks. After treatment, the lesion (red arrows) was decreased in size and was markedly hypointense on T2W (e), hypointense on ADC (f), and hypointense on DWI (g) consistent with cCR. The mesorectal nodes had resolved. DRE revealed a 1-cm firmness in the left lateral position with a smooth mucosal coating, and endoscopy (h) showed a flat white scar with telangiectasias (yellow arrow). Key: cCR complete clinical response, MRI magnetic resonance imaging, DRE digital rectal exam, T2W T2-weighted imaging, DWI diffusion-weighted imaging, ADC apparent diffusion coefficient, FOLFOX folinic acid, 5-FU, oxaliplatin
57-year-old male with Stage IIA, T3b N0 M0 adenocarcinoma of the rectum. Initial staging MRI demonstrated a left lateral wall mass (red arrows) which had intermediate intensity on T2W imaging (a), was hypointense on ADC map (b), and was hyperintense on DWI (c). The extramural depth of invasion extended 3 mm. DRE and endoscopy (d) revealed a nearly circumferential mass 3 cm from the dentate line. Treatment involved 5 cycles of induction CAPOX q3wks followed 2 months later by LCRT to max dose of 5400 cGy concurrent with capecitabine. Ten weeks following LCRT, MRI showed the tumor (red arrows) had decreased in size but there was residual disease (red arrows) which had intermediate intensity on T2W (e), was hypointense on ADC (f), and was hyperintense on DWI (g). There was a rim of marked T2W hypointensity (yellow arrow) (a) representing fibrosis in area of treated tumor. h Endoscopy revealed regression and necrosis but still clear residual disease. He proceeded to APR and was found to have ypT2 N0 disease. Key: MRI magnetic resonance imaging, DRE digital rectal exam, DWI diffusion-weighted imaging, T2W T2-weighted imaging, ADC apparent diffusion coefficient, LCRT long-course concurrent chemoradiation, CAPOX capecitabine and oxaliplatin
Initial Assessment and Surveillance
There is an increasing amount of data noting the importance of allowing patients undergoing NOM with a near cCR to continue close follow-up, as excellent oncologic outcomes have been achieved with this approach [19]. Hupkens et al. found that > 90% of patients with a near cCR 8–10 weeks after LCRT (none received induction or consolidation chemotherapy) will achieve a cCR 6–12 weeks later [70•]. Although those achieving a cCR at the 2nd time point had a non-significant numerically higher chancer of regrowth (27% vs. 16%), 2-year OS was equivalent (98% vs. 99%). In a retrospective review of 49 consecutive patients who received the São Paulo “extended” LCRT NOM approach of 54 Gy followed by consolidation chemotherapy, Habr-Gama et al. found that only 38% of patients achieved a cCR within 10–16 weeks of neoadjuvant LCRT. The median time to a strict cCR was 18.7 weeks, with earlier T-stage patients (cT2-T3a) achieving a cCR significantly earlier than more advanced disease (cTb-d/4) [71]. Therefore, the authors of these studies offer the logical conclusion that the cCR observation period should be extended rather than proceeding directly to surgery.
It is important to note that if recurrences are identified promptly, the vast majority may be salvaged underlining the importance of close surveillance (Table 2). As noted previously, the majority of recurrences occur during the first 3 years, so closer follow-up is required initially via DRE, endoscopy, rectal protocol MRI, and CT of the chest/abdomen/pelvis with contrast [72]. Close surveillance has been found acceptable to patients and their providers [73], and even with the frequent assessments, NOM still remains more cost effective than planned surgical approaches [74]. Worse outcomes have been found in series where patient compliance with surveillance and salvage surgery is compromised [75, 76]. The location of the recurrences is almost always entirely in the bowel wall and is thus identifiable via DRE and/or endoscopy [19]. Imaging is required to identify nodal recurrences, although fortunately the risk has been found to be low with crude rates at 0–3% [19,20,21, 23] (Table 2). In a retrospective series of 90 patients, every patient without DWI nodal abnormalities was found to be ypN0, with the presence of DWI abnormalities noted to have a sensitivity, NPV, specificity, and PPV of 100%, 100%, 14%, and 24%, respectively [80]. Based on prospectively gathered data, the positive posttest probability for detecting a true cCR has been reported to be as high as 98% when DRE, endoscopy, T2W, and DWI MRI all indicate a cCR [77•]. Combining modalities was also found to improve the negative posttest probability to 15% from 20% and 26% with endoscopy or MRI (T2W and DWI) alone, respectively. This signified that when all tests indicated residual disease was still present the chance of a complete response still actually being present dropped to 15%.
Follow-up should continue for a minimum of 5 years, but follow-up beyond this time is not thought necessary for cT1-2 N0 patients undergoing LE following neoadjuvant therapy given the very low risk of recurrence beyond that time. However, long-term outcomes for patients treated with NOM are still evolving. Conditional survival estimates have been calculated for a São Paulo patient population as a function of time, showing that the chance of recurrence decreases the further from treatment completion with no patients expected to recur past 8 years [78]. Patients were found to have a significantly lower risk (≤ 10%) of developing recurrences 2 years after achieving a cCR following LCRT, with no regrowths expected past 3 years for patients treated with LCRT to 54 Gy with consolidation chemotherapy (extended LCRT). While the authors recognize follow-up past 5 years might detect a small number of late recurrences, it is unclear if prolonged surveillance will have an impact on OS. The authors did note that after 2 years of follow-up, the known risk factor for relapse involving T-stage becomes less relevant, and RT dose escalation to 54 Gy combined with consolidation chemotherapy may significantly decrease recurrence at later time points.
Conclusions
Although there are no RCT data indicating the long-term safety of NOM, outcome data from Phase 1–2 studies have indicated that there are a number of patients who may be able to successfully achieve organ preservation. Based on the literature, approximately 1/3 to 2/3 of patients undergoing NOM achieve a cCR, with regrowth occurring in about 1/5 to 1/3 of patients and overall organ preservation successful in about 1/5 to 1/2 of patients (Table 2). It is understandable that before widespread acceptance of this approach, further prospective data with more universally standardized definitions of treatment response and a follow-up regimen are required (e.g., Magnetic Resonance Tumour Regression Grade as Biomarker for Stratified Management of Rectal Cancer Patients (TRIGGER, NCT02704520) and Can the Rectum be Saved by Watchful Waiting or TransAnal Surgery Following (Chemo)Radiotherapy Versus Total Mesorectal Excision for Early REctal Cancer? (STAR-TREC, NCT02945566)). For those institutions with strong multidisciplinary groups employing high-quality rectal MRIs with skilled radiologist oversight and expertise in assessing for response and recurrence, NOM may be offered to patients of any stage with significant QoL concerns particularly if they have a distal rectal cancer. As always, shared patient-provider decision making is essential, and prospective series must emphasize PROs. With regard to the treatment regimen, more is not always better, and biology may surpass brute force through treatment escalation [26]. At present, LCRT to 50–54 Gy with strong consideration for up to 4 months of consolidation chemotherapy is in line with favorable outcomes noted by the studies found within this literature review as well as the initial results of the OPRA trial (Table 2). Table 3 describes the approach taken at the University of Vermont Cancer Center based on our experience and review of the literature. Our approach agrees well with the ASTRO Clinical Practice Guidelines for rectal cancer [82], and while our follow-up intervals are on the longer side they still fit within previously described surveillance schedules that resulted in successful outcomes (Table 1). It is important to remember that most recurrences occur within the first 3 years, and with close follow-up, the salvage rate is excellent, with the data thus far not suggesting any added surgical complications or worse oncologic outcomes.
Abbreviations
- 5-FU:
-
Fluorouracil
- ADC:
-
Apparent diffusion coefficient
- CAPOX:
-
Capecitabine and oxaliplatin
- CEA:
-
Carcinogenic embryonic antigen
- cCR:
-
Complete clinical response
- CRT:
-
Chemoradiation
- CT:
-
Computed tomography
- CTV:
-
Clinical target volume
- CXB:
-
Contact brachytherapy
- DRE:
-
Digital rectal exam
- DWI:
-
Diffusion-weighted imaging
- EMVI:
-
Extramural vascular invasion
- FOLFOX:
-
Folinic acid, 5-FU, oxaliplatin
- GTV:
-
Gross tumor volume
- HDR:
-
High-dose rate
- LE:
-
Local excision
- LCRT:
-
Long-course chemoradiation
- MRI:
-
Magnetic resonance imaging
- NOM:
-
Non-operative management
- pCR:
-
Pathologic complete response
- PICOS:
-
Population, Intervention, Comparator, Outcome, and Study design
- PRISMA-S:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses Literature Search Extension
- PRO:
-
Patient-reported outcome
- PTV:
-
Planning target volume
- QoL:
-
Quality of life
- RT:
-
Radiation therapy
- RCT:
-
Randomized controlled trial
- TEM:
-
Transanal endoscopic microsurgery
- TME:
-
Total mesorectal excision
- TNT:
-
Total neoadjuvant therapy
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Sauer R, Becker H, Hohenberger W, Rödel C, Wittekind C, Fietkau R, et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med. 2004;351:1731–40.
Dossa F, Chesney TR, Acuna SA, Baxter NN. A watch-and-wait approach for locally advanced rectal cancer after a clinical complete response following neoadjuvant chemoradiation: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol. 2017;2:501–13 Meta-analysis comparing oncologic outcomes for NOM vs. patients who either had a cCR before surgery or pCR at time of surgery, with findings including no differences in non-regrowth recurrences or cancer-specific mortality between groups.
Ruppert R, Kube R, Strassburg J, et al. Avoidance of overtreatment of rectal cancer by selective chemoradiotherapy: results of the optimized surgery and MRI-based multimodal therapy trial. J Am Coll Surg. 2020. https://doi.org/10.1016/j.jamcollsurg.2020.06.023.
Battersby NJ, How P, Moran B, Stelzner S, West NP, Branagan G, et al. Prospective validation of a low rectal cancer magnetic resonance imaging staging system and development of a local recurrence risk stratification model: the MERCURY II study. Ann Surg. 2016;263:751–60.
Wrenn SM, Cepeda-Benito A, Ramos-Valadez DI, Cataldo PA. Patient perceptions and quality of life after colon and rectal surgery: what do patients really want? Dis Colon Rectum. 2018;61:971–8.
Couwenberg AM, Intven MPW, Burbach JPM, Emaus MJ, van Grevenstein WMU, Verkooijen HM. Utility scores and preferences for surgical and organ-sparing approaches for treatment of intermediate and high-risk rectal cancer. Dis Colon Rectum. 2018;61:911–9.
2017 European Society of Coloproctology (ESCP) collaborating group. Evaluating the incidence of pathological complete response in current international rectal cancer practice: the barriers to widespread safe deferral of surgery. Color Dis. 2018;20(Suppl 6):58–68.
Habr-Gama A, Perez RO, Nadalin W, Sabbaga J, Ribeiro U, Silva e Sousa AH, et al. Operative versus nonoperative treatment for stage 0 distal rectal cancer following chemoradiation therapy: long-term results. Ann Surg. 2004;240:711–7 discussion 717-718.
Crawford A, Firtell J, Caycedo-Marulanda A. How is rectal cancer managed: a survey exploring current practice patterns in Canada. J Gastrointest Cancer. 2019;50:260–8.
National Comprehensive Care Network. Rectal Carcinoma (Version 6.2020). https://www.nccn.org/professionals/physician_gls/pdf/rectal_blocks.pdf. All right reserved Accessed September 7, 2020.
Yahya J, Herzig D, Farrell M, Degnin C, Chen Y, Holland J, et al. Survey results of US radiation oncology providers’ contextual engagement of watch-and-wait beliefs after a complete clinical response to chemoradiation in patients with local rectal cancer. J Gastrointest Oncol. 2018;9:1127–32.
Kennedy ED, Borowiec AM, Schmocker S, Cho C, Brierley J, Li S, et al. Patient and physician preferences for nonoperative management for low rectal cancer: is it a reasonable treatment option? Dis Colon Rectum. 2018;61:1281–9.
Dattani M, Heald RJ, Goussous G, Broadhurst J, Sao Juliao GP, Habr-Gama A, et al. Oncological and survival outcomes in watch and wait patients with a clinical complete response after neoadjuvant chemoradiotherapy for rectal cancer: a systematic review and pooled analysis. Ann Surg. 2018;268:955–67 Meta-analysis noting frequency of cCR and the timing and frequency of the various patterns-of-failure including rectal tumor regrowth, nonregrowth pelvic recurrences, and distant metastases. An 82% R0 surgical salvage rate was noted.
Fiorica F, Trovo M, Anania G, Marcello D, Di Benedetto F, Marzola M, et al. Is it possible a conservative approach after radiochemotherapy in locally advanced rectal Cancer (LARC)? A systematic review of the literature and meta-analysis. J Gastrointest Cancer. 2019;50:98–108.
Huh JW, Maeda K, Liu Z, Wang X, Roslani AC, Lee WY. Current status of “watch-and-wait” rectal cancer treatment in Asia-Pacific countries. Ann Coloproctol. 2020;36:70–7.
Rethlefsen ML, Kirtley S, Waffenschmidt S, Ayala AP, Moher D, Page MJ, Koffel JB; PRISMA-S Group. PRISMA-S: an extension to the PRISMA Statement for Reporting Literature Searches in Systematic Reviews. Syst Rev. 2021;26:1–39.
Chadi SA, Malcomson L, Ensor J, et al. Factors affecting local regrowth after watch and wait for patients with a clinical complete response following chemoradiotherapy in rectal cancer (InterCoRe consortium): an individual participant data meta-analysis. Lancet Gastroenterol Hepatol. 2018;3:825–36 Individual patient data meta-analysis showing that among 20 core variables across 11 data sets, a higher T-stage was the only factor associated with a risk of increased rectal tumor regrowth.
Smith JJ, Strombom P, Chow OS, Roxburgh CS, Lynn P, Eaton A, et al. Assessment of a watch-and-wait strategy for rectal cancer in patients with a complete response after neoadjuvant therapy. JAMA Oncol. 2019;5:e185896.
van der Valk MJM, Hilling DE, Bastiaannet E, Meershoek-Klein Kranenbarg E, Beets GL, Figueiredo NL, et al. Long-term outcomes of clinical complete responders after neoadjuvant treatment for rectal cancer in the International Watch & Wait Database (IWWD): an international multicentre registry study. Lancet. 2018;391:2537–45.
Renehan AG, Malcomson L, Emsley R, Gollins S, Maw A, Myint AS, et al. Watch-and-wait approach versus surgical resection after chemoradiotherapy for patients with rectal cancer (the OnCoRe project): a propensity-score matched cohort analysis. Lancet Oncol. 2016;17:174–83.
Habr-Gama A, Sabbaga J, Gama-Rodrigues J, São Julião GP, Proscurshim I, Bailão Aguilar P, et al. Watch and wait approach following extended neoadjuvant chemoradiation for distal rectal cancer: are we getting closer to anal cancer management? Dis Colon Rectum. 2013;56:1109–17.
Habr-Gama A, Gama-Rodrigues J, São Julião GP, Proscurshim I, Sabbagh C, Lynn PB, et al. Local recurrence after complete clinical response and watch and wait in rectal cancer after neoadjuvant chemoradiation: impact of salvage therapy on local disease control. Int J Radiat Oncol Biol Phys. 2014;88:822–8.
Martens MH, Maas M, Heijnen LA, Lambregts DMJ, Leijtens JWA, Stassen LPS, et al. Long-term outcome of an organ preservation program after neoadjuvant treatment for rectal cancer. J Natl Cancer Inst. 2016;108:djw171. https://doi.org/10.1093/jnci/djw171.
van der Sande ME, Figueiredo N, Beets GL. Management and outcome of local regrowths in a watch-and-wait prospective cohort for complete responses in rectal cancer. Ann Surg. 2020. https://doi.org/10.1097/SLA.0000000000003738.
Roxburgh CSD, Strombom P, Lynn P, Gonen M, Paty PB, Guillem JG, et al. Role of the interval from completion of neoadjuvant therapy to surgery in postoperative morbidity in patients with locally advanced rectal cancer. Ann Surg Oncol. 2019;26:2019–27.
Couwenberg AM, JPM B, Berbee M, et al. Efficacy of dose-escalated chemoradiation on complete tumor response in patients with locally advanced rectal cancer (RECTAL-BOOST): a phase 2 randomized controlled trial. Int J Radiat Oncol Biol Phys. 2020. https://doi.org/10.1016/j.ijrobp.2020.06.013Phase II trial RCT that did not find improvement in the rate of pCR or sustained cCR through dose escalation, with the experimental arm receiving a further 5 × 3 Gy boost following the standard arm’s 25 × 2 Gy with concurrent capecitabine.
Sao Juliao GP, Habr-Gama A, Vailati BB, et al. Is neoadjuvant chemoradiation with dose-escalation and consolidation chemotherapy sufficient to increase surgery-free and distant metastases-free survival in baseline cT3 rectal cancer? Eur J Surg Oncol. 2018;44:93–9.
Habr-Gama A, Sao Juliao GP, Vailati BB, Sabbaga J, Aguilar PB, Fernandez LM, et al. Organ preservation in cT2N0 rectal cancer after neoadjuvant chemoradiation therapy: the impact of radiation therapy dose-escalation and consolidation chemotherapy. Ann Surg. 2019;269:102–7.
Socha J, Pietrzak L, Zawadzka A, Paciorkiewicz A, Krupa A, Bujko K. A systematic review and meta-analysis of pT2 rectal cancer spread and recurrence pattern: implications for target design in radiation therapy for organ preservation. Radiother Oncol. 2019;133:20–7.
van der Sande ME, Hupkens BJP, Berbee M, van Kuijk SMJ, Maas M, Melenhorst J, et al. Impact of radiotherapy on anorectal function in patients with rectal cancer following a watch and wait programme. Radiother Oncol. 2019;132:79–84.
Rombouts AJM, Hugen N, Verhoeven RHA, Elferink MAG, Poortmans PMP, Nagtegaal ID, et al. Tumor response after long interval comparing 5x5Gy radiation therapy with chemoradiation therapy in rectal cancer patients. Eur J Surg Oncol. 2018;44:1018–24.
Lorenzon L, Evrard S, Beets G, Gonzalez-Moreno S, Kovacs T, D’Ugo D, et al. Global variation in the long-term outcomes of ypT0 rectal cancers. Eur J Surg Oncol. 2020;46:420–8.
Smart CJ, Korsgen S, Hill J, Speake D, Levy B, Steward M, et al. Multicentre study of short-course radiotherapy and transanal endoscopic microsurgery for early rectal cancer. Br J Surg. 2016;103:1069–75.
Jones HJS, Al-Najami I, Cunningham C. Quality of life after rectal-preserving treatment of rectal cancer. Eur J Surg Oncol. 2020;46:2050–6. https://doi.org/10.1016/j.ejso.2020.07.018.
Latkauskas T, Pauzas H, Kairevice L, Petrauskas A, Saladzinskas Z, Janciauskiene R, et al. Preoperative conventional chemoradiotherapy versus short-course radiotherapy with delayed surgery for rectal cancer: results of a randomized controlled trial. BMC Cancer. 2016;16:927.
Ciseł B, Pietrzak L, Michalski W, Wyrwicz L, Rutkowski A, Kosakowska E, et al. Long-course preoperative chemoradiation versus 5 × 5 Gy and consolidation chemotherapy for clinical T4 and fixed clinical T3 rectal cancer: long-term results of the randomized Polish II study. Ann Oncol. 2019;30:1298–303.
van der Valk MJM, Marijnen CAM, van Etten B, Dijkstra EA, Hilling DE, Kranenbarg EMK, et al. Compliance and tolerability of short-course radiotherapy followed by preoperative chemotherapy and surgery for high-risk rectal cancer - results of the international randomized RAPIDO-trial. Radiother Oncol. 2020;147:75–83.
Appelt AL, Ploen J, Harling H, Jensen FS, Jensen LH, Jorgensen JCR, et al. High-dose chemoradiotherapy and watchful waiting for distal rectal cancer: a prospective observational study. Lancet Oncol. 2015;16:919–27.
Dizdarevic E, Frostrup Hansen T, Ploen J, Henrik Jensen L, Lindebjerg J, Rafaelsen S, et al. Long-term patient-reported outcomes after high-dose chemoradiation therapy for nonsurgical management of distal rectal cancer. Int J Radiat Oncol Biol Phys. 2020;106:556–63.
Gerard J-P, Barbet N, Gal J, et al. Planned organ preservation for early T2-3 rectal adenocarcinoma: a French, multicentre study. Eur J Cancer. 2019;108:1–16.
Sun Myint A, Smith FM, Gollins SW, et al. Dose escalation using contact X-ray brachytherapy (Papillon) for rectal cancer: does it improve the chance of organ preservation? Br J Radiol. 2017;90:20170175.
Breugom AJ, Swets M, Bosset J-F, Collette L, Sainato A, Cionini L, et al. Adjuvant chemotherapy after preoperative (chemo)radiotherapy and surgery for patients with rectal cancer: a systematic review and meta-analysis of individual patient data. Lancet Oncol. 2015;16:200–7.
Cercek A, Roxburgh CSD, Strombom P, Smith JJ, Temple LKF, Nash GM, et al. Adoption of total neoadjuvant therapy for locally advanced rectal cancer. JAMA Oncol. 2018;4:e180071.
Garcia-Aguilar J, Chow OS, Smith DD, Marcet JE, Cataldo PA, Varma MG, et al. Effect of adding mFOLFOX6 after neoadjuvant chemoradiation in locally advanced rectal cancer: a multicentre, phase 2 trial. Lancet Oncol. 2015;16:957–66.
Smith RK, Fry RD, Mahmoud NN, Paulson EC. Surveillance after neoadjuvant therapy in advanced rectal cancer with complete clinical response can have comparable outcomes to total mesorectal excision. Int J Color Dis. 2015;30:769–74.
Fokas E, Allgäuer M, Polat B, et al. Randomized phase II trial of chemoradiotherapy plus induction or consolidation chemotherapy as total neoadjuvant therapy for locally advanced rectal cancer: CAO/ARO/AIO-12. J Clin Oncol. 2019;37:3212–22 Phase IIR study showing increased pCR with consolidation (i.e., post-chemoradiation) chemotherapy as opposed to induction chemotherapy (i.e., pre-chemoradiation).
Lezoche E, Baldarelli M, Lezoche G, Paganini AM, Gesuita R, Guerrieri M. Randomized clinical trial of endoluminal locoregional resection versus laparoscopic total mesorectal excision for T2 rectal cancer after neoadjuvant therapy. Br J Surg. 2012;99:1211–8 RCT of 100 Stage I, T2 N0 M0 rectal cancer patients who all received chemoradiation randomized to either LE or TME, with equivalent outcomes noted and no nodal failures despite no requirement for completion TME in the LE group for poor treatment response.
Garcia-Aguilar J, Renfro LA, Chow OS, Shi Q, Carrero XW, Lynn PB, et al. Organ preservation for clinical T2N0 distal rectal cancer using neoadjuvant chemoradiotherapy and local excision (ACOSOG Z6041): results of an open-label, single-arm, multi-institutional, phase 2 trial. Lancet Oncol. 2015;16:1537–46.
Rullier E, Rouanet P, Tuech J-J, et al. Organ preservation for rectal cancer (GRECCAR 2): a prospective, randomised, open-label, multicentre, phase 3 trial. Lancet. 2017;390:469–79 Phase III study of T2-3 N0-1 M0 patients showing no difference in outcomes following LCRT for LE vs. TME, although completion TME was required for adverse pathologic features at LE. Following LCRT, QoL was worst in the completion TME group, followed by the upfront TME patients and then LE alone patients.
Rullier E, Vendrely V, Asselineau J, Rouanet P, Tuech JJ, Valverde A, et al. Organ preservation with chemoradiotherapy plus local excision for rectal cancer: 5-year results of the GRECCAR 2 randomised trial. Lancet Gastroenterol Hepatol. 2020;5:465–74.
Vallam KC, Engineer R, Desouza A, Patil P, Saklani A. High nodal positivity rates even in good clinical responders after chemoradiation of rectal cancer: is organ preservation feasible? Color Dis. 2016;18:976–82.
Baucom RB, Maguire LH, Kavalukas SL, Geiger TM, Ford MM, Muldoon RL, et al. Nodal disease in rectal cancer patients with complete tumor response after neoadjuvant chemoradiation: danger below calm waters. Dis Colon Rectum. 2017;60:1260–6.
Creavin B, Ryan E, Martin ST, Hanly A, O’Connell PR, Sheahan K, et al. Organ preservation with local excision or active surveillance following chemoradiotherapy for rectal cancer. Br J Cancer. 2017;116:169–74.
Dindo D, Demartines N, Clavien P-A. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13.
Lynn PB, Strombom P, Garcia-Aguilar J. Organ-preserving strategies for the management of near-complete responses in rectal cancer after neoadjuvant chemoradiation. Clin Colon Rectal Surg. 2017;30:395–403.
Habr-Gama A, Lynn PB, Jorge JMN, Sao Juliao GP, Proscurshim I, Gama-Rodrigues J, et al. Impact of organ-preserving strategies on anorectal function in patients with distal rectal cancer following neoadjuvant chemoradiation. Dis Colon Rectum. 2016;59:264–9.
Mcmullen C, Liu L, Bulkley JE, Hornbrook MC, Wendel C, Grant M, et al. Participation in activities associated with quality of life for long-term survivors of rectal cancer. Perm J. 2017;21:16–011.
Hupkens BJP, Martens MH, Stoot JH, Berbee M, Melenhorst J, Beets-Tan RG, et al. Quality of life in rectal cancer patients after chemoradiation: watch-and-wait policy versus standard resection - a matched-controlled study. Dis Colon Rectum. 2017;60:1032–40 Matched controlled study of 41 patients who received NOM vs. 41 who received chemoradiation and surgery after minimum f/u of 2 years, with the NOM group having improved QoL in numerous domains based on validated questionnaires although significant side effects noted in each group.
Keane C, O’Grady G, Bissett I, Woodfield J. Comparison of bowel dysfunction between colorectal cancer survivors and a non-operative non-cancer control group. Color Dis. 2020;22:806–13.
Quezada-Diaz FF, Smith JJ, Jimenez-Rodriguez RM, Wasserman I, Pappou EP, Patil S, et al. Patient-reported bowel function in patients with rectal cancer managed by a watch-and-wait strategy after neoadjuvant therapy: a case-control study. Dis Colon Rectum. 2020;63:897–902.
Miller JA, Wang H, Chang DT, Pollom EL. Cost-effectiveness and quality-adjusted survival of watch and wait after complete response to chemoradiotherapy for rectal cancer. J Natl Cancer Inst. 2020;112:792–801 Markov decision analysis showing improved quality adjusted life years (QALYs) and decreased costs with comparable oncologic outcomes with NOM as compared to neoadjuvant CRT followed by surgery.
de Buck van Overstraeten A, Khorasani S, Kennedy E, Look Hong NJ. Nonoperative management versus radical surgery of rectal cancer after neoadjuvant therapy-induced clinical complete response: a Markov decision analysis. Dis Colon Rectum. 2020;63:1080–9.
Sclafani F, Brown G, Cunningham D, Wotherspoon A, Mendes LST, Balyasnikova S, et al. Comparison between MRI and pathology in the assessment of tumour regression grade in rectal cancer. Br J Cancer. 2017;117:1478–85.
van der Sande ME, Maas M, Melenhorst J, Breukink SO, van Leerdam ME, Beets GL. Predictive value of endoscopic features for a complete response after Chemoradiotherapy for rectal Cancer. Ann Surg. 2019. https://doi.org/10.1097/SLA.0000000000003718.
Nagtegaal ID, Glynne-Jones R. How to measure tumour response in rectal cancer? An explanation of discrepancies and suggestions for improvement. Cancer Treat Rev. 2020;84:101964.
Perez RO, Habr-Gama A, Pereira GV, Lynn PB, Alves PA, Proscurshim I, et al. Role of biopsies in patients with residual rectal cancer following neoadjuvant chemoradiation after downsizing: can they rule out persisting cancer? Color Dis. 2012;14:714–20.
van der Sande ME, Beets GL, Hupkens BJ, Breukink SO, Melenhorst J, Bakers FC, et al. Response assessment after (chemo)radiotherapy for rectal cancer: why are we missing complete responses with MRI and endoscopy? Eur J Surg Oncol. 2019;45:1011–7.
Liu S, Zhong G-X, Zhou W-X, Xue HD, Pan WD, Xu L, et al. Can endorectal ultrasound, MRI, and mucosa integrity accurately predict the complete response for mid-low rectal cancer after preoperative chemoradiation? A prospective observational study from a single medical center. Dis Colon Rectum. 2018;61:903–10.
Sao Juliao GP, Ortega CD, Vailati BB, Habr-Gama A, Fernandez LM, Gama-Rodrigues J, et al. Magnetic resonance imaging following neoadjuvant chemoradiation and transanal endoscopic microsurgery for rectal cancer. Color Dis. 2017;19:O196–203.
Hupkens BJP, Maas M, Martens MH, et al. Organ preservation in rectal cancer after chemoradiation: should we extend the observation period in patients with a clinical near-complete response? Ann Surg Oncol. 2018;25:197–203 Retrospective analysis of 102 patients found > 90% of patients with a near cCR 8-10 weeks after CRT will achieve a cCR 6–12 weeks later.
Habr-Gama A, Sao Juliao GP, Fernandez LM, Vailati BB, Andrade A, Araujo SEA, et al. Achieving a complete clinical response after neoadjuvant chemoradiation that does not require surgical resection: it may take longer than you think! Dis Colon Rectum. 2019;62:802–8. https://doi.org/10.1097/DCR.0000000000001338.
Sammour T, Price BA, Krause KJ, Chang GJ. Nonoperative management or “watch and wait” for rectal cancer with complete clinical response after neoadjuvant chemoradiotherapy: a critical appraisal. Ann Surg Oncol. 2017;24:1904–15.
Gani C, Kirschniak A, Zips D. Watchful waiting after radiochemotherapy in rectal cancer: when is it feasible? Visc Med. 2019;35:119–23.
Gani C, Grosse U, Clasen S, Kirschniak A, Goetz M, Rodel C, et al. Cost analysis of a wait-and-see strategy after radiochemotherapy in distal rectal cancer. Strahlenther Onkol. 2018;194:985–90.
Song K-S, Park SC, Sohn DK, et al. Oncologic risk of rectal preservation against medical advice after chemoradiotherapy for rectal cancer: a multicenter comparative cross-sectional study with rectal preservation as supported by surgeon. World J Surg. 2019;43:3216–23.
Oh BY, Huh JW, Lee WY, Park YA, Cho YB, Yun SH, et al. Are we predicting disease progress of the rectal cancer patients without surgery after neoadjuvant chemoradiotherapy? Cancer Res Treat. 2018;50:634–45.
Maas M, Lambregts DMJ, Nelemans PJ, et al. Assessment of clinical complete response after chemoradiation for rectal cancer with digital rectal examination, endoscopy, and MRI: selection for organ-saving treatment. Ann Surg Oncol. 2015;22:3873–80 Prospective cohort study of 50 patients that assessed likelihood of determining cCR based on DRE, endoscopy, T2W-MRI, and DWI 6–8 weeks after CRT with best accuracy noted with combined modality approach.
Sao Juliao GP, Karagkounis G, Fernandez LM, Habr-Gama A, Vailati BB, Dattani M, et al. Conditional survival in patients with rectal cancer and complete clinical response managed by watch and wait after chemoradiation: recurrence risk over time. Ann Surg. 2020;272:138–44.
Stijns RCH, de Graaf EJR, Punt CJA, Nagtegaal ID, Nuyttens JJME, van Meerten E, et al. Long-term oncological and functional outcomes of chemoradiotherapy followed by organ-sparing transanal endoscopic microsurgery for distal rectal cancer: the CARTS study. JAMA Surg. 2019;154:47–54.
van Heeswijk MM, Lambregts DMJ, Palm WM, Hendriks BMF, Maas M, Beets GL, et al. DWI for assessment of rectal cancer nodes after chemoradiotherapy: is the absence of nodes at DWI proof of a negative nodal status? AJR Am J Roentgenol. 2017;208:W79–84.
Santiago I, Barata M, Figueiredo N, Pares O, Henriques V, Galzerano A, et al. The split scar sign as an indicator of sustained complete response after neoadjuvant therapy in rectal cancer. Eur Radiol. 2020;30:224–38.
Wo JY, Anker CJ, Ashman JB, et al. Radiation therapy for rectal cancer: executive summary of an ASTRO clinical practice guideline. Pract Radiat Oncol. 2020. https://doi.org/10.1016/j.prro.2020.08.004.
Russo S, Anker CJ, Abdel-Wahab M, Azad N, Das P, Dragovic J, et al. Executive summary of the American Radium Society Appropriate Use Criteria for Local Excision in Rectal Cancer. Int J Radiat Oncol Biol Phys. 2019;105:977–93.
Garcia-Aguilar J, Patil S, Kim J. Preliminary results of the organ preservation of rectal adenocarcinoma (OPRA) trial. J Clin Oncol. 2020;38(suppl; abstr 4008).
Smith JJ, Chow OS, Gollub MJ, et al. Organ preservation in rectal adenocarcinoma: a phase II randomized controlled trial evaluating 3-year disease-free survival in patients with locally advanced rectal cancer treated with chemoradiation plus induction or consolidation chemotherapy, and total mesorectal excision or nonoperative management. BMC Cancer. 2015;15:767.
Acknowledgments
We would like to thank Rebecca Wilcox, MD, Director of Gastrointestinal Pathology at the University of Vermont, for her thorough read of this manuscript’s first draft.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Radiation Therapy and Radiation Therapy Innovations in Colorectal Cancer
Appendices
Appendix 1. Literature search strategy for non-operative management (NOM) of rectal adenocarcinoma

Appendix 2. Study selection flowsheet for the non-operative treatment (NOM) of rectal adenocarcinoma

Appendix 3
Rights and permissions
About this article
Cite this article
Anker, C.J., Akselrod, D., Ades, S. et al. Non-operative Management (NOM) of Rectal Cancer: Literature Review and Translation of Evidence into Practice. Curr Colorectal Cancer Rep 17, 23–41 (2021). https://doi.org/10.1007/s11888-020-00463-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11888-020-00463-2