Abstract
Background
Despite screening initiatives, rectal cancer remains one of the most prevalent malignancies diagnosed in patients worldwide with a high mortality. The introduction of neoadjuvant therapy has resulted in a paradigm shift in the treatment and outcomes of rectal cancer. Surgeons play an intricate role in the pre-operative, operative, and post-operative management of these patients.
Purpose
The purpose of this comprehensive literature review was to summarize the evolution of the use chemotherapy and radiation and the process of differentiation into specific neoadjuvant chemoradiation protocols in the treatment of locally advanced rectal cancer. This will provide a concise summary for practicing surgeons of the current evidence for neoadjuvant chemoradiation as well as the various implications of therapy on operative outcomes.
Conclusion
The initial benefit of adjuvant therapy in the treatment of rectal cancer patients became evident with prospective studies demonstrating improvements in various oncologic survival outcomes. Due to the improved compliance and reduced toxicity, as well as the potential for tumor down-staging and sphincter preservation, neoadjuvant approaches became the preferred method of administering chemotherapy and radiation. Furthermore, a subgroup of patients has been shown to present with complete clinical response to neoadjuvant therapy. This has resulted in the development of the non-operative “watch and wait” approach, which has initiated discussions on changing the interval from the completion of neoadjuvant therapy to surgical resection. The continued development of the multidisciplinary approach will only further improve our ability to provide patients with the best possible oncologic outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neoadjuvant chemoradiotherapy (NACRT) has become the standard of care in the treatment of locally advanced rectal cancer. National guidelines have included recommendations for the use of various chemoradiation regimens in order to try to decrease rates of local recurrence, with the potential to improve overall survival in this patient population [1].
Prior to the advent of perioperative chemotherapy or radiation, recurrence rates were as high as 40 % in patients with locally advanced rectal cancers [2]. In the majority of these studies, locally advanced disease was defined as extension through the muscularis propria (T3) and/or lymph node positive disease (N1+). This problem initiated two movements that seemed to develop with the intention of addressing these recurrence rates. Richard “Bill” Heald from Basingstoke, UK, improved the surgical approach to a proctectomy with the advent of the total mesorectal excision (TME) [3], while other authors began to focus on the use of adjuvant measures of chemotherapy and radiation, specifically in the post-operative period [4–6].
The evidence for adjuvant therapy
Initial efforts to study the effects of adjuvant chemotherapy and radiation were demonstrated in various trials. Chronologically, the Gastrointestinal Tumor Study Group (GTSG 7175) was the first to publish the findings of a trial in which patients were randomized to one of four groups: no adjuvant therapy, adjuvant chemotherapy with 5-fluorouracil (5-FU) and semustine, adjuvant radiation between 4000 and 4800 rad or a combination of chemotherapy and radiation. A total of 202 of 227 randomized patients were analyzed. A significant decrease in overall recurrences was seen in the adjuvant chemotherapy and radiation group (33 %) as compared to the control group (55 %; p = 0.04) with an associated prolongation in time to tumor recurrence. Despite the improvement in recurrence-free survival, overall survival was not found to be different between the groups. Interestingly, local recurrence rates were found to be lowest in the chemoradiation group (11 %) when compared with radiation alone (20 %), with no observed impact identified in the chemotherapy and surgery alone groups (27 vs 24 %, respectively) [7]. Multiple randomized trials followed investigating various patterns of adjuvant treatment. The National Surgical Adjuvant Breast and Bowel Program 3-arm trial (NSABP R-01) compared surgery alone with adjuvant radiation or adjuvant chemotherapy as single independent adjuvants. Patients treated with adjuvant chemotherapy were found to have an improvement in disease-free survival (DFS; p = 0.006), although no difference in local or distant recurrence rates was observed. Interestingly, patients treated with adjuvant radiation were found to have a significant decrease in local recurrence rates from 25 to 16 %, with no observed difference in overall survival. However, the first trial to demonstrate a benefit of adjuvant chemoradiation on local recurrence rates as well as 5-year overall survival and DFS was the North Central Cancer Treatment Group (NCCTG 794751) trial in which patients were randomized to either surgery alone or adjuvant chemoradiation [5]. In this study, full-dose chemotherapy was used both before and after combined chemoradiation in an attempt to decrease distant metastases. The Norwegian Adjuvant Rectal Cancer Project Group followed in designing a study whereby patients were randomized to either surgery alone or with adjuvant chemoradiation. Chemotherapeutic treatment differed in this trial in that 5-FU was administered only in bolus form, concomitantly with external beam radiation therapy (EBRT) with no form of maintenance chemotherapy. Significant decreases in local recurrence rates to as low as 12 % in the chemoradiation group as compared to 30 % in the surgery alone group were observed. Despite the use of bolus 5-FU, a significant benefit in overall survival was observed (64 vs 50 % in the surgery along group; p = 0.01) [8].
The evidence for a total mesorectal excision
Various pathological assessments of rectal cancers and mesorectal disease have demonstrated and outlined the patterns of lymphatic drainage and metastatic spread [9]. Well-designed pathological studies have postulated that one of the major causes of pelvic or local recurrence of rectal cancer is the persistence of tumor foci within parts of a retained mesorectum [10, 11]. Initial attempts to address this issue prior to the availability of these hypotheses were pioneered by Dr. Heald, with the first description of the TME in 1982 [3]. With this technique, rates of local recurrence as low as 5 to 10 % were described, independent of the administration of adjuvant therapy. The need for a complete resection of the mesorectal specimen emphasizes the importance of pre-operative evaluation of the mesorectal circumferential resection margin (CRM) with various imaging modalities.
The evidence for neoadjuvant therapy
Initial efforts to further improve rates of local control and increase rates of sphincter preservation led many investigators to further assess the potential advantages of NACRT. These included tumor down-staging allowing for ease of resectability, decreased rates of small bowel irradiation, and decreased rates of anastomotic irradiation, both of which result in significant functional issues in this patient population [12]. However, studies have varied in terms of the amount of radiation administered to the tumor bed. A dose-dependent response was demonstrated by Gray and colleagues in their systematic review where NACRT were found to be associated with significantly improved rates of local recurrence and overall survival as long as a minimal dose of 30 Gy is administered to the tumor bed [13].
Oncological outcomes
A recurring theme in studies that have assessed the oncological benefits of neoadjuvant therapy in the treatment of rectal cancer have demonstrated improvements in local control, although with inconsistent benefits in the areas of disease-free and overall survival. Three of the earliest large-scale randomized trials to assess the role of neoadjuvant therapy were the German Rectal Cancer Trial, the Swedish Rectal Cancer Trial, and the Dutch TME trial. Each assessed the role of neoadjuvant therapy based on different interventional parameters, surgical technique, and stages of disease. In the Swedish phase III trial, 1186 patients with Dukes A, B, or C rectal cancer were randomized to either pre-operative short-course radiation (5 Gy daily for 5 days) with subsequent surgery or surgery alone. In this trial, there was no standardization of surgical technique, although time was taken to ensure clear margins had been obtained by the surgeons involved. A significantly lower rate of local recurrence was observed in patients treated with the neoadjuvant regimen (11 vs 27 %; p < 0.001). With a median follow-up of 75 months (range 60–96 months), the 5-year overall survival was found to be 58 % in the neoadjuvant therapy group as compared with 48 % in the surgery alone group (p = 0.004). Additionally, an improvement in cancer-specific survival was observed at 9 years (74 vs 65 %; p = 0.002). In this study, the authors comment that the use of a standardized technique to optimize surgical resection may help address variations that could emanate from differences in the quality of resection. Furthermore, an attempt was made to discuss the potential benefits to their wide inclusion criteria of Dukes staged rectal cancers in indicating that a proportional reduction of local recurrence rates occurred in all Dukes stages [14].
Subsequently, two main trials went on to assess the role of neoadjuvant therapy in the era of the TME dissection. The Dutch TME trial then went on to randomize patients with resectable rectal cancer to either a short course of neoadjuvant radiation followed by surgery vs surgery alone. Interestingly, almost half of the patients had early stage disease. Despite this fact, the local recurrence rates were observed to be 8.4 % in the control group as compared to 2.4 % in the interventional group (p < 0.001), with no benefit in overall survival [15]. Twelve-year follow-up data revealed a persistence of lower local recurrence rates in the neoadjuvant therapy group at 5 % as compared to 11 % in the control group (p < 0.0001) [16]. The German Rectal Cancer Trial went on to randomize 423 patients to pre-operative vs post-operative chemoradiation therapy in patients with stage II and III rectal cancers. In this study, the authors were careful in their attempts to ensure an appropriate TME had been performed and as such stratified by surgeon during the randomization process. Significant improvements in local recurrences (6 vs 13 %; p = 0.006), chemotherapy-associated toxicity (27 vs 40 %; p = 0.01), and rates of sphincter preservation were observed in patients treated with NACRT. No difference in overall survival was identified between the two groups [17]. Furthermore, 10-year follow-up data demonstrated the advantage in local control to persist with no continued difference in overall survival [18].
The European Organization for Treatment of Cancer Radiotherapy Study group trial (EORTC 22921) published the results of a multi-arm randomized controlled trial in which patients with a known diagnosis of a T3/T4 rectal cancer were randomized to one of several arms of adjuvant therapy. These arms included pre-operative radiotherapy, pre-operative chemoradiotherapy, pre-operative radiotherapy with post-operative chemotherapy, and pre-operative chemoradiotherapy with post-operative chemotherapy. In this trial, pre-operative radiotherapy consisted of long-course radiation with 45 Gy distributed in 25 fractions over 5 weeks. Although the trial had started recruitment in 1993, a TME dissection was only recommended as of 1999. As such, between 35 to 40 % of patients in each arm received a TME dissection. After the randomization of 1011 patients, the authors found that regardless of the addition of chemotherapy in the neoadjuvant or adjuvant settings, no difference was found in overall survival. However, the addition of chemotherapy to neoadjuvant radiotherapy was found to confer a significant benefit in local control. At 5 years, local recurrences were highest in the pre-operative radiotherapy alone at 17.1 %, whereas pre-operative chemoradiotherapy and post-operative chemotherapy conferred the strongest local control advantage with a 5-year local recurrence rate of 7.6 %. This treatment effect was noted to be homogenous regardless of the height within the rectum at which the tumor was identified (≤5 vs >5 cm; p = 0.74) [19].
However, one of the questions that remained unanswered was the oncological outcome of pre-operative radiation therapy as compared with surgery and adjuvant therapy when indicated in the era of the TME dissection. One of the largest prospective randomized trials that took place during this time in addition to the increased rigor in circumferential resection margin analysis was the MRC CR07 (combined with the NCIC-CTG C016) trial. The authors randomized all patients with resectable rectal cancer, regardless of stage, to either standard short-course neoadjuvant radiation therapy followed by surgery compared to immediate surgery with adjuvant chemoradiation when indicated by a positive CRM (≤1 mm). The primary outcome of 5-year local recurrence was significantly lower in the pre-operative radiotherapy group (4.7 vs 11.5 %; p < 0.0001). Although there was no detectable difference in overall survival at 5 years, an improvement in disease-free survival was seen in the pre-operative radiotherapy group (73.6 vs 66.7 %; p = 0.013) [20].
Outcomes with varying the type of chemotherapy
Recently, oral capecitabine has been demonstrated to be an equivalent substitute for infusional 5-FU chemotherapy administered in the neoadjuvant setting. Capecitabine is a fluoropyrimidine derivative of 5-FU that has been found to be equivalent in efficacy with a favorable adverse event profile, when compared to 5-FU/folinic acid in the adjuvant treatment of stage III colon cancer [21]. In the NSABP-R04 study, capecitabine, with or without oxaliplatin, was compared to infusional 5-FU with or without oxaliplatin in the neoadjuvant treatment of stage II and III rectal cancers, when combined with radiation. The use of oxaliplatin was found to increase the rates of toxicity, whereas the use of either oral capecitabine or infused 5-FU was not found to affect sphincter preservation and pathological complete responsiveness rates. Furthermore, no difference in the rates of tumor down-staging was observed [22]. This finding was further established in a phase 3, non-inferiority designed randomized controlled trial in patients with stage II and III rectal cancer where 5-FU or capecitabine chemoradiation was administered. Although patients in this trial received their chemoradiation in either the pre- or post-operative setting, capecitabine was found to be non-inferior to 5-FU with regard to 5-year overall survival, with a significant improvement in disease-free survival observed in patients receiving capecitabine (75.2 vs 66.6 %; p = 0.034) [23].
Induction chemotherapy, prior to chemoradiotherapy, has also been investigated in various forms in order to address the risks of systemic disease in more aggressive primary tumors. One of the earliest trials to investigate this assessed the use of 5-FU with concurrent mitomycin-C in the context of neoadjuvant radiotherapy with optimistic results [24]. However, in the era of chemotherapeutic agents with more specific activity against colorectal malignancies, various non-randomized trials have demonstrated a significant benefit of FOLFOX (5-FU/Folinic acid/Oxaliplatin) and CapeOx (Capecitabine and Oxaliplatin) in tumor down-staging, with no demonstrable concern of tumor progression [25, 26]. In order to test this, Maréchal and colleagues conducted a trial in which patients with locally advanced rectal cancers were randomized to the control of neoadjuvant chemoradiation with radiosensitizing infusional 5-FU vs short-course induction FOLFOX chemotherapy (2 cycles) followed by neoadjuvant chemoradiation as performed in the control arm. Fifty-seven patients were randomized after which the trial was closed prematurely due to futility. No difference was identified in the ypT0-1 N0 rates between groups and, furthermore, an increase in toxicity was identified in patients treated with induction therapy (35 vs 7 %; p = 0.017) [27]. However, these concerns regarding toxicity have been observed in a more pronounced fashion when chemotherapy is administered in the adjuvant setting. As an example, in the Spanish GCR-3 trial, patients with a locally advanced rectal cancer were randomized to induction CapeOx with neoadjuvant radiotherapy as compared to the intervention of NACRT with induction CapeOx followed by adjuvant CapeOx therapy. Although no differences were identified in either 5-year disease-free survival rates or local recurrence rates, a significantly higher rate of grade 3 and 4 toxicity (Common Terminology Criteria for Adverse Events, Version 3.0) was identified in the interventional group (54 %) as compared to those treated neoadjuvantly alone (19 %). Furthermore, the percentage of patients completing the entire cycle of therapy was higher in those not receiving adjuvant therapy (94 vs 57 %) [28].
Various randomized trials have been performed to investigate the role the addition of neoadjuvant oxaliplatin may have on affecting oncologic outcomes. The ACCORD (Actions Concertées dans les Cancers Colorectaux et Digestifs) 12 trial aimed to compare neoadjuvant capecitabine (CAP) with neoadjuvant capecitabine and oxaliplatin (CapeOx) in patients receiving long-course neoadjuvant radiotherapy (45–50 Gy over 5 weeks) for locally advanced rectal cancers (T3-4NxMO), followed by TME surgery [29]. After randomizing 598 patients, no difference was identified in the rate of pathological complete response (pCR) between groups (CAP 13.9 vs 19.2 %; p = 0.09). Furthermore, no difference was identified in overall survival, disease-free survival, and local recurrence in each group at 3 years. Other trials with similar designs have failed to show any benefits in rates of pCR, disease-free or overall survival thus questioning the role, if any, of adding oxaliplatin to neoadjuvant regimens [22, 30].
Outcomes with varying the technique of radiotherapy
Although studies have varied in their use of various established radiotherapy regimens in the neoadjuvant setting, few studies have compared these two approaches in a head to head fashion. Long-course, conventional therapy includes the administration of a total of 45 Gy of radiation over 20–25 fractions divided over a course of 5 to 6 weeks with the potential for an additional boost to the tumor bed of approximately 5.4 Gy. Short-course therapy is usually characterized by the administration of 25 Gy of radiotherapy in 5 Gy fractions over 5 days followed by surgery 1 week later. Various benefits have been proposed to each approach. Short-course therapy has been found to be less costly and associated with lower rates of early toxicity, although with the chance for delayed toxicity [17, 31, 32].
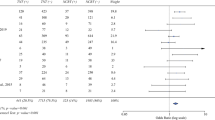
Given the equipoise that exists in the literature surrounding these approaches, the Polish Colorectal Study Group established a randomized trial comparing the two forms of therapy. After 312 patients with locally advanced rectal cancers were randomized to either short-course neoadjuvant radiotherapy vs neoadjuvant long-course radiotherapy and 5-FU/Folinic acid, follow-up was conducted to a median of 48 (range 31–69) months. The study’s findings failed to show any oncologic benefit in the area of local recurrence (9 vs 14.2 %; p = 0.17), disease-free survival (58.4 vs 55.6 %; p = 0.82), and overall survival (67.2 vs 66.2 %; p = 0.96) in the short- and long-course groups. Early radiation toxicity was expectedly higher in the long-course group (18.2 vs 3.2 %; p < 0.001) [33]. These findings were echoed by the Tran-Tasman Radiation Oncology Group trial (TROG-01.04) where no difference in overall and disease-free survival, local recurrence, and incidence of late toxicity were identified [34]. More recently, Lautkauskas and colleagues conducted a trial investigating the tumor down-staging effects of short- vs long-course neoadjuvant radiotherapy. The authors report a smaller tumor size in patients reassessed following long-course chemoradiation (2.5 vs 3.3 cm; p = 0.04), with a trend towards higher pCR rates (39.1 vs 21.6 %; p = 0.07) [35]. To further corroborate these findings, a recently published meta-analysis of randomized and non-randomized controlled trials demonstrated the lack of any difference in local recurrence, disease-free, and overall survival rates in patients treated with short- or long-course radiotherapy for locally advanced rectal cancers. Despite finding an increase in the rate of grade 3–4 toxicity in patients treated with long-course radiotherapy (RR: 0.13, p < 0.00001), no difference was demonstrated in the rates of long-term toxic effects of treatment [36]. The authors also demonstrate a higher rate of pCR in the long-course radiotherapy group (RR 0.15; p = 0.003).
Toxicity and compliance with neoadjuvant therapy
The turn towards neoadjuvant therapy in the 1990s was based on many presumed benefits, one of which was the potentially improved patient compliance with treatment regimens [37]. In one of the earliest studies, Pahlman and colleagues began comparing pre-operative radiation to post-operative regimens and demonstrated significant improvements in the patients’ ability to tolerate the entire therapeutic treatment plan as compared to those in the adjuvant therapy group [38]. This result was further substantiated as one of the many benefits of neoadjuvant therapy in addition to the potential for tumor down-staging and the theorized increased effect on well-oxygenated tissue [12]. The comparative tolerance of and toxicity rates with short- and long-course regimens has been described in various randomized trials which we have discussed above [33–35]. Furthermore, Zhou and colleagues conducted a comprehensive meta-analysis comparing the various outcomes of trials using short- and long-course radiation therapy in the treatment of rectal cancers. Their assessment was divided into acute and long-term toxicity, although one would assume the acute effects of therapy to be the only form to affect compliance. When analyzing the outcomes in all grades of toxicity, their analysis was limited because of the significant heterogeneity of patients. Their initial, statistically appropriate, random effects comparison failed to reveal a significant difference in all grades of toxicity between the groups; this difference subsequently became significant when using a fixed effects model suggesting higher rates of toxicity of all grades with long-course therapy (RR 0.06, 95 % CI 0.02–0.16, p < 0.00001). One is therefore limited in the utility of these results. Evaluation of the higher grades of toxicity (3 and 4) between groups was undertaken by meta-analysis of a total of 1435 patients from 6 trials, demonstrating minimal patient heterogeneity and a significantly higher rate of acute toxicity in the long-course therapy group (RR 0.13 95 % CI 0.06–0.28, p < 0.00001) [36].
The EORTC trial allowed for a comparative assessment of toxicities to therapy in patients randomized to various groups involving pre- and post-operative therapy. It was demonstrated that adherence rates to the protocol were high with relatively low toxicity rates, depending on the randomization group. Radiotherapy was well tolerated with adherence rates of 98 % in patients receiving radiotherapy alone as compared to 95.5 % in patients receiving combination chemoradiotherapy. The authors demonstrated that 82 % of patients were able to tolerate and adhere to neoadjuvant fluorouracil infusions as compared to only 42.9 % in the adjuvant setting, of which 25 % had refused further therapy [19]. This can potentially be explained by the lower rate of grade 2 or higher toxicity observed in patients treated neoadjuvantly as compared to the adjuvant therapy groups. These findings are echoed by other trials that have investigated the role of neoadjuvant therapy. In a recent Cochrane review comparing neoadjuvant radiation with NACRT, a significant increase in grade 3 and 4 toxicity was observed with an OR of 1.68–10 (p < 0.002) in patients receiving chemoradiation. Despite this fact, chemotherapy adherence rates remained relatively high [39].
The addition of oxaliplatin to neoadjuvant regimens has been the subject of various randomized trials with minimal demonstrable oncologic benefits [22, 29, 30]. Although many of these studies commented on slightly increased rates of toxicity in patients receiving oxaliplatin, one study went further to comment on differences in compliance to therapy [30]. In this study, the addition of oxaliplatin to the neoadjuvant therapy appeared to affect compliance with both radiation and fluorouracil infusions. As an example, 84 % of patients receiving combined oxaliplatin were able to complete their full dose of radiotherapy as compared to 92 % of patients in the control group without oxaliplatin therapy. Similar differences were seen with compliance to 5-FU infusions with only 69 % of patients completing all 6 cycles in the intervention group as compared to 84 % of controls.
Surgery-related outcomes following neoadjuvant therapy: sphincter preservation rates
Sphincter preservation (SP) rates have been reported in a number of trials as one of the patient-centered outcomes of choice given the strong association observed in quality of life studies [40]. Studies have demonstrated obvious improvements in the rates of SP that have occurred over the course of the past few decades. Earlier reports demonstrated rates of abdominoperineal resection as high as 90 % when investigating the effects of neoadjuvant therapy in rectal cancer [41]. The applicability of such results is minimal given the changes that have occurred in surgical technique with the development of the TME dissection, the timing of surgery, as well as the changes in neoadjuvant therapy. In a review of various centers associated with the National Comprehensive Cancer Network, it was found that rates of SP in patients managed for rectal cancer were as high as 77 %. The authors attributed this high rate of SP to various factors including the availability of specialty centers with expertise in rectal surgery as well as techniques that have made rectal surgery easier such as laparoscopy and newer stapling devices [42]. Furthermore, the change in dogma that distal resection margins of <2 and >3 cm does not result in any differences in local recurrence and overall survival has likely encouraged surgeons to perform a colorectal or coloanal anastomosis when they otherwise would not have [43, 44].
Some initial reports and reviews have suggested an improved rate of sphincter preservation with neoadjuvant chemoradiotherapy as compared to adjuvant therapy [45]. Multiple studies have investigated this as a secondary outcome in trials designed for another primary outcome variable; however, few have been designed for the primary outcome of SP [31, 46]. In the Lyon R90-01 trial, the authors investigated the effect of varying intervals from neoadjuvant therapy to surgery by randomizing 201 patients to either surgery within 2 weeks or 6–8 weeks after the completion of radiotherapy and the effect on SP. Despite identifying an improvement in pathological down-staging in patients operated on following a longer interval from neoadjuvant radiotherapy, no difference was identified in the rate of SP between groups (long interval 76 % vs short interval 68 %; p = 0.27) [46]. Similarly, the Polish trial that compared short- and long-course neoadjuvant radiotherapy on the primary outcome of SP failed to demonstrate any difference between each group. More recently, a systematic review of the role of neoadjuvant therapy on sphincter preservation was published, reporting data from 17 trials including the two aforementioned studies [47]. Unfortunately, as demonstrated by the authors, the trials are significantly heterogeneous which compromises the ability to perform a meta-analysis of the results. This heterogeneity exists in areas of the surgical technique, the method of radiation therapy, the type and volume of chemotherapy, as well as the interval to surgery. Despite demonstrating improved rates of pCR of up to 16 to 19 % in some of the most recent trials, no benefit was observed in SP rates in patients treated with external beam radiation therapy (EBRT) and chemotherapy [29, 30].
Many hypotheses have been expressed to explain the reasons for which previous randomized trials have failed to demonstrate a difference in the outcome of SP following neoadjuvant therapy. One major reason is that many surgeons have previously expressed reluctance to veer from the originally planned procedure upon initial assessment of a patient prior to neoadjuvant therapy. Furthermore, the majority of these trials were performed at a time when distal resection margins of >2 cm had been suggested or prior to the advent of the intersphincteric proctectomy. Many oncologists have also theorized a benefit to high doses of radiation to the tumor given the proposed radiation dose-tumor response relationship often mentioned [48]. The Lyon R96-02 trial was performed to address the role of boost endoluminal contact radiotherapy (CRT) may have in affecting outcomes in patients with locally advanced rectal cancers. After randomizing 88 patients to the EBRT (total 39 Gy over 17 days) or EBRT with boost CRT (84 Gy in three fractions), the authors reported a significant increase in the primary outcome of SP in the CRT group (76 vs 44 %; p = 0.004). Unfortunately, this technology is not as widely available or frequently used internationally, although it is the subject of further study.
Surgery-related outcomes following neoadjuvant therapy: anastomotic concerns
Anastomotic leak (AL) rates have been reported in the literature to occur in 1 to 30 % of rectal resections, with the highest rates occurring in low colorectal or coloanal anastomoses [49–52]. This post-operative complication represents one of the most concerning potential morbidities that occur in this patient population for a variety of reasons including poorer gastrointestinal function and quality of life [53, 54], increased rate of recurrence [55, 56], and decreased frequency of ultimate sphincter preservation [57].
As has been discussed above, multiple randomized controlled trials have been performed examining the various permutations of perioperative therapy in locally advanced rectal cancers. In a Cochrane review of the literature, insufficient data was available to meta-analyze from randomized controlled trials when it came to the outcome of AL and dehiscence [58]. De Caluwé and colleagues performed an updated review in 2013 whereby no significant effect of NACRT was identified on the rates of AL. It should be emphasized that this endpoint was not the primary outcome of these studies and, as such, the studies were likely insufficiently powered to identify a difference. Additionally, the occurrence of this outcome is quite low, and therefore, an exceptionally high number of patients would be required in a randomized trial to be appropriately powered to detect such a difference. Interestingly, in a separate meta-analysis, Qin and colleagues demonstrate the same conclusion despite stratification of the trials by method of neoadjuvant therapy, whether purely radiotherapy or combined NACRT.
However, observational data do exist with larger patient sample sizes and appropriate, bias-reducing analyses and have been performed to bypass the concerns of inadequate power. Unfortunately, the literature remains somewhat vague in this area. Although some smaller observational trials have demonstrated a significant increase in AL rates with NACRT [59–61], Chang and colleagues were able to demonstrate through a larger, statistically sound analysis that this did not appear to be the case [62]. The authors performed a propensity score matched analysis in 1437 patients comparing the primary endpoint of anastomotic leak rates between patients treated with and without neoadjuvant chemoradiotherapy; after controlling for differences in known baseline variables, the authors failed to demonstrate a difference in AL rates between the two groups (7.5 and 8.1 %; p = 0.78). As it stands, there is an insufficient amount of evidence to conclude that any association exists between the use of neoadjuvant chemoradiotherapy and AL. Larger and more adequately powered studies would be needed. Furthermore, given that most of these patients are diverted, uncensored data from after the first 30-day post-operative period would be important to obtain given the continued incidence and detection of AL more than 30-days post-operatively [63].
Surgery-related outcomes following neoadjuvant therapy: functional outcomes
Most studies that have assessed the functional outcomes that occur following rectal cancer surgery have focused on gastrointestinal functionality as well as general quality of life indices. A smaller subset has also looked into the potential implications on long-term bladder as well as sexual function; however, the issue also becomes more difficult to analyze due to the need for intraoperative preservation of the autonomic nerve plexuses [64]. Despite the large number of randomized trials that have investigated the role of various regimens of neoadjuvant therapy, few have done so with a standardized TME dissection protocol for participating surgeons. In the follow-up study to the Dutch trial, a comprehensive analysis was performed of various quality of life and functional outcomes for patients who had been randomized to either TME dissection or neoadjuvant short-course radiotherapy with subsequent TME dissection [65]. Although the authors demonstrated that no difference existed in the rates of urinary incontinence, there was a clear difference in the rates of fecal incontinence between groups. Patients without a stoma who had been treated with neoadjuvant radiation were found to have significantly higher rates of daytime and night incontinence, anal mucus loss, anal blood loss, and daily pad use. In a stratified analysis, the difference was found to exist mainly in patients with a primary lesion below 10 cm.
Sexual function has become an important part of the pre-treatment and pre-operative conversation in the management of patients with rectal malignancies. Various observational and randomized studies have demonstrated differences in the rates of sexual dysfunction in post-proctectomy patients [66–68], with additional analyses that have suggested an exacerbation of symptoms with radiotherapy. In a follow-up to a randomized trial, male and female patients treated with pre-operative short-course radiotherapy demonstrated higher rates of sexual dysfunction. Furthermore, male patients were specifically found to have higher incidences of ejaculatory and erectile dysfunction. These rates did not differ in patients with a SP procedure or an APR [67]. In a follow-up study from the MRC CR07/NCIC-CTG C016 trial, the authors found that the main adverse effect identified in male patients was sexual dysfunction; in these analyses, surgery, and not radiotherapy was found to be the principally associated cause [69]. Furthermore, these changes in sexual dysfunction were not found to resolve 3 years after surgery. The authors also concluded that their patients treated with radiotherapy did not appear to have any difference in gastrointestinal function or incontinence as compared to those treated with surgery alone. The study is limited by the varying completion rate of follow-up quality of life questionnaires and the potential for feedback bias. Given the scattered reports of associations between neoadjuvant therapy and quality of life indices, others have questioned whether there may be a difference in function based on the form of neoadjuvant radiation provided. In a large population level analysis, Bregendahl and colleagues demonstrated a 41 % rate of major dysfunction in patients following low anterior resection. Despite an increased risk of dysfunction in patients treated with neoadjuvant radiotherapy, no increased risk was demonstrable based on the form of neoadjuvant radiation administered [53]. A comprehensive meta-analysis of 25 observational and prospective trials involving 6548 patients revealed an increased rate of stool incontinence (RR 1.67, p < 0.00001) with worse manometric results in irradiated patients as assessed by mean resting and maximum squeeze pressures. Despite being reported by only a few studies, no significant effect of radiation was identified related to the incidence of sexual and urinary dysfunction indices [70].
Indications for neoadjuvant therapy in rectal cancer
After review of numerous studies that have investigated the role of NACRT in rectal cancer, it is evident that there is a definite heterogeneity in the indications for treatment. Earlier studies have included any resectable rectal cancer for consideration of NACRT [14, 15]; however, a number of studies have used pre-operatively staged T3/T4 tumors or node positivity [17, 19] as the inclusion criteria for therapy. More recently, there has been a gradual trend towards the pre-operative identification of a threatened CRM as an indication for NACRT, although this is more often used as an adjunct to the aforementioned indications. At present, there is no international consensus although many national associations have been developed to establish guidelines and quality measures in the treatment of rectal cancer.
Management of the patient post-neoadjuvant therapy
Optimizing patient outcomes post-neoadjuvant therapy
Despite the improved oncologic outcomes, recent data have demonstrated a significant deterioration in the physical fitness as well as the perioperative morbidity of patients following NACRT. Recent studies have relied upon cardiopulmonary surrogates, specifically oxygen uptake, measured prior to and during exercise in assessing the physical fitness of patients. West and colleagues performed a comprehensive prospective observational study in which decreases in the level of physical fitness were demonstrated in patients’ post-NACRT [71]. The authors subsequently introduced a structured responsive exercise-training program (SRETP) involving three sessions of exercise per week on a training bike, with assessments of surrogates of physical fitness. The authors demonstrated a significant improvement in the physical fitness of patients with this intervention [72]. Although this study was the first to investigate physical fitness changes in rectal cancer patients’ post-NACRT with subsequent improvement following SRETP, others have demonstrated the significant benefits of a pre-habilitation program in optimizing the perioperative and post-operative outcomes of surgical patients [73, 74]. Pre-habilitation programs are thus being gradually incorporated into various enhanced recovery pathways to improve patient outcomes.
Complete response rates and the “watch and wait” approach
Given the attempts to demonstrate a potential role of NACRT in sphincter preservation, a natural next step would be to assess the role of therapy in preserving the organ as a whole. Additionally, we have seen that patients treated with NACRT and surgery have clear differences in gastrointestinal function in addition to the high morbidity and oncologic implications of an anastomotic leak. However, for this to be an option, a complete absence of tumor on pathological assessment would be necessary to ensure rectal preservation. Many studies have reported complete tumor regression in the resected specimens of locally advanced rectal cancers treated with neoadjuvant therapy—termed a pathologic complete response (pCR) [75, 76]. Currently, clinical complete response (cCR) rates have been reported to occur in 11 and 28 % of patients [77]. The majority of series in the literature describe chemotherapy with either capecitabine or 5-FU/Folinic acid with long-course radiotherapy administering a total of 45–50.4 Gy over 25–28 fractions [78]. The majority of reports have come from Habr-Gama and colleagues who have pioneered this approach [79, 80]. In one of the largest series, the authors described a 69 % 5-year local recurrence-free survival rate that increased to 94 % after salvage surgery. This led to an overall rate of organ preservation of 78 % and an overall survival of 91 % in these patients [81]. In a retrospective series by Smith and colleagues with a 28-month follow-up period, 265 patients were treated demonstrating a cCR of 12 % and a locoregional failure rate of 19 %. The disease-free survival in this series approached 88 % with an overall survival of 96 % [82]. Furthermore, a prospective Dutch series identified 21 (11 %) cCR patients from a total of 192 treated patients. Maas reports a locoregional failure rate of only 5 % with a disease-free survival rate at 2 years of 89 % and an overall survival of 100 % [83]. Chawla and colleagues theorized that the difference between the locoregional recurrence rates in these studies likely arose from the retrospective design of the study by Smith et al., given that similar chemoradiotherapy regimens were used; in this case series, patients were accrued based on physician recall that likely created a selection bias [77, 82]. Additionally, some evidence has suggested the increased likelihood of SP when a cCR is suspected, although surgery is still offered [84].
Although grading systems exist for pCR [75], there is a lack of consensus on the definition and method of determination of cCR [78]. To address the dynamic nature of these assessments, clinical and endoscopic findings are termed as the initial cCR when assessed at 8 weeks, with subsequent assessments between 10 weeks and 12 months termed sustained cCR, when evidence of cCR persists. The importance of the 1-year landmark appears to emanate from the fact that more than 50 % of local recurrences that have been observed to occur in these patients tend to do so within the first year.
Chawla and colleagues outline a detailed review of the evidence behind various aspects of the clinical assessment of a cCR [77]. The protocolized nature of the assessment is meant to address the significant discordance that has been noted between cCR and pCR [85]. The first step in this assessment involves digital rectal examination, which has been shown in previous prospective and retrospective studies to be associated with a low degree of correlation with true pCR. Habr-Gama and colleagues have published recommendations for the standardization of the clinical and endoscopic features associated with cCR. These authors discuss various visual and tactile features characteristic of cCR that differentiate between an initial and sustained response (discussed earlier), as well as a complete and incomplete response, the latter of which includes residual nodularity and superficial and deep ulceration [80]. Furthermore, the authors advise against proceeding directly to surgery in cases of suspicion such as rectal wall thickening, densification of the perirectal fat, and small perirectal nodes (<5 mm). This recommendation is further supported by recent data, which have questioned the accuracy of some of these clinical features. In a retrospective study, Smith and colleagues assessed the gross mucosal appearance of residual disease as compared with final pathological stage. Sixty-one patients were identified with ypT0 lesions; 74 % had residual mucosal changes, of which 40 had a residual ulcer and 5 had exophytic lesions. The recommendation stated that alternative means of restaging should be attempted if rectal conservation is to be considered in these patients [86].
Adjuncts to the clinical assessment are also often recommended. This includes the use of carcinoembryonic antigen (CEA) levels, endoscopic ultrasonography, and various forms of cross-sectional imaging. When using CEA levels, the majority of evidence seems to point towards employing normalization in CEA levels post-NACRT as the most significant predictor of cCR. A recent article published by Kleiman and colleagues describes a retrospective cohort of 141 patients treated with NACRT, in whom a 13.5 % cCR was identified. Normalization of CEA was associated with an odds ratio of 65 (95 % CI: 2.53–18,371) in predicting the outcome of a pCR. Despite the smaller sample size and the retrospective design, this was highly suggestive of a strong association with the outcome of pCR [87].
Further substantiation of the clinical assessment of cCR is performed with cross-sectional imaging. CT, endorectal ultrasound, and MRI have been shown to lack accuracy in predicting cCR [88]. The functional and microstructural information provided in using diffusion-weighted imaging MRI (DWI-MRI) and PET-CT [with infused 18 F-fluorodeoxyglucose (FDG)] have shown some promise in independent series in increasing the accuracy of cCR. A recent systematic review performed on both DWI-MRI and PET-CT revealed a low positive predictive value of the outcome of cCR (DWI—54 % and PET-CT—39 %). The general conclusion of the authors was that neither imaging modality was accurate enough to predict the outcome of cCR or pCR. Interestingly, a longer time interval between the completion of NACRT and imaging with PET-CT was associated with higher rates of pCR [89]. Perez and colleagues found that, when added to their protocol of assessing cCR, the accuracy of PET-CT increased from 84 to 96 % when performed at 12 weeks after completion of NACRT [90]. The authors have also advised that increases in the 1-h SUV uptake performed post-FDG infusion when compared at 6 and 12 weeks are associated with poorer prognoses. Unfortunately, most series are small in sample size, which, despite their prospective design, can result in significant weakness in power and external validity.
Changing the interval to surgery
The timing of surgery has been a topic of much debate as surgeons attempt to balance the time-dependent maximal benefits to radiotherapy with the oncologic implications of waiting to remove the primary neoplasm. The recommended intervals have been constantly changing since the sentinel Lyon R90-01 trial, establishing the benefits of waiting until at least 6 weeks following completion of NACRT [45, 46]. Recent data have also emerged to suggest an increase in pCR rates with delaying surgery [91]. Furthermore, increasing pCR rates have also been associated with a significantly better long-term outcome [92, 93]. Unfortunately, all of the data to support increasing this interval since the randomized Lyon R90-01 have come from smaller cohort studies. These studies are also varied in their indications for neoadjuvant therapy with some recommending therapy for a high T-stage (T3/4) and suspected nodal involvement, whereas others focused on the potential for a threatened CRM, which may compromise the oncologic quality of surgery. Furthermore, the studies were heterogeneous in terms of the type of NACRT offered, which varied within and between studies as well as the differing increasing interval offered [94]. Quality of resection was assessed by the majority of studies, with no study demonstrating a difference in the rates of CRM positivity. Larger cohorts appeared to demonstrate higher rates of pCR in their patients. Wolthius and colleagues reported the largest series of patients where ≤7 weeks and >7 weeks intervals from NACRT were used. A total of 356 patients were reported, although this included stage II and III rectal cancers with 201 patients in the ≤7 weeks and 155 patients in the >7 weeks group. The rate of pCR was found to be significantly higher in the longer interval group (28 vs 16 %; p = 0.006) with no difference in perioperative morbidity or mortality. Furthermore, they demonstrated an improvement in overall and disease-free survival in patients treated with longer intervals from surgery [95].
The notion of a surgeon’s reluctance to delay surgery due to the potential effects on the dissection was investigated in a prospective study. In this study, patients were offered NACRT followed by surgery at 6 weeks or two additional cycles of FOLFOX with surgery 3–5 weeks later; this latter option would only be offered when evidence of a clinical response was seen. Despite finding higher rates of reported pelvic fibrosis in patients with delayed surgery, the authors did not find any difference in the rates of surgeon-reported operative complexity in both groups [96]. In a systematic review, the authors found a few studies that had reported on surrogates of surgical complexity in patients receiving a delayed operation, such as bleeding and operative time. One study identified a slight increase in time when surgery was delayed, but there was no difference in bleeding among the studies [94].
The current available data have been highly suggestive of a significant short- and long-term benefit to increasing the interval to surgery; however, prospective randomized trials are required. Currently, the Royal Marsden Hospital has completed its enrollment and is in a follow-up phase of a prospective randomized trial comparing tumor regression and down-staging outcomes when resected 6 and 12 weeks post-NACRT (Clinicaltrials.gov ID: NCT01037049). Furthermore, the French Greccar 6 trial is enrolling patients in a randomized design comparing pCR rates at 7 and 11 weeks post-NACRT (Clinicaltrials.gov ID: NCT01648894). The early and late outcomes of these trials will likely result in significant changes to the currently accepted recommended intervals to surgery, post-NACRT.
Conclusion
It has been established in the literature that NACRT decreases rates of local recurrence following surgery for locally advanced rectal cancers. This result may be due to a down-staging of lesions with the additional benefit of potentially allowing for preservation of the anal sphincter or even the entire rectum. In the era of patient-centered approaches to care, patients are becoming increasingly involved in the sensitive decisions being made. Discussions regarding the benefits of NACRT as well as the immediate and perioperative morbidity are crucial components of any discussion. Furthermore, quality of life is of utmost importance to most patients and significantly affects the choice of therapy, such as whether sphincter preservation is offered or chosen. At a time when non-operative management is being entertained as an option for favorably responsive rectal cancers, it is crucial that oncologists be sufficiently informed on the therapeutic options available to patients, as well as the quality of evidence. We are currently at a dynamic point in the management of rectal cancer; the outcomes of ongoing prospective trials will shed light on many of these topics and likely result in a paradigm shift in how we see rectal cancer treated over the next few years.
References
Benson AB, Bekaii-Saab T, Chan E, Chen Y-J, Choti MA, Cooper HS et al (2012) Rectal cancer. J Natl Compr Cancer Netw 10(12):1528–1564
Wanebo HJ, Koness RJ, Vezeridis MP, Cohen SI, Wrobleski DE (1994) Pelvic resection of recurrent rectal cancer. Ann Surg 220(4):586–595, discussion595–7
Heald RJ, Husband EM, Ryall RD (1982) The mesorectum in rectal cancer surgery—the clue to pelvic recurrence? Br J Surg 69(10):613–616
Shingleton WW, Prosnitz LR (1985) Adjuvant therapy of colorectal cancer. Curr Probl Cancer 9(10):1–34
Krook JE, Moertel CG, Gunderson LL, Wieand HS, Collins RT, Beart RW et al (1991) Effective surgical adjuvant therapy for high-risk rectal carcinoma. N Engl J Med 324(11):709–715
O’Connell MJ, Martenson JA, Wieand HS, Krook JE, Macdonald JS, Haller DG et al (1994) Improving adjuvant therapy for rectal cancer by combining protracted-infusion fluorouracil with radiation therapy after curative surgery. N Engl J Med 331(8):502–507
Gastrointestinal Tumor Study Group (1985) Prolongation of the disease-free interval in surgically treated rectal carcinoma. N Engl J Med 312(23):1465–1472
Tveit KM, Guldvog I, Hagen S, Trondsen E, Harbitz T, Nygaard K et al (1997) Randomized controlled trial of postoperative radiotherapy and short-term time-scheduled 5-fluorouracil against surgery alone in the treatment of Dukes B and C rectal cancer. Norwegian Adjuvant Rectal Cancer Project Group. Br J Surg 84(8):1130–1135
Steup WH, Moriya Y, van de Velde CJH (2002) Patterns of lymphatic spread in rectal cancer. A topographical analysis on lymph node metastases. Eur J Cancer 38(7):911–918
Quirke P, Durdey P, Dixon MF, Williams NS (1986) Local recurrence of rectal adenocarcinoma due to inadequate surgical resection. Histopathological study of lateral tumour spread and surgical excision. Lancet 2(8514):996–999
Quirke P (2003) Training and quality assurance for rectal cancer: 20 years of data is enough. Lancet Oncol 4(11):695–702
Glimelius BLG (2002) The role of preoperative and postoperative radiotherapy in rectal cancer. Clin Colorectal Cancer 2(2):82–92
Colorectal Cancer Collaborative Group (2001) Adjuvant radiotherapy for rectal cancer: a systematic overview of 8,507 patients from 22 randomised trials. Lancet 358(9290):1291–1304, Elsevier
(1997) Improved survival with preoperative radiotherapy in resectable rectal cancer. Swedish Rectal Cancer Trial. N Engl J Med 336(14):980–7
Kapiteijn E, Marijnen CA, Nagtegaal ID, Putter H, Steup WH, Wiggers T et al (2001) Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med 345(9):638–646
van Gijn W, Marijnen CA, Nagtegaal ID, Kranenbarg EM, Putter H, Wiggers T et al (2011) Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer: 12-year follow-up of the multicentre, randomised controlled TME trial. Lancet Oncol 12(6):575–582, Elsevier Ltd
Sauer R, Becker H, Hohenberger W, Rödel C, Wittekind C, Fietkau R et al (2004) Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med 351(17):1731–1740
Sauer R, Liersch T, Merkel S, Fietkau R, Hohenberger W, Hess C et al (2012) Preoperative versus postoperative chemoradiotherapy for locally advanced rectal cancer: results of the German CAO/ARO/AIO-94 randomized phase III trial after a median follow-up of 11 years. J Clin Oncol 30(16):1926–1933
Bosset J-F, Collette L, Calais G, Mineur L, Maingon P, Radosevic-Jelic L et al (2006) Chemotherapy with preoperative radiotherapy in rectal cancer. N Engl J Med 355(11):1114–1123
Sebag-Montefiore D, Stephens RJ, Steele R, Monson J, Grieve R, Khanna S et al (2009) Preoperative radiotherapy versus selective postoperative chemoradiotherapy in patients with rectal cancer (MRC CR07 and NCIC-CTG C016): a multicentre, randomised trial. Lancet 373(9666):811–820, Elsevier Ltd
Twelves C, Wong A, Nowacki MP, Abt M, Burris H, Carrato A et al (2005) Capecitabine as adjuvant treatment for stage III colon cancer. N Engl J Med 352(26):2696–2704
Roh MS, Colangelo LH, O’Connell MJ, Yothers G, Deutsch M, Allegra CJ et al (2009) Preoperative multimodality therapy improves disease-free survival in patients with carcinoma of the rectum: NSABP R-03. J Clin Oncol 27(31):5124–5130
Hofheinz RD, Wenz F, Post S, Matzdorff A, Laechelt S, Hartmann JT et al (2012) Chemoradiotherapy with capecitabine versus fluorouracil for locally advanced rectal cancer: a randomised, multicentre, non-inferiority, phase 3 trial. Lancet Oncol 13(6):579–588, Elsevier Ltd
Chau I, Allen M, Cunningham D, Tait D, Brown G, Hill M et al (2003) Neoadjuvant systemic fluorouracil and mitomycin C prior to synchronous chemoradiation is an effective strategy in locally advanced rectal cancer. Br J Cancer 88(7):1017–1024, Nature Publishing Group
Chau I, Brown G, Cunningham D, Tait D, Wotherspoon A, Norman AR et al (2006) Neoadjuvant capecitabine and oxaliplatin followed by synchronous chemoradiation and total mesorectal excision in magnetic resonance imaging-defined poor-risk rectal cancer. J Clin Oncol 24(4):668–674
Calvo FA, Serrano FJ, Diaz-González JA, Gomez-Espi M, Lozano E, Garcia R et al (2006) Improved incidence of pT0 downstaged surgical specimens in locally advanced rectal cancer (LARC) treated with induction oxaliplatin plus 5-fluorouracil and preoperative chemoradiation. Ann Oncol 17(7):1103–1110, Oxford University Press
Maréchal R, Vos B, Polus M, Delaunoit T, Peeters M, Demetter P et al (2012) Short course chemotherapy followed by concomitant chemoradiotherapy and surgery in locally advanced rectal cancer: a randomized multicentric phase II study. Ann Oncol 23(6):1525–1530, Oxford University Press
Fernández-Martos C, Pericay C, Aparicio J, Salud A, Safont M, Massuti B et al (2010) Phase II, randomized study of concomitant chemoradiotherapy followed by surgery and adjuvant capecitabine plus oxaliplatin (CAPOX) compared with induction CAPOX followed by concomitant chemoradiotherapy and surgery in magnetic resonance imaging-defined, locally advanced rectal cancer: Grupo cancer de recto 3 study. J Clin Oncol Am Soc Clin Oncol 28(5):859–865
Gérard J-P, Azria D, Gourgou-Bourgade S, Martel-Lafay I, Hennequin C, Etienne P-L et al (2012) Clinical outcome of the ACCORD 12/0405 PRODIGE 2 randomized trial in rectal cancer. J Clin Oncol Am Soc Clin Oncol 30(36):4558–4565
Aschele C, Cionini L, Lonardi S, Pinto C, Cordio S, Rosati G et al (2011) Primary tumor response to preoperative chemoradiation with or without oxaliplatin in locally advanced rectal cancer: pathologic results of the STAR-01 randomized phase III trial. J Clin Oncol Am Soc Clin Oncol 29(20):2773–2780
Bujko K, Nowacki MP, Nasierowska-Guttmejer A, Michalski W, Bebenek M, Pudełko M et al (2004) Sphincter preservation following preoperative radiotherapy for rectal cancer: report of a randomised trial comparing short-term radiotherapy vs. conventionally fractionated radiochemotherapy. Radiother Oncol 72(1):15–24, Elsevier
Birgisson H, Påhlman L, Gunnarsson U, Glimelius B, Swedish Rectal Cancer Trial Group (2005) Adverse effects of preoperative radiation therapy for rectal cancer: long-term follow-up of the Swedish Rectal Cancer Trial. J Clin Oncol Am Soc Clin Oncol 23(34):8697–8705
Bujko K, Nowacki MP, Nasierowska-Guttmejer A, Michalski W, Bebenek M, Kryj M et al (2006) Long-term results of a randomized trial comparing preoperative short-course radiotherapy with preoperative conventionally fractionated chemoradiation for rectal cancer. Br J Surg 93(10):1215–1223, John Wiley & Sons, Ltd
Ngan SY, Burmeister B, Fisher RJ, Solomon M, Goldstein D, Joseph D et al (2012) Randomized trial of short-course radiotherapy versus long-course chemoradiation comparing rates of local recurrence in patients with T3 rectal cancer: Trans-Tasman Radiation Oncology Group trial 01.04. J Clin Oncol 30(31):3827–3833
Latkauskas T, Pauzas H, Gineikiene I, Janciauskiene R, Juozaityte E, Saladzinskas Z et al (2012) Initial results of a randomized controlled trial comparing clinical and pathological downstaging of rectal cancer after preoperative short-course radiotherapy or long-term chemoradiotherapy, both with delayed surgery. Color Dis 14(3):294–298, Blackwell Publishing Ltd
Zhou Z-R, Liu S-X, Zhang T-S, Chen L-X, Xia J, Hu Z-D et al (2014) Short-course preoperative radiotherapy with immediate surgery versus long-course chemoradiation with delayed surgery in the treatment of rectal cancer: a systematic review and meta-analysis. Surg Oncol 23(4):211–221, Elsevier Ltd
Onaitis MW, Noone RB, Hartwig M, Hurwitz H, Morse M, Jowell P et al (2001) Neoadjuvant chemoradiation for rectal cancer: analysis of clinical outcomes from a 13-year institutional experience. Ann Surg 233(6):778–785
Påhlman L, Glimelius B, Graffman S (1985) Pre- versus postoperative radiotherapy in rectal carcinoma: an interim report from a randomized multicentre trial. Br J Surg 72(12):961–966
De Caluwé L, Van Nieuwenhove Y, Ceelen WP (2013) Preoperative chemoradiation versus radiation alone for stage II and III resectable rectal cancer. Ceelen WP, editor. Cochrane Database Syst Rev. Chichester, UK: John Wiley & Sons, Ltd 2:CD006041
Krouse RS, Herrinton LJ, Grant M, Wendel CS, Green SB, Mohler MJ et al (2009) Health-related quality of life among long-term rectal cancer survivors with an ostomy: manifestations by sex. J Clin Oncol Am Soc Clin Oncol 27(28):4664–4670
Boulis-Wassif S, Gerard A, Loygue J, Camelot D, Buyse M, Duez N (1984) Final results of a randomized trial on the treatment of rectal cancer with preoperative radiotherapy alone or in combination with 5-fluorouracil, followed by radical surgery. Trial of the European Organization on Research and Treatment of Cancer Gastrointestinal Tract Cancer Cooperative Group. Cancer 53(9):1811–1818
Temple LK, Romanus D, Niland J, Veer AT, Weiser MR, Skibber J et al (2009) Factors associated with sphincter-preserving surgery for rectal cancer at national comprehensive cancer network centers. Ann Surg 250(2):260–267
Wolmark N, Fisher B (1986) An analysis of survival and treatment failure following abdominoperineal and sphincter-saving resection in Dukes’ B and C rectal carcinoma. A report of the NSABP clinical trials. National Surgical Adjuvant Breast and Bowel Project. Ann Surg 204(4):480–489
Moore HG, Riedel E, Minsky BD, Saltz L, Paty P, Wong D et al (2003) Adequacy of 1-cm distal margin after restorative rectal cancer resection with sharp mesorectal excision and preoperative combined-modality therapy. Ann Surg Oncol 10(1):80–85
Valentini V, Glimelius B, Minsky BD, Van Cutsem E, Bartelink H, Beets-Tan RGH et al (2005) The multidisciplinary rectal cancer treatment: main convergences, controversial aspects and investigational areas which support the need for an European Consensus. Radiother Oncol 76(3):241–250
Francois Y, Nemoz CJ, Baulieux J, Vignal J, Grandjean JP, Partensky C et al (1999) Influence of the interval between preoperative radiation therapy and surgery on downstaging and on the rate of sphincter-sparing surgery for rectal cancer: the Lyon R90-01 randomized trial. J Clin Oncol 17(8):2396
Gérard J-P, Rostom Y, Gal J, Benchimol D, Ortholan C, Aschele C et al (2012) Can we increase the chance of sphincter saving surgery in rectal cancer with neoadjuvant treatments: lessons from a systematic review of recent randomized trials. Crit Rev Oncol Hematol 81(1):21–28, Elsevier Ireland Ltd
Gérard J-P, Chapet O, Ramaioli A, Romestaing P (2002) Long-term control of T2-T3 rectal adenocarcinoma with radiotherapy alone. Int J Radiat Oncol Biol Phys 54(1):142–149
Hedrick TL, Sawyer RG, Foley EF, Friel CM (2006) Anastomotic leak and the loop ileostomy: friend or foe? Dis Colon Rectum 49(8):1167–1176
Phitayakorn R, Delaney CP, Reynolds HL, Champagne BJ, Heriot AG, Neary P et al (2008) Standardized algorithms for management of anastomotic leaks and related abdominal and pelvic abscesses after colorectal surgery. World J Surg 32(6):1147–1156, Springer-Verlag
Boccola MA, Lin J, Rozen WM, Ho Y-H (2010) Reducing anastomotic leakage in oncologic colorectal surgery: an evidence-based review. Anticancer Res 30(2):601–607
Moran B, Heald R (2000) Anastomotic leakage after colorectal anastomosis. Semin Surg Oncol 18(3):244–248
Bregendahl S, Emmertsen KJ, Lous J, Laurberg S (2013) Bowel dysfunction after low anterior resection with and without neoadjuvant therapy for rectal cancer: a population-based cross-sectional study. Color Dis 15(9):1130–1139
Mongin C, Maggiori L, Agostini J, Ferron M, Panis Y (2014) Does anastomotic leakage impair functional results and quality of life after laparoscopic sphincter-saving total mesorectal excision for rectal cancer? A case-matched study. Int J Color Dis 29(4):459–467, Springer Berlin Heidelberg
Law WL, Choi HK, Lee YM, Ho JWC, Seto CL (2007) Anastomotic leakage is associated with poor long-term outcome in patients after curative colorectal resection for malignancy. J Gastrointest Surg 11(1):8–15, Springer-Verlag
Mirnezami A, Mirnezami R, Chandrakumaran K, Sasapu K, Sagar P, Finan P (2011) Increased local recurrence and reduced survival from colorectal cancer following anastomotic leak: systematic review and meta-analysis. Ann Surg 253(5):890–899
Dinnewitzer A, Jäger T, Nawara C, Buchner S, Wolfgang H, Öfner D (2013) Cumulative incidence of permanent stoma after sphincter preserving low anterior resection of mid and low rectal cancer. Dis Colon Rectum 56(10):1134–1142
McCarthy K, Pearson K, Fulton R, Hewitt J (2012) Pre-operative chemoradiation for non-metastatic locally advanced rectal cancer. McCarthy K, editor. Cochrane Database Syst Rev. Chichester, UK: John Wiley & Sons, Ltd 12:CD008368.
Jestin P, Påhlman L, Gunnarsson U (2008) Risk factors for anastomotic leakage after rectal cancer surgery: a case-control study. Color Dis 10(7):715–721, Blackwell Publishing Ltd
Warschkow R, Steffen T, Thierbach J, Bruckner T, Lange J, Tarantino I (2011) Risk factors for anastomotic leakage after rectal cancer resection and reconstruction with colorectostomy. A retrospective study with bootstrap analysis. Ann Surg Oncol 18(10):2772–2782, Springer-Verlag
Lee W-S, Yun SH, Roh Y-N, Yun H-R, Lee WY, Cho YB et al (2008) Risk factors and clinical outcome for anastomotic leakage after total mesorectal excision for rectal cancer. World J Surg 32(6):1124–1129, Springer-Verlag
Qin C, Ren X, Xu K, Chen Z, He Y, Song X (2014) Does preoperative radio(chemo)therapy increase anastomotic leakage in rectal cancer surgery? A meta-analysis of randomized controlled trials. Gastroenterol Res Pract 2014(2):910956–910957, Hindawi Publishing Corporation
Leahy J, Schoetz D, Marcello P, Read T, Hall J, Roberts P et al (2014) What is the risk of clinical anastomotic leak in the diverted colorectal anastomosis? J Gastrointest Surg 18(10):1812–1816, Springer US
Garlipp B, Ptok H, Schmidt U, Meyer F, Gastinger I, Lippert H (2010) Neoadjuvant chemoradiotherapy for rectal carcinoma: effects on anastomotic leak rate and postoperative bladder dysfunction after non-emergency sphincter-preserving anterior rectal resection. Results of the Quality Assurance in Rectal Cancer Surgery multicenter observational trial. Langenbecks Arch Surg 395(8):1031–1038, Springer-Verlag
Peeters KCMJ (2005) Late side effects of short-course preoperative radiotherapy combined with total mesorectal excision for rectal cancer: increased bowel dysfunction in irradiated patients—a Dutch colorectal cancer group study. J Clin Oncol 23(25):6199–6206
Hendren SK, O’Connor BI, Liu M, Asano T, Cohen Z, Swallow CJ et al (2005) Prevalence of male and female sexual dysfunction is high following surgery for rectal cancer. Ann Surg 242(2):212–223
Marijnen CAM, van de Velde CJH, Putter H, van den Brink M, Maas CP, Martijn H et al (2005) Impact of short-term preoperative radiotherapy on health-related quality of life and sexual functioning in primary rectal cancer: report of a multicenter randomized trial. J Clin Oncol 23(9):1847–1858
Pietrangeli A, Pugliese P, Perrone M, Sperduti I, Cosimelli M, Jandolo B (2009) Sexual dysfunction following surgery for rectal cancer—a clinical and neurophysiological study. J Exp Clin Cancer Res 28(1):128, BioMed Central Ltd
Stephens RJ, Thompson LC, Quirke P, Steele R, Grieve R, Couture J et al (2010) Impact of short-course preoperative radiotherapy for rectal cancer on patients’ quality of life: data from the Medical Research Council CR07/National Cancer Institute of Canada Clinical Trials Group C016 randomized clinical trial. J Clin Oncol Am Soc Clin Oncol 28(27):4233–4239
Loos M, Quentmeier P, Schuster T, Nitsche U, Gertler R, Keerl A et al (2013) Effect of preoperative radio(chemo)therapy on long-term functional outcome in rectal cancer patients: a systematic review and meta-analysis. Ann Surg Oncol 20(6):1816–1828, Springer-Verlag
West MA, Loughney L, Barben CP, Sripadam R, Kemp GJ, Grocott MPW et al (2014) The effects of neoadjuvant chemoradiotherapy on physical fitness and morbidity in rectal cancer surgery patients. Eur J Surg Oncol 40(11):1421–1428, Elsevier Ltd
West MA, Loughney L, Lythgoe D, Barben CP, Sripadam R, Kemp GJ et al (2015) Effect of prehabilitation on objectively measured physical fitness after neoadjuvant treatment in preoperative rectal cancer patients: a blinded interventional pilot study. Br J Anaesth 114(2):244–251
Dronkers JJ, Lamberts H, Reutelingsperger IMMD, Naber RH, Dronkers-Landman CM, Veldman A et al (2010) Preoperative therapeutic programme for elderly patients scheduled for elective abdominal oncological surgery: a randomized controlled pilot study. Clin Rehabil 24(7):614–622, SAGE Publications
Li C, Carli F, Lee L, Charlebois P, Stein B, Liberman AS et al (2013) Impact of a trimodal prehabilitation program on functional recovery after colorectal cancer surgery: a pilot study. Surg Endosc 27(4):1072–1082, Springer-Verlag
Dworak O, Keilholz L, Hoffmann A (1997) Pathological features of rectal cancer after preoperative radiochemotherapy. Int J Color Dis 12(1):19–23
Sanghera P, Wong DWY, McConkey CC, Geh JI, Hartley A (2008) Chemoradiotherapy for rectal cancer: an updated analysis of factors affecting pathological response. Clin Oncol (R Coll Radiol) 20(2):176–183, Elsevier
Chawla S, Katz AW, Rauh SM, Monson JRT (2014) Can surgery be avoided after preoperative chemoradiation for rectal cancer in the era of organ preservation? Current review of literature. Am J Clin Oncol. doi:10.1097/COC.0000000000000122
Glynne-Jones R, Hughes R (2012) Critical appraisal of the “wait and see” approach in rectal cancer for clinical complete responders after chemoradiation. Br J Surg 99(7):897–909
Habr-Gama A, Perez R, Proscurshim I, Gama-Rodrigues J (2010) Complete clinical response after neoadjuvant chemoradiation for distal rectal cancer. Surg Oncol Clin N Am 19(4):829–845, Elsevier
Habr-Gama A, Perez RO, Wynn G, Marks J, Kessler H, Gama-Rodrigues J (2010) Complete clinical response after neoadjuvant chemoradiation therapy for distal rectal cancer: characterization of clinical and endoscopic findings for standardization. Dis Colon Rectum 53(12):1692–1698
Habr-Gama A, Gama-Rodrigues J, São Julião GP, Proscurshim I, Sabbagh C, Lynn PB et al (2014) Local recurrence after complete clinical response and watch and wait in rectal cancer after neoadjuvant chemoradiation: impact of salvage therapy on local disease control. Int J Radiat Oncol Biol Phys 88(4):822–828, Elsevier
Smith JD, Ruby JA, Goodman KA, Saltz LB, Guillem JG, Weiser MR et al (2012) Nonoperative management of rectal cancer with complete clinical response after neoadjuvant therapy. Ann Surg 256(6):965–972
Maas M, Nelemans PJ, Valentini V, Crane CH, Capirci C, Rödel C et al (2014) Adjuvant chemotherapy in rectal cancer: defining subgroups who may benefit after neoadjuvant chemoradiation and resection: a pooled analysis of 3,313 patients. Int J Cancer 137(1):212–220
Gérard JP, Chamorey E, Gourgou-Bourgade S, Benezery K, de Laroche G, Mahé MA et al (2015) Clinical complete response (cCR) after neoadjuvant chemoradiotherapy and conservative treatment in rectal cancer. Findings from the ACCORD 12/PRODIGE 2 randomized trial. Radiother Oncol 115(2):246–252
Glynne-Jones R, Wallace M, Livingstone JIL, Meyrick-Thomas J (2008) Complete clinical response after preoperative chemoradiation in rectal cancer: is a “wait and see” policy justified? Dis Colon Rectum 51(1):10–19, discussion19–20
Smith FM, Wiland H, Mace A, Pai RK, Kalady MF (2014) Clinical criteria underestimate complete pathological response in rectal cancer treated with neoadjuvant chemoradiotherapy. Dis Colon Rectum 57(3):311–315
Kleiman A, Al-Khamis A, Farsi A, Kezouh A, Vuong T, Gordon PH et al (2015) Normalization of CEA levels post-neoadjuvant therapy is a strong predictor of pathologic complete response in rectal cancer. J Gastrointest Surg 19(6):1106–1112, Springer US
Zhao R-S, Wang H, Zhou Z-Y, Zhou Q, Mulholland MW (2014) Restaging of locally advanced rectal cancer with magnetic resonance imaging and endoluminal ultrasound after preoperative chemoradiotherapy. Dis Colon Rectum 57(3):388–395
Joye I, Deroose CM, Vandecaveye V, Haustermans K (2014) The role of diffusion-weighted MRI and 18F-FDG PET/CT in the prediction of pathologic complete response after radiochemotherapy for rectal cancer: a systematic review. Radiother Oncol 113(2):158–165, Elsevier Ireland Ltd
Perez RO, Habr-Gama A, Gama-Rodrigues J, Proscurshim I, Julião GPS, Lynn P et al (2011) Accuracy of positron emission tomography/computed tomography and clinical assessment in the detection of complete rectal tumor regression after neoadjuvant chemoradiation. Cancer 118(14):3501–3511
de Campos-Lobato LF, Geisler DP, da Luz Moreira A, Stocchi L, Dietz D, Kalady MF (2011) Neoadjuvant therapy for rectal cancer: the impact of longer interval between chemoradiation and surgery. J Gastrointest Surg 15(3):444–450, Springer-Verlag
Maas M, Nelemans PJ, Valentini V, Das P, Rödel C, Kuo L-J et al (2010) Long-term outcome in patients with a pathological complete response after chemoradiation for rectal cancer: a pooled analysis of individual patient data. Lancet Oncol 11(9):835–844, Elsevier Ltd
Kerr SF, Norton S, Glynne-Jones R (2008) Delaying surgery after neoadjuvant chemoradiotherapy for rectal cancer may reduce postoperative morbidity without compromising prognosis. Br J Surg 95(12):1534–1540
Foster JD, Jones EL, Falk S, Cooper EJ, Francis NK (2013) Timing of surgery after long-course neoadjuvant chemoradiotherapy for rectal cancer. Dis Colon Rectum 56(7):921–930
Wolthuis AM, Penninckx F, Haustermans K, De Hertogh G, Fieuws S, Van Cutsem E et al (2012) Impact of interval between neoadjuvant chemoradiotherapy and TME for locally advanced rectal cancer on pathologic response and oncologic outcome. Ann Surg Oncol 19(9):2833–2841
Garcia-Aguilar J, Smith DD, Avila K, Bergsland EK, Chu P, Krieg RM (2011) Optimal timing of surgery after chemoradiation for advanced rectal cancer. Ann Surg 254(1):97–102
Compliance with ethical standards
Funding
No funding was provided for this review article.
Conflicts of interest
None.
Ethical approval
Given the nature of this article being a review of the published literature, no ethical approval was sought.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chadi, S.A., Berho, M. & Wexner, S.D. Surgeon perspectives on the use and effects of neoadjuvant chemoradiation in the treatment of rectal cancer: a comprehensive review of the literature. Langenbecks Arch Surg 400, 661–673 (2015). https://doi.org/10.1007/s00423-015-1328-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-015-1328-5