Abstract
Purpose of Review
Interstitial cystitis/bladder pain syndrome (IC/BPS) is a disease that causes bladder symptoms such as pelvic pain and frequent urination and is often an intractable disease affecting a patient’s quality of life. The etiology of IC/BPS remains elusive, and treatment strategies are still not fully established. To better understand the underlying pathophysiology, many studies have strived to recreate an animal model of IC/BPS to help further expand the treatment options of this difficult disease.
Recent Findings
Basic animal studies of IC/BPS have often been conducted by provoking inflammation in the bladder, which is useful at least in part due to the similarity of the pathophysiology to profound inflammatory responses in IC/BPS, especially in the Hunner lesion subtype. Also, other animal models such as bladder stimulation models, pelvic organ cross-sensitization models, autoimmune models, and psychological stress models have been explored and shown various new outsights. However, the predicted underlying etiology of IC/BPS is complex often with a combination of inflammation, ischemia, and neurogenic changes, which makes it challenging for researchers to translate the results in animal models to clinical applications.
Summary
Each animal model that is containing a piece of the underlying etiology of IC/BPS cannot be obtained alone, but by forming a picture by using each piece adequately will enable us to expand the horizon of the unexplored pathophysiology, which will lead us to identify novel therapeutic targets.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Interstitial cystitis/bladder pain syndrome (IC/BPS) is a chronic disease that causes severe pelvic pain and lower urinary tract symptoms (LUTS) such as urinary frequency, urgency, and nocturia [1•], which leads to chronic stress, sleep dysfunction, anxiety, depression, leading to decrease of quality of life. The etiology is thought to be multifactorial such as inflammatory, neurogenic, autoimmune, and/or vascular abnormalities [2]; thus, further studies are needed to better understand the IC/BPS pathophysiology. There are many animal experimental models that mimic IC/BPS, at least some parts, to better understand its pathophysiological mechanisms. Each of the models usually focusses on a certain system to recreate bladder dysfunction, which is useful to help understand each of the contributing mechanisms. However, IC/BPS is a condition that consists of multiple factors and involves multiple systems, which makes it difficult to represent complex pathophysiological mechanisms and their interactions in one model.
In addition, although IC and BPS is commonly taken as a condition that is closely related, the condition of each disease exhibits that there are two major phenotypes in IC/BPS; namely, “interstitial cystitis (IC)”, which is a chronic inflammatory disorder with Hunner lesions, and “bladder pain syndrome (BPS)”, whose inflammatory changes are minimal without Hunner lesions [3•]. The existence of these two different phenotypes could be the reason for making the selection of the adequate experimental model for IC/BPS difficult. The present review focuses on various models commonly used to mimic the features in IC/BPS patients, by dividing into the following categories: (1) bladder inflammation/irritation models, (2) pelvic organ cross sensitization models, (3) psychological stress models, and discuss the characteristics of each of these models.
Bladder Inflammation Models
The diagnosis of IC/BPS is often made by biopsy of the bladder for confirmation of inflammation and exclusion of other diseases. Many animal models have been explored to study the relation of inflammation and bladder dysfunction [4]. These models show several IC/BPS-like phenotypes, such as shortening of voiding intervals, bladder pain, and denudation of epithelial cells. However, because of the lack of understanding of the factors that initiate IC/BPS, one should note that it is unclear whether bladder inflammation models are an absolute fit for the study of IC/BPS.
The inflammation of these models is often caused by chemical irritation or intravesical infection [2], which does not develop naturally in IC/BPS. Another point that researchers should keep in mind is that the effect of irritants does not last long enough to mimic the chronic aspect of IC/BPS. Symptoms of IC/BPS last for a prolonged period that may cause further changes whereas the effect of exposure to irritants is temporary. However, this does not mean that inflammation animal models are without a value, and that results of inflammation model experiments have provided numerous aspects useful for the understanding of IC/BPS. Therefore, researchers must understand the characteristics of the experimental model used, and evaluate which part of the results can be applied for understanding the IC/BPS pathophysiology and which part cannot.
Chemically Induced Cystitis
Majority of animal models used to study IC/BPS have been generated by inducing bladder inflammation with or without epithelial damage using intravesical or systemic instillation of chemical agents or irritants [4]. Although the inflammation of the bladder in IC/BPS patients is not caused by these chemicals, they exhibit some of the characteristics of inflammation and clinical features such as urinary frequency and bladder pain observed in IC/BPS. Each irritant has their specific characteristics and should be taken into consideration when used for research.
Hydrogen Peroxide (HP)
HP is a reactive oxygen species that causes lipid peroxidation and oxidation of DNA and proteins. A single intravesical administration of HP is reported to induce a relatively long-lasting bladder inflammation and bladder dysfunction for up to 2 weeks in the rat model [5, 6]. The histological changes and enhanced urothelial permeability are similar to those observed in IC/BPS. It is also reported that intravesical administration of hydrogen peroxide increases nerve growth factor (NGF) in the bladder mucosa [6], which is also confirmed in IC/BPS patients.
Hyaluronidase
Hyaluronidase, which is a type of endoglycosidase, can hydrolyze the extracellular matrix, which compose the GAG layer [7]. Degrading the GAG layer on the endothelial cell surface increases permeability of the bladder epithelium, which causes bladder inflammation, diffused fibrosis, stimulation of afferent neurons, which will develop an animal model of bladder dysfunction [8]. The effect of hyaluronidase acts as a long-lasting, mild inflammatory stimulus, which is similar to human IC/BPS bladders; thus, this model may potentially be a valuable IC/BPS animal model.
Protamine Sulfate (PS)
PS increases the apical membrane permeability causing bladder dysfunction depending on the concentration [9]. High-dose PS causes strong inflammation, which provokes urinary frequency and pain sensation although administration of low-dose PS shows no effect in the normal rat [10]. However, in certain bladder hypersensitive conditions including a psychologically stressed condition, which will be discussed later, low-dose PS penetrates the bladder wall causing inflammation and denudation of the bladder urothelium. Continuous administration of PS is reported to cause storage dysfunction of the bladder, which is a commonly observed characteristic in IC/BPS and is considered a useful modality for investigating IC/BPS [9].
E. coli Lipopolysaccharide (LPS)
E. coli LPS is a bacterial product that is commonly used to produce cystitis. Instillation of E. coli LPS can produce bladder dysfunction and suprapubic pain caused by infiltration of neutrophils in the bladder wall [11]. With a combination of other irritants such as PS, which can destroy the GAG layer of the urothelium, E. coli LPS can also cross the bladder wall barrier and penetrate into the body systemically [12]. Systemic administration also causes bladder inflammation and could produce a model that exhibits IC/BPS-like symptoms [13].
Cytokine Overexpression
Previous studies have demonstrated that various cytokines and chemokines including TNF-α are detected in urine and/or bladder specimens from IC/BPS patients [14]. Furthermore, a randomized, double-blind, placebo-controlled trial showed that subcutaneous administration of certolizumab pegol, an anti-TNF-α monoclonal antibody, improved global response assessment, Interstitial Cystitis Symptom & Problem Indices, and a numeric rating scale for pain and urgency in moderate-to-severe IC/BPS women [15]. Accordingly, a transgenic mouse model with urothelial overexpression of TNF-α has been produced and exhibited significant pelvic pain, storage dysfunction, urothelial lesions, and enhanced sensory input [16], suggesting that this is an appropriate model for studying the cytokine-related bladder inflammation mechanisms underlying IC/BPS pathophysiology.
Claudin-2 Overexpression in the Urothelium
It has been proposed that increased urothelial permeability in the bladder is an important pathophysiological basis of IC/BPS, which is associated with changes in tight junction proteins such as reduced expression of ZO-1 or overexpression of pore-forming claudin-2 [17]. To mimic this urothelial hyper-permeability condition of IC/BPS, a rat model with adenoviral transduction claudin-2 in the urothelium has been produced and exhibited increased urothelial permeability, suburothelial inflammation, pelvic pain, small bladder capacity and bladder afferent sensitization [18, 19]. These results suggest that this claudin-2 overexpression model could be useful for studying urothelial dysfunction mechanisms leading to bladder inflammation, which underly IC/BPS pathogenesis.
Feline Spontaneous Cystitis
A certain strain of domestic cats develop a bladder disease that presents urinary frequency, urgency, and hematuria [20]. A decrease in the urine glycosaminoglycan level, which is also observed in human IC/BPS patients, has suggested that this cat model would be an ideal experimental animal model of IC/BPS [21]. Basic research has shown that this cat model represents numerous similarities to IC/BPS; thus, this model has the advantage of developing IC/BPS symptoms without application of bladder irritating substances. However, the underlying causes for developing cystitis in the feline model is still not fully identified. Further understanding this model may provide us knowledge of clarifying the IC/BPS etiology.
Viral-Induced Cystitis
In previous studies, injection of pseudorabies virus into the abductor coccygeus tail muscle in the rat caused hemorrhagic cystitis, leading to the understanding that certain areas of the spinal cord are involved in the tail-to-bladder neural network inducing cystitis [22]. This model showed bladder inflammation with infiltrated mast cells, leading to bladder pain and bladder dysfunction due to the loss of the barrier function in the urothelium. Further studies have shown that release of neuropeptides in the spinal cord leads to release of mast cells within the bladder wall [23,24,25]. Thus, this model may provide understandings of the IC/BPS pathogenesis; however, future studies are needed to clarify whether the IC/BPS-like condition in this model is induced through the central nervous system pathway.
Bladder Irritation Models
Urinary substances such as potassium and uric acid are proposed as a factor stimulating C-fiber afferent fibers in the bladder mucosa, which leads to bladder symptoms in human IC/BPS patients [26]. Increased permeability and disruption of the bladder barrier function are proposed as pathophysiological mechanisms causing these symptoms [27]. Many animal experiments have been conducted by using a specific substance found in the urine or intravesical administration of irritants such as acetic acid and cyclophosphamide (CYP) [4, 28].
Also, animals with systemic CYP administration are a commonly used model that exhibits IC/BPS-like symptoms such as pain-related behaviors and bladder dysfunction due to bladder inflammation. CYP-induced cystitis is a model that can be obtained by a single intraperitoneal infection of CYP, which is degraded to acrolein, a TRPA1 agonist [29], and symptoms occur within 24 h after injection. This model shows strong bladder inflammation, resulting in mucosal destruction and hemorrhage, which makes this model more suitable as a hemorrhagic cystitis model, rather than an IC/BPS-like model [30]. Recent studies with a lower dose of CYP showed mild inflammation and symptoms [31], which may have the potential as a suitable model for IC/BPS.
The limitation for these bladder irritation models is that the experimental results are the mere consequence of what is happening in the bladder (e.g., bladder inflammation), but not what is causing the pathological changes seen in IC/BPS bladders. Other limitations include that bladder inflammation is usually short-lasting and that hemorrhagic cystitis does not usually take place in IC/BPS patients. Therefore, these models are of use for evaluating treatments of cystitis-like changes and for examining the correlation of pathological and morphological changes and bladder dysfunction, but may not be suitable for searching the cause of IC/BPS.
Autoimmune Cystitis
Recent studies have shown that IC/BPS with Hunner lesions, which is characterized as reddish mucosal lesions with microvessel formation confirmed by cystoscopic examinations [1•], are associated with autoimmunity to the bladder tissue induced by B-cell clonal expansion [32]. To develop autoimmunity in the animal model, various methods have been explored. Autoimmunity induced by bladder tissue homogenization shows mucosal edema, increased urothelial permeability and lymphocytic infiltration, which lead to bladder dysfunction and suprapubic pain-related behavior [33, 34•]. Also, bladder symptoms induced by bladder tissue homogenization lasted for several months [35, 36]. These models have proven that anti-immune therapy may be a potential option as a treatment strategy against certain types of IC/BPS, especially with the Hunner lesion type with severe bladder inflammation. In addition, bladder urothelial antigens such as those against uroplakin, T2 peptide that is an antigenic epitope of TRPM8 protein, or UPK3A-derived immunogenic peptide have been used to produce IC/BPS animal models [37, 38]. These models show inflammation with T-cell infiltration in the suburothelial layer, leading to storage dysfunction and increased suprapubic pain. Furthermore, transgenic autoimmune models have also been explored. By generating mice expressing a specific antigen against urothelial cells along with transferring specific T cells from mice that express specific T-cell receptors, these mice show increased bladder nociceptive responses and bladder dysfunction. Also, these conditions last for almost 20 weeks, proving that these transgenic mice are the long-lasting model of IC/BPS [39]. Thus, these genetically produced, antigen-specific animal models enable us to explore the specific roles of immune cells and receptors in the IC/BPS-like condition. However, it is not known whether bladder tissue antigens are involved in human IC/BPS pathogenesis. Overall, autoimmune animal models are proposed to be a suitable model of IC/BPS, especially Hunner type IC with urothelial dysfunction; however, researchers should well understand the limitation of these models to explore which aspects in these models are applicable for the condition of two different phenotypes of IC/BPS; namely IC with Hunner lesion or BPS without.
Pelvic Organ Cross Sensitization Models
Previous studies have provided evidence for neural cross-talk and bidirectional cross sensitization between pelvic organs, in which chemical irritation of the colon by 2,4,6-trinitrobenzenesulfonic acid (TNBS) increased pain sensitivity in the bladder via activation of C-fiber afferent pathways due to colon-to-bladder cross sensitization in the rodent models [40•, 41•]. Dichotomizing afferents that send axonal branches to different target organs and/or the convergence of sensory innervation from different pelvic organs onto the same second-order neurons in the spinal cord have been put forward as mechanisms inducing this viscero-visceral cross-organ sensitization [42,43,44]. This mechanism could contribute to the symptoms in some IC/BPS patients.
Cross sensitization in the pelvic organ is also found between the bladder and the uterus as the co-existence of IC/BPS and endometriosis was reportedly as high as 65 to 69% [45, 46]. Accordingly, it has been reported that implantation of uterine tissue fragments to ectopic sites such as the peritoneum or the abdominal wall in rodents induces pelvic pain and bladder hypersensitivity [47, 48•]. A recent study has also demonstrated that female rats with uterine tissue implants to the mesocolon and the pelvic peritoneum exhibited bladder overactivity during TRPA1 receptor activation along with TRPA1 upregulation in afferent pathways, suggesting that TRPA1-dependent bladder cross-sensitization due to endometriosis could be involved in overlapping symptoms in IC/BPS and endometriosis [49•]. Overall, animal models with colonic inflammation or endometriosis could be useful for studying the cross-sensitization mechanism of pelvic organs that are involved as the outside-the-bladder etiology in the IC/BPS pathogenesis.
Psychological and Physical Stress Models
Recent studies have shown that various types of psychological or physical stress can cause urinary frequency and bladder pain in animal models [50•]. Psychological stress has been proposed as an important factor of provoking and worsening IC/BPS symptoms because previous clinical studies have demonstrated that IC/BPS symptoms had a correlation with stress levels in humans [51•]. Other studies have also shown that physical or psychological stress increases the risk of provoking IC/BPS symptoms in women who had experience of active military combat during service in the military [52,53,54]. In this regard, basic research studies have proven that psychological stress induced by water avoidance stress (WAS) can result in clinical and morphological features that are present in human IC/BPS patients, such as bladder hypersensitivity, denudation of the urothelium, and increased NGF in the bladder mucosa [55, 56•, 57,58,59,60]. WAS-induced psychological stress in rats also exhibits increased colon mobilization, which mimics the symptom of irritable bowel syndrome, a gastro-intestinal disorder that often coexisted in IC/BPS patients [7, 61]. Also, psychological stress induced by WAS in rats shows increased mast cell infiltration and NGF levels in the urothelium, increased extracellular distance and permeability of the bladder mucosa, leading to shortening of inter-contraction interval and increased bladder pain [50•, 62]. The WAS rat model does not require bladder irritation or any chemical injections, which makes this model very unique as it is a naturally occurring etiology. Further studies are expected to lead us to better understanding of the relation between the outside-the-bladder factors such as psychological stress and bladder dysfunction and pain sensation in IC/BPS.
Models of Multiple Mechanisms
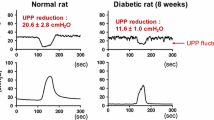
As discussed above, each model not only has its unique character, but also limitations. Therefore, recent studies have explored the IC/BPS pathogenesis by using multiple methods that have been utilized in IC/BPS research. This may be a reasonable approach, due to the recent evidence that Hunner type IC is a disease with an underlying condition of autoimmune disorders and that onset of occurring mucosal lesions is triggered by bladder inflammation [3•, 63•]. From this point of view, natural cause or autoimmune models combined with either inflammation or bladder irritation may be an adequate approach for evaluating the IC/BPS etiology. Recent studies have also reported the usage of the psychological stress model induced by WAS in rats with the combination of intravesical low-dose PS administration, which does not cause bladder stimulating effects in normal rats [56•]. Based on the results in this combination model, IC/BPS-like symptoms such as urinary frequency was observed accompanied by increased urothelial permeability, which was detected by MRI evaluation. The strongest point of these multiple mechanism models is that combination of different methods can compensate for each method’s shortfalls and can still maximize each method’s usefulness. The combination model could enable us to further understand the unclarified underlying etiology of IC/BPS in the future.
Summary and Conclusions
In this review article, we summarized the common animal models used for basic research of IC/BPS (Table 1). Although the etiology of IC/BPS is still not completely understood, the underlying mechanism is multifactorial, which makes it difficult to fully clarify the pathophysiological process of IC/BPS. Furthermore, the disease concept of IC and BPS, which used to be thought as related, has been proposed as two different phenotypes with different bladder pathologies [3•]. Thus, it remains challenging to expect a specific animal model to reproduce morphological and functional changes of IC/BPS completely as seen in human patients. Tomaszewski reported 4 statistically significant pathologic changes in IC/BPS bladders, which are mast cell infiltration, loss of the urothelium, and decreases of granulation tissues and vascular density in the lamina propria [64]. However, the diagnosis of IC/BPS are not always made by histological confirmation by bladder biopsy. Even with the absence of inflammation in the bladder mucosa, IC/BPS are often diagnosed by cystoscopic findings without biopsy [1•]. Thus, the proper diagnosis and treatment of IC/BPS phenotypes is often hindered. It has been proposed that the underlying causes of IC/BPS include inflammatory, vascular, and neurogenic factors, and these can cause IC/BPS symptoms by either a single or multiple combined factors. Currently, each animal model mimicking IC/BPS-like symptoms cannot cover all aspects of IC/BPS. Therefore, researchers should understand the pros and cons of each model and identify which animal model best represents the pathophysiological mechanisms of IC/BPS that are sought to be investigated. It is hoped that these research efforts would lead us to further understanding and development of treatment targets with better outcomes in clinical management of IC/BPS in the future.
Data Availability
No datasets were generated or analysed during the current study.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
• Clemens JQ, Erickson DR, Varela NP, Lai HH. Diagnosis and treatment of interstitial cystitis/bladder pain syndrome. J Urol. 2022;208(1):34–42. This article provides general information such as diagnosis and treatment of IC/BPS.
Birder L, Andersson KE. Animal modelling of interstitial cystitis/bladder pain syndrome. Int Neurourol J. 2018;22(Suppl 1):S3-9.
• Akiyama Y, et al. Interstitial cystitis/bladder pain syndrome: the evolving landscape, animal models and future perspectives. Int J Urol. 2020;27(6):491–503. This article provides updated information that Hunner type IC should be recognized as a different pathology compared to non-Hunner type IC and BPS.
Bjorling DE, Wang ZY, Bushman W. Models of inflammation of the lower urinary tract. Neurourol Urodyn. 2011;30(5):673–82.
Homan T, et al. Novel mouse model of chronic inflammatory and overactive bladder by a single intravesical injection of hydrogen peroxide. J Pharmacol Sci. 2013;121(4):327–37.
Dogishi K, Okamoto K, Majima T, Konishi-Shiotsu S, Homan T, Kodera M, Oyama S, Oyama T, Shirakawa H, Yoshimura N, Nakagawa T, Kaneko S. A rat long-lasting cystitis model induced by intravesical injection of hydrogen peroxide. Physiol Rep. 2017;5(4):e13127.
Lee UJ, et al. Chronic psychological stress in high-anxiety rats induces sustained bladder hyperalgesia. Physiol Behav. 2015;139:541–8.
Meuwese MC, et al. Endothelial surface layer degradation by chronic hyaluronidase infusion induces proteinuria in apolipoprotein E-deficient mice. PLoS ONE. 2010;5(12):e14262.
Shioyama R, et al. Long-lasting breaches in the bladder epithelium lead to storage dysfunction with increase in bladder PGE2 levels in the rat. Am J Physiol Regul Integr Comp Physiol. 2008;295(2):R714–8.
Chuang YC, et al. Intravesical protamine sulfate and potassium chloride as a model for bladder hyperactivity. Urology. 2003;61(3):664–70.
Jerde TJ, et al. Determination of mouse bladder inflammatory response to E. coli lipopolysaccharide. Urol Res. 2000;28(4):269–73.
Stein PC, Pham H, Ito T, Parsons CL. Bladder injury model induced in rats by exposure to protamine sulfate followed by bacterial endotoxin. J Urol. 1996;155(3):1133–8.
Olsson LE, Wheeler MA, Sessa WC, Weiss RM. Bladder instillation and intraperitoneal injection of Escherichia coli lipopolysaccharide up-regulate cytokines and iNOS in rat urinary bladder. J Pharmacol Exp Ther. 1998;284(3):1203–8.
Ogawa T, et al. CXCR3 binding chemokine and TNFSF14 over expression in bladder urothelium of patients with ulcerative interstitial cystitis. J Urol. 2010;183(3):1206–12.
Bosch PC. A randomized, double-blind, placebo-controlled trial of certolizumab pegol in women with refractory interstitial cystitis/bladder pain syndrome. Eur Urol. 2018;74(5):623–30.
Yang W, et al. A MAPP Network study: overexpression of tumor necrosis factor-alpha in mouse urothelium mimics interstitial cystitis. Am J Physiol Renal Physiol. 2018;315(1):F36–44.
Sanchez Freire V, et al. MicroRNAs may mediate the down-regulation of neurokinin-1 receptor in chronic bladder pain syndrome. Am J Pathol. 2010;176(1):288–303.
Montalbetti N, et al. Increased urothelial paracellular transport promotes cystitis. Am J Physiol Renal Physiol. 2015;309(12):F1070–81.
Montalbetti N, Rued AC, Taiclet SN, Birder LA, Kullmann FA, Carattino MD. Urothelial tight junction barrier dysfunction sensitizes bladder afferents. eNeuro. 2017;4(3):e0381-16.2017 1–18.
Osbaldiston GW, Taussig RA. Clinical report on 46 cases of feline urological syndrome. Vet Med Small Anim Clin. 1970;65(5):461–8.
Gao X, Buffington CA, Au JL. Effect of interstitial cystitis on drug absorption from urinary bladder. J Pharmacol Exp Ther. 1994;271(2):818–23.
Jasmin L, Carstens E, Basbaum AI. Interneurons presynaptic to rat tail-flick motoneurons as mapped by transneuronal transport of pseudorabies virus: few have long ascending collaterals. Neuroscience. 1997;76(3):859–76.
Rudick CN, Schaeffer AJ, Klumpp DJ. Pharmacologic attenuation of pelvic pain in a murine model of interstitial cystitis. BMC Urol. 2009;9:16.
Rudick CN, et al. Mast cell-derived histamine mediates cystitis pain. PLoS ONE. 2008;3(5):e2096.
Chen MC, Keshavan P, Gregory GD, Klumpp DJ. RANTES mediates TNF-dependent lamina propria mast cell accumulation and barrier dysfunction in neurogenic cystitis. Am J Physiol Renal Physiol. 2007;292(5):F1372–9.
de Groat WC, Yoshimura N. Afferent nerve regulation of bladder function in health and disease. Handb Exp Pharmacol. 2009;194:91–138.
Funahashi Y, et al. Intravesical application of rebamipide promotes urothelial healing in a rat cystitis model. J Urol. 2014;192(6):1864–70.
Song PH, et al. Comparison of 5 different rat models to establish a standard animal model for research into interstitial cystitis. Int Neurourol J. 2017;21(3):163–70.
Dang K, Bielefeldt K, Gebhart GF. Cyclophosphamide-induced cystitis reduces ASIC channel but enhances TRPV1 receptor function in rat bladder sensory neurons. J Neurophysiol. 2013;110(2):408–17.
Bon K, Lichtensteiger CA, Wilson SG, Mogil J. Characterization of cyclophosphamide cystitis, a model of visceral and referred pain, in the mouse: species and strain differences. J Urol. 2003;170(3):1008–12.
Hu VY, et al. COX-2 and prostanoid expression in micturition pathways after cyclophosphamide-induced cystitis in the rat. Am J Physiol Regul Integr Comp Physiol. 2003;284(2):R574–85.
Maeda D, et al. Hunner-type (classic) interstitial cystitis: a distinct inflammatory disorder characterized by pancystitis, with frequent expansion of clonal B-cells and epithelial denudation. PLoS ONE. 2015;10(11):e0143316.
Jin XW, et al. Establishment of a novel autoimmune experimental model of bladder pain syndrome/interstitial cystitis in C57BL/6 mice. Inflammation. 2017;40(3):861–70.
• Liu BK, et al. The effects of neurokinin-1 receptor antagonist in an experimental autoimmune cystitis model resembling bladder pain syndrome/interstitial cystitis. Inflammation. 2019;42(1):246–54. This article proposes the effect of neurokinin-1 antagonist on autoimmune cystitis in the animal model.
Bullock AD, Becich MJ, Klutke CG, Ratliff TL. Experimental autoimmune cystitis: a potential murine model for ulcerative interstitial cystitis. J Urol. 1992;148(6):1951–6.
Luber-Narod J, et al. Experimental autoimmune cystitis in the Lewis rat: a potential animal model for interstitial cystitis. Urol Res. 1996;24(6):367–73.
Zhang L, et al. An immunogenic peptide, T2 induces interstitial cystitis/painful bladder syndrome: an autoimmune mouse model for interstitial cystitis/painful bladder syndrome. Inflammation. 2017;40(6):2033–41.
Izgi K, et al. Uroplakin peptide-specific autoimmunity initiates interstitial cystitis/painful bladder syndrome in mice. PLoS ONE. 2013;8(8):e72067.
Kogan P, et al. Sub-noxious intravesical lipopolysaccharide triggers bladder inflammation and symptom onset in a transgenic autoimmune cystitis model: a MAPP network animal study. Sci Rep. 2018;8(1):6573.
• Yoshikawa S, et al. Pelvic organ cross-sensitization to enhance bladder and urethral pain behaviors in rats with experimental colitis. Neuroscience. 2015;284:422–9. This article explored the pelvic organ cross-sensitization between the bladder and the colon.
• Kawamorita N, et al. Liposome based intravesical therapy targeting nerve growth factor ameliorates bladder hypersensitivity in rats with experimental colitis. J Urol. 2016;195(6):1920–6. This study explored the effect of intravesical NGF treatment agaisnt bladder dysfunction.
Christianson JA, et al. Convergence of bladder and colon sensory innervation occurs at the primary afferent level. Pain. 2007;128(3):235–43.
Pezzone MA, Liang R, Fraser MO. A model of neural cross-talk and irritation in the pelvis: implications for the overlap of chronic pelvic pain disorders. Gastroenterology. 2005;128(7):1953–64.
Qin C, Malykhina AP, Akbarali HI, Foreman RD. Cross-organ sensitization of lumbosacral spinal neurons receiving urinary bladder input in rats with inflamed colon. Gastroenterology. 2005;129(6):1967–78.
Paulson JD, Delgado M. Chronic pelvic pain: the occurrence of interstitial cystitis in a gynecological population. JSLS. 2005;9(4):426–30.
Wu CC, Chung SD, Lin HC. Endometriosis increased the risk of bladder pain syndrome/interstitial cystitis: a population-based study. Neurourol Urodyn. 2018;37(4):1413–8.
Morrison TC, Dmitrieva N, Winnard KP, Berkley KJ. Opposing viscerovisceral effects of surgically induced endometriosis and a control abdominal surgery on the rat bladder. Fertil Steril. 2006;86(4 Suppl):1067–73.
• Nunez-Badinez P, et al. Preclinical models of endometriosis and interstitial cystitis/bladder pain syndrome: an Innovative Medicines Initiative-PainCare initiative to improve their value for translational research in pelvic pain. Pain. 2021;162(9):2349–65. This article highlights a variety of animal models for translational research of IC/BPS.
• Hayashi N, et al. Ectopic endometriosis in the pelvic cavity evokes bladder hypersensitivity via transient receptor potential ankyrin 1 hyperexpression in rats. Int Urogynecol J. 2023;34(6):1211–8. This article explored the relation of endometriosis and IC/BPS induced by bladder cross-sensitization in the animal model.
• Smith AL, et al. The effects of acute and chronic psychological stress on bladder function in a rodent model. Urology. 2011;78(4):967 e1-7. This article explored the effect of psychological stress induced by WAS against bladder dysfunction.
• Lutgendorf SK, et al. Stress and symptomatology in patients with interstitial cystitis: a laboratory stress model. J Urol. 2000;164(4):1265–9. This article showed the correlation of stress and bladder symptoms in interstitial cystitis patients.
McKernan LC, et al. Posttraumatic stress disorder in interstitial cystitis/bladder pain syndrome: relationship to patient phenotype and clinical practice implications. Neurourol Urodyn. 2019;38(1):353–62.
Jamal GA. Gulf War syndrome–a model for the complexity of biological and environmental interaction with human health. Adverse Drug React Toxicol Rev. 1998;17(1):1–17.
Bradley CS, et al. Overactive bladder and mental health symptoms in recently deployed female veterans. J Urol. 2014;191(5):1327–32.
Matos R, et al. The water avoidance stress induces bladder pain due to a prolonged alpha1A adrenoceptor stimulation. Naunyn Schmiedebergs Arch Pharmacol. 2017;390(8):839–44.
• Saito T, et al. Functional and histologic imaging of urinary bladder wall after exposure to psychological stress and protamine sulfate. Sci Rep. 2021;11(1):19440. This article showed the effect of stress against bladder permeability in the urothelium in rats which was evaluated by MRI.
Chen W, et al. Elevated level of nerve growth factor in the bladder pain syndrome/interstitial cystitis: a meta-analysis. Springerplus. 2016;5(1):1072.
Ackerman AL, et al. The Glt1 glutamate receptor mediates the establishment and perpetuation of chronic visceral pain in an animal model of stress-induced bladder hyperalgesia. Am J Physiol Renal Physiol. 2016;310(7):F628–36.
Hurst RE, et al. Increased bladder permeability in interstitial cystitis/painful bladder syndrome. Transl Androl Urol. 2015;4(5):563–71.
Gao Y, Zhang R, Chang HH, Rodriguez LV. The role of C-fibers in the development of chronic psychological stress induced enhanced bladder sensations and nociceptive responses: a multidisciplinary approach to the study of urologic chronic pelvic pain syndrome (MAPP) research network study. Neurourol Urodyn. 2018;37(2):673–80.
Qin HY, Cheng CW, Tang XD, Bian ZX. Impact of psychological stress on irritable bowel syndrome. World J Gastroenterol. 2014;20(39):14126–31.
Cetinel S, et al. Protective effect of melatonin on water avoidance stress induced degeneration of the bladder. J Urol. 2005;173(1):267–70.
• Akiyama Y, et al. Increased CXCR3 expression of infiltrating plasma cells in Hunner type interstitial cystitis. Sci Rep. 2016;6:28652. This article revieled the differencce between hunner type interstitial cystitis and other diseases causing bladder pain.
Tomaszewski JE, et al. Biopsy features are associated with primary symptoms in interstitial cystitis: results from the interstitial cystitis database study. Urology. 2001;57(6 Suppl 1):67–81.
Funding
No funding was received for this article.
Author information
Authors and Affiliations
Contributions
T.S wrote the main manuscript. T.O, P.T and N.Y reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Saito, T., Ogawa, T., Tyagi, P. et al. Experimental Animal Models for IC/BPS. Curr Bladder Dysfunct Rep 19, 119–126 (2024). https://doi.org/10.1007/s11884-024-00753-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11884-024-00753-7