Abstract
Purpose of Review
Non-invasive measurements such as arterial stiffness serve as proxy surrogates for detection of early atherosclerosis and ASCVD risk stratification. These surrogate measurements are influenced by age, gender, and ethnicity and affected by the physiological changes of puberty and somatic growth in children and adolescents.
Recent Findings
There is no consensus of the ideal method to measure surrogate markers in youth (< 18 years of age), nor standardized imaging protocols for youth. Currently, pediatric normative data are available but not generalizable.
Summary of the Review
In this review, we provide rationale on how currently used surrogates can help identify subclinical atherosclerosis in youth and affirm their role in identifying youth at risk for premature CVD.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Atherosclerosis: Evidence of origins in youth
Vascular aging begins at conception, and precursors of atherosclerosis are present as early as fetal life [1, 2]. Atherosclerosis is a chronic process that begins early in life and accelerated by adverse genetic and acquired atherosclerotic cardiovascular disease (ASCVD) risk factors such as obesity, hypertension, dyslipidemia, and insulin resistance. An autopsy study of 204 young persons, 2–39 years, showed that as the number of ante-mortem ASCVD risk factors increased, so did the severity of asymptomatic coronary and aortic atherosclerosis [3].
Table 1 provides ASCVD risk factors as updated by the American Heart Association [4••].
How to Assess the Vasculature for CVD in Youth
Several non-invasive methods have been proposed to assess vascular health in youth, including (1) vascular structure which measures carotid intima media thickness (cIMT), (2) endothelial function which measures metabolic capability of endothelium to release nitrous oxide in response to stimuli, and (3) arterial stiffness which measures the intrinsic “elastic” properties of the arterial wall [5–7].
These measures are defined as “surrogates” as they are noninvasive measurements which are convenient to perform, have shorter imaging time, and do not require use of radioactive intravenous contrast materials. Therefore, they serve as a “proxy” measurements of other gold standard techniques used for CVD risk stratification such as angiography, cardiac MRI (magnetic resonance imaging), cardiac positron emission tomography (PET) scanning, and coronary computed tomographic (CT) angiography.
Non-invasive methods examining structural and functional vascular parameters such as arterial wall thickness, stiffness, and endothelial function are commonly used in adults for risk stratification and prediction of CVD such as myocardial infraction (MI) and stroke. Adult with elevated ASCVD risk factors (n = 2232; 63 years, 58% women) had thicker measurements of cIMT, which predicted stroke and myocardial infarction [8], and elevated baseline pulse wave velocity (PWV) was associated with a 48% in CVD risk even after adjustment for ASCVD risk factors [9]. While these techniques are available in youth studies, validating their utility is limited.
In this review, we provide rationale on how currently available surrogates can help identify the presence of subclinical atherosclerosis and affirm their role in identifying ASCVD risk.
Most measurements of vascular surrogates require an overnight fast and performed after the subject has been supine ≥ 10 min in a quiet room. In this review, we provide information from the literature within the past 5 years for the most commonly used surrogates. Surrogates are rated from those that are the most clinically relevant and useful to those that are less so.
Vascular Structure
**Carotid intima media thickness (cIMT) is the average of the end diastolic intima-media thickness of the right and left common carotid arterial far wall (10 mm proximal to the bulb) using B mode imaging and a 12-MHz linear array transducer, with automatic edge detection analysis technology. Imaging protocols are used in pediatric studies and may not align with the standard assessment guidelines published by American Heart Association (1). Sass et al. studied cIMT in 160 children (10–18 years) and found no correlation with age and sex [10].
In normal-weight children (n = 141; age 12.5 years), Torigoe [11••] reported mean cIMT 0.44 (interquartile range = 0.41–0.47).cIMT has been measured in high-risk groups such as familial hypercholesterolemia (FH) and diabetes with over 400 publication reporting results using this surrogate in the past 5 years (Table 2). cIMT increases across CVD risk factors, with the highest values reported in adolescents with type 2 diabetes (T2D), compared to those with hypertension, high triglycerides/low HDL (insulin resistance), followed by youth with obesity, being significantly higher compared to lean peers [12, 13]. In a 40-year longitudinal study of 3 to 18-year-old Finnish children (Young Finns Study: YFS; n = 1809), low HDL/LDL ratio in childhood and adulthood translated to a greater adult cIMT compared to other ratio trajectories (improving, deteriorating, consistently good) [14]. Studies of obese, T2D, and lean adolescents have shown cIMT progression (average 4.6 years, n = 226) is determined by age, baseline cIMT, glucose, and LDL-C at baseline [15].
Advantages and Disadvantages
cIMT is a safe and reproducible surrogate which can track subclinical atherosclerosis and can also be used to assess effectiveness of interventions to reverse early atherosclerosis. cIMT physiologically increases with age, growth [16–19], male gender [19, 20], pubertal maturation [20], ethnicity [17], and geography [21, 22]. Normal values of cIMT in youth differ by tracing method (point to point versus manual trace versus auto trace) at locations such as common carotid, bulb, and internal and composite cIMT. When manual tracing was used in 275 healthy lean children, cIMT measurements differed by site, the common carotid versus bulb versus internal cIMT. Combined AHA and European Pediatric Cardiology Working Group [23] published normal values but recognized that scanning and readings differed by the side (right versus left carotid or both) and site (common vs. bulb vs. internal vs. composite) which were measured (1).
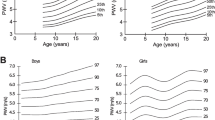
Recently, semi-automated edge detection programs such as radiofrequency signal tracing quality intima media thickness (RF-QIMT) have emerged as more accurate method since they circumvent B mode image quality and the level of experience of the vascular ultrasonographer. Torkar et al. published mean CIMT using the RF-QIMT in 1137 non-obese normotensive children (mean age 12 + 3.5 years, females n = 625) using age, height, and gender-specific percentile tables, showing cIMT increased with age, height, hip circumference, BMI, and is higher in males [24].
Endothelial Function
**Flow mediated dilatation (FMD) uses a 5–12 MHz linear array transducer and automatic edge detection algorithm to obtain longitudinal end diastolic images of the brachial artery above the antecubital fossa. Images are obtained 1 min before blood pressure cuff inflation, during the 5-min inflation (50 mmHg > systolic blood pressure to induce ischemia) and 5-min post deflation (usually at 60, 90, and 120 s). FMD is calculated as the percentage increase in diameter after reactive hyperemia compared to baseline (1). FMD reaches a peak at 10 years-of-age and declines after 60 years-of-age, being affected by age, BMI, and resting blood flow [25]. Torigoe [11••] showed in normal weight children (n = 141; age 12.5 years) a change in FMD% of 7.1% (IQR 5.2–9.7).
Studies
Table 3 shows some key studies among over 100 articles published in the last 5 years of disease states which are considered high to moderate risk for CVD. In healthy adolescents, a lower apolipoprotein B/apolipoprotein a ratio was associated with lower FMD measured 21 years later, a finding which was independent of LDL-C levels at baseline [26, 27]. In youth with FH (n = 60; 7–17 years), there is lower mean FMD compared to healthy controls although there is wide variability [28]. Urbina et al. showed FMD to be significantly different between lean (n = 241) versus obese (n = 234) versus T2D (n = 195) in youth aged 10–24 years (6.97 ± 1.19 vs 5.51 ± 1.04 vs 5.28 ± 1.00: all p < 0.05) [29]. Youth with T2D (n = 60) have reduced FMD (5.2 ± 0.9 vs. 6.1 ± 1.2%/mmHg: p < 0.01) compared to those with T1D (n = 535) [30].
Peripheral Arterial Tonometry (PAT: Non-Ultrasound Measure)
An appropriate finger cuff is placed on the index finger of each hand and inflates to sense blood volume at baseline and after ischemia (cuff inflated for 5 min), and the difference was used to derive the reactive hyperemia index (RHI). Laser flow Doppler (LFD) measures microvascular function and correlates with FMD [31].
Advantages and Disadvantages
All endothelial measurements (FMD, PAT, and LFD) require expertise and operator training as repeat measurements can vary by 5–10%, have biological variability [32, 33], and are affected by fasting versus non-fasting state, temperature, position of probe, and physiological hemodynamic changes such as menstruation in females [34, 35]. FMD when used as the primary surrogate often does not show measurement differences between the ASCVD risk and control group, and the need to correct for shear rate (mean velocity at baseline) is unclear as the associations between ASCVD risk factors, and FMD may be attributable to reduce stimulus for dilation rather than impaired response to hyperemia (9). Other investigators choose not to correct for shear rate as they state that the relationship between shear rate and FMD is weak, nonlinear, or varies between samples, and that ratio normalization should not be applied [36].
***Arterial stiffness describes the stiffness of the arterial wall which is modulated by the integrity of the extracellular matrix as well as the tone of the smooth muscle tone (endothelial function) in the vessel wall. Arterial stiffness measures the rate at which a pressure waves along a vessel segment. The American Heart Association [37] has published a recommendation of standardizing vascular research dealing with arterial stiffness.
Arterial stiffness can be measured using MRI (higher cost, requires access to a scanner), ultrasound measures (arterial distensibility of carotid, aorta and brachial vessels) or echocardiography (pulse wave velocity), or non-imaging modalities like pulse wave velocity (PWV) and augmentation index.
Carotid stiffness (ultrasound) is the baseline 2D image measurement of the artery followed by M mode cursor to measure minimum and maximum stiffness of the carotid artery. Instead of manual measurements, a radiofrequency wall tracker can be used.
Pulse wave velocity (PWV) records electrocardiographic-gated waveforms between carotid and femoral arteries (cf PWV: stiffness of central arteries) or carotid and radial arteries (cr PWV: stiffness of peripheral arteries). The distance between the two points is measured and PWV = length/ transit time in m/s, with higher PWV reflective of stiffer vessels. Tonometry uses pressure sensors (hand held, clamps, or cuffs) with applanation tonometer (Sphygmocor AtCor Medical, Australia) being the most widely used. Published reproducibility of PWV using with SphygmorCor by Bland Altman analysis is excellent [38]. Mechanotransducer-based techniques (Complior, ALAM Medical France) and pulse pen (DiaTecne, Milan Italy) are devices used widely in Europe. Volumetric, photoplethysmographic, and oscillometric methods are also used. Torigoe et al. (11) showed in normal weight children (n = 141; age 12.5 years) cf PWV is 5.2 (4.4–5.6 m/s) and cr PWV 6.8 (6.2–7.5 m/s).
Table 4 lists key studies among the over 500 PWV publications within the last 5 years. The number of ASCVD risk factors (high LDL-C) present in childhood is associated with increased PWV measured at 30–45 years [39]. When obese and lean adolescents were compared a high TG/HDL ratio reflected more atherogenic particles, and an increased ratio was associated with greater PWV in obese youth [40, 41]. Wadwa et al. reported in the SEARCH study that youth (age 10–23 years) with T2D (n = 60) have greater impairments in PWV than age-matched youth with T1D (n = 535 PWV: 6.4 ± 1.3 vs. 5.3 ± 0.8 m/s: p < 0.01) [30]. Studies in adolescents with FH have shown that LDL-C, LDL sub particle size, and number were not independent predictors of PWV, though HDL-size did appear to be a predictor, independent of ASCVD risk markers [42]. Overall, determinants of PWV progression over time include adiposity, BP, glycemic control, and LDL [43•].
Augmentation index (AI) and central waveform are also measured. Pressure peaks created by the antegrade waveform (from the left ventricle) and retrograde (reflected from the periphery to the center) create the augmentation pressure; AI is derived as the augmentation pressure (difference in the amplitude of the two waves)/pulse pressure (difference between systolic and diastolic central arterial pressure) × 100 adjusted to a heart rate of 75 beats/min [37]. Healthy flexible vessels will return waveform slowly arriving late in the cardiac cycle while stiff vessels return the waveform during early systole augmenting central aortic pressure [44]. The augmentation index adjusted to 75 beats/min (AIx 75) in study of 141 children and adolescents (age = 12.5 years (6.7–15.2 years); 48% male, weight 43.4 kg (23.9–57) was − 5 (− 13 to 5). AIx 75 was significantly different between lean (n = 241) versus obese (n = 234) versus T2D (n = 195) aged 10–24 years (− 0.5 ± 10.8 vs 2.7 ± 11.6 vs 6.6 ± 11.3: all p < 0.05) (29). Recent follow up of adolescents with T2D (Treatment Options of Adolescents and Youth: TODAY n = 304, 34% male; duration of diabetes 8 years) reported indices of PWV and AIx (75%) worsened over the 5-year assessment interval (cf PWV 6.3 to 7.1 m/s; cr PWV 7.8 to 9 m/s; AIx 9.4 to 14.9), and these changes tracked with higher BP measurements and increasing levels of HbA1c [45].
Advantages and Disadvantages
Longitudinal cohorts such as the Cardiovascular Risk in Young Finns have demonstrated higher PWV in adulthood with clustering of ASCVD in childhood [46]. Investigators have found that arterial stiffness increases with age [47, 48] which is related to the vessel wall size and distensibility of the vessel wall, starting around age 2.3 years-of-age and plateauing around age 15 years as measured using MRI imaging [49]. Fischer et al. found sex differences in PWV both before and after puberty [48] while in contrast, Voges found none [49]. PWV also changed by race and sex in a study of 559 young adults (mean 22 years) [50]. Factors confounding the measurement of the arterial stiffness are mean arterial pressure and heart rate recorded at the time of measurements [51, 52]. Measurements should be conducted in a quiet temperature-controlled room, performed after participants have supine for 10 min, caffeine avoided for 2–4 h, and in female subjects at the same stage during their menstrual cycle. These methodological confounders should be considered when comparing indexes obtained from different vascular beds (carotid femoral; cf versus brachial; ba PWV). Selective devices (SphycomoCor versus Complior) report 5–15% differences in values related to the algorithm used. There is also a lack of agreement of what constitutes normal PWV in youth when comparing oscillometric device (single point estimate) which tend to be lower, versus results utilizing a tonometric device. Brachial ankle PWV is reported in cm/s rather than m/s, but results are much higher than carotid femoral PWV (n = 262 adolescents; 12–18 years) [53]. Tonometric devices report similar results, and some have been cross validated [1, 54] [11••, 55]. The most important confounder is the distance (surface measurements between the recorded sites) which is often performed using a tape measure (calipers being preferred) and can account for up to 30% difference in the PWV calculation. Operators performing arterial stiffness require training and should be able to demonstrate consistently reproducible results.
*CAC
Agatston et al. used helical and spiral CT measurement of microcrystalline calcium within the lipid core to calculate a volume composite, which was calculated as coronary artery calcification (CAC). This modality has not been extensively used to study early atherosclerosis in youth, due to concern for radiation exposure, except in a few studies for Kawasaki disease [56], FH [57], and diabetes [58]. There exists no correlation with other vascular surrogates, and no threshold exists about the amount calcification by age, ethnicity, and sex. CAC is valuable as a surrogate for advanced vascular lesion; thus, it has a limited role in youth.
Issues with Measuring Vascular Surrogates in Youth
To date, the literature for measuring vascular parameters has been limited by the lack of references and the lack of standardization of the equipment and protocols used across centers. Vascular surrogates have a complex relationship with age and anthropometric variables as there are physiological changes in the arterial wall during periods of rapid somatic growth such as infancy and adolescence. Torigoe et al. [11••] studied the most common used vascular studies in 292 healthy children (0–18 years) and proposed pediatric reference values using multivariate regression models adjusting for the effect weight, height, and age.
Conclusions
Measurement of vascular health is important in primary prevention, and in those with subclinical disease, a helpful guide to determine the need for more aggressive treatment in high-risk ASCVD groups. Use of vascular surrogates in longitudinal studies has independently predicted cardiovascular end points such as MI, stroke, and death. Over the last few decades, several devices and different approaches have been used which have created challenges but also provided opportunities to better delineate the utility of surrogates in children and adolescents. There exist gaps in our understanding of surrogates in children and adolescents.
-
Lack of validation of measurement methods in children. Can dedicated devices be identified which are reliable non-invasive tools? This will require validation studies in youth undergoing simultaneous invasive catherization or MRI-based imaging modalities. Alternatively, it may be reasonable to validate studies using dedicated devices that have been widely used in prospective trials such as PWV measurements by SphygmoCor.
-
Lack of normative data by age/body, size/puberty stage, sex, and race. In the last 5 years, several studies have been performed by single centers to provide age, sex, and gender-specific normative data [11••, 24]. A comparison of different cohorts demonstrates high heterogeneity beyond ethnic and geographical factors limiting the generalizability of results. The American Heart Association [59], European Pediatric Cardiology [23], and American Society of Echocardiography [17] recognize the value of surrogates to provide actionable information on CVD risk especially in pediatric populations with moderate to high-risk ASCVD risk conditions. Such organization (1) needs to analyze the currently available literature and provided updated consensus statement on the acceptable imaging protocols, devices, and how to account for the confounding variables such as age, gender, sex, and ethnic differences. To date, in the USA, there is no normative data on vascular surrogates in children based on racial and ethnic differences. Therefore, such guidelines will serve as valuable resource for investigators planning to use surrogates in prospective studies.
-
Longitudinal data in children with high-risk ASCVD in the in Bogalusa study, Young Finns, and Avon Longitudinal Study of Parents and Children (ALSPAC) have shown over the past several decades that these surrogates can predict ASCVD outcomes. CIMT and PWV have predicted hard CV events, although normative data across pediatric populations are lacking. Endothelial function testing has high variability. With consensus and better reference values, surrogates will increasingly become standardized and offer a valid and reliable tool for ASCVD risk stratification, and to assess the effect of interventions in high-risk ASCVD groups
References
Urbina E, Williams R, Alpert B, Collins R, Daniels S, Hayman L, et al. Noninvasive assessment of subclinical atherosclerosis in children and adolescents: recommendations for standard assessment for clinical research: a scientific statement from the American Heart Association. Hypertension. 2009;54(5):919–50.
McGill HC Jr, McMahan CA, Herderick EE, Malcom GT, Tracy RE, Strong JP. Origin of atherosclerosis in childhood and adolescence. Am J Clin Nutr. 2000;72(5 Suppl):1307S–15S.
Berenson GS, Srinivasan SR, Bao W, Newman WP 3rd, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa heart study. N Engl J Med. 1998;338(23):1650–6.
de Ferranti SD, Steinberger J, Ameduri R, Baker A, Gooding H, Kelly AS, et al. Cardiovascular risk reduction in high-risk pediatric patients: a scientific statement from the American Heart Association. Circulation. 2019;139(13):e603–e34.
Stein JH, Korcarz CE, Mays ME, Douglas PS, Palta M, Zhang H, et al. A semiautomated ultrasound border detection program that facilitates clinical measurement of ultrasound carotid intima-media thickness. Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 2005;18(3):244–51.
Gepner AD, Keevil JG, Wyman RA, Korcarz CE, Aeschlimann SE, Busse KL, et al. Use of carotid intima-media thickness and vascular age to modify cardiovascular risk prediction. Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 2006;19(9):1170–4.
Bots ML, Evans GW, Riley WA, Grobbee DE. Carotid intima-media thickness measurements in intervention studies: design options, progression rates, and sample size considerations: a point of view. Stroke. 2003;34(12):2985–94.
O'Leary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL, Wolfson SK Jr. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular health study collaborative research group. N Engl J Med. 1999;340(1):14–22.
Mitchell GF, Hwang SJ, Vasan RS, Larson MG, Pencina MJ, Hamburg NM, et al. Arterial stiffness and cardiovascular events: the Framingham heart study. Circulation. 2010;121(4):505–11.
Sass C, Herbeth B, Chapet O, Siest G, Visvikis S, Zannad F. Intima-media thickness and diameter of carotid and femoral arteries in children, adolescents and adults from the Stanislas cohort: effect of age, sex, anthropometry and blood pressure. J Hypertens. 1998;16(11):1593–602.
Torigoe T, Dallaire F, Slorach C, Cardinal MP, Hui W, Bradley TJ, et al. New comprehensive reference values for arterial vascular parameters in children. Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 2020;33(8):1014–22.e4.
Shah AS, Dolan LM, Khoury PR, Gao Z, Kimball TR, Urbina EM. Severe obesity in adolescents and young adults is associated with sub-clinical cardiac and vascular changes. J Clin Endocrinol Metab. 2015:jc20144562.
Urbina EM, Khoury PR, McCoy C, Daniels SR, Kimball TR, Dolan LM. Cardiac and vascular consequences of pre-hypertension in youth. J Clin Hypertens (Greenwich, Conn). 2011;13(5):332–42.
Juonala M, Magnussen CG, Venn A, Dwyer T, Burns TL, Davis PH, et al. Influence of age on associations between childhood risk factors and carotid intima-media thickness in adulthood: the cardiovascular risk in young Finns study, the childhood determinants of adult health study, the Bogalusa heart study, and the Muscatine study for the international childhood cardiovascular cohort (i3C) consortium. Circulation. 2010;122(24):2514–20.
Ryder JR, Northrop E, Rudser KD, Kelly AS, Gao Z, Khoury PR, et al. Accelerated early vascular aging among adolescents with obesity and/or type 2 diabetes mellitus. J Am Heart Assoc. 2020;9(10):e014891.
Doyon A, Kracht D, Bayazit AK, Deveci M, Duzova A, Krmar RT, et al. Carotid artery intima-media thickness and distensibility in children and adolescents: reference values and role of body dimensions. Hypertension. 2013;62(3):550–6.
Stein JH, Korcarz CE, Hurst RT, Lonn E, Kendall CB, Mohler ER, et al. Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American Society of Echocardiography carotid intima-media thickness task force. Endorsed by the Society for Vascular Medicine. Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 2008;21(2):93–111. quiz 89-90
McMahan CA, Gidding SS, Viikari JS, Juonala M, Kähönen M, Hutri-Kähönen N, et al. Association of Pathobiologic Determinants of atherosclerosis in youth risk score and 15-year change in risk score with carotid artery intima-media thickness in young adults (from the cardiovascular risk in young Finns study). Am J Cardiol. 2007;100(7):1124–9.
Bohm B, Hartmann K, Buck M, Oberhoffer R. Sex differences of carotid intima-media thickness in healthy children and adolescents. Atherosclerosis. 2009;
Zanini J, Rodrigues TMB, Barra CB, Filgueiras M, Silva IN. Intima-media thickness of the carotid arteries is affected by pubertal maturation in healthy adolescents. Revista paulista de pediatria : orgao oficial da Sociedade de Pediatria de Sao Paulo. 2019;37(4):428–34.
Baldassarre D, Nyyssönen K, Rauramaa R, de Faire U, Hamsten A, Smit AJ, et al. Cross-sectional analysis of baseline data to identify the major determinants of carotid intima-media thickness in a European population: the IMPROVE study. Eur Heart J. 2010;31(5):614–22.
Kivimäki M, Lawlor DA, Juonala M, Smith GD, Elovainio M, Keltikangas-Järvinen L, et al. Lifecourse socioeconomic position, C-reactive protein, and carotid intima-media thickness in young adults: the cardiovascular risk in young Finns study. Arterioscler Thromb Vasc Biol. 2005;25(10):2197–202.
Dalla Pozza R, Ehringer-Schetitska D, Fritsch P, Jokinen E, Petropoulos A, Oberhoffer R. Intima media thickness measurement in children: a statement from the Association for European Paediatric Cardiology (AEPC) working group on cardiovascular prevention endorsed by the Association for European Paediatric Cardiology. Atherosclerosis. 2015;238(2):380–7.
Torkar AD, Plesnik E, Groselj U, Battelino T, Kotnik P. Carotid intima-media thickness in healthy children and adolescents: normative data and systematic literature review. Front Cardiovasc Med. 2020;7:597768.
Thijssen DH, Bullens LM, van Bemmel MM, Dawson EA, Hopkins N, Tinken TM, et al. Does arterial shear explain the magnitude of flow-mediated dilation?: a comparison between young and older humans. Am J Physiol Heart Circ Physiol. 2009;296(1):H57–64.
Juonala M, Viikari JSA, Khnen M, Solakivi T, Helenius H, Jula A, et al. Childhood levels of serum apolipoproteins B and A-I predict carotid intima-media thickness and brachial endothelial function in adulthood: the cardiovascular risk in young Finns study. J Am Coll Cardiol. 2008;52(4):293–9.
Juonala M, Viikari JS, Ronnemaa T, Marniemi J, Jula A, Loo BM, et al. Associations of dyslipidemias from childhood to adulthood with carotid intima-media thickness, elasticity, and brachial flow-mediated dilatation in adulthood: the cardiovascular risk in young Finns study. Arterioscler Thromb Vasc Biol. 2008;28(5):1012–7.
Sorensen KE, Celermajer DS, Georgakopoulos D, Hatcher G, Betteridge DJ, Deanfield JE. Impairment of endothelium-dependent dilation is an early event in children with familial hypercholesterolemia and is related to the lipoprotein(a) level. J Clin Invest. 1994;93(1):50–5.
Urbina EM, Kimball TR, Khoury PR, Daniels SR, Dolan LM. Increased arterial stiffness is found in adolescents with obesity or obesity-related type 2 diabetes mellitus. J Hypertens. 2010;28(8):1692–8.
Wadwa RP, Urbina E, Anderson A, Hamman R, Dolan L, Rodriguez B, et al. Measures of arterial stiffness in youth with type 1 and type 2 diabetes: the SEARCH for diabetes in youth study. Diabetes Care. 2010;
Cracowski JL, Minson CT, Salvat-Melis M, Halliwill JR. Methodological issues in the assessment of skin microvascular endothelial function in humans. Trends Pharmacol Sci. 2006;27(9):503–8.
Mahmud FH, Hill DJ, Cuerden MS, Clarson CL. Impaired vascular function in obese adolescents with insulin resistance. J Pediatr. 2009;155(5):678–82.
Shah AS, Gao Z, Dolan LM, Dabelea D, D'Agostino RB Jr, Urbina EM. Assessing endothelial dysfunction in adolescents and young adults with type 1 diabetes mellitus using a non-invasive heat stimulus. Pediatr Diabetes. 2015;16(6):434–40.
Donald AE, Charakida M, Falaschetti E, Lawlor DA, Halcox JP, Golding J, et al. Determinants of vascular phenotype in a large childhood population: the Avon longitudinal study of parents and children (ALSPAC). Eur Heart J. 2010;31(12):1502–10.
Shah AS, Gao Z, Urbina EM, Kimball TR, Dolan LM. Prediabetes: the effects on arterial thickness and stiffness in obese youth. J Clin Endocrinol Metab. 2014;99(3):1037–43.
Atkinson G, Batterham AM, Black MA, Cable NT, Hopkins ND, Dawson EA, et al. Is the ratio of flow-mediated dilation and shear rate a statistically sound approach to normalization in cross-sectional studies on endothelial function? J Appl Physiol (Bethesda, Md : 1985). 2009;107(6):1893–9.
Townsend RR, Wilkinson IB, Schiffrin EL, Avolio AP, Chirinos JA, Cockcroft JR, et al. Recommendations for improving and standardizing vascular research on arterial stiffness: a scientific statement from the American Heart Association. Hypertension. 2015;66(3):698–722.
Wimmer NJ, Townsend RR, Joffe MM, Lash JP, Go AS. Correlation between pulse wave velocity and other measures of arterial stiffness in chronic kidney disease. Clin Nephrol. 2007;68(3):133–43.
Aatola H, Hutri-Kähönen N, Juonala M, Viikari JS, Hulkkonen J, Laitinen T, et al. Lifetime risk factors and arterial pulse wave velocity in adulthood: the cardiovascular risk in young Finns study. Hypertension. 2010;55(3):806–11.
Shah AS, Dolan LM, Khoury PR, Gao Z, Kimball TR, Urbina EM. Severe obesity in adolescents and young adults is associated with subclinical cardiac and vascular changes. J Clin Endocrinol Metab. 2015;100(7):2751–7.
Shah AS, Khoury PR, Dolan LM, Ippisch HM, Urbina EM, Daniels SR, et al. The effects of obesity and type 2 diabetes mellitus on cardiac structure and function in adolescents and young adults. Diabetologia. 2011;54(4):722–30.
Urbina EM, McCoy CE, Gao Z, Khoury PR, Shah AS, Dolan LM, et al. Lipoprotein particle number and size predict vascular structure and function better than traditional lipids in adolescents and young adults. J Clin Lipidol. 2017;11(4):1023–31.
Shah AS, Gidding SS, El Ghormli L, Tryggestad JB, Nadeau KJ, Bacha F, et al. Relationship between arterial stiffness and subsequent cardiac structure and function in young adults with youth-onset type 2 diabetes: results from the TODAY study. Journal of the American Society of Echocardiography : official publication of the American Society of Echocardiography. 2022;35(6):620–8.e4.
Patange AR, Valentini RP, Du W, Pettersen MD. Vitamin D deficiency and arterial wall stiffness in children with chronic kidney disease. Pediatr Cardiol. 2012;33(1):122–8.
Shah AS, El Ghormli L, Gidding SS, Hughan KS, Levitt Katz LE, Koren D, et al. Longitudinal changes in vascular stiffness and heart rate variability among young adults with youth-onset type 2 diabetes: results from the follow-up observational treatment options for type 2 diabetes in adolescents and youth (TODAY) study. Acta Diabetol. 2022;59(2):197–205.
Koivistoinen T, Hutri-Kähönen N, Juonala M, Aatola H, Kööbi T, Lehtimäki T, et al. Metabolic syndrome in childhood and increased arterial stiffness in adulthood: the cardiovascular risk in young Finns study. Ann Med. 2011;43(4):312–9.
Salvi P, Revera M, Joly L, Reusz G, Iaia M, Benkhedda S, et al. Role of birth weight and postnatal growth on pulse wave velocity in teenagers. J Adolesc Health. 2012;51(4):373–9.
Fischer DC, Schreiver C, Heimhalt M, Noerenberg A, Haffner D. Pediatric reference values of carotid-femoral pulse wave velocity determined with an oscillometric device. J Hypertens. 2012;30(11):2159–67.
Voges I, Jerosch-Herold M, Hedderich J, Pardun E, Hart C, Gabbert DD, et al. Normal values of aortic dimensions, distensibility, and pulse wave velocity in children and young adults: a cross-sectional study. Journal of cardiovascular magnetic resonance : official journal of the Society for Cardiovascular Magnetic Resonance. 2012;14(1):77.
Liang X, Su S, Hao G, Snieder H, Treiber F, Kapuku G, et al. Determinants of pulse wave velocity trajectories from youth to young adulthood: the Georgia stress and heart study. J Hypertens. 2019;37(3):563–71.
Kim EJ, Park CG, Park JS, Suh SY, Choi CU, Kim JW, et al. Relationship between blood pressure parameters and pulse wave velocity in normotensive and hypertensive subjects: invasive study. J Hum Hypertens. 2007;21(2):141–8.
Giannattasio C, Failla M, Mangoni AA, Scandola L, Fraschini N, Mancia G. Evaluation of arterial compliance in humans. Clinical and experimental hypertension (New York, NY : 1993). 1996;18(3–4):347–62.
Im JA, Lee JW, Shim JY, Lee HR, Lee DC. Association between brachial-ankle pulse wave velocity and cardiovascular risk factors in healthy adolescents. J Pediatr. 2007;150(3):247–51.
Elmenhorst J, Hulpke-Wette M, Barta C, Dalla Pozza R, Springer S, Oberhoffer R. Percentiles for central blood pressure and pulse wave velocity in children and adolescents recorded with an oscillometric device. Atherosclerosis. 2015;238(1):9–16.
Antza C, Doundoulakis I, Stabouli S, Tziomalos K, Kotsis V. Masked hypertensives: a disguised arterial stiffness population. J Clin Hypertens (Greenwich, Conn). 2019;21(10):1473–80.
Frey EE, Matherne GP, Mahoney LT, Sato Y, Stanford W, Smith WL. Coronary artery aneurysms due to Kawasaki disease: diagnosis with ultrafast CT. Radiology. 1988;167(3):725–6.
Gidding SS, Bookstein LC, Chomka EV. Usefulness of electron beam tomography in adolescents and young adults with heterozygous familial hypercholesterolemia. Circulation. 1998;98(23):2580–3.
Bacha F, Edmundowicz D, Sutton-Tyrell K, Lee S, Tfayli H, Arslanian SA. Coronary artery calcification in obese youth: what are the phenotypic and metabolic determinants? Diabetes Care. 2014;37(9):2632–9.
Steinberger J, Daniels SR, Hagberg N, Isasi CR, Kelly AS, Lloyd-Jones D, et al. Cardiovascular health promotion in children: challenges and opportunities for 2020 and beyond: a scientific statement from the American Heart Association. Circulation. 2016;134(12):e236–55.
Monasso GS, Santos S, Silva CCV, Geurtsen ML, Oei E, Gaillard R, et al. Body fat, pericardial fat, liver fat and arterial health at age 10 years. Pediatr Obes. 2022;17(10):e12926.
Agbaje AO, Barker AR, Mitchell GF, Tuomainen TP. Effect of arterial stiffness and carotid intima-media thickness progression on the risk of Dysglycemia, insulin resistance, and dyslipidemia: a temporal causal longitudinal study. Hypertension. 2022;79(3):667–78.
Juonala M, Wu F, Sinaiko A, Woo JG, Urbina EM, Jacobs D, et al. Non-HDL cholesterol levels in childhood and carotid intima-media thickness in adulthood. Pediatrics. 2020;145(4)
Farello G, Antenucci A, Stagi S, Mazzocchetti C, Ciocca F, Verrotti A. Metabolically healthy and metabolically unhealthy obese children both have increased carotid intima-media thickness: a case control study. BMC Cardiovasc Disord. 2018;18(1):140.
Garcia-Espinosa V, Bia D, Castro J, Zinoveev A, Marin M, Giachetto G, et al. Peripheral and central aortic pressure, wave-derived reflection parameters, local and regional arterial stiffness and structural parameters in children and adolescents: impact of body mass index variations. High blood Pressure & Cardiovascular Prevention : the official journal of the Italian Society of Hypertension. 2018;25(3):267–80.
Gooty VD, Sinaiko AR, Ryder JR, Dengel DR, Jacobs DR Jr, Steinberger J. Association between carotid intima media thickness, age, and cardiovascular risk factors in children and adolescents. Metab Syndr Relat Disord. 2018;16(3):122–6.
Calabrò MP, Carerj S, Russo MS, Luca FL, Onofrio MT, Antonini-Canterin F, et al. Carotid artery intima-media thickness and stiffness index β changes in normal children: role of age, height and sex. J Cardiovasc Med (Hagerstown). 2017;18(1):19–27.
Bruzzi P, Predieri B, Madeo S, Lami F, Iughetti L. Longitudinal evaluation of endothelial markers in children and adolescents with familial hypercholesterolemia. Acta bio-medica : Atenei Parmensis. 2021;92(5):e2021343.
Kosmeri C, Milionis H, Vlahos AP, Benekos T, Bairaktari E, Cholevas V, et al. The impact of dyslipidemia on early markers of endothelial and renal dysfunction in children. J Clin Lipidol. 2021;15(2):292–300.
Kosmeri C, Siomou E, Vlahos AP, Milionis H. Review shows that lipid disorders are associated with endothelial but not renal dysfunction in children. Acta Paediatr. 2019;108(1):19–27.
Hussain KS, Gulati R, Satheesh S, Negi VS. Early-onset subclinical cardiovascular damage assessed by non-invasive methods in children with juvenile idiopathic arthritis: analytical cross-sectional study. Rheumatol Int. 2021;41(2):423–9.
Couch SC, Saelens BE, Khoury PR, Dart KB, Hinn K, Mitsnefes MM, et al. Dietary approaches to stop hypertension dietary intervention improves blood pressure and vascular health in youth with elevated blood pressure. Hypertension. 2021;77(1):241–51.
Ishikawa T, Seki K. The association between oxidative stress and endothelial dysfunction in early childhood patients with Kawasaki disease. BMC Cardiovasc Disord. 2018;18(1):30.
Pillay S, Anderson J, Couper J, Maftei O, Gent R, Peña AS. Children with type 1 diabetes have delayed flow-mediated dilation. Can J Diabetes. 2018;42(3):276–80.
Li AM, Celermajer DS, Chan MH, Sung RY, Woo KS. Reference range for brachial artery flow-mediated dilation in healthy Chinese children and adolescents Hong Kong medical journal = Xianggang yi xue za zhi 2018;24 Suppl 3(3):36–38.
Anderson JJA, Couper JJ, Giles LC, Leggett CE, Gent R, Coppin B, et al. Effect of metformin on vascular function in children with type 1 diabetes: a 12-month randomized controlled trial. J Clin Endocrinol Metab. 2017;102(12):4448–56.
Haley JE, Woodly SA, Daniels SR, Falkner B, Ferguson MA, Flynn JT, et al. Association of Blood Pressure-Related Increase in vascular stiffness on other measures of target organ damage in youth. Hypertension. 2022;79(9):2042–50.
Fan B, Zhang T, Li S, Yan Y, Fan L, Bazzano L, et al. Differential roles of life-course cumulative burden of cardiovascular risk factors in arterial stiffness and thickness. Can J Cardiol. 2022;38(8):1253–62.
Shah AS, Isom S, D'Agostino R, Dolan LM, Dabelea D, Imperatore G, et al. Longitudinal changes in arterial stiffness and heart rate variability in youth-onset type 1 versus type 2 diabetes: the SEARCH for diabetes in youth study. Diabetes Care. 2022;45(7):1647–56.
Higgins S, Zemel BS, Khoury PR, Urbina EM, Kindler JM. Visceral fat and arterial stiffness in youth with healthy weight, obesity, and type 2 diabetes. Pediatr Obes. 2022;17(4):e12865.
Agbaje AO, Barker AR, Tuomainen TP. Cardiorespiratory fitness, fat mass, and Cardiometabolic health with endothelial function, arterial elasticity, and stiffness. Med Sci Sports Exerc. 2022;54(1):141–52.
Chien KJ, Huang HW, Weng KP, Huang SH, Li SC, Lin CC, et al. Arterial stiffness late after Kawasaki disease in children: assessment by performing brachial-ankle pulse wave velocity. Journal of the Chinese Medical Association : JCMA. 2020;83(10):931–5.
Wiromrat P, Bjornstad P, Vinovskis C, Chung LT, Roncal C, Pyle L, et al. Elevated copeptin, arterial stiffness, and elevated albumin excretion in adolescents with type 1 diabetes. Pediatr Diabetes. 2019;20(8):1110–7.
Skrzypczyk P, Przychodzień J, Mizerska-Wasiak M, Kuźma-Mroczkowska E, Stelmaszczyk-Emmel A, GóRska E, et al. Asymmetric dimethylarginine is not a marker of arterial damage in children with glomerular kidney diseases. Cent Eur J Immunol. 2019;44(4):370–9.
Hudson L, Kinra S, Wong I, Cole TJ, Deanfield J, Viner R. Is arterial stiffening associated with adiposity, severity of obesity and other contemporary cardiometabolic markers in a community sample of adolescents with obesity in the UK? BMJ Paediatr Open. 2017;1(1):e000061.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Preneet Cheema Brar declares no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Brar, P.C. Can Surrogate Markers Help Define Cardiovascular Disease in Youth?. Curr Atheroscler Rep 25, 275–298 (2023). https://doi.org/10.1007/s11883-023-01101-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11883-023-01101-6