Abstract
Pollution-related air quality deterioration has affected public health in many large cities worldwide, including Ho Chi Minh city (HCMC) in Vietnam. The health effects in this area attributed to fine particulate matter (PM2.5) account for 81.31% of all major air pollutant-related deaths. Over the past two decades, epidemiological studies have demonstrated that both short- and long-term PM2.5 pollution exposures are associated with increased mortality and morbidity. However, research on the economic damages caused by this type of pollution is lacking. The goal of this study was to assess PM2.5-related human health impacts and the corresponding economic damage in HCMC. The modelling approach applied in this study, including the coupled Weather Research and Forecasting (WRF)/Community Multiscale Air Quality Modelling System (CMAQ) models, for estimating PM2.5 distribution was combined with the models of short-term human health impacts and economic valuation quantification. Results indicated the short-term effects of health endpoints caused by PM2.5, including 174 (95% CI: 16; 340) premature deaths, 117,632 (95% CI: 231, 850; 368,926) hospital admission cases and 162,455 (95% CI: − 710.465; 531,153) emergency visits. The total economic losses have been estimated to exceed 3 trillion VND (equivalent to approximately 410 million USD), accounting for approximately 0.25% of the total gross regional domestic product (GRDP) of HCMC in 2018. Therefore, the results of this study provide compelling and up-to-date evidence for HCMC’s policymakers to propose PM2.5 pollution control measures and develop a clean air action plan with Vision 2025 to reduce adverse impacts on public health and obtain economic benefits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vietnam is among the top 10 countries most strongly affected by air pollution, tending to increase in big urban and industrial zones. The current rapid urbanisation and accelerating economic development in large cities, such as Ho Chi Minh city (HCMC), have caused a multitude of environmental and social issues, posing a serious challenge to PM2.5 pollution management. Short- and long-term exposures to PM2.5 pollution has been shown to be one of the leading causes of the global burden of disease, especially in low- and middle-income countries (Stanaway et al., 2018). According to the World Air Quality Report of 2020 (IQAir, 2020), Vietnam suffers 10.8 to 13.2 billion USD in economic losses related to ambient air pollution each year, equivalent to approximately 5% gross domestic product of the entire nation. Associations between PM2.5 concentrations and human health have been demonstrated in several epidemiological studies in Vietnam. However, there have not been any available studies that comprehensively clarify the true impact of PM2.5 on public health and quantify the losses in economic valuation due to PM2.5 pollution in Vietnam. This is a crucial foundation for the development of a clean air action plan for HCMC, and the basis for determining compensation for damage caused by pollution, as the principle of “polluters must pay money” is clearly defined in the Law on Environmental Protection 2014 and the Civil Code 2015 of Vietnam.
Additionally, the legal policy on air pollution control that focuses on PM2.5 is still quite limited and lacks synchronisation among localities in Vietnam. As of the end of October 2013, this is the first time that the Ministry of Natural Resources and Environment of Vietnam has added a new threshold for PM2.5 concentrations to the national ambient air quality standard (NAAQS), also known as QCVN 05:2013/BTNMT, based on the proposal of the Vietnam Environment Administration. When comparing NAAQS with international standards, such as the European Union air quality guidelines (Europe, 2000) or the World Health Organisation air quality guidelines (WHO Standard) (WHO, 2021), Vietnam’s NAAQS on the average limit of PM2.5 concentration in the short-term (50 µg/m3, 24-h mean) and long-term (25 µg/m3, annual mean) is relatively low. This demonstrates the fact that if controlled according to NAAQS, the people of Vietnam, who are breathing in the PM2.5-contaminated air, still face a higher health risk than by other countries in the world, such as Europe and North America. In June 2016, the Prime Minister of Vietnam issued a decision approving the National Action Plan on air quality management to 2020, with a vision to 2025 (hereinafter referred to as the National Action Plan) (Decision on Approving the National Action Plan on Air Quality Management to 2020, Vision to 2025, 2016), which includes objectives to determine the current status of PM2.5 pollution in special urban areas; these are defined as urban areas directly under Central government, able to implement measures to reduce PM2.5 pollution from the main emission sources. However, currently in HCMC, the PM2.5 monitoring system from the National Environmental Monitoring Network managed by the Department of Natural Resources and Environment has not yet been formed. The reference PM2.5 concentration measurement results are extracted primarily from the database source of AirNow from one monitoring station located at the US Consulate General located in District 1, HCMC. The recorded results showed that the PM2.5 pollution levels in HCMC are relatively serious. The average PM2.5 concentration in 2016 at 29.6 µg/m3 also exceeded the limit specified by NAAQS and WHO Standard by approximately 1.2 and 3.0 times, respectively; and in 2017, there were 222 days (61% of the total number of days in the year) when PM2.5 concentration exceeded the daily average of WHO Standard 2006 (25 µg/m3) (Thu et al., 2018).
Therefore, given the urgency of the situation, to develop an effective air quality management strategy focusing on the main target of PM2.5, according to the future National Action Plan, an assessment of the current spatiotemporal variation of pollution levels of PM2.5 affecting public health and economic loss in HCMC is necessary to serve as a scientific basis for the proposal of PM2.5 control measures. The objectives of this study were to evaluate the acute mortality/morbidity burdens due to short-term PM2.5 exposure and the corresponding economic burden due to the types of health endpoints associated with respiratory and cardiovascular diseases in 2018. The research was implemented by applying modelling methods from the combined model system from the Weather Research and Forecasting and Community Multiscale Air Quality Modelling Systems (WRF/CMAQ) and Environmental Benefits Mapping and Analysis Program—Community Edition (BenMAP-CE) to maximise the limitations from the lack of PM2.5 data in HCMC and provide spatiotemporal estimation results. The results obtained from this study have contributed to determining the current status of PM2.5 pollution in HCMC, a city directly under the central government, and providing evidence for proposing measures to reduce PM2.5 pollution levels when the HCMC’s authority organises and implements them according to the National Action Plan with an orientation towards 2025.
Literature review
Exposure to PM2.5, a major urban air pollutant (Fold et al., 2020), has various adverse health effects and ultimate societal costs (Chowdhury and Dey, 2016; Fold et al., 2020; Jie Li et al., 2021; Yin et al., 2017a). Rapid urbanisation and industrialisation in developing countries are continuing to increase the concentration of air pollutants, attracting public attention (Xiong et al., 2019). Over the past two decades, the number of research papers on the relationship between PM2.5 pollution and its socioeconomic losses has increased rapidly, especially in studies from China (Y. Li et al., 2017; Lu et al., 2019; Luo et al., 2020; Xiao et al., 2022; Ye et al., 2021). In particular, a large number of epidemiological studies have demonstrated an increased risk of premature death (Apte et al., 2015; Arden Pope et al., 2011; Krewski et al., 2009; Lim et al., 2012; Mehta et al., 2013; A. C. Pope et al., 2009) and acute respiratory and cardiovascular diseases (Brook et al., 2004; Englert, 2004; C. A. Pope & Dockery, 2006) associated with short-term exposure to PM2.5 pollution. There is also evidence suggesting that exposure to PM2.5 exacerbates asthma and cardiovascular and pulmonary diseases (Yu et al., 2019; Zhang et al., 2021). According to the estimates of the Global Burden of Disease project, the number of premature deaths each year due to PM2.5 rose sharply from approximately 3.2 million people in 2010 (Evans et al., 2013) to 4.2 million by 2015 (Forouzanfar et al., 2016; Huy et al., 2018; Jin Li et al., 2018). The studies by Chen et al. (2017), Krewski et al. (2009) and Bayat et al. (2019) reported that when the PM2.5 concentration increased by 10 µg/m3, the related risks of all deaths, cardiopulmonary disease, lung cancer and ischaemic heart disease (IHD) increased by approximately 4%, 9%, 9% and 17%, respectively.
Several recent epidemiological studies in Vietnam, performed by Nhung et al. (2013) and L. M. T. Luong et al. (2017, 2020) have shown the impact of air pollution on the number of hospitalisations for respiratory and cardiovascular diseases in HCMC. However, these studies only investigated the effects of PM10, ground-level O3 and common air pollutants (SO2 and NO2), without much attention paid to PM2.5, which is considered a risk factor that affects human health and leads to premature death (Cohen et al., 2017; Fu et al., 2020; Huy et al., 2018). One study, by L. T. M. Luong et al. (2020), reported a 3.51% increase in the risk of hospitalisation for acute lower respiratory tract infection in children with every 10 µg/m3 increase in PM2.5. The studies that have reported on health risks due to PM2.5 were conducted mainly in Hanoi City (Chi et al., 2020; L. M. T. Luong et al., 2017; Nhung et al., 2013, 2018, 2019). Typically, an increase in the risk of hospital admission for respiratory disease and pneumonia by about 2.3% and 6.3%, respectively, was associated with an increase in PM2.5 exposure to 10 µg/m3 in children under five years of age as reported by L. M. T. Luong et al. (2017) and Nhung et al. (2013).
Illnesses due to PM2.5, the levels of which show wide regional variations, can have global impacts owing to its transboundary transport (Tang et al., 2018). The limitations of ground monitoring stations and their location-specific dispersion have created significant challenges for large-scale, high-resolution air quality monitoring in Vietnam (Do et al., 2021). Therefore, air quality models are considered a simpler approach to solving the problem of large-scale air pollution to provide air quality management and regional pollution conversion, long-range transport and community risk assessment studies (Chen et al., 2017; Do et al., 2021). Studies by Ho et al. (2020) and Vu et al. (2020) have presented the negative impacts of PM2.5 pollution on public health in HCMC via modelling, showing that up to 81.45% of total deaths were caused by PM2.5, SO2 and NO2 (1397 cases), with roughly 1136, 89 and 172 deaths, respectively, in 2017. Over the past decade, air quality models have been widely used to understand the physical and chemical processes involved in PM2.5 pollution (Tao et al., 2020). These models can perform air quality simulations from local to global scales with different resolutions depending on the research purpose (Tao et al., 2020). In particular, the CMAQ model system has been developed to study environmental issues and has been applied to multiscale (urban and regional) air pollution problems as well as multi-pollutant contamination (oxidants, acid deposits, and particulate matter) (Jun and Stein, 2004; Toledo et al., 2018).
From the modelling perspective, most studies investigating the extent of illnesses caused by air pollution in Vietnam are based primarily on the response‒exposure approach, based on the theory of the BenMAP-CE model. Table 1 summarises the above research for different localities in Vietnam. This approach typically considers pollutant concentration, concentration‒response functions (CRFs), exposed population and baseline mortality/morbidity instances as the main factors that determine the number of affected cases. The role of pollutant concentration in these models is decisive, followed by population (Guan et al., 2021). Some studies, such as Maji et al. (2019) and Wang et al. (2020a, b), used population-weighted PM2.5 concentrations to estimate health risks. As detailed in Table 1, this is a significant limitation of previous studies. Furthermore, previously published data have become obsolete because of rapid industrialisation, and urbanisation must be considered to a greater extent.
Data and methods
Study area
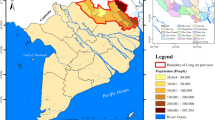
HCMC is the nucleus of the southern key economic regions, one of the three largest key economic regions in Vietnam. Although it accounts for only 0.6% of the country’s area and 9% of the population, HCMC contributes 22% of the country’s GDP. The total GDP value of the whole country in 2018 reached approximately 236.1 billion USD (Ho Chi Minh City Statistical Office, 2019), while that of HCMC itself has reached 52.2 billion USD. The area of the whole city is 2095.4 km2, divided into 19 urban districts and 5 rural districts. The GRDP Contribution of HCMC in 2010 was 21.8 billion USD, accounting for approximately 24%, which is roughly 1/4 of the national contribution (Ho Chi Minh City Statistical Office, 2019) (Fig. 1).
PM2.5 pollution in HCMC has a large variation between hours of the day but little seasonal variation (GreenID, 2017), and the highest dust concentration occurs immediately after the morning rush hour (Huy et al., 2018). The average PM2.5 dust concentration from 2013 to 2017 was 28.0 ± 18.1 µg/m3, and the average concentration over the years almost exceeded NAAQS (25 µg/m3, annual mean) as well as WHO Standard 2006 (10 µg/m3, annual mean) (Huy et al., 2018). Most of the time, PM2.5 concentration peaks were related to air masses moving along the coast, accumulating pollution from transport, power plants and public facilities (GreenID, 2017; Hien et al., 2019; MONRE, 2018). Moreover, the concentration of PM2.5 also fluctuated between monitoring locations, and the relative PM2.5 concentration values increased in the following order: city zoo (background monitoring) < rural area < residential area < roadside < city road; at the same time, the concentration of PM2.5 in the roadside and city road areas has a corresponding clear linear relationship with traffic activities (Hien et al., 2019; Phan et al., 2020), which showed that the mobile form of traffic emission sources contributed the largest amount of emissions for all air pollutants in HCMC: 99%, 97%, 93%, 78%, 76%, 64% and 45% of the total emissions of CO, NMVOCs, NOx, SO2, TSP, CH4 and PM2.5, respectively. Meanwhile, the proportion of BC/PM2.5 composition in HCMC ranged from 6.5 to 43%; the highest percentage was found in city road areas, and the lowest was mainly in city zoos and rural areas (Phan et al., 2020). The variability in BC composition is directly related to changes in meteorological conditions and has a significant impact on regional air quality (Hien et al., 2019; Phan et al., 2020). In addition, other important heavy metal components present in PM2.5 dust (Cr, As, Cd, Cu, Fe, Mn, Mo, Ni, Pb and Zn) account for 131.77 ± 42.13 to 233.13 ± 79.88 µg/m3 (Phan et al., 2020).
Data and models
To determine the excess number of early deaths and disease treatment due to ambient PM2.5 and quantify the economic losses, six types of input data needed to be captured: (i) datasets in terms of the grid-based exposed population size, (ii) estimations of modelled 24-h mean ambient PM2.5 concentrations to consider and assess the effects of short-term exposure, (iii) health endpoint types associated with premature mortality and morbidity, (iv) baseline incidence of premature mortality and morbidity rates, (v) estimates of concentration–response functions (CRFs) corresponding to the selected human health impact categories, and (vi) estimates of the unit economic value of the respective considered health endpoint types. Based on this, the following sections explain in detail the information and data sources, as well as the crucial models.
Exposed population size
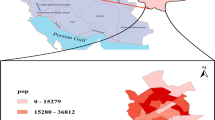
The spatial distribution of the grid-based exposed population was performed from the datasets recording HCMC population in 2018. Population density exposed to PM2.5 was allocated on each grid cell belonging to the domain D03 with a resolution size of ~ 3.14 × 3.14 km2. Specific population exposure datasets, including age- and gender-specific populations, were collected from the Statistical Yearbook reports (GSO, 2020; HCMC Statistical Office, 2019b, 2020) These datasets were divided into three main age groups by sex (male and female): children (0–14 years old), adults (15–64 years old) and elderly (≥ 65 years old). Details of the population data of the HCMC hierarchy, in accordance with, administrative unit, age groups and gender are shown in Figs. 1 and 2.
The process of estimating spatial exposed population distribution was conducted according to these following steps (L. Chen et al., 2017; Bayat et al., 2019): (1) determine the general exposed population density in 2018 (DenDist,i,2018) for each district i of HCMC by taking the total population (POPDist,i,2018) divided by the total area (SDist,i) of district i as in Eq. (1); (2) to calculate the average population density for each grid cell j, it is necessary to estimate the area ratio (RatioDist,i,j) of the area of district i (SDist,i,j) at the grid cell j compared to the total area of the whole district i (SDist,i) according to Eqs. (1,2); (3) the estimated population density outcomes at each grid cell j (Deni,j,2018) based on POPDist,i,2018 and calculated RatioDist,i,j that n is the number of districts included in the estimated grid cell j as in Eq. (3).
where Deni,,j,2018 is the HCMC population density at each estimated grid cell j; POPDist,i,2018 is the total population in 2018 as per district i in the study area; SDist,i is the total area of district i; and SDist,i,j is the total area of district i in grid cell j in the range of the computing domain D03 covering the entire HCMC.
Based on the calculated and analysed results (HCMC Statistical Office, 2019a, b; HCMC Statistical Office, 2020; Ministry of Health, 2019), the total population exposed to ambient PM2.5, pollution was 8,831,865 people, of which it was estimated that there were 4,301,118 men (accounting for approximately 48.70%) and 4,530,747 women (approximately 51.30%); see Fig. 2, as well as the HCMC’s exposed population by district shown in Fig. 3. According to the age group structure, there were 2,275,088 people 0 to 14 years old (25.76%); 5,982,705 15 to 64 years old (67.74%) and in the age group of over 65 years old, 574,071 (6.5%) (Figs. 2 and 3).
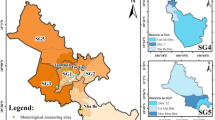
Simulated 24-h mean PM2.5 concentration distribution
The hourly simulated PM2.5 concentration datasets were obtained from the coupled WRF/CMAQ, in which the three-level nested computational domains of D01, D02 and D03 were set up to meet the requirements of the coupled WRF/CMAQ. The domain D01 had a spatial resolution of approximately 30.43 km × 30.43 km, which was the highest. The area of the D01 domain was approximately 5.41 × 106 km2. The domain D02 had a spatial resolution of roughly 9.55 km × 9.55 km; this was the second nested domain within D01. The D02 domain area was approximately 2.11 × 105 km2. The D03 domain had a spatial resolution of approximately 3.14 km × 3.14 km; it was the smallest calculation domain nested within D01 and D02, with an area of approximately 2.64 × 104 km2.
On an hourly PM2.5 concentration data basis for domain D03, the daily average PM2.5 concentration level (or C in Eq. (4)) at each estimated grid cell location was identified (Fig. S1–Fig. S12). It was the input data source for estimates in human health impact modelling for different health endpoint types attributed to short-term PM2.5 exposure and corresponded to the choice of the estimated threshold value. To ensure the reliability of the simulated dataset, validation comparisons were also performed on the basis of the measurement results of ambient PM2.5 concentration at the monitoring sites. However, the threshold PM2.5 concentration (or C0) in (4) was applied to the human health impact models. This is the 24-h average PM2.5 threshold value according to the guidelines of the National Ambient Air Quality Standard (NAAQS); specifically, QCVN 05:2013/BTNMT with a threshold value of 50 μg/m3 was used as the reference for the human health effect calculations.
Identification and classification of short-term health endpoints due to PM2.5 pollution
Most non-accidental premature deaths (> 99.0%) are caused by non-communicable diseases (NCDs) and lower respiratory infections (LRIs) (Bayat et al., 2019; Liu et al., 2021; Burnett et al., 2018). Thus, this study limited the estimation and assessment of non-accidental premature deaths and diseases and focused on two subgroups: NCDs and LRIs. The study was also limited to health endpoints with concentration–response coefficients clearly classified according to the 10th version of the International Classification of Diseases (ICD-10, 2016). In particular, there are six main categories of diseases related to ambient PM2.5, including circulatory system, respiratory, endocrine, nutritional and metabolic diseases, neoplasms, mental and behavioural disorders and nervous system diseases (ICD-10, 2016).
In this study, three different health endpoint groups were estimated; specifically, for the health impact group (1) of premature mortality, all-cause diseases were assessed, including mortality due to all-cause respiratory diseases (RDs), cardiovascular diseases (CVDs), and other circulatory system diseases (CSDs) (Yin et al., 2017b). With the health effect group (2) of hospital admissions includes hospitalisations attributed to the RDs such as acute LRI due to pneumonia and acute bronchiolitis in children, chronic obstructive pulmonary disease (COPD), community-acquired pneumonia (CAP); and related to the CVDs such as heart failure (HF), myocardial infarction (MI)), and stroke. Moreover, the health endpoint group (3) of emergency visits consisted of emergency cases caused by RDs, such as COPD and CAP, and CVDs, such as HF, HF MI and stroke (Table 2).
Baseline incidences of premature mortality and morbidity
The early death and morbidity baseline data are statistics that estimate the average number of people with disease or death in a given population over a given period of time (Bayat et al., 2019; Liu et al., 2021). In this study, the statistical data were applied from the 2018 Health Statistical Yearbooks published by the Vietnamese Ministry of Health (Ministry of Health, 2019), based on the number of cases of each health endpoint and population data, and combined with references from the open-source website of the Institute for Health Metrics and Evaluation (IHME) on the website of GDP 2019 (Global Burden of Disease Collaborative Network, 2019), which is a dataset that provides annual, age-specific, sex-specific estimates for each of the five age groups with categorical detail and also incorporates available studies (L. M. T. Luong et al., 2017; L. T. M. Luong et al., 2020; Bui et al., 2021) to determine the baseline incidence of premature deaths and morbidities in HCMC (Table 3).
Concentration—response function coefficients
The coefficients of CRFs or beta (β) coefficients were determined based on the parameters from the original epidemiological studies for each type of health endpoint (Table 3). In epidemiological studies, a Cox proportional hazards model or a log-linear model was used to calculate relative risk (RR) values, from which the beta coefficient values were calculated according to Eqs. (5), (6) and (7) (L. Chen et al., 2017; Sacks et al., 2018; Luo et al., 2020) as follows:
where RR values for related health endpoints including early deaths and morbidities can be found in the available epidemiological studies of health endpoint i due to short-term ambient PM2.5 exposure; ΔCPM2.5 is the change in ambient PM2.5 concentration, commonly ΔCPM2.5 = 10 μg/m3 (Willian Lemker Andreão et al., 2020) or 1 μg/m3 (Zhao et al., 2019);\({\sigma_\beta }\) (the standard error of \(\beta\)) is calculated as the average of the standard errors implied by the reported lower (RRmin) and upper bounds (RRmax) of the RR in the corresponding epidemiologic studies.
For the health endpoint group (1) of premature mortality due to RDs, CVDs and other CSDs, beta coefficients were determined for all age and sex groups. This was similar for some cases in the health impact group (2) of hospital admission attributed to COPD, CAP, HF, MI, stroke and for all cases in the health effect group (3) of emergency visits. In particular, for the remaining cases in the health endpoint group (2), such as hospitalisation for acute LRIs due to pneumonia and acute bronchiolitis, the beta coefficients were only determined for the group of children (from 0 to 14 years) in both men and women.
Economic valuation of PM2.5 human health impacts
The value of a statistical life (VSL) is applied to assess the willingness of individuals to pay to reduce premature mortality risks (Yin et al., 2017b). To calculate the economic losses for the health endpoint of early death, a specific VSL was applied. However, there are currently no national studies assessing VSL loss; therefore, (9) was used to transfer unit health costs from international studies to the local context in HCMC, a “Transfer Benefits” approach as suggested by Narain and Sall (2016), Kim et al. (2019) and Johnson et al. (2015), with the main idea of the adjustment taking into account differences in income levels to expand the VSL (Yin et al., 2017b). Therefore, to determine the VSL for Vietnam, this study used VSL data from the Organisation for Cooperation and Development (OECD) (VSLOECD) as the starting value for calculation. Vietnam’s VSL value for the target year 2018 was estimated based on the base VSL starting in 2011 applied from Eq. (8) (Long et al., 2020; Bui et al., 2021s; Hammitt and Robinson, 2011).
where \(VS{L_{Vietnam - 2011,USD}}\) is the VSL of Vietnam in 2011 calculated in USD (USD in 2011); \(VS{L_{OECD - 2011,USD}}\) is the background average VSL estimated from the WTP’s available research for OECD countries in 2011 calculated in USD (USD in 2011); \({Y_{Vietnam - 2011}}\) is the real GDP per capita at the purchasing power parity (PPP) of Vietnam in 2011 (USD in 2011); \({Y_{OECD - 2011}}\) is the baseline real GDP per capita at the PPP of OECD countries in 2011 (USD in 2011); and e is the income elasticity of the VSL. In this study, coefficient e is equal to 1.3 (according to the OECD study) to reflect the significant difference between Vietnam and the developed countries of the OECD group in terms of income level (OECD, 2012; Long et al., 2020; Bui et al., 2021). The Eq. (9) below (Long et al., 2020Bui et al., 2021; Kim et al., 2019) describes the VSL adjustment for the target year 2018 based on the baseline VSL of 2011 (VSLVietnam-2011, USD). PPP2011-2018, the PPP-adjusted exchange rate for each year of the 2011–2018 period, was applied to convert the US dollar (USD) to Vietnam dong (VND).
where \(VS{L_{Vietnam,2018(VND)}}\) is Vietnam’s VSL adjusted for the year 2018 calculated in VND;\(\Delta {P_{2011 - 2018}}\) is the percentage (%) that increased in consumer price from 2011 to 2018; \(\Delta {Y_{2011 - 2018}}\) is the percentage (%) that rose in the real GDP per capita growth between 2011 and 2018; and PPP2011-2018 is the PPP-adjusted exchange rate of the year 2011 by the World Bank data (2018) and the year 2018 from the World Bank data (2020). Thus, based on the above estimation framework, it was determined that the value of VSLVietnam,2018 was 4788.95 million VND (equivalent to approximately 0.642 million USD on the basis of the exchange rate adjusted for purchasing power parity in 2018 or PPP2018).
For the economic valuation of losses related to disease treatment, the cost of illness (COI) approach has been applied, including the assessment of the costs of medical treatment, hospitalisation and emergency visit costs and productivity losses (Hoffmann et al., 2012; D. Huang et al., 2012; Quah & Boon, 2003; Kalkan et al., 2014). In this study, the total costs of the COI approach associated with the health endpoint groups (2) and (3) were determined using the average values from previous studies by Chinh Nguyen (2013), Long et al. (2020) and Bui et al. (2021). Finally, based on assessments of the public health impacts of PM2.5, combined with the unit economic values for each type of health impact, the total risk of economic losses when quantified into money was estimated using Eq. (10) (Long et al., 2020;Bui et al., 2021; Ding et al., 2016; Yin et al., 2017) as follows:
where ∆Yi is the impact degree of the type of health effects i, \(Cos{t_i}\) is the value of the economic unit of the type of health endpoint i (Vietnam Dong, VND or US Dollar, USD) and EC is the total economic loss from the results of the health impact types (Vietnam Dong, VND or US dollar, USD). The result of the estimated EC value is relative to the total economic impact of public health effects due to exposure to PM2.5, pollution in the ambient air in HCMC.
Conceptual model and procedural steps
This study was carried out in three steps, as shown in Fig. 4. First, to build the PM2.5 concentration data set, WRF/CMAQ models were used. The WRF model generates hourly meteorological datasets, while the CMAQ model generates the hourly PM2.5 levels. As a next step, a dataset of mean PM2.5 concentrations was used, combined with a dataset of population exposure estimates, short-term health classification, background rates of early mortality and morbidity and a set of concentration–response function coefficients for public health impact analysis. This is the end of step 2. Finally, the results of step two, combined with the VSL method, were used to assess economic losses.
Results
Health impact analysis
Short-term (acute) health damage based on average daily PM2.5 concentrations exceeding the NAAQS threshold (24-h mean; 50 µ/m3) was estimated. The results show that the total number of losses due to premature death is estimated at 174 (95% CI: 16; 340) cases; due to hospitalisation for inpatient treatment was 117,632 (95% CI: 231,850; 368,926) cases; and due to emergency examination was 162,455 (95% CI: − 710.465; 531,153) cases. Table 3 summarises the level of health damage by month; each group of objects and each group of different types of health damage, especially for the damage group (1) all daily premature deaths (by respiratory and cardiovascular diseases (all causes) are illustrated in Fig. 5 A, B, C and D.
In the first quarter, there were 61 (95% CI: 5; 127) deaths from all causes. The details of the impact level in damage group (1) for each type of damage are as follows: 56,805 (95% CI: 6,077; 117,085), 3851 (95% CI: − 1,133; 8,747) and 0.614 (95% CI: 0.056; 1.168) cases were due to respiratory, cardiovascular and other circulatory diseases of all causes, respectively. The level of damage was the highest in the first quarter, with the number of cases due to 27 cases of early death (95% CI: 5; 53). The second quarter was considered to have the highest total number of premature deaths; specifically, the loss due to premature death was 78 (95% CI: 7; 164) cases, which was 1.28 times higher than that of the first quarter. A detailed assessment of the impact level in the damage group (1) for each type of damage in the second quarter showed that respiratory diseases still prevailed. The number of deaths due to respiratory diseases, cardiovascular and other circulatory systems by all causes reached 72.66 (95% CI: 8282; 152,116) cases, 4602 (95% CI: − 1.349; 10,475) cases and 0.737 (95% CI: 0.067; 1.409) cases, respectively. In the third and fourth quarters, the total number of premature deaths due to PM2.5 decreased significantly compared to the first and second quarters, with a sharp decrease in the third quarter and a slight increase again in the fourth quarter. In the third quarter, the loss due to premature death was 5 (95% CI: 0; 7) cases, which was 15.60 times lower than that in the second quarter and 21 (95% CI: 4; 42) cases in the fourth quarter. Detailed assessment of the impact level by type of disease in the third quarter showed there were 4,678 (95% CI: 0.077; 6284) deaths due to respiratory diseases, 0.277 (95% CI: − 0.081; 0.631) deaths from cardiovascular diseases and 0.045 (95% CI: 0.004; 0.085) deaths from other circulatory diseases; the fourth quarter had 16,254 (95% CI: 4.424; 29,142) deaths from respiratory diseases, 1508 (95% CI: − 0.446; 3,409) deaths from cardiovascular diseases, and 0.238 ( 95% CI: 0.022; 0.449) deaths from other circulatory diseases (Table 4).
In the damage group (2) in the first quarter, the number of inpatient hospitalisations accounted for a significant proportion of the total number of cases of short-term health damage (only after the number of emergency visits), at approximately 54.313 (95% CI: − 94,523; 137,672). Detailed assessment for each type of damage (disease) in the second quarter showed that there were 26,895 (95% CI: 903.9; 77,674.7) cases due to respiratory diseases with mainly 21,847.9 (95% CI: 6371.4; 34,522.2) cases due to COPD and 18,427.4 (95% CI: 9536.1; 26,020.9) cases due to acute bronchiolitis (ALRI) and 18,185.5 (95% CI: − 116.332.3; 82,650.2) cases due to cardiovascular diseases mainly due to stroke with 14,628.9 (95% CI: − 5152; 29,294.5) and 1369.4 (95% CI: -54,979.5; 26,612) cases due to MI. The trend of inpatient hospitalisation changed significantly in the second, third and fourth quarters. The number of hospital admissions for inpatient treatment in the second quarter was 67,839 (95% CI: − 81,892; 174,184), 1.25 times higher than that in the first quarter; approximately 4390 (95% CI: − 4,152; 11.846) cases in the third quarter were 15.45 times lower than that in the second quarter, and approximately 18,904 (95% CI: − 51,283; 45,224) cases in the fourth quarter. A detailed assessment of the impact level for each type of damage in the second quarter resulted in 54,233.2 cases due to respiratory diseases (95% CI: 2,735.2; 97,023.7) with the majority being 27,219.9 (95% CI): 7731; 43,263.5) cases due to COPD and 23,079.6 (95% CI: 11,784.2; 32,530.6) cases due to acute bronchiolitis (ALRI). The number of cases due to cardiovascular diseases was 22,444.1 (95% CI: − 103,234.4; 105,028) mainly caused by stroke and MI with 18,167 (95% CI: − 6016.8; 36,690.7) and 2730.6 (CI: − 6,016.8; 36,690.7) cases, respectively. 95% CI: − 48,383.4; 34.830 cases. For the third and fourth quarters, the number of inpatient hospitalisations due to respiratory and cardiovascular diseases was 3532.8 (95% CI: 258.1; 6547); 1494.8 (95% CI: − 5379.5; 7190.9) cases in the third quarter and 14,904.3 (95% CI: − 721.2; 25,514) cases, 9159.2 (95% CI: − 222,683.6; 44,163) cases in the fourth quarter (Table 4).
In the damage group (3), there were 66,904 (95% CI: − 320,083; 200,745) cases, of which there were approximately 55,786.8 (95% CI: − 6692.1; 103,565.1) due to respiratory diseases of all causes. However, when evaluating the details based on the CRFs classified for each specific disease in the respiratory group (typically COPD), the number of cases tended to be higher, with 59,193.9 (95% CI: 18,158.8; 90,512.5) cases and only approximately 25,564.4 (95% CI: − 377.522.1; 139,895.8) cases due to cardiovascular diseases (mainly stroke) (21,187.4 (95% CI: − 16,537.7; 47,245.9), MI disease with 3404.1 (95% CI: − 304,261; 60,823.5), HF with 973.1 (95% CI: -56,724.5; 31,826.4) cases (Table 4).
In the second quarter, the number of emergency visits reached 83,782 (95% CI: − 191,695; 249.545), which was 1.26 times higher than in the first quarter; while in the third and fourth quarters, respectively, 5659 (95% CI: − 9209; 17,855) cases were 14.81 times lower than in the second quarter, and 21,992 (95% CI: − 189,478; 63,008) cases occurred in the quarter. In the second quarter, there were approximately 70,085 (95% CI: − 6,075.8; 127.173.7) cases of respiratory diseases with 74,103.1 (95% CI: 22,307.5; 111,077) cases due to COPD and 31,549.1 (95% CI: − 223,647; 174,688.6) due to cardiovascular diseases, mainly stroke. MI and HF with 26,289.4 (95% CI: − 13,855.2; 59,644.2) cases, 4095.9 (95% CI: − 150.004.4; 75,193.4) cases and 1163.7 (95% CI: − 54.855.9; 39,851) cases, respectively. In the third quarter, the number of cases occurred as follows: respiratory diseases had 4798.8 (95% CI: − 189.8; 9,344.3) cases, mainly due to COPD with 5033 (95% CI: 1391.5; 8332.9) cases, total cardiovascular disease with 2016.9 (95% CI: − 10,901.7; 12,258.4) cases, with the majority due to stroke. MI and HF caused 1675.7 (95% CI: − 1083; 4101.4) cases, 268.6 (95% CI: − 6888.5; 5513.8) cases and 72.5 (95% CI: − 2930.2; 2643.3) cases, respectively. In the fourth quarter, the total number of emergency visits due to respiratory diseases was 17,512 (95% CI: − 5537.8; 29,055.7), mainly due to COPD 18,881.7 (95% CI: 6633.1; 27,347.8). The total number of cases due to cardiovascular diseases was 9159.2 (95% CI: − 222,683.6; 44,163), with the majority of cases due to strokes. MI and HF caused 7465.4 (95% CI: − 7067.8; 14,994.2) cases, 1313.4 (95% CI: − 169,125.1; 18,569.4) cases and 380.4 (95% CI: − 28,516.4; 10,599.4) cases, respectively. Thus, the total number of cases of premature death and disease treatment (including hospitalisation and emergency) in the second quarter of 2018 was the highest, with approximately 151,699 (95% CI: − 273,580; 423.923) cases, followed by the first and fourth quarters with 121,278 (95% CI: − 414.601; 338.544) cases and 40,917 (95% CI: − 240,757; 108,274) cases, respectively, and the lowest was in the third quarter of 2018 with only approximately 10,054 (95% CI: − 13,361; 29,708) cases (Table 4).
Assessment of economic valuation loss
The economic (monetary) value lost is quantified here. The quantification is based on Vietnam’s estimated 2018 VSL value of 4788.95 million VND, or approximately 642 million USD (converted to US$ 2018) and COI cost assumptions (Chinh Nguyen, 2013; Bui et al., 2020, 2021). In the first quarter, the loss of economic value from short-term impacts due to the risk of premature death was estimated at 204.89 billion VND (approximately 27.71 million USD), with an increasing trend from 1 January to March. The highest loss occurred in March at approximately 78.86 billion VND (equivalent to approximately 10.66 million USD). The loss of economic value due to the costs of hospitalisation for inpatient treatment and emergency visits reached approximately VND 785.48 billion (equivalent to approximately USD 106.27 million) and VND 43.33 billion (equivalent to approximately 5.85 million VND). Economic losses also occurred due to loss of income and reduced labour productivity in the adult population (from 15 to 64 years old), with the loss reaching approximately 100.60 billion VND (equivalent to approximately 13.61 million USD) and 4.72 billion VND (equivalent to approximately 631.21 thousand USD). Thus, the total economic value of the damage to public health caused by PM2.5 in the first quarter was VND 1139.02 billion (equivalent to approximately USD 154.07 million), among which costs and losses due to hospitalisation for treatment inpatients and due to the number of premature deaths accounted for the highest proportion, accounting for approximately 68.96% and 17.99%, respectively (Fig. 6A).
For the second quarter (Fig. 6B), the economic value of losses due to premature deaths increased compared to the first quarter, whereas those in the third quarter decreased significantly compared to the first and second quarters. The second quarter reached approximately 331.35 billion VND (equivalent to approximately 44.81 million USD), 1.62 times higher than the first quarter and for the third quarter reached 20.86 billion VND (equivalent to 2.83 million USD), 9.82 times lower than the first quarter. The total economic losses due to the costs of hospitalisation for inpatient treatment and emergency visits in the second quarter were VND 875.94 billion (equivalent to approximately USD 118.45 million) and VND 51.18 billion (equivalent to approximately 6.92 million USD, respectively); for the third quarter, these values are VND 59.24 billion (approximately USD 8.02 million) and VND 3.61 billion (approximately USD 487.96 thousand) respectively (Fig. 6C). Total losses due to loss of income as well as decrease in labour productivity in both the second and third quarters reached approximately 132.11 billion VND (equivalent to approximately 17.86 million USD) and 8.90 billion VND (equivalent to 1.21 million USD), respectively. Thus, the costs of loss due to inpatient hospitalisation and premature death accounted for the highest proportion, reaching 63.05% and 23.75% of the total lost economic costs in the second quarter and the second quarter, respectively. III is 1483.19 billion VND (equivalent to approximately 199.38 million USD).
For the fourth quarter, the economic value of loss due to premature deaths increased slightly compared to the third quarter, reaching approximately 110.25 billion VND (equivalent to 14.91 million USD), which was 5.27 times higher than that of the third quarter. Meanwhile, for the total economic loss due to the costs of hospitalisation for inpatient treatment and emergency visits in the fourth quarter, respectively, VND 252.94 billion (equivalent to approximately USD 34.21 million) was 4.94 times higher, respectively, compared to the third quarter and 14.02 billion dong (equivalent to approximately 1.89 million USD) 3.88 times higher than that of the third quarter. Similarly, the total loss due to loss of income as well as the decrease in labour productivity in the fourth quarter was approximately 4.29 times higher than in the third quarter, with the loss reaching approximately 38.40 billion VND (equivalent to approximately 5.19 million USD) (Fig. 6D).
Thus, the total value of economic losses due to PM2.5 daily in HCMC exceeded the meeting threshold of NAAQS (QCVN 05:2013/BTNMT) in 2018 by approximately 3038.31 billion VND (equivalent to 410.79 million USD). If compared with the value of GRDP of HCMC in 2018 (1225.6 trillion VND (HCMC Statistical Office, 2019a), the total economic loss value accounts for approximately 0.248% of the total GRDP.
Uncertainty analysis
In this study, it is inevitable that some uncertainty points must be discussed. Among the types of health damage, premature deaths are considered the most significant, accounting for over 90% of the exposure to air pollution (mainly PM10 and PM2.5 dust), which has been demonstrated in several studies (Ho, 2017; Vu et al. 2020; Bui et al., 2021). Identifying categories of acute health damage to premature mortality from PM2.5, and applying CRFs relationships suggests that the selection of time-series epidemiological studies has some limitations in comparing the use of cohort epidemiological studies based on quantitative studies. In this study, CRFs functions were based on cohort studies for analysis and evaluation. The relationship between PM2.5 pollution levels and early mortality in HCMC is based on epidemiological cohorts that have not been performed. Therefore, the β coefficients for the estimate of the damage group (1) early death were obtained from China and Brazil. This leads to an error that is usually higher. This is exactly the same for the estimates of the effects of the damage group (2) inpatient hospitalisation (except for the type of hospitalisation loss due to acute lower respiratory tract infection by pneumonia and acute bronchiolitis in children aged 0–14 years) and damage group (3) emergency visits.
Second, the general application of CRFs to districts in HCMC for calculation is also an uncertainty factor in this study. The impact of PM2.5 pollution is not only caused by the total concentration level but is also significantly influenced by the aerosol chemical constituents of PM2.5 (such as PSO42−, PNO3− and PNH4+), the size distribution of PM2.5 aerosols varies and the emission sources contribute from different geographical areas. This issue was discussed by Bart et al. (2015) and Wang et al. (2020a, b). It proved to be one of the factors that created errors in the calculation results. Therefore, further studies and future epidemiological studies need to focus on developing and updating CRFs functions for each district of HCMC; HCMC has classified each specific exposure group.
Selecting only PM2.5 as an indicator of air pollution, ignoring NOx, SO2 and other harmful compounds will lead to certain errors. In addition, SO2 and NOx lead to the formation of secondary PM2.5, which further increases the damage caused by particulate pollution. The current research results only consider the public health effects of PM2.5 pollution outside and have not mentioned the negative effects caused by exposure to PM2.5 indoors. The process of burning fuel in households, cooking for people’s living, operation of decorative materials and household and personal care products can all emit gaseous and particulate pollutants. Thus, the assessment of types of health damage related to PM2.5, when considering only outdoor exposure, does not fully and comprehensively reflect the impacts on human health. From there, developing CRFs that consider future indoor PM2.5 exposure in HCMC is an important basis for subsequent analysis and evaluation.
Third, research focuses on some types of damage, while many other types of health damage such as subclinical symptoms, reduced lung function and human health effects from exposure to infection causing lung cancer have not been included in the calculation and detailed analysis in this study because of the limitation of the accessible CRFs; however, in previous cohort epidemiological studies, possible associations have been demonstrated by Pope III et al. (2002).
Fourth, simulation of the combined coupled WRF/CMAQ models in the study was performed at a resolution of ~ 3.14 × 3.14 km2 over the entire HCMC area has a low resolution. One of the results of a case study by Wang et al. (2020a, b) demonstrated that estimating the number of premature deaths/illnesses is relatively sensitive to the resolution of the simulation system because of the persistence of time levels of PM2.5 is relatively long, and it has the potential to be transferred on a regional scale. In addition, the top-down emission inventory dataset used in this study has errors in the level of detail when simulating heavily polluted and densely populated areas when there is no certainty in approximating the emission load of the precursors. Therefore, in future studies, higher-resolution models incorporating small-scale precursor emission load datasets should be encouraged as they may be more useful for estimations of health impact due to their smoothed resolution. Uncertainty may arise regarding the PM2.5 concentration values. In this study, PM2.5 measurement data was performed manually and intermittently for one month only at 7:30 am and 15:00 pm in the period from 8 to 12 measurement days from January to June 2018 at 8 locations, and at 9:00, 11:00, 13:00 and 15:00 in the period from 8 to 12 measuring days from July to December 2018. Therefore, uncertainty may arise from the simulation results of the WRF/CMAQ model because of the lack of data for detailed verification.
Fifth, the current level of change in PM2.5 concentrations is a sensitive parameter for both health impacts and loss cost estimates. Some case studies include Smith and Jantunen (2002) and R. T. Burnett et al. (2014) recommends using the threshold value recommended by the World Health Organisation WHO (with 25 µg/m3, 24-h average) (WHO, 2006); in this study, the cut-off value of NAAQS (with 50 g/m3, 24-h average) was used, leading to lower health impact estimates than when WHO standards are applied.
Finally, a further uncertainty that needs to be discussed is the approach to assessing the economic benefits of premature deaths caused by PM2.5 pollution. The present study used the VSL value as the basis for calculating economic value losses for premature deaths; however, a certain limitation to the use of VSL values is the lack of adequate consideration of the age structure between the population susceptible to exposure to air pollution and the normal population size. This has caused the evaluation results with VSL values to tend to be higher than when using the same approach from the Years of Life Lost (YOLL) or the YOLL value. The WTP was surveyed in detail using different classifications in the study area.
Discussion
This is the first study in Vietnam, specifically HCMC, to comprehensively evaluate the impact of PM2.5 pollution on public health in the form illnesses, such as premature death and hospitalisation, inpatient treatment and outpatient visits, and successfully quantify economic losses by applying combined simulation methods from the WRF/CMAQ and BenMAP-CE.
Our results show that the average PM2.5 concentration in 2018 was estimated to range from 55.8 to 65.3 µg/m3, which exceeded the threshold of NAAQS (25 µg/m3) by 2.23‒2.61 times. Previous studies have also suggested similar PM2.5 pollution. Specifically, the report of the HCMC Department of Natural Resources and Environment states that the average PM2.5 concentration in 2016 was 42.0 µg/m3 (1.68 times higher than NAAQS) (Nguyen et al., 2018), and by 2017, the annual average PM2.5 had decreased to 29.6 µg/m3 (1.18 times higher than NAAQS) (Thu et al., 2018), and only 23.0 µg/m3 (lower than NAAQS threshold) (Vu et al., 2020). Previous evidence combined with our research results demonstrates that PM2.5 pollution in HCMC tends to increase dramatically. Specifically, the average concentration in 2018 was increased by 1.33–1.55 times compared to that in 2016 and 1.89–2.21 times compared to that in 2017. The total number of premature deaths due to respiratory and cardiovascular diseases (all causes), when estimated according to the WHO Standard (WHO, 2006) in 2018, may reach 5,440 cases > 1136 cases in 2017, according to the results of Vu et al. (2020).
Furthermore, with the trend of days in 2018, the 24-h average concentration level in the dry season (January–April and December) is typically higher than that in the rainy season (May–November), similar to the trend in 2017 (Thu et al., 2018). Because the 24-h average PM2.5 concentration is a major determinant of the number of cases of short-term health problems, this leads to a much higher damage estimate in the dry season than in the wet season of 2018. Specifically, the total number of deaths was 105 (95% CI: 8; 188) in the dry season and > 69 (95% CI: 10; 117) in the rainy season. Moreover, the total number of hospitalisations for inpatient treatment was 68,349 (95% CI: − 126.269; 186.623) in the dry season and > 49,283 (95% CI: − 54,623; 126,804) in the rainy season, and the total number of emergency visits was 95,956 (95% CI: − 491.756; 292,881) in the dry season and > 66.498 (95% CI: − 147,900; 198.892) in the rainy season. However, when we comprehensively estimated short-term health losses from PM2.5, including premature death, inpatient hospitalisation and outpatient visits, the total economic loss (approximately 3.050 trillion VND) is also much higher than the previous estimate of Dang et al. (2021) at 2.942 trillion VND (approximately 1.04 times higher) when assessing only the number of deaths from cardiovascular disease.
Moreover, our 2018 estimate of 174 (95% CI: 16–340) premature deaths is similar to the studies performed in China and Spain. In particular, Ding et al. (2016) reported that premature deaths occurred in 106 (95% CI: 44–162) cases in 2010 in Guangzhou, China, resulting in economic losses of approximately 150 million yuan (equivalent to 24 million USD). In Spain, there were approximately 30 premature deaths in 2007, which increased by 18% in 2014, as reported by Boldo et al. (2014), which is 4.92 times lower than that reported in our results. However, a wide range of similar studies in South Africa, India, Iran and Brazil showed several times higher values than those in this study. A study by Altieri and Keen (2019) showed that the number of premature mortality cases in 2012 was 14,000, calculated on the basis of South Africa’s NAAQS (20 µg/m3), 80.5 times higher than that in HCMC. The related damage valuation was estimated at roughly 14 billion USD (in 2011), which was also 33.9 times higher than in this study (Altieri and Keen, 2019). Manojkumar and Srimuruganandam (2021) reported that the PM2.5-attributed premature deaths in 2019 reached 2.10 million individuals in India, in which the lowest number of deaths occurred mainly in the north-eastern states with 0.79 million people (4.54 times higher than in our study). According to the studies of Bayat et al. (2019) and Willian L. Andreão et al. (2018), public health effects and economic losses due to PM2.5 exposure were significantly higher than those in this study. In particular, the total number of mortality cases in 2017 was 7146 (95% CI: 6,596; 7,513) in Tehran and its 349 surrounding districts (41.07 times higher), and the total economic losses were up to 2.894 trillion USD (7.02 times higher) (Bayat et al., 2019). In São Paulo, Brazil, the numbers of premature deaths in 2000 and 2017 were 28,874 and 82,720, respectively (Willian L. Andreão et al., 2018), which were 165.94 and 475.40 times higher than in HCMC, respectively.
The results of this study provide convincing, up-to-date scientific evidence on the impact of PM2.5 pollution on public health. This information can be the basis for supporting the development of appropriate intervention policies to reduce PM2.5 levels according to the National Action Plan to 2025 (Decision on Approving the National Action Plan on Air Quality Management to 2020, Vision to 2025, 2016) and protect human health.
Conclusion
The results of the study provide evidence that the concentration of PM2.5 in HCMC exceeds safe air quality standards of NAAQS and causes adverse health effects, contributing to increased mortality and morbidity as well as the significant economic burden. The specific results are as follows.
First, acute health impacts due to PM2.5 exposure mainly included premature mortality in 174 (95% CI: 16; 340) cases, hospitalisation for inpatient treatment in 117,632 (95% CI: 231,850; 368,926) cases and emergency visits in 162,455 (95% CI: − 710.465; 531,153) cases.
Second, the total economic damage caused by PM2.5 pollution in a year, quantified using 2018 as an example, was found to be approximately 3.03831 trillion VND (equivalent to approximately 410.79 million USD), accounting for 0.248% of the total gross regional domestic product (GRDP) value of HCMC, varying by month and quarter.
Third, a modelling framework that integrates models and databases was proposed to quantify the economic damage resulting from short-term PM2.5 pollution exposure. The model combines five groups of data on exposed population size, 24-h average PM2.5 concentration, health endpoint types related to early deaths and morbidity, baseline incidents and unit economic values of health impact types calculated using the WRF/CMAQ simulation, human health impact assessment and economic loss assessment models for reduced health effects.
These results are an important source of information for health communication programs to reduce the harm caused by PM2.5, and a reference source for policymakers to develop warning strategies and reduce environmental pollution to protect public health. Specifically, the solutions aim to control and minimise PM2.5 concentration in the main emission sources of HCMC, such as industry, energy, traffic and construction. Moreover, the applied research framework is considered a typical model that can be extended to many other localities in Vietnam to determine the status of PM2.5 as required by the National Action Plan.
Data availability
We declare that all data relating to this manuscript are truthful and we will gladly share it with any interested readers or at the request of the editor board.
References
Altieri KE, Keen SL (2019) Public health benefits of reducing exposure to ambient fine particulate matter in South Africa. Sci Total Environ 684:610–620. https://doi.org/10.1016/j.scitotenv.2019.05.355
Andreão WL, Albuquerque TTA, Kumar P (2018) Excess deaths associated with fine particulate matter in Brazilian cities. Atmos Environ 194(September):71–81. https://doi.org/10.1016/j.atmosenv.2018.09.034
Andreão, Willian Lemker, Pinto, J. A., Pedruzzi, R., Kumar, P., & Albuquerque, T. T. de A. (2020). Quantifying the impact of particle matter on mortality and hospitalizations in four Brazilian metropolitan areas. Journal of Environmental Management, 270(January). https://doi.org/10.1016/j.jenvman.2020.110840
Apte JS, Marshall JD, Cohen AJ, Brauer M (2015) Addressing global mortality from ambient PM2.5. Environmental Science and Technology 49(13):8057–8066. https://doi.org/10.1021/acs.est.5b01236
Arden Pope C, Burnett RT, Turner MC, Cohen A, Krewski D, Jerrett M, Gapstur SM, Thun MJ (2011) Lung cancer and cardiovascular disease mortality associated with ambient air pollution and cigarette smoke: Shape of the exposure-response relationships. Environ Health Perspect 119(11):1616–1621. https://doi.org/10.1289/ehp.1103639
Bart O, Jianlin H, Debbie G, Peggy R, Andrew H, Leslie B, J., K. M. (2015) Associations of mortality with long-term exposures to fine and ultrafine particles, species and sources: results from the California teachers study cohort. Environ Health Perspect 123(6):549–556. https://doi.org/10.1289/ehp.1408565
Bayat, R., Ashrafi, K., Shafiepour Motlagh, M., Hassanvand, M. S., Daroudi, R., Fink, G., & Künzli, N. (2019). Health impact and related cost of ambient air pollution in Tehran. Environmental Research, 176(June). https://doi.org/10.1016/j.envres.2019.108547
Boldo E, Linares C, Aragonés N, Lumbreras J, Borge R, de la Paz D, Pérez-Gómez B, Fernández-Navarro P, García-Pérez J, Pollán M, Ramis R, Moreno T, Karanasiou A, López-Abente G (2014) Air quality modeling and mortality impact of fine particles reduction policies in Spain. Environ Res 128:15–26. https://doi.org/10.1016/j.envres.2013.10.009
Brook RD, Franklin B, Cascio W, Hong Y, Howard G, Lipsett M, Luepker R, Mittleman M, Samet J, Smith SC, Tager I (2004) Air pollution and cardiovascular disease: a statement for healthcare professionals from the expert panel on population and prevention science of the American Heart Association. Circulation 109(21):2655–2671. https://doi.org/10.1161/01.CIR.0000128587.30041.C8
Bui LT, Nguyen PH, Nguyen DCM (2020) Model for assessing health damage from air pollution in quarrying area—case study at Tan Uyen quarry, Ho Chi Minh megapolis. Vietnam Heliyon 6(9):e05045. https://doi.org/10.1016/j.heliyon.2020.e05045
Bui LT, Nguyen PH, My Nguyen DC (2021) Linking air quality, health, and economic effect models for use in air pollution epidemiology studies with uncertain factors. Atmos Pollut Res 12(7):101118. https://doi.org/10.1016/j.apr.2021.101118
Burnett, R. T., Arden Pope, C., Ezzati, M., Olives, C., Lim, S. S., Mehta, S., Shin, H. H., Singh, G., Hubbell, B., Brauer, M., Ross Anderson, H., Smith, K. R., Balmes, J. R., Bruce, N. G., Kan, H., Laden, F., Prüss-Ustün, A., Turner, M. C., Gapstur, S. M., … Cohen, A. (2014). An integrated risk function for estimating the global burden of disease attributable to ambient fine particulate matter exposure. Environmental Health Perspectives, 122(4), 397–403. https://doi.org/10.1289/ehp.1307049
Burnett, R., Chen, H., Szyszkowicz, M., Fann, N., Hubbell, B., Pope, C. A., Apte, J. S., Brauer, M., Cohen, A., Weichenthal, S., Coggins, J., Di, Q., Brunekreef, B., Frostad, J., Lim, S. S., Kan, H., Walker, K. D., Thurston, G. D., Hayes, R. B., … Spadaro, J. V. (2018). Global estimates of mortality associated with longterm exposure to outdoor fine particulate matter. Proceedings of the National Academy of Sciences of the United States of America, 115(38), 9592–9597. https://doi.org/10.1073/pnas.1803222115
Chen L, Shi M, Gao S, Li S, Mao J, Zhang H, Sun Y, Bai Z, Wang Z (2017) Assessment of population exposure to PM2.5 for mortality in China and its public health benefit based on BenMAP. Environ Pollut 221:311–317. https://doi.org/10.1016/j.envpol.2016.11.080
Chinh Nguyen. (2013). Assessment of economic losses due to pollution and environmental degradation. National Political Publishing House;
Chi DTL, Toan VD, Linh QH, Van Chien V, Huyen VT (2020) Risk assessment for PM10 and PM2.5 in Hanoi, Vietnam: An ecological study. Pollution Research 39(4):971–979
Chowdhury S, Dey S (2016) Cause-specific premature death from ambient PM2.5 exposure in India: Estimate adjusted for baseline mortality. Environ Int 91:283–290. https://doi.org/10.1016/j.envint.2016.03.004
Cohen, A. J., Brauer, M., Burnett, R., Anderson, H. R., Frostad, J., Estep, K., Balakrishnan, K., Brunekreef, B., Dandona, L., Dandona, R., Feigin, V., Freedman, G., Hubbell, B., Jobling, A., Kan, H., Knibbs, L., Liu, Y., Martin, R., Morawska, L., … Forouzanfar, M. H. (2017). Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. The Lancet, 389(10082), 1907–1918. https://doi.org/10.1016/S0140-6736(17)30505-6
Dang, T. N., Thanh, N. N. N., Vien, N. T., Dung, P. H. T., An, N. D. T., Dung, T. T. T., & Giang, D. T. (2021). Mortality and economic burden of PM2.5 on cardiovascular disease in Ho Chi Minh City in 2018. Vietnam Journal of Preventive Medicine, 31(6), 9–18. https://doi.org/10.51403/0868-2836/2021/369
Decision on approving the National Action Plan on Air Quality Management to 2020, Vision to 2025, Pub. L. No. No: 985a/QD-TTg, 1 (2016).
Ding D, Zhu Y, Jang C, Lin CJ, Wang S, Fu J, Gao J, Deng S, Xie J, Qiu X (2016) Evaluation of health benefit using BenMAP-CE with an integrated scheme of model and monitor data during Guangzhou Asian Games. J Environ Sci (china) 42:9–18. https://doi.org/10.1016/j.jes.2015.06.003
Do TNN, Ngo XT, Pham VH, Vuong NL, Le HA, Pham CT, Bui QH, Nguyen TNT (2021) Application of WRF-Chem to simulate air quality over Northern Vietnam. Environ Sci Pollut Res 28(10):12067–12081. https://doi.org/10.1007/s11356-020-08913-y
Englert N (2004) Fine particles and human health—a review of epidemiological studies. Toxicol Lett 149(1–3):235–242. https://doi.org/10.1016/j.toxlet.2003.12.035
Europe WHORO, for. (2000) Air quality guidelines for Europe, 2nd edn. World Health Organization, Regional Office for Europe
Evans J, van Donkelaar A, Martin RV, Burnett R, Rainham DG, Birkett NJ, Krewski D (2013) Estimates of global mortality attributable to particulate air pollution using satellite imagery. Environ Res 120:33–42. https://doi.org/10.1016/j.envres.2012.08.005
Fold NR, Allison MR, Wood BC, Thao PTB, Bonnet S, Garivait S, Kamens R, Pengjan S (2020) An assessment of annual mortality attributable to ambient PM2.5 in Bangkok, Thailand. Int J Environ Res Public Health 17(19):1–14. https://doi.org/10.3390/ijerph17197298
Forouzanfar, M. H., Afshin, A., Alexander, L. T., Biryukov, S., Brauer, M., Cercy, K., Charlson, F. J., Cohen, A. J., Dandona, L., Estep, K., Ferrari, A. J., Frostad, J. J., Fullman, N., Godwin, W. W., Griswold, M., Hay, S. I., Kyu, H. H., Larson, H. J., Lim, S. S., … Zhu, J. (2016). Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet, 388(10053), 1659–1724. https://doi.org/10.1016/S0140-6736(16)31679-8
Fu G, An X, Liu H, Tian Y, Wang P (2020) Assessment of the impact of PM2.5 exposure on the daily mortality of circulatory system in Shijiazhuang, China. Atmosphere 11(9):1–11
Global Burden of disease collaborative network. (2019). Global Burden of Disease Study 2018 (GBD 2018) Population Estimates 1950–2018. Institute for Health Metrics and Evaluation (IHME).
GreenID. (2017). Report of Air Quality in 2017.
GSO. (2020). Completed results of the 2019 Vietnam population and housing census.
Guan Y, Xiao Y, Wang F, Qiu X, Zhang N (2021) Health impacts attributable to ambient PM2.5 and ozone pollution in major Chinese cities at seasonal-level. J Cleaner Production 311(May):127510. https://doi.org/10.1016/j.jclepro.2021.127510
Hammitt JK, Robinson LA (2011) The income elasticity of the value per statistical life: transferring estimates between high and low income populations. J Benefit-Cost Anal 2(1):1–29. https://doi.org/10.2202/2152-2812.1009
HCMC Statistical Office. (2019a). Part II: actual situation of economic growth of key economic region of South Vietnam in the period of 2010–2018. In Ho Chi Minh City Economy and the Southern Key Economic Region (19–30). Ho Chi Minh City Statistical Office.
HCMC Statistical Office. (2019b). Statistical Yearbook of Ho Chi Minh City 2018.
HCMC Statistical Office. (2020). Statistical Yearbook of Ho Chi Minh City 2019.
Hien TT, Chi NDT, Nguyen NT, Vinh LX, Takenaka N, Huy DH (2019) Current status of fine particulate matter (Pm2.5) in vietnam’s most populous city, ho chi minh city. Aerosol and Air Quality Research 19(10):2239–2251
Hieu VV, Quynh LX, Ho PN, Hens L (2013) Health risk assessment of mobility-related air pollution in Ha Noi Vietnam. J Environ Protection 04(10):1165–1172. https://doi.org/10.4236/jep.2013.410133
Ho BQ (2017) Modeling PM10 in Ho Chi Minh City, Vietnam and evaluation of its impact on human health. Susta Environ Res 27(2):95–102. https://doi.org/10.1016/j.serj.2017.01.001
Ho, B. Q., Vu, H. N. K., Nguyen, T. T., Nguyen, T. T. T., Nguyen, T. T. H., Khoa, N. T. D., Vu, N. V., & Hung, H. B. (2020). Develop a clean air action plan based on scientific data: a case of Ho Chi Minh city. Science and Technology Development Journal - Natural Sciences, 4(SI SE-Original Research). https://doi.org/10.32508/stdjns.v4i1.991
Hoffmann S, Batz MB, Morris JG Jr (2012) Annual cost of illness and quality-adjusted life year losses in the United States due to 14 foodborne pathogens†. J Food Prot 75(7):1292–1302. https://doi.org/10.4315/0362-028X.JFP-11-417
Huang D, Xu J, Zhang S (2012) Valuing the health risks of particulate air pollution in the Pearl River Delta China. Environ Sci Policy 15(1):38–47. https://doi.org/10.1016/j.envsci.2011.09.007
Huy DH, Chi NDT, Phu NLS, Hien TT (2018) Fine particulate matter (PM25) in Ho Chi Minh City: analysis of the status and the temporal variation based on the continuous data from 2013–2017. Sci Technol Dev J: Nat Sci 2(5):130–137
ICD-10. (2016). International Statistical Classification of Diseases and Related Health Problems 10th Revision.
IQAir. (2020). 2019 world air quality report—region and City PM2.5 Ranking.
Johnson RJ, Rolfe J, Windle J, Benner J (2015) The economics of non-market goods and resources benefit transfer of environmental and resource values. In Benefit Transfer Environ Res Values. https://doi.org/10.1007/978-94-017-9930-0
Jun M, Stein ML (2004) Statistical comparison of observed and CMAQ modeled daily sulfate levels. Atmos Environ 38(27):4427–4436. https://doi.org/10.1016/j.atmosenv.2004.05.019
Kalkan A, Hallert E, Bernfort L, Husberg M, Carlsson P (2014) Costs of rheumatoid arthritis during the period 1990–2010: a register-based cost-of-illness study in Sweden. Rheumatology 53(1):153–160. https://doi.org/10.1093/rheumatology/ket290
Khanh U. Le, Nguyen PH, Bui LT (2022) Risk assessment of hospital admission due to all–cause respiratory and cardiovascular diseases attributed to ground–level O3 short–term exposure in Dong Nai Province. Vietnam J Hydrometeorol 742:1–18
Kim D, Kim J, Jeong J, Choi M (2019) Estimation of health benefits from air quality improvement using the MODIS AOD dataset in Seoul Korea. Environmental Research 173(March):452–461. https://doi.org/10.1016/j.envres.2019.03.042
Krewski, D., Jerrett, M., Burnett, R. T., Ma, R., Hughes, E., Shi, Y., Turner, M. C., Pope, C. A. 3rd, Thurston, G., Calle, E. E., Thun, M. J., Beckerman, B., DeLuca, P., Finkelstein, N., Ito, K., Moore, D. K., Newbold, K. B., Ramsay, T., Ross, Z., … Tempalski, B. (2009). Extended follow-up and spatial analysis of the American Cancer Society study linking particulate air pollution and mortality. Research Report (Health Effects Institute), 140, 5–36
Li J, Liu H, Lv Z, Zhao R, Deng F, Wang C, Qin A, Yang X (2018) Estimation of PM2.5 mortality burden in China with new exposure estimation and local concentration-response function. Environ Pollut 243:1710–1718. https://doi.org/10.1016/j.envpol.2018.09.089
Li Jie, Huang L, Han B, van der Kuijp TJ, Xia Y, Chen K (2021) Exposure and perception of PM2.5 pollution on the mental stress of pregnant women. Environment International 156:106686
Li, Y., Chen, Z., & Li, J. (2017). How many people died due to PM2.5 and where the mortality risks increased? A case study in Beijing. 2017 IEEE International Geoscience and Remote Sensing Symposium (IGARSS), 485–488. https://doi.org/10.1109/IGARSS.2017.8126997
Lim, S. S., Vos, T., Flaxman, A. D., Danaei, G., Shibuya, K., Adair-Rohani, H., Amann, M., Anderson, H. R., Andrews, K. G., Aryee, M., Atkinson, C., Bacchus, L. J., Bahalim, A. N., Balakrishnan, K., Balmes, J., Barker-Collo, S., Baxter, A., Bell, M. L., Blore, J. D., … Ezzati, M. (2012). A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: A systematic analysis for the Global Burden of Disease Study 2010. The Lancet, 380(9859), 2224–2260. https://doi.org/10.1016/S0140-6736(12)61766-8
Liu M, Saari RK, Zhou G, Li J, Han L, Liu X (2021) Recent trends in premature mortality and health disparities attributable to ambient PM25 exposure in China: 2005–2017. Environmental Pollution 279:116882
Lu X, Lin C, Li W, Chen Y, Huang Y, Fung JCH, Lau AKH (2019) Analysis of the adverse health effects of PM2.5 from 2001 to 2017 in China and the role of urbanization in aggravating the health burden. Sci Total Environ 652:683–695. https://doi.org/10.1016/j.scitotenv.2018.10.140
Luo G, Zhang L, Hu X, Qiu R (2020) Quantifying public health benefits of PM2.5 reduction and spatial distribution analysis in China. Science of the Total Environment 719:137445
Luong LMT, Phung D, Sly PD, Morawska L, Thai PK (2017) The association between particulate air pollution and respiratory admissions among young children in Hanoi. Vietnam Sci Total Environ 578:249–255. https://doi.org/10.1016/j.scitotenv.2016.08.012
Luong LTM, Dang TN, Thanh Huong NT, Phung D, Tran LK, Van Dung D, Thai PK (2020) Particulate air pollution in Ho Chi Minh city and risk of hospital admission for acute lower respiratory infection (ALRI) among young children. Environ Pollut 257:113424. https://doi.org/10.1016/j.envpol.2019.113424
Maji KJ, Ye WF, Arora M, Nagendra SMS (2019) Ozone pollution in Chinese cities: assessment of seasonal variation, health effects and economic burden. Environmental Pollution 247(1):792–801. https://doi.org/10.1016/j.envpol.2019.01.049
Manojkumar, N., & Srimuruganandam, B. (2021). Health benefits of achieving fine particulate matter standards in India—a nationwide assessment. Science of the Total Environment, 763. https://doi.org/10.1016/j.scitotenv.2020.142999
Mehta S, Shin H, Burnett R, North T, Cohen AJ (2013) Ambient particulate air pollution and acute lower respiratory infections: a systematic review and implications for estimating the global burden of disease. Air Qual Atmos Health 6(1):69–83. https://doi.org/10.1007/s11869-011-0146-3
Ministry of Health. (2019). The Health Statistics Yearbook 2018.
MONRE. (2018). Vietnam National Environmental Report 2017.
Narain, U., & Sall, C. (2016). Methodology for valuing the health impacts of air pollution.
Nguyen TNT, Le HA, Mac TMT, Nguyen TTN, Pham VH, Bui QH (2018) Current Status of PM25 pollution and its mitigation in Vietnam. Global Environ Res 22(3):073–083
Nhung NTT, Long TK, Linh BN, Vos T, Huong NT, Anh ND (2013) Estimation of Vietnam National Burden of Disease 2008. Asia Pacific J Publ Health 26(5):527–535. https://doi.org/10.1177/1010539513510556
Nhung NTT, Schindler C, Dien TM, Probst-Hensch N, Perez L, Künzli N (2018) Acute effects of ambient air pollution on lower respiratory infections in Hanoi children: an eight-year time series study. Environ Int 110:139–148. https://doi.org/10.1016/j.envint.2017.10.024
Nhung NTT, Schindler C, Dien TM, Probst-Hensch N, Künzli N (2019) Association of ambient air pollution with lengths of hospital stay for hanoi children with acute lower-respiratory infection, 2007–2016. Environ Pollut 247:752–762. https://doi.org/10.1016/j.envpol.2019.01.115
OECD. (2012). Mortality risk valuation in environment, health and transport policies. https://doi.org/10.1787/9789264130807-en
Ho Chi Minh City Statistical Office. (2019). Ho Chi Minh City statistical Yearbook 2018.
Phan CC, Nguyen TQH, Nguyen MK, Park KH, Bae GN, Seung-bok L, Bach QV (2020) Aerosol mass and major composition characterization of ambient air in Ho Chi Minh City Vietnam. Internat J Environ Sci Technol 17(6):3189–3198. https://doi.org/10.1007/s13762-020-02640-0
Pope CA, Dockery DW (2006) Health effects of fine particulate air pollution: lines that connect. J Air Waste Manag Assoc 56(6):709–742. https://doi.org/10.1080/10473289.2006.10464485
Pope CA III, Burnett RT, Thun MJ, Calle EE, Krewski D, Ito K, Thurston GD (2002) Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. JAMA 287(9):1132–1141. https://doi.org/10.1001/jama.287.9.1132
Pope AC, Burnett RT, Krewski D, Jerrett M, Shi Y, Calle EE, Thun MJ (2009) Cardiovascular mortality and exposure to airborne fine particulate matter and cigarette smoke shape of the exposure-response relationship. Circulation 120(11):941–948. https://doi.org/10.1161/CIRCULATIONAHA.109.857888
Quah E, Boon TL (2003) The economic cost of particulate air pollution on health in Singapore. J Asian Econ 14(1):73–90. https://doi.org/10.1016/S1049-0078(02)00240-3
Sacks JD, Lloyd JM, Zhu Y, Anderton J, Jang CJ, Hubbell B, Fann N (2018) The environmental benefits mapping and analysis program—community edition (BenMAP–CE): a tool to estimate the health and economic benefits of reducing air pollution. Environ Model Softw 104(2):118–129. https://doi.org/10.1016/j.envsoft.2018.02.009
Smith KR, Jantunen M (2002) Why particles? Chemosphere 49(9):867–871. https://doi.org/10.1016/S0045-6535(02)00235-7
Stanaway, J. D., Afshin, A., Gakidou, E., Lim, S. S., Abate, D., Abate, K. H., Abbafati, C., Abbasi, N., Abbastabar, H., Abd-Allah, F., Abdela, J., Abdelalim, A., Abdollahpour, I., Abdulkader, R. S., Abebe, M., Abebe, Z., Abera, S. F., Abil, O. Z., Abraha, H. N., … Murray, C. J. L. (2018). Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Stu. The Lancet, 392(10159), 1923–1994. https://doi.org/10.1016/S0140-6736(18)32225-6
Tang L, Nagashima T, Hasegawa K, Ohara T, Sudo K, Itsubo N (2018) Development of human health damage factors for PM25 based on a global chemical transport model. Int J Life Cycle Assessment 23(12):2300–2310
Tao H, Xing J, Zhou H, Pleim J, Ran L, Chang X, Wang S, Chen F, Zheng H, Li J (2020) Impacts of improved modeling resolution on the simulation of meteorology, air quality, and human exposure to PM2.5, O3 in Beijing China. J Cleaner Prod 243:118574
The World Bank. (2018). GDP per capita, PPP (constant 2011 international $) and PPP conversion factor, GDP (LCU per international $) | Vietnam | 2006 - 2017. The TrendEconomy.
The World Bank Data. (2020). GDP per capita, PPP (current international $)—Data of Vietnam. The World Bank Data.
Thu, N. T. A., Blume, L., Addison, E., & Franielczyk, K. (2018). Air quality in Vietnam in 2017. In Air Quality Report - GreenID (Issue 2).
Toledo T, Albuquerque DA, Andrade MDF, Ynoue RY, Moreira DM, Andreão WL, Soares F (2018) WRF-SMOKE-CMAQ modeling system for air quality evaluation in São Paulo megacity with a 2008 experimental campaign data. Environ Sci Pollut Res 25:36555–36569
Vu HNK, Ha QP, Nguyen DH, Nguyen TTT, Nguyen TT, Nguyen TTH, Tran ND, Ho BQ (2020) Poor air quality and its association with mortality in Ho Chi Minh city: Case study. Atmosphere 11(7):1–20. https://doi.org/10.3390/atmos11070750
Wang Y, Wild O, Chen X, Wu Q, Gao M, Chen H, Qi Y, Wang Z (2020) Health impacts of long-term ozone exposure in China over 2013–2017. Environ Int 144:106030. https://doi.org/10.1016/j.envint.2020.106030
Wang, Y., Wild, O., Chen, H., Gao, M., Wu, Q., Qi, Y., Chen, X., & Wang, Z. (2020a). Acute and chronic health impacts of PM2.5 in China and the influence of interannual meteorological variability. Atmospheric Environment, 229(February). https://doi.org/10.1016/j.atmosenv.2020a.117397
WHO. (2006). WHO Air quality guidelines for particulate matter, ozone, nitrogen dioxide and sulfur dioxide. In World Health Organization (Vol. 51, Issue 6).
WHO. (2021). WHO global air quality guidelines. Particulate matter (PM2.5 and PM10), Ozone, nitrogen dioxide, sulfur dioxide and carbon monoxide. In World Health Organization.
Xiao Q, Geng G, Xue T, Liu S, Cai C, He K, Zhang Q (2022) Tracking PM25 and O3 Pollution and the Related Health Burden in China 2013–2020. Environ Sci Technol 56(11):6922–6932
Xiong, J., Ye, C., Zhou, T., & Cheng, W. (2019). Health risk and resilience assessment with respect to the main air pollutants in sichuan. International Journal of Environmental Research and Public Health, 16(15). https://doi.org/10.3390/ijerph16152796
Ye T, Guo S, Xie Y, Chen Z, Abramson MJ, Heyworth J, Hales S, Woodward A, Bell M, Guo Y, Li S (2021) Health and related economic benefits associated with reduction in air pollution during COVID-19 outbreak in 367 cities in China. Ecotoxicol Environ Saf 222(June):112481. https://doi.org/10.1016/j.ecoenv.2021.112481
Yin H, Pizzol M, Xu L (2017) External costs of PM2.5 pollution in Beijing, China: uncertainty analysis of multiple health impacts and costs. Environ Pollut 226:356–369. https://doi.org/10.1016/j.envpol.2017.02.029
Yorifuji, T., Bae, S., Kashima, S., Tsuda, T., Doi, H., Honda, Y., Kim, H., & Hong, Y.-C. (2015). Health impact assessment of PM10 and PM2.5 in 27 Southeast and East Asian cities. Journal of Occupational and Environmental Medicine, 57(7).
Yu G, Wang F, Hu J, Liao Y, Liu X (2019) Value assessment of health losses caused by PM25 in Changsha city, China. Int J Environ Res Public Health 16(11):1–21. https://doi.org/10.3390/ijerph16112063
Zhang L, He X, Xiong Y, Ran Q, Xiong A, Wang J, Wu D, Niu B, Li G (2021) Transcriptome-wide profiling discover: PM25 aggravates airway dysfunction through epithelial barrier damage regulated by Stanniocalcin 2 in an OVA-induced model. Ecotoxicology and Environmental Safety 220:112408. https://doi.org/10.1016/j.ecoenv.2021.112408
Zhao B, Wang S, Ding D, Wu W, Chang X, Wang J, Xing J, Jang C, Fu JS, Zhu Y, Zheng M, Gu Y (2019) Nonlinear relationships between air pollutant emissions and PM 2.5 -related health impacts in the Beijing-Tianjin-Hebei region. Sci Total Environ 661:375–385. https://doi.org/10.1016/j.scitotenv.2019.01.169
Acknowledgements
We acknowledge the support of time and facilities from Ho Chi Minh City University of Technology (HCMUT), VNU-HCM for this study.
Funding
We acknowledge the support of time and facilities from Ho Chi Minh City University of Technology (HCMUT), VNU- HCM for this study.
Author information
Authors and Affiliations
Contributions
Long Ta Bui: conceptualization, funding acquisition, investigation, project administration, resources, supervision, methodology, models, writing—original draft, writing—review and editing. Phong Hoang Nguyen: Data curation, data analysis, formal analysis, validation, GIS.
Corresponding authors
Ethics declarations
Ethics approval
The authors declare that the manuscript is not submitted to more than one journal for simultaneous consideration. The manuscript is original and not have been published elsewhere in any form or language (partially or in full), unless the new work concerns an expansion of previous work. The manuscript is not split up into several parts to increase the quantity of submissions and submitted to various journals or to one journal over time (i.e. “salami-slicing/publishing”). Results are presented clearly, honestly and without fabrication, falsification or inappropriate data manipulation. We adhere to discipline-specific rules for acquiring, selecting and processing data. We have provided all data and proper mentions of other works.
Consent to participate
I consent to participate publish my manuscript entitled “Evaluation of the annual economic costs associated with PM2.5-based health damage—A case study in Ho Chi Minh City, Vietnam” to the Air Quality, Atmosphere & Health (AIRQ).
Consent for publication
I consent to publish my manuscript entitled “Evaluation of the annual economic costs associated with PM2.5-based health damage—A case study in Ho Chi Minh City, Vietnam” to the Air Quality, Atmosphere & Health (AIRQ).
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Bui, L.T., Nguyen, P.H. Evaluation of the annual economic costs associated with PM2.5-based health damage—a case study in Ho Chi Minh City, Vietnam. Air Qual Atmos Health 16, 415–435 (2023). https://doi.org/10.1007/s11869-022-01282-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11869-022-01282-0