Abstract
Background
Retinal microvascular diameters and large artery stiffness are valid biomarkers of cardiovascular risk. This study assessed short- and long-term micro- and macrovascular improvements after bariatric surgery (BS).
Methods
Sixteen patients (44 ± 12 years) underwent BS in this observational study. Two weeks before as well as 6 weeks and 4 years after surgery, retinal vessel analysis and assessment of brachial-ankle pulse wave velocity (baPWV), cardio-ankle vascular index (CAVI), and anthropometry were performed. Three patients were lost to follow-up.
Results
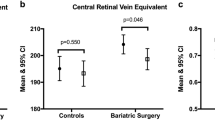
Six weeks after BS, retinal arteriolar diameters (CRAE) were wider (180.1 μm vs. 188.1 μm; p = 0.001), and the arteriolar-to-venular diameter ratio (AVR) was higher (0.82 vs. 0.86; p < 0.001) compared to baseline levels. During the 4 years of follow-up, the retinal changes sustained but further improvements did not occur. Both indices of large artery stiffness, baPWV and CAVI, remained unchanged 6 weeks and 4 years after surgery.
Conclusions
Retinal microvascular phenotype improved 6 weeks after BS. The improvements in microvascular health were maintained during 4 years of follow-up but, despite significant further reductions in body mass index, did not improve further long-term. baPWV and CAVI were unaffected after surgery indicating that BS primarily affects microvascular phenotype rather than large artery stiffness. Retinal vessel imaging seems to be a feasible diagnostic tool to monitor microvascular health after BS. Normalization of BMI and blood pressure may be necessary to achieve long-term improvement of large artery phenotype after BS.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Bariatric surgery (BS) reduces cardiovascular morbidity and mortality [1,2,3] by improving associated risk factors, such as high body fat, inflammatory status, glucose and lipid metabolism, blood pressure, and left ventricular diastolic function [4,5,6]. Several studies show that these pleiotropic effects of weight-loss by surgery translate into reduced cardiovascular risk by improving different vascular biomarkers. Habib et al. showed a reduced intima-media thickness and higher flow-mediated dilation in 50 subjects 24 months after BS [7]. Aortic elastic properties and left ventricular diastolic function improved during a 36 months follow-up after BS in 60 subjects [8]. Shargorodsky et al. showed improved large arterial elasticity, which is assessed by pulse wave contour analysis in 21 patients with a high cardiovascular risk 16 weeks after BS [9]. Carotid intima-media thickness was reduced in a type 2 diabetic population 12 months after BS [10]. Bäckdahl et al. found a reduced aortic pulse wave velocity (PWV) in 82 subjects 2 years after BS and associated this effect to a reduction in white adipose tissue [11]. However, the effects of BS on the microvascular structure and function are less clear. Nerla and Tarzia showed an improved microcirculatory coronary blood flow in response to intravenous adenosine application and cold pressure test 3 months and 4 years after BS [12, 13]. Martin-Rodriguez et al. found improved post-occlusive reactive hyperemia in the forearm skin in obese patients without signs of metabolic syndrome after BS [14].
No study to date has investigated the combined short- and long-term effects of BS on macro- and microvascular phenotypes in the same population. It remains to be shown which vascular bed is most sensitive to the metabolic changes after BS. Retinal vascular diameters and arterial stiffness are sensitive micro- and macrovascular biomarkers, which may be used for monitoring cardiovascular risk after BS. Therefore, the aim of this observational study was to assess short- and long-term improvements of both, small and large artery structure and function 6 weeks and 4 years after BS.
Methods
Study Design
Between January and June 2012, we recruited participants scheduled for BS at St. Claraspital Basel (Switzerland). After signing the informed consent, participants had to attend three appointments: the pre-surgery appointment 2 weeks before surgery and two post-surgery appointments 6 weeks and 4 years after surgery. The surgery was performed in the Claraspital Basel. All measurements and data analysis were performed in the Department of Sport, Exercise, and Health of the University Basel in accordance with the Declaration of Helsinki. The local ethical committee (Ethikkommission Nordwest- und Zentralschweiz 2015-00250) approved the study.
Inclusion and Exclusion Criteria
Inclusion criteria were a (body mass index) BMI > 40 kg/m2 or a BMI > 35 with comorbidities, such as hypertension or diabetes. Exclusion criteria were age > 65 years, macular degeneration, glaucoma, or any chronic eye disease, which might affect the retinal microcirculation.
Assessment of Anthropometric Data
Assessment of anthropometric data included standardized measurement of height, total body mass, waist circumference, and BMI.
Macrovascular Assessment
Patients were advised to refrain from moderate and vigorous physical activity for 24 h, to refrain from smoking on the day of assessment and to remain fasting for 12 h with the exception to drink water or unsweetened tea up to 2 h prior to the appointment. We used the non-invasive oscillometric VaSera VS-1500N vascular screening system (Fukuda Denshi Co. Ltd., Tokyo, Japan) to obtain brachial-ankle pulse wave velocity (baPWV) and cardio-ankle vascular index (CAVI). Both parameters are well established and widely used as surrogate markers of arterial stiffness and are associated with overall cardiovascular morbidity and mortality [15]. Reproducibility of this method is excellent with mean variation coefficients of 3.9% for baPWV and 4.4% for CAVI, respectively [16]. The basic methodological principle has been described elsewhere, and the procedure was conducted as previously described [16]. After the participant had rested for at least 10 min in a lying position, two measurements on each side were taken in a supine position at 3–5-min intervals. Measurements with a good or very good quality, quantified by the VaSera System, were used for further analysis. Additionally, heart rate and oscillometric blood pressure were measured non-invasively twice at each arm with a VaSera VS-1500N device. Systolic and diastolic blood pressure and mean arterial pressure (MAP = [2 × diastolic blood pressure + systolic blood pressure] / 3) were calculated as the mean of two measurements on the left and two on the right side.
Microvascular Assessment
After 5minutes of rest in a sitting position, retinal microvascular imaging was conducted with a static retinal vessel analyzer (SVA-T, Imedos Systems UG, Jena, Germany). For static retinal vessel analysis, we analyzed two valid pictures from both eyes with an angle of 45° and the optic disc in the center. Venular and arteriolar diameters were analyzed semi-automatically by coursing through an area of 0.5–1 disc diameter from the optic disc margin, at higher magnification and using special analyzing software (Vesselmap 2, Visualis, Imedos Systems UG). Diameters were averaged to the central retinal arteriolar equivalent (CRAE) and the central retinal venular equivalent (CRVE) by using the Parr-Hubbard formula [17]. The retinal arteriolar-to-venular ratio (AVR) was calculated from the CRAE and CRVE. The inter-observer and intra-observer interclass correlation coefficient for the measurement of retinal vessel diameters ranges from 0.97 to 0.98.
Statistical Analysis and Sample Size Calculation
Data analysis was performed with R version 3.4.2 for Windows (R Foundation for Statistical Computing, Vienna, Austria). Descriptive analysis included means and standard deviation (SD). The level of significance was set at p < 0.05. To analyze the progression of our main outcome (AVR) from baseline to 4-years follow up, we used multi-level modeling as an analysis tool for repeated measures data [18]. Model selection was based on Akaike’s information criterion. In case of significance, we applied post hoc tests for pairwise analysis. In the presence of repeated measurements, observations are no longer independent, which makes usual analysis methods, such as linear regression model unsuitable for the analysis of our data. Multilevel models (or linear mixed models) are regression models that take the correlation between repeated measurements into account [18].
Based on previous findings, we assumed an expected difference in AVR between baseline and 4-years follow-up of 0.04 with a SD of 0.08 [19]. A total sample size of 15 patients was needed to reach a target power of 80% with a two-sided significance level of 0.05. G*Power software 3.1.9.2 was used for the sample size calculation.
Results
Patients’ Characteristics at Baseline and 6 Weeks and 4 Years After Bariatric Surgery
Sixteen participants with a mean age of 44 ± 12 years (22–61 years, 13 male and three female) at the baseline appointment were included in this trial. Three participants refused to participate in the follow-up appointment after a mean follow-up of 4 years (Fig. 1). Three patients were smokers and seven were ex-smokers. Fasting metabolic blood parameters at baseline were total cholesterol (5.1 ± 1.1 mmol/L), high-density lipoprotein (1.4 ± 0.3 mmol/L), low-density lipoprotein (3.1 ± 0.9 mmol/L), triglycerides (1.4 ± 0.6 mmol/L), fasting blood glucose (5.2 ± 1.1 mmol/L), and HbA1c (5.7 ± 0.4%). The inflammatory markers were high sensitivity C-reactive protein (5.0 ± 4.6 mg/L) and leucocytes (7.4 ± 2.0 × 109/L). Markers for hepatic function were aspartate aminotransferase (25.2 ± 6.7 U/L), alanine aminotransferase (33.8 ± 18.3 U/L), and γ-glutamyltransferase (42.3 ± 17.8 U/L). Ten participants took anti-hypertensive medication, and ten patients were on lipid-lowering medication. The surgical method of choice was laparoscopic sleeve gastrectomy in five patients and Roux-en-Y gastric bypass in 11 patients. Anthropometric measures and blood pressure improved throughout the study period (Table 1). Three participants reduced their anti-hypertensive medications after 6 weeks post-surgery, and seven participants reduced their anti-hypertensive medications until the follow-up after 4 years. Despite improved blood pressure, three patients still had high-normal values, and six patients were hypertensive 4 years after BS. The mean weight loss during the study period was 39.5 kg (Fig. 2). Despite extensive weight loss, six patients were still overweight and obesity remained in seven patients after 4 years.
Microvascular Changes after Bariatric Surgery
The retinal microcirculation showed wider arteriolar diameters 6 weeks and 4 years after BS compared to baseline, without further significant improvements between 6 weeks and 4 years after BS (Table 1). Venular diameters did not change between the time points. AVR increased 6 weeks and 4 years after BS compared to baseline, without further changes between 6 weeks and 4 years after BS. Microvascular short- and long-term effects were independent of MAP changes (p < 0.01).
Macrovascular Changes After Bariatric Surgery
CAVI and baPWV did not change significantly during the follow-up period compared to baseline in the models without and with adjustment for MAP (Table 1).
Discussion
This study was designed to investigate microvascular and macrovascular improvements 6 weeks and 4 years after BS. Our preliminary results demonstrated an improved microvascular phenotype independent of blood pressure changes in the early post-surgical phase after 6 weeks. CAVI and baPWV did not change, suggesting that the macrovascular system might be less sensitive to early metabolic changes after BS than the microvascular system. Neither retinal vessel diameters nor CAVI or baPWV further improved during the 4 years of follow-up despite ongoing body weight reduction in our patients.
Short- and Long-Term Changes in Microvascular Function After BS
Subacute improvements in the coronary microcirculation and peripheral endothelial function after BS have been shown before [12]. Our results demonstrate that retinal vessels might also be sensitive to the surgery-related metabolic and physiological changes in the early post-surgical period. These changes are reflected by reductions in blood pressure and weight loss, which might therefore be the main contributors for early microvascular improvements after BS. Blood pressure changes are known as an important factor for alterations of retinal arteriolar diameters [20]. Nevertheless, we demonstrated an MAP-independent increase in AVR based on wider arteriolar diameters, indicating that there are blood pressure independent mechanisms responsible for the microvascular improvements. A previous meta-analysis demonstrated that higher BMI is associated with narrower arterioles and wider venules [21]. Systemic inflammation has been argued to be responsible for wider venular diameters in patients with obesity [21]. Nevertheless, CRVE did not change in our study population after BS, despite considerable improvements in body composition. As overweight or obesity were still prevalent in most patients at this point, normalization of body weight might be necessary to achieve relevant improvements of CRVE.
In contrast, retinal arterioles widened in our study population post-surgery. Stapleton and colleagues showed that the bioavailability of nitric oxide is reduced in an obesogenic environment and that weight loss may lead to an attenuation of this deficit [22]. Therefore, increased bioavailability of nitric oxide after BS may be a main reason for the widening of arterioles. Further studies should include biomarkers of systemic inflammation, glucose, and lipid metabolism in order to identify possible metabolic effects of BS on the microcirculation.
Tarzia and colleagues showed no further changes of subacute improvements in micro- and macrovascular function 4 years after BS despite ongoing weight loss and reduced cardiovascular risk factors in 19 patients [13]. However, they used flow mediated dilation and ultrasound-guided coronary flow reserve as markers of vascular function. Thus, our study is the first to investigate transition of short-term to long-term changes in retinal microvascular health compared to large artery stiffness after BS. Our results are in line with findings of Tarzia and colleagues, showing no additional improvement of microvascular health despite ongoing weight loss and reduced waist-circumference. Based on our results and two previous studies on the effects of BS on retinal microvascular health, we would like to postulate the following assumptions: The positive effects of BS on retinal microvascular health seem to occur during the first post-surgical year [19, 23]. We performed a short-term follow-up after 6 weeks in our study, and the effects of BS were more or less immediate. Lammert et al. [18] found wider arterioles, narrower venules, and a higher AVR 9 months after BS. However, the time of post-surgical follow-up varied from six to 23 months in their sample of 30 patients. Bachmayer et al. [22] also observed an improved microvascular phenotype in a population of 21 patients 10 months after BS. They reported narrower venules and a higher AVR, whereas the retinal arterioles were unaffected after BS. Depending on the development of the individual risk profiles of the patients after BS, amelioration of retinal microvascular health is detected by improvements of either retinal arteriolar or venular diameter or both. This finding is supported by the above-mentioned meta-analysis by Boillot et al. [20], which demonstrated that obesity is associated with either retinal arteriolar narrowing or venular widening. In line with our findings, retinal arteriolar diameters have been found to be more strongly associated with the CV risk profile in obesity.
Further improvements in microvascular health after BS do not seem to be facilitated by further continuous weight loss alone. Although considerable weight loss was achieved in our patients, overweight or obesity was still prevalent, and blood pressure levels were still elevated or high-normal in most of our patients. Further improvements and actual amelioration of microvascular health may depend on achieving normal values for weight, blood pressure, and metabolic regulation. In addition to dietary measures and drug treatment of comorbidities, an active lifestyle may play a key role in improvement of microvascular health. We have previously shown that endurance exercise training can reverse alterations of retinal vessel diameters in individuals with obesity [24]. A tendency towards further improvement of AVR after 4 years was detected and may also have reached statistical and clinical significance in a larger cohort.
Short- and Long-Term Changes in Macrovascular Function After BS
In contrast to the microvascular markers, CAVI and baPWV did not change during the early post-surgical phase, despite reductions in blood pressure. These results are in contrast to previous reports, which found a reduction in PWV after weight loss [25, 26]. However, baseline baPWV was not elevated in all but two of our patients, and a post-surgical improvement was seen only in these two participants. Accordingly, the previously reported independent effect of weight loss on PWV might occur in people with increased PWV but not in those with baPWV values within the normal range [5]. Our observation that CAVI and baPWV did improve neither short-term nor long-term after BS seems to stand in contrast to several other studies [27, 28]. Based on our data, we would like to speculate that baPWV and CAVI do not improve after BS unless pre-surgical values are elevated. Moreover, most of the above referenced studies assessed carotid-femoral PWV, which is calculated including the superficial distance between the two measurement points [29]. Hence, this method is vulnerable to overestimation of PWV especially in individuals with extensive central obesity [30]. Therefore, the use of carotid-femoral PWV for monitoring of changes in arterial stiffness after BS-induced weight loss carries the risk of misinterpretation, as a reduction in follow-up measurements might simply reflect the concurrent weight loss. Utilization of baPWV might be advantageous in studies with participants having morbid obesity, as the simplified measurement of pulse wave travel distance, using linear regression of body height, eliminates body surface-related measurement errors [31]. This is also the reason why we applied measures of systemic (global) arterial stiffness in our study setting. We further considered the oscillometric nature of baPWV and CAVI measurement to enhance accuracy compared to tonometric measurement of arterial stiffness. This study is the first to use markers of systemic arterial stiffness (baPWV and CAVI) rather than central arterial stiffness to assess changes in arterial wall integrity after BS. However, systemic arterial stiffness may not be the best marker to pick up changes in arterial stiffness after BS. Future studies should consider the concomitant use of diagnostic methods to assess both central and systemic arterial stiffness in patients with metabolic disease.
Previous studies showed an association of PWV with collagen depositioning, serum elastase activity, and metalloproteinase-9, suggesting that obesity might cause arterial stiffening by promotion of vascular wall remodeling [32]. The regression of such profound structural alterations is likely to take longer than a few weeks. Hence, post-surgical improvements of central arterial stiffness may need months or years to occur. This suggests that the macrovascular system might be less sensitive to early metabolic changes after BS than the microvascular system. However, in our study, baPWV and CAVI did not change during the 4-year follow-up period despite ongoing weight loss and blood pressure reduction. The normal baseline values of baPWV and CAVI might help explain the results of our study. Moreover, arterial stiffness was our secondary endpoint, and the study was not powered to detect changes in large artery stiffness. Larger sample size may be necessary to detect significant changes in arterial stiffness after BS.
Limitations
This study was powered for the main outcome AVR. Due to the patients lost to follow-up, the long-term follow-up was slightly underpowered. Nevertheless, the retinal microcirculation seems to be sufficiently sensitive to monitor vascular regeneration after BS in a short- and a long-term setting. Future prospective larger scale studies are warranted to investigate the predictive value of retinal microvascular health for long-term cardiovascular outcome after BS.
In patients with metabolic syndrome, the effect of BS on micro- and macrovascular health may be different compared to metabolically healthy patients [14]. Hence, it is important to note that the small sample size of our study did not allow grouping of our patients according to metabolic criteria, such as glucose tolerance, insulin sensitivity, blood lipids, free fatty acids, and inflammatory markers. The normal baseline values of baPWV and CAVI might be responsible for the lack of significant results for these macrovascular biomarkers. In terms of their interpretation, it is important to note that current reference values only exist for central Asian populations [33, 34]. We did not monitor changes in lifestyle behavior. Changes in physical activity and eating habits may influence weight loss and should therefore be considered in future studies on vascular changes after BS. Three patients did not attend the follow-up appointment 4 years after BS. However, tendencies of changes in retinal vessel analysis parameters, CAVI and baPWV in the early post-surgical appointment, were in line with those of the whole study cohort.
Conclusions and Perspectives
This study is the first to investigate early post-surgical changes of macro- and microvascular phenotype in patients with morbid obesity 6 weeks after BS and to track long-term effects over a 4-year follow-up period. CAVI and baPWV were used for the first time to investigate macrovascular effects of BS. We found an amelioration of the microvascular phenotype 6 weeks after BS, which was maintained but not improved any further after 4 years, despite further long-term reduction in BMI. Large artery stiffness remained unaffected after BS both short- as well as long-term. Despite extensive weight loss, normalization of body weight and blood pressure might be necessary to achieve further improvements of vascular health and risk reduction. In the future, a larger prospective cohort study should aim at exploring the underlying mechanisms and causality of post-surgical changes in micro- and macrovascular phenotype. Our results indicate that retinal vessel phenotyping may proof to be a valid diagnostic and more sensitive diagnostic tool than large artery stiffness to monitor development of cardiovascular risk after BS.
Abbreviations
- AVR:
-
retinal arteriolar-to-venular diameter ratio
- baPWV:
-
brachial-ankle pulse wave velocity (m/s)
- BMI:
-
body mass index (kg/m2)
- BS:
-
bariatric surgery
- CAVI:
-
cardio-ankle vascular index
- CRAE:
-
central retinal arteriolar equivalent (μm)
- CRVE:
-
central retinal venular equivalent (μm)
- MAP:
-
mean arterial pressure (mmHg)
- PWV:
-
pulse wave velocity (m/s)
References
Kwok CS, Pradhan A, Khan MA, et al. Bariatric surgery and its impact on cardiovascular disease and mortality: a systematic review and meta-analysis. Int J Cardiol. 2014;173(1):20–8. https://doi.org/10.1016/j.ijcard.2014.02.026.
Sjostrom L, Peltonen M, Jacobson P, et al. Bariatric surgery and long-term cardiovascular events. JAMA. 2012;307(1):56–65. https://doi.org/10.1001/jama.2011.1914.
Sjostrom L, Peltonen M, Jacobson P, et al. Association of bariatric surgery with long-term remission of type 2 diabetes and with microvascular and macrovascular complications. JAMA. 2014;311(22):2297–304. https://doi.org/10.1001/jama.2014.5988.
Vest AR, Heneghan HM, Agarwal S, et al. Bariatric surgery and cardiovascular outcomes: a systematic review. Heart. 2012;98(24):1763–77. https://doi.org/10.1136/heartjnl-2012-301778.
Petersen KS, Blanch N, Keogh JB, et al. Effect of weight loss on pulse wave velocity: systematic review and meta-analysis. Arterioscler Thromb Vasc Biol. 2015;35(1):243–52. https://doi.org/10.1161/atvbaha.114.304798.
Boido A, Ceriani V, Cetta F, et al. Bariatric surgery and prevention of cardiovascular events and mortality in morbid obesity: mechanisms of action and choice of surgery. Nutr Metab Cardiovasc Dis. 2015;25(5):437–43. https://doi.org/10.1016/j.numecd.2015.01.011.
Habib P, Scrocco JD, Terek M, et al. Effects of bariatric surgery on inflammatory, functional and structural markers of coronary atherosclerosis. Am J Cardiol. 2009;104(9):1251–5. https://doi.org/10.1016/j.amjcard.2009.06.042.
Ikonomidis I, Mazarakis A, Papadopoulos C, et al. Weight loss after bariatric surgery improves aortic elastic properties and left ventricular function in individuals with morbid obesity: a 3-year follow-up study. J Hypertens. 2007;25(2):439–47. https://doi.org/10.1097/HJH.0b013e3280115bfb.
Shargorodsky M, Fleed A, Boaz M, et al. The effect of a rapid weight loss induced by laparoscopic adjustable gastric banding on arterial stiffness, metabolic and inflammatory parameters in patients with morbid obesity. Int J Obes. 2006;30(11):1632–8. https://doi.org/10.1038/sj.ijo.0803320.
Lundby-Christensen L, Tarnow L, Hansen DL, et al. Carotid intima-media thickness is reduced 12 months after gastric bypass surgery in obese patients with type 2 diabetes or impaired glucose tolerance. J Diabetes Complicat. 2014;28(4):517–22. https://doi.org/10.1016/j.jdiacomp.2014.03.005.
Backdahl J, Andersson DP, Eriksson-Hogling D, et al. Long-term improvement in aortic pulse wave velocity after weight loss can be predicted by white adipose tissue factors. Am J Hypertens. 2017;31:450–7. https://doi.org/10.1093/ajh/hpx201.
Nerla R, Tarzia P, Sestito A, et al. Effect of bariatric surgery on peripheral flow-mediated dilation and coronary microvascular function. Nutr Metab Cardiovasc Dis. 2012;22(8):626–34. https://doi.org/10.1016/j.numecd.2010.10.004.
Tarzia P, Lanza GA, Sestito A, et al. Long-term effects of bariatric surgery on peripheral endothelial function and coronary microvascular function. Obes Res Clin Pract. 2017;11(1):114–7. https://doi.org/10.1016/j.orcp.2016.12.005.
Martin-Rodriguez JF, Cervera-Barajas A, Madrazo-Atutxa A, et al. Effect of bariatric surgery on microvascular dysfunction associated to metabolic syndrome: a 12-month prospective study. Int J Obes. 2014;38(11):1410–5. https://doi.org/10.1038/ijo.2014.15.
Vlachopoulos C, Ioakeimidis N, Aznaouridis K, et al. Association of interleukin-18 levels with global arterial function and early structural changes in men without cardiovascular disease. Am J Hypertens. 2010;23(4):351–7. https://doi.org/10.1038/ajh.2009.256.
Li Y, Hanssen H, Cordes M, et al. Aerobic, resistance and combined exercise training on arterial stiffness in normotensive and hypertensive adults: a review. Eur J Sport Sci. 2015;15(5):443–57. https://doi.org/10.1080/17461391.2014.955129.
Hubbard LD, Brothers RJ, King WN, et al. Methods for evaluation of retinal microvascular abnormalities associated with hypertension/sclerosis in the Atherosclerosis Risk in Communities Study. Ophthalmology. 1999;106(12):2269–80.
Quené H, van den Bergh H. On multi-level modeling of data from repeated measures designs: a tutorial. Speech Comm. 2004;43(1–2):103–21. https://doi.org/10.1016/j.specom.2004.02.004.
Lammert A, Hasenberg T, Kräupner C, et al. Improved arteriole-to-venule ratio of retinal vessels resulting from bariatric surgery. Obesity (Silver Spring, Md). 2012;20(11):2262–7. https://doi.org/10.1038/oby.2012.122.
He Y, Li SM, Kang MT, et al. Association between blood pressure and retinal arteriolar and venular diameters in Chinese early adolescent children, and whether the association has gender difference: a cross-sectional study. BMC Ophthalmol. 2018;18(1):133. https://doi.org/10.1186/s12886-018-0799-x.
Boillot A, Zoungas S, Mitchell P, et al. Obesity and the microvasculature: a systematic review and meta-analysis. PLoS One. 2013;8(2):e52708. https://doi.org/10.1371/journal.pone.0052708.
Stapleton PA, James ME, Goodwill AG, et al. Obesity and vascular dysfunction. Pathophysiology. 2008;15(2):79–89. https://doi.org/10.1016/j.pathophys.2008.04.007.
Bachmayer C, Lammert A, Hasenberg T, et al. Healthy obese and post bariatric patients—metabolic and vascular patterns. Exp Clin Endocrinol Diabetes. 2013;121(8):483–7. https://doi.org/10.1055/s-0033-1347248.
Hanssen H, Nickel T, Drexel V, et al. Exercise-induced alterations of retinal vessel diameters and cardiovascular risk reduction in obesity. Atherosclerosis. 2011;216(2):433–9. https://doi.org/10.1016/j.atherosclerosis.2011.02.009.
Samaras K, Viardot A, Lee PN, et al. Reduced arterial stiffness after weight loss in obese type 2 diabetes and impaired glucose tolerance: the role of immune cell activation and insulin resistance. Diab Vasc Dis Res. 2013;10(1):40–8. https://doi.org/10.1177/1479164112443375.
Rider OJ, Tayal U, Francis JM, et al. The effect of obesity and weight loss on aortic pulse wave velocity as assessed by magnetic resonance imaging. Obesity. 2010;18(12):2311–6. https://doi.org/10.1038/oby.2010.64.
Domienik-Karlowicz J, Lisik W, Rymarczyk Z, et al. The short-term effect of bariatric surgery on non-invasive markers of artery function in patients with metabolic syndrome. Diabetol Metab Syndr. 2015;7:76. https://doi.org/10.1186/s13098-015-0076-6.
Yu H, Chen J, Lu J, et al. Decreased visceral fat area correlates with improved arterial stiffness after Roux-en-Y gastric bypass in Chinese obese patients with type 2 diabetes mellitus: a 12-month follow-up. Surg Obes Relat Dis. 2016;12(3):550–5. https://doi.org/10.1016/j.soard.2015.09.003.
Huybrechts SA, Devos DG, Vermeersch SJ, et al. Carotid to femoral pulse wave velocity: a comparison of real travelled aortic path lengths determined by MRI and superficial measurements. J Hypertens. 2011;29(8):1577–82. https://doi.org/10.1097/HJH.0b013e3283487841.
Canepa M, AlGhatrif M, Pestelli G, et al. Impact of central obesity on the estimation of carotid-femoral pulse wave velocity. Am J Hypertens. 2014;27(9):1209–17. https://doi.org/10.1093/ajh/hpu038.
Munakata M. Brachial-ankle pulse wave velocity in the measurement of arterial stiffness: recent evidence and clinical applications. Curr Hypertens Rev. 2014;10(1):49–57.
Yasmin, McEniery CM, Wallace S, et al. Matrix metalloproteinase-9 (MMP-9), MMP-2, and serum elastase activity are associated with systolic hypertension and arterial stiffness. Arterioscler Thromb Vasc Biol. 2005;25(2):372. https://doi.org/10.1161/01.ATV.0000151373.33830.41.
Yiming G, Zhou X, Lv W, et al. Reference values of brachial-ankle pulse wave velocity according to age and blood pressure in a central Asia population. PLoS One. 2017;12(4):e0171737. https://doi.org/10.1371/journal.pone.0171737.
Wang X, Xie J, Zhang LJ, et al. Reference values of brachial-ankle pulse wave velocity for Northern Chinese. Chin Med J. 2009;122(18):2103–6.
Acknowledgments
We would like to thank all study participants and supporting staff wholeheartedly, which facilitated the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Streese, L., Königstein, K., Goricki, L. et al. Short- and Long-Term Effects of Bariatric Surgery on Vascular Phenotype. OBES SURG 29, 1301–1308 (2019). https://doi.org/10.1007/s11695-018-03679-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-018-03679-2