Abstract
Purpose
Obesity is associated with increased cardiovascular risk. Bariatric surgery (BS) improves the clinical and metabolic profile. Retinal caliber changes could precede cardiovascular events. Different studies have shown an improvement in retinal caliber after BS. The aim of this study was to examine retinal caliber and other cardiovascular target organ damage before and after BS.
Materials and Methods
Monocentric, prospective cohort study at the Montpellier University Hospital. Biologic features, vessel stiffness, echocardiograph variables, and retinal caliber at baseline and 6 and 12 months were assessed in consecutive patients with class 2 or 3 obesity undergoing BS. A mixed linear model adjusted for age and sex was used.
Results
We included 88 patients (75 women). The mean (SD) age was 43 years (11) and mean (SD) baseline weight 117 (21) Kg. Mean changes in the first year after BS were − 5.1 µm in central retinal vein equivalent (CRVE) (p < 0.0001), + 0.02 in arteriole-to-venule ratio (AVR) (p < 0.0001), − 1.4 mmol/L in glycemia (p < 0.0001), − 1.0 mg/L in natural logarithm of C-reactive protein (p < 0.0001), and − 54.0 g in left ventricular mass (p = 0.0005). We observed no significant improvement in arterial stiffness markers. Predictors of improvement in CRVE were high baseline weight (p = 0.030), male sex (p = 0.025), and no diabetes history (p Dynamic links between variations
= 0.047).
Conclusion
The retinal microvascular phenotype improved during the first year after bariatric surgery, with decreased CRVE and increased AVR. Factors associated with retinal microvascular plasticity were male sex, high baseline weight, and absence of diabetes. Longitudinal assessment of retinal vascular calibers may offer new insights into the pathophysiology of subclinical vascular processes.
Graphical abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
High body mass index (BMI) is strongly associated with mortality risk, especially cardiovascular (CV) mortality [1]. Various mechanisms can be evoked to explain this increase in CV risk, most being part of the metabolic syndrome: carbohydrate abnormalities, insulin resistance, and arterial hypertension [2].
In the concept of CV disease, the occurrence of preclinical target organ damage (TOD) is the main step in the management because it precedes CV events [3]. Target organs are the heart, arteries and their stiffness, kidneys, brain, and retina. The early detection of TOD could allow for adapting the therapeutic management to prevent a CV event. Bariatric surgery (BS) allows for resolution of the metabolic syndrome, diabetes, and reduces all-cause mortality, particularly that secondary to CV events [4].
Regarding retinal microvascularisation, fundus retinophotographs allow for an accurate and non-invasive analysis. Central retinal arteriolar equivalent (CRAE) narrowing and larger central retinal vein equivalent (CRVE) are associated with increased CV risk [5] and can predict mortality from coronary heart disease and stroke [6]. Larger CRVE is associated with increased BMI [7]. This finding raises the question of the reversibility of microvascular damages in patients with obesity and which patients could benefit the most from BS. Only 6 studies — with modest sample sizes (n < 52) — have investigated retinal caliber after BS (Appendix 1 ). Results are conflicting; a trend in decreased CRVE is frequently found [8,9,10]. CRAE and the arteriovenous ratio (AVR) tend to increase but not always [11,12,13]. These studies did not provide an analysis of factors improvement in the retinal microvascular profile. A study evaluating retinal microvascular changes after BS as well as changes in renal function, metabolic, and macrovascular parameters with a larger sample would better characterize the type of response and determine predictors of microvascular remodeling after BS.
The purpose of our study was to prospectively evaluate the effect of BS on retinal microvascularisation in patients with obesity and investigate the baseline factors predicting these changes.
Methods
Design
The present study is an analysis of the bariatric surgery, arterial stiffness, and target organ damage (BASTOD) study, a prospective longitudinal single-center study with non-invasive evaluation before BS, then at 6 months and 1 year after surgery. Methodological details are provided in Supplementary material Appendix 2.
Setting and Population
This observational study was carried out in a French university hospital. Patients were prospectively included between December 2011 and March 2016. The surgical indication and the operative method (Roux-en-Y gastric bypass, laparoscopic sleeve gastrectomy with or without preservation of the gastric antrum) were validated during a multidisciplinary meeting. All surgical procedures were performed by an experienced bariatric surgeon. Selected patients were then referred for preoperative assessment, and clinical and paraclinical data were collected. Patients included were adults from age 18 to 60 years, with World Health Organization (WHO) class 2 or 3 obesity for more than 5 years, failure of medical treatment, no hormonal causes, and no contraindication to surgery. Patients were excluded if they had uncontrolled hypertension (systolic blood pressure [BP] > 160 mmHg and diastolic [BP] > 100 mmHg), chronic kidney disease (creatinine clearance according to the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) < 60 ml/min/1.73 m2 and/or proteinuria > 300 mg/24 h and/or hematuria on urine test strip), a history of cardiovascular disease or signs of clinical atheroma (stroke, myocardial infarction, and coronary artery disease (angina), obliterative arteritis of the lower limbs (absence of pulse, claudication), aortic aneurysm (abdominal palpation or previous imaging), and carotid murmur).
Ethics
Written informed consent was obtained for each patient in accordance with the 1995 Declaration of Helsinki. The study was approved by the medical ethics committee of the University Hospital of Montpellier and was registered at ClinicalTrials.gov (NCT01494168).
Outcomes and Measurements
Retinophotographs of both eyes were obtained by use of a nonmydriatic camera (CR5-NM45; Canon Inc., Tokyo; and TRC, Topcon Inc., Tokyo), centered on the optical disc. Retinal vascular caliber was measured with Integrative Vessel Analysis (IVAN) software according to a standardized protocol (Fig. 1).
IVAN software, change in vascular caliber post bariatric surgery in subject 87. Retinal vascular caliber is measured in the circle area between 0.5 and 1 disc diameter surrounding the optic disc. Areas highlighted in red indicate retinal arteriolar caliber, and areas in blue indicate retinal venular caliber. CRVE has decreased and AVR has increased between visits 1, 2, and 3. Abbreviations: DD, disc diameter; BMI, body mass index; CRVE, central retinal vein equivalent; CRAE, central retinal arteriolar equivalent; AVR, arteriole-to-venule ratio
Patients were measured (Microbeam 04–116; Stanley Black & Decker, New Britain, CT, USA) and weighed (Model 703; CKSeca, Hamburg, Deutschland), for calculating BMI (weight/height2 in kg/m2). BP and heart rate were measured. Standard blood test was performed and patients submitted a 24-h urine collection.
Echocardiography assessment of left ventricle morphology involved use of an Acuson 128 XP 10 system (Acuson, Mountain View, CA, USA). Pulse wave velocity (PWV) is the velocity of propagation, along an artery, of the pressure wave. It is directly related to the elastic modulus of the arterial wall and represents the most accessible non-invasive technique to assess arterial stiffness. The 2 velocity measures were carotid-femoral PWV and carotid-radial PWV. They were measured with an applanation tonometer (SphygmoCor, AtCor Medical, Australia) after at least 5 min of rest and once BP had stabilized.
Statistical Analysis
Continuous variables are described with mean (standard deviation (SD)) and categorical variables with number (percentage); any missing data are indicated. Linear mixed regressions adjusted for age and sex were performed. P < 0.05 was considered statistically significant and all statistical tests were two-sided. Statistical analyses were performed with R 4.0.3 (Vienna, Austria).
Results
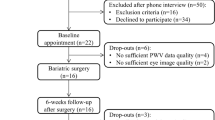
Results at Baseline (Table 1, Fig. 2)
In total, 90 patients were eligible and 88 were enrolled (one lacked consent and one declined surgery); 75 were women. The mean (SD) age was 43 (11) years and mean (SD) baseline weight 117 (21) kg. All patients underwent BS and 73 were followed up until the last visit (Fig. 2). The mean (SD) follow-up was 14.5 (2.5) months. The surgical method was Roux-en-Y gastric bypass in 4 (4%) patients, laparoscopic sleeve gastrectomy with preservation of the gastric antrum in 72 (82%) or without preservation in 12 (14%).
Effect of BS: Linear Mixed Regression (Table 2)
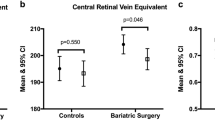
Mean changes during the first year after BS for retinal parameters were − 5.1 µm in CRVE (p = 0.0005) and + 0.02 in AVR (p < 0.0001). CRAE did not significantly increase (p = 0.32).
Mean changes during the first year after BS for clinical variables were − 48.1 kg in weight (p < 0.0001), − 35.4 cm in waist circumference (p < 0.0001), and − 4.0 mmHg in systolic BP (p = 0.04). Diastolic BP did not significantly change (p = 0.70).
Mean changes during the first year after BS for biological variables were − 0.7% in Hba1c level (p < 0.0001), − 4.5 in HOMA-IR (p < 0.0001), − 1.3 µmol/L in creatininemia (p = 0.03), − 1.0 mg/L in ln(CRP) (p < 0.0001), − 0.86 g/L in triglycerides level (p < 0.0001), and + 0.10 g/L in high-density lipoprotein cholesterol (p < 0.0001). Estimated GFR and level of low-density lipoprotein (LDL) cholesterol changed without significance.
Mean changes during the first year after BS in macrovascular variables were − 54.0 g in LVM (p = 0.0005) and − 2.6% in RWT (p = 0.002). Central pulse BP, femoral PWV, and radial PWV did not change significantly.
Baseline Determinants of Change Over Time in Retinal Parameters (Tables 3 and 4)
The slope of CRVE over time was significantly associated with baseline weight (p = 0.030), waist circumference (p = 0.017), and absence of diabetes history (p = 0.047) and that of AVR over time was associated with baseline weight (p = 0.013). For example, a 10-kg higher weight at inclusion was associated with greater decrease in CRVE, 1.3 µm/year. In people with diabetes, the CRVE did not decrease over time; the coefficient of the slope of the CRVE was + 3.54 and − 5.06 µm/year for people with and without diabetes (p = 0.047).
We found no other significant association of potential predictors with the evolution kinetics of the retinal parameters, such as history of high BP (CRVE: p = 0.72; AVR: p = 0.87), sleep apnea syndrome (CRVE: p = 0.50; AVR: p = 0.46), diabetes for AVR (AVR: p = 0.37), and baseline eGFR (CRVE: p = 0.64; AVR: p = 0.60).
To find the relative contribution of factors associated with retinal microvascular changes (i.e., decrease in CRVE or increase in AVR), we performed the 2 multivariate linear mixed regressions presented in Table 3. A greater decrease slope in CRVE after BS was associated with the absence of diabetes history, obesity class 3, and male sex (p < 0.001, p = 0.010, p = 0.025, respectively).
Dynamic links between variations in retinal parameters and other variables were tested after BS (Appendix 2). A decrease in CRVE was correlated with an increase in eGFR (r = − 0.29, p < 0.001) and greater weight loss (r = 0.29, p < 0.001). As well, an increase in AVR was correlated with a greater weight loss (r = − 0.21, p = 0.001). We found no correlation between change in CRP level and change in CRVE (r = 0.016, p = 0.81).
Discussion
In this study of patients with obesity, we found a decrease in venous caliber (CRVE) and an increase in AVR after BS. The factors associated with decreased CRVE were pre-operative absence of diabetes and high body weight. High body weight before surgery was associated with increased AVR. Greater weight loss was associated with a greater increase in AVR and a greater decrease in CRVE. We observed no significant macrovascular changes except for a decrease in LVM and relative wall thickness.
Change in Retinal Caliber After BS
We found a decrease in the mean CRVE after BS (225.8 to 218.1 µm) at a median follow-up of 14.7 months. Some longitudinal studies have shown a significant decrease in CRVE after BS, the mean ranging from 202.9 to 197.3 µm at 6 months in 22 female patients with obesity [10], 220.5 to 214.8 µm at 10.5 months in 30 patients with obesity [9], and 223.8 to 211.9 µm at 10 months in 21 patients with obesity [8]. Our results agree with these northern European studies.
Other studies did not find a decrease in CRVE after BS: Streese et al. [13] did not find a decrease at 6 weeks (16 patients) or at 4 years (13 patients), but this result could be explained by the modest sample size. Brynskov et al. [12] did not find a decrease in 51 diabetic patients with obesity, but this observation agrees with our study because we reported that diabetic status was associated with no decrease in CRVE. The Brynskov et al. results and ours support the hypothesis of reduced retinal microvascular plasticity in people with diabetes.
Our pathophysiologic hypothesis is that the decrease in CRVE after BS could be related to a decrease in CRP level even if we did not find a significant correlation between a decrease in CRVE and a decrease in CRP level, given the small number of patients. Indeed, Daien et al. [14] reported an association between CRP level and venous diameter in older people without obesity (n = 1224). An increase in CRVE in people with obesity is probably related to chronic inflammation after interleukin 6 (IL-6) production by adipokines stimulating CRP production [15]. This hypothesis agrees with the work of Tapp et al. [16] studying 8550 UK participants, finding a positive association between venular diameter and adiposity. In our study, the relatively small number of participants and the dispersal of values did not allow for confirming this hypothesis.
Concerning the predictors of improvement in venous caliber, we found that high pre-BS weight, class 3 (vs class 2) obesity, high waist circumference, and male sex were associated with greater slope of decrease over time in venous caliber. These factors may be predictive of other intermediate outcomes. For example, higher preoperative weight is associated with higher weight reduction and thus greater improvement in some obesity-associated comorbidities, such as dyslipidemia [17]. As for inflammation, a mediation study of the effect of metabolic parameters on the relation between pre-BS obesity class and retinal microvasculature would be of interest with a larger cohort.
The association of male sex with an improvement in venous caliber must be confirmed by other studies given the limited number of men in our study (13/88) and in other studies, obesity affecting mainly women.
We also found an increase from baseline in AVR after BS (0.69 vs 0.72), which is consistent with most studies [9, 10, 13]. Other studies did not find an increase in this ratio probably because of limited number of participants (n = 30 and n = 21) [8, 11].
We did not find an increase in CRAE after BS. This observation could be explained by a lower quality of the arteriolar caliber measurements in our study, with an inter-operator reproducibility of 0.66 (p < 0.001) for CRAE. In fact, the semi-automatic delineation of the arteries is complex because of not much caliber difference in color between the reddish retina and the arteries. This point underlines the reduced feasibility of measuring arteriolar caliber versus venular caliber in current practice.
Change in Biological Variables After BS
We observed an improvement in the lipid profile at 1 year after BS, with an increase in HDL level and a decrease in TG cholesterol level, which agrees with the literature [17]. We did not find a decrease in LDL cholesterol level as in the study of Cunha et al. [18], which had more than twice as many participants (n = 229). Our result can be explained by a reduced number of participants confirmed by the number of needed participants calculated post hoc (n = 421).
The improvement in the glycemic profile we noted is in accordance with the literature. In the meta-analysis of Buchwald et al., diabetes status improved or diabetes resolved in 86.6% of patients [19].
We observed a significant decrease in creatinine level but no significant improvement in renal function (eGFR, albuminuria). In many studies, eGFR increased after BS only in patients with preoperative renal dysfunction (< 90 mL/min) and remained stable when renal function was normal before BS [20]. In our study, only 4 patients had a mean eGFR < 90 mL/min. The apparent discrepancy between a decrease in serum creatinine and no change in eGFR is probably due in part to the decrease in lean mass following bariatric surgery but also to the inaccuracy of serum creatinine-based formula to predict GFR in subjects with obesity [21].
Concomitant Changes in Clinical-Biological Variables and Retinal Caliber
This is the first study to investigate the relation between changes in clinico-biological variables and retinal parameters after BS. Even if eGFR did not change after BS, we observed a correlation between a decrease in CRVE and improvement in renal function. An association between CRVE and renal function had been shown in a cross-sectional observational study [19], but the longitudinal nature of our study suggests that improvement in retinal caliber over time may be associated with improved renal function. Further studies are needed to support this concept.
Change in Macrovascular Variables
Studies have shown conflicting results regarding PWV; it has been reported to be decreased [22], unchanged [13], and even increased [23]. The most recent study published in 2021 [23] showed a paradoxical increase in arterial stiffness at 6 months after BS. In our study, PWV remained unchanged. In conclusion, the results concerning vascular stiffness after BS are discordant and physicians should interpret arterial stiffness measurements with caution.
The reduction in LVM after BS in our study (− 6.1%) is in accordance with Rider et al. [24] and Owan et al. [25] who reported a reduction of 14% and 13.6% respectively.
Strengths
The present study demonstrated decreased CRVE and increased AVR after BS. The use of a linear mixed model allowed us to consider the correlation between repeated measurements and the different evolutionary profile of individuals. This is the largest study evaluating retinal microcirculation after BS, with 88 patients versus 51 in the preceding largest study [12]. We assessed the determinants of retinal microvascular caliber changes after BS. The longitudinal nature of the study allowed us to develop pathophysiologic hypotheses based on these correlations.
Limitations
Our study has some limitations, several results of the linear mixed models are significant, but some covariates measured closely related entities (weight, BMI, and waist circumference) and the magnitude of significant effect remains sometimes limited. The Spearman correlations are statistically significant but all are quite modest. Further studies are needed to confirm these correlations.
In order to keep the trend of the results, we did not decrease the significance level (set at p < 0.05) to account for multiple testing, which may increase the type I error rate. The significant results should therefore be interpreted in this context. In regard to our measurement instrument, we did not perform an analysis of vessel tortuosity, unlike Viljanen et al. [10] who found no change in tortuosity after BS.
We did not use optical coherence tomography angiography (OCTA), which is a very precise, rapid, and automatic measurement instrument for analyzing the retinal capillary network. Agarwal et al. [11] did use OCTA but did not observe any change in the retinal capillary network.
Lastly, the study sample size does not allow a detailed analysis of the physiological mechanism involved in the modifications of retinal microvasculature after BS.
Conclusions
Data for this cohort indicate that the retinal microvascular phenotype improved after BS, with a decrease in CRVE and increase in AVR. Predictors of retinal microvascular improvement were no diabetes history, male sex, and high baseline weight. The determinants and natural history of microvascular remodeling are still poorly understood. Our data suggest retinal vascular caliber offers new insights into the pathophysiology of subclinical vascular processes. Factors predictive of retinal microvascular improvement after BS need to be confirmed in other studies.
References
Calle EE, Thun MJ, Petrelli JM, et al. Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. 1999;341(15):1097–105.
Must A, Spadano J, Coakley EH, et al. The disease burden associated with overweight and obesity. JAMA. 1999;282(16):1523–9.
Safar ME, Struijker-Boudier HAJ. New goals in hypertension management: target-organ protection beyond blood pressure lowering. Drugs. 2003;63 Spec No 1:45–7.
Adams TD, Gress RE, Smith SC, et al. Long-term mortality after gastric bypass surgery. N Engl J Med. 2007;357(8):753–61.
McGeechan K. Meta-analysis: retinal vessel caliber and risk for coronary heart disease. Ann Intern Med. 2009;151(6):404.
Wang JJ, Liew G, Klein R, et al. Retinal vessel diameter and cardiovascular mortality: pooled data analysis from two older populations. Eur Heart J. 2007;28(16):1984–92.
Boillot A, Zoungas S, Mitchell P, et al. Obesity and the microvasculature: a systematic review and meta-analysis. PLOS ONE 2013 févr;8(2):e52708
Bachmayer C, Lammert A, Hasenberg T, et al. Healthy obese and post bariatric patients - metabolic and vascular patterns. Exp Clin Endocrinol Diabetes. 2013;121(8):483–7.
Lammert A, Hasenberg T, Kräupner C, et al. Improved arteriole-to-venule ratio of retinal vessels resulting from bariatric surgery. Obesity. 2012;20(11):2262–7.
Viljanen A, Soinio M, Cheung CY, et al. Effects of bariatric surgery on retinal microvascular architecture in obese patients. Int J Obes. 2019;43(9):1675–80.
Agarwal A, Saini A, Mahajan S, et al. Effect of weight loss on the retinochoroidal structural alterations among patients with exogenous obesity. PLoS ONE. 2020;15(7):e0235926.
Brynskov T, Laugesen CS, Floyd AK, et al. Thickening of inner retinal layers in the parafovea after bariatric surgery in patients with type 2 diabetes. Acta Ophthalmol. 2016;94(7):668–74.
Streese L, Königstein K, Goricki L, et al. Short- and long-term effects of bariatric surgery on vascular phenotype. Obes Surg. 2019;29(4):1301–8.
Daien V, Carriere I, Kawasaki R, et al. Retinal vascular caliber is associated with cardiovascular biomarkers of oxidative stress and inflammation: the POLA study. PLoS ONE. 2013;8(7):e71089.
Illán-Gómez F, Gonzálvez-Ortega M, Orea-Soler I, et al. Obesity and inflammation: change in adiponectin, C-reactive protein, tumour necrosis factor-alpha and interleukin-6 after bariatric surgery. Obes Surg. 2012;22(6):950–5.
Tapp RJ, Owen CG, Barman SA, et al. Retinal vascular tortuosity and diameter associations with adiposity and components of body composition. Obesity (Silver Spring). 2020;28(9):1750–60.
Nienov OH, Machado FD, Dias LS, et al. Effect of bariatric surgery on high-density lipoprotein (HDL) cholesterol in non-diabetic patients with severe obesity. Obes Surg. 2020;30(1):154–60.
Cunha FM, Oliveira J, Preto J, et al. The effect of bariatric surgery type on lipid profile: an age, sex, body mass index and excess weight loss matched study. Obes Surg. 2016;26(5):1041–7.
Buchwald H, Estok R, Fahrbach K, et al. Weight and type 2 diabetes after bariatric surgery: systematic review and meta-analysis. Am J Med. 2009;122(3):248-256.e5.
Seghieri M, Vitolo E, Giannini L, et al. Determinants of glomerular filtration rate following bariatric surgery in individuals with severe, otherwise uncomplicated, obesity: an observational, prospective study. Acta Diabetol. 2017;54(6):593–8.
Fesler P, Mimran A. Estimation of glomerular filtration rate: what are the pitfalls? Curr Hypertens Rep. 2011;13(2):116–21.
Giudici A, Palombo C, Kozakova M, et al. Weight loss after bariatric surgery significantly improves carotid and cardiac function in apparently healthy people with morbid obesity. Obes Surg. 2020;30(10):3776–83.
Wang FM, Yang C, Tanaka H, et al. Increase in arterial stiffness measures after bariatric surgery. Atherosclerosis. 2021;320:19–23.
Rider OJ, Francis JM, Ali MK, et al. Beneficial cardiovascular effects of bariatric surgical and dietary weight loss in obesity. J Am Coll Cardiol. 2009;54(8):718–26.
Owan T, Avelar E, Morley K, et al. Favorable changes in cardiac geometry and function following gastric bypass surgery: 2-year follow-up in the Utah obesity study. J Am Coll Cardiol. 2011;57(6):732–9.
Funding
The university scholarship “année recherche” from Montpellier University. The sponsors or funding organization had no role in the design or conduct of this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
• The retinal microvascular phenotype improved during the first year after bariatric surgery, with decreased central retinal vein equivalent (− 5.1 µm, p < 0.0001), and increased arteriole-to-venule ratio (+ 0.02, p < 0.0001).
• Factors associated with retinal microvascular plasticity were male sex, high baseline weight, and absence of diabetes.
• Longitudinal assessment of retinal vascular calibers may offer new insights into the pathophysiology of subclinical vascular processes.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendices
Appendix
Table 5
Appendix 2
Figure
Rights and permissions
About this article
Cite this article
Debourdeau, E., Gardes, G., Nocca, D. et al. Longitudinal Effect of Bariatric Surgery on Retinal Microcirculation and Target Organ Damage: the BASTOD Study. OBES SURG 32, 1–10 (2022). https://doi.org/10.1007/s11695-022-06064-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11695-022-06064-2