ABSTRACT
BACKGROUND
Little is known about factors contributing to the career decisions of internal medicine residents.
OBJECTIVE
To evaluate factors self-reported by internal medicine residents nationally as important to their career decisions.
DESIGN
Cross-sectional survey conducted in October of 2005, 2006, and 2007 as part of the national Internal Medicine In-Training Examination (IM-ITE).
PARTICIPANTS
Postgraduate year 3 internal medicine residents taking the IM-ITE.
MEASUREMENTS
Residents rated the importance of nine factors in their career decisions on 5-point Likert scales. Univariate statistics characterized the distribution of responses. Associations between variables were evaluated using Cochran-Mantel-Haenszel statistics for ordinal data. Multivariate analyses were conducted using logistic regression.
RESULTS
Of 17,044 eligible residents taking the IM-ITE, 14,890 (87.4%) completed the career decision survey questions. Overall, time with family was the factor most commonly reported as of high or very high importance to career decisions (69.6%). Women were more likely to assign greatest importance to family time (OR 1.22, 95% confidence interval 1.12–1.31, p < 0.001) and long-term patient relationships (OR 1.34, 95% confidence interval 1.23–1.46, p < 0.001). Across debt levels, financial considerations were of greatest importance more often for residents owing >$150,000 (OR 1.33, 95% confidence interval 1.09–1.62, p < 0.001). Across specialties, mentor specialty was rated lowest in importance by residents pursuing hospitalist and general internal medicine careers.
CONCLUSIONS
Greater attention to factors reported by residents as important to their career decisions may assist efforts to optimize the distribution of physicians across disciplines. In addition to lifestyle and practice considerations, these factors may include mentor specialty. As this factor is less commonly reported as important by residents planning careers in generalist fields, attention to effective mentoring may be an important element of efforts to increase interest in these areas.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
Understanding the factors contributing to career decisions in internal medicine is critical in light of increasing concerns regarding distribution of the physician workforce across disciplines. To this end, significant work has focused on factors influencing medical student career decisions. Proposed factors have included future income expectations, debt, and length of training, but the perception of “controllable lifestyle,” educational experiences and role models in medical school, the intellectual content of a specialty, and gender have emerged as key drivers of medical student career choices.1–5
Once medical students have selected internal medicine, little is known about what influences their subsequent career decisions. Educational debt appears to remain important,6 and a single national survey of internal medicine residents in 2002 (prior to Accreditation Council for Graduate Medical Education duty hour regulations) found that future generalists, hospitalists, and subspecialists differed on the importance of income, practice scope, long-term relationships with patients, and time for non-work activities or family.7 Other variables, such as the impact of mentors, the desire to provide what is perceived to be a needed service, job opportunities, or the performance of clinical procedures, were not assessed in this prior research.
To further understand a broader range of factors that may influence decisions to choose subspecialty versus non-subspecialty careers, we examined the self-reported importance of factors in career determination for a large national cohort of internal medicine residents in their third year of training between 2005–7, with duty hour regulations in effect.
METHODS
The Internal Medicine In-Training Exam (IM-ITE) is a standardized 340-item multiple-choice self assessment exam offered yearly to internal medicine residents enrolled in US programs. Demographic data including gender, location of medical school, age, postgraduate year, and career interests are captured, and examinees are also requested to voluntarily complete an accompanying survey at the end of the exam with questions regarding perceptions of the exam, career interests, educational debt, use of study materials, and perceptions of their training environment. One of the item modules in the 2005–2007 surveys pertained to factors involved in career decisions. After reporting their ultimate career plan, postgraduate year 3 residents were asked to rate the importance of eight factors in their career decision from 1= very low to 5= very high on a 5-point Likert scale: broad area of practice, desire to provide a needed service, financial considerations, job opportunities after training, long-term relationships with patients, time available for non-work activities, time with family, and type/number of clinical procedures. In the 2006 and 2007 surveys, an additional question regarding the impact of the principal specialty or subspecialty of a mentor was also included (see online Appendix).
The examination was completed by 17,044 postgraduate year 3 internal medicine residents in October of 2005, 2006, and 2007. This represents 92.2% of the 18,482 postgraduate year 3 internal medicine residents in training during the 2005–2007 academic year (personal communication, George Lonsdorf, American Board of Internal Medicine, October 2008). Of those completing the examination, 15,104 (88.6%) returned surveys, and 14,890 (87.4%) residents in US training programs completed the questions on career decision and factors important to that decision.
We report primarily descriptive results, using standard univariate statistics to characterize the sample. Where appropriate, statistical analyses were conducted using SAS Version 9.1 (SAS Institute Inc, Cary, NC). Two-tailed statistical significance was set at an α level of 0.01, and given the large sample size, we also required group differences of greater than 0.25 on the 1 to 5 integer Likert scale for reporting. Associations between each response category and demographic factors were analyzed using Cochran-Mantel-Haenszel statistics. Multivariate analyses focused on the likelihood of a factor being rated “very high” in importance by each resident were conducted using logistic regression analysis. This analysis was approved by the Institutional Review Board of the Mayo Clinic College of Medicine.
RESULTS
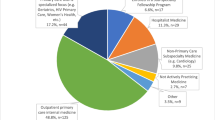
Demographic characteristics of the study participants are shown in Table 1. Of the respondents, 58.6% were male and 46.9% were US medical graduates. Debt patterns differed markedly for US medical graduates and international medical graduates, with 56.7% of the former reporting at least $100,000 of debt and 57.2% of the latter reporting no debt.
Self-reported importance of factors related to career decisions is shown in Tables 2 and 3, for US and international medical graduates, respectively. Of the factors queried, time with family was the factor rated most important overall, with 69.6% of residents rating this of high or very high importance, and only 5.5% rating this of low or very low importance. Financial considerations, procedures, and mentor specialty were rated least important overall, with 36.9%, 42.7%, and 47.2% of residents, respectively, rating each factor of high or very high importance; 18.5%, 23.3%, and 20.3% of residents, respectively, rated each factor of low or very low importance to their career decision.
Average self-reported importance of these factors varied across demographic factors. Average differences between men and women were generally small. International medical graduates rated mentor specialty (3.51 vs. 3.16, p < 0.001) and type/number of procedures (3.41 vs. 3.07, p < 0.001) higher than US medical graduates. No consistent trends were observed by program type or debt status.
The importance of factors in career decisions differed by career plan within internal medicine (Table 4). Those planning geriatrics careers rated the average importance of providing a needed service most highly. Financial considerations were rated least highly by those planning careers in infectious disease, endocrinology, and geriatrics. Long-term relationships with patients were rated most highly by those interested in geriatrics, hematology/oncology, general internal medicine, and rheumatology, and least highly by those interested in hospitalist careers and pulmonary/critical care. The principal specialty of an influential mentor was most important to those interested in nephrology and cardiology, and least important to those interested in hospitalist careers and general internal medicine. Time for non-work activities and with family was most important to those interested in rheumatology and endocrinology, and least important to those interested in cardiology and pulmonary/critical care. Type and number of procedures were rated most highly by those interested in gastroenterology, pulmonary/critical care, and cardiology, and least highly by those interested in infectious disease, geriatrics, endocrinology, hematology/oncology, and general internal medicine.
Multivariate models focused not on average ratings but on factors rated as most important by each resident and including gender, medical school location, program type, debt, and career plan showed additional differences. Only statistically significant associations are reported here. Desire to provide a needed service (OR 1.25, 95% confidence interval 1.14–1.36, p < 0.001), long-term patient relationships with patients (OR 1.34, 95% confidence interval 1.23–1.46, p < 0.001), mentor specialty (OR 1.20, 95% confidence interval 1.06–1.35, p = 0.003), time for non-work activities (OR 1.23, 95% confidence interval 1.13–1.34, p < 0.001), and time with family (OR 1.22, 95% confidence interval 1.12–1.31, p < 0.001) were more important and financial considerations (OR 0.76, 95% confidence interval 0.65–0.88, p < 0.001) were less important to women residents. All factors except time for non-work activities were more likely to be rated as most important to international medical graduates (all p < 0.001, OR and 95% confidence interval for broad area of practice: 1.60 (1.41–1.80); desire to provide a needed service: 1.38 (1.25–1.53); financial considerations: 1.78 (1.52–2.10); job opportunities after training: 1.83 (1.64–2.04); long-term relationships with patients: 1.40 (1.27–1.55); mentor specialty: 1.76 (1.53–2.02); time with family: 1.32 (1.21–1.45); type and number of procedures: 1.74 (1.54–1.97). Long-term patient relationships (OR 1.28, 95% confidence interval 1.11–1.47, p < 0.001) were more important for primary care program residents. Across debt levels, financial considerations were only more likely to be rated as a most important factor for the highest-debt group, owing >$150,000 (OR 1.33 relative to no-debt group, 95% confidence interval 1.09–1.62, p < 0.001). Differences by career plan were similar in these models to the previously reported results.
DISCUSSION
This study presents a national cohort of graduating internal medicine residents reporting on reasons for career decisions. Overall, time with family was the most highly rated factor in career choice, while financial considerations, procedures, and mentor specialty were the least important reported factors in this study. We did not observe meaningful differences in average importance ratings of the evaluated factors between men and women, residents in categorical or primary care programs, or debt levels in reported factors affecting career decisions. However, we did find differences in reporting of which factors were rated as most highly important. Women were more likely to assign the greatest importance to family time and long-term patient relationships and less likely to focus on financial considerations. Long-term relationships with patients were also most important to primary care program residents. Financial considerations were of greatest importance only in residents with the most debt (>$150,000).
International medical graduates were more likely than US graduates to report multiple factors as very highly important, even after adjustment for career decision. This observation differs markedly from results reported previously.7 Our data do not suggest a reason for these differences.
Although we are unaware of previous research evaluating the role of type/number of procedures on career decisions, it is not surprising that residents planning careers in procedural specialties such as cardiology and gastroenterology should consider this factor highly important in their career planning. This may reflect one specific element of the broader concepts of intellectual attraction to and passion for a discipline’s content material.
Another unique finding is that residents planning careers in hospital medicine or general internal medicine were the least likely to rate the specialty of a mentor as highly important to their career decision. This may emphasize the need for effective mentorship from within these disciplines in aligning residents with career plans best suiting their goals and expectations, as has been suggested by others.5, 8–10
This study has several limitations. First, this report is based on resident self-report of factors important to each individual resident in his or her career decision. Second, the list of factors included on this survey was not exhaustive, and many other factors impact career decisions as described earlier in this paper. For example, a resident’s intellectual attraction to and passion for a discipline’s content material have not been assessed in this or previous studies of internal medicine residents, although these have been shown to be important to medical students in their career decisions. Therefore, the factors identified in this paper should be considered complementary to those identified in previous research, and no conclusions concerning the relative importance of these factors across studies should be drawn. Third, this study reports results for postgraduate year 3 residents only. Many career decisions are made prior to this year of training,11 and it is possible that reasons for career plans could differ among residents earlier in training. Fourth, as this study suggests that international medical graduates may rate factors in their career decisions differently than do US medical graduates, it will be important to better understand the contributors to career decisions made by international medical graduates as this group comprises an increasing proportion of internal medicine trainees. Finally, despite the high overall survey response rate, some individual item responses were categorized as missing. It is possible that response bias could result from these missing data, although nonresponders appeared generally similar to responders on measurable demographic variables such as gender.
In summary, our study describes the relative importance of factors reported by internal medicine residents to impact their decisions regarding subsequent career choice. Greater attention to these factors during training and within the subsequent work environment may influence resident career decisions and the mix of internists across disciplines.
References
Kassebaum DG, Szenas PL. Relationship between indebtedness and the specialty choices of graduating medical students. Acad Med. 1992;67:700–7.
Kassebaum DG, Szenas PL. Factors influencing the specialty choices of 1993 medical school graduates. Acad Med. 1994;69:164–70.
Dorsey ER, Jarjoura D, Rutecki GW. Influence of controllable lifestyle on recent trends in specialty choice by US medical students. JAMA. 2003;290:1173–8.
Dorsey ER, Jarjoura D, Rutecki GW. The influence of contrallable lifestyle and sex on the specialty choices of graduating US medical students, 1996–2003. Acad Med. 2005;80:791–6.
Hauer KE, Durning SJ, Kernan WN, et al. Factors associated with medical students’ career choices regarding internal medicine. JAMA. 2008;300:1154–64.
McDonald FS, West CP, Popkave C, Kolars JC. Educational debt and reported career plans among internal medicine residents. Ann Intern Med. 2008;149:416–20.
Garibaldi RA, Popkave C, Bylsma W. Career plans for trainees in internal medicine residency programs. Acad Med. 2005;80:507–12.
Griffith CH III, Georgesen JC, Wilson JF. Specialty choices of students who actually have choices: the influence of excellent clinical teachers. Acad Med. 2000;75:278–82.
Levy BD, Katz JT, Wolf MA, Sillman JS, Handin RI, Dzau VJ. An initiative in mentoring to promote residents’ and faculty members’ careers. Acad Med. 2004;79:845–50.
Ramanan RA, Taylor WC, Davis RB, Phillips RS. Mentoring matters: mentoring and career preparation in internal medicine residency training. J Gen Intern Med. 2006;21:340–5.
West CP, Popkave C, Schultz HJ, Weinberger SE, Kolars JC. Changes in career decisions of internal medicine residents during training. Ann Intern Med. 2006;145:774–9.
Acknowledgments
The authors wish to acknowledge the assistance of George Lonsdorf with the American Board of Internal Medicine in providing data on the number of internal medicine residents in training in 2005–7.
Funding source
None.
Conflicts of Interest
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Additional information
Research sponsors/prior presentations: None.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 119 kb)
Rights and permissions
About this article
Cite this article
West, C.P., Drefahl, M.M., Popkave, C. et al. Internal Medicine Resident Self-report of Factors Associated with Career Decisions. J GEN INTERN MED 24, 946–949 (2009). https://doi.org/10.1007/s11606-009-1039-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-009-1039-0