Abstract
Background
Laparoscopic surgery is regarded as the gold standard for the surgical management of cholelithiasis. To improve post-operative pain, low-pressure laparoscopic cholecystectomies (LPLC) have been trialed. A recent systematic review found that LPLC reduced pain; however, many of the randomised control trials were at a high risk of bias and the overall quality of evidence was low.
Methods
One hundred patients undergoing elective laparoscopic cholecystectomy were randomised to a LPLC (8 mmHg) or a standard pressure laparoscopic cholecystectomy (12 mmHg) (SPLC) with surgeons and anaesthetists blinded to the pressure. Pressures were increased if vision was compromised. Primary outcomes were post-operative pain and analgesia requirements at 4–6 h and 24 h.
Results
Intra-operative visibility was significantly reduced in LPLC (p<0.01) resulting in a higher number of operations requiring the pressure to be increased (29% vs 8%, p=0.010); however, there were no differences in length of operation or post-operative outcomes. Pain scores were comparable at all time points across all pressures; however, recovery room fentanyl requirement was more than four times higher when comparing 8 to 12 mmHg (12.5mcg vs 60mcg, p=0.047). Nausea and vomiting was also higher when comparing these pressures (0/36 vs 7/60, p=0.033). Interestingly, when surgeons estimated the operating pressure, they were correct in only 69% of cases.
Conclusion
Although pain scores were similar, there was a significant reduction in fentanyl requirement and nausea/vomiting in LPLC. Although LPLC compromised intra-operative visibility requiring increased pressure in some cases, there was no difference in complications, suggesting LPLC is safe and beneficial to attempt in all patients.
Trial Registration
Registered with the Australia and New Zealand Clinical Trials Registry (ACTRN12619000205134).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Post-operative pain following laparoscopic cholecystectomy (LC) remains the major issue that prevents early discharge of patients, with most patients still staying overnight 1,2. Post-operative pain following LC may be visceral or parietal, with a major source of pain also being that of shoulder tip pain which is attributed to the stretching of the diaphragm with the carbon dioxide insufflation 3. Traditionally, an intra-abdominal pressure of 12 to 15 mmHg is considered satisfactory for the visualisation of the anatomy and manipulation of surgical equipment 4. It has been shown to be feasible to perform LC with no difference in morbidity or mortality at lower intra-abdominal pressures (7–10 mmHg) with potential benefits in organ function 5,6. This suggests that low-pressure LC (LPLC) may be a method to reduce post-operative pain attributable to barotrauma, as well as having implications for performing LC in high-risk patients 5,7,8.
There is some evidence that LPLC is associated with decreased pain; however, these results are still open to debate as many of the clinical trials detailing the benefits were found to be at a high risk of bias and inadequate blinding 9. There is also controversy regarding the role of higher pressure in the causation of shoulder tip pain, with the common theory being that the causative factors are distention and irritation by carbon dioxide; however, many studies show no significant difference in shoulder tip pain in LPLC 10,11,12. Clarification that LPLC can lead to an improvement in post-operative pain may lead to more day case LC with an increase in bed availability as well as patient satisfaction 6.
To test the hypothesis that LPLC reduces post-operative pain, as measured by both post-operative pain scores and analgesia requirement, we performed a double-blinded randomised controlled trial with blinded trial investigators to minimise bias.
Materials and Methods
This study was conducted at Northern Health, Melbourne, Australia from February 2019 to October 2019. Ethical approval was sought from an independent review board (IRB) and was granted by the Austin High Risk Ethics Committee (HREC/45804/Austin-2018). The study was registered with the Australia and New Zealand Clinical Trials Registry (ACTRN12619000205134). This study was conducted and reported according to CONSORT guidelines for randomised trials.
Study Population
All patients who were booked for an elective laparoscopic cholecystectomy at Northern Health during the study period were assessed for the study and once consented were randomised to have their laparoscopic cholecystectomy performed at either low pressure (8 mmHg) or standard pressure (12 mmHg) in a 1:1 ratio. Exclusion criteria included patients who underwent emergency laparoscopic cholecystectomy, a secondary operation (hernia repair, endoscopic retrograde cholangiopancreatography or common bile duct exploration), were under 18 years of age, had chronic pain syndrome, regular consumption of opiate medication, were allergic to opiate medications or unable to communicate in English for the purposes of consent and post-operative pain scores. Written consent was performed by a trained investigator and documentation was maintained according to ethical and institution regulations.
The sample size was calculated by a continuous endpoint; two independent sample study power calculations were performed. Assuming that the pain scores are 10% higher with standard intra-abdominal pressure laparoscopic cholecystectomy with a standard deviation of 15% of the measurements, and assuming a type I error of 0.05 and a type II error of 0.2, power calculations reveal that 86 participants (43 in each group) will give a significant result. Allowing for participant dropout, 100 patients were recruited.
Randomisation, Allocation Concealment and Blinding
Randomisation was achieved by an electronic random number generator (www.randomizer.org), with randomised pressure settings placed into consecutively numbered envelopes by an independent investigator who was not involved in data collection. At operation, theatre technicians, who were trained in the study protocols but independent of the data collection and analysis, opened the consecutively numbered envelope and set the machine to the allocated pressure setting. The pressure settings on the laparoscopic towers were covered with black card to ensure surgeons could not read the pressure settings.
Surgical Intervention
After infiltration with local anaesthetic (20 ml 0.75% ropivocaine or 0.5% bupivacaine with adrenaline), pneumoperitoneum was achieved by an open technique using a Hassan Port. Intra-abdominal pressure was determined and delivered as described above. Insufflation was initiated with room temperature carbon dioxide with low flow (3 L/min) before proceeding to high flow (20 L/min). LC was performed using the standard 4-port ‘American’ technique with routine intra-operative cholangiogram. If at any time throughout the operation the surgeon felt that the intra-abdominal pressure was inadequate for safety reasons, they could request for an increase in pressure. The laparoscopic pressure settings were increased from 8 to 12 mmHg, or from 12 to 15 mmHg depending on the starting pressure, according to the protocol (Supplementary Fig. 1). This process was also performed by the trained theatre technicians. At the conclusion of the intra-abdominal operation, the liver bed was irrigated and suctioned thoroughly and all gas evacuated.
Anaesthetic Intervention
All patients were nil by mouth for 6 h prior to their admission. Oral paracetamol was administered by the peri-operative nurses prior to general anaesthesia. Anaesthesia was induced with fentanyl and propofol, and maintained with sevoflurane in O2. Neuromuscular blockade was achieved by non-depolarising muscle relaxants (rocuronium, atracurium or vercuronium) and monitored with GE M-NMT kinemyography monitoring at the adductor pollicis muscle with Train of Four (TOF) analysis. A TOF ratio of 1 twitch or less was monitored and targeted by anaesthetists to ensure a consistent neuromuscular blockade across both groups. Intraoperative analgesia was achieved with 8 mg of dexamethasone, 40 mg of parecoxib, and boluses of fentanyl, titrated as required. Depth of anaesthesia was monitored by GE entropy and titrated to an entropy reading between 40 and 60 to ensure consistency between patients. At the end of the surgery, neuromuscular blockade was reversed with neostigmine and glycopyrrolate. Post-operative recovery included regular paracetamol, ibuprofen and intravenous fentanyl was given by recovery room nurses according to institutional policies and titrated to effect. Post-operative nausea and vomiting prevention treatment was not protocolised for this study; however, intra-operative dexamethasone and post-operative ondansetron were commonly used for this purpose. Post-operative and discharge analgesia comprised of oral analgesics; paracetamol 1 g, ibuprofen 400 mg and oxycodone 5 mg as required.
Data Collection
Baseline characteristics, American Society of Anaesthesiologists (ASA) grade, operative time, intra-operative data including requirement for pressure change, hyper- or hypotension during laparoscopy (as defined by greater or lesser than 20% from baseline) or a bradycardic event (< 40 beats per minute) were recorded. Medical records were interrogated for type and quantities of anaesthetic agents and analgesia used, and post-operative complications within 30 days. Post-operative pain scores were obtained on a Likert scale from 0 (no pain) to 10 (worse pain ever felt) at 4–6 h and 24 h by a trained investigator who was blinded to the operative laparoscopic pressure. Nausea or vomiting, as reported by the patient, at 4–6 h was also recorded. Primary outcomes of pain scores at 4–6 h were obtained with a face-to-face consultation, and secondary outcomes of 24-h pain scores were obtained over the telephone regardless of whether the patient was still admitted or discharged. Patients were called three times over the space of a 4-h period. If the patient did not answer after the third attempt, then a 24-h pain score was not recorded. Surgeon operative visibility was assessed at the end of the operation on a Likert scale of 1 (terrible view) to 5 (excellent view). Additionally, surgeons were asked to state which pressure they thought they were initially operating at. Study codes were only matched with randomisation data once all data for all patients was collected.
Statistical Analysis
Descriptive statistics were prepared to compare the patient and clinical characteristics between the two randomised groups. Subset analysis was performed with groups determined by lower post-operative scores between both groups, with secondary measures of analgesia requirement. For categorical variables, chi-squared tests or Fishers Exact tests were used to compare groups, whilst for continuous variables, Students t tests or Analysis of Variance (ANOVA) and/or Mann-Whitney (ranksum) or Kruskal-Wallis tests were applied, depending on the distribution and number of groups being compared. Data was collated in Microsoft Excel, before importing to Stata version 15.1 (StataCorp, College Station, TX, USA) for statistical analysis, with a p value of less than 0.05 indicating statistical significance.
Results
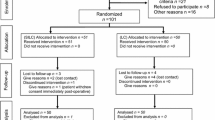
A total of 148 patients that underwent elective LC during the study period were assessed for inclusion into the study. After exclusions, 100 patients were randomised with 51 patients allocated to LPLC and 49 to a SPLC as shown in Fig. 1. Baseline characteristics including age, gender and BMI were not significantly different between both groups (Table 1). Similarly, there were no differences in the anaesthetic and operative characteristics including primary surgeon, type of local anaesthetic agent, muscle relaxant and use of non-opioid analgesia. There was a higher number of ASA grade 1 patients in the standard pressure group, and higher number of ASA grade 2 patients in the low-pressure group (p=0.025).
The satisfaction with the view by surgeons was significantly worse with low pressure with only 22% of surgeons operating at 8 mmHg rating the intra-abdominal view as excellent when compared to 65% in the standard pressure group (p<0.001) (Table 2.) Significantly, more patients in the LPLC group required a pressure increase to a higher pressure than in the SPLC group (29% vs 8%, p=0.010) (Table 2). Interestingly, whilst surgeons more often estimated the pressure setting correctly, the number of times the pressure was guessed incorrectly was 31%.
Outcome data analysis was calculated within eventual pressure groups in an attempt to demonstrate pressure-related outcomes as opposed to intention-to-treat outcomes as this has far greater clinical implications. Thus, 36 patients operated on at 8 mmHg, 60 patients operated on at 12 mmHg and 4 patients operated on at 15 mmHg were analysed (Fig. 1).
In terms of safety, operative times were comparable across both groups, with a median duration of 68 min (Inter-quartile range (IQR): 49 to 83) in LPLC group compared to 62 min (IQR: 48 to 77) in the SPLC group (p=0.48). Post-operative complications in the LPLC group consisted of two wound infections, one post-operative deep vein thrombosis and one bile leak that required laparoscopy and re-clipping of the cystic duct. Post-operative complications in the SPLC group consisted of four wound infections and one bile leak that was managed conservatively.
Median overall pain scores and shoulder tip pain scores at 4 h and 24 h did not differ significantly between 8, 12 and 15 mmHg (Table 3). Frequency of shoulder tip pain at 4–6 h and 24 h was observed to be higher in those patients operated on at 8 mmHg when compared to those operated on at 12 mmHg; however, this did not reach statistical significance.
The operating time in the three groups was not significantly different with a median time of 62.5 (IQR: 47, 77) min in the 8 mmHg group, 67 (IQR: 49, 78.5) min in the 12 mmHg group and 76.5 (IQR: 55.5, 104) min in the 15 mmHg group (p=0.56) (Table 4). There was no difference in bradycardic or blood pressure events, or post-operative complications between groups. Nausea or vomiting was noted in 7 patients (13%) in the 12 mmHg group with none in the 8 mmHg or 15 mmHg groups, with the comparison between 8 and 12 mmHg reaching significance (p=0.033).
There was no difference in the dose of intra-operative fentanyl given between groups (Table 4). However, there was a significant difference in post-operative recovery fentanyl requirement between patients operated on at 8 mmHg and 12 mmHg (12.5mcg vs 60mcg, p=0.047). Total inpatient oxycodone use was not significantly different between groups.
Discussion
This study has been designed to answer the question as to whether reduced intra-abdominal pressure reduces post-operative pain with minimal bias. With a significant reduction in post-operative fentanyl noted, but no difference in pain scores, the result of this study is that LPLC does indeed reduce pain, but only by a small degree that is easily compensated for by an increase in recovery room opiates. The significant increase in nausea and vomiting may be associated with this increased fentanyl use, with these symptoms potentially reducing the ability to discharge patients on the same day. Thus, whilst the observed differences may be small, the consequences may still have clinical and economic impact.
The study’s findings concur with several studies which demonstrate modest reduction in pain scores or analgesic requirements 13,14,15. According to the most recent Cochrane review of this topic, however, only one study was performed with low risk of bias 6,8,16. Interestingly, this study demonstrated no difference in pain scores or analgesia requirement between low pressure (8 mmHg) and high pressure (14 mmHg) groups. Although rated as lowest risk of bias by the Cochrane review, it appears that surgeons were still aware of the pressure at which they were operating 16. In addition to blinding the operating surgeons and anaesthetists in this study, we have also performed this study with a standardised anaesthetic approach to ensure that there is minimal bias from different levels of relaxation. Whilst there are many studies that contradict our findings and demonstrate no difference in pain scores or analgesia requirements, these studies are not free from bias 10,11,17.
Shoulder tip pain is a not infrequent consequence of all laparoscopic surgery, including LC as well as laparoscopic appendicectomy, laparoscopic gynaecological surgery and more major oncological resections 18,19. The most commonly accepted theory of parietal pain following laparoscopic surgery is that of barotrauma with pressure on the diaphragm and peritoneum causes tearing of peritoneal muscle and tissue, the release of inflammatory mediators and traction on nerves 20. Residual pneumoperitoneum and peritoneal carbonic acid production have also been linked to shoulder tip pain 21. We did not show any significant difference in shoulder tip pain between groups, suggesting either that there is minimal clinical difference in barotrauma of parietal tissues when comparing 8 to 12 mmHg, or that the operating time of a LC is insufficient to demonstrate a clinical difference. Interestingly, we observed a higher, though insignificant, frequency of patients in the 8 mmHg group report shoulder tip pain at 4–6 h. It is possible that barotrauma is not responsible for shoulder tip pain, and may be due to another mechanism such as retained blood and bile that is more difficult to irrigate and suction at lower pressure with less space around the liver. This may also explain why other causes of abdominal distension such as acute large bowel obstruction and ascites often present without significant pain or shoulder tip pain. Our findings suggest the cause of shoulder tip pain is far from established and that further studies are required.
The major argument against LPLC is that of safety with a frequent complaint that low pressure leads to poor views and thus unsafe dissection 22. Poor view is associated with low pressure, and our study has shown this with 44% of LPLC operations rated at 3/5 or less, compared with 16% in the SPLC group. Whilst some poorer view simply makes the surgeon’s job more tedious, there is a cohort of these patients where surgeons would deem the operation to confer more risk to the patient. Our study confirms that this is an issue for a moderate number of patients, with 29% of patients in the LPLC group requiring a protocol driven increase in pressure to 12 mmHg. No patient required a further increase in pressure, although 4 patients in the SPLC group also required a pressure increase. However, there was no difference in morbidity and none of the complications noted in the LPLC groups appears directly linked to a pressure-related technical issue. When compared with other studies with observed ‘conversion to standard pressure’ rates between 2.3 and 15%, our results appear much higher 4,10,12,16. Assuming our rigorous anaesthetic protocol allowed for adequate relaxation, it is unclear whether our increased rate of conversion reflects a patient cohort that has poor abdominal wall compliance, or a surgeon cohort that is not prepared to work with a less than perfect view. Whilst complication rates have been reported in the range of 5.4 to 35% 11,13,14,18 in LPLC, to our knowledge, no study has reported an increase in morbidity with low-pressure LC compared with standard pressure. Our complication rate is low in comparison to this literature, possibly justifying a meticulous requirement for optimal vision. Thus, it appears that LPLC is safe to perform and therefore justifiable to commence the operation under low pressure given the ability to increase pressure easily if vision is considered suboptimal.
Post-operative nausea and vomiting is a common side effect of general anaesthesia and the exact mechanism of this side effect is unknown. Although laparoscopic surgery has generally improved patient outcomes when compared with open surgery, there is a higher incidence of post-operative nausea and vomiting associated with this procedure 23,24. The use of low intra-abdominal pressure on post-operative nausea and vomiting has not been adequately studied in the literature. The results of this study demonstrated a significant reduction in post-operative nausea and vomiting when operating with lower intra-abdominal pressures; however, this difference may be attributed to the difference in post-operative fentanyl requirement, and further studies would be required to ascertain the true nature of the relationship between low intra-abdominal pressure and nausea/vomiting.
It is human nature that blinded surgeons would guess and assume they are operating at a certain pressure, and potentially behave in a way that could influence the study. There are also subtle signs that an experienced surgeon could use, such as time taken to re-expand following gas release, or degree of anterior abdominal wall distention that may indicate the correct pressure. Thus, it was interesting that surgeons were correct in only 69% of cases when asked their opinion, less than 20% above the pure guess of 50%. The other main limitation of the study is the sample size, with the potential for type II errors given that the study was powered to detect a 10% difference in pain scores. Further multi-centre studies with a larger study population could confirm this study’s findings more definitively.
Conclusions
Whilst there was no difference in pain scores, the results of this study demonstrate a marked reduction of recovery room opiate analgesia requirement with low pressure (8 mmHg) laparoscopic cholecystectomy when compared with a normal pressure of 12 mmHg. This suggests that lower pressure does reduce pain, but to a level that is compensated for by opiate analgesia. An increase in nausea and vomiting may be associated with the increased opiate requirement and could potentially increase costs with delayed discharge. Intra-abdominal visibility was compromised in some patients that underwent LPLC; however, operative times and complications rate were comparable across the two groups and with the ease of being able to simply increase the pressure when needed; this should not prevent low-pressure laparoscopic cholecystectomy from being attempted in all patients to access the potential benefits.
References
Ahn Y, Woods J, Connor S (2011) A systematic review of interventions to facilitate ambulatory laparoscopic cholecystectomy. HPB 13:677-686
Watters D (2016) Clinical Variation: Procedure in profile: Laparoscopic Cholecystectomy. Surgical News 17:38 [available from: https://umbraco.surgeons.org/media/1415/art-2016-1404-1401-surgical-news-april-for-web.pdf. Accessed 16th of November 2020]
Yasir M, Mehta KS, Banday VH, Aiman A, Masood I, Iqbal B (2012) Evaluation of post operative shoulder tip pain in low pressure versus standard pressure pneumoperitoneum during laparoscopic cholecystectomy. Surgeon 10:71-74
Bhattacharjee HK, Jalaludeen A, Bansal V, Krishna A, Kumar S, Subramanium R, Ramachandran R, Misra M (2017) Impact of standard-pressure and low-pressure pneumoperitoneum on shoulder pain following laparoscopic cholecystectomy: a randomised controlled trial. Surg Endosc 31:1287-1295
Cheng Z-J, Wang Y-B, Chen L, Gong J-P, Zhang W (2018) Effects of Different Levels of Intra-Abdominal Pressure on the Postoperative Hepatic Function of Patients Undergoing Laparoscopic Cholecystectomy: A Systematic Review and Meta-Analysis. Surg Laparosc Endosc Percutan Tech 28:275-281
Hua J, Gong J, Yao L, Zhou B, Song Z (2014) Low-pressure versus standard-pressure pneumoperitoneum for laparoscopic cholecystectomy: a systematic review and meta-analysis. Am J Surg 208:143-150
Wallace DH, Serpell MG, Baxter JN, O'Dwyer PJ (1997) Randomized trial of different insufflation pressures for laparoscopic cholecystectomy. Br J Surg 84:455-458
Özdemir-van Brunschot DMD, van Laarhoven KCJHM, Scheffer G-J, Pouwels S, Wever KE, Warlé MC (2016) What is the evidence for the use of low-pressure pneumoperitoneum? A systematic review. Surg Endosc 30:2049-2065
Gurusamy KS, Vaughan J, Davidson BR (2014) Low pressure versus standard pressure pneumoperitoneum in laparoscopic cholecystectomy. Cochrane Database Syst Rev CD006930
Chok KS, Yuen WK, Lau H, Fan ST (2006) Prospective randomized trial on low-pressure versus standard-pressure pneumoperitoneum in outpatient laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech 16:383-386
Perrakis E, Vezakis A, Velimezis G, Savanis G, Deverakis S, Antoniades J, Sagkana E (2003) Randomized comparison between different insufflation pressures for laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech 13:245-249
Kanwer DB, Kaman L, Nedounsejiane M, Medhi B, Verma GR, Bala I (2009) Comparative study of low pressure versus standard pressure pneumoperitoneum in laparoscopic cholecystectomy--a randomised controlled trial. Trop Gastroenterol 30:171-174
Joshipura VP, Haribhakti SP, Patel NR, Naik RP, Soni HN, Patel B, Bhavsar MS, Narwaria MB, Thakker R (2009) A prospective randomized, controlled study comparing low pressure versus high pressure pneumoperitoneum during laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech 19:234-240
Barczynski M, Herman RM (2003) A prospective randomized trial on comparison of low-pressure (LP) and standard-pressure (SP) pneumoperitoneum for laparoscopic cholecystectomy. Surg Endosc 17:533-538
Singla S, Mittal G, Raghav, Mittal RK (2014) Pain management after laparoscopic cholecystectomy-a randomized prospective trial of low pressure and standard pressure pneumoperitoneum. J Clin Diagn Res 8:92-94
Sandhu T, Yamada S, Ariyakachon V, Chakrabandhu T, Chongruksut W, Ko-iam W (2009) Low-pressure pneumoperitoneum versus standard pneumoperitoneum in laparoscopic cholecystectomy, a prospective randomized clinical trial. Surg Endosc 23:1044-1047
Koc M, Ertan T, Tez M, Kocpinar MA, Kilic M, Gocmen E, Aslar AK (2005) Randomized, prospective comparison of postoperative pain in low- versus high-pressure pneumoperitoneum. ANZ J Surg 75:693-696
Sarli L, Costi R, Sansebastiano G, Trivelli M, Roncoroni L (2000) Prospective randomized trial of low-pressure pneumoperitoneum for reduction of shoulder-tip pain following laparoscopy. Br J Surg 87:1161-1165
Bogani G, Uccella S, Cromi A, Serati M, Casarin J, Pinelli C, Ghezzi F (2014) Low vs Standard Pneumoperitoneum Pressure During Laparoscopic Hysterectomy: Prospective Randomized Trial. J Minim Invasive Gynecol 466
Donatsky AM, Bjerrum F, Gogenur I (2013) Surgical techniques to minimize shoulder pain after laparoscopic cholecystectomy. A systematic review. Surg Endosc 27:2275-2282
Lee JS, Kim EY, Lee SH, Han JH, Park SK, Na GH, You YK, Kim DG, Hong TH (2014) A simple method of reducing residual intraperitoneal carbon dioxide after laparoscopic cholecystectomy: a prospective, randomized, controlled study. J Laparoendosc Adv Surg Tech A 24:563-566
Vijayaraghavan N, Sistla SC, Kundra P, Ananthanarayan PH, Karthikeyan VS, Ali SM, Sasi SP, Vikram K (2014) Comparison of standard-pressure and low-pressure pneumoperitoneum in laparoscopic cholecystectomy: a double blinded randomized controlled study. Surg Laparosc Endosc Percutan Tech 24:127-133
Son J-S, Oh J-Y, Ko S (2017) Effects of hypercapnia on postoperative nausea and vomiting after laparoscopic surgery: a double-blind randomized controlled study. Surg Endosc 31:4576-4582
Nasajiyan N, Javaherfourosh F, Ghomeishi A, Akhondzadeh R, Pazyar F, Hamoonpou N (2014) Comparison of low and standard pressure gas injection at abdominal cavity on postoperative nausea and vomiting in laparoscopic cholecystectomy. Pak J Med Sci 30:1083-1087
Funding
This research was awarded a small research grant of AUD$5000 from the Northern Health Foundation which covered ethics applications and stationary.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary Fig. 1
Intraoperative pressure protocol (PNG 176 kb)
Rights and permissions
About this article
Cite this article
Gin, E., Lowen, D., Tacey, M. et al. Reduced Laparoscopic Intra-abdominal Pressure During Laparoscopic Cholecystectomy and Its Effect on Post-operative Pain: a Double-Blinded Randomised Control Trial. J Gastrointest Surg 25, 2806–2813 (2021). https://doi.org/10.1007/s11605-021-04919-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-021-04919-0