Abstract
Introduction
Single-incision approaches to laparoscopic cholecystectomy typically involve increasing the size of the umbilical incision and eliminating three smaller incisions, but it is not intuitive that patients would view this as a benefit. We hypothesize that when patient satisfaction with standard laparoscopic cholecystectomy is assessed, most dissatisfaction will be linked to the umbilical incision and, given the option, patients would actually wish to eliminate this incision.
Methods
Two hundred eighty-one female patients aged 18 to 40 years who underwent laparoscopic cholecystectomy over a 2-year period were identified, and data were collected on 125 patients.
Results
Fewer than half of patients correctly remembered the number of incisions they had, with 57 patients (45.6%) recalling fewer incisions than were present. Of 58 patients reporting one site to be more painful, 38 (65.5%) cited the umbilical site as the most painful. Eighty-one patients (68.6%) would have preferred to eliminate an incision, with 51 of these (63.0%) choosing to eliminate the umbilical incision.
Conclusion
As single-incision cholecystectomy enlarges what is already a painful and undesirable incision, and since patients often do not recall the smaller incisions, we should ask ourselves whether surgeons and industry care more about this technique than do the patients to whom we offer it.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The current standard approach to laparoscopic cholecystectomy involves a 10-mm incision at the umbilicus, a 5 or 10-mm incision in the epigastric or subxiphoid region, and two 5-mm incisions in the right upper quadrant. Recent technology and operative techniques have allowed for surgical procedures to be performed with fewer incisions. This has progressed to the procedure being performed through a single skin incision at the umbilicus.
In the last 16 years since the first report of single-incision laparoscopic cholecystectomy in 1995,1 over 100 articles have been published on this topic. The approach typically involves a 12–20-mm incision at or within the umbilicus, through which either multiple fascial openings are made with trocars, or a large fascial opening is made to accommodate a specialized multi-access port.
Studies comparing standard and single-port laparoscopic cholecystectomy have demonstrated either equivalency or statistical superiority of single-port techniques with regard to operative time, blood loss, and complications,2–4 but the clinical benefit appears harder to define. However, statements regarding the “obvious” benefits and “patient demand” of a single-incision technique abound,5–8 though there are few objective data to support these claims. A recent randomized study comparing standard with single-incision cholecystectomy found that the single-incision approach resulted in less pain postoperatively, both “abdominal” and “shoulder tip” pain.9 However, even the authors could not explain why pain from the pneumoperitoneum would be any different, and a placebo effect could explain the results. In addition, the difference of a pain score of 0 and 1 on a ten-point Likert scale is not clearly clinically relevant. A recent randomized, patient-blinded comparison of the two techniques failed to demonstrate differences in pain or satisfaction between the two approaches.10 In addition to pain, other outcome factors to consider in the single-incision approach include the complications that may come with a larger incision, such as wound infection and incisional hernia, with recently reported rates of approximately 1.6% and 5% of the time, respectively,11,12 in the standard approach.
It would seem prudent to perform a needs assessment prior to altering a highly accepted procedure. Since the new approach involves increasing the size of the incision, patients have reported as the most painful port site,13 it is not clear that patients would readily wish to undergo the same operation with a larger and potentially more painful incision simply to eliminate three smaller incisions. We hypothesize that the poorest patient satisfaction outcome is due to the umbilical port site, and given the choice, patients would wish to eliminate this incision.
Methods
Study Design
The study was conducted at the Cleveland Clinic in compliance with and approval of the hospital’s Institutional Review Board. The target population consisted of female patients 18 to 40 years of age who underwent laparoscopic cholecystectomy over a 2-year period from January 1, 2008 through December 31, 2009. Patients were identified by ICD-9 codes 574, 575, and subcodes for relevance to cholecystectomy. Patients who underwent combined operations or open cholecystectomy, or operations requiring conversion to open cholecystectomy, were excluded.
Patients were contacted by mail concerning the nature of the study, that a telephone survey would be conducted, and that patients could decline or participate. Patients were not informed what questions would be asked. Telephone surveys were conducted by two physicians and one nurse using a standardized telephone script (see Appendix).
Three attempts were made to contact patients at various times during the day and night. If no response was obtained, then these individuals were regarded as nonresponders. Charts were reviewed, and details of the operative technique were recorded. The data obtained were then compiled and analyzed. Means with standard deviation were calculated for patient age and length of follow-up. Follow-up was determined as the time between the date of surgery and the date of the telephone questionnaire. Calculations of statistical significance were performed using two-tailed unpaired t tests for comparative analysis of nominal data based upon mean age and follow-up. Chi-square analysis was used to determine p values for comparison between two nominal groups.
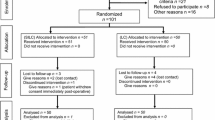
Results
Two hundred eighty-one female patients fitting the inclusion criteria were identified. Laparoscopic cholecystectomy was performed at our main campus and three satellite hospitals. Of the 281 patients identified, 125 were successfully contacted and consented to inclusion, yielding a 44.5% response rate. The mean age of the respondents at the time of surgery was 31.4 ± 5.5 years. Mean follow-up was 21.0 ± 7.2 months with a range of 7–36 months. Fourteen patients had prior operations (See Table 1 for patient characteristics).
Sixty patients (47.2%) correctly recalled the number of incisions, while 57 patients (45.6%) recalled fewer incisions than the actual number of ports utilized. Eight patients (7.2%) recalled more incisions than they actually had. No correlation was found between either age or length of follow-up and correctly or incorrectly recalling the number of incisions (see Table 2).
Four of the 125 patients had undergone a single-incision cholecystectomy, while another 3 patients underwent a reduced port cholecystectomy with two ports. One patient underwent a mini-laparoscopic procedure with two 3-mm instruments replacing the standard 5-mm right-sided trocars. Three of the patients who underwent single-incision laparoscopic cholecystectomy correctly recalled having one incision, whereas one patient believed they had three incisions. None of the patients who had the reduced port or the mini-laparoscopic cholecystectomy correctly recalled the number of incisions. One patient had a four-port laparoscopic cholecystectomy but required an additional port; that patient correctly recalled five ports.
One hundred sixteen patients underwent standard four-port laparoscopic cholecystectomy. Five patients (4.3%) incorrectly remembered having five incisions. Fifty-six patients (48.3%) correctly recalled four incisions, and 46 patients (39.7%) recalled three incisions. Seven patients (6.0%) and two patients (1.7%) recalled two incisions and one incision, respectively.
One hundred nineteen patients altogether recalled more than one incision. Fifty-eight of these patients (48.7%) identified one port site that was distinctly more painful than the others. Thirty-eight patients (31.9%) reported the umbilical site as having been distinctly more painful, while 14 patients (11.8%) recalled the epigastric site as more painful. Six patients identified one of the right-sided port sites as having been most painful. The mean follow-up for patients who recalled one incision as more painful versus those who did not was 18.3 ± 6.2 versus 24.0 ± 7.1 months (p = 0.00013). There was no significant difference in age (31.4 ± 5.8 versus 31.0 ± 5.3 years, p = 0.76) between the two groups (see Table 2).
Two patients reported a hernia postoperatively, both at the umbilical site. Two additional patients reported wound infection, one at a right-sided port site and the other involving “both” of her incisions; the latter patient recalled only two incisions, both of which were 10 mm in size. Three patients reported complications of pain lasting more than 30 days, one at the umbilicus and one involving the right-sided port sites. Two patients reported keloid formation, one at the umbilicus and one involving all port sites. One patient reported complications of bleeding, but could not recall which incision this involved (see Table 3). One of these patients recalled only two incisions but was notable for having had a prior open ventral hernia repair with the need for alternate site surgery and had a 10-mm trocar in the right upper quadrant.
Eighty-one of 118 patients (68.6%) said that in retrospect they would eliminate one incision given the opportunity. Seven patients were excluded from this calculation as they had or believed they had only a single incision (n = 6) or because of incomplete data (n = 1). Fifty-one patients (43.2%) said that they would eliminate the umbilical incision. Eighteen patients (15.3%) said they would eliminate the epigastric incision, while 12 patients (10.2%) would eliminate one of the right-sided incisions (see Table 2). Although there was a trend towards longer follow-up among patients not interested in eliminating an incision, this did not reach statistical significance (20.4 ± 7.2 versus 23.2 ± 7.0 months, p = 0.095).
Eleven of the 18 patients who would eliminate the epigastric incision (61.1%) had a 10- to 12-mm port at that site. Out of 38 patients who recalled the umbilical incision as the most painful, 31 patients (81.6%) would also eliminate the same incision (p < 0.001), as did 12 of the 14 (85.7%) patients who cited the epigastric incision as the most painful (p < 0.001). Of 52 patients who had both a 10-mm umbilical incision and a 10- to 12-mm epigastric incision, 36 patients (69.2%) would eliminate one of them (p = 0.035).
Discussion
This study was intended to determine whether single-incision approaches to laparoscopic cholecystectomy might be desirable to patients by asking them about their experiences with their wounds following laparoscopic cholecystectomy. The single-incision technique has not consistently demonstrated superiority to the standard technique with respect to outcomes relevant to the operation itself, and cosmesis may be presumed to be the only advantage in question. Therefore, the study population chosen was intended to represent the group most likely to benefit from the presumed cosmetic advantages of a single-incision approach. The reason for adopting this study design was that we were concerned that prospective studies, in which patients are randomized to standard versus single-incision approaches, have the potential to introduce bias to the patients as the patients are aware that the study intends to look at a new and implicitly “superior” technique. Nonetheless, certain limitations of the study exist, namely its retrospective nature and lack of standardization or significant cohort.
The primary finding of the study is that patients do appear interested in reducing the number of incisions, with 68.6% of patients indicating a desire to eliminate one incision. Not unexpectedly, pain seems to be a motivating factor as an overwhelming majority of patients who identified one incision as most painful were interested in eliminating that same incision. Given the larger size of the umbilical incision and the larger size of the epigastric incision in most of the patients who cited that site as the most painful, it is reasonable to conclude a relationship between the size of the incision and recollection of pain. The majority of patients who would eliminate one incision would eliminate the umbilical incision (63.0%). This presents a significant challenge to single-access approaches through the umbilicus, especially because even larger incisions are required with this technique.
Despite the apparent desire to eliminate an incision, it is interesting to note that even after a relatively short follow-up period, most of the study patients do not correctly recall the number of incisions they had. This suggests that the overall number of incisions is less important than whether they were painful or not. Of the 61 patients who recalled more than one incision but could not recall any specific incision as being more painful, 34 patients (55.7%) would not have eliminated any incision. Most of the remaining patients would still eliminate the umbilical incision, however, suggesting dissatisfaction with this incision for reasons other than pain, such as cosmesis.
These findings highlight the need to reduce port site pain. One technique includes liberal use of local anesthetics including local infiltration prior to incision, which has been demonstrated to significantly reduce postoperative pain.14 Furthermore, the learning points that single-incision surgery has to offer, such as refinement of surgical techniques to reduce the visibility of the umbilical scar by means of trans-umbilical rather than supra- or infra-umbilical incisions, may result in added patient satisfaction. Additional means of improving patient satisfaction based upon our findings include using a 5-mm rather than a 10-mm epigastric incision as there is no need for a larger trocar at that site given the current instruments available. In addition, the larger trocar site was associated with a higher risk for pain and desire to eliminate that incision. This is contrary to previously reported findings that a 10-mm versus a 5-mm epigastric incision does not impact postoperative pain,15 but this study addresses the issue in a new way.
Finally, when taking into account the few patients who were ambivalent to elimination of an incision, the fact that 74.6% of patients either would either not eliminate an incision or would eliminate the umbilical incision suggests that the single-incision technique for laparoscopic cholecystectomy does not address patient dissatisfaction with the current standard technique. This begs the question of whether single-site cholecystectomy is surgeon and industry driven, rather than by patient demand.
Conclusion
Patients are dissatisfied with the larger incisions associated with laparoscopic cholecystectomy, pain being the primary concern. Single-incision laparoscopic cholecystectomy does not address patient dissatisfaction with the current standard technique. Our needs assessment approach suggests that patients are not the driving factor behind the recent interest in the single-incision approach, and we should rethink why we are offering this to patients.
References
Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I. “One-Wound Laparoscopic Cholecystectomy.” Br J Surg. 1997;84:695.
Wu SD, Han JY, Tian Y. “Single-incision laparoscopic cholecystectomy versus conventional laparoscopic cholecystectomy: a retrospective comparative study.” J Laparoendosc Adv Surg Tech A. 2011;21:25–8.
Chang SK, Tay CW, Bicol RA, Lee YY, Madhavan K. “A case–control study of single-incision versus standard laparoscopic cholecystectomy.” World J Surg. 2011;35:289–93.
Chow A, Purkayastha S, Aziz O, Pefanis D, Paraskeva P. “Single-Incision Laparoscopic Surgery for Cholecystectomy: A Retrospective Comparison with 4-Port Laparoscopic Cholecystectomy.” Arch Surg. 2010;145:1187–1191.
Aprea G, Bottazzi EC, Guida F, Masone S, Persico G. “Laparoendoscopic Single Site (LESS) Versus Classic Video-Laparoscopic Cholecystectomy: A Randomized Prospective Study.” J Surg Res. 2011;166:e109-e112.
Han HJ, Choi SB, Kim WB, Choi SY. “Single Incision Multiport Laparoscopic Cholecystectomy: Things to Overcome.” Arch Surg. 2011;146:68–73.
Edwards C, Bradshaw A, Ahearne P, Dematos P, Humble T, Johnson R, Mauterer D, Soosaar P. “Single-incision Laparoscopic Cholecystectomy is Feasible: Initial Experience with 80 Cases.” Surg Endosc. 2010;24:2241–2247.
Ji W, Ding K, Yang R, Liu XD, Li N, Li JS. “Outpatient Single-incision Laparoscopic Cholecystectomy in 22 Patients with Gallbladder Disease.” Hepatobiliary Pancreat Dis Int. 2010;9:629–633.
Tsimoyiannis EC, Tsimogiannis KE, Pappas-Gogos G, Farantos C, Benetatos N, Mavridou P, Manataki A. “Different Pain Scores in Single Transumbilical Incision Laparoscopic Cholecystectomy Versus Classic Laparoscopic Cholecystectomy: A Randomized Controlled Trial.” Surg Endosc. 2010;24:1842–1848.
Marks J, Tacchino R, Roberts K, Onders R, Denoto G, Paraskeva P, Rivas H, Soper N, Rosemurgy A, Shah S. “Prospective Randomized Controlled Trial of Traditional Laparoscopic Cholecystectomy Versus Single-incision Laparoscopic Cholecystectomy: Report of Preliminary Data.” Am J Surg. 2011;201:369–373.
Zhou H, Zhang J, Wang Q, Hu Z. “Meta-analysis: Antibiotic Prophylaxis in Elective Laparoscopic Cholecystectomy.” Aliment Pharmacol Ther. 2009;29:1086–1095.
Uslu HY, Erkek AB, Cakmak A, Kepenekci I, Sozener U, Koccay FA, Turkcapar AG, Kuterdem E. “Trocar Site Hernia After Laparoscopic Cholecystectomy.” J Laparoendosc Adv Surg Tech A. 2007;17:600–603.
Ure BM, Troidl H, Spangenberger W, Dietrich A, Lefering R, Neugebauer E. “Pain After Laparoscopic Cholecystectomy.” Surg Endosc. 1994;8:90–96.
Cantore F, Boni L, Di Giuseppe M, Giavarini L, Rovera F, Dionigi G. “Pre-incision Local Infiltration with Levobupivicaine Reduces Pain and Analgesic Consumption After Laparoscopic Cholecystectomy: A New Device For Day-case Procedure.” International Journal of Surgery. 2008;6:S89-S92.
Golder M, Rhodes M. “Prospective Randomized Trial of 5- and 10-mm Epigastric Ports in Laparoscopic Cholecystectomy.” Br J Surg. 1998;85:1066–1067.
Acknowledgments
Thanks to Christine Bodnar and Myra Buttram for their assistance in coordinating the patient selection, with special thanks to Jane Bast for her work in collecting patient data.
Disclosures
Both Dr. Chalikonda and Dr. Kroh have received consulting fees and speaker fees for Covidien, Bard, Ethicon, and Intuitive.
Author information
Authors and Affiliations
Corresponding author
Appendix: Scripted questions in phone survey
Appendix: Scripted questions in phone survey
Good afternoon, my name is ____ and I am calling from the Cleveland Clinic in relation to the gallbladder surgery that you had performed at ____ Hospital on ____. You should recently have received a letter from the Cleveland Clinic Research Department explaining the purpose of this call. As stated in the letter, your responses are confidential and your identity will not be revealed.
-
1.
How many incisions do you remember having?
-
2.
Was one more painful than the others?
If so, which one?
-
3.
Can you please tell me if you had any wound complications such as pain, bleeding or infection following your surgery?
If so, what and which incision did it involve?
-
4.
Have you been told you developed a hernia after your surgery?
If so, where?
-
5.
With advances in technology, there are trends to using fewer incisions to perform the gallbladder surgery. If you were to have the operation again and could have one less incision, which one would you choose?
Thank you for your help with this survey.
Rights and permissions
About this article
Cite this article
Bencsath, K.P., Falk, G., Morris-Stiff, G. et al. Single-Incision Laparoscopic Cholecystectomy: Do Patients Care?. J Gastrointest Surg 16, 535–539 (2012). https://doi.org/10.1007/s11605-011-1785-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-011-1785-2