Abstract
Background
The attempt to further reduce operative trauma in laparoscopic cholecystectomy has led to new techniques such as natural orifice transluminal endoscopic surgery (NOTES) and single-incision laparoscopic surgery (SILS). These new techniques are considered to be painless procedures, but no published studies investigate the possibility of different pain scores in these new techniques versus classic laparoscopic cholecystectomy. In this randomized control study, we investigated pain scores in SILS cholecystectomy versus classic laparoscopic cholecystectomy.
Patients and methods
Forty patients (34 women and 6 men) were randomly assigned to two groups. In group A (n = 20) four-port classic laparoscopic cholecystectomy was performed. Patients in group B (n = 20) underwent SILS cholecystectomy. In all patients, preincisional local infiltration of ropivacaine around the trocar wounds was performed. Infusion of ropivacaine solution in the right subdiaphragmatic area at the beginning of the procedure plus normal saline infusion in the same area at the end of the procedure was performed in all patients as well. Shoulder tip and abdominal pain were registered at 2, 6, 12, 24, 48, and 72 h postoperatively using visual analog scale (VAS).
Results
Significantly lower pain scores were observed in the SILS group versus the classic laparoscopic cholecystectomy group after the first 12 h for abdominal pain, and after the first 6 h for shoulder pain. Total pain after the first 24 h was nonexistent in the SILS group. Also, requests for analgesics were significantly less in the SILS group, while no difference was observed in incidence of nausea and vomiting between the two groups.
Conclusion
SILS cholecystectomy, as well as the invisible scar, has significantly lower abdominal and shoulder pain scores, especially after the first 24 h postoperatively, when this pain is nonexistent. (Registration Clinical Trial number: NTC00872287, www.clinicaltrials.gov).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Laparoscopic cholecystectomy is the gold-standard procedure for gallbladder removal. The advantages of this procedure over the open approach include better cosmetic result, less postoperative pain, and shorter recovery time.
Recently, in order to reduce operative trauma and improve cosmetic result following laparoscopic cholecystectomy, new operative techniques have been developed. The introduction of natural orifice transluminal endoscopic surgery (NOTES) has enabled treatment of digestive diseases such as acute appendicitis and gallstones, and even the creation of some kinds of fundoplication, by means of a flexible scope introduced through the stomach, rectum or vagina [1–3].
Single-incision laparoscopic surgery (SILS) was developed with the aim of reducing the invasiveness of traditional laparoscopy [4, 5]. This approach can be performed using refinements of existing technology, such as instrumentation that allows greater articulation and rotation, and new retraction systems [5]. Although SILS has excellent cosmetic result and is considered a painless procedure, no published studies have investigated the possibility of different pain scores in SILS versus classic laparoscopic cholecystectomy. In this prospective, randomized, double-blind, controlled study we investigated pain scores in SILS cholecystectomy versus classic laparoscopic cholecystectomy.
Patients and methods
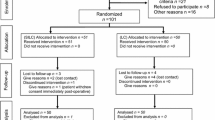
Forty patients (34 women and 6 men) aged from 28 to 75 years (mean 49 ± 13 years) were randomly assigned to two groups using a closed envelope containing information regarding placement into group A or B. In group A (n = 20) four-port classic laparoscopic cholecystectomy was performed. Patients in group B (n = 20) underwent SILS cholecystectomy. All procedures were performed by the same group of surgeons at “G. Hatzikosta” General Hospital of Ioannina, Greece. All patients were informed about the intervention technique and provided written informed consent. Inclusion criteria were: (a) body mass index (BMI) less than 30 kg/m2, (b) some attacks of pain from cholelithiasis, (c) American Society of Anesthesiology (ASA) grade I or II classification, and (d) written informed consent. Exclusion criteria were: (a) BMI more than 30 kg/m2, (b) signs of acute cholecystitis or choledocholithiasis or attacks of acute pancreatitis, (c) ASA grade more than II, and (d) lack of written informed consent. The 40 patients included in the study were selected from among 56 consecutive patients with diagnosed cholelithiasis. Sixteen patients were excluded because of: signs of acute cholecystitis (9 patients), clinical and laboratory findings of choledocholithiasis (3 patients; preoperative endoscopic retrograde cholangiopancreatography (ERCP) was performed), attacks of acute pancreatitis (2 patients), and ASA grade III classification (2 patients).
All patients meeting the inclusion criteria were assigned 1 of 40 closed envelopes. Surgeons were informed about the group of each patient in the operating room. Two other investigators, blinded to the group of each patient, independently recorded postoperative pain score, need for analgesics, and incidences of nausea and vomiting. Final pain scores were expressed as the mean score of the two independent investigators for each patient. No difference was found between the investigators in terms of nausea or vomiting incidence or analgesics request after the procedures.
Operative technique
In both groups, during laparoscopy the gas used was CO2 and intra-abdominal pressure was maintained at 10–11 mmHg. Anesthesiologists followed the same general anesthetic protocol. All patients were premedicated with intravenous paracetamol, ondansetron hydrochloride, and ranitidine. Anesthesia was induced using fentanyl (1.5 μg/kg), propofol (2–2.5 mg/kg), and cis atracurium (0.16 mg/kg). After endotracheal intubation, all patients were provided with mechanical ventilation using sevoflurane (1–2%) and an air/oxygen mixture (30% O2). In all patients a nasogastric tube was inserted at the beginning and removed after the intervention. In all patients of the two groups, 40 ml ropivacaine solution (2 mg/ml) was infused at the beginning of the procedure under the right hemidiaphragm. Local anesthetic infusion was performed using the suction device under visual control. At the end of the procedure, suction was placed under the right hemidiaphragm under visual control, 30 ml/kg normal saline at 37°C was infused, and once the pneumoperitoneum was deflated, the normal saline was suctioned [6].
Classic four-port laparoscopic cholecystectomy
All patients were placed in reverse Trendelenburg position (30º) with the table tilted downward to the patient’s left. After infiltration of 5 ml ropivacaine hydrochloride solution (7.5 mg/ml) around the umbilicus, pneumoperitoneum was created with an 11-mm umbilical trocar using Hasson technique. Another 5-mm trocar was placed in the midepigastrium just to the right of the falciform ligament, and two 5-mm trocars were placed in the right upper abdomen two fingerbreadths below the right coastal margin in the midclavicular and the midaxillary line. Before insertion of all trocars, 5 ml ropivacaine hydrochloride (7.5 mg/kg) was infiltrated around all trocar wounds. Dissection of the gallbladder was performed using ultrasonically activated coagulating shears (Harmonic Ace; Ethicon Endosurgery, Inc., Smithfield, RI, USA). Subhepatic closed drain was placed in three patients with difficult dissection of the bed of the gallbladder. The umbilical fascia was closed with absorbable suture, and the trocar wounds were sutured by intracutaneous stitches and covered by dermal glue (Dermabond; Ethicon Endosurgery, Inc., Smithfield, RI, USA).
SILS cholecystectomy
The patients were placed in the French position with the surgeon between the legs, the cameraman (first assistant) on the left of the patient, the second assistant on the right, the nurse near the right hand of the surgeon, and the monitor(s) at the shoulder level of the patient.
After infiltration around the umbilicus of 5 ml ropivacaine hydrochloride solution (7.5 mg/ml), a single intraumbilical 12-mm incision was made and the umbilicus was pulled out, exposing the fascia. Pneumoperitoneum was induced with a 10-mm atraumatic trocar (Versastep; Covidien, Norwalk, CT, USA) introduced into the abdomen by open (Hasson) technique. Pneumoperitoneum was maintained at 10–11 mmHg. Second and third trocars of 5-mm (Versastep; Covidien, Norwalk, CT, USA) were introduced, respectively, to the left and right, slightly above the first 10-mm trocar, leaving a small bridge of fascia between them to avoid leakage of carbon dioxide. The 12-mm skin wound was dilated and easily allowed the introduction of all trocars, parallel to one another. A 10-mm 45° long scope with a cable connection on the lateral down aspect was introduced through the 10-mm umbilical trocar.
The patient was placed in an anti-Trendelenburg position and rotated to the left. One straight-needle suture was passed transabdominally into the right subcostal and placed at the gallbladder fundus for suspension of the gallbladder from the abdominal wall. Dissection was performed using ultrasonically activated coagulating shears (Harmonic Ace; Ethicon Endosurgery, Inc., Smithfield, RI, USA), while an Endograsper roticulator (Covidien, Norwalk, CT, USA) was used for traction of the gallbladder, initially to ensure optimal exposure of the triangle of Callot.
The cystic artery and duct were firstly dissected and then separately clipped with a standard 5-mm clip applicator (Covidien, Norwalk, CT, USA) and excised. The gallbladder was pushed upright and dissected free from the liver by means of the ultrasonic shears. Once the gallbladder was free from the adjacent tissues, the 10-mm laparoscope was exchanged for a 5-mm 30º laparoscope and, through the 10-mm port, a standard Endocatch bag (Endocatch Gold, 10-mm; Covidien, Norwalk, CT, USA) was inserted and the gallbladder was extracted after removal of the suspending stitch from the abdominal wall.
Careful hemostasis was achieved; a subhepatic closed drain was placed in one patient with difficult dissection of the bed of the gallbladder, through a 5-mm trocar placed for this reason below the right coastal margin. Through a percutaneous needle puncture or a 5-mm trocar placed in the same area, a intraoperative cholangiography had been scheduled to be performed in indicated cases. The umbilical fascia was closed with absorbable suture, and the natural scar of the umbilicus was restored by intracutaneous stitches and covered by dermal glue (Dermabond; Ethicon Endosurgery, Inc., Smithfield, RI, USA).
Abdominal and shoulder tip pain were registered at 2, 4, 6, 12, 24, 48, and 72 h postoperatively. To assess postoperative pain, a visual analog scale (VAS) with a 10-cm vertical score ranging from “no pain” (score 0) to “worst possible pain” (score 10) was used. After the patients had been adequately instructed about the range for measuring pain, they selected a value on the scale (between 0 and 10). Pain intensity was monitored in this way at the designated points in time. At each time point, one score was obtained for abdominal pain and a second score for shoulder tip pain. Nausea and vomiting were assessed at the same time points.
All patients were given suppositories of 400 mg 4-(acetyl-amino)-phenol with 20 mg codeine phosphate plus 50 mg caffeine (Lonarid N; Boehringer, Ingelheim, Germany) on demand. In case of failure, additional analgesia consisting of 200 mg ketoprofen (Oruvail; Phône Poulenc Rorer, Germany) was administered as an intravenous dose of 1 mg/kg.
Based on previous studies [6–8] and with the pain score as the primary criterion, power analysis (p = 0.90, α = 0.05) by using StudySize software (version 2.0.4) with H1: Prob(sample 2 > sample 1) = 0.8 and equal size for samples 1 and 2 (two-tailed difference) showed that 20 patients (sample size 19.95) were required for each group. Statistical analysis for pain intensity scores was performed by using the Mann–Whitney U test. Differences between groups regarding nausea and vomiting incidence were assessed by use of the chi-square test. Patient demographic data, need for analgesics, and some demographic data (Table 1) were compared using the t-test. All statistical analyses were conducted by using SPSS statistical software (version 15.0; SPSS, Inc., Chicago, IL, USA). The level of significance was set at 0.05.
Results
Demographic characteristics of the patients of the two groups are presented in Table 1. There was a statistically significant difference in mean operative time. This difference, based on significant less experience in the SILS procedure, may be shortened through improved experience and instruments. One patient of group A and two patients of group B had mild bile leak for 2–4 days, treated conservatively through a closed subhepatic drain placed in those patients because of difficult dissection of the bed of the gallbladder. None of the patients had an indication for intraoperative cholangiography.
Nausea and vomiting (Table 2) occurred in a small number of patients in both groups, but no significant difference was observed between them.
Pain score (Table 3) analyses showed statistically significant differences after the first 12 h postoperatively regarding abdominal pain, and after the first 6 h postoperatively regarding shoulder tip pain. Patients in the SILS group (group B) reported significantly lower pain scores than patients in the classic four-port laparoscopic cholecystectomy group (group A). Especially in the SILS group, total pain (abdominal and shoulder pain) was nonexistent after the first 24 h postoperatively.
A significant lower number of suppository (Lonarid N) requests as well as additional analgesic (ketoprofen) demands were recorded in group B versus group A after the first 2 h postoperatively (Table 4).
Discussion
The important advantages of laparoscopic surgery result from preservation of the integrity of abdominal wall, including less operative trauma and complications, and better recovery and cosmetics [4]. For many operations, such as laparoscopic cholecystectomy, several attempts have been made to reduce operative trauma further by decreasing the number and size of the trocars used in the procedure [4]. The use of three trocars instead of four, and the use of mini-instruments, is definitely a step in this direction [9, 10].
Single-incision laparoscopic cholecystectomy is a step towards an even less invasive surgical procedure [5]. The umbilical access we use is a well-known and standardized site for access to the abdominal cavity for laparoscopy. It does not add new risks, and results in the same operative view as in standard laparoscopic cholecystectomy [5]. To enhance good cosmetic result, a particular intraumbilical technique is developed whereby the umbilicus is completely extroflexed and the skin incision is longitudinal and about 12–20 mm long. When the fascia is exposed, it is possible to enter the abdominal cavity with various devices or using open Hasson technique [5].
The careful reconstruction of the umbilicus and the percutaneous stitch for gallbladder suspension leave no scar in the abdominal wall, yielding a completely invisible scar.
Although the cosmetic result of SILS cholecystectomy is obvious, no published studies investigate the possibility of different pain scores in SILS versus classic laparoscopic cholecystectomy.
The results of the present study revealed significant less pain after SILS cholecystectomy versus four-port classic laparoscopic cholecystectomy, especially after the first 12 h postoperatively for abdominal pain and after the first 6 h postoperatively for shoulder tip pain. Total abdominal and shoulder pain after the first 6 h postoperatively in the SILS group was so low that more patients of this group asked to go home at this time point. Total pain was about zero and general condition was excellent after the first 24 h postoperatively, and some patients asked to return immediately to all activities.
Preincisional local infiltration plus intraperitoneal infusion of ropivacaine at the beginning of laparoscopic cholecystectomy, combined with normal saline infusion at the end of the procedure, is a well-established method for reducing pain after laparoscopic cholecystectomy [6–8].
Preincisional wound infiltration with local anesthetic seems to have provided some benefit in early postoperative pain reduction [6, 11], while other studies found no benefit [12]. The instillation of 150 mg ropivacaine intraperitoneally at the beginning of the procedure led to benefit in terms of both postoperative pain and postoperative analgesic consumption, without any toxic effect [13].
Intraperitoneal infusion of normal saline at the end of the procedure is the only way to remove the carbon dioxide from the subdiaphragmatic area. The carbon dioxide gas between liver and diaphragm increases the space between them, producing tension of the peritoneal reflection and shoulder pain through mechanical irritation of the right phrenic nerve [7, 14]. The 37°C temperature of the infused normal saline improves the hypothermia caused by carbon dioxide gas used for pneumoperitoneum. The heating of the peritoneum reduces the freezing peritoneal irritation and thus abdominal and shoulder pain [8, 15].
In the present study, all attempts for reduction of postoperative abdominal and shoulder pain were the same for classic laparoscopic and SILS cholecystectomy. The only difference was the extent of total incisional trauma, as well as the location of the umbilical incision. In classic four-port laparoscopic cholecystectomy, except for the three subcostal small incisions, the umbilical incision was located subumbilically. In SILS cholecystectomy the single incision was located intraumbilically. Although the amount of ropivacaine used for umbilical infiltration was the same in the two groups, postoperative pain was lower in the SILS group. This result suggests that the different neurosis in subumbilical and intraumbilical regions may cause this difference in postoperative pain. It is obvious that the three smaller incisions in classic laparoscopic cholecystectomy are absent in the SILS procedure, thus any pain from these wounds is absent in the SILS patients.
Shoulder tip pain was significantly lower in the SILS group versus the classic laparoscopic cholecystectomy group after the first 6 h postoperatively. It is difficult to explain this difference, since the kind and amount of the gas used for pneumoperitoneum were similar and the procedures for reduction of postoperative shoulder pain were also the same. It is possible that the subcostal trocar wounds, which are located near to the right hemidiaphragmatic peritoneum, may increase phrenic irritation and shoulder pain, although this is only a hypothesis.
In conclusion, today SILS cholecystectomy is a feasible and safe invisible-scar technique with significantly reduced postoperative abdominal and shoulder pain. SILS cholecystectomy in combination with preincisional and intraperitoneal ropivacaine plus subdiaphragmatic normal saline infusion at the end of the surgical procedure may facilitate 1-day surgery and early return to full activities for surgical treatment of uncomplicated cholelithiasis.
References
Zorron R, Maggioni LC, Pombo L, Oliveira AL, Carvalho GL, Filgueiras M (2008) NOTES transvaginal cholecystectomy: preliminary clinical application. Surg Endosc 22:542–547
McGee MF, Rosen MJ, Marks J, Onders RP, Chak A, Faulx A, Chen VK, Ponsky J (2006) A primer on natural orifice transluminal endoscopic surgery: building a new paradigm. Surg Inn 13:86–93
Rattner D, Kalloo A (2006) ASGE/SAGES working group on natural orifice transluminal endoscopic surgery. Surg Endosc 20:329–333
Cuesta MA, Berends F, Veenhof AAFA (2008) The “invisible cholecystectomy”: a transumbilical laparoscopic operation without a scar. Surg Endosc 22:1211–1213
Tacchino R, Greco F, Matera D (2008) Single-incision laparoscopic cholecystectomy: surgery without a visible scar. Surg Endosc 23:896–899
Pappas-Gogos G, Tsimogiannis KE, Zikos N, Nikas K, Manataki A, Tsimoyiannis EC (2008) Preincisional and intraperitoneal ropivacaine plus normal saline infusion for postoperative pain relief after laparoscopic cholecystectomy: a randomized double-blind controlled trial. Surg Endosc 22:2036–2045
Tsimoyiannis EC, Siakas P, Tassis A, Lekkas ET, Tzourou H, Kambili M (1998) Intraperitoneal normal saline infusion for postoperative pain after laparoscopic cholecystectomy. World J Surg 22:824–828
Tsimoyiannis EC, Glantzounis G, Lekkas ET, Siakas P, Jabarin M, Tzourou H (1998) Intraperitoneal normal saline and bupivacaine infusion for reduction of postoperative pain after laparoscopic cholecystectomy. Surg Laparosc Endosc Percutan Tech 8:416–420
Leggett PL, Churchman-Winn R, Miller G (2000) Minimizing ports to improve laparoscopic cholecystectomy. Surg Endosc 14:32–36
Sarli S, Iusco D, Gobbi S, Porrini C, Ferro M, Roncoroni L (2003) Randomized clinical trial of laparoscopic cholecystectomy performed with mini-instruments. Br J Surg 90:1345–1348
Papagiannopoulou P, Argiriadou H, Georgiou M, Papaziogas B, Sfyra E, Kanakoudis F (2003) Preincisional local infiltration of levobupivacaine vs ropivacaine for pain control after laparoscopic cholecystectomy. Surg Endosc 17:1961–1964
Elfberg BA, Sjovall-Mjoberg S (2000) Intraperitoneal bupivacaine does not effectively reduce pain after laparoscopic cholecystectomy: a randomized, placebo-controlled and double blind study. Surg Laparosc Endosc Percutan Tech 10:375–379
Kucuk C, Kadiogullari N, Canoler O, Savli S (2007) A placebo-controlled comparison of bupivacaine and ropivacaine instillation for preventing postoperative pain after laparoscopic cholecystectomy. Surg Today 37:396–400
Bisgaard T, Klarskov B, Kristiansen VB, Callesen T, Svend D, Kehlet H, Rosenberg J (1999) Multiregional local anesthetic infiltration during laparoscopic cholecystectomy in patients receiving prophylactic multimodal analgesia: a randomized, double-blinded, placebo-controlled study. Anesth Analg 89:1017–1024
Korell M, Schmaus F, Strowitzki T, Schneeweiss SG, Hepp H (1996) Pain intensity following laparoscopy. Surg Laparosc Endosc Percutan Tech 6:375–379
Disclosures
Evangelos Tsimoyiannis, Konstadinos Tsimogiannis, George Pappas-Gogos, Charalampos Farantos, Nikolaos Benetatos, Paraskevi Mavridou, and Manataki Adamantia have no financial support from any private institution, and the authors have no financial relationships with any pharmaceutical or device company.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tsimoyiannis, E.C., Tsimogiannis, K.E., Pappas-Gogos, G. et al. Different pain scores in single transumbilical incision laparoscopic cholecystectomy versus classic laparoscopic cholecystectomy: a randomized controlled trial. Surg Endosc 24, 1842–1848 (2010). https://doi.org/10.1007/s00464-010-0887-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00464-010-0887-3