Abstract
Purpose
To develop an in vitro methodology for prediction of concentrations and potential precipitation of highly permeable, lipophilic weak bases in fasted upper small intestine based on ketoconazole and dipyridamole luminal data. Evaluate usefulness of methodology in predicting luminal precipitation of AZD0865 and SB705498 based on plasma data.
Methods
A three-compartment in vitro setup was used. Depending on the dosage form administered in in vivo studies, a solution or a suspension was placed in the gastric compartment. A medium simulating the luminal environment (FaSSIF-V2plus) was initially placed in the duodenal compartment. Concentrated FaSSIF-V2plus was placed in the reservoir compartment.
Results
In vitro ketoconazole and dipyridamole concentrations and precipitated fractions adequately reflected luminal data. Unlike luminal precipitates, in vitro ketoconazole precipitates were crystalline. In vitro AZD0865 data confirmed previously published human pharmacokinetic data suggesting that absorption rates are not affected by luminal precipitation. In vitro SB705498 data predicted that significant luminal precipitation occurs after a 100 mg or 400 mg but not after a 10 mg dose, consistent with human pharmacokinetic data.
Conclusions
An in vitro methodology for predicting concentrations and potential precipitation in fasted upper small intestine, after administration of highly permeable, lipophilic weak bases in fasted upper small intestine was developed and evaluated for its predictability in regard to luminal precipitation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Weak bases constitute a significant portion of orally administered active pharmaceutical ingredients (APIs) (1). Due to their ionization characteristics, they dissolve more readily at acidic pHs. Depending on their lipophilicity and the administered dose, API concentration in the fluids emptying from the stomach is likely to exceed the saturation solubility in the upper small intestine (duodenum and first part of the jejunum), especially in the fasted state. Precipitation in the upper intestinal lumen will decrease early exposure and, perhaps, peak exposure and can also contribute to an overall increase in variability in exposure. Supersaturated drug concentrations on the other hand, will lead to plasma levels higher than anticipated from equilibrium solubility data. It has recently been shown that, depending on intragastric concentrations, exposure after administration of a suspension of posaconazole (a poorly soluble weak base) can be significantly increased, due to supersaturated drug levels in the small intestine (2).
Prediction of luminal supersaturation after administration of weak bases has been recently evaluated by applying in vitro solvent-shift methods (3,4). Although these approaches are very useful for initial evaluations, one issue is that estimation of degree of supersaturation of luminal contents is contingent on equilibrium solubility of the administered form, e.g. of a salt, a hydrate, or another crystal form (5).
To date, two approaches have been used for predicting lumenal concentrations of weak bases, In the first, concentrations of lipophilic weak bases in the upper small intestine after oral administration in the fasted state have been modelled by combining theoretical particle dissolution and particle growth kinetic models (6,7) or, in the case of administration of liquid dosage forms, by combining nucleation and particle growth models (8), according to the classical theory of crystallization. These approaches have been shown to be useful in forecasting the average plasma profile (7), the cumulative % dose absorbed vs. time plots (6) and the linearity of C max vs. Dose and AUC vs. Dose data (8) in humans. In the second approach, concentrations of lipophilic weak bases in the upper small intestine after oral administration in the fasted state have been modelled using in vitro setups either in the form of single compartment systems (8) or, more frequently, in the form of multiple compartment systems (9–12). One of these systems has been shown to be useful in forecasting the total % dose absorbed in humans (9). Another, the so called artificial stomach and duodenum (ASD) model, has been shown to be useful in selecting the most appropriate formulation of weak bases, based on pharmacokinetic data in dogs pretreated with pentagastrin (12).
One issue for both the theoretical and the in vitro models is that their ability to predict luminal concentrations of weak bases in the upper small intestine has, at best, been evaluated indirectly, i.e. by using plasma data or pharmacokinetic parameters in animals or in humans rather than by using luminal data in humans. In addition, with the exception of a few theoretical models (7,8), such evaluations are based on predictability of AUC t or of % dose absorbed. Luminal concentrations and the extent of precipitation of lipophilic (highly permeable) weak bases in the upper small intestine are likely to affect early exposure and C max to a greater extent than total exposure, as total exposure is more dependent upon efficient dissolution of the dose throughout the GI tract. As a result, validation of both theoretical and in vitro models remains a challenge with current methodologies.
The present investigation had two objectives. The first was to develop an in vitro methodology for prediction of concentrations and potential precipitation of highly permeable, lipophilic weak bases in fasted upper small intestine based on luminal data of ketoconazole and dipyridamole (5). The second objective was to evaluate the usefulness of the methodology in predicting luminal precipitation of AZD0865 and SB705498 based on plasma data (8,13, GSK data on file). AZD0865 (MW 366.46 g/mol) has an alkaline pKa of 6.1 and logP of 4.2 (8). SB705498 (MW 429.23 g/mol) has an alkaline pKa of 4.38 and logP of 3.6 (GSK data on file).
Materials and Methods
Materials
Ketoconazole (KCZ) was from Janssen Pharmaceutical Ltd. (Little Ireland, Cork, Republic of Ireland, lot# 0712003723). Dipyridamole (DPD) was from Boehringer Ingelheim Espanã, S.A. (Malgrat De Mar, Spain, lot# 08342). AZD0865 (AZD) was from AstraZeneca PLC (London, U.K.). SB705498 (SB) was from GlaxoSmithKline, Corporate Environment, Health & Safety (Brentford, UK). Αcetonitrile, dichloromethane and methanol of HPLC grade were from E. Merck (Darmstadt, Germany). Egg phosphatidylcholine (Lipoid E PC® 99.1% pure, lot# 105019-1/14) was kindly donated by Lipoid GmbH (Ludwigshafen, Germany). Maleic acid (ReagentPlus® ≥99% pure), sodium oleate (88.9% w/w pure) and cholesterol (Sigma grade, minimum 99%) were purchased from Sigma-Aldrich (St. Louis, U.S.A.). Sodium chloride and sodium hydroxide pellets were of analytical grade and purchased from Riedel-de Haën® (Seelze, Germany) and AppliChem GmbH (Darmstadt, Germany), respectively. Sodium taurocholate (>99.0%) was purchased from Prodotti Chimici e Alimentari S.p.A. (Basaluzzo, Italy). Water of HPLC grade was obtained by using a Labconco® water pro ps. System (Kansas City, USA). Hydrochloric acid, trifluoroacetic acid and ethanol 99.5% v/v were purchased from Panreac Co. (Barcelona, Spain). Diethylamine was purchased from Riedel-de Haën® (Seelze, Germany). PEG400 (SABOPEG 400, lot# 2-55247) was from CELLCO chemical Ltd. (Athens, Greece). HPMC [Pharmacoat 603 (lot# 0118458) and Pharmacoat 606 (lot# 9038173)] were from ShinEtsu (Tokyo, Japan).
In Vitro Setup
The setup is schematically presented in Fig. 1. All three compartments were made of double wall glass and maintained at 37 ± 0.5°C. The duodenal compartment was a cylindrical vessel with an internal diameter of 5.5 cm. Flow rates were controlled by a multi-channel peristaltic pump that allowed for simultaneous operation of various channels at different flow rates (IPC-12, ISM762, Ismatec S.A., Zurich, Switzerland). The sum of flow rates coming in the duodenal compartment equalled the outgoing flow rate (Fig. 1). During each experiment, the volume of contents of duodenal compartment was maintained at 60 ml.
During each experiment, contents of gastric and reservoir compartments were mildly agitated by means of a teflon magnetic stirrer. The contents of the duodenal compartment were agitated with a paddle having a U shape (Fig. 1). The paddle was rotated at 200 rpm [model RW 20 DZM overhead stirrer, IKA® LABORTECHNIK (Staufen, Germany)]. The paddle was positioned at the center and as close as possible to the bottom of the duodenal compartment. These conditions ensured perfect tank mixing conditions with minimal vortex, and, subsequently, representative sampling with respect to potentially precipitated material.
Composition of Gastric Compartment
Experiments with KCZ and DPD
To simulate the administration conditions applied in the recent clinical study (5), two HCl solutions of KCZ and two HCl solutions of DPD were studied; a low dose KCZ (100 mg) solution (KCZ-L), a high dose KCZ (300 mg) solution (KCZ-H), a low dose DPD (30 mg) solution (DPD-L) and a high dose DPD (90 mg) solution (DPD-H). The solutions were prepared by dissolving the relevant doses of KCZ and DPD in 240 ml HCl solutions. The final pH of all solutions was 2.7 (5). To take into account the resting gastric contents in the fasted state (5), 240 ml of each solution and 10 ml HCl solution, pH 1.8, were brought in the gastric compartment prior to the initiation of the experiment. The resulting pH of contents in the gastric compartment was ~2.5.
Experiments with AZD
Two formulations (oral solutions) were studied. These formulations contained the maximum AZD doses previously administered to healthy adults (8). As doses in the relevant clinical studies had been administered on mg/kg basis (8), in order to prepare and test the formulations in vitro, the body weight of an adult was assumed to be 75 Kg. For preparation of AZD Solution 1 (AZD-1), 310 mg of AZD were dissolved in 110 ml of an aqueous solution containing 22 ml PEG400 (20% v/v), 5.5 ml EtOH 99.5% (5% v/v) and the necessary amount of HCl for the final apparent pH to be 3 (8). AZD-1 had been co-administered with 240 ml of water in vivo and in order to also take into account the resting gastric contents, AZD-1 was diluted with 250 ml HCl solution pH 3. For preparation of AZD Solution 2 (AZD-2), 65 mg of AZD were dissolved in 21.3 ml of an aqueous solution containing 4.26 ml PEG400 (20% v/v), 1.065 ml EtOH 99.5% (5% v/v) and the necessary amount of HCl for the final apparent pH to be 3 (8). AZD-2 had been co-administered with 100 ml of water in vivo and in order to also take into account the resting gastric content, AZD-2 was diluted with 110 ml HCl solution pH 3.
Experiments with SB
Three suspensions simulating the intragastric conditions, after administration of immediate release tablets of SB, were studied. SB Suspension 1, SB Suspension 2 and SB Suspension 3 simulate the intragastric conditions immediately upon administration of 2 SB tablets (5 mg/tab), 4 SB tablets (25 mg/tab), and 16 SB tablets (25 mg/tab), respectively. These doses had been previously administered to healthy adults with a glass of water (GSK data on file).
Drug suspensions were used to mimic the conditions likely after disintegration of tablets in the stomach. On the one hand, the tablet is dispersed into solid particles, from which the drug must dissolve, and on the other hand, especially in the case of the two higher doses considered for SB, the solubility will quickly be achieved as the dissolution of the drug from the dispersed particles proceeds; the dose/solubility ratios of SB in acidic solutions with pH values as low as 2 are 165 ml, 1,653 ml, and 6,611 ml for the 10 mg, 100 mg and 400 mg doses, respectively (GSK data on file).
Since each of the tablets administered to humans contained 12.5 mg Pharmacoat 603, 5.5 mg Pharmacoat 606 and 0.61 mg PEG400, appropriate amounts of these excipients were also included in each suspension. Considering that each dose had been administered with 240 ml of water, one liter of SB Suspension 1 was prepared by dissolving 104.2 mg Pharmacoat 603, 45.8 mg Pharmacoat 606 and 5.1 mg PEG400 in one liter of HCl solution, pH 2.5, and by suspending 41.6 mg of SB in the solution. For preparation of one liter SB Suspension 2, 208.4 mg Pharmacoat 603, 91.6 mg Pharmacoat 606 and 10.2 mg PEG400 were dissolved in one liter HCl solution, pH 2.5, and 416.6 mg of SB were suspended in the solution. For preparation of SB Suspension 3, 0.8334 g Pharmacoat 603, 0.3666 g Pharmacoat 606 and 40.6 mg PEG400 were dissolved in one liter HCl solution, pH 2.5, and 1.6666 g of SB were suspended in the solution.
In order to reach meaningful conclusions and quantify precipitation (if any) in the in vitro test, reproducible emptying of particles is required, i.e. the suspension should not consist of aggregated particles. Therefore, although the correlation between in vitro and in vivo data would be affected in case of significant particle aggregation occurs in vivo, each suspension underwent five cycles of sonication (20 min/cycle) and agitation (magnetic stirrer, 30 min/cycle) at 37°C, after addition of the appropriate amount of SB, and was then stirred in USP II dissolution apparatus with the paddle rotating at 150 rpm for 48 h at 37°C. On the following day (experimental day), the suspension was sonicated for 20 min at 37°C, and was then agitated by means of a magnetic stirrer at 37°C for 1 h.
Saturated suspensions enabled study of the effect of solid particles on precipitation without the complicating effects of particle dissolution. Approximately half of each suspension was filtered through polytetrafluoroethylene filters [PTFE] (Whatman®, 30 mm, 0.45 μm, Whatman GmbH, Dassel, Germany) using glass syringes. Depending on the suspension, the filtrate was designated as SB Solution 1, SB Solution 2, and SB Solution 3. At each dose, a separate experiment was performed for the suspension and the corresponding solution (without the presence of the particles).
Composition of Duodenal Compartment
At the beginning of each experiment, the duodenal compartment contained a medium that simulates the composition of contents in the fasted upper small intestine (FaSSIF-V2plus). Compared with FaSSIF-V2 (14), FaSSIF-V2plus also contained free fatty acid (sodium oleate, 0.5 mM) and cholesterol (0.2 mM) (5). For preparation of FaSSIF-V2plus, 0.1712 g of sodium oleate was dissolved in 1 l FaSSIF-V2. Then, 0.0781 g of cholesterol, dissolved in ~10 ml dichloromethane, was added and an emulsion was formed. Dichloromethane was evaporated at about 40°C under magnetic stirring. The resulting micellar solution was slightly hazy and had no perceptible odour of dichloromethane. After cooling to room temperature, the volume was adjusted to 1 l with purified water. Macroscopic appearance of FaSSIF-V2plus as well as oleates and cholesterol concentrations remained unchanged at room temperature for at least 48 h (data not shown). Superiority of FaSSIF-V2plus over FaSSIF-V2 in predicting luminal concentrations was confirmed by using KCZ-H in the gastric compartment.
Composition of Reservoir Compartment
The reservoir compartment contained concentrated FaSSIF-V2plus that was pumped into the duodenal compartment to compensate for the dilution and the pH change caused by the incoming gastric fluid. By using FaSSIF-V2plus in the duodenal compartment it was found that concentrated FaSSIF-V2plus in the reservoir compartment must have six times higher buffer capacity than FaSSIF-V2plus in order for the pH in the duodenal compartment to remain at about 6.5 during the experiment. In addition, since the volume that enters the duodenal compartment from gastric compartment is four times higher than the volume that enters from the reservoir compartment (Fig. 1), concentration of all other components of concentrated FaSSIF-V2plus was four times higher than in FaSSIF-V2plus.
In Vitro experiments
The overall process of emptying from the gastric compartment follows first-order kinetics with t½ approximately 15 min (e.g. 15,16). However, within a specific 15-min interval, emptying occurred at a constant rate (Table I). The continuous drop of intraluminal concentration (5), due to rapid absorption of lipophilic compounds and rapid transit of duodenal contents, was simulated by evaluating the environment in the duodenal compartment during each 15-min time interval independently i.e. with a separate experiment. For each interval the corresponding gastric emptying rate was applied (Table I) and one sample was collected at the middle time point, i.e. at 7.5 min.
Upon collection, each sample was divided in three parts:
-
i)
The first part was immediately filtered through regenerated cellulose filters (Titan 2, 17 mm, 0.45 μm, SUN SRi, Rockwood, U.S.A.) for KCZ, DPD and AZD, and through PTFE filters for SB. The filtrate was divided in three portions:
-
The first, after appropriate dilution with mobile phase (so that precipitation during subsequent handling was avoided), was used for measuring the drug concentration, C.
-
The second was incubated (37°C, 48 h, 75 oscillations/min). One half was filtered through a 0.45 μm filter and the drug concentration, C inc , was measured. The other half was centrifuged (37°C, 12,560 × g, 10 min) to collect the precipitate for XRPD analysis.
-
The third was incubated (37°C, 48 h, 75 oscillations/min) in presence of excess of API and, after filtration through a 0.45 μm filter, equilibrium solubility, C s , was measured.
-
-
ii)
The second part was used for measuring the total drug content (solid and in solution), after appropriate dilution with mobile phase, C t .
-
iii)
The third part was centrifuged (37°C, 12,560 × g, 10 min) to collect the solids for XRPD analysis.
The choice of filters was based on the lack of adsorption, as confirmed previously for DPD and KCZ (17,18) and in preliminary experiments for AZD and SB. In experiments with AZD and SB, glass vials and syringes had to be used to avoid drug adsorption on the plastic. All APIs were found to be stable in FaSSIF-V2plus at 37°C for at least 48 h. Forty-eight hours were considered adequate for reaching equilibrium with the specific shaking setup (75 oscillations/min, model UNITRONIC OR, J.P. SELECTA,s.a., Barcelona, Spain) based on previous measurements (17). Samples for XRPD analysis were stored at −70°C without prior drying.
For all APIs, experiments were performed in triplicate. For each API, solubility values in filtrates corresponding to various time intervals were similar; coefficient of variation varied with the API from 2.32% to 11.5%. Therefore, solubility during a specific time interval was evaluated by measuring it in only one filtrate. Since coefficient of variation for concentrations in the duodenal compartment at each time interval was also very small (0.92-13.5% for all APIs), concentration after 48 h incubation at 37°C was also evaluated by measuring it in only one filtrate at each time interval.
Assays for KCZ and DPD were performed by using previously published HPLC-UV methods (5,18). Assays for both AZD and SB, involved the use of a BDS C18 (250 × 4.6 mm, 5 μm, Hypersil®, ThermoQuest Inc., U.S.A) column with a BDS C18 (10 × 4,6 mm, 5 μm, Hypersil®, ThermoQuest Inc., U.S.A.) pre-column and a flow rate of 1 ml/min. For AZD, the mobile phase consisted of acetonitrile:water:diethylamine 50:50:0.1 v/v/v, the wavelength was set at 258 nm and the injection volume was 20 μl. Quantification limit was 50 ng/ml. For SB, the mobile phase consisted of acetonitrile:water:trifluoroacetic acid 50:50:0.1 v/v/v, the wavelength was set at 240 nm and the injection volume was 50 μl. Quantification limit was 40 ng/ml.
Data Analysis
In vitro data on the presence of API in duodenal compartment are presented as Mean ± SD values. Previously collected luminal and in vivo data are presented as Box-Whisker plots showing the median value, the 10th, 25th, 75th, and 90th percentiles, and the 5th and 95th percentiles as symbols whereas the mean values are indicated with a solid white line (arithmetic mean) or with a black closed symbol (geometric mean). Precipitated fractions in the duodenal compartment, π, were estimated by using the following equation (5):
where C is the drug concentration and C t is the total amount of drug (solid and in solution) per unit volume.
Precipitated fractions after incubation of filtrates of individual samples from the duodenal compartment were estimated using Eq. 1, with C as C t and C inc as C (5). In all cases, values of precipitated fractions followed a normal distribution [SigmaStat 3.5 (SPSS Science Inc., New York, USA)]. The significance of the precipitated fraction was evaluated with one-sample one-tailed t-test by setting Type I error to 0.05 (S-Plus 4.5, Insightful Corporation, Seattle, USA).
XRPD Analysis
Crystallinity of precipitates was assessed by XRPD analysis using a PANalytical X’Pert Pro diffractometer Model PW3040/60 equipped with an X’Celerator detector (PANalytical B.V., Almelo, The Netherlands) and Cu Kα radiation at 40 kV and 45 mA. Samples were scanned from 2.0° to 40.0° (2θ) using a 0.0167° 2θ step size and 190.5 s time count. Each sample was prepared by applying a few milligrams to a Si wafer (zero background substrate), resulting in a thin layer of material suitable for analysis. Based on previous experience, freezing and thawing is unlikely to have an impact on the morphic form and all diffractograms were obtained under ambient temperature.
Results and Discussion
Prediction of Luminal Concentrations and Precipitated Fractions of KCZ
Total amount per ml and concentration in the duodenal compartment closely matched the corresponding average luminal data during the first 30 min of gastric emptying of KCZ-L (Fig. 2, upper graphs) and during the entire gastric emptying period of KCZ-H (Fig. 2, lower graphs). KCZ presence in the lumen 40-70 min post dosing of KCZ-L was only slightly overestimated by the in vitro data (Fig. 2, upper graphs). Unlike FaSSIF-V2plus, FaSSIF-V2 does not lead to concentrations of KCZ in duodenal compartment similar to those observed intraluminally during the first 30 min, after the administration of KCZ-H (Fig. 2, lower graphs). The equilibrium solubility of KCZ [Mean(SD), (n = 3)] in FaSSIF-V2 and in FaSSIF-V2plus was measured to be 14.75(0.90) and 22.78(0.25) μg/ml, respectively. Although the solubility of KCZ in FaSSIF-V2plus still underestimates median luminal solubility of KCZ (36–73 μg/ml, depending on the time after administration of a glass of water) (5), it is closer to the luminal value than the solubility in FaSSIF-V2. These data indicate that FaSSIF-V2plus is more appropriate than FaSSIF-V2 for the duodenal compartment. For KCZ-L, significant precipitation was observed both intraluminally [5 min, 20–30 min, and 50–70 min post dosing (5)] and in vitro [at 0–15 min and 15–30 min time intervals (this study)]. For KCZ-H, significant precipitation was observed both intraluminally [up to 70 min post dosing (5)] and in vitro [up to the 45–60 min time interval (this study)]. Precipitated fractions of KCZ in vitro were up to 0.08 during the emptying of KCZ-L in the duodenal compartment and up to 0.20 during the emptying of KCZ-H, similar to average luminal data [up to 0.11 and 0.16 after KCZ-L and KCZ-H, respectively (5)]. Deviations from in vivo data and high between-subject variability of luminal data may be related to the dynamic changes of contents in the region, e.g. movement of contents (and, therefore, of the drug) towards various directions. The hydrodynamics applied in the in vitro experiments [type of agitation and volume of contents in the duodenal compartment (60 ml)] were based on preliminary data (not shown) and constitute a compromise between biorelevance [fluid volumes in the small intestine of fasted subjects are between 45 and 319 ml (19)] and the need to take into account the rapid duodenal transit and absorption of highly permeable compounds.
Total amount (solid and in solution) of KCZ per ml (left graphs) and concentration of KCZ (right graphs) in the duodenal compartment (squares, mean±SD, n = 3, this study) and in the upper small intestine of adults [box plots, n = 7–12, (5)], at various times, after the initiation of gastric emptying of KCZ-L (upper graphs) and KCZ-H (lower graphs). Triangles show data collected when FaSSIF-V2 and concentrated FaSSIF-V2 were used in the duodenal and reservoir compartment, respectively.
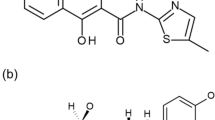
Compared with the spectrum of reference KCZ sample, almost all XRPD spectra exhibited additional peaks at approximately 5o and/or 32o 2θ, presumably due to an organic material (e.g. an alternative solid state form or version of KCZ) and inorganic salts (e.g. NaCl), respectively. XRPD data suggest that, during the emptying of KCZ-H, two different forms of KCZ are precipitated in the duodenal compartment: one form corresponds to the KCZ reference material that was used to prepare the KCZ-H (Fig. 3, image a vs. image b); the alternative form (assumed) presents a characteristic low angle peak at 5.2° 2θ (Fig. 3, image a vs. image c). Unlike these data, luminal precipitates of KCZ observed immediately upon collection of aspirates were primarily amorphous (5). After incubation of the in vitro filtrates for 48 h at 37°C precipitates were always crystalline and predominantly adopted the form of the reference material (Fig. 3, image a vs. image d) similar to previous observations with precipitates of KCZ after incubation of luminal supernatants (5). It may worth mentioning that a number of signature peaks (17–30° 2θ) are missing from many spectra of the in vitro precipitates (Fig. 3, image a vs. image b, c and d), due to preferred orientation of particles. Due to limited sample availability, however, alternative particle orientation could not be achieved.
Representative XRPD spectra of (a) KCZ reference material used for preparing solutions for the gastric compartment and measuring equilibrium solubilities, (b) precipitate in the duodenal compartment 7.5 min after the initiation of emptying of KCZ-H solution, (c) precipitate in the duodenal compartment 52.5 min after the initiation of emptying of KCZ-H solution, and (d) precipitate in the incubated (37°C/48 h) filtrate of the sample collected from the duodenal compartment 7.5 min after the initiation of emptying of KCZ-H solution.
Based on equilibrium solubility data in FaSSIF-V2plus (presented above) and Fig. 2, contents of duodenal compartment are supersaturated in regard to the free base during the emptying of KCZ-L and KCZ-H. This was further confirmed by data collected after incubation of samples: significant precipitation was observed in samples collected at all time intervals during the emptying of KCZ-L or KCZ-H with the precipitated fractions ranging from 0.15 to 0.90 or from 0.30 to 0.96, respectively. These data are in agreement with previous data from incubated luminal samples indicating significant precipitation in all samples collected during the first hour after administration of KCZ-L or KCZ-H with precipitated fractions being 0.17–0.52 or 0.22–0.73, respectively (5).
Prediction of Luminal Concentrations and Precipitated Fractions of DPD
Total amount per ml and concentration in the duodenal compartment reflected the corresponding average luminal data during the gastric emptying of both DPD-L (Fig. 4, upper graphs) and DPD-H (Fig. 4, lower graphs). Statistically significant precipitation was observed only during the emptying of DPD-H both intraluminally [50 min, 60 min and 70 min post dosing (5)] and in vitro [at 0–15 min and 30–45 min time intervals (this study)]. Inability to statistically detect a significant precipitation in vitro at the 15–30 min time interval could be attributed to the very low precipitated fraction and, therefore, to the relatively inaccurate estimation of it. Precipitated fractions of DPD in vitro were practically non-existent during the emptying of DPD-L in the duodenal compartment and up to 0.09 during the emptying of DPD-H, similar to average luminal data that were up to 0.05 and 0.07 after DPD-L and DPD-H, respectively (5).
Total amount (solid and in solution) of DPD per ml (left graphs) and concentration of DPD (right graphs) in the duodenal compartment (squares, mean±SD, n = 3, this study) and in the upper small intestine of adults [box plots, n = 7–12, (5)], at various times, after the initiation of gastric emptying of DPD-L (upper graphs) and DPD-H (lower graphs).
Due to the limited amounts of precipitates, crystal structure could not be evaluated with certainty.
Equilibrium solubility of DPD in FaSSIF-V2plus [Mean(SD), (n = 3)] was measured to be 12.919(0.039) μg/ml. Therefore, according to Fig. 4 contents of duodenal compartment are supersaturated in regard to the free base during the emptying of DPD-L and DPD-H up to the 30–45 min and the 60–75 min interval, respectively. This was further confirmed by data collected in incubated samples. After incubation, significant precipitation was observed in samples, collected during the emptying of DPD-L at the 0–15, 15–30 and 30–45 min intervals with the precipitated fractions ranging from 0.12 to 0.63. For incubated DPD-H samples, precipitation was observed in all cases and fractions were 0.19–0.92. These data are in agreement with previous data from incubated luminal samples indicating significant precipitation in all samples collected during the first hour after administration of DPD-L or DPD-H and precipitated fractions were 0.22–0.40 or 0.15–0.41, respectively (5).
Prediction of Luminal Precipitation of AZD
Mean ± SD precipitated fractions in duodenal compartment during the emptying of AZD-1 and AZD-2 from the gastric compartment are presented in Table II. Precipitation after AZD-1 seems to be substantial during the first half hour (about 15–20%), whereas precipitation after AZD-2 is limited over the same time period (up to about 8%). It should be noted that AZD-2 would be practically emptied within the first half of hour after administration, since the total volume in stomach at the time of administration is about 130 ml. Volumes of about 100 ml may not empty according to first order kinetics in the fasted state (16) but, based on data in Table II, alternative emptying rates would not have an impact on precipitation in the upper small intestine. After incubation of contents for 48 h at 37°C, precipitated fractions varied for AZD-1 from 0.950 (8 ml/min) to 0.720 (0.5 ml/min) and for AZD-2 from 0.934 (8 ml/min) to 0.451 (0.5 ml/min). These data indicate significant supersaturation in the duodenal compartment.
XRPD data for precipitates of AZD in the duodenal compartment during the emptying of AZD-1 solution revealed the presence of amorphous material and also the presence of peaks which partially matched the reference crystal structure (Fig. 5, image a vs. image b). XRPD data for precipitates collected after incubation for 48 h at 37°C, revealed the presence of amounts of AZD in the form of the reference material (Fig. 5a vs. c). The amounts of reference material were higher in samples collected at later times from the duodenal compartment. As in spectra of KCZ precipitates (Fig. 3), in most spectra of AZD precipicates additional peaks at approximately 5o and/or 32o 2θ, were observed presumably due to an organic material (e.g. an alternative solid state form or version of AZD) and/or inorganic salts (e.g. NaCl), respectively.
Representative XRPD spectra of (a) reference AZD material used for preparing solutions for the gastric compartment, (b) precipitate in the duodenal compartment 22.5 min after the initiation of emptying of AZD-1 solution, and (c) precipitate in the incubated (48 h/37°C) filtrate of the sample collected from the duodenal compartment 22.5 min after the initiation of emptying of AZD-1 solution.
Previously collected in vivo data indicate that for various formulations including AZD-1 and AZD-2, both the AUC t vs. Dose and C max vs. Dose plots are linear (8). Therefore, absorption rates are not affected by the dose, and it is unlikely that precipitation in upper SI (a process which would at least delay absorption) occurs to an extent that would affect the rate and extent of absorption. It has been previously shown for KCZ (a highly permeable weak base having similar absorption and elimination kinetics with AZD) that up to 20% precipitation in the upper small intestine after single dose administration of 300 mg (5) does not affect linearity of either AUC t vs. Dose or C max vs. Dose plot, since linear relevant plots have been reported for the 200–800 mg dose range (20). In vitro data with AZD-1 and AZD-2 also indicate up to 20% precipitation in the upper small intestine (Table II) and similarities in the in vitro morphic forms of the precipitates. Therefore, the in vitro data are consistent with in vivo pharmacokinetic data.
Prediction of Luminal Precipitation of SB
Based on Fig. 6 minimal (if any) precipitation occurs in the duodenal compartment during the emptying of SB solution 1, SB solution 2 and SB Solution 3. Indeed, precipitated fractions did not reach significance during the emptying of SB 1, were up to 0.01 during the emptying of SB 2 and up to 0.08 during the emptying of SB 3. Since all three solutions had similar (saturated) concentrations (20.1–24.0 μg/ml), small differences in precipitation behaviour may be attributed to the precipitation inhibitor (HPMC) and/or solubilizer (PEG) content of the administered formulations. After incubation of contents of duodenal compartment, precipitated fractions varied from 0.71 to 0.87 for SB 1 filtrates, 0.72–0.93 for SB 2 filtrates and 0.71–0.85 for SB 3 filtrates, confirming that filtrates were supersaturated to similar degrees. XRPD data for precipitates in duodenal compartment during the emptying of SB solutions or precipitates collected after incubation of filtrates could not be studied with certainty, due to the very limited amounts of precipitate available.
Mean ± SD total amount (solid and in solution) of SB (μg) per mL (a) and mean ± SD concentrations of SB (b) in the duodenal compartment (n = 3), after the initiation of emptying of SB Solution 1, i.e. the filtrate of corresponding SB Suspension 1 with total dose of 10 mg (triangles), SB Solution 2, i.e. the filtrate of corresponding SB Suspension 2 with total dose of 100 mg (circles), and SB Solution 3, i.e. the filtrate of corresponding SB Suspension 3 with total dose of 400 mg (diamonds). Dotted line corresponds to equilibrium solubility of SB in FaSSIF-V2plus.
Concentrations in the duodenal compartment during the emptying of SB Suspension 1 were identical to concentrations during the emptying of SB Solution 1 (Fig. 7b vs. Fig. 6b), i.e. there was no precipitation during the emptying of SB Suspension 1. In contrast, concentrations during the emptying of SB Suspension 2 during the first (0–15 min) and the second (15–30 min) interval were 29% and 38% of the concentration measured during the emptying of SB Solution 2 during the same intervals. Since practically no precipitation was observed during the emptying of SB Solution 2, it is reasonable to estimate that precipitated fractions in vitro after the initiation of emptying of SB Suspension 2 are 1–0.29 = 0.71 during the 0–15 min interval and 1–0.38 = 0.62 during the 15–30 min interval. Similarly, concentrations during the emptying of SB Suspension 3 during the first two time intervals were 26% and 37% of the concentration measured during the emptying of SB Solution 3 during the same intervals, i.e. precipitated fractions were 1–0.26 = 0.74 and 1–0.37 = 0.63, respectively. Therefore, the in vitro data suggest that when SB is administered at doses of 100 mg or 400 mg, substantial precipitation is likely to occur in the upper small intestine, much greater than that observed with the other three APIs.
Mean ± SD total amount (solid and in solution) of SB (μg) per mL (a) and mean ± SD concentrations of SB (b) in the duodenal compartment (n = 3), after the initiation of emptying of SB Suspension 1 (corresponding to the composition of gastric contents after administration of the 10 mg tablet dose, triangles), SB Suspension 2 (corresponding to the composition of gastric contents after administration of the 100 mg tablet dose, circles), and SB Suspension 3 (corresponding to the composition of gastric contents after administration of the 400 mg tablet dose, diamonds).
Precipitated fractions measured after incubation (48 h/37°C) of filtrates of contents of duodenal compartment collected during the emptying of SB Suspension 1, SB Suspension 2 and SB Suspension 3 were 0.69–0.86, 0.83–0.92 and 0.53–0.82, respectively, confirming that filtrates were significantly supersaturated.
AUC t vs. Dose plot indicates a small deviation from linearity, while C max vs. Dose plot shows a clear deviation from linearity at dose higher than about 20 mg (GSK data on file). Therefore, a conclusion as to whether the rate of input process is affected by the dose cannot be drawn from these data. C max /AUC t reflects an overall input rate constant without being affected by the fraction of the dose absorbed (21,22). Alternatively, AUC 1h /AUC t reflects early exposure normalized by AUC t (23,24). Based on Fig. 8, both C max /AUC t and AUC 1h /AUC t decrease as dose increases. This could be related to changes in luminal dissolution, solubilization capacity of luminal contents and/or precipitation in upper small intestine as dose increases.
For doses up to 20 mg, C max /AUC t and AUC 1h /AUC t decrease substantially as dose increases (Fig. 8). This could be attributed primarily to changes in the dissolution process which may, at least partly, be related to the different amounts of excipients in the administered doses. At doses higher than 20 mg, drug concentrations and the number of undissolved particles that reach the small intestine increase and precipitation becomes likely. At high doses (100–400 mg), both C max /AUC t and AUC 1h /AUC t are only slightly affected by the dose. It is, therefore, reasonable to argue that precipitation should be extensive and rapid, with SB concentrations in upper SI being close to saturation level and absorption rates being similar (solubility limited absorption) for as long as saturation level is maintained. In vivo pharmacokinetics are, therefore, consistent with the in vitro data from this study which indicate that no substantial precipitation after administration of the 10 mg dose would occur but that significant precipitation after administration of 100 mg and 400 mg doses would be observed. Further, in vitro data predict that luminal concentrations are practically similar at the 100–400 mg dose range (Fig. 7b), in agreement with the practically similar absorption rates observed after single administrations at this dose range (Fig. 8). Finally, and in line with previously performed simulations (6), in vitro data confirm the importance of the presence of undissolved particles on precipitation (Fig. 7b vs. Fig. 6b).
Conclusion
Tools for the prediction of the extent of luminal precipitation of poorly soluble, highly permeable weak bases after oral administration would facilitate their development, since such a prediction would show whether a modification of the formulation is necessary to reduce luminal precipitation. In turn, reduction of precipitation would increase early and, perhaps, peak exposure whereas it would decrease variability in exposure, after oral administration.
Experience with in vitro models (8) together with recently reported intraluminal data (5) indicates that simulation of the decreasing concentrations in the lumen and the applied in vitro hydrodynamics are key for valid predictions of intraluminal concentrations and potential precipitation of lipophilic weak bases in the upper small intestine. Indeed, a key characteristic of the proposed methodology vs. previously proposed in vitro methodologies is that the decreased drug concentration in the upper intestinal lumen with time after administration is adequately simulated. These parameters may have to be adjusted when low permeability compounds are studied. Also, optimization of hydrodynamics in the gastric compartment is required for drugs that are partially dissolved in the stomach. Composition of contents in the duodenal compartment seems also to be important; although FaSSIF-V2 is better than FaSSIF in assessing intraluminal dissolution (6), FaSSIF-V2 is not as suitable as FaSSIF-V2plus for the evaluation of intraluminal precipitation of KCZ.
The in vitro methodology developed and applied in this investigation proved adequate for reproducing both luminal concentrations and precipitated fractions of KCZ and DPD, after administration of solutions of these APIs in the fasted state at two different doses. The methodology was additionally successfully used to evaluate two other lipophilic weak bases, AZD and SB using previously collected plasma data in humans.
References
Paulekuhn GS, Dressman JB, Saal C. Trends in active pharmaceutical ingredient salt selection based on analysis of the orange book database. J Med Chem. 2007;50(26):6665–72.
Walravens J, Brouwers J, Spriet I, Tack J, Annaert P, Augustijns P. Effect of pH and comedication on gastrointestinal absorption of posaconazole: monitoring of intraluminal and plasma drug concentrations. Clin Pharmacokinet. 2011;50(11):725–34.
Box K, Comer JE, Gravestock T, Stuart M. New ideas about the solubility of drugs. Chem Biodivers. 2009;6(11):1767–88.
Bevernage J, Brouwers J, Clarysse S, Vertzoni M, Tack J, Annaert P, et al. Drug supersaturation in simulated and human intestinal fluids representing different nutritional states. J Pharm Sci. 2010;99(11):4525–34.
Psachoulias D, Vertzoni M, Goumas K, Kalioras V, Beato S, Butler J, et al. Precipitation in and supersaturation of contents of the upper small intestine after administration of two weak bases to fasted adults. Pharm Res. 2011;28(12):3145–58.
Sugano K. Computational oral absorption simulation of free base drugs. Int J Pharm. 2010;398(1–2):73–82.
Shono Y, Jantratid E, Dressman JB. Precipitation in the small intestine may play a more important role in the in vivo performance of poorly soluble weak bases in the fasted state: case example nelfinavir. Eur J Pharm Biopharm. 2011;79(2):349–56.
Carlert S, Pålsson A, Hanisch G, von Corswant C, Nilsson C, Lindfors L, et al. Predicting intestinal precipitation-a case example for a basic BCS class II drug. Pharm Res. 2010;27(10):2119–30.
Kobayashi M, Sada N, Sugawara M, Iseki K, Miyazaki K. Development of a new system for prediction of drug absorption that takes into account drug dissolution and pH change in the gastro-intestinal tract. Int J Pharm. 2001;221(1–2):87–94.
Kostewicz ES, Wunderlich M, Brauns U, Becker R, Bock T, Dressman JB. Predicting the precipitation of poorly soluble weak bases upon entry in the small intestine. J Pharm Pharmacol. 2004;56(1):43–51.
Gu CH, Rao D, Gandhi RB, Hilden J, Raghavan K. Using a novel multicompartment dissolution system to predict the effect of gastric pH on the oral absorption of weak bases with poor intrinsic solubility. J Pharm Sci. 2005;94(1):199–208.
Bhattachar SN, Perkins EJ, Tan JS, Burns LJ. Effect of gastric pH on the pharmacokinetics of a BCS class II compound in dogs: utilization of an artificial stomach and duodenum dissolution model and Gastroplus™ simulations to predict absorption. J Pharm Sci. 2011;100(11):4756–65.
Chizh BA, O’Donnell MB, Napolitano A, Wang J, Brooke AC, Aylott MC, et al. The effects of the TRPV1 antagonist SB-705498 on TRPV1 receptor-mediated activity and inflammatory hyperalgesia in humans. Pain. 2007;132(1–2):132–41.
Jantratid E, Janssen N, Reppas C, Dressman JB. Dissolution media simulating conditions in the proximal human gastrointestinal tract: an update. Pharm Res. 2008;25(7):1663–76.
Kelly K, O’Mahony B, Lindsay B, Jones T, Grattan TJ, Rostami-Hodjegan A, et al. Comparison of the rates of disintegration, gastric emptying, and drug absorption following administration of a new and a conventional paracetamol formulation, using gamma scintigraphy. Pharm Res. 2003;20(10):1668–73.
Oberle RL, Chen TS, Lloyd C, Barnett JL, Owyang C, Meyer J, et al. The influence of the interdigestive migrating myoelectric complex on the gastric emptying of liquids. Gastroenterology. 1990;99(5):1275–82.
Kalantzi L, Persson E, Polentarutti B, Abrahamsson B, Goumas K, Dressman JB, et al. Canine intestinal contents vs. simulated media for the assessment of solubility of two weak bases in the human small intestinal contents. Pharm Res. 2006;23(6):1373–81.
Vertzoni M, Pastelli E, Psachoulias D, Kalantzi L, Reppas C. Estimation of intragastric solubility of drugs: in what medium? Pharm Res. 2007;24(5):909–17.
Schiller C, Fröhlich CP, Giessmann T, Siegmund W, Mönnikes H, Hosten N, et al. Intestinal fluid volumes and transit of dosage forms as assessed by magnetic resonance imaging. Aliment Pharmacol Ther. 2005;22(10):971–9.
Huang YC, Colaizzi JL, Bierman RH, Woestenborghs R, Heykants J. Pharmacokinetics and dose proportionality of ketoconazole in normal volunteers. Antimicrob Agents Chemother. 1986;30(2):206–10.
Endrenyi L, Fritsch S, Yan W. Cmax/AUC is a clearer measure than Cmax for absorption rates in investigations of bioequivalence. Int J Clin Pharmacol Ther Toxicol. 1991;29(10):394–9.
Lacey LF, Keene ON, Duquesnoy C, Bye A. Evaluation of different indirect measures of rate of drug absorption in comparative pharmacokinetic studies. J Pharm Sci. 1994;83(2):212–5.
Chen M-L. An alternative approach for assessment of rate of absorption in bioequivalence studies. Pharm Res. 1992;9(11):1380–5.
Macheras P, Symillides M, Reppas C. The cutoff time point of the partial area method for assessment of rate of absorption in bioequivalence studies. Pharm Res. 1994;11(6):831–4.
Acknowledgments And Disclosures
Authors would like to thank B. Abrahamsson (Pharmaceutical Development, AstraZeneca R&D, Mölndal, Sweden) for providing the AZD0865 material and valuable comments, N. Koumandrakis and M. Dimopoulou (Department of Pharmaceutical Technology, National and Kapodistrian University of Athens, Athens, Greece) for their assistance in the evaluation of FaSSIF-V2plus, and S. Beato (Phad oral dosage forms 1, Novartis Pharma AG, Basel, Switzerland) for valuable comments during the design of the in vitro experiments.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Psachoulias, D., Vertzoni, M., Butler, J. et al. An In Vitro Methodology for Forecasting Luminal Concentrations and Precipitation of Highly Permeable Lipophilic Weak Bases in the Fasted Upper Small Intestine. Pharm Res 29, 3486–3498 (2012). https://doi.org/10.1007/s11095-012-0844-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-012-0844-z