Abstract
Strokes are one of the leading causes of death and disability in the world. Previously we have found that conventional protein kinase Cγ (cPKCγ) plays neuroprotective role in ischemic strokes. Further, we found that cPKCγ knockdown increased the level of cleaved (cl)-Caspase-3. However, the precise mechanisms underlying cPKCγ-mediated neuronal death remain unclear. To this end, a model incorporating 1 h oxygen–glucose deprivation/24 h reoxygenation (1 h OGD/24 h R) was established in cortical neurons. We found that cPKCγ knockdown remarkably increased neuronal death after OGD. We also found that cPKCγ knockdown increased the level of cl-Caspase-3 through the upstream initiators Capsases-9 (not Caspase-8/12) in OGD-treated neurons. Overexpression of cPKCγ could decrease neuronal death and cl-Caspase-3 and -9 levels. Moreover, cPKCγ knockdown further reduced the phosphorylation levels of p38 MAPK, p90RSK, and Bad. In addition, the protein levels of Bcl-2 and Bcl-xl were decreased after cPKCγ knockdown, whereas that of Bax was increased. In conclusion, our results suggest that cPKCγ partly alleviates ischemic injury through activating the p38 MAPK-p90RSK-Bad pathway and inhibiting Caspase-9 initiated apoptosis. This may have potential as a therapeutic target for ischemic stroke.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ischemic strokes result in high morbidity, mortality, and disability [1]. However, treatment is limited to recombinant tissue plasminogen activator (rtPA) thrombolysis or mechanical thrombectomy [2]. Due to the narrow therapeutic window and hemorrhagic side effects, therapeutic strategies for ischemic stroke remain unsatisfactory [3]. Thus, the mechanisms of neuronal death in ischemic injury have received particular attention. Conventional protein kinase Cγ (cPKCγ) is exclusively expressed in neurons of the central nervous system [4]. We have found that cPKCγ plays a neuroprotective role in cerebral ischemia [5]. However, the detailed molecular mechanisms underlying cPKCγ-mediated neuronal death have not been clearly defined.
It is generally known that apoptosis is involved in brain injury after ischemia [6], and 86% of cell death is based on apoptosis as opposed to 14% on necrosis in ischemic injury [7]. Inhibiting the apoptosis of neurons is a key strategy to alleviate ischemic injury [8]. Many molecules and pathways participate in the activation of neuronal apoptosis after ischemia, and many studies have focused on endogenous molecules [9]. cPKCγ, an important isoform of the serine/threonine protein kinase C family, is involved in ischemic reperfusion injury [10, 11]. A noticeable increase in cPKCγ expression is found in the penumbra regions of patients who have suffered strokes [12]. We have reported that cPKCγ alleviates neuronal death after stroke through the Akt-mTOR pathway and autophagy [5]. However, it has been reported that activation of cPKCγ during cerebral ischemic insult contributes to brain injury [13]. The inhibition of cPKCγ membrane translocation can also decrease decapitation-induced ischemic injury in mice [14]. However, the role of cPKCγ in mediating apoptosis in cerebral ischemic injury remains undefined.
The ability of cPKC to protect or injure neurons during cerebral ischemia suggests that it has the potential to be used in stroke treatment. In this study, the models of 1 h oxygen–glucose deprivation/24 h reoxygenation (1 h OGD/24 h R) cortical neurons, an in vitro insult mimicking ischemic stroke, were used to explore the effect of cPKC on apoptosis.
Materials and Methods
Establishment of Oxygen–Glucose Deprivation Models in Cultured Neurons
The primary cultured cortical neurons were prepared from postnatal 24 h C57BL/6J mice. Neurons were dissociated carefully and seeded onto plates in DMEM medium (Gibco Inc., Carlsbad, USA). The DMEM medium was replaced by serum-free neurobasal medium (Gibco Inc.) with 2% B27 supplement (Gibco Inc.) Half of the medium was replaced every third day.
Oxygen–glucose deprivation (OGD) model serves as an in vitro model of ischemic stroke. The cultured primary cortical neurons were subjected to oxygen–glucose deprivation for 1 h followed by 24 h of reoxygenation. For OGD treatment, the neurons were replaced with glucose-free DMEM medium and then placed under hypoxic conditions (5% CO2/2% O2/93% N2) at 37 °C for 1 h. After that, glucose-free DMEM was replaced by neurobasal medium under normoxic conditions (5% CO2/21% O2/74% N2) for a 24 h period of reoxygenation. All animal protocols were in strict accordance with the National Institutes of Health Guide for the Care and Use of Laboratory Animals. All experimental protocols were approved by the Experimental Animal Ethics Committee of Lanzhou University Second Hospital.
Transduction of Short Hairpin RNAs into Cultured Neurons
The neurons were transduced with lentiviral vectors containing the cPKCγ short hairpin RNA (shRNA) gene or the negative control (NC), Lv-cPKCγ or Lv-GFP, after 3 days of culture according to the manufacturer’s instructions (MDL Biotech, Beijing, China). After a 72 h period of lentiviral transduction, neurons were subjected to 1 h OGD/24 h reoxygenation (1 h OGD/24 h R) treatment. The efficiency of transduction of the lentiviral vectors into the primary cultured neurons was about 70%.
Measurement of Cell Viability
Neurons were seeded into 96-well plates and cultured overnight for adherence. The neuron survival rate was determined by using thiazolyl blue tetrazolium bromide (MTT; Promega, Madison, USA), and neuron death rate was detected by the LDH release rate using the CytoTox 96 Non-Radioactive Cytotoxicity Assay (Promega) as per the manufacturer’s instructions.
Western Blot Assay and Analysis
Total proteins were extracted from cultured neurons, and 30 µg of total protein was loaded onto an SDS-PAGE gel (12% SDS) and transferred to a nitrocellulose membrane which was then blocked with 5% nonfat milk in Tween/Tris-buffered salt solution (TTBS) for 1 h. Primary antibodies against Caspase-3/8/9/12 (CST, Danver, USA), P-ERK1/2 (Thr202/Tyr204, Millipore, St. Louis, MA, USA), ERK1/2 (Millipore), P-JNK (Thr183/Tyr185, CST), JNK (CST), P-p38 MAPK (Thr180/Tyr182, CST), p38 MAPK (CST), P-p90RSK (Thr359/Ser363, CST), p90RSK (CST), P-Bad (Ser112, CST), Bad (CST), HSP70 (CST), cPKC (Santa Cruz Biotechnology, Heidelberg, Germany), Bcl-2 (CST), Bcl-xl (CST), Bax (CST), β-tubulin (Sigma-Aldrich, Darmstadt, Germany), and β-actin (Proteintech, Rosemont, USA) were added. Secondary antibodies against rabbit or mouse IgG (Jackson Immuno Research, West Grove, PA, USA) were added. The densitometry of proteins was normalized to β-actin or β-tubulin, as an internal standard.
Statistical Analysis
The SPSS 17.0 software was used for statistical analysis. All values were expressed as the mean ± standard deviations (SD). Statistical analysis was assessed by one-way analysis of variance (ANOVA) and by the Bonferroni multiple comparison test. Statistical significance was set at p < 0.05.
Results
cPKCγ Knockdown Aggravated Ischemic Injury in the OGD Model
To explore the role of cPKCγ in cortical neurons after OGD, three cPKCγ shRNA candidates were used. cPKCγ shRNA2 which effectively inhibits the expression of cPKCγ was chosen for the following experiment (Fig. 1a). After the neurons were exposed to OGD for 30, 60, 90, and 120 min, the MTT results showed that neuronal survival rate was decreased with the extension of OGD time and reached a minimum at 120 min when compared with the normoxic group (Fig. 1b). When neurons were treated with 1 h OGD and 0, 12, 24, and 48 h of reoxygenation, the neuronal survival rate increased slightly at 24 h to 48 h when compared with the 1 h OGD/0 h R group (Fig. 1c). Here, in vitro models of ischemic stroke were constructed by keeping neurons in an OGD condition for 1 h followed by 24 h of reoxygenation. As per the MTT and LDH results shown in Fig. 1d, e, the 1 h OGD/24 h R treatment significantly decreased the neuronal survival rate and simultaneously increased the neuronal death rate compared with their normoxic group, respectively. Moreover, cPKCγ knockdown further decreased the neuronal survival rate and simultaneously increased the neuronal death rate. These results provide further evidence that cPKCγ may play a protective role in OGD-treated neurons.
Effects of cPKCγ on the survival and death rate of cortical neurons after 1 h OGD/24 h R. A Western blot showing that cPKCγ shRNA2 decreases the protein expression of cPKCγ. B Quantitative analysis of the neuronal survival rate after exposure to OGD for 30, 60, 90, and 120 min. C Quantitative analysis of the neuronal survival rate after exposure to 1 h OGD and 0, 12, 24, and 48 h R. Quantitative analysis showed the effect of cPKCγ shRNA2 treatment on the neuronal survival rate (D) and the death rate (E) from the Normoxic and OGD groups. NC: negative control. ***p < 0.001 versus Normoxic group (B, C, D, and E), $$p < 0.01 versus 1 h OGD/0 h R (C) ###p < 0.001 versus 1 h OGD/24 h R + NC group (D and E)
cPKCγ Knockdown Increased Caspase-9-Initiated Apoptosis in Neurons after 1 h OGD/24 h R
Accumulated studies have confirmed that caspases were activated in neurons after cerebral ischemia [15]. To explore the role of cPKCγ in apoptosis after ischemic injury, we used western blot analysis to assess the cleaved (cl)-Caspase-3 in neurons with 1 h OGD/24 h R. We found that the level of cl-Caspase-3 significantly increased after 1 h OGD/24 h R and further increased in cPKCγ shRNA2 neurons compared with that in NC neurons (Fig. 2b).
Effects of cPKC on the ratios of cl-Caspase/pro-Caspase-3/8/9/12 in neurons after 1 h OGD/24 h R. Results (A, C, E, and G) and quantitative analysis (B, D, F, and H) of western blot showed the effect of cPKCγ knockdown on the ratios of cl-Caspase-3/pro-Caspase-3, cl-Caspase-8/pro-Caspase-8, cl-Caspase-9/pro-Caspase- 9, and cl-Caspase-12/pro-Caspase-12 in neurons after 1 h OGD/24 h R, respectively. NS: no significance. ***p < 0.001 versus Normoxic group (B, D, F, and H),.###p < 0.001 versus 1 h OGD/24 h R + NC group (B and F)
There are three possible pathways causing Caspase-3 activation: the mitochondria-mediated intrinsic pathway via Caspase-9, the death receptors-mediated extrinsic pathway via Caspase-8, and the endoplasmic reticulum (ER)-stress pathway via Caspase-12. These three pathways have been reported to be activated in cerebral ischemia [16]. To further examine the effect of cPKCγ on initiator Caspases, we used western blot to determine whether cPKCγ could affect the levels of cl-Caspases-8, -9 and -12. We found that the levels of cl-Caspase-8 (Fig. 2d), -9 (Fig. 2f) and -12 (Fig. 2h) significantly increased in the 1 h OGD/24 h R group, but the level of cl-Caspase-3 and -9 further increased while both cl-Caspase-8 and -12 showed no difference in the cPKCγ shRNA2 group compared with that of the NC group, respectively. These results suggest that cPKCγ could decrease Caspase-9-initiated apoptosis in neurons after 1 h OGD/24 h R.
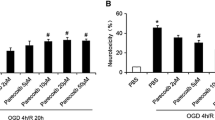
To further confirm that cPKCγ could decrease neuronal death and Caspase-9-initiated apoptosis after OGD, the neurons were transfected with lv-cPKCγ or lv-GFP. The cPKCγ proteins were upregulated in the lv-cPKCγ group (Fig. 3a). As the MTT (Fig. 3b) and LDH (Fig. 3c) assays show, lv-cPKCγ reduced neuronal death relative to the lv-GFP group. The western blot analysis results showed that lv-cPKCγ reversed the high levels of cl-Caspase-3 (Fig. 3e) and -9 (Fig. 3g) that were induced in the neurons after 1 h OGD/24 h R compared with the lv-GFP group. These data further confirm that cPKCγ alleviates neuronal death and apoptosis after 1 h OGD/24 h R.
Effects of lv-cPKC on the neuronal death and the ratios of cl-Caspase/pro-Caspase-3/9 in neurons after 1 h OGD/24 h R. A Western blot showing cPKCγ protein expression in the lv-cPKCγ group in neurons after 1 h OGD/24 h R. Quantitative analysis of the neuronal survival rate (B) and death rate (C) in neurons transfected with lv-cPKCγ or lv-GFP after OGD. Results (D and F) and quantitative analysis (E and G) of the western blot showing the effect of lv-cPKCγ knockdown on the ratios of cl-Caspase-3/pro-Caspase-3 and cl-Caspase-9/pro-Caspase-9 in neurons after 1 h OGD/24 h R, respectively. ***p < 0.001 versus Normoxia group (B, C, E, and G), #p < 0.001 versus 1 h OGD/24 h R + NC group (B) ###p < 0.001 versus 1 h OGD/24 h R + NC group (C, e, and g)
cPKCγ Knockdown Reduced the Phosphorylation Level of p38 MAPK in Neurons with 1 h OGD/24 h R
It is generally known that MAPKs can regulate apoptosis in ischemic stroke [17, 18]. PKC family can regulate the phosphorylation of MAPKs [19]. To further elucidate whether MAPKs are involved in cPKCγ-mediated apoptosis in OGD-treated neurons, western blot analysis showed that 1 h OGD/24 h R treatment significantly increased the phosphorylation levels of ERK (Fig. 4b) and JNK (Fig. 4d), and decreased the phosphorylation levels of p38 MAPK (Fig. 4f) when compared with that in the normoxic group, but only the phosphorylation level of p38 MAPK significantly decreased in cPKCγ shRNA2 neurons relative to the NC neurons. These results indicate that cPKCγ inhibits OGD-induced apoptosis by increasing the p38 MAPK phosphorylation level.
Effects of cPKC on the phosphorylation levels of MAPKs in neurons after 1 h OGD/24 h R. Results (A, C, and E) and quantitative analysis (B, D, and F) of the western blot showed the effect of cPKCγ knockdown on the phosphorylation levels of ERK, JNK and p38 MAPK in neurons after 1 h OGD/24 h R, respectively. **p < 0.01 versus Normoxic group (D) ***p < 0.001 versus Normoxic group (B and F), ###p < 0.001 versus 1 h OGD/24 h R + NC group (F)
cPKCγ Knockdown Reduced the Phosphorylation Levels of p90RSK and Bad in Neurons with 1 h OGD/24 h R
Heat shock protein 70 (HSP70) is a downstream target of MAPKs and plays a role in anti-apoptosis [20]. ERK1/2 can regulate the phosphorylation level of protein 90 ribosomal S6 kinase (p90RSK), and p-p90RSK could sequentially phosphorylate the proapoptotic protein Bad during cerebral ischemia [21]. Western blot analysis showed that HSP70 protein expression was significantly decreased in the OGD-treated group when compared with the normoxic group, but showed no difference between the cPKCγ shRNA2 group and the NC group (Fig. 5d). After OGD/R injury, the phosphorylation levels of p90RSK and Bad diminished, and cPKCγ knockdown further reduced the phosphorylation levels of p90RSK (Fig. 5b) and Bad (Fig. 5f) relative to the NC group. These data show that cPKCγ enhances the phosphorylation levels of p90RSK and Bad in neurons after 1 h OGD/24 h R.
Effects of cPKC on the protein expression level of HSP70 and phosphorylation levels of p90RSK and Bad in neurons after 1 h OGD/24 h R. Results (A, C, and E) and quantitative analysis (B, D, and F) of the western blot showed the effects of cPKCγ knockdown on the protein level of HSP70 and phosphorylation levels of p90RSK and Bad in neurons after 1 h OGD/24 h R, respectively. ***p < 0.001 versus Normoxic group (B, D, and F), ###p < 0.001 versus 1 h OGD/24 h R + NC group (B and f)
cPKCγ Knockdown Reduced the Levels of Antiapoptotic Proteins (Bcl-2 and Bcl-xl) and Increased the Level of Proapoptotic Protein (Bax) in Neurons after 1 h OGD/24 h R
The results from western blot analysis revealed that the protein levels of B-cell lymphoma-2 (Bcl-2) and B-cell lymphoma-xl (Bcl-xl) were substantially low, and Bcl-2 associated X protein (Bax) protein level was significantly high in the 1 h OGD/24 h R group when compared with that of the normoxic group. Compared with the NC group, cPKCγ shRNA2 group had lower levels of Bcl-2 (Fig. 6b) and Bcl-xl (Fig. 6d), whereas the protein level of Bax (Fig. 6f) was significantly higher. These results suggest that cPKCγ increases the levels of antiapoptotic proteins and decreases proapoptotic protein levels in ischemic neurons, further suggesting that cPKC is involved in the apoptosis after ischemic injury.
Effects of cPKC on the protein expression level of Bcl-2, Bcl-xl and Bax in neurons after 1 h OGD/24 h R. Results (A, C, and E) and quantitative analysis (B, D, and F) of the western blot showed the effects of cPKCγ knockdown on the protein levels of Bcl-2, Bcl-xl and Bax in neurons after 1 h OGD/24 h R, respectively. ***p < 0.001 versus Normoxic group (B, D, and F), ###p < 0.001 versus 1 h OGD/24 h R + NC group (B, D and F)
Discussion
Stroke is one of the leading causes of death worldwide [22]. Its management involves intravenous thrombolysis followed by mechanical thrombectomy, and less than 50% of treated patients eventually enjoy an independent life [23]. It is therefore important to explore the underlying mechanisms of ischemic injury and identify novel therapeutic targets. Apoptosis, autophagy, and necrosis are three main types of cell death involved in ischemic stroke pathogenesis [24]. We previously found that cPKCγ alleviated ischemic injury in ischemic stroke through the Akt-mTOR Pathway and downstream autophagy [5]. However, the role of cPKCγ in apoptosis after stroke remains unclear. Using OGD neuron models, our data demonstrates three main findings. Firstly, we found that cPKC knockdown promoted neuronal death. Moreover, cPKC knockdown increased the cleavage of Caspase-9/3 and Bax protein levels, while decreased Bcl-2 and Bcl-xl protein levels. cPKCγ overexpression could decrease neuronal death and Caspase-9-initiated apoptosis after OGD. Finally, we found that cPKC knockdown reduced the phosphorylation levels of p38 MAPK, p90RSK and Bad. Our results suggest that cPKC is beneficial to neuronal survival and improved stroke outcome.
In general, neuronal survival requires adequate supply of oxygen and glucose. In the process of oxygen and glucose deprivation, there is energy depletion that decreases neuronal survival [25]. Moreover, the degree of neuronal damage is closely related to the duration and degree of OGD [26]. We opted for 1 h OGD in cultured neurons through the optimization of the duration of OGD insult. Reoxygenation after OGD increases neuronal survival and alleviates ischemic injury [27]. Reoxygenation after OGD not only brings oxygen and glucose to neurons and attenuates oxidative stress, but also contributes to neuronal reperfusion injury that can cause brain damage [28, 29]. Although the injury in reoxygenation stage is not as serious as that in the OGD alone stage, the survival rate of neurons reduced in the reoxygenation stage. In our experiment, we used an MTT assay to measure the survival rate of neurons at 1 h OGD/R 0, 12, 24, and 48 h, and the results showed that the survival rate of neurons increased slightly at three different time points of reoxygenation, which was different from previous reports. The main reason is that apoptosis does occur after 1 h OGD/R 0−48 h, and some apoptotic neurons might be tested by the MTT assay. Because in the early stage of apoptosis, neurons still have intact organelles, such as mitochondria. The MTT assay results showed that the survival rate of neurons increased slightly at R 0−48 h post OGD. In this study, we explored the neuronal apoptosis in the mitochondrial pathway after 1 h OGD/24 h R. These protein measurements may be affected by several factors that influence the proteome of dead cells.
cPKCγ has been found to increase as high as 24-fold in penumbra tissue samples obtained from ischemic stroke patients [12]. cPKCγ knockout increases the ratio of cleaved/pro-Caspase-3 and TUNEL-positive cells to total neurons [30]. Previous studies suggest that cPKCγ plays an essential role in neuroprotection after ischemic injury [13]. Here, we concluded that one of the mechanisms utilized by cPKCγ to extend its protective effect was the inhibition of Caspase-9-initiated apoptosis. MAPKs, including JNK, ERK1/2 and p38 MAPK, are mediators of neuronal viability after cerebral ischemia [31]. p38 MAPK plays a dual role in the regulation of cell death. p38 MAPK activation induces apoptosis and exacerbates infarction in rats after MCAO [32]. On the contrary, the activation of p38 MAPK exerts antiapoptotic effects in ischemic stroke [33]. The activation of ERK1/2 regulates neuronal survival through apoptosis signals during cerebral ischemic injury [34]. It has been reported that JNK activation can induce apoptosis in ischemic stress [35]. We have found that cPKCγ alleviates ischemic injury through the Akt-mTOR pathway, suggesting that PKC is upstream of the ischemic signaling pathway [5]. Our results showed that cPKCγ knockdown significantly decreased the p38 MAPK phosphorylation level following 1 h OGD/24 h R, while the phosphorylation level of ERK1/2 and JNK were not altered by cPKCγ shRNA2.
It has been reported that activated ERK1/2 can phosphorylate p90RSK and subsequently activate Bad, playing a neuroprotective role in MCAO rats [21]. When p90RSK is phosphorylated and activated, its downstream kinase is subsequently phosphorylated to trigger apoptosis [36]. We concluded that cPKC knockdown reduced the phosphorylation levels of P90RSK and Bad, suggesting that cPKC is upstream of p90RSK and Bad. HSP70 is also a downstream target of p38 MAPK and inhibits apoptosis in vitro and in vivo ischemic models [37]. In our study, we found that HSP70 markedly decreased in the OGD model as reported previously, but cPKC knockdown had no effect on HSP70 protein expression. These results suggest that cPKC promotes the upregulation of P-p90RSK and P-Bad, but not HSP70 expression in antiapoptotic signaling. We did not further validate the upstream and downstream relationship between p38 MAPK, p90RSK and Bad. The precise mechanism underlying ischemic stroke that triggers apoptotic cascades needs to be fully elucidated.
In the Bcl-2 protein family, the dynamic balance between proapoptotic protein (Bax) and antiapoptotic proteins (Bcl-2 and Bcl-xL) determines cell fate during cerebral ischemia [38]. In response to stimuli, Bax translocates to the mitochondria and results in cytochrome c (cyt c) release [39]. Cyt c activates pro-Caspase-9 to form an apoptosome, and then initiates Caspase-3-mediated apoptosis [40]. Our results indicate that cPKC knockdown further downregulates the OGD-induced decreased expression of Bcl-2 and Bcl-xL, and upregulates Bax expression. These results indicate that cPKC upregulates the ratio of the antiapoptotic proteins, Bcl-2 and Bcl-xL, and the proapoptotic protein, Bax, and consequently inhibits Caspase-3 activation. Thus, we speculated that p38 MAPK/p90RSK/Bad and the Bcl-2 family may be involved in the neuroprotective effect of cPKC and that the role of cPKC in apoptosis can be further attributed to the Caspase-3 signaling pathway. However, further studies are needed to explore whether cPKC can serve as a biomarker for clinical diagnosis and therapy in ischemic stroke.
Conclusion
In summary, we concluded that cPKCγ mediates Caspase-9-initiated apoptosis through the activation of the phosphorylation levels of p38 MAPK/p90RSK/Bad in OGD-treated neurons. Therefore, the novel concept of cPKCγ-modulating apoptosis may be a potential therapeutic target for ischemic stroke.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Deng Y, Chen D, Wang L, Gao F, Jin B, Lv H, Zhang G, Sun X, Liu L, Mo D, Ma N, Song L, Huo X, Yan T, Miao Z (2019) Silencing of long noncoding RNA nespas aggravates microglial cell death and neuroinflammation in ischemic stroke. Stroke 50:1850–1858
Candelario-Jalil E, Surojit P (2021) Impact of aging and comorbidities on ischemic stroke outcomes in preclinical animal models: a translational perspective. Exp Neurol 335:113494
Zeng S, Zhao Z, Zheng S, Wu M, Song X, Li Y, Zheng Y, Liu B, Chen L, Gao C, Liu H (2021) The E3 ubiquitin ligase TRIM31 is involved in cerebral ischemic injury by promoting degradation of TIGAR. Redox Biol 45:102058
Yagi K, Shirai Y, Hirai M, Sakai N, Saito N (2004) Phospholipase A2 products retain a neuron specific gamma isoform of PKC on the plasma membrane through the C1 domain–a molecular mechanism for sustained enzyme activity. Neurochem Int 45:39–47
Wei H, Li Y, Han S, Liu S, Zhang N, Zhao L, Li S, Li J (2016) cPKCγ-modulated autophagy in neurons alleviates ischemic injury in brain of mice with ischemic stroke through Akt-mTOR pathway. Transl Stroke Res 7:497–511
Zhang YP, Zhang Y, Xiao ZB, Zhang YB, Zhang J, Li ZQ, Zhu YB (2018) CFTR prevents neuronal apoptosis following cerebral ischemia reperfusion via regulating mitochondrial oxidative stress. J Mol Med 96:611–620
Eefting F, Rensing B, Wigman J, Pannekoek WJ, Liu WM, Cramer MJ, Lips DJ, Doevendans PA (2004) Role of apoptosis in reperfusion injury. Cardiovasc Res 61:414–426
He R, Jiang Y, Shi Y, Liang J, Zhao L (2020) Curcumin-laden exosomes target ischemic brain tissue and alleviate cerebral ischemia-reperfusion injury by inhibiting ROS-mediated mitochondrial apoptosis. Mater Sci Eng C 117:111314
Garcia-Bonilla L, Brea D, Benakis C, Lane DA, Murphy M, Moore J, Racchumi G, Jiang X, Iadecola C, Anrather J (2018) Endogenous protection from ischemic brain injury by preconditioned monocytes. J Neurosci 38:6722–6736
Chou WH, Messing RO (2005) Protein kinase C isozymes in stroke. Trends Cardiovasc Med 15:47–51
Zhang N, Zhu H, Han S, Sui L, Li J (2018) cPKCγ alleviates ischemic injury through modulating synapsin Ia/b phosphorylation in neurons of mice. Brain Res Bull 142:156–162
Krupiński J, Slevin MA, Kumar P, Gaffney J, Kałuza J (1998) Protein kinase C expression and activity in the human brain after ischaemic stroke. Acta Neurobiol Exp 58:13–21
Liu Y, Li J, Yang J, Ji F, Bu X, Zhang N, Zhang B (2008) Inhibition of PKCgamma membrane translocation mediated morphine preconditioning-induced neuroprotection against oxygen–glucose deprivation in the hippocampus slices of mice. Neurosci Lett 444:87–91
Matsumoto S, Murozono M, Nagaoka D, Matsuoka S, Takeda A, Narita H, Watanabe S, Isshiki A, Watanabe Y (2008) Isoflurane inhibits protein kinase Cgamma and calcium/calmodulin dependent protein kinase II-alpha translocation to synaptic membranes in ischemic mice brains. Neurochem Res 33:2302–2309
Li X, Zheng L, Xia Q, Liu L, Mao M, Zhou H, Zhao Y, Shi J (2019) A novel cell-penetrating peptide protects against neuron apoptosis after cerebral ischemia by inhibiting the nuclear translocation of annexin A1. Cell Death Differ 26:260–275
Korkmaz-Icöz S, Zhou P, Guo Y, Loganathan S, Brlecic P, Radovits T, Sayour AA, Ruppert M, Veres G, Karck M, Szabó G (2021) Mesenchymal stem cell-derived conditioned medium protects vascular grafts of brain-dead rats against in vitro ischemia/reperfusion injury. Stem Cell Res Ther 12:144
Xiang Y, Zhang Y, Xia Y, Zhao H, Liu A, Chen Y (2020) LncRNA MEG3 targeting miR-424-5p via MAPK signaling pathway mediates neuronal apoptosis in ischemic stroke. Aging 12:3156–3174
Wesley UV, Sutton IC, Cunningham K, Jaeger JW, Phan AQ, Hatcher JF, Dempsey RJ (2021) Galectin-3 protects against ischemic stroke by promoting neuro-angiogenesis via apoptosis inhibition and Akt/Caspase regulation. J Cereb Blood Flow Metab 41:857–873
Lien LM, Lin KH, Huang LT, Tseng MF, Chiu HC, Chen RJ, Lu WJ (2017) Licochalcone a prevents platelet activation and thrombus formation through the inhibition of PLCγ2-PKC, Akt, and MAPK pathways. Int JMol Sci 18:1500
Qi Z, Qi S, Gui L, Shen L, Feng Z (2016) Daphnetin protects oxidative stress-induced neuronal apoptosis via regulation of MAPK signaling and HSP70 expression. Oncol Lett 12:1959–1964
Cheng CY, Lin JG, Su SY, Tang NY, Kao ST, Hsieh CL (2014) Electroacupuncture-like stimulation at Baihui and Dazhui acupoints exerts neuroprotective effects through activation of the brain-derived neurotrophic factor-mediated MEK1/2/ERK1/2/p90RSK/bad signaling pathway in mild transient focal cerebral ischemia in rats. BMC Complement Altern Med 14:92
Gendron TF, Badi MK, Heckman MG, Jansen-West KR, Vilanilam GK, Johnson PW, Burch AR, Walton RL, Ross OA, Brott TG, Miller TM, Berry JD, Nicholson KA, Wszolek ZK, Oskarsson BE, Sheth KN, Sansing LH, Falcone GJ, Cucchiara BL, Meschia JF, Petrucelli L (2020) Plasma neurofilament light predicts mortality in patients with stroke. Sci Transl Med 12(569):eaay1913
Morris RS, Simon Jones P, Alawneh JA, Hong YT, Fryer TD, Aigbirhio FI, Warburton EA, Baron JC (2018) Relationships between selective neuronal loss and microglial activation after ischaemic stroke in man. Brain 141:2098–2111
Puyal J, Ginet V, Clarke PG (2013) Multiple interacting cell death mechanisms in the mediation of excitotoxicity and ischemic brain damage: a challenge for neuroprotection. Prog Neurobiol 105:24–48
Ma Q, Zhang LJEn (2018) C-type natriuretic peptide functions as an innate neuroprotectant in neonatal hypoxic-ischemic brain injury in mouse via natriuretic peptide receptor 2. Exp neurol 304:58–66
Martin RL, Lloyd HG, Cowan AI (1994) The early events of oxygen and glucose deprivation: setting the scene for neuronal death? Trends neurosci 17:251–257
Olivares-Hernández JD, Balderas-Márquez JE, Carranza M, Luna M, Martínez-Moreno CG, Arámburo C (2021) Growth hormone (GH) enhances endogenous mechanisms of neuroprotection and neuroplasticity after oxygen and glucose deprivation injury (OGD) and reoxygenation (OGD/R) in chicken hippocampal cell cultures. Neural Plast 2021:9990166
Coimbra-Costa D, Alva N, Duran M, Carbonell T, Rama R (2017) Oxidative stress and apoptosis after acute respiratory hypoxia and reoxygenation in rat brain. Redox Biol 12:216–225
Kesaraju S, Schmidt-Kastner R, Prentice HM, Milton SL (2009) Modulation of stress proteins and apoptotic regulators in the anoxia tolerant turtle brain. J Neurochem 109:1413–1426
Zhang D, Han S, Wang S, Luo Y, Zhao L, Li J (2017) cPKCγ-mediated down-regulation of UCHL1 alleviates ischaemic neuronal injuries by decreasing autophagy via ERK-mTOR pathway. J Cell Mol Med 21:3641–3657
Jiang M, Li J, Peng Q, Liu Y, Liu W, Luo C, Peng J, Li J, Yung KK, Mo Z (2014) Neuroprotective effects of bilobalide on cerebral ischemia and reperfusion injury are associated with inhibition of pro-inflammatory mediator production and down-regulation of JNK1/2 and p38 MAPK activation. J Neuroinflamm 11:167
Wu X, Li L, Zhang L, Wu J, Zhou Y, Zhou Y, Zhao Y, Zhao J (2015) Inhibition of thioredoxin-1 with siRNA exacerbates apoptosis by activating the ASK1-JNK/p38 pathway in brain of a stroke model rats. Brain Res 1599:20–31
Cheng CY, Ho TY, Hsiang CY, Tang NY, Hsieh CL, Kao ST, Lee YC (2017) Angelica sinensis exerts angiogenic and anti-apoptotic effects against cerebral ischemia-reperfusion injury by activating p38MAPK/HIF-1[Formula: see text]/VEGF-A signaling in rats. Am J Chin Med 45:1683–1708
Kovalska M, Kovalska L, Pavlikova M, Janickova M, Mikuskova K, Adamkov M, Kaplan P, Tatarkova Z, Lehotsky J (2012) Intracellular signaling MAPK pathway after cerebral ischemia-reperfusion injury. NeurochemRes 37:1568–1577
Liu J, Wang Q, Yang S, Huang J, Feng X, Peng J, Lin Z, Liu W, Tao J, Chen L (2018) Electroacupuncture inhibits apoptosis of peri-ischemic regions via modulating p38, extracellular signal-regulated kinase (ERK1/2), and c-Jun N Terminal Kinases (JNK) in cerebral ischemia-reperfusion-injured rats. Med Sci Monit 24:4395–4404
Heo KS, Le NT, Cushman HJ, Giancursio CJ, Chang E, Woo CH, Sullivan MA, Taunton J, Yeh ET, Fujiwara K, Abe J (2015) Disturbed flow-activated p90RSK kinase accelerates atherosclerosis by inhibiting SENP2 function. J Clin Invest 125:1299–1310
Sun XC, Xian XH, Li WB, Li L, Yan CZ, Li QJ, Zhang M (2010) Activation of p38 MAPK participates in brain ischemic tolerance induced by limb ischemic preconditioning by up-regulating HSP 70. Exp Neurol 224:347–355
Hu XL, Olsson T, Johansson IM, Brännström T, Wester P (2004) Dynamic changes of the anti- and pro-apoptotic proteins Bcl-w, Bcl-2, and Bax with Smac/Diablo mitochondrial release after photothrombotic ring stroke in rats. Eur J Neurosci 20:1177–1188
Gross A, Jockel J, Wei MC, Korsmeyer SJ (1998) Enforced dimerization of BAX results in its translocation, mitochondrial dysfunction and apoptosis. EMBO J 17:3878–3885
Li Z, Guo D, Yin X, Ding S, Shen M, Zhang R, Wang Y, Xu R (2020) Zinc oxide nanoparticles induce human multiple myeloma cell death via reactive oxygen species and Cyt-C/Apaf-1/Caspase-3 signaling pathway in vitro. Biomed Pharmacother 33:723–728
Funding
This work was supported by the National Natural Science Foundation of China (Grant No. 81960225), the Second Hospital of Lanzhou University “Cuiying Science and Technology Innovation” Plan for the Applied Basic Research-youth Program (Grant No. CY2018-QN04), the Higher Education Innovation Capacity Enhancement Project of Gansu Province (Grant No. 2019B-016), the National Innovation and Entrepreneurship Training Program for College Students (Grant No. 202110730213), and the Cuiying Scientific Training Program for Undergraduates of Lanzhou University Second Hospital (Grant No. CYXZ2021-18).
Author information
Authors and Affiliations
Contributions
WHP conceived and performed the experiment. PZF performed the experiment, and wrote the manuscript. SKM, ZPH, CL, HJA, CH, and LJM revised the manuscript. All the authors have revised the full manuscript and confirmed submission.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All experiments were approved by Animal Care and Use Committee in Lanzhou University Second Hospital.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wei, Hp., Peng, Zf., Shao, Km. et al. cPKCγ Inhibits Caspase-9-Initiated Neuronal Apoptosis in an Ischemia Reperfusion Model In Vitro Through p38 MAPK-p90RSK-Bad Pathway. Neurochem Res 48, 362–374 (2023). https://doi.org/10.1007/s11064-022-03747-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-022-03747-1









