Abstract
Silibinin has been widely used to treat liver diseases due to its antioxidant activity. However, the effects of silibinin on the central nervous system have not been thoroughly investigated. The pathological hallmarks of Alzheimer’s disease are the accumulation of amyloid β protein, development of neurofibrillary tangles and increased oxidative stress, which ultimately lead to irreversible neuronal loss and cognitive impairment. Our findings show that silibinin ameliorated memory impairments in APP/PS1 mice in the Morris water maze via suppression of oxidative stress and inhibition of apoptosis. Treatment with silibinin reduced malondialdehyde content level and increased glutathione and superoxide dismutase activity in APP/PS1 mice. A terminal deoxynucleotidyl transferase dUTP nick end labeling assay revealed an anti-apoptotic effect of silibinin. Silibinin suppressed the activation of caspase-3 by inhibiting Jun N-terminal kinase phosphorylation and the downstream hippocampal Bax/Bcl-2 ratio. Silibinin treatment significantly increased levels of synaptophysin and PSD95 in APP/PS1 transgenic mice. These results suggest that silibinin could be a potential therapeutic agent for the treatment of Alzheimer’s disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
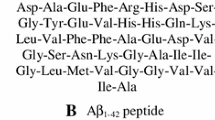
Alzheimer’s disease (AD) is the most common cause of dementia. Approximately 5% of AD cases are caused by missense mutations; however, the causes of sporadic AD remain unclear. In addition to the accumulation of amyloid β protein (Aβ) and neurofibrillary tangles (NFT), there are constant evidence [1] of reactive oxygen species (ROS)—mediated injury plays an important role in the pathogenesis of AD [2, 3]. Aβ with a critical methionine residue at position 35 [4] is markedly elevated in AD or AD-like models [5], and may increase ROS generation and induce oxidative stress [3]. In addition to the pro-oxidative role of Aβ, oxidative stress creates positive feedback on APP levels and on its proteolytic pathway. Oxidative stress can increase APP levels and modulate the activity and levels of key enzymes such as β-secretase and γ-secretase. Oxidative stress is closely correlated with amyloid pathology and tau pathology forming vicious pathophysiological cycles [6] that induce mitochondrial dysfunction and promote metal toxicity, ultimately causing cell malfunction and progressive neuronal loss, predominantly by apoptosis. Excess cellular levels of ROS cause damage to lipids, membranes and organelles [7], which can lead to activation of cell death processes such as apoptosis. Aβ induces neuronal apoptosis by releasing calcium from the endoplasmic reticulum [8] or by activating Jun N-terminal kinase (JNK) and the downstream Bcl-2 family [9, 10], ultimately leading to caspase activation and apoptotic death.
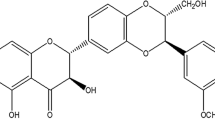
Silybum marianum L. is a medicinal plant of Asian origin that is widely used in traditional European medicine [11]. Silibinin is the major pharmacologically active compound of silymarin, a flavonoid complex obtained from the seeds of S. marianum L. Historically, silibinin has been used to treat liver diseases due to its anti-inflammatory and antioxidative hepatoprotective properties [12]. Previous studies have shown that silibinin can prevent memory impairment induced by intrastriatal MPP + injection, intracerebroventricular injection of LPS, intracerebral administration of streptozotocin, and intracerebroventricular injection of Aβ25–35 [13,14,15,16]. In the present study, we investigated whether silibinin prevents memory impairment and oxidative stress events in APP/PS1 transgenic mice. Further, we examined the effects of silibinin on apoptosis and synaptic protection in vivo.
Methods
Animals and Drug Administration
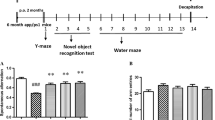
The APP/PS1 transgenic mice were procured from HFK Bioscience Co., Ltd., Beijing, China. These mice express a human APP containing the K595N/M596L Swedish mutations and a mutant human PS1 carrying the exon 9-deleted variant with a C57BL/6J background [17]. We adapt 5 months male APP/PS1 mice in our study, sex- and age-matched C57BL/6J mice as control. Animals were housed in a temperature-controlled (22 ± 2 °C) and humidity-controlled (60 ± 5%) environment with a 12-h light–dark cycle and had free access to food and water. APP/PS1 mice were randomly divided into model, memantine, and two silibinin treatment groups. Each group had 10 animals. Either 100 or 200 mg/kg of silibinin (Green Biological Development Co., Ltd., Panjin, China) was administered orally once per day to APP/PS1 mice. C57BL/6J mice and model APP/PS1 mice were administered vehicle by gavage. Drug administration started from animals 5 months old continued 8 consecutive weeks. Animal studies were performed in accordance with the PR China legislation on the use and care of laboratory animals and with the guidelines established by the Institute for Experimental Animals of Shenyang Medical College.
Morris Water Maze Test
Mice behavior was tested after 8 weeks of drug administration. As described in our previous report [18], the Morris water maze (MWM) test was performed to assess spatial learning and memory. The MWM consisted of a black circular tank (diameter = 100 cm; height = 50 cm) filled with water (25 ± 1 °C and 30 cm in depth). A black round platform (diameter = 8 cm) was placed 1 cm below the surface of water in a fixed position. During the acquisition trial phase, mice were trained twice a day for 5 consecutive days (days 1–5). The mice were given a maximum time of 60 s to find the hidden platform and were allowed to stay on it for 10 s. If a mouse failed to locate the platform within 60 s, it was guided to the hidden platform by the experimenter and allowed to rest on it for 10 s. Escape latency and swimming distance were recorded. During the probe trial phase, which was 24 h after the last acquisition trial, the escape platform was removed and each mouse was allowed to explore the pool for 60 s. The time spent in the target quadrant and platform-site crossovers were measured using a computer system with a video camera.
Measurement of GSH and SOD Activity and MDA Content Level
Cortex tissues were collected from the sacrificed animals after anesthesia. The cortex samples were removed on an ice-cold box. Tissues were homogenized in PBS. After centrifuging at 3000×g for 20 min, the protein concentration of the supernatant was tested by the BCA Assay Kit (Beyotime, Jiangsu, China). The concentrations of GSH, SOD and MDA content level were measured by standard assay ELISA kits (Elabscience, Wuhan, China) according to the manufacturer’s instructions.
Western Blot Analysis
Mice were decapitated under Chloral hydrate anesthesia. The hippocampus was homogenized and then centrifuged at 12,000×g for 20 min at 4 °C. The protein concentration was determined using a Bicinchoninic Acid Protein Assay Kit (Kangwei Biotechnology, China). Proteins (25–50 μg of protein per lane) were run on an 8 or 10% SDS poly-acrylamide gel and primary antibodies included anti-synaptophysin (1:2000 Abcam), anti-PSD95 (1:2000 Abcam), anti-JNK (1:1000 Santa Cruz), anti-p-JNK (1:800 Santa Cruz), anti-Bcl-2 (1:500 Santa Cruz), anti-Bax (1:500 Santa Cruz), anti-Caspase-3 (1:1000 Cell Signaling Technology), anti-Cleaved Caspase-3 (1:400 Cell Signaling Technology). Protein bands were visualized with an ECL Western blot kit (Kangwei Biotechnology, China). The intensity was quantified by densitometry using Quantity One 4.6.2 software (Bio-Rad, Hercules, CA, USA) and corrected with the corresponding β-actin level. The results are expressed as a percentage of the control.
Terminal Deoxynucleotidyl Transferase dUTP Nick End Labeling (TUNEL)
After MWM testing, mice were anaesthetized and then perfused transcardially with heparinized 0.9% saline followed by phosphate buffer (pH 7.4) containing 4% formaldehyde. Their brains were removed and immersed in 4% paraformaldehyde. TUNEL staining was performed in hippocampal paraffin sections (5 μm) using the In Situ Cell Death Detection Kit (Roche, Germany). Briefly, after deparaffinization, slices were incubated with proteinase K (20 μg/ml) for 10 min at room temperature and then their endogenous peroxidase activity was quenched by incubating in 3% H2O2 in PBS for 10 min. Sections were subsequently incubated in equilibration buffer for 30 min at 37 °C, followed by the TUNEL reaction mixture for 1 h at 37 °C. After a 5 min PBS wash, sections were incubated in peroxidase, detected with diaminobenzidine (DAB) solution, and counterstained with hematoxylin. The results were calculated as a percentage of the total number of neurons in the CA1 of the hippocampus. For each animal, four sections were quantified using high power fields objective (×40).
Statistical Analysis
Statistical analysis was performed using one-way or two-way ANOVA followed by Fisher’s least significant difference (LSD) multiple comparisons test (p < 0.05 was significant) in SPSS 17.0 software. The results are presented as the mean ± SEM.
Results
Silibinin Ameliorates Memory Impairments in APP/PS1 Transgenic Mice in the MWM
There were significant differences in MWM performance during the acquisition trail phase. As shown in Fig. 1a, b, model mice showed longer swimming distances and escape latencies than control mice (p < 0.01); however, treatment with silibinin caused significant decreases in escape latency (p < 0.05 in day 3, p < 0.01 in day 4 and p < 0.01 in day 5) and swimming distance (p < 0.001 in day 4 and p < 0.01 in day 5). During probe trial testing (Fig. 1c, d), the silibinin-treated mice showed an increased number of platform crossings (p < 0.01) and spent more time in the target quadrant (p < 0.05 in 100 mg/kg group and p < 0.01 in 200 mg/kg group) compared to model mice. The mice treated with memantine, a positive control, showed decreased escape latencies (p < 0.05) and swimming distances (p < 0.05) in the acquisition phase and exhibited significantly prolonged time in the target quadrant (p < 0.01) and increased number of platform crossings (p < 0.05) in the probe trial phase compared with model mice.
Morris water maze test performed to assess learning abilities of mice. Escape latency (a), swimming distance (b). Mean time spent in the trained quadrant (c) and mean number of platform crossings (d) during the probe trial test. The path traces in control (e), model (f), memantine (g), silibinin 100 mg/kg (h), silibinin 200 mg/kg (i) in probe trial test. Data are presented as the mean ± SEM (n = 10 mice in each experimental group; *p < 0.05, **p < 0.01 and ***p < 0.001 compared with model mice, ##p < 0.01 and ###p < 0.001 compared with control mice)
Measurement of Oxidative Stress Markers
As shown in Table 1 the model group MDA expression increased, which was significantly decreased by silibinin group (100 mg/kg p < 0.01 and 200 mg/kg p < 0.001). Expression levels of SOD and GSH of silibinin group increased in the cortex compared with model group. SOD (p < 0.05), GSH (100 mg/kg, p < 0.05 and 200 mg/kg p < 0.01).
Apoptosis in the Hippocampus of APP/PS1 Transgenic Mice and Anti-Apoptotic Effect of Silibinin
TUNEL assay was performed to detect DNA fragmentation. No or few TUNEL-positive cells (<2%) were seen in the CA1 region of control mice. In contrast, APP/PS1 group slices showed prominent TUNEL staining compared with control slices (p < 0.001, Fig. 2b). The TUNEL-positive cells exhibited shrinkage of the nucleus and chromatin condensation. Silibinin treatment significantly decreased the population of TUNEL-positive cells (100 mg/kg, p < 0.001; 200 mg/kg, p < 0.001, Fig. 2b) in the CA1 region of APP/PS1 mice.
Silibinin attenuates apoptosis in the hippocampus of APP/PS1 transgenic mice. a Representative TUNEL staining in the CA1 region of hippocampus, arrow indicates the TUNEL-positive cells or apoptotic bodies which were stained brown and characterized by a round and shrunken morphology (sections were quantified using high power fields objective 40). b Quantification of TUNEL-positive cells in each group. Results were calculated as the percentage of the total number of neurons. Data are presented as the mean ± SEM from five animals per group with four sections for each animal. ###p < 0.001 versus the control group, **p < 0.01 versus the model group
Silibinin Suppresses the Activation of Caspase-3 by Inhibiting JNK Phosphorylation
Activation of caspase-3 is regarded as a proximate mediator of apoptosis. Therefore, we examined whether silibinin affected cleaved caspase-3 levels in the hippocampus of APP/PS1 mice. The cleaved caspase-3/caspase-3 ratio in APP/PS1 mice increased 1.36-fold compared to the control group. After 8 weeks of silibinin treatment, this ratio decreased (100 mg/kg, p < 0.05; 200 mg/kg p < 0.01, Fig. 3) compared to the model group. The ratio of Bax/Bcl-2 also increased 1.77-fold in APP/PS1 mice compared to control mice. However, silibinin treatment decreased the ratio of Bax/Bcl-2 (100 mg/kg, p < 0.05; 200 mg/kg p < 0.001, Fig. 3). Furthermore, we evaluated the activation of JNK, which plays a critical role in apoptotic pathways. Phosphorylation of JNK in APP/PS1 mice was increased by 45% compared to the control group; however, silibinin treatment significantly decreased the p-JNK/JNK ratio (100 mg/kg, p < 0.01; 200 mg/kg p < 0.01, Fig. 3).
Representative Western blots showing expression levels of p-JNK, JNK, Bax, Bcl-2, cleaved caspase-3 and caspase-3 in the hippocampus of APP/PS1 mice. After 8 weeks of treatment, silibinin significantly decreased the ratio of p-JNK/JNK, Bax/Bcl-2 and cleaved caspase-3/caspase-3 in the hippocampus of APP/PS1 mice. Data are presented as the mean ± SEM from five animals per group. ###p < 0.001 versus the control group; *p < 0.05, **p < 0.01 and ***p < 0.001 versus the model group
Protection of Synapses in APP/PS1 Transgenic Mice
Protein expression levels of synaptophysin and PSD95 were evaluated by Western blot. In the hippocampus of APP/PS1 mice, synaptophysin and PSD95 levels decreased significantly (p < 0.001, Fig. 4) compared to controls. However, silibinin treatment significantly increased levels of synaptophysin (100 mg/kg, p < 0.01; 200 mg/kg, p < 0.001, Fig. 4) and PSD95 (p < 0.001, Fig. 4).
Silibinin treatment increased levels of synaptophysin and PSD95 in the hippocampus of APP/PS1 mice. Representative Western blots showing levels of synaptophysin and PSD95. Data are presented as the mean ± SEM from five animals per group. ###p < 0.001 versus the control group; **p < 0.01 and ***p < 0.001 versus the model group
Discussion
Previous studies have indicated that silibinin could significantly ameliorate memory impairment in AD animal models [14,15,16] through inhibition of acetylcholinesterase activity and Aβ aggregation and prevention of neuronal death. Our data show that silibinin-mediated attenuation of learning and memory impairment may be related to anti-apoptotic and antioxidative effects in APP/PS1 transgenic mice. Oxidative stress plays a crucial role in the pathogenesis of AD. In the AD brain, increased oxidative stress has been demonstrated using DNA, RNA, and protein oxidation markers and lipid peroxidation [19]. In the human brain, polyunsaturated fatty acids are abundant and highly oxidizable; however, the AD brain has relatively low levels of antioxidants. Free radical oxidation of polyunsaturated fatty acids leads to the formation of MDA [19]. Increased levels of MDA have been identified in the AD brain [20, 21]. Moreover, significant decreases in glutathione levels and the activity of antioxidant enzymes such as superoxide dismutase were also reported in the AD brain [22]. At 3 months of age and it consistently increases with age [23], APP/PS1 mice showed increased oxidative stress which was consistent with our findings. Our results show that treatment with silibinin reduced MDA content level and increased GSH and SOD activity in APP/PS1 mice, which is consistent with previous studies [24] that silibinin increased GSH levels and decreased MDA levels in the Aβ25–35-injected rats. Our findings show that silibinin acted as a suppressor of oxidative stress, which is consistent with previous reports [12].
JNKs belong to the superfamily of MAP-kinases [25] and play a critical role in apoptotic pathways. Activation of JNKs can upregulate pro-apoptotic genes or directly modulate the mitochondrial pro- and anti-apoptotic singing pathway [26, 27]. A potential mechanism of pro-apoptotic signaling is that JNK increases p53 stability and transcriptional activation and that JNK potentiates the ability of p53 to initiate programmed cell death [28]. Expression of p53 upregulates the Bax gene, which encodes two proteins: Bcl-2, which enhances cell survival, and Bax, which promotes cell death. Alteration of the Bax/Bcl-2 ratio causes the release of cytochrome c from mitochondria into the cytosol, which increases the expression of cleaved caspase-3. Cleaved caspase-3 is regarded as a proximate mediator of apoptosis [29].
Silibinin may improve memory impairment in AD animal models [13,14,15,16] by potentially decreasing the extent of neuronal apoptosis caused by oxidative stress [30]. As reported in pretreatment of silibinin significantly inhibited OGD/re-oxygenation-induced necrosis and apoptosis of neuronal cells [31]. However, our study shows that silibinin attenuated apoptosis in vivo in the hippocampus of APP/PS1 transgenic mice and decreased activation of caspase-3 and the Bax/Bcl-2 ratio. The anti-apoptotic effect of silibinin may be caused by its inhibition of JNK phosphorylation. In a model of PD, silibinin protected dopaminergic neurons and inhibited JNK phosphorylation [32]. In our previous study, silibinin decreased the expression levels of phosphorylated JNK [33]. In the present study, silibinin decreased the phosphorylation of JNK and the ratio of Bax/Bcl-2. Moreover, the anti-apoptotic effect of silibinin caused an increase in the protein expression of SYP and PSD95.
In the present study, we showed that silibinin inhibits apoptotic signaling in vivo in APP/PS1 transgenic mice. Neuronal and synaptic protection by silibinin occurs via inhibition of the JNK/Bax/caspase-3 signaling pathway. Ultimately, silibinin attenuates learning and memory deficits via suppression of oxidative stress and inhibition of apoptosis in APP/PS1 transgenic mice.
References
Pratico D, Sung S (2004) Lipid peroxidation and oxidative imbalance: Early functional events in Alzheimer’s disease. J Alzheimers Dis 6:171–175
Pourkhodadad S, Alirezaei M, Moghaddasi M, Ahmadvand H, Karami M, Delfan B, Khanipour Z (2016) Neuroprotective effects of oleuropein against cognitive dysfunction induced by colchicine in hippocampal CA1 area in rats. J Physiol Sci 66:397–405
Pratico D (2008) Oxidative stress hypothesis in Alzheimer’s disease: a reappraisal. Trends Pharmacol Sci 29:609–615
Holcomb L, Gordon MN, McGowan E, Yu X, Benkovic S, Jantzen P, Wright K, Saad I, Mueller R, Morgan D, Sanders S, Zehr C, O’Campo K, Hardy J, Prada CM, Eckman C, Younkin S, Hsiao K, Duff K (1998) Accelerated Alzheimer-type phenotype in transgenic mice carrying both mutant amyloid precursor protein and presenilin 1 transgenes. Nat Med 4:97–100
Butterfield DA, Boyd-Kimball D (2005) The critical role of methionine 35 in Alzheimer’s amyloid beta-peptide (1–42)-induced oxidative stress and neurotoxicity. Biochim Biophys Acta 1703:149–156
Chen Z, Zhong C (2014) Oxidative stress in Alzheimer’s disease. Neurosci Bull 30:271–281
Redza-Dutordoir M, Averill-Bates DA (2016) Activation of apoptosis signalling pathways by reactive oxygen species. Biochim Biophys Acta 1863:2977–2992
Ferreiro E, Oliveira CR, Pereira CM (2008) The release of calcium from the endoplasmic reticulum induced by amyloid-beta and prion peptides activates the mitochondrial apoptotic pathway. Neurobiol Dis 30:331–342
Morishima Y, Gotoh Y, Zieg J, Barrett T, Takano H, Flavell R, Davis RJ, Shirasaki Y, Greenberg ME (2001) Beta-amyloid induces neuronal apoptosis via a mechanism that involves the c-Jun N-terminal kinase pathway and the induction of Fas ligand. J Neurosci 21:7551–7560
Yao M, Nguyen TV, Pike CJ (2005) Beta-amyloid-induced neuronal apoptosis involves c-Jun N-terminal kinase-dependent downregulation of Bcl-w. J Neurosci 25:1149–1158
Morazzoni P, Bombardelli E (1995) Silybum marianum (Carduus marianum). Fitoterapia 66:3–42
Souza CO, Peracoli MT, Weel IC, Bannwart CF, Romao M, Nakaira-Takahagi E, Medeiros LT, Silva MG, Peracoli JC (2012) Hepatoprotective and anti-inflammatory effects of silibinin on experimental preeclampsia induced by L-NAME in rats. Life Sci 91:159–165
Geed M, Garabadu D, Ahmad A, Krishnamurthy S (2014) Silibinin pretreatment attenuates biochemical and behavioral changes induced by intrastriatal MPP+ injection in rats. Pharmacol Biochem Behav 117:92–103
Joshi R, Garabadu D, Teja GR, Krishnamurthy S (2014) Silibinin ameliorates LPS-induced memory deficits in experimental animals. Neurobiol Learn Mem 116:117–131
Tota S, Kamat PK, Shukla R, Nath C (2011) Improvement of brain energy metabolism and cholinergic functions contributes to the beneficial effects of silibinin against streptozotocin induced memory impairment. Behav Brain Res 221:207–215
Lu P, Mamiya T, Lu LL, Mouri A, Niwa M, Hiramatsu M, Zou LB, Nagai T, Ikejima T, Nabeshima T (2009) Silibinin attenuates amyloid beta(25–35) peptide-induced memory impairments: implication of inducible nitric-oxide synthase and tumor necrosis factor-alpha in mice. J Pharmacol Exp Ther 331:319–326
Jankowsky JL, Slunt HH, Gonzales V, Jenkins NA, Copeland NG, Borchelt DR (2004) APP processing and amyloid deposition in mice haplo-insufficient for presenilin 1. Neurobiol Aging 25:885–892
Xu Q, Ji XF, Chi TY, Liu P, Jin G, Gu SL, Zou LB (2015) Sigma 1 receptor activation regulates brain-derived neurotrophic factor through NR2A-CaMKIV-TORC1 pathway to rescue the impairment of learning and memory induced by brain ischaemia/reperfusion. Psychopharmacology 232:1779–1791
Butterfield DA, Reed T, Newman SF, Sultana R (2007) Roles of amyloid beta-peptide-associated oxidative stress and brain protein modifications in the pathogenesis of Alzheimer’s disease and mild cognitive impairment. Free Radic Biol Med 43:658–677
Sultana R, Perluigi M, Allan Butterfield D (2013) Lipid peroxidation triggers neurodegeneration: a redox proteomics view into the Alzheimer disease brain. Free Radic Biol Med 62:157–169
Lovell MA, Ehmann WD, Butler SM, Markesbery WR (1995) Elevated thiobarbituric acid-reactive substances and antioxidant enzyme activity in the brain in Alzheimer’s disease. Neurology 45:1594–1601
Venkateshappa C, Harish G, Mahadevan A, Srinivas Bharath MM, Shankar SK (2012) Elevated oxidative stress and decreased antioxidant function in the human hippocampus and frontal cortex with increasing age: implications for neurodegeneration in Alzheimer’s disease. Neurochem Res 37:1601–1614
Hamilton A, Holscher C (2012) The effect of ageing on neurogenesis and oxidative stress in the APP (swe)/PS1 (deltaE9) mouse model of Alzheimer’s disease. Brain Res 1449:83–93
Song X, Zhou B, Cui L, Lei D, Zhang P, Yao G, Xia M, Hayashi T, Hattori S, Ushiki-Kaku Y, Tashiro SI, Onodera S, Ikejima T (2016) Silibinin ameliorates Abeta25-35-induced memory deficits in rats by modulating autophagy and attenuating neuroinflammation as well as oxidative stress. Neurochem Res 42:1073–1083
Smith WW, Gorospe M, Kusiak JW (2006) Signaling mechanisms underlying Abeta toxicity: potential therapeutic targets for Alzheimer’s disease. CNS Neurol Disord Drug Targets 5:355–361
Oleinik NV, Krupenko NI, Krupenko SA (2007) Cooperation between JNK1 and JNK2 in activation of p53 apoptotic pathway. Oncogene 26:7222–7230
Dhanasekaran DN, Reddy EP (2008) JNK signaling in apoptosis. Oncogene 27:6245–6251
Fuchs SY, Adler V, Pincus MR, Ronai Z (1998) MEKK1/JNK signaling stabilizes and activates p53. Proc Natl Acad Sci USA 95:10541–10546
Ko LJ, Prives C (1996) p53: puzzle and paradigm. Genes Dev 10:1054–1072
Wang M, Li YJ, Ding Y, Zhang HN, Sun T, Zhang K, Yang L, Guo YY, Liu SB, Zhao MG, Wu YM (2016) Silibinin prevents autophagic cell death upon oxidative stress in cortical neurons and cerebral ischemia-reperfusion injury. Mol Neurobiol 53:932–943
Xie Z, Ding SQ, Shen YF (2014) Silibinin activates AMP-activated protein kinase to protect neuronal cells from oxygen and glucose deprivation-re-oxygenation. Biochem Biophys Res Commun 454:313–319
Lee Y, Chun HJ, Lee KM, Jung YS, Lee J (2015) Silibinin suppresses astroglial activation in a mouse model of acute Parkinson’s disease by modulating the ERK and JNK signaling pathways. Brain Res 1627:233–242
Jin G, Bai D, Yin S, Yang Z, Zou D, Zhang Z, Li X, Sun Y, Zhu Q (2016) Silibinin rescues learning and memory deficits by attenuating microglia activation and preventing neuroinflammatory reactions in SAMP8 mice. Neurosci Lett 629:256–261
Acknowledgements
This study was supported by Subject of Liaoning natural science fund (20170540880), Liaoning education department project (L2014409), Shenyang science and Technology Bureau subject of China (F13-220-9-27).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bai, D., Jin, G., Yin, S. et al. Antioxidative and Anti-Apoptotic Roles of Silibinin in Reversing Learning and Memory Deficits in APP/PS1 Mice. Neurochem Res 42, 3439–3445 (2017). https://doi.org/10.1007/s11064-017-2389-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11064-017-2389-3